HSHM546 Essay: Managing Quality Service in Healthcare
VerifiedAdded on 2022/08/30
|20
|5867
|41
Essay
AI Summary
This essay delves into the critical aspects of managing quality service in healthcare, using the Royal Melbourne Hospital in Australia as a case study. It examines the hospital's organizational structure, specifically its auditing department, and the leadership actions required for effective healthcare model development. The essay explores whether the model aligns with evidence-based practice, detailing how Cynthia Struck's six steps can be incorporated. It also addresses the importance of quality assurance, risk management, and cost-effectiveness in healthcare. The essay discusses specific actions leaders should take, the role of transformational leadership, and the necessity of an evidence-based approach in healthcare service delivery, referencing the VNAHPO case study. The author also provides a detailed breakdown of Struck's six steps, emphasizing their relevance in developing a robust healthcare model, and concludes with recommendations for improving patient care and operational efficiency.

Running Head: Managing Quality Service In healthcare 1
Managing Quality service in healthcare
Student’s Name
Institution
Date
Managing Quality service in healthcare
Student’s Name
Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Managing quality service in healthcare 2
Managing Quality, Risk and Cost in Health Care Service
Introduction
Enhancing quality is a task that is vital in every health care set up. This is a responsibility to
every member in the health care system as they offer care to patients. Quality care goes in line
with maintaining the patient's right as one offers care regarding evidence-based – practice
(Dobbs, 2019). This paper shall address the Royal Melbourne Hospital, Located in Australia. It
will discuss the functions of its organizational structure, especially the auditing department, as
well as the leadership specific actions needed in the health model development. It will also be
discussed whether the health model’s development is in regard to evidence-based practice,
details on how the six steps, as discussed by Cynthia Struck can be incorporated in the model
(Dobbs, 2019). Finally, conclusions on the model development will be made.
The Royal Melbourne Hospital
The Royal Melbourne Hospital is located in Australia which treats all people and has always
offered services for treating children over the ages. It provides anesthetic services, cardiothoracic
surgery, offers services for children and adolescents, offers critical care, endocrinology and
metabolic medicine, genetics services, and immunology ("Royal Children’s Hospital Melbourne,
Australia Billard Leece Partnership; Bates Smart," 2018). This hospital also offers
neurophysiology services, neuropsychology services, occupational therapy services, Pediatric
intensive care palliative care, pharmacy, respiratory medicine, services for speech and language.
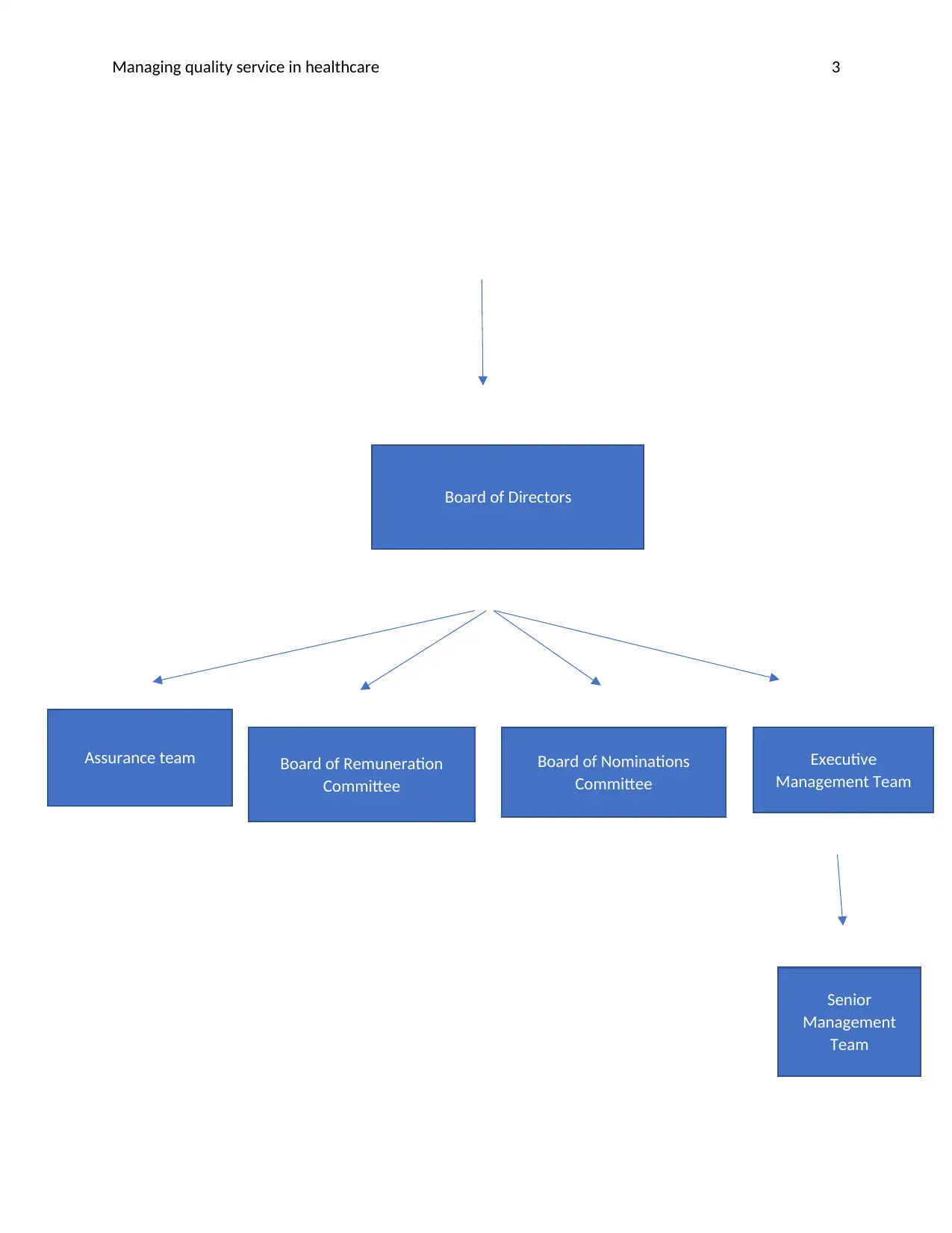
All its specialists are contained in one roof. Its organisational structure is a governance structure
that is made up of different parties with different organisational functions.
Member’s council
(Council of Governors)
Managing Quality, Risk and Cost in Health Care Service
Introduction
Enhancing quality is a task that is vital in every health care set up. This is a responsibility to
every member in the health care system as they offer care to patients. Quality care goes in line
with maintaining the patient's right as one offers care regarding evidence-based – practice
(Dobbs, 2019). This paper shall address the Royal Melbourne Hospital, Located in Australia. It
will discuss the functions of its organizational structure, especially the auditing department, as
well as the leadership specific actions needed in the health model development. It will also be
discussed whether the health model’s development is in regard to evidence-based practice,
details on how the six steps, as discussed by Cynthia Struck can be incorporated in the model
(Dobbs, 2019). Finally, conclusions on the model development will be made.
The Royal Melbourne Hospital
The Royal Melbourne Hospital is located in Australia which treats all people and has always
offered services for treating children over the ages. It provides anesthetic services, cardiothoracic
surgery, offers services for children and adolescents, offers critical care, endocrinology and
metabolic medicine, genetics services, and immunology ("Royal Children’s Hospital Melbourne,
Australia Billard Leece Partnership; Bates Smart," 2018). This hospital also offers
neurophysiology services, neuropsychology services, occupational therapy services, Pediatric
intensive care palliative care, pharmacy, respiratory medicine, services for speech and language.
All its specialists are contained in one roof. Its organisational structure is a governance structure
that is made up of different parties with different organisational functions.
Member’s council
(Council of Governors)
Managing quality service in healthcare 3
Board of Directors
Board of Remuneration
Committee
Board of Nominations
Committee
Assurance team Executive
Management Team
Senior
Management
Team
Board of Directors
Board of Remuneration
Committee
Board of Nominations
Committee
Assurance team Executive
Management Team
Senior
Management
Team
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Managing quality service in healthcare 4
The functions of the executive management team in Melbourne hospital include performing
various functions of management such as, the delivery of operations and performance, ensuring
patients’ safety and quality outcomes. It also ensures risk assurance and compliance as well as
successful operations of all the group’s subcommittees whose function is ensuring the safety of
the patients, planning, improvement of quality, offering education and research (Jones, Finkler,
& Kovner, 2012). Its senior management team has the role of leadership engagement that is
accomplished by executive directors, clinical leads, divisional and corporate management teams.
The quality assurance functions are done by the finance and investment committee, quality and
safety assurance committee and the audit committee. These committees perform the review and
evaluation monitoring, surveillance and appraisal activities. To enhance quality, the necessary
things and activities are done to meet the needs of the clients and even go beyond those needs.
Everything is done at the right time and in the right manner to ensure the hospital’s successful
operations. A review is done by healthcare professionals in this hospital to make sure that they
do their critical reflection and assess their performance or that of their peers. The audit
committee performs continuous and routine review of the activities carried out in this hospital.
Auditing is conducted at times by looking at the financial analysis of the accounting department
in this hospital. To ensure quality assurance service, evaluation is done on how activities are
carried out in this hospital to know its health’s indices (Prasad, 2015). Surveillance is done
through consistent evaluation in this hospital, and to enhance the delivery of healthcare, an
appraisal is performed through ad hoc collection and analysis of data. This department performs
continuous monitoring of the ongoing appraisal. Through conducting these activities, in the
hospital results safety, the keeping of time, the effectiveness of operations, efficacy
The functions of the executive management team in Melbourne hospital include performing
various functions of management such as, the delivery of operations and performance, ensuring
patients’ safety and quality outcomes. It also ensures risk assurance and compliance as well as
successful operations of all the group’s subcommittees whose function is ensuring the safety of
the patients, planning, improvement of quality, offering education and research (Jones, Finkler,
& Kovner, 2012). Its senior management team has the role of leadership engagement that is
accomplished by executive directors, clinical leads, divisional and corporate management teams.
The quality assurance functions are done by the finance and investment committee, quality and
safety assurance committee and the audit committee. These committees perform the review and
evaluation monitoring, surveillance and appraisal activities. To enhance quality, the necessary
things and activities are done to meet the needs of the clients and even go beyond those needs.
Everything is done at the right time and in the right manner to ensure the hospital’s successful
operations. A review is done by healthcare professionals in this hospital to make sure that they
do their critical reflection and assess their performance or that of their peers. The audit
committee performs continuous and routine review of the activities carried out in this hospital.
Auditing is conducted at times by looking at the financial analysis of the accounting department
in this hospital. To ensure quality assurance service, evaluation is done on how activities are
carried out in this hospital to know its health’s indices (Prasad, 2015). Surveillance is done
through consistent evaluation in this hospital, and to enhance the delivery of healthcare, an
appraisal is performed through ad hoc collection and analysis of data. This department performs
continuous monitoring of the ongoing appraisal. Through conducting these activities, in the
hospital results safety, the keeping of time, the effectiveness of operations, efficacy
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Managing quality service in healthcare 5
appropriateness, and equity in service, availability and continuity of the healthcare facility.
Through quality assurance, this hospital has provided a good team spirit, improved systems, and
standardised procedures. It has also reduced the client’s complaints, improved care, offered
guaranteed quality, enhanced job satisfaction, and increased clients’ confidence (Bobby, 2019).
The quality assurance team has developed a system that promotes quality and corrects quality.
Quality is promoted through the determination of the requirements of quality, promoting the
hospital’s standards and guidelines and managing these systems for quality. Quality is corrected
via decision making on policy and management, empowering the beneficiaries and participation
and monitoring of quality. It is monitored by assessing the health outcome, practices in the
hospital by all teams, assessing satisfaction and complaints. Policy and management decision
making is done through regulations, information, payments, and systems management
(Lazakidou, 2011). An organisational structure helps the hospital in planning its activities
through the division of roles in its team members. When every team member plays his/her role
effectively, activities run out ensuring quality services in the health care set up.
specific actions of leadership needed to develop and implement the model in line with
clinical and corporate governance
The specific actions of leadership that I would incorporate when developing this model include
the criteria and the standards. To ensure this, a manager should be fully informed and conversant
with how a quality system model should be framed. A health system for collecting data must
include the types of diseases, their number, number of surgeries performed and the number of
patients seen each day. The data is tabulated in the department for medical records in hospitals.
A quality monitoring system must meet the set criteria and standards, (Zaccagnini & Pechacek,
2019). To meet the set criteria, the actions a person should engage in include participating in
appropriateness, and equity in service, availability and continuity of the healthcare facility.
Through quality assurance, this hospital has provided a good team spirit, improved systems, and
standardised procedures. It has also reduced the client’s complaints, improved care, offered
guaranteed quality, enhanced job satisfaction, and increased clients’ confidence (Bobby, 2019).
The quality assurance team has developed a system that promotes quality and corrects quality.
Quality is promoted through the determination of the requirements of quality, promoting the
hospital’s standards and guidelines and managing these systems for quality. Quality is corrected
via decision making on policy and management, empowering the beneficiaries and participation
and monitoring of quality. It is monitored by assessing the health outcome, practices in the
hospital by all teams, assessing satisfaction and complaints. Policy and management decision
making is done through regulations, information, payments, and systems management
(Lazakidou, 2011). An organisational structure helps the hospital in planning its activities
through the division of roles in its team members. When every team member plays his/her role
effectively, activities run out ensuring quality services in the health care set up.
specific actions of leadership needed to develop and implement the model in line with
clinical and corporate governance
The specific actions of leadership that I would incorporate when developing this model include
the criteria and the standards. To ensure this, a manager should be fully informed and conversant
with how a quality system model should be framed. A health system for collecting data must
include the types of diseases, their number, number of surgeries performed and the number of
patients seen each day. The data is tabulated in the department for medical records in hospitals.
A quality monitoring system must meet the set criteria and standards, (Zaccagnini & Pechacek,
2019). To meet the set criteria, the actions a person should engage in include participating in
Managing quality service in healthcare 6
regular collection of data for a particular period of time to identify the hospital trends in its
indicators. This data should be collected daily and be integrated into the tasks of every day. The
collected data should then be used in the identification of the present systematic problems and its
causative factors that results in poor performance in the health care system. The data collected
should be used in guiding the decision making of the management.
To meet the standards of healthcare in this model, one should research to gather implicit
information on the wide range of healthcare professionals in specific environments. The implicit
standards of information should then be converted into explicit standards to bring uniformity in
the provision of healthcare. They also provide a baseline in which monitoring of quality is
measured. One should be conversant with the healthcare standards that have been developed by
the ministry of health and other organisations such as the World Health Organisation. In
developing the model, the standards to be applied should be after thorough research and should
be realistic, reliable, valid, clear and measurable. Realistic standards are the ones that can easily
be met by using the available resources while the reliable standards are those which a specific
intervention for a single standard leads to the same outcome (Levine, Galloway, & Peskin,
2011). A valid standard has the basis of scientific evidence and includes; experience that is
acceptable, clearly understood by every person who is concerned, and cannot be misinterpreted
or distorted (OECD, 2013). A clear standard is the one that is amenable through assessment and
quantification (OECD, 2013). The core processes of service delivery include inputs, process, and
the outcomes which are determined by the various personnel in the hospital system, (Harvey,
2015).
The support system includes housekeeping through their inputs and the processes which
all contribute to the client’s quality service. Transformational leadership is very vital when
regular collection of data for a particular period of time to identify the hospital trends in its
indicators. This data should be collected daily and be integrated into the tasks of every day. The
collected data should then be used in the identification of the present systematic problems and its
causative factors that results in poor performance in the health care system. The data collected
should be used in guiding the decision making of the management.
To meet the standards of healthcare in this model, one should research to gather implicit
information on the wide range of healthcare professionals in specific environments. The implicit
standards of information should then be converted into explicit standards to bring uniformity in
the provision of healthcare. They also provide a baseline in which monitoring of quality is
measured. One should be conversant with the healthcare standards that have been developed by
the ministry of health and other organisations such as the World Health Organisation. In
developing the model, the standards to be applied should be after thorough research and should
be realistic, reliable, valid, clear and measurable. Realistic standards are the ones that can easily
be met by using the available resources while the reliable standards are those which a specific
intervention for a single standard leads to the same outcome (Levine, Galloway, & Peskin,
2011). A valid standard has the basis of scientific evidence and includes; experience that is
acceptable, clearly understood by every person who is concerned, and cannot be misinterpreted
or distorted (OECD, 2013). A clear standard is the one that is amenable through assessment and
quantification (OECD, 2013). The core processes of service delivery include inputs, process, and
the outcomes which are determined by the various personnel in the hospital system, (Harvey,
2015).
The support system includes housekeeping through their inputs and the processes which
all contribute to the client’s quality service. Transformational leadership is very vital when
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Managing quality service in healthcare 7
coming up with this initiative. Successful model implementation needs the following actions for
management. These practices include balancing the tension that arises from quality efficiency
and reliability. The manager should create and sustain trust throughout the organisation and
managing the process of implementation effectively by using the appropriate management
techniques (Sharma & GOYAL, 2017). Workers should be engaged in the implementation
process in coming up with its design and how it should be involved in the workflow. Knowledge
should be used in the entire development and the implementation process, which can lead to the
development of a quality model. Such a model shall be used to keep the patients safe if applied
consistently in the workplace by all healthcare professionals.
Discussion on whether the development of the model should be based on an evidence-based
approach, as mentioned in the VNAHPO case study about evidence-based practice
implementation and the reasons.
Everything done in the health care system should be done in line with evidence-based practice.
Developing this model should be based on an evidence/ based approach, as mentioned in the
Visiting Nurse Association Health Care Partners of Ohio (VNAHPO) case study. Evidence-
based practice should be carried out by all clinicians and other parties in their language, decision
making, by policymakers, managers, and clinicians in the entire world. Through systematic
research, decisions are made about the caring of individual patients. Developing this model must
include diseases and their treatment options, the numbers treated, and the surgeries which can
only be obtained through thorough research. Empirical evidence should be included in the
management model by obtaining empirical data by carrying out practice research. To make
decisions about the model and various actions needed, one should assess systematic records and
precisely evaluate them.This will lead to further evidence and the basis for model development
coming up with this initiative. Successful model implementation needs the following actions for
management. These practices include balancing the tension that arises from quality efficiency
and reliability. The manager should create and sustain trust throughout the organisation and
managing the process of implementation effectively by using the appropriate management
techniques (Sharma & GOYAL, 2017). Workers should be engaged in the implementation
process in coming up with its design and how it should be involved in the workflow. Knowledge
should be used in the entire development and the implementation process, which can lead to the
development of a quality model. Such a model shall be used to keep the patients safe if applied
consistently in the workplace by all healthcare professionals.
Discussion on whether the development of the model should be based on an evidence-based
approach, as mentioned in the VNAHPO case study about evidence-based practice
implementation and the reasons.
Everything done in the health care system should be done in line with evidence-based practice.
Developing this model should be based on an evidence/ based approach, as mentioned in the
Visiting Nurse Association Health Care Partners of Ohio (VNAHPO) case study. Evidence-
based practice should be carried out by all clinicians and other parties in their language, decision
making, by policymakers, managers, and clinicians in the entire world. Through systematic
research, decisions are made about the caring of individual patients. Developing this model must
include diseases and their treatment options, the numbers treated, and the surgeries which can
only be obtained through thorough research. Empirical evidence should be included in the
management model by obtaining empirical data by carrying out practice research. To make
decisions about the model and various actions needed, one should assess systematic records and
precisely evaluate them.This will lead to further evidence and the basis for model development
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Managing quality service in healthcare 8
(Hall & Roussel, 2012). The evidence-based approach should be used to make sure that in this
model, mutual trust is promoted between the nursing staff and the management. Through
evidence-based practice, this model shall facilitate the direct care input of the staff and their
impact on decision making and the flow of work. The evidence-based approach provided via this
model helps in providing clinical leadership to support the acquisition of knowledge and the
uptake of various staff in the healthcare organisation and its set up.
Details of how one would conduct the six steps, as Cynthia Struk did, to develop the model.
The six steps carried out by Cynthia Struck are very relevant in the development of the
healthcare model.
Formulating questions Rationale
The rationale of formulating questions is essential for it helps in coming up with evidence-
based management, (Hopper Koppelman, 2015). For example, how can we better Alfred
Hospital Melbourne by utilizing diverse data and meet the diverse client’s needs, and those of
the management? This question will help in critical decision making when developing the
model. This question is at the end of the day called the PICO question. The model’s
framework helps in coming up with the population of interest in the organizational setup, the
need interventions for particular condition/the needed diagnostic procedures, the comparator
and the expected outcomes. In this case, a test may be used, treatment, prognosis or
optimization to rule in and rule out treatment options. The questions asked are vital in helping
the management to make diagnostic decisions, screening decisions operational and financial
decisions, or performance decisions that shall at the end of the day help the management in
getting the outcomes that will help to design the model framework in relation to economic and
(Hall & Roussel, 2012). The evidence-based approach should be used to make sure that in this
model, mutual trust is promoted between the nursing staff and the management. Through
evidence-based practice, this model shall facilitate the direct care input of the staff and their
impact on decision making and the flow of work. The evidence-based approach provided via this
model helps in providing clinical leadership to support the acquisition of knowledge and the
uptake of various staff in the healthcare organisation and its set up.
Details of how one would conduct the six steps, as Cynthia Struk did, to develop the model.
The six steps carried out by Cynthia Struck are very relevant in the development of the
healthcare model.
Formulating questions Rationale
The rationale of formulating questions is essential for it helps in coming up with evidence-
based management, (Hopper Koppelman, 2015). For example, how can we better Alfred
Hospital Melbourne by utilizing diverse data and meet the diverse client’s needs, and those of
the management? This question will help in critical decision making when developing the
model. This question is at the end of the day called the PICO question. The model’s
framework helps in coming up with the population of interest in the organizational setup, the
need interventions for particular condition/the needed diagnostic procedures, the comparator
and the expected outcomes. In this case, a test may be used, treatment, prognosis or
optimization to rule in and rule out treatment options. The questions asked are vital in helping
the management to make diagnostic decisions, screening decisions operational and financial
decisions, or performance decisions that shall at the end of the day help the management in
getting the outcomes that will help to design the model framework in relation to economic and
Managing quality service in healthcare 9
operational outcomes. This question helps in assessing evidence used for developing the
guidelines for clinical practice through diagnostic tests. When developing the question, the
population of interest must be described succinctly, implications on the patients must be
considered, a test and act intervention should be carried out, validated solid outcome should
be looked at and operational questions must look at the impact of the developed model on the
patients. The outcome of this rationale is that at the end of the day, a model that ensures
quality and quantity shall be developed. The patient’s needs and rights shall be met for every
healthcare facility must ensure through its professionals that it provides the best quality
services to patients without violating their rights. When the needs of patients are met,
complaints about the facility are reduced, and a good image of the facility is created to the
public.
Assessing the internet for evidence Rationale
Through the internet, one can acquire evidence-based performance indicators. There are many
indicators of evidence-based practice in health organisations which, when acquired via the
internet, can be of very great help in the management. Although the information is of wide
scope, not all of it is accessible, and so one should examine what is assessable on the internet that
can help in quality assurance. These online sites can be assessed, and from them, one gets what is
relevant for health quality and evidence-based practice for management purposes. Various
websites were obtained to help with the organizational approach towards quality management
consistently. One of these sites is the Medicare Quality Improvement Community (medQIC). It
is assessed through www.medqic.org which helps in making sure that there are quality
improvements in healthcare organizations and helps service providers to find, use and share
resources for quality improvement. This website helps one to find tools that can be used in
operational outcomes. This question helps in assessing evidence used for developing the
guidelines for clinical practice through diagnostic tests. When developing the question, the
population of interest must be described succinctly, implications on the patients must be
considered, a test and act intervention should be carried out, validated solid outcome should
be looked at and operational questions must look at the impact of the developed model on the
patients. The outcome of this rationale is that at the end of the day, a model that ensures
quality and quantity shall be developed. The patient’s needs and rights shall be met for every
healthcare facility must ensure through its professionals that it provides the best quality
services to patients without violating their rights. When the needs of patients are met,
complaints about the facility are reduced, and a good image of the facility is created to the
public.
Assessing the internet for evidence Rationale
Through the internet, one can acquire evidence-based performance indicators. There are many
indicators of evidence-based practice in health organisations which, when acquired via the
internet, can be of very great help in the management. Although the information is of wide
scope, not all of it is accessible, and so one should examine what is assessable on the internet that
can help in quality assurance. These online sites can be assessed, and from them, one gets what is
relevant for health quality and evidence-based practice for management purposes. Various
websites were obtained to help with the organizational approach towards quality management
consistently. One of these sites is the Medicare Quality Improvement Community (medQIC). It
is assessed through www.medqic.org which helps in making sure that there are quality
improvements in healthcare organizations and helps service providers to find, use and share
resources for quality improvement. This website helps one to find tools that can be used in
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Managing quality service in healthcare 10
sharing these results and identify the critical points used for control, help explain and solve
problems and at the same time suggest the areas that need to be improved. This site provides the
user with the knowledge of using flow charts, Pareto diagrams, diagrams for cause-and-effect,
various charts, and check sheets that are filled up with diverse data analyzed with the approaches
that is currently under use by VNAHPO. The manager is then equipped with knowledge,
measures and tools that can be effectively used in coming up with a new quality monitoring
model in health care in the best way. The second website is the Institute for Healthcare
Improvement (IHI), which can be accessed via www.ihi.org .This site helps a person to get
information on the need to make definitions of initiatives of quality improvement and support
Plan –Do-Study –Act cycle usage. This website informs that the whole system measures
encourage a person to create a set of measures of strategic performance in the entire system. The
measures can enable the leaders to get the information needed for the crucial processes and
outcomes over a set time. A person is provided with metrics that can be used to do benchmarking
in the entire system and come up with a plan strategic enough for quality improvement. The six
dimensions of quality as identified by the institute of medicines include safety, effectiveness,
equitability, efficiency, timeliness, and patient-centeredness, (Kyriakides, Creemers, &
Charalambous, 2018). This approach supports models found in most of the healthcare
organisations and is compatible with the multi-corporate structure of VNAHPO’S. The Joint
Commission website. This website contains objectives of the evaluation process, which helps all
organisations in the entire world in measuring, assessing, and improving their performance. They
focus on the patient in need, the care needed for the individual or a resident, and the essential
functions of the organisation needed to provide safety to its members, and high-quality care to its
clients. There are a variety of performance measures that are used and their selection criteria
sharing these results and identify the critical points used for control, help explain and solve
problems and at the same time suggest the areas that need to be improved. This site provides the
user with the knowledge of using flow charts, Pareto diagrams, diagrams for cause-and-effect,
various charts, and check sheets that are filled up with diverse data analyzed with the approaches
that is currently under use by VNAHPO. The manager is then equipped with knowledge,
measures and tools that can be effectively used in coming up with a new quality monitoring
model in health care in the best way. The second website is the Institute for Healthcare
Improvement (IHI), which can be accessed via www.ihi.org .This site helps a person to get
information on the need to make definitions of initiatives of quality improvement and support
Plan –Do-Study –Act cycle usage. This website informs that the whole system measures
encourage a person to create a set of measures of strategic performance in the entire system. The
measures can enable the leaders to get the information needed for the crucial processes and
outcomes over a set time. A person is provided with metrics that can be used to do benchmarking
in the entire system and come up with a plan strategic enough for quality improvement. The six
dimensions of quality as identified by the institute of medicines include safety, effectiveness,
equitability, efficiency, timeliness, and patient-centeredness, (Kyriakides, Creemers, &
Charalambous, 2018). This approach supports models found in most of the healthcare
organisations and is compatible with the multi-corporate structure of VNAHPO’S. The Joint
Commission website. This website contains objectives of the evaluation process, which helps all
organisations in the entire world in measuring, assessing, and improving their performance. They
focus on the patient in need, the care needed for the individual or a resident, and the essential
functions of the organisation needed to provide safety to its members, and high-quality care to its
clients. There are a variety of performance measures that are used and their selection criteria
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Managing quality service in healthcare 11
when it comes to quality improvement. The managers of quality assurance are urged to address
particular areas in the healthcare system and, at the same time, target specific populations of
health with a target of offering protection and ensuring quality provision. The site managers
should be specific and accurately define the sources of standardized data, identify the procedures
used in sampling, calculation algorithms, and adjustment of risks if necessary. The measures
identified should be reliable and create room for continuous measuring and bear results when
used across populations. These measures should be valid regarding the available evidence and
can be interpreted and understood when subjected to the stakeholders and any other member.
The measures should also be available in the public domain and help the organisation in its
accreditation process or in the efforts of quality improvement decision making. The accreditation
process involves the health sector determination of quality standards and upholds them in service
delivery, (David&Marcinko 2010). There is a very extensive external review that is carried out
during the accreditation process. During this process also, quality self-assessment is done
through various components that ensure that the relevant standards have been identified. The
process ensures that the standards are dynamic, written and published, cover the domain of
structure, and produce valid outcome, (Koutoukidis & Stainton, 2016). The accreditation process
should be administered by an external body for accreditation .The aim of accreditation should be
to encourage development of the organization
and its optimal practice. Accreditation is done by the collaboration between the authorities of the
government and the private professional bodies that all work together to make sure that they
meet the requirements of accreditation. When services are delivered to an accredited level in an
organization, the operations in the health facility becomes efficient, and the patients can
recognize those services as being reputable and of high quality. The chief global accreditation
when it comes to quality improvement. The managers of quality assurance are urged to address
particular areas in the healthcare system and, at the same time, target specific populations of
health with a target of offering protection and ensuring quality provision. The site managers
should be specific and accurately define the sources of standardized data, identify the procedures
used in sampling, calculation algorithms, and adjustment of risks if necessary. The measures
identified should be reliable and create room for continuous measuring and bear results when
used across populations. These measures should be valid regarding the available evidence and
can be interpreted and understood when subjected to the stakeholders and any other member.
The measures should also be available in the public domain and help the organisation in its
accreditation process or in the efforts of quality improvement decision making. The accreditation
process involves the health sector determination of quality standards and upholds them in service
delivery, (David&Marcinko 2010). There is a very extensive external review that is carried out
during the accreditation process. During this process also, quality self-assessment is done
through various components that ensure that the relevant standards have been identified. The
process ensures that the standards are dynamic, written and published, cover the domain of
structure, and produce valid outcome, (Koutoukidis & Stainton, 2016). The accreditation process
should be administered by an external body for accreditation .The aim of accreditation should be
to encourage development of the organization
and its optimal practice. Accreditation is done by the collaboration between the authorities of the
government and the private professional bodies that all work together to make sure that they
meet the requirements of accreditation. When services are delivered to an accredited level in an
organization, the operations in the health facility becomes efficient, and the patients can
recognize those services as being reputable and of high quality. The chief global accreditation
Managing quality service in healthcare 12
body in the health sector is the International Society for Quality in Healthcare (ISQH), whose
functions are the promotion of quality health in the entire world. It works with the world’s key
organisations such as WHO, to develop the directions of quality and perform the accreditation of
the accrediting agencies. They offer accreditation to other private bodies that can perform the
accreditation tasks to health organizations. Australia contains the Australian National Safety and
Quality Health Services Standards (ACSQH) that offers accreditation to public hospitals, offer
day procedure services and accreditation to dental clinics. There are private nominated bodies for
accreditation which have been recognized as accreditation agencies. These agencies help in
facilitating consultation services and render status of accreditation to hospitals. There are ten
National Safety and Quality Health Service Standards that has been guiding Australian
Accreditation since the first of January 2013 (Australian Commission on Safety and Quality in
Health care, 2015). These standards include safety and quality in health service organisations
governance, consumers’ partnerships, healthcare-associated infections control and prevention,
ensuring the safety of medications and identification of patients, and matching of procedures.
Other standards include clinical handover, the standard of blood and its products,
pressure injuries management and prevention , clinical deterioration in Acute health care
recognition and response and prevention of
falls and harms that result when one is subjected to the risk of falling. The current standards
model includes eight standards that can be included in the model for clinical governance
framework. It is essential in the healthcare system because it contains elements for clinical
governance, the element for consumers’ partnership, ways of preventing infections emerging
from healthcare, the safety of medications, the element of offering comprehensive care,
enhancing communication for safety, management of blood recognition and response to acute
body in the health sector is the International Society for Quality in Healthcare (ISQH), whose
functions are the promotion of quality health in the entire world. It works with the world’s key
organisations such as WHO, to develop the directions of quality and perform the accreditation of
the accrediting agencies. They offer accreditation to other private bodies that can perform the
accreditation tasks to health organizations. Australia contains the Australian National Safety and
Quality Health Services Standards (ACSQH) that offers accreditation to public hospitals, offer
day procedure services and accreditation to dental clinics. There are private nominated bodies for
accreditation which have been recognized as accreditation agencies. These agencies help in
facilitating consultation services and render status of accreditation to hospitals. There are ten
National Safety and Quality Health Service Standards that has been guiding Australian
Accreditation since the first of January 2013 (Australian Commission on Safety and Quality in
Health care, 2015). These standards include safety and quality in health service organisations
governance, consumers’ partnerships, healthcare-associated infections control and prevention,
ensuring the safety of medications and identification of patients, and matching of procedures.
Other standards include clinical handover, the standard of blood and its products,
pressure injuries management and prevention , clinical deterioration in Acute health care
recognition and response and prevention of
falls and harms that result when one is subjected to the risk of falling. The current standards
model includes eight standards that can be included in the model for clinical governance
framework. It is essential in the healthcare system because it contains elements for clinical
governance, the element for consumers’ partnership, ways of preventing infections emerging
from healthcare, the safety of medications, the element of offering comprehensive care,
enhancing communication for safety, management of blood recognition and response to acute
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





