Health Care Management: Maori Infant Health and Immunization Report
VerifiedAdded on 2020/05/16
|19
|4759
|49
Report
AI Summary
This report investigates the health status of Maori infants in New Zealand, highlighting disparities in health outcomes compared to the general population, particularly concerning high infant hospitalization rates. It examines the relationship between low immunization coverage and increased hospitalization, supported by local and national health statistics. The report critically analyzes the New Zealand government's role in addressing these health inequities and proposes three recommendations grounded in the principles of Te Tiriti O Waitangi to improve health outcomes for Maori infants. The rationale behind each recommendation is thoroughly explained, demonstrating how these strategies aim to reduce disparities and promote better health for the Maori community. The report also reviews Maori immunization rates and the government's efforts to improve coverage, including the use of the National Immunization Register and other strategic initiatives. The findings underscore the need for tailored interventions and a stronger emphasis on addressing socioeconomic factors and improving communication between healthcare professionals and Maori families. The report provides a detailed overview of the challenges and potential solutions, including the need for the government to analyze patterns of coverage at the regional level, identify factors contributing to vaccine hesitancy in the Maori population, and enhance the timeliness of vaccination. The report concludes that by addressing the health issues of Maori infants, the government can play a vital role in reducing health disparities.

Running head: HEALTH CARE MANAGEMENT
Health care management
Name of the student:
Name of the University:
Author’s note
Health care management
Name of the student:
Name of the University:
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTH CARE MANAGEMENT
Executive summary:
Maori are over represented in many negative health statistics in New Zealand and
disparities in Maori infant health is one of the issue in the population group. The disparities in
health outcome of Maori infants compared to rest of the population has been seen mainly
because low immunization coverage in the group. This report has given an insight into the poorer
heath outcome in Maori infants using local and national health statistics related to immunization
rate and infant hospitalization rate in the country. The role of the government in addressing the
health issue has been examined and three recommendations have been proposed to address the
health issue applying the Principle of Te Teriti O Waitangi. The rationale for each
recommendation has been justified by explaining the ways in which the strategies target
inequities and promote health for Maori.
Executive summary:
Maori are over represented in many negative health statistics in New Zealand and
disparities in Maori infant health is one of the issue in the population group. The disparities in
health outcome of Maori infants compared to rest of the population has been seen mainly
because low immunization coverage in the group. This report has given an insight into the poorer
heath outcome in Maori infants using local and national health statistics related to immunization
rate and infant hospitalization rate in the country. The role of the government in addressing the
health issue has been examined and three recommendations have been proposed to address the
health issue applying the Principle of Te Teriti O Waitangi. The rationale for each
recommendation has been justified by explaining the ways in which the strategies target
inequities and promote health for Maori.
2HEALTH CARE MANAGEMENT
Table of Contents
Executive summary:........................................................................................................................1
Introduction:....................................................................................................................................3
Review of Maori immunization rate:...............................................................................................4
Role of government in addressing health issues for Maori:............................................................6
Using principle of Te Teriti O Waintangi to propose three recommendations to address the health
issue:................................................................................................................................................9
Rational for the recommendation:.................................................................................................10
Conclusion:....................................................................................................................................13
Reference.......................................................................................................................................14
Table of Contents
Executive summary:........................................................................................................................1
Introduction:....................................................................................................................................3
Review of Maori immunization rate:...............................................................................................4
Role of government in addressing health issues for Maori:............................................................6
Using principle of Te Teriti O Waintangi to propose three recommendations to address the health
issue:................................................................................................................................................9
Rational for the recommendation:.................................................................................................10
Conclusion:....................................................................................................................................13
Reference.......................................................................................................................................14
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTH CARE MANAGEMENT
Introduction:
The health status of Maori has been a major focus of attention among researchers because
of over-representation of Maori in many negative health statistics of New Zealand. Although
there are many illness or health issues that give insight into poor health outcome in Maoris,
however this report specifically looks at issues of high infant hospitalization rate in Maoris and
relation of the high infant hospitalization rate to immunization coverage for the population
group. With support from local and national health statistics, the report discusses about poor
immunization coverage in the population group. The report also provides a critical discussion on
the role of the government in addressing health inequities for Maoris. In addition, three
recommendations to address immunization issue are also presented by application of the
principles of Te Tiriti O Waitangi. Lastly, the rationale for each recommendation is discussed to
show how they can address health inequities and improve health outcomes for Maori.
Review of Maori immunization rate:
The immunization schedule for New Zealand mainly covers vaccines like Rotavirus, DPT
(Diptheria/Tetanus/Pertusis), measle, varicella and many other vaccines. Childhood respiratory
infection is a large burden of disease in New Zealand with lifelong health consequence. The
immunization schedule focuses on the delivery of special child immunization for pertussis and
influenza to reduce hospitalizations due to childhood respiratory infection (Chang et al., 2015).
Children have been hospitalized mainly for respiratory conditions, skin-related disorders and
dental problems. Due to high rate of hospitalization for respiratory infection, the Ministry of
Health in New Zealand has made asthma a priority area to reduce hospitalization rates among
children aged 0-4 years (Ministry of Health, 2017). One of the issues that have increased rate of
Introduction:
The health status of Maori has been a major focus of attention among researchers because
of over-representation of Maori in many negative health statistics of New Zealand. Although
there are many illness or health issues that give insight into poor health outcome in Maoris,
however this report specifically looks at issues of high infant hospitalization rate in Maoris and
relation of the high infant hospitalization rate to immunization coverage for the population
group. With support from local and national health statistics, the report discusses about poor
immunization coverage in the population group. The report also provides a critical discussion on
the role of the government in addressing health inequities for Maoris. In addition, three
recommendations to address immunization issue are also presented by application of the
principles of Te Tiriti O Waitangi. Lastly, the rationale for each recommendation is discussed to
show how they can address health inequities and improve health outcomes for Maori.
Review of Maori immunization rate:
The immunization schedule for New Zealand mainly covers vaccines like Rotavirus, DPT
(Diptheria/Tetanus/Pertusis), measle, varicella and many other vaccines. Childhood respiratory
infection is a large burden of disease in New Zealand with lifelong health consequence. The
immunization schedule focuses on the delivery of special child immunization for pertussis and
influenza to reduce hospitalizations due to childhood respiratory infection (Chang et al., 2015).
Children have been hospitalized mainly for respiratory conditions, skin-related disorders and
dental problems. Due to high rate of hospitalization for respiratory infection, the Ministry of
Health in New Zealand has made asthma a priority area to reduce hospitalization rates among
children aged 0-4 years (Ministry of Health, 2017). One of the issues that have increased rate of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HEALTH CARE MANAGEMENT
childhood hospitalization and deteriorated health of Maori infant is the poor rate of vaccination
coverage in the group. Hence, to find out the reason for poor infant health status, there is a need
assess immunization rates in the group. This is necessary because childhood vaccination is the
most effective strategy to prevent disease and reviewing the rate of coverage in Maori may
indicate the role of government in improving immunization uptake in the group (Ventola, 2016).
The Maori population experience great disparities in health compared to other population
group. Infant death rate is also one health indicator that shows the status of health in Maori
infants. High rate of infant hospitalization and infant mortality is a major health problem in
Maori. The local statistics on infants health in Rotorua has revealed that infant death rate in the
region was 7.0 per 1, 000 live births in 2011 (rotorualakescouncil.nz, 2011). In contrast, the
national rate for infant death was 75.2 per 1, 000 live births (health.govt.nz, 2011). This statistics
gives an idea about difference in rate between Maori population and non-Maori population. In
terms of infant hospitalization statistics, it has been found that high rate of children admission to
hospitals has occurred because of respiratory infections, skin infections and acute rheumatic
fever. For example, for there were about 1700 respiratory infection related hospitalization in
children per year between 2008 and 2012. The four conditions that were responsible for 80% of
respiratory hospitalization for children includes upper and lower respiratory infection,
pneumonia and bronchiolitis. The sudden increase in childhood hospitalization for respiratory
infection among Maori living in Rotorua district was mainly seen in 2008 and 2009. Over-
representation of childhood hospitalization data has been seen mainly for infant less than 1 year
(because of bronchiolitis) (Toi Te Ora Public Health Service, 2012).
The review of national and local statistics on hospitalization rate among Maoris in New
Zealand indicates that ambulatory sensitive hospitalization (ASH) is high in the group. ASH
childhood hospitalization and deteriorated health of Maori infant is the poor rate of vaccination
coverage in the group. Hence, to find out the reason for poor infant health status, there is a need
assess immunization rates in the group. This is necessary because childhood vaccination is the
most effective strategy to prevent disease and reviewing the rate of coverage in Maori may
indicate the role of government in improving immunization uptake in the group (Ventola, 2016).
The Maori population experience great disparities in health compared to other population
group. Infant death rate is also one health indicator that shows the status of health in Maori
infants. High rate of infant hospitalization and infant mortality is a major health problem in
Maori. The local statistics on infants health in Rotorua has revealed that infant death rate in the
region was 7.0 per 1, 000 live births in 2011 (rotorualakescouncil.nz, 2011). In contrast, the
national rate for infant death was 75.2 per 1, 000 live births (health.govt.nz, 2011). This statistics
gives an idea about difference in rate between Maori population and non-Maori population. In
terms of infant hospitalization statistics, it has been found that high rate of children admission to
hospitals has occurred because of respiratory infections, skin infections and acute rheumatic
fever. For example, for there were about 1700 respiratory infection related hospitalization in
children per year between 2008 and 2012. The four conditions that were responsible for 80% of
respiratory hospitalization for children includes upper and lower respiratory infection,
pneumonia and bronchiolitis. The sudden increase in childhood hospitalization for respiratory
infection among Maori living in Rotorua district was mainly seen in 2008 and 2009. Over-
representation of childhood hospitalization data has been seen mainly for infant less than 1 year
(because of bronchiolitis) (Toi Te Ora Public Health Service, 2012).
The review of national and local statistics on hospitalization rate among Maoris in New
Zealand indicates that ambulatory sensitive hospitalization (ASH) is high in the group. ASH
5HEALTH CARE MANAGEMENT
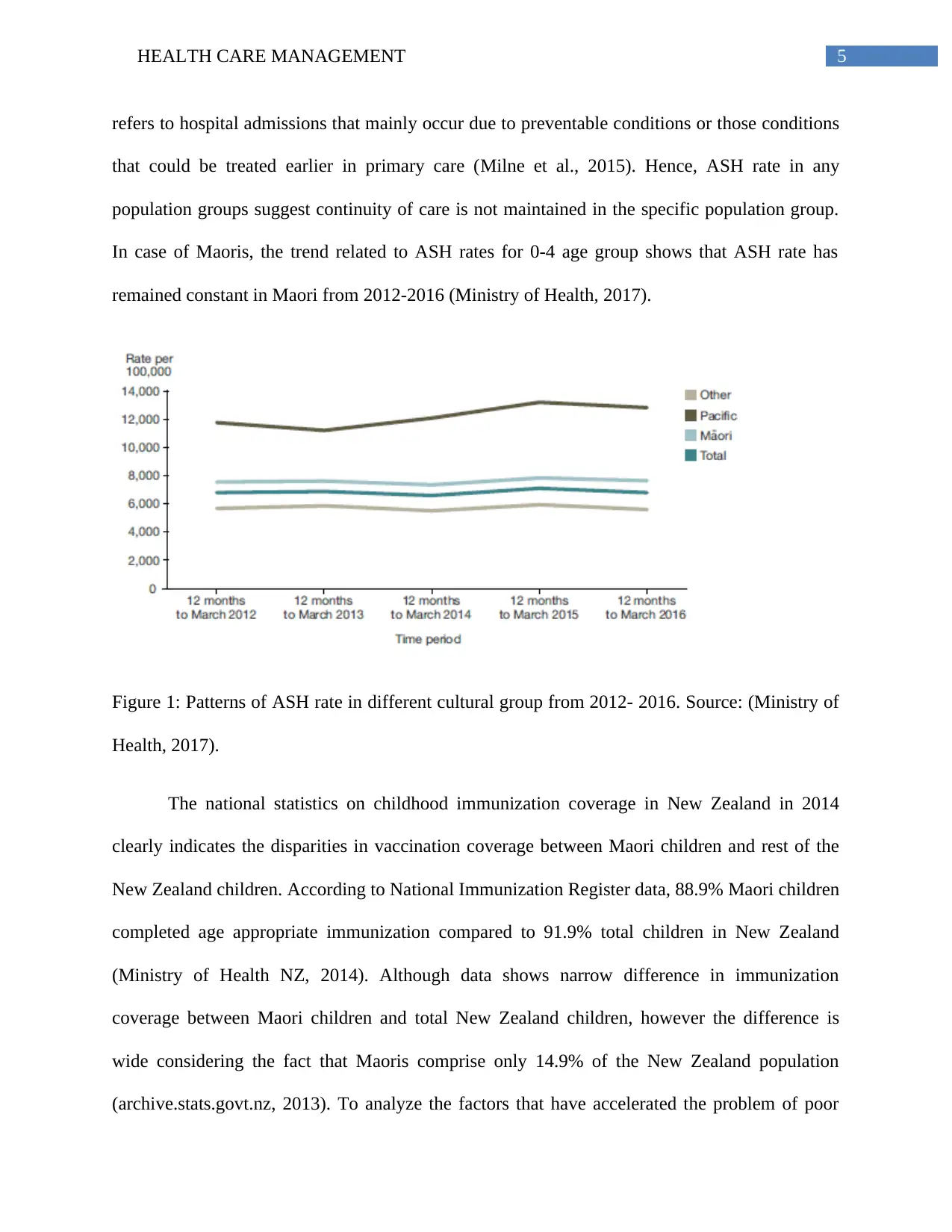
refers to hospital admissions that mainly occur due to preventable conditions or those conditions
that could be treated earlier in primary care (Milne et al., 2015). Hence, ASH rate in any
population groups suggest continuity of care is not maintained in the specific population group.
In case of Maoris, the trend related to ASH rates for 0-4 age group shows that ASH rate has
remained constant in Maori from 2012-2016 (Ministry of Health, 2017).
Figure 1: Patterns of ASH rate in different cultural group from 2012- 2016. Source: (Ministry of
Health, 2017).
The national statistics on childhood immunization coverage in New Zealand in 2014
clearly indicates the disparities in vaccination coverage between Maori children and rest of the
New Zealand children. According to National Immunization Register data, 88.9% Maori children
completed age appropriate immunization compared to 91.9% total children in New Zealand
(Ministry of Health NZ, 2014). Although data shows narrow difference in immunization
coverage between Maori children and total New Zealand children, however the difference is
wide considering the fact that Maoris comprise only 14.9% of the New Zealand population
(archive.stats.govt.nz, 2013). To analyze the factors that have accelerated the problem of poor
refers to hospital admissions that mainly occur due to preventable conditions or those conditions
that could be treated earlier in primary care (Milne et al., 2015). Hence, ASH rate in any
population groups suggest continuity of care is not maintained in the specific population group.
In case of Maoris, the trend related to ASH rates for 0-4 age group shows that ASH rate has
remained constant in Maori from 2012-2016 (Ministry of Health, 2017).
Figure 1: Patterns of ASH rate in different cultural group from 2012- 2016. Source: (Ministry of
Health, 2017).
The national statistics on childhood immunization coverage in New Zealand in 2014
clearly indicates the disparities in vaccination coverage between Maori children and rest of the
New Zealand children. According to National Immunization Register data, 88.9% Maori children
completed age appropriate immunization compared to 91.9% total children in New Zealand
(Ministry of Health NZ, 2014). Although data shows narrow difference in immunization
coverage between Maori children and total New Zealand children, however the difference is
wide considering the fact that Maoris comprise only 14.9% of the New Zealand population
(archive.stats.govt.nz, 2013). To analyze the factors that have accelerated the problem of poor
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6HEALTH CARE MANAGEMENT
infant’s health in Maori population, understanding the New Zealand’s government’s action in
addressing inequities in the group is necessary.
Role of government in addressing health issues for Maori:
The above national and local statistics proves that poor immunization coverage is a major
reason for poorer health outcome in Maori infants. As per the Maori health strategy, it is
necessary for health sector as well as government sector to work together with iwi (Maori
community) to improve their quality of life and reduce disparities compared to other New
Zealanders. However, Grant et al. (2010) has reported that immunization coverage has remained
lower than expected because of many structural and organization factors. This can be said
because the study showed that immunization coverage and timeliness differed in different areas.
Secondly, socio economic deprivation was also a dominant factor behind low rate of coverage.
The expected rate has not been achieved because there are still certain fractions of parents who
have declined vaccination. Children from Maori community do not get immunized at the same
rate as their peers. This is mainly because of lack of awareness, language differences and poverty
and deprivation in the group (Grant et al., 2010).
The review of health statistics of Maori infants in New Zealand has revealed that poor
immunization coverage rate and vaccine preventable disease is a challenge for the New Zealand
government today. One of the most significant issues in immunization coverage is the large
disparities for Maori children. To track the number of children who have immunized at birth,
New Zealand implemented a National Immunization Register (NIR). The NIR has helped to
track progress in immunization coverage and the data shows that equity gap is slowly decreasing
For example, the immunization rate has reached 80% by 2009 and by June 2011, it reached to
infant’s health in Maori population, understanding the New Zealand’s government’s action in
addressing inequities in the group is necessary.
Role of government in addressing health issues for Maori:
The above national and local statistics proves that poor immunization coverage is a major
reason for poorer health outcome in Maori infants. As per the Maori health strategy, it is
necessary for health sector as well as government sector to work together with iwi (Maori
community) to improve their quality of life and reduce disparities compared to other New
Zealanders. However, Grant et al. (2010) has reported that immunization coverage has remained
lower than expected because of many structural and organization factors. This can be said
because the study showed that immunization coverage and timeliness differed in different areas.
Secondly, socio economic deprivation was also a dominant factor behind low rate of coverage.
The expected rate has not been achieved because there are still certain fractions of parents who
have declined vaccination. Children from Maori community do not get immunized at the same
rate as their peers. This is mainly because of lack of awareness, language differences and poverty
and deprivation in the group (Grant et al., 2010).
The review of health statistics of Maori infants in New Zealand has revealed that poor
immunization coverage rate and vaccine preventable disease is a challenge for the New Zealand
government today. One of the most significant issues in immunization coverage is the large
disparities for Maori children. To track the number of children who have immunized at birth,
New Zealand implemented a National Immunization Register (NIR). The NIR has helped to
track progress in immunization coverage and the data shows that equity gap is slowly decreasing
For example, the immunization rate has reached 80% by 2009 and by June 2011, it reached to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTH CARE MANAGEMENT
90% (Turner 2012). The immunization coverage rate for Maori in 2011 was 88% (Turner 2012).
This has happened because of government policy and local health board attention. The New
Zealand Ministry of Health implemented many strategic goals to improve coverage. The NIR
tool was one of the strategies to monitor and report about immunization delivery. Introducing the
tool was a commendable act by the government as it helped to get real time data about
immunization coverage (Turner 2012). This supported staffs to give feedback about
immunization services. However, to achieve the target of 95% immunization coverage, New
Zealand governments needs to future actions to change the attitude of Maori parents regarding
immunization. This is because Maori people have poor perception about immunization and they
lack confidence in the effectiveness of vaccination process (Lee, Duck & Sibley, 2017).
Apart from improving records related to immunization coverage and vaccine delivery
through NIR tool, other strategies that New Zealand government implemented included
increasing surveillance for vaccine preventable disease and outbreak preparedness. However,
New Zealand government has not yet been successful in addressing poverty and family
characteristics of Maori people that creates barrier to achieving immunization targets. In case of
management system for immunization coverage, it was found that immunization program did not
worked in a stable manner because of poor staffing ratio (Turner 2012). Little evidence has been
found regarding the government’s role in supporting health care staffs for effective immunization
service delivery (Roberts et al., 2017). However, in the future, New Zealand government needs
to pay attention in this area because health care professionals have not been found to positively
engage with Maori children and their families (Grant & Reid, 2010). Hence, gap in knowledge
exist regarding effectively communicating with parents which is the most crucial aspect to
improve immunization coverage (Turner et al., 2017). The government should also pay
90% (Turner 2012). The immunization coverage rate for Maori in 2011 was 88% (Turner 2012).
This has happened because of government policy and local health board attention. The New
Zealand Ministry of Health implemented many strategic goals to improve coverage. The NIR
tool was one of the strategies to monitor and report about immunization delivery. Introducing the
tool was a commendable act by the government as it helped to get real time data about
immunization coverage (Turner 2012). This supported staffs to give feedback about
immunization services. However, to achieve the target of 95% immunization coverage, New
Zealand governments needs to future actions to change the attitude of Maori parents regarding
immunization. This is because Maori people have poor perception about immunization and they
lack confidence in the effectiveness of vaccination process (Lee, Duck & Sibley, 2017).
Apart from improving records related to immunization coverage and vaccine delivery
through NIR tool, other strategies that New Zealand government implemented included
increasing surveillance for vaccine preventable disease and outbreak preparedness. However,
New Zealand government has not yet been successful in addressing poverty and family
characteristics of Maori people that creates barrier to achieving immunization targets. In case of
management system for immunization coverage, it was found that immunization program did not
worked in a stable manner because of poor staffing ratio (Turner 2012). Little evidence has been
found regarding the government’s role in supporting health care staffs for effective immunization
service delivery (Roberts et al., 2017). However, in the future, New Zealand government needs
to pay attention in this area because health care professionals have not been found to positively
engage with Maori children and their families (Grant & Reid, 2010). Hence, gap in knowledge
exist regarding effectively communicating with parents which is the most crucial aspect to
improve immunization coverage (Turner et al., 2017). The government should also pay
8HEALTH CARE MANAGEMENT
emphasis on the role of Maori in health service planning to address the problem of
communication gaps between health professionals and clients. Maori participation in health
service delivery is part of the five principles of the New Zealand Health strategy and this is likely
to empower the community too (Ministry of Health NZ, 2018).
The review of New Zealand government’s role in immunization coverage has also
revealed that they have made improvement in immunization coverage because of prioritization of
immunization coverage in national policy. This was an effective step to implement funding and
implement financial barrier to accessing primary care service for children. However, the main
shortcoming of the strategy is that certain groups like Maori children have sub-optimal coverage
rate compared to other population groups in New Zealand. For example, people living in
Northland region particularly has lower coverage compared to national average. It is the least
urbanized region of the country and the higher percentages of Maori lives in the region. Only
87% of Northland babies were immunized till March 2015 (Rumball-Smith & Kenealy, 2016).
This means coverage is below the national target. There were some groups in low coverage who
did not received vaccines on a timely basis, whereas there were other groups whose caregivers
actively declines coverage. Hence, the government needs to address these issues in the future.
They need to analyze patterns of coverage at regional level and identify the factors contributes to
vaccine hesitancy in Maori population. This step can help the government to implement tailor
made interventions for groups who actively deny immunization for their child.
New Zealand government prioritized immunization coverage in health policy, however
timeliness is also one factor where the government need to take future action. This is because
receiving the first dose of primary vaccine on time is crucial to decrease susceptibility to vaccine
emphasis on the role of Maori in health service planning to address the problem of
communication gaps between health professionals and clients. Maori participation in health
service delivery is part of the five principles of the New Zealand Health strategy and this is likely
to empower the community too (Ministry of Health NZ, 2018).
The review of New Zealand government’s role in immunization coverage has also
revealed that they have made improvement in immunization coverage because of prioritization of
immunization coverage in national policy. This was an effective step to implement funding and
implement financial barrier to accessing primary care service for children. However, the main
shortcoming of the strategy is that certain groups like Maori children have sub-optimal coverage
rate compared to other population groups in New Zealand. For example, people living in
Northland region particularly has lower coverage compared to national average. It is the least
urbanized region of the country and the higher percentages of Maori lives in the region. Only
87% of Northland babies were immunized till March 2015 (Rumball-Smith & Kenealy, 2016).
This means coverage is below the national target. There were some groups in low coverage who
did not received vaccines on a timely basis, whereas there were other groups whose caregivers
actively declines coverage. Hence, the government needs to address these issues in the future.
They need to analyze patterns of coverage at regional level and identify the factors contributes to
vaccine hesitancy in Maori population. This step can help the government to implement tailor
made interventions for groups who actively deny immunization for their child.
New Zealand government prioritized immunization coverage in health policy, however
timeliness is also one factor where the government need to take future action. This is because
receiving the first dose of primary vaccine on time is crucial to decrease susceptibility to vaccine
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9HEALTH CARE MANAGEMENT
preventable disease in Maori children (Walton et al., 2017). Hence, the government should take
strategic steps to enhance timeliness of vaccination.
Using principle of Te Teriti O Waintangi to propose three recommendations to address the
health issue:
In response to the challenges found in immunization coverage for Maori population, the
problem can be addressed by using the principles of Te Teriti o Waitangi. The first principle is
the partnership principle that focuses on working in partnership with Maori communities to
develop health gain and improvement strategies. The second principles relates to participation of
Maoris in decision making, planning and delivery of care. The third principle is related to the
protection principle which states that the government has a role in safeguarding Maori and
preserving their cultural values and practices. All the three principles have been applied to
propose three recommendations to address immunization issues in Maori and improve infant
health outcomes.
The three recommendations that have been proposed to address immunization coverage issue
in Maori population include the following:
1. The first strategy is to increase the knowledge and confident of health care professionals
in effectively communicating with Maori families so that rate of missed opportunities to
immunization is reduced. This strategy has relevance with the protecting principles of the
Te Tiriti O Waitangi as increasing the skills of health care professionals will serve to
reduce missed opportunities of vaccination and protect Maori children from risk of
vaccine preventable disease. Taking step in this area is important because evidence has
preventable disease in Maori children (Walton et al., 2017). Hence, the government should take
strategic steps to enhance timeliness of vaccination.
Using principle of Te Teriti O Waintangi to propose three recommendations to address the
health issue:
In response to the challenges found in immunization coverage for Maori population, the
problem can be addressed by using the principles of Te Teriti o Waitangi. The first principle is
the partnership principle that focuses on working in partnership with Maori communities to
develop health gain and improvement strategies. The second principles relates to participation of
Maoris in decision making, planning and delivery of care. The third principle is related to the
protection principle which states that the government has a role in safeguarding Maori and
preserving their cultural values and practices. All the three principles have been applied to
propose three recommendations to address immunization issues in Maori and improve infant
health outcomes.
The three recommendations that have been proposed to address immunization coverage issue
in Maori population include the following:
1. The first strategy is to increase the knowledge and confident of health care professionals
in effectively communicating with Maori families so that rate of missed opportunities to
immunization is reduced. This strategy has relevance with the protecting principles of the
Te Tiriti O Waitangi as increasing the skills of health care professionals will serve to
reduce missed opportunities of vaccination and protect Maori children from risk of
vaccine preventable disease. Taking step in this area is important because evidence has
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10HEALTH CARE MANAGEMENT
revealed that poor health care staff confidence and knowledge towards immunization is a
barrier at practice level that creates inequities in coverage (Turner et al., 2017).
2. The second strategy to address the issue of immunization coverage is to implement health
education programme for Maori to change their attitude and perception towards
immunization coverage. This strategy is related to the partnership principle as
implementing educations programs with Maori people will help health promotion staffs
to effectively partner with them and facilitate health improvement. Maori’s perception
about the effectiveness of immunization has been proposed to reduce health inequity in
the population because research evidence proved that many of them do not immunize
their children because they do not felt the immunization was necessary or they distrusted
vaccines for its effectiveness (Guiney & Walton, 2014).
3. The third strategy is to involve Maori in immunization service delivery to increase the
gap in communication and enhance timeliness of immunization process. This strategy is
relevant to the participation principle of Te Tiriti O Waitnagi as it will be an opportunity
to bring Maori people in immunization service planning. It will also reduce socio-
cultural and communication barrier in immunization coverage (Veerasingam et al., 2017).
Rational for the recommendation:
1. The first recommendation of improving staff’s knowledge towards vaccination and
communicating with Maori people is necessary as it would help to enhance engagement
with Maori parents. This is crucial because better engagement with Maori families can
help them be aware about immunization schedule and not miss opportunities for
immunizing their children on time. Secondly, skills of health care staffs towards
immunization services and communicating with Maori people is necessary as it would
revealed that poor health care staff confidence and knowledge towards immunization is a
barrier at practice level that creates inequities in coverage (Turner et al., 2017).
2. The second strategy to address the issue of immunization coverage is to implement health
education programme for Maori to change their attitude and perception towards
immunization coverage. This strategy is related to the partnership principle as
implementing educations programs with Maori people will help health promotion staffs
to effectively partner with them and facilitate health improvement. Maori’s perception
about the effectiveness of immunization has been proposed to reduce health inequity in
the population because research evidence proved that many of them do not immunize
their children because they do not felt the immunization was necessary or they distrusted
vaccines for its effectiveness (Guiney & Walton, 2014).
3. The third strategy is to involve Maori in immunization service delivery to increase the
gap in communication and enhance timeliness of immunization process. This strategy is
relevant to the participation principle of Te Tiriti O Waitnagi as it will be an opportunity
to bring Maori people in immunization service planning. It will also reduce socio-
cultural and communication barrier in immunization coverage (Veerasingam et al., 2017).
Rational for the recommendation:
1. The first recommendation of improving staff’s knowledge towards vaccination and
communicating with Maori people is necessary as it would help to enhance engagement
with Maori parents. This is crucial because better engagement with Maori families can
help them be aware about immunization schedule and not miss opportunities for
immunizing their children on time. Secondly, skills of health care staffs towards
immunization services and communicating with Maori people is necessary as it would
11HEALTH CARE MANAGEMENT
support primary care to have a confident and engaged health care professional who can
pay full attention to coverage schedule and missed cases of immunization (Grant et al,
2010). A confident health care professional can stabilize the immunization program and
take the right steps to minimize missed opportunities of immunization. Providing
culturally competent communication skill training may also help staffs in relationship
building (Turner et al., 2017). For example, they can inform new parents about
immunization and answer to the queries of parents when they come for their child’s
immunization for the first time.
2. The second recommendation of addressing Maori people’s attitude towards immunization
can be effectiveness in achieving target immunization rate because changing parent’s and
Maori family’s attitude towards immunization can increase the likelihood of receiving
first dose of vaccination on time. Lee, Duck and Sibley (2017) has investigated about
skeptical attitude towards safety of childhood immunization in New Zealand population.
The demographic and personality correlates of people revealed that lower confidence was
found in Maori people and people living in rural areas. In contrast, high income and
educational attainment was associated with greater confidence for immunization. This
finding gives implications to the New Zealand government that public education about
necessity of vaccination is necessary to address the issues of infant health and
preventable disease in Maori infants (Odone et al., 2015). Hence, in accordance with this
evidence too, educating parents regarding necessity of vaccination can positively
influence parent’s attitude towards vaccination.
Low education and health literacy is the factor leading to poor perceptions about
immunization in Maori people. Hence, Maori parents can be empowered by providing them
support primary care to have a confident and engaged health care professional who can
pay full attention to coverage schedule and missed cases of immunization (Grant et al,
2010). A confident health care professional can stabilize the immunization program and
take the right steps to minimize missed opportunities of immunization. Providing
culturally competent communication skill training may also help staffs in relationship
building (Turner et al., 2017). For example, they can inform new parents about
immunization and answer to the queries of parents when they come for their child’s
immunization for the first time.
2. The second recommendation of addressing Maori people’s attitude towards immunization
can be effectiveness in achieving target immunization rate because changing parent’s and
Maori family’s attitude towards immunization can increase the likelihood of receiving
first dose of vaccination on time. Lee, Duck and Sibley (2017) has investigated about
skeptical attitude towards safety of childhood immunization in New Zealand population.
The demographic and personality correlates of people revealed that lower confidence was
found in Maori people and people living in rural areas. In contrast, high income and
educational attainment was associated with greater confidence for immunization. This
finding gives implications to the New Zealand government that public education about
necessity of vaccination is necessary to address the issues of infant health and
preventable disease in Maori infants (Odone et al., 2015). Hence, in accordance with this
evidence too, educating parents regarding necessity of vaccination can positively
influence parent’s attitude towards vaccination.
Low education and health literacy is the factor leading to poor perceptions about
immunization in Maori people. Hence, Maori parents can be empowered by providing them
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





