Optimizing Prehospital Asthma Care: Management and Interventions
VerifiedAdded on 2024/07/22
|9
|1311
|98
Report
AI Summary
This report provides a detailed overview of managing asthma in the prehospital environment, emphasizing strategies to reduce hospital admissions. It begins by defining asthma as a chronic inflammatory disease affecting the airways and lungs, highlighting the importance of effective prehospital management to prevent exacerbations. The report discusses the causes of asthma, including allergies, infections, and environmental irritants, and explains the pathophysiology involving inflammation, airflow obstruction, and increased airway responsiveness. Key management and treatment approaches include periodic assessment, written action plans, allergen reduction, and pharmacological therapies such as corticosteroids and inhaled beta-agonists. The report concludes that implementing these strategies can significantly decrease hospitalization rates for asthma patients, underscoring the benefits of extended care and monitoring.
MANAGING ASTHMA IN THE
PREHOSPITAL ENVIRONMENT
1
PREHOSPITAL ENVIRONMENT
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ABSTRACT
Introduction
Asthma is a very common cause for admission into hospital beds. Asthma
is a long-term inflammatory disease that affects the air passage ways and
lungs. Admission to hospital due to an attack of asthma denotes letdown
of pre hospital management to check or bring its reduction ( Rognås, et al,
2011). Numerous factors have been recognized that may impact and avert
the admission of patients to hospital with an attack of asthma. The pre-
hospital management of asthma has been discussed in the following
abstract. The pre hospital management includes proper monitoring, regular
treatment by a physician (every three months), providing of an individual
with written management plan, suitable for early controlling of asthma in
the home, good understanding with preventive treatment, and an
satisfactory level of asthma knowledge ( Torgerson, et al, 2011) .
2
Introduction
Asthma is a very common cause for admission into hospital beds. Asthma
is a long-term inflammatory disease that affects the air passage ways and
lungs. Admission to hospital due to an attack of asthma denotes letdown
of pre hospital management to check or bring its reduction ( Rognås, et al,
2011). Numerous factors have been recognized that may impact and avert
the admission of patients to hospital with an attack of asthma. The pre-
hospital management of asthma has been discussed in the following
abstract. The pre hospital management includes proper monitoring, regular
treatment by a physician (every three months), providing of an individual
with written management plan, suitable for early controlling of asthma in
the home, good understanding with preventive treatment, and an
satisfactory level of asthma knowledge ( Torgerson, et al, 2011) .
2
Body
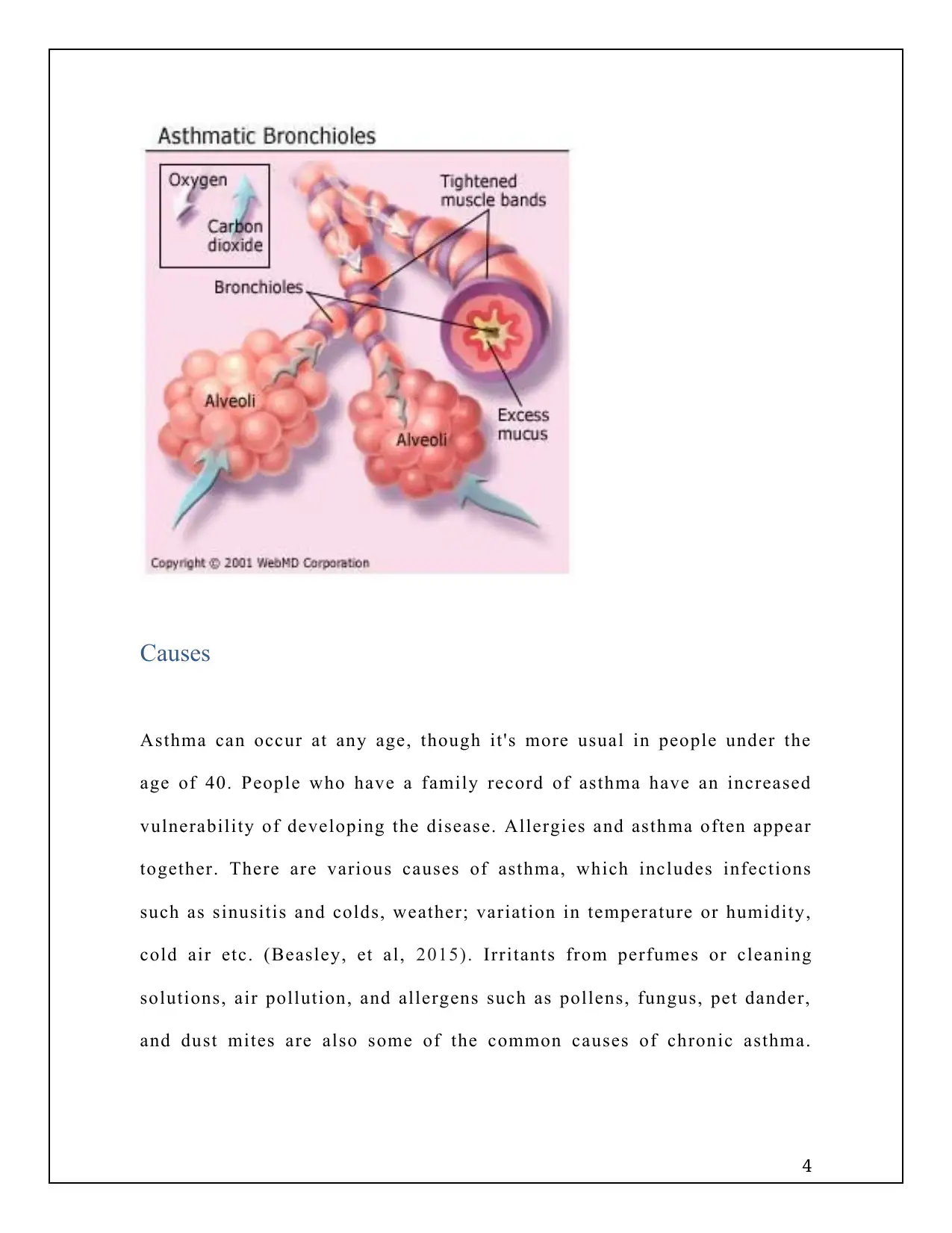
Asthma is a chronic disease of the airways that makes inhalation and
exhalation difficult due to temporary contraction of the passage that carry
oxygen to the lungs. This results in asthmatic indications, which includes
coughing, breathlessness and wheezing( Prosen, et al, 2011) . It is also
referred to as "bronchial asthma". When the body is functioning normally,
the smooth muscles that surround the airways is relaxed, and air moves
easily. But in people with asthma, allergens, respiratory virus, and
environmental causes prompts the bands of muscle surrounding the
airways tighten ( Snyder, et al, 2011) . The people with asthma have
particularly sensitive airways ( Lötvall, et al, 2011).
3
Asthma is a chronic disease of the airways that makes inhalation and
exhalation difficult due to temporary contraction of the passage that carry
oxygen to the lungs. This results in asthmatic indications, which includes
coughing, breathlessness and wheezing( Prosen, et al, 2011) . It is also
referred to as "bronchial asthma". When the body is functioning normally,
the smooth muscles that surround the airways is relaxed, and air moves
easily. But in people with asthma, allergens, respiratory virus, and
environmental causes prompts the bands of muscle surrounding the
airways tighten ( Snyder, et al, 2011) . The people with asthma have
particularly sensitive airways ( Lötvall, et al, 2011).
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Causes
Asthma can occur at any age, though it's more usual in people under the
age of 40. People who have a family record of asthma have an increased
vulnerability of developing the disease. Allergies and asthma often appear
together. There are various causes of asthma, which includes infections
such as sinusitis and colds, weather; variation in temperature or humidity,
cold air etc. (Beasley, et al, 2015). Irritants from perfumes or cleaning
solutions, air pollution, and allergens such as pollens, fungus, pet dander,
and dust mites are also some of the common causes of chronic asthma.
4
Asthma can occur at any age, though it's more usual in people under the
age of 40. People who have a family record of asthma have an increased
vulnerability of developing the disease. Allergies and asthma often appear
together. There are various causes of asthma, which includes infections
such as sinusitis and colds, weather; variation in temperature or humidity,
cold air etc. (Beasley, et al, 2015). Irritants from perfumes or cleaning
solutions, air pollution, and allergens such as pollens, fungus, pet dander,
and dust mites are also some of the common causes of chronic asthma.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The other types of asthma include exercise induced asthma and aspirin
sensitive asthma ( Edwards, et al, 2012).
Pathophysiology
The pathophysiology of asthma is complex and comprises airway
inflammation, recurrent airflow blockade, and increased bronchial
responsiveness. During asthma attack there is sudden worsening of the
symptoms and the airways constrict by either swelling, fill with mucus.
There is bronchospasm, which leads to coughing, shortness of breath,
chest pressure ( Lim, et al, 2010) . Due to hypersensitivity caused by the
allergens, the inflammatory process occurs along the entire air passage
from nose to the lungs. Once the airway becomes puffed-up and inflamed,
it becomes constricted, and less air gets through to the alveoli of lungs.
Management and Treatment
Understanding of asthmatic symptoms and the various types of asthmas
can help in discovering the right treatment and management of the
condition. Periodic assessment and monitoring is necessary to maintain
regular pulmonary function, and prevent recurrent attacks of asthma and
5
sensitive asthma ( Edwards, et al, 2012).
Pathophysiology
The pathophysiology of asthma is complex and comprises airway
inflammation, recurrent airflow blockade, and increased bronchial
responsiveness. During asthma attack there is sudden worsening of the
symptoms and the airways constrict by either swelling, fill with mucus.
There is bronchospasm, which leads to coughing, shortness of breath,
chest pressure ( Lim, et al, 2010) . Due to hypersensitivity caused by the
allergens, the inflammatory process occurs along the entire air passage
from nose to the lungs. Once the airway becomes puffed-up and inflamed,
it becomes constricted, and less air gets through to the alveoli of lungs.
Management and Treatment
Understanding of asthmatic symptoms and the various types of asthmas
can help in discovering the right treatment and management of the
condition. Periodic assessment and monitoring is necessary to maintain
regular pulmonary function, and prevent recurrent attacks of asthma and
5
the need for frequent hospitalizations. Several types of monitoring which
are recommended are signs and symptoms of asthma, history of
exacerbations, pharmacotherapy, and quality of life and patient provider
communication.
Patients with moderate to severe asthma are recommended to be provided
with a written action plan in accordance with the individual’s signs and
symptoms. Exposure of sensitive patients to allergens should be reduced
so that there is reduction in asthmatic attacks.
Pharmacological therapy includes long-term medications to regulate
persistent asthma, and quick relief medications aimed at treating
exacerbations and symptoms. Corticosteroids can be helpful in
maintaining normal lung functions ( Pollart, 2011).
However, patient and provider communication remains the cornerstone for
management of asthma. Self-management education, tailored for
individuals is also extremely helpful. Inhaled beta-agonist therapy is one
of the extensively suggested first choice of treatment for pre hospital
management, but anticholinergic agents may also be used ( Network, G.A.,
2014).
6
are recommended are signs and symptoms of asthma, history of
exacerbations, pharmacotherapy, and quality of life and patient provider
communication.
Patients with moderate to severe asthma are recommended to be provided
with a written action plan in accordance with the individual’s signs and
symptoms. Exposure of sensitive patients to allergens should be reduced
so that there is reduction in asthmatic attacks.
Pharmacological therapy includes long-term medications to regulate
persistent asthma, and quick relief medications aimed at treating
exacerbations and symptoms. Corticosteroids can be helpful in
maintaining normal lung functions ( Pollart, 2011).
However, patient and provider communication remains the cornerstone for
management of asthma. Self-management education, tailored for
individuals is also extremely helpful. Inhaled beta-agonist therapy is one
of the extensively suggested first choice of treatment for pre hospital
management, but anticholinergic agents may also be used ( Network, G.A.,
2014).
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Conclusion
Pre hospital management can prevent the requirement of hospital presence
in most cases if they apply currently acclaimed actions or treatments for
exacerbations. This would effect in a drop in rates of hospitalization for
asthma. Extended care and monitori ng can benefit the patients of asthma.
REFERENCE
7
Pre hospital management can prevent the requirement of hospital presence
in most cases if they apply currently acclaimed actions or treatments for
exacerbations. This would effect in a drop in rates of hospitalization for
asthma. Extended care and monitori ng can benefit the patients of asthma.
REFERENCE
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Beasley, R., Semprini, A. and Mitchell, E.A., 2015. Risk factors for
asthma: is prevention possible?. The Lancet, 386(9998), pp.1075-
1085.
Edwards, M.R., Bartlett, N.W., Hussell, T., Openshaw, P. and
Johnston, S.L., 2012. The microbiology of asthma. Nature Reviews
Microbiology, 10(7), p.459.
Lim, J.S., Woo, S.I., Kwon, H.I., Baek, Y.H., Choi, Y.K. and Hahn,
Y.S., 2010. Clinical characteristics of acute lower respiratory tract
infections due to 13 respiratory viruses detected by multiplex PCR
in children. Korean Journal of Pediatrics, 53(3), pp.373-379.
Lötvall, J., Akdis, C.A., Bacharier, L.B., Bjermer, L., Casale, T.B.,
Custovic, A., Lemanske Jr, R.F., Wardlaw, A.J., Wenzel, S.E. and
Greenberger, P.A., 2011. Asthma endotypes: a new approach to
classification of disease entities within the asthma
syndrome. Journal of Allergy and Clinical Immunology, 127(2),
pp.355-360.
Network, G.A., 2014. The global asthma report 2014.Auckland, New
Zealand, 769.
Pollart, S.M., Compton, R.M. and Elward, K.S., 2011. Management
of acute asthma exacerbations. American family physician, 84(1).
Prosen, G., Klemen, P., Strnad, M. and Grmec, Š., 2011.
Combination of lung ultrasound (a comet-tail sign) and N-terminal
pro-brain natriuretic peptide in differentiating acute heart failure
from chronic obstructive pulmonary disease and asthma as cause of
acute dyspnea in prehospital emergency setting. Critical
Care, 15(2), p.R114.
Rognås, L., Hansen, T.M., Kirkegaard, H. and Tønnesen, E., 2013.
Pre-hospital advanced airway management by experienced
anaesthesiologists: a prospective descriptive study. Scandinavian
journal of trauma, resuscitation and emergency medicine, 21(1),
p.58.
8
asthma: is prevention possible?. The Lancet, 386(9998), pp.1075-
1085.
Edwards, M.R., Bartlett, N.W., Hussell, T., Openshaw, P. and
Johnston, S.L., 2012. The microbiology of asthma. Nature Reviews
Microbiology, 10(7), p.459.
Lim, J.S., Woo, S.I., Kwon, H.I., Baek, Y.H., Choi, Y.K. and Hahn,
Y.S., 2010. Clinical characteristics of acute lower respiratory tract
infections due to 13 respiratory viruses detected by multiplex PCR
in children. Korean Journal of Pediatrics, 53(3), pp.373-379.
Lötvall, J., Akdis, C.A., Bacharier, L.B., Bjermer, L., Casale, T.B.,
Custovic, A., Lemanske Jr, R.F., Wardlaw, A.J., Wenzel, S.E. and
Greenberger, P.A., 2011. Asthma endotypes: a new approach to
classification of disease entities within the asthma
syndrome. Journal of Allergy and Clinical Immunology, 127(2),
pp.355-360.
Network, G.A., 2014. The global asthma report 2014.Auckland, New
Zealand, 769.
Pollart, S.M., Compton, R.M. and Elward, K.S., 2011. Management
of acute asthma exacerbations. American family physician, 84(1).
Prosen, G., Klemen, P., Strnad, M. and Grmec, Š., 2011.
Combination of lung ultrasound (a comet-tail sign) and N-terminal
pro-brain natriuretic peptide in differentiating acute heart failure
from chronic obstructive pulmonary disease and asthma as cause of
acute dyspnea in prehospital emergency setting. Critical
Care, 15(2), p.R114.
Rognås, L., Hansen, T.M., Kirkegaard, H. and Tønnesen, E., 2013.
Pre-hospital advanced airway management by experienced
anaesthesiologists: a prospective descriptive study. Scandinavian
journal of trauma, resuscitation and emergency medicine, 21(1),
p.58.
8
Snyder, S.R., Santiago, M. and Collopy, K.T., 2011. Wheezing in
the pediatric patient. A review of prehospital management of two
childhood diseases--bronchiolitis and asthma. EMS world,40(1),
pp.40-42.
Torgerson, D.G., Ampleford, E.J., Chiu, G.Y., Gauderman, W.J.,
Gignoux, C.R., Graves, P.E., Himes, B.E., Levin, A.M., Mathias,
R.A., Hancock, D.B. and Baurley, J.W., 2011. Meta-analysis of
genome-wide association studies of asthma in ethnically diverse
North American populations. Nature genetics, 43(9), p.887.
9
the pediatric patient. A review of prehospital management of two
childhood diseases--bronchiolitis and asthma. EMS world,40(1),
pp.40-42.
Torgerson, D.G., Ampleford, E.J., Chiu, G.Y., Gauderman, W.J.,
Gignoux, C.R., Graves, P.E., Himes, B.E., Levin, A.M., Mathias,
R.A., Hancock, D.B. and Baurley, J.W., 2011. Meta-analysis of
genome-wide association studies of asthma in ethnically diverse
North American populations. Nature genetics, 43(9), p.887.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





