Mandy Case Study: Analysis of Cardiac and Respiratory Dysfunction
VerifiedAdded on 2022/09/16
|12
|3374
|24
Case Study
AI Summary
This case study analyzes the case of Mandy, a 6-month-old female presenting with cardiac and respiratory issues. The paper details subjective and objective findings, including reduced food intake, breathing difficulties, high heart and respiration rates, and crackles in the lungs, indicative of potential cardiac and respiratory dysfunction. The analysis includes a discussion of the patient's history, symptoms, and lab findings, such as elevated BUN and BNP levels. The study outlines a priority list of nursing orders, including lab tests, echocardiogram, and chest X-ray, along with interventions like NG tube insertion, oxygen administration, and IV fluids. The paper also addresses necessary supplies and steps for NG tube insertion, nursing interventions during ECG, and precautions related to RSV. Family-centered interventions are also discussed, emphasizing the importance of parental involvement and understanding. The paper concludes with a discussion of abnormal lab findings and the impact of a respiratory virus on Mandy's condition, along with potential medications and nursing interventions.

Running head: MANDY CASE STUDY
MANDY CASE STUDY
Name of the Student
Name of the University
Author note
MANDY CASE STUDY
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
MANDY CASE STUDY
The paper discusses about a six months old baby Mandy suffering from heart
problem. The paper is structured to discuss about different nursing interpretation and analysis
done to interpret the disease Mandy is suffering and find a proper diagnostic measure for the
cure of the disease.
Answer 1
Various objective and subjective finding showing that Mandy was suffering from cardiac as
well as circulatory dysfunction are as follows-
Mandy have reduced her food intake along with the drinking of water. Mandy’s mom has
observed that Mandy is having breathing difficulty. Mandy appears in toxic in nurse’s eyes
and was hence recommended for further diagnosis. Mandy is having a heart rate of 160,
which is very high. This might be sign of sinus tachycardia (Matiasz & Rigolin, 2018).
Mandy is also diagnosed to have holosystolic murmur that might be a sign of septal defect.
The signs and symptoms of heart disease includes breathing shortness, faster breathing,
fatigue, and very less gain in the weight. Hence, in-toxic appearance suggests that Mandy is
having deoxygenated blood flow or she might be having low red blood cell count in her body
(Chen & Levy, 2016). Moreover, she was having dry oral mucosa that means she is having
dehydration. Therefore, all the diagnostic features obtained after physical exam suggests that
Mandy is having heart problem and there is flow of deoxygenated blood in her body which is
making her look pale and pink
Answer 2
The subjective and objective analysis that proves that Mandy is suffering from
respiratory dysfunction are her respiration rate which is high 65 minutes per minute.
Normally infants have respiration rate of 20-60 breaths per minute. Faster breathing might be
a sign of tachypnea (Sanchis-Gomar, Perez-Quilis, Leischik & Lucia, 2016). She is having
MANDY CASE STUDY
The paper discusses about a six months old baby Mandy suffering from heart
problem. The paper is structured to discuss about different nursing interpretation and analysis
done to interpret the disease Mandy is suffering and find a proper diagnostic measure for the
cure of the disease.
Answer 1
Various objective and subjective finding showing that Mandy was suffering from cardiac as
well as circulatory dysfunction are as follows-
Mandy have reduced her food intake along with the drinking of water. Mandy’s mom has
observed that Mandy is having breathing difficulty. Mandy appears in toxic in nurse’s eyes
and was hence recommended for further diagnosis. Mandy is having a heart rate of 160,
which is very high. This might be sign of sinus tachycardia (Matiasz & Rigolin, 2018).
Mandy is also diagnosed to have holosystolic murmur that might be a sign of septal defect.
The signs and symptoms of heart disease includes breathing shortness, faster breathing,
fatigue, and very less gain in the weight. Hence, in-toxic appearance suggests that Mandy is
having deoxygenated blood flow or she might be having low red blood cell count in her body
(Chen & Levy, 2016). Moreover, she was having dry oral mucosa that means she is having
dehydration. Therefore, all the diagnostic features obtained after physical exam suggests that
Mandy is having heart problem and there is flow of deoxygenated blood in her body which is
making her look pale and pink
Answer 2
The subjective and objective analysis that proves that Mandy is suffering from
respiratory dysfunction are her respiration rate which is high 65 minutes per minute.
Normally infants have respiration rate of 20-60 breaths per minute. Faster breathing might be
a sign of tachypnea (Sanchis-Gomar, Perez-Quilis, Leischik & Lucia, 2016). She is having
2
MANDY CASE STUDY
cough and nose drainage. Mandy was also having breathing difficulty and she was suffering
from breathing shortness and is having dry lips. Mandy was having upper airway congestion
along with average subcostal retraction, crackles, bobbing and tachypnea. All this shows that
her lung is not working properly and she needs immediate treatment (Anderson et al., 2016).
Mandy was having crackles in lungs which means that there might be some inflammation in
her lungs or infection in alveoli, bronchi or bronchioles. Crackles after coughing indicate
edema (pulmonary). This crackling might also be a sign of heart disease indicating fluid in
the alveoli due to failure in the heart.
Answer 3
The patient Mandy is having fever for last 3 days, she is having difficulty in breathing
and is having fast breathing, food intake has decreased and she looks pale and pinkish, her
breathing rate is high as well as her heart rate (Michael, Scharf, Letzkus & Vergales, 2016).
Oxygen content in her blood is less.
The background history of Mandy displayed that Mandy was delivered in 40 weeks
and 2 days’ time without any complication during birth, her birth weight was 3.8 kg and she
was of 50 cm in length. However, Mandy had to stay in NICU, as she is having a hole in her
heart. However, her mother said that there is no family history of hypertension,
hyperlipidaemia, heart disease, bleeding disorder, and chromosomal abnormalities neither
from Mandy’s mom or dad’s side (Michael, Scharf, Letzkus & Vergales, 2016). However, it
was noted that her 18months old cousin is suffering from hole in heart and hence underwent
surgery six months ago.
After analysing all the signs and symptoms along with past data it was assessed that
Mandy is suffering from cardiac as well pulmonary distress. Low oxygen content states that
the level of oxygenated blood in her blood is less and her high respiration and heart rate
suggested that Mandy is suffering breathing difficulty and heart problems (Shrivastava,
MANDY CASE STUDY
cough and nose drainage. Mandy was also having breathing difficulty and she was suffering
from breathing shortness and is having dry lips. Mandy was having upper airway congestion
along with average subcostal retraction, crackles, bobbing and tachypnea. All this shows that
her lung is not working properly and she needs immediate treatment (Anderson et al., 2016).
Mandy was having crackles in lungs which means that there might be some inflammation in
her lungs or infection in alveoli, bronchi or bronchioles. Crackles after coughing indicate
edema (pulmonary). This crackling might also be a sign of heart disease indicating fluid in
the alveoli due to failure in the heart.
Answer 3
The patient Mandy is having fever for last 3 days, she is having difficulty in breathing
and is having fast breathing, food intake has decreased and she looks pale and pinkish, her
breathing rate is high as well as her heart rate (Michael, Scharf, Letzkus & Vergales, 2016).
Oxygen content in her blood is less.
The background history of Mandy displayed that Mandy was delivered in 40 weeks
and 2 days’ time without any complication during birth, her birth weight was 3.8 kg and she
was of 50 cm in length. However, Mandy had to stay in NICU, as she is having a hole in her
heart. However, her mother said that there is no family history of hypertension,
hyperlipidaemia, heart disease, bleeding disorder, and chromosomal abnormalities neither
from Mandy’s mom or dad’s side (Michael, Scharf, Letzkus & Vergales, 2016). However, it
was noted that her 18months old cousin is suffering from hole in heart and hence underwent
surgery six months ago.
After analysing all the signs and symptoms along with past data it was assessed that
Mandy is suffering from cardiac as well pulmonary distress. Low oxygen content states that
the level of oxygenated blood in her blood is less and her high respiration and heart rate
suggested that Mandy is suffering breathing difficulty and heart problems (Shrivastava,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
MANDY CASE STUDY
Singh, Raizada & Singh, 2015). As she is having crackling while breathing, Mandy is not
taking food and water that is causing no weight gain. The temperature of her body is high.
Hence all above sign indicates disorder Mandy is going through. However, nose drainage is
clear and her blood pressure is in stable state. She is having soft and round abdomen which is
a good sign.
It is recommended that Mandy must undergo immediate diagnosis and medication.
Moreover, it is better she must go surgery so that the hole in heart can be blocked and she can
have a normal life (Belialov, 2017). Blocking the hole in her heart would improve Mandy’s
difficulty, reduce her respiratory distress and hence she can have a normal life.
Answer 4
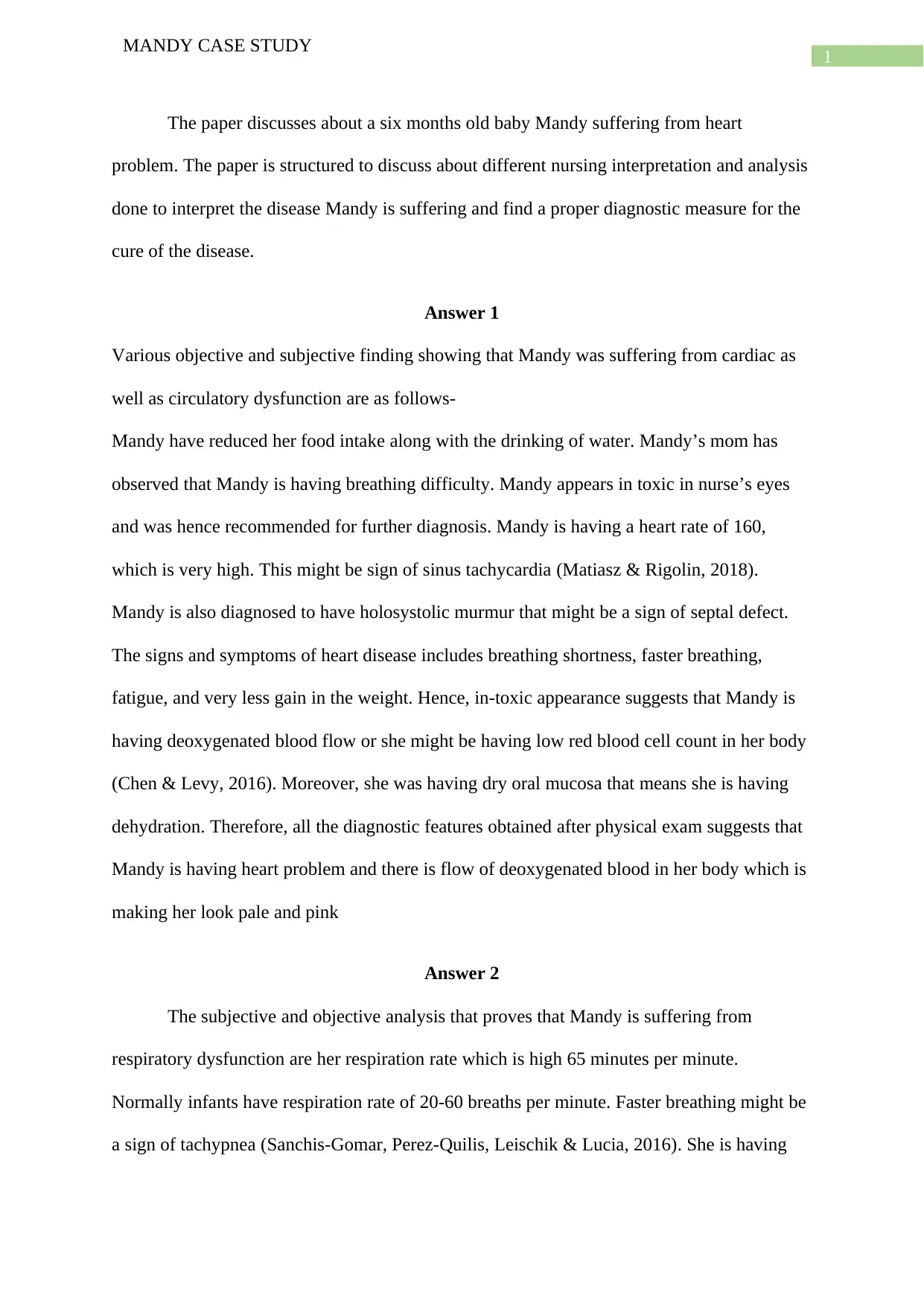
Priority list according to nurse
Priority Orders
1 Laboratory Orders: CBC, chem 8, BNP, Respiratory viral panel
2 Echocardiogram stat
3 Chest x-ray stat
4 Insert NG tube
5 Suction nose before each feed
6 Oxygen 100% 1 L via nasal cannula
7 IV insertion
8 Administer 10 ml/kg of normal saline IV over 30 minutes
9 Offer 150 ml of formula every 4 hours PO. Gavage the remainder over
30 minutes.
As all the symptoms suggests that Mandy is suffering from cardiac problem. First
CBC necessary to blood testing to see the overall health of the person. This blood count test
would help in predicting the blood composition for Mandy at present. Chem8 test is done to
understand the basic metabolic panel for Mandy as, it was reported that Mandy was not
MANDY CASE STUDY
Singh, Raizada & Singh, 2015). As she is having crackling while breathing, Mandy is not
taking food and water that is causing no weight gain. The temperature of her body is high.
Hence all above sign indicates disorder Mandy is going through. However, nose drainage is
clear and her blood pressure is in stable state. She is having soft and round abdomen which is
a good sign.
It is recommended that Mandy must undergo immediate diagnosis and medication.
Moreover, it is better she must go surgery so that the hole in heart can be blocked and she can
have a normal life (Belialov, 2017). Blocking the hole in her heart would improve Mandy’s
difficulty, reduce her respiratory distress and hence she can have a normal life.
Answer 4
Priority list according to nurse
Priority Orders
1 Laboratory Orders: CBC, chem 8, BNP, Respiratory viral panel
2 Echocardiogram stat
3 Chest x-ray stat
4 Insert NG tube
5 Suction nose before each feed
6 Oxygen 100% 1 L via nasal cannula
7 IV insertion
8 Administer 10 ml/kg of normal saline IV over 30 minutes
9 Offer 150 ml of formula every 4 hours PO. Gavage the remainder over
30 minutes.
As all the symptoms suggests that Mandy is suffering from cardiac problem. First
CBC necessary to blood testing to see the overall health of the person. This blood count test
would help in predicting the blood composition for Mandy at present. Chem8 test is done to
understand the basic metabolic panel for Mandy as, it was reported that Mandy was not
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
MANDY CASE STUDY
eating and drinking. It was also reported that Mandy was cough and was having nose
discharge, hence rrespiratory viral panel would help her detecting any presence of respiratory
viruses in Mandy.
After blood test, ECG and chest x-ray is recommended so that function of heart can be
identified through ECG and if there is any lung damage of any pulmonary defect can be
identified through chest x-ray (The Lancet, 2015).
As Mandy was having nasal flow, NG tube would help in removing the lavage that
would make her breathing easier. Nose suction is also necessary before feeding as blockage
in nose prevents breathing, while Mandy is eating it further blocks breathing through lips
hence, Mandy cannot breathe and refuses to eat. Therefore, clearing of nasal passage is
required for making Mandy eat (Eichstaedt et al., 2015).
Mandy’s previous report have shown that Mandy’s SPO2 is low hence, her blood
requires more oxygen. However, due to heart hole in her body cannot receive oxygenated
blood. Hence, supplementary source is necessary so that Mandy can receive oxygenated
blood for better functioning of her body.
Now when, blood report available, ECG, chest x-ray report, nasal passage cleaned and
there is oxygen supply to te blood, Mandy requires medication. As she is an infant with
deoxygenated blood, it is necessary that Mandy’s cells receive direct medicinal supply.
Hence, IV is recommended as well 150 ml formula that will energize her and can help in
further treatment (Nature reviews, 2016).
Answer 5
Necessary supplies required to complete the procedure successfully are-gloves,
lubricant that is water based, fine nasogastric tube that is required for feeding or nasogastric
tube which is 16Fr, bile bag, syringe, pH indicator, anesthetic throat spray, water and syringe.
MANDY CASE STUDY
eating and drinking. It was also reported that Mandy was cough and was having nose
discharge, hence rrespiratory viral panel would help her detecting any presence of respiratory
viruses in Mandy.
After blood test, ECG and chest x-ray is recommended so that function of heart can be
identified through ECG and if there is any lung damage of any pulmonary defect can be
identified through chest x-ray (The Lancet, 2015).
As Mandy was having nasal flow, NG tube would help in removing the lavage that
would make her breathing easier. Nose suction is also necessary before feeding as blockage
in nose prevents breathing, while Mandy is eating it further blocks breathing through lips
hence, Mandy cannot breathe and refuses to eat. Therefore, clearing of nasal passage is
required for making Mandy eat (Eichstaedt et al., 2015).
Mandy’s previous report have shown that Mandy’s SPO2 is low hence, her blood
requires more oxygen. However, due to heart hole in her body cannot receive oxygenated
blood. Hence, supplementary source is necessary so that Mandy can receive oxygenated
blood for better functioning of her body.
Now when, blood report available, ECG, chest x-ray report, nasal passage cleaned and
there is oxygen supply to te blood, Mandy requires medication. As she is an infant with
deoxygenated blood, it is necessary that Mandy’s cells receive direct medicinal supply.
Hence, IV is recommended as well 150 ml formula that will energize her and can help in
further treatment (Nature reviews, 2016).
Answer 5
Necessary supplies required to complete the procedure successfully are-gloves,
lubricant that is water based, fine nasogastric tube that is required for feeding or nasogastric
tube which is 16Fr, bile bag, syringe, pH indicator, anesthetic throat spray, water and syringe.
5
MANDY CASE STUDY
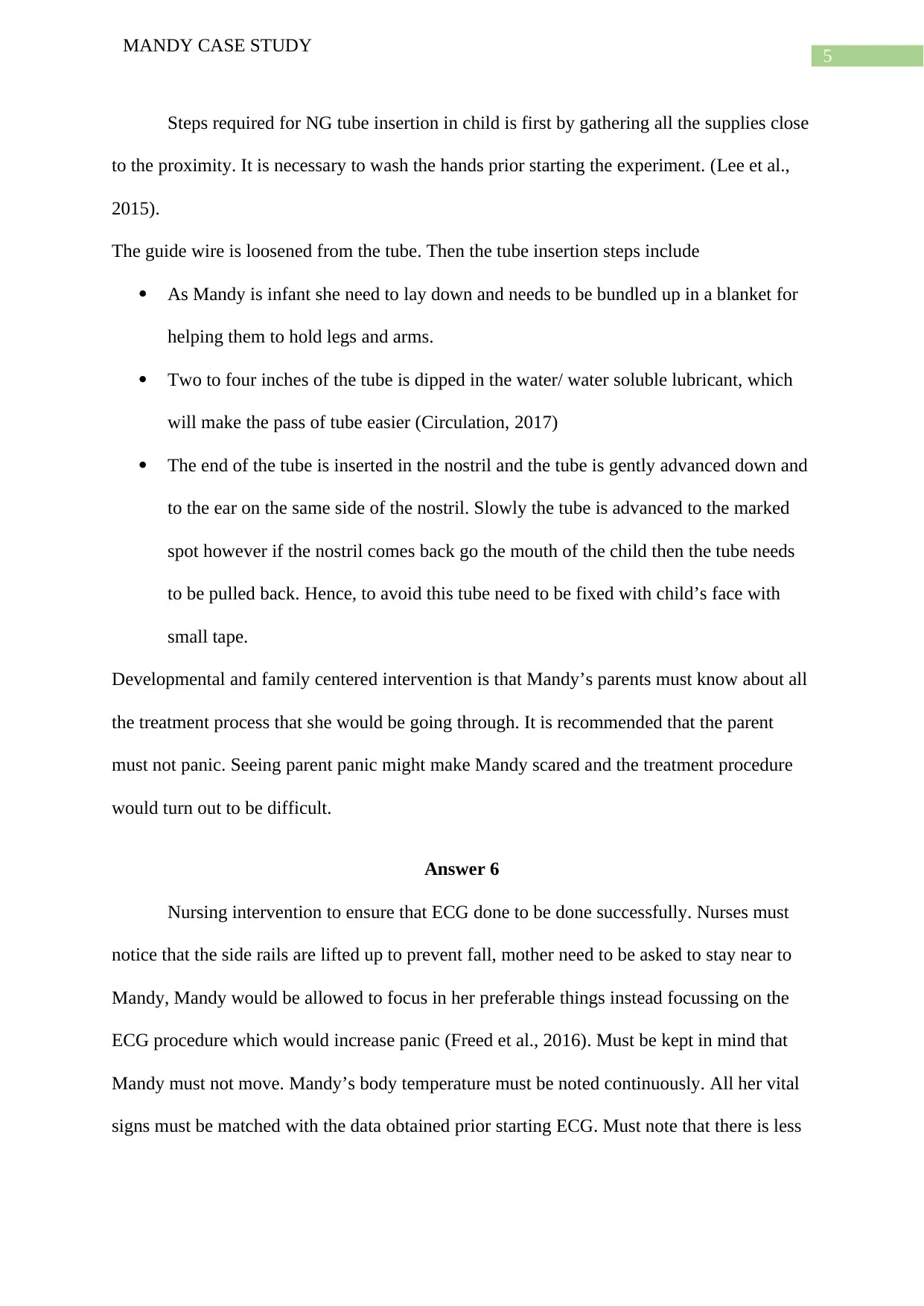
Steps required for NG tube insertion in child is first by gathering all the supplies close
to the proximity. It is necessary to wash the hands prior starting the experiment. (Lee et al.,
2015).
The guide wire is loosened from the tube. Then the tube insertion steps include
As Mandy is infant she need to lay down and needs to be bundled up in a blanket for
helping them to hold legs and arms.
Two to four inches of the tube is dipped in the water/ water soluble lubricant, which
will make the pass of tube easier (Circulation, 2017)
The end of the tube is inserted in the nostril and the tube is gently advanced down and
to the ear on the same side of the nostril. Slowly the tube is advanced to the marked
spot however if the nostril comes back go the mouth of the child then the tube needs
to be pulled back. Hence, to avoid this tube need to be fixed with child’s face with
small tape.
Developmental and family centered intervention is that Mandy’s parents must know about all
the treatment process that she would be going through. It is recommended that the parent
must not panic. Seeing parent panic might make Mandy scared and the treatment procedure
would turn out to be difficult.
Answer 6
Nursing intervention to ensure that ECG done to be done successfully. Nurses must
notice that the side rails are lifted up to prevent fall, mother need to be asked to stay near to
Mandy, Mandy would be allowed to focus in her preferable things instead focussing on the
ECG procedure which would increase panic (Freed et al., 2016). Must be kept in mind that
Mandy must not move. Mandy’s body temperature must be noted continuously. All her vital
signs must be matched with the data obtained prior starting ECG. Must note that there is less
MANDY CASE STUDY
Steps required for NG tube insertion in child is first by gathering all the supplies close
to the proximity. It is necessary to wash the hands prior starting the experiment. (Lee et al.,
2015).
The guide wire is loosened from the tube. Then the tube insertion steps include
As Mandy is infant she need to lay down and needs to be bundled up in a blanket for
helping them to hold legs and arms.
Two to four inches of the tube is dipped in the water/ water soluble lubricant, which
will make the pass of tube easier (Circulation, 2017)
The end of the tube is inserted in the nostril and the tube is gently advanced down and
to the ear on the same side of the nostril. Slowly the tube is advanced to the marked
spot however if the nostril comes back go the mouth of the child then the tube needs
to be pulled back. Hence, to avoid this tube need to be fixed with child’s face with
small tape.
Developmental and family centered intervention is that Mandy’s parents must know about all
the treatment process that she would be going through. It is recommended that the parent
must not panic. Seeing parent panic might make Mandy scared and the treatment procedure
would turn out to be difficult.
Answer 6
Nursing intervention to ensure that ECG done to be done successfully. Nurses must
notice that the side rails are lifted up to prevent fall, mother need to be asked to stay near to
Mandy, Mandy would be allowed to focus in her preferable things instead focussing on the
ECG procedure which would increase panic (Freed et al., 2016). Must be kept in mind that
Mandy must not move. Mandy’s body temperature must be noted continuously. All her vital
signs must be matched with the data obtained prior starting ECG. Must note that there is less
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
MANDY CASE STUDY
movement from Mandy’s side and there must not be panic. If Mandy is scared about the
procedure, she might cry that would make the diagnosis difficult.
Answer 7
As Mandy was suffering from RSV which means that respiratory syncytial virus, that
is highly contagious hence Mandy must be kept in isolation as it can cause contamination.
Moreover, nurses must be wearing gloves and mask while treating Mandy. It is also
recommended that the nurses must wear gowns as a precautionary measure. The BUN and
BNP for patient is high that proved that Mandy was suffering from serious heart disease and
them she also got affected with respiratory disease. Hence, immediate treatment is necessary
(Bank et al., 2017).
As Mandy is suffering from respiratory syncytial virus, precautionary measures need
to be taken by her parents. The parent need to wear gloves, gown and mask before meeting
Mandy. Moreover, it can be assumed that Mandy’s parents might also be affected with the
disease as the virus is contagious. This virus mainly spreads when the infected person is
coughing or sneezing. Hence there might be chances that Mandy’s parents are already
affected with this disease. Hence it is suggested that the parents must also
Answer 8
The abnormal lab finding for Mandy was BUN, Calcium and BNP.
Abnormal BUN level with normal creatinine suggest that Mandy is having significant GI
loss. The level of nitrogen is high in her blood as her heart cannot purify deoxygenated blood
into oxygenated blood (Tokitsu, Yamamoto, Hirata & Ogawa, 2015). The level of oxygen is
also low in her blood because she is having low oxygen in her blood, and episodes of low
oxygen level causes lowering of calcium. Her BNP is very high is suggests that the heart
cannot pump any more oxygen and it is approaching towards heart failure.
MANDY CASE STUDY
movement from Mandy’s side and there must not be panic. If Mandy is scared about the
procedure, she might cry that would make the diagnosis difficult.
Answer 7
As Mandy was suffering from RSV which means that respiratory syncytial virus, that
is highly contagious hence Mandy must be kept in isolation as it can cause contamination.
Moreover, nurses must be wearing gloves and mask while treating Mandy. It is also
recommended that the nurses must wear gowns as a precautionary measure. The BUN and
BNP for patient is high that proved that Mandy was suffering from serious heart disease and
them she also got affected with respiratory disease. Hence, immediate treatment is necessary
(Bank et al., 2017).
As Mandy is suffering from respiratory syncytial virus, precautionary measures need
to be taken by her parents. The parent need to wear gloves, gown and mask before meeting
Mandy. Moreover, it can be assumed that Mandy’s parents might also be affected with the
disease as the virus is contagious. This virus mainly spreads when the infected person is
coughing or sneezing. Hence there might be chances that Mandy’s parents are already
affected with this disease. Hence it is suggested that the parents must also
Answer 8
The abnormal lab finding for Mandy was BUN, Calcium and BNP.
Abnormal BUN level with normal creatinine suggest that Mandy is having significant GI
loss. The level of nitrogen is high in her blood as her heart cannot purify deoxygenated blood
into oxygenated blood (Tokitsu, Yamamoto, Hirata & Ogawa, 2015). The level of oxygen is
also low in her blood because she is having low oxygen in her blood, and episodes of low
oxygen level causes lowering of calcium. Her BNP is very high is suggests that the heart
cannot pump any more oxygen and it is approaching towards heart failure.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
MANDY CASE STUDY
Answer 9
Respiratory virus affects the respiratory track. It causes respiratory track infections.
Mandy was suffering from cough, running nose, high respiration rate, high BUN and BNP.
All together states that Mandy was weak and hence it was easy to get affected with viruses.
As her lung is already weak it got viral infection which enhanced her fever, sever cough, pale
skin colour, difficulty in breathing, rapid breathing and wheezing This virus causes irritation
or inflammation in the trachea causing Mandy to cough, sneeze and have all viral symptoms
(Circulation, 2017). Possible medication provided is to stay in clean place, better to sit as
lying would cause more pain. Nursing intervention related to mediation is that Mandy must
be treated with NG tube. The NG tube would help Mandy in cleaning all her nose blocks that
would help her in breathing, moreover lung cleaning supplementary equipment need to be
used so that it acts as a suction for better flow of air. Along with this Mandy must be treated
with IV so that all medication reaches directly her cells as the blood is impure.
Family centred interventions is that as Mandy is suffering from RSV which is
contagious it is required that her parents must also do a test to check if they are infected or
not. Along with this it intervened that the parents must also wear protection such as gloves,
masks and gown before meeting Mandy. Nurse also need to suggest that Mandy need to stay
in isolation and meeting her requires special permission (Shrivastava, Singh, Raizada &
Singh, 2015).
It is also the duty of the nurse to make Mandy’s family aware about the disease. They
must explain parents that immediate treatment s required as the heart condition is very poor
and on other hand Mandy got affected with virus. Nurses need to explain parents and family
members why it is suggested that Mandy must be in isolation and various necessary
treatments that is to be given to her.
MANDY CASE STUDY
Answer 9
Respiratory virus affects the respiratory track. It causes respiratory track infections.
Mandy was suffering from cough, running nose, high respiration rate, high BUN and BNP.
All together states that Mandy was weak and hence it was easy to get affected with viruses.
As her lung is already weak it got viral infection which enhanced her fever, sever cough, pale
skin colour, difficulty in breathing, rapid breathing and wheezing This virus causes irritation
or inflammation in the trachea causing Mandy to cough, sneeze and have all viral symptoms
(Circulation, 2017). Possible medication provided is to stay in clean place, better to sit as
lying would cause more pain. Nursing intervention related to mediation is that Mandy must
be treated with NG tube. The NG tube would help Mandy in cleaning all her nose blocks that
would help her in breathing, moreover lung cleaning supplementary equipment need to be
used so that it acts as a suction for better flow of air. Along with this Mandy must be treated
with IV so that all medication reaches directly her cells as the blood is impure.
Family centred interventions is that as Mandy is suffering from RSV which is
contagious it is required that her parents must also do a test to check if they are infected or
not. Along with this it intervened that the parents must also wear protection such as gloves,
masks and gown before meeting Mandy. Nurse also need to suggest that Mandy need to stay
in isolation and meeting her requires special permission (Shrivastava, Singh, Raizada &
Singh, 2015).
It is also the duty of the nurse to make Mandy’s family aware about the disease. They
must explain parents that immediate treatment s required as the heart condition is very poor
and on other hand Mandy got affected with virus. Nurses need to explain parents and family
members why it is suggested that Mandy must be in isolation and various necessary
treatments that is to be given to her.
8
MANDY CASE STUDY
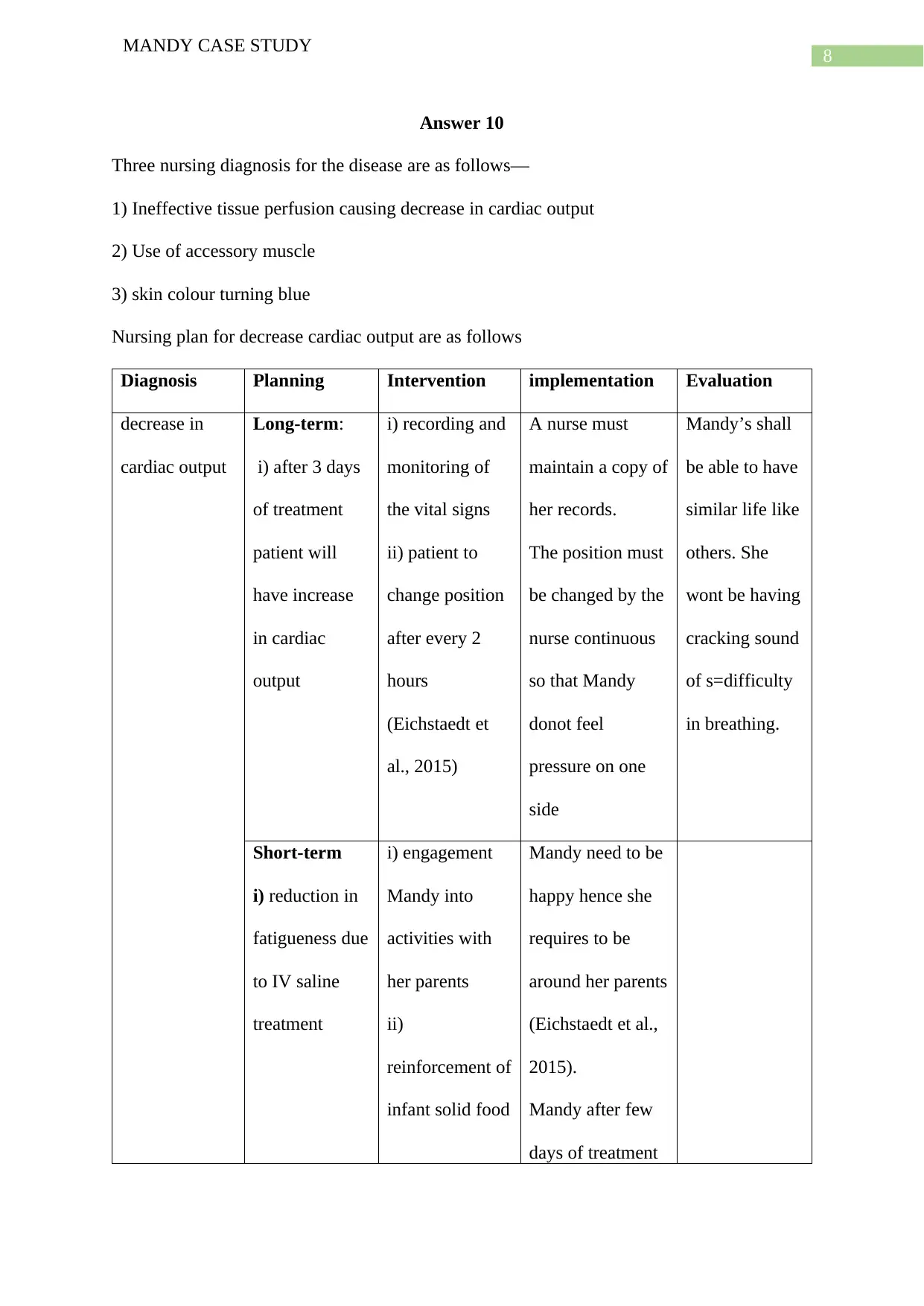
Answer 10
Three nursing diagnosis for the disease are as follows—
1) Ineffective tissue perfusion causing decrease in cardiac output
2) Use of accessory muscle
3) skin colour turning blue
Nursing plan for decrease cardiac output are as follows
Diagnosis Planning Intervention implementation Evaluation
decrease in
cardiac output
Long-term:
i) after 3 days
of treatment
patient will
have increase
in cardiac
output
i) recording and
monitoring of
the vital signs
ii) patient to
change position
after every 2
hours
(Eichstaedt et
al., 2015)
A nurse must
maintain a copy of
her records.
The position must
be changed by the
nurse continuous
so that Mandy
donot feel
pressure on one
side
Mandy’s shall
be able to have
similar life like
others. She
wont be having
cracking sound
of s=difficulty
in breathing.
Short-term
i) reduction in
fatigueness due
to IV saline
treatment
i) engagement
Mandy into
activities with
her parents
ii)
reinforcement of
infant solid food
Mandy need to be
happy hence she
requires to be
around her parents
(Eichstaedt et al.,
2015).
Mandy after few
days of treatment
MANDY CASE STUDY
Answer 10
Three nursing diagnosis for the disease are as follows—
1) Ineffective tissue perfusion causing decrease in cardiac output
2) Use of accessory muscle
3) skin colour turning blue
Nursing plan for decrease cardiac output are as follows
Diagnosis Planning Intervention implementation Evaluation
decrease in
cardiac output
Long-term:
i) after 3 days
of treatment
patient will
have increase
in cardiac
output
i) recording and
monitoring of
the vital signs
ii) patient to
change position
after every 2
hours
(Eichstaedt et
al., 2015)
A nurse must
maintain a copy of
her records.
The position must
be changed by the
nurse continuous
so that Mandy
donot feel
pressure on one
side
Mandy’s shall
be able to have
similar life like
others. She
wont be having
cracking sound
of s=difficulty
in breathing.
Short-term
i) reduction in
fatigueness due
to IV saline
treatment
i) engagement
Mandy into
activities with
her parents
ii)
reinforcement of
infant solid food
Mandy need to be
happy hence she
requires to be
around her parents
(Eichstaedt et al.,
2015).
Mandy after few
days of treatment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
MANDY CASE STUDY
must be given
some food so that
she can gain
weight and
nutrition.
MANDY CASE STUDY
must be given
some food so that
she can gain
weight and
nutrition.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
MANDY CASE STUDY
References
Anderson, L., Thompson, D., Oldridge, N., Zwisler, A., Rees, K., Martin, N., & Taylor, R.
(2016). Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane
Database Of Systematic Reviews. doi: 10.1002/14651858.cd001800.pub3
Bank, I., Gijsberts, C., Teng, T., Benson, L., Sim, D., & Yeo, P. et al. (2017). Prevalence and
Clinical Significance of Diabetes in Asian Versus White Patients With Heart Failure.
JACC: Heart Failure, 5(1), 14-24. doi: 10.1016/j.jchf.2016.09.015
Belialov, F. (2017). Depression, anxiety, and stress in patients with coronary heart disease.
Terapevticheskii Arkhiv, 89(8), 104. doi: 10.17116/terarkh2017898104-109
Chen, G., & Levy, D. (2016). Contributions of the Framingham Heart Study to the
Epidemiology of Coronary Heart Disease. JAMA Cardiology, 1(7), 825. doi:
10.1001/jamacardio.2016.2050
Circulation. (2017). Correction to: Heart Disease and Stroke Statistics—2017 Update: A
Report From the American Heart Association. Circulation, 135(10). doi:
10.1161/cir.0000000000000491
Eichstaedt, J., Schwartz, H., Kern, M., Park, G., Labarthe, D., & Merchant, R. et al. (2015).
Psychological Language on Twitter Predicts County-Level Heart Disease Mortality.
Psychological Science, 26(2), 159-169. doi: 10.1177/0956797614557867
Freed, B., Daruwalla, V., Cheng, J., Aguilar, F., Beussink, L., & Choi, A. et al. (2016).
Prognostic Utility and Clinical Significance of Cardiac Mechanics in Heart Failure
With Preserved Ejection Fraction. Circulation: Cardiovascular Imaging, 9(3). doi:
10.1161/circimaging.115.003754
Lee, D., Zhu, G., Sasaki, T., Cho, G., Hamdani, N., & Holewinski, R. et al. (2015).
Phosphodiesterase 9A controls nitric-oxide-independent cGMP and hypertrophic
heart disease. Nature, 519(7544), 472-476. doi: 10.1038/nature14332
MANDY CASE STUDY
References
Anderson, L., Thompson, D., Oldridge, N., Zwisler, A., Rees, K., Martin, N., & Taylor, R.
(2016). Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane
Database Of Systematic Reviews. doi: 10.1002/14651858.cd001800.pub3
Bank, I., Gijsberts, C., Teng, T., Benson, L., Sim, D., & Yeo, P. et al. (2017). Prevalence and
Clinical Significance of Diabetes in Asian Versus White Patients With Heart Failure.
JACC: Heart Failure, 5(1), 14-24. doi: 10.1016/j.jchf.2016.09.015
Belialov, F. (2017). Depression, anxiety, and stress in patients with coronary heart disease.
Terapevticheskii Arkhiv, 89(8), 104. doi: 10.17116/terarkh2017898104-109
Chen, G., & Levy, D. (2016). Contributions of the Framingham Heart Study to the
Epidemiology of Coronary Heart Disease. JAMA Cardiology, 1(7), 825. doi:
10.1001/jamacardio.2016.2050
Circulation. (2017). Correction to: Heart Disease and Stroke Statistics—2017 Update: A
Report From the American Heart Association. Circulation, 135(10). doi:
10.1161/cir.0000000000000491
Eichstaedt, J., Schwartz, H., Kern, M., Park, G., Labarthe, D., & Merchant, R. et al. (2015).
Psychological Language on Twitter Predicts County-Level Heart Disease Mortality.
Psychological Science, 26(2), 159-169. doi: 10.1177/0956797614557867
Freed, B., Daruwalla, V., Cheng, J., Aguilar, F., Beussink, L., & Choi, A. et al. (2016).
Prognostic Utility and Clinical Significance of Cardiac Mechanics in Heart Failure
With Preserved Ejection Fraction. Circulation: Cardiovascular Imaging, 9(3). doi:
10.1161/circimaging.115.003754
Lee, D., Zhu, G., Sasaki, T., Cho, G., Hamdani, N., & Holewinski, R. et al. (2015).
Phosphodiesterase 9A controls nitric-oxide-independent cGMP and hypertrophic
heart disease. Nature, 519(7544), 472-476. doi: 10.1038/nature14332
11
MANDY CASE STUDY
Matiasz, R., & Rigolin, V. (2018). 2017 Focused Update for Management of Patients With
Valvular Heart Disease: Summary of New Recommendations. Journal Of The
American Heart Association, 7(1). doi: 10.1161/jaha.117.007596
Michael, M., Scharf, R., Letzkus, L., & Vergales, J. (2016). Improving Neurodevelopmental
Surveillance and Follow-up in Infants with Congenital Heart Disease. Congenital
Heart Disease, 11(2), 183-188. doi: 10.1111/chd.12333
Michael, M., Scharf, R., Letzkus, L., & Vergales, J. (2016). Improving Neurodevelopmental
Surveillance and Follow-up in Infants with Congenital Heart Disease. Congenital
Heart Disease, 11(2), 183-188. doi: 10.1111/chd.12333
Nature reviews. (2016). Acute rheumatic fever and rheumatic heart disease. Nature Reviews
Disease Primers, 2(1). doi: 10.1038/nrdp.2015.85
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals Of Translational
Medicine, 4(13), 256-256. doi: 10.21037/atm.2016.06.33
Shrivastava, A., Singh, H., Raizada, A., & Singh, S. (2015). C-reactive protein, inflammation
and coronary heart disease. The Egyptian Heart Journal, 67(2), 89-97. doi:
10.1016/j.ehj.2014.11.005
The Lancet. (2015). CT coronary angiography in patients with suspected angina due to
coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre
trial. The Lancet, 385(9985), 2383-2391. doi: 10.1016/s0140-6736(15)60291-4
Tokitsu, T., Yamamoto, E., Hirata, Y., & Ogawa, H. (2015). The Clinical Significance of
Pulse Pressure in Patients with Heart Failure with Preserved Ejection Fraction.
Journal Of Cardiac Failure, 21(10), S146. doi: 10.1016/j.cardfail.2015.08.011
MANDY CASE STUDY
Matiasz, R., & Rigolin, V. (2018). 2017 Focused Update for Management of Patients With
Valvular Heart Disease: Summary of New Recommendations. Journal Of The
American Heart Association, 7(1). doi: 10.1161/jaha.117.007596
Michael, M., Scharf, R., Letzkus, L., & Vergales, J. (2016). Improving Neurodevelopmental
Surveillance and Follow-up in Infants with Congenital Heart Disease. Congenital
Heart Disease, 11(2), 183-188. doi: 10.1111/chd.12333
Michael, M., Scharf, R., Letzkus, L., & Vergales, J. (2016). Improving Neurodevelopmental
Surveillance and Follow-up in Infants with Congenital Heart Disease. Congenital
Heart Disease, 11(2), 183-188. doi: 10.1111/chd.12333
Nature reviews. (2016). Acute rheumatic fever and rheumatic heart disease. Nature Reviews
Disease Primers, 2(1). doi: 10.1038/nrdp.2015.85
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals Of Translational
Medicine, 4(13), 256-256. doi: 10.21037/atm.2016.06.33
Shrivastava, A., Singh, H., Raizada, A., & Singh, S. (2015). C-reactive protein, inflammation
and coronary heart disease. The Egyptian Heart Journal, 67(2), 89-97. doi:
10.1016/j.ehj.2014.11.005
The Lancet. (2015). CT coronary angiography in patients with suspected angina due to
coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre
trial. The Lancet, 385(9985), 2383-2391. doi: 10.1016/s0140-6736(15)60291-4
Tokitsu, T., Yamamoto, E., Hirata, Y., & Ogawa, H. (2015). The Clinical Significance of
Pulse Pressure in Patients with Heart Failure with Preserved Ejection Fraction.
Journal Of Cardiac Failure, 21(10), S146. doi: 10.1016/j.cardfail.2015.08.011
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




