Case Study: Nursing Care for Maria's Unconjugated Hyperbilirubinemia
VerifiedAdded on 2022/10/06
|11
|3117
|351
Case Study
AI Summary
This case study analyzes the case of Maria, a newborn diagnosed with breastfeeding-associated unconjugated hyperbilirubinemia. The assignment details Maria's condition, including vital signs, risk factors, and the Bhutani nomogram assessment. It explores the nursing diagnosis, which is breastfeeding-associated unconjugated hyperbilirubinemia related to poor latching, evidenced by dehydration, yellow skin, and weight loss. The study outlines a comprehensive care plan, emphasizing increased feeding frequency, lactation consultation, and family-centered interventions. It also discusses the implications of Maria's condition on her psychosocial development, based on Erikson's stages, and highlights the potential for complications like bilirubin-induced neurologic dysfunction (BIND) if the condition is not addressed. The interventions include lactation consultation, increased feeding, and family education to improve breastfeeding and monitor the baby's health. This comprehensive approach aims to reduce bilirubin levels, improve weight gain, and promote the newborn's well-being, emphasizing the importance of early intervention and ongoing monitoring.
Nursing interventions in treating
unconjugated hyperbilirubinemia in
newborn infants
unconjugated hyperbilirubinemia in
newborn infants
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1. On first day, the vital signs of Maria were: Temperature 37, Heart rate 130-155, Respiratory
rate 32-55, SpO2 99% and pain N-PASS 0. She was calm, feeding well every 4 hours, had
soft flat fontanelles, with intact reflexes, normal cardiac and respiratory signs. Her first stool
was normal with a little yellowish coloring in the night, with normal passage of colorless
urine and having pink skin and moist mouth. Her weight was 4.5kg, and length 52cms.
The vital signs from the second day showed a decline in some features. Her temperature was
on the incline at 37.2, Heart rate 165 above normalcy, Respiratory rate 44, and N-PASS at 5
suggesting irritability. She was less comfortable, showing clear signs of irritation and crying
at pitched voice, having sunken yet soft fontanelles suggesting dehydration (Mansor et al.,
2012).
This was more closely observed upon dry mucous membranes in mouth, which deviated from
normal. She was dehydrated, passed little urine and had yellow colored stool. Although her
skin was clean dry, in place of pink coloration she was starting to have a yellow tint on her
face, moving downwards towards her bilateral nipple line, which was early signs of
developing neo-natal jaundice (Maisels et al., 2014). Upon weighing, she had decreased in
weight and currently stood at 4.25kg with decline of 250 grams, implicating abnormal
conditions. Moreover, upon talking with parents, it was understood that Maria had not been
feeding well on breast milk, and was tired, not latching to nipples properly and was irritated.
All the signs show abnormal trends towards developing jaundiced tendencies, with
drowsiness, poor feeding, coloration in stool, yellow tint in skin, irritability, dehydration and
decrease in weight (Amos, Jacob & Leith, 2017).
2.
Situation (S) Maria is a 48 hour baby, with gestation period >38 weeks, showing
abnormal signs in some vital stats from the 2nd day of life. She is
dehydrated, has yellow stool and tint in skin, drowsy, irritated, dehydrated
mouth, less urine discharges, and decline in birth weight.
Background (B) Maria’s mother had been 2 times pregnant before with 2 abortions, and
rate 32-55, SpO2 99% and pain N-PASS 0. She was calm, feeding well every 4 hours, had
soft flat fontanelles, with intact reflexes, normal cardiac and respiratory signs. Her first stool
was normal with a little yellowish coloring in the night, with normal passage of colorless
urine and having pink skin and moist mouth. Her weight was 4.5kg, and length 52cms.
The vital signs from the second day showed a decline in some features. Her temperature was
on the incline at 37.2, Heart rate 165 above normalcy, Respiratory rate 44, and N-PASS at 5
suggesting irritability. She was less comfortable, showing clear signs of irritation and crying
at pitched voice, having sunken yet soft fontanelles suggesting dehydration (Mansor et al.,
2012).
This was more closely observed upon dry mucous membranes in mouth, which deviated from
normal. She was dehydrated, passed little urine and had yellow colored stool. Although her
skin was clean dry, in place of pink coloration she was starting to have a yellow tint on her
face, moving downwards towards her bilateral nipple line, which was early signs of
developing neo-natal jaundice (Maisels et al., 2014). Upon weighing, she had decreased in
weight and currently stood at 4.25kg with decline of 250 grams, implicating abnormal
conditions. Moreover, upon talking with parents, it was understood that Maria had not been
feeding well on breast milk, and was tired, not latching to nipples properly and was irritated.
All the signs show abnormal trends towards developing jaundiced tendencies, with
drowsiness, poor feeding, coloration in stool, yellow tint in skin, irritability, dehydration and
decrease in weight (Amos, Jacob & Leith, 2017).
2.
Situation (S) Maria is a 48 hour baby, with gestation period >38 weeks, showing
abnormal signs in some vital stats from the 2nd day of life. She is
dehydrated, has yellow stool and tint in skin, drowsy, irritated, dehydrated
mouth, less urine discharges, and decline in birth weight.
Background (B) Maria’s mother had been 2 times pregnant before with 2 abortions, and
Maria was a vaginal delivery case. Her APGAR score 1 minute after birth
was 8 and 9 after 5 minutes. She was 4.5kgs, 52cms length and head
circumference 36cms. She has blood group O negative like her mother. Her
mother had intake of Selective Serotonin Reuptake Inhibitor
Antidepressants like Fluoxetine before pregnancy along with RhoGam
during the 28th week. All her reflexes are normal, with good cardio and
respiratory signs, no birthmark, bruising or lesions.
Assessment (A) Upon assessment she is dehydrated, with sunken flontanelles, dry mouth
and less urine discharge. Stool is yellow, along with skin color. She is
drowsy, irritated, and not feeding properly (Whyte, 2012). Her weight has
decreased and she is lethargic. Assessment stats signify high chances of
unconjugated hyperbilirubinemia.
Recommendation
(R)
Show pediatrician the abnormal signs and get checked immediately, along
with checking for blood serum levels and bilirubin levels, and further
postponing discharge for a few days, until vital-stats are normal.
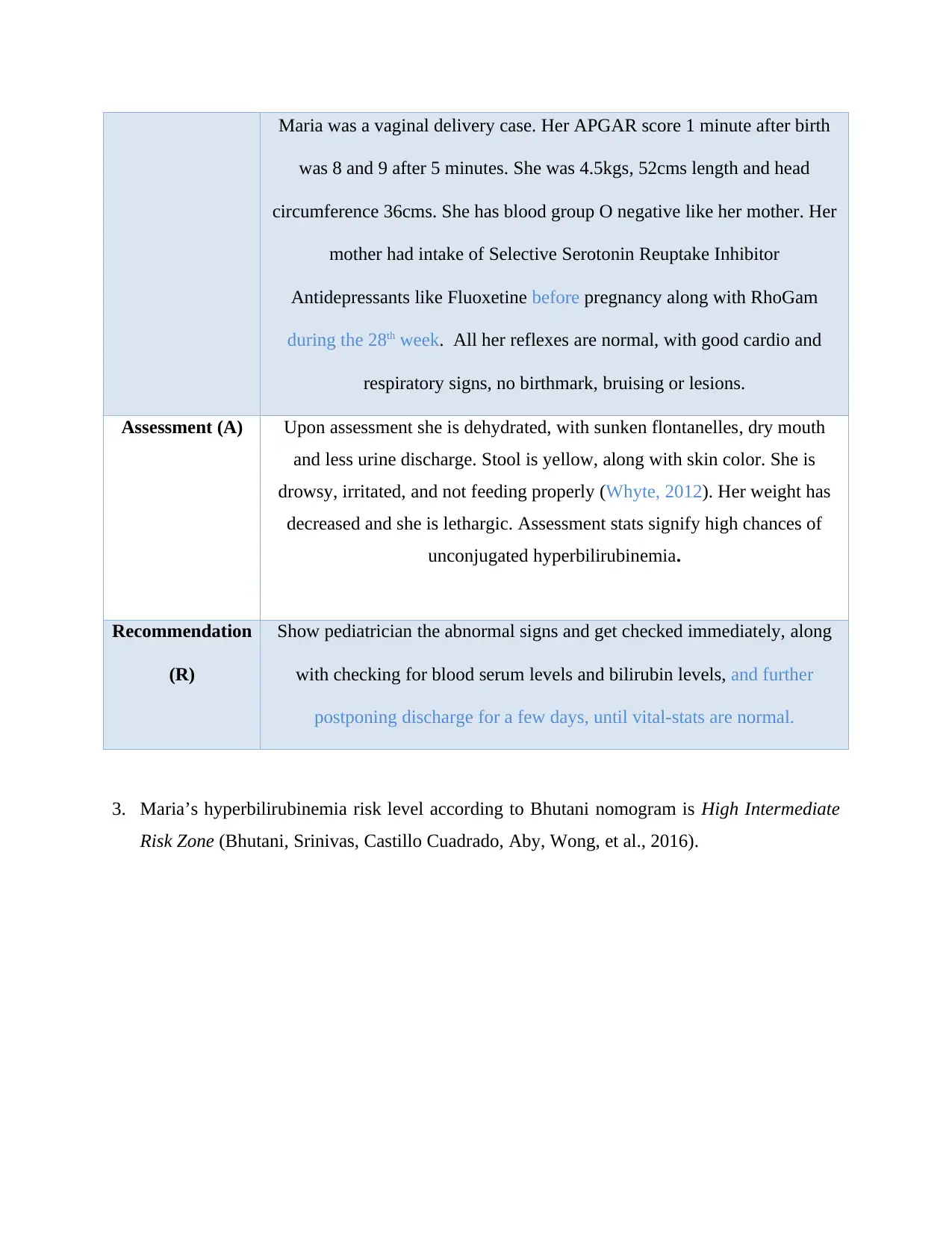
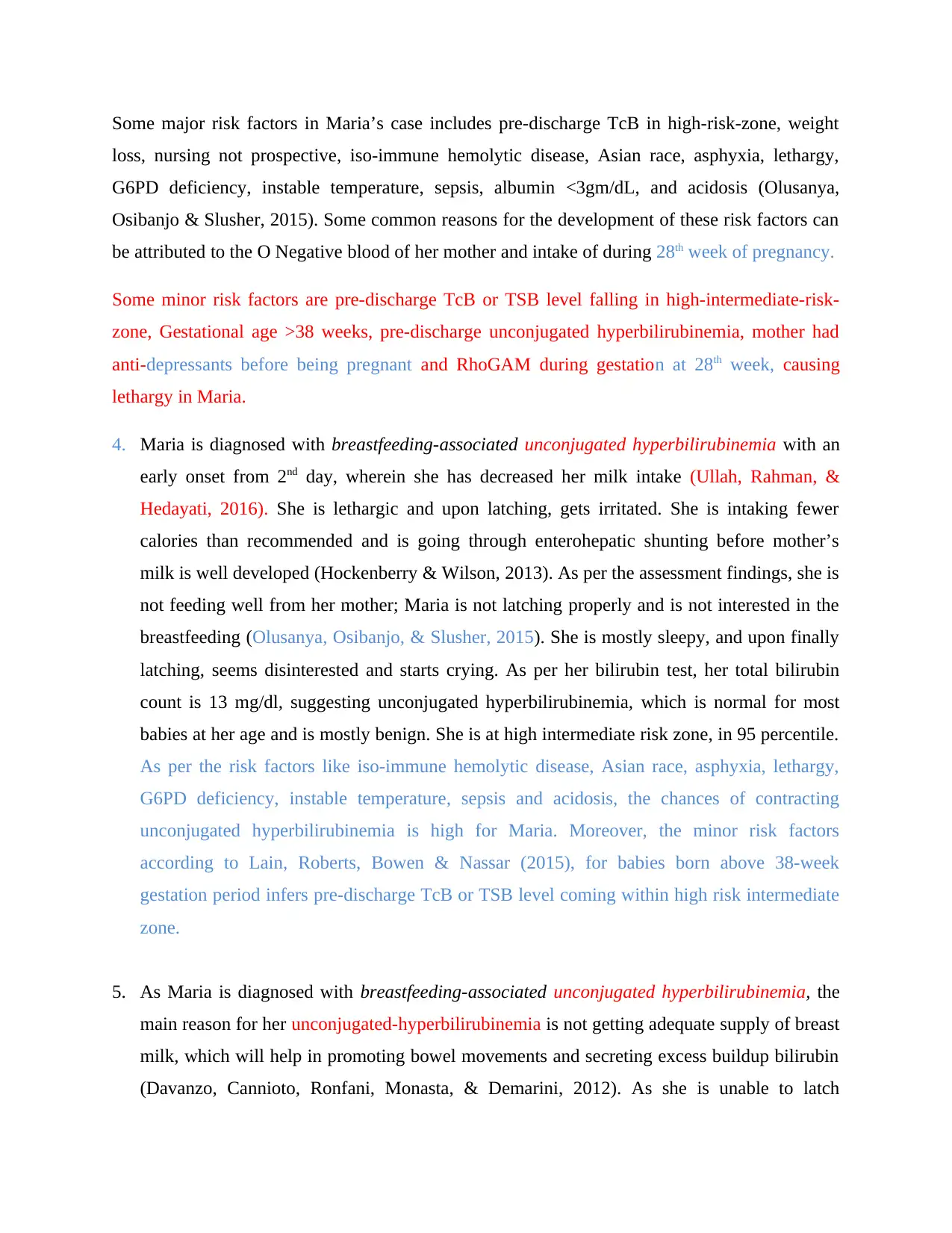
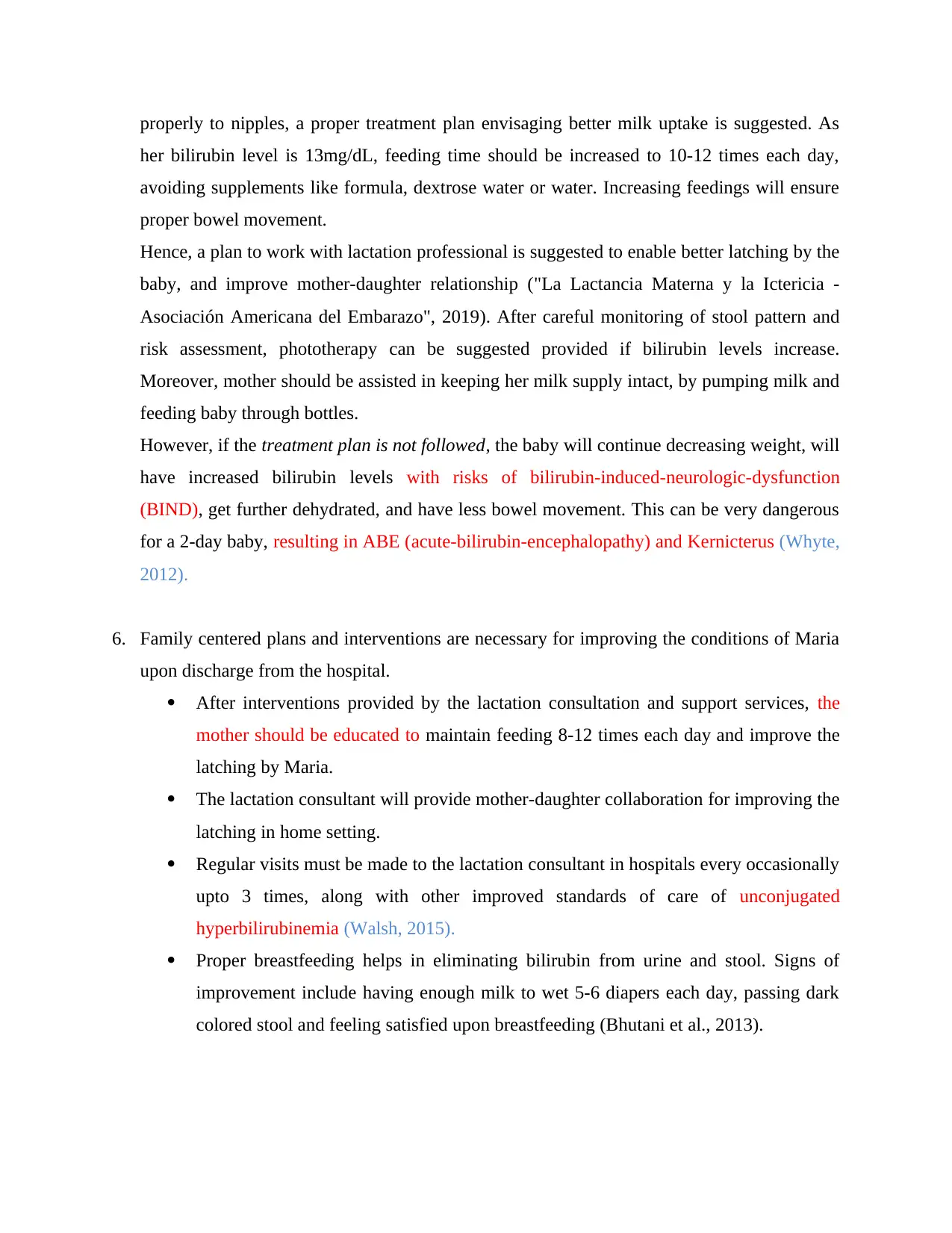
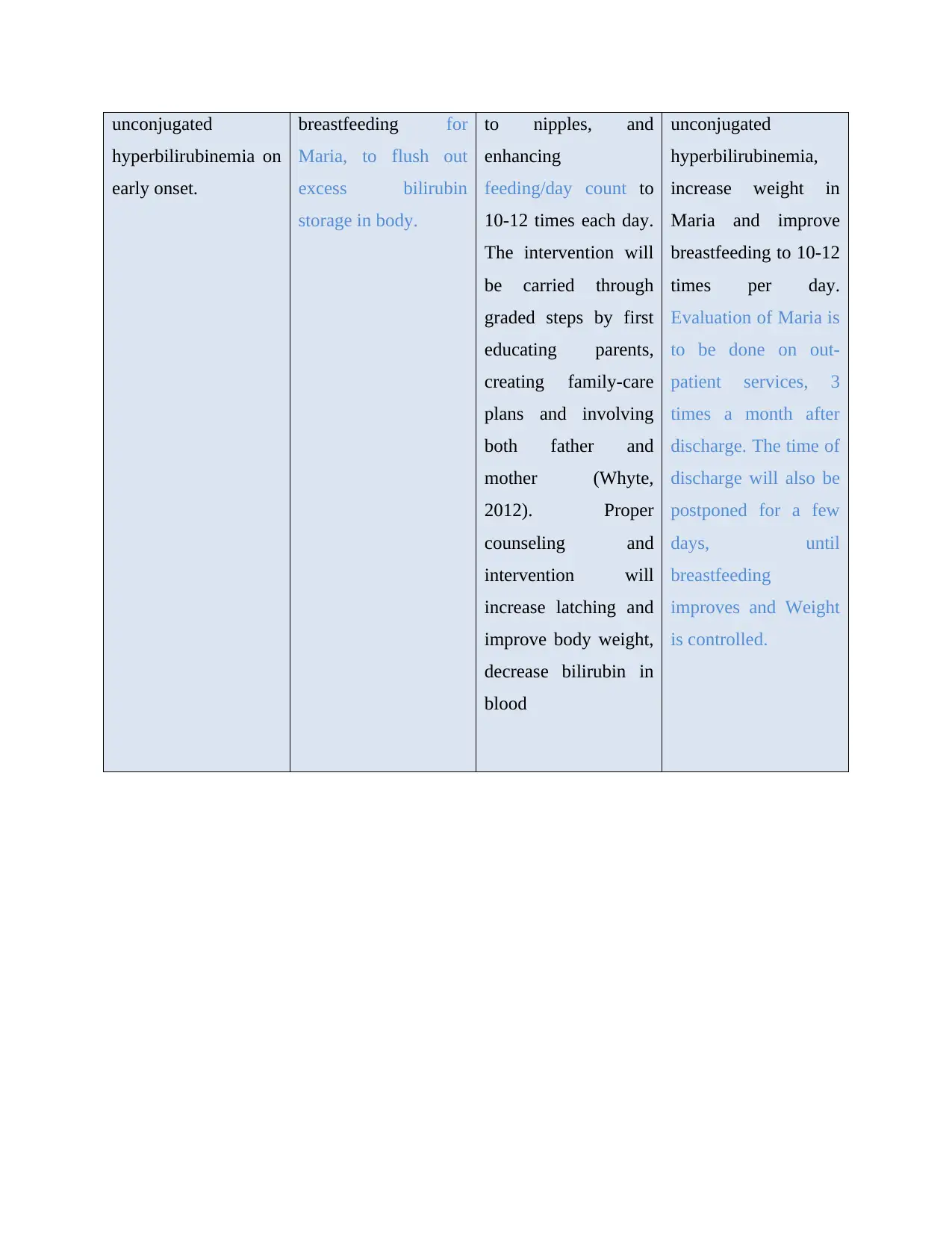
3. Maria’s hyperbilirubinemia risk level according to Bhutani nomogram is High Intermediate
Risk Zone (Bhutani, Srinivas, Castillo Cuadrado, Aby, Wong, et al., 2016).
was 8 and 9 after 5 minutes. She was 4.5kgs, 52cms length and head
circumference 36cms. She has blood group O negative like her mother. Her
mother had intake of Selective Serotonin Reuptake Inhibitor
Antidepressants like Fluoxetine before pregnancy along with RhoGam
during the 28th week. All her reflexes are normal, with good cardio and
respiratory signs, no birthmark, bruising or lesions.
Assessment (A) Upon assessment she is dehydrated, with sunken flontanelles, dry mouth
and less urine discharge. Stool is yellow, along with skin color. She is
drowsy, irritated, and not feeding properly (Whyte, 2012). Her weight has
decreased and she is lethargic. Assessment stats signify high chances of
unconjugated hyperbilirubinemia.
Recommendation
(R)
Show pediatrician the abnormal signs and get checked immediately, along
with checking for blood serum levels and bilirubin levels, and further
postponing discharge for a few days, until vital-stats are normal.
3. Maria’s hyperbilirubinemia risk level according to Bhutani nomogram is High Intermediate
Risk Zone (Bhutani, Srinivas, Castillo Cuadrado, Aby, Wong, et al., 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
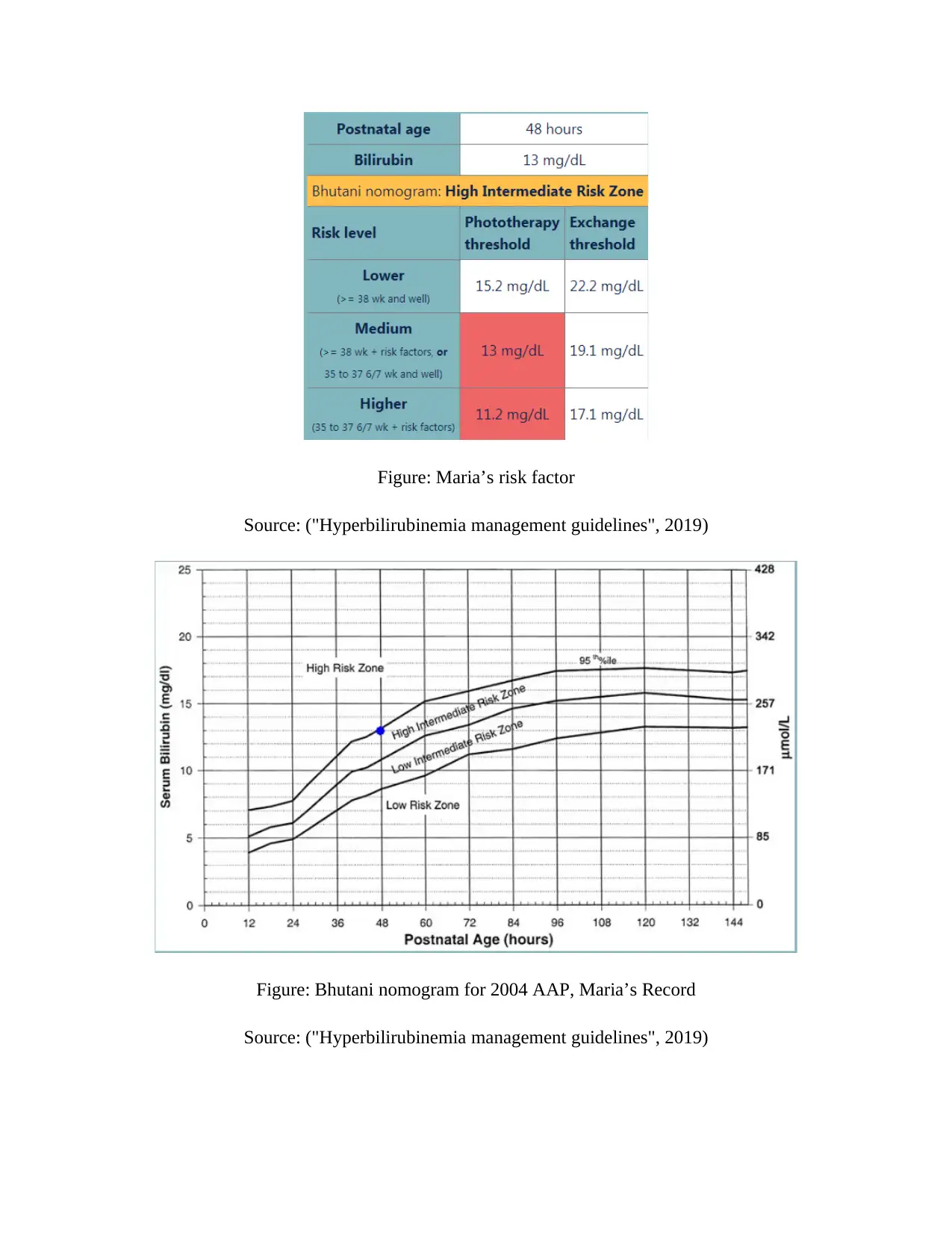
Figure: Maria’s risk factor
Source: ("Hyperbilirubinemia management guidelines", 2019)
Figure: Bhutani nomogram for 2004 AAP, Maria’s Record
Source: ("Hyperbilirubinemia management guidelines", 2019)
Source: ("Hyperbilirubinemia management guidelines", 2019)
Figure: Bhutani nomogram for 2004 AAP, Maria’s Record
Source: ("Hyperbilirubinemia management guidelines", 2019)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Some major risk factors in Maria’s case includes pre-discharge TcB in high-risk-zone, weight
loss, nursing not prospective, iso-immune hemolytic disease, Asian race, asphyxia, lethargy,
G6PD deficiency, instable temperature, sepsis, albumin <3gm/dL, and acidosis (Olusanya,
Osibanjo & Slusher, 2015). Some common reasons for the development of these risk factors can
be attributed to the O Negative blood of her mother and intake of during 28th week of pregnancy.
Some minor risk factors are pre-discharge TcB or TSB level falling in high-intermediate-risk-
zone, Gestational age >38 weeks, pre-discharge unconjugated hyperbilirubinemia, mother had
anti-depressants before being pregnant and RhoGAM during gestation at 28th week, causing
lethargy in Maria.
4. Maria is diagnosed with breastfeeding-associated unconjugated hyperbilirubinemia with an
early onset from 2nd day, wherein she has decreased her milk intake (Ullah, Rahman, &
Hedayati, 2016). She is lethargic and upon latching, gets irritated. She is intaking fewer
calories than recommended and is going through enterohepatic shunting before mother’s
milk is well developed (Hockenberry & Wilson, 2013). As per the assessment findings, she is
not feeding well from her mother; Maria is not latching properly and is not interested in the
breastfeeding (Olusanya, Osibanjo, & Slusher, 2015). She is mostly sleepy, and upon finally
latching, seems disinterested and starts crying. As per her bilirubin test, her total bilirubin
count is 13 mg/dl, suggesting unconjugated hyperbilirubinemia, which is normal for most
babies at her age and is mostly benign. She is at high intermediate risk zone, in 95 percentile.
As per the risk factors like iso-immune hemolytic disease, Asian race, asphyxia, lethargy,
G6PD deficiency, instable temperature, sepsis and acidosis, the chances of contracting
unconjugated hyperbilirubinemia is high for Maria. Moreover, the minor risk factors
according to Lain, Roberts, Bowen & Nassar (2015), for babies born above 38-week
gestation period infers pre-discharge TcB or TSB level coming within high risk intermediate
zone.
5. As Maria is diagnosed with breastfeeding-associated unconjugated hyperbilirubinemia, the
main reason for her unconjugated-hyperbilirubinemia is not getting adequate supply of breast
milk, which will help in promoting bowel movements and secreting excess buildup bilirubin
(Davanzo, Cannioto, Ronfani, Monasta, & Demarini, 2012). As she is unable to latch
loss, nursing not prospective, iso-immune hemolytic disease, Asian race, asphyxia, lethargy,
G6PD deficiency, instable temperature, sepsis, albumin <3gm/dL, and acidosis (Olusanya,
Osibanjo & Slusher, 2015). Some common reasons for the development of these risk factors can
be attributed to the O Negative blood of her mother and intake of during 28th week of pregnancy.
Some minor risk factors are pre-discharge TcB or TSB level falling in high-intermediate-risk-
zone, Gestational age >38 weeks, pre-discharge unconjugated hyperbilirubinemia, mother had
anti-depressants before being pregnant and RhoGAM during gestation at 28th week, causing
lethargy in Maria.
4. Maria is diagnosed with breastfeeding-associated unconjugated hyperbilirubinemia with an
early onset from 2nd day, wherein she has decreased her milk intake (Ullah, Rahman, &
Hedayati, 2016). She is lethargic and upon latching, gets irritated. She is intaking fewer
calories than recommended and is going through enterohepatic shunting before mother’s
milk is well developed (Hockenberry & Wilson, 2013). As per the assessment findings, she is
not feeding well from her mother; Maria is not latching properly and is not interested in the
breastfeeding (Olusanya, Osibanjo, & Slusher, 2015). She is mostly sleepy, and upon finally
latching, seems disinterested and starts crying. As per her bilirubin test, her total bilirubin
count is 13 mg/dl, suggesting unconjugated hyperbilirubinemia, which is normal for most
babies at her age and is mostly benign. She is at high intermediate risk zone, in 95 percentile.
As per the risk factors like iso-immune hemolytic disease, Asian race, asphyxia, lethargy,
G6PD deficiency, instable temperature, sepsis and acidosis, the chances of contracting
unconjugated hyperbilirubinemia is high for Maria. Moreover, the minor risk factors
according to Lain, Roberts, Bowen & Nassar (2015), for babies born above 38-week
gestation period infers pre-discharge TcB or TSB level coming within high risk intermediate
zone.
5. As Maria is diagnosed with breastfeeding-associated unconjugated hyperbilirubinemia, the
main reason for her unconjugated-hyperbilirubinemia is not getting adequate supply of breast
milk, which will help in promoting bowel movements and secreting excess buildup bilirubin
(Davanzo, Cannioto, Ronfani, Monasta, & Demarini, 2012). As she is unable to latch
properly to nipples, a proper treatment plan envisaging better milk uptake is suggested. As
her bilirubin level is 13mg/dL, feeding time should be increased to 10-12 times each day,
avoiding supplements like formula, dextrose water or water. Increasing feedings will ensure
proper bowel movement.
Hence, a plan to work with lactation professional is suggested to enable better latching by the
baby, and improve mother-daughter relationship ("La Lactancia Materna y la Ictericia -
Asociación Americana del Embarazo", 2019). After careful monitoring of stool pattern and
risk assessment, phototherapy can be suggested provided if bilirubin levels increase.
Moreover, mother should be assisted in keeping her milk supply intact, by pumping milk and
feeding baby through bottles.
However, if the treatment plan is not followed, the baby will continue decreasing weight, will
have increased bilirubin levels with risks of bilirubin-induced-neurologic-dysfunction
(BIND), get further dehydrated, and have less bowel movement. This can be very dangerous
for a 2-day baby, resulting in ABE (acute-bilirubin-encephalopathy) and Kernicterus (Whyte,
2012).
6. Family centered plans and interventions are necessary for improving the conditions of Maria
upon discharge from the hospital.
After interventions provided by the lactation consultation and support services, the
mother should be educated to maintain feeding 8-12 times each day and improve the
latching by Maria.
The lactation consultant will provide mother-daughter collaboration for improving the
latching in home setting.
Regular visits must be made to the lactation consultant in hospitals every occasionally
upto 3 times, along with other improved standards of care of unconjugated
hyperbilirubinemia (Walsh, 2015).
Proper breastfeeding helps in eliminating bilirubin from urine and stool. Signs of
improvement include having enough milk to wet 5-6 diapers each day, passing dark
colored stool and feeling satisfied upon breastfeeding (Bhutani et al., 2013).
her bilirubin level is 13mg/dL, feeding time should be increased to 10-12 times each day,
avoiding supplements like formula, dextrose water or water. Increasing feedings will ensure
proper bowel movement.
Hence, a plan to work with lactation professional is suggested to enable better latching by the
baby, and improve mother-daughter relationship ("La Lactancia Materna y la Ictericia -
Asociación Americana del Embarazo", 2019). After careful monitoring of stool pattern and
risk assessment, phototherapy can be suggested provided if bilirubin levels increase.
Moreover, mother should be assisted in keeping her milk supply intact, by pumping milk and
feeding baby through bottles.
However, if the treatment plan is not followed, the baby will continue decreasing weight, will
have increased bilirubin levels with risks of bilirubin-induced-neurologic-dysfunction
(BIND), get further dehydrated, and have less bowel movement. This can be very dangerous
for a 2-day baby, resulting in ABE (acute-bilirubin-encephalopathy) and Kernicterus (Whyte,
2012).
6. Family centered plans and interventions are necessary for improving the conditions of Maria
upon discharge from the hospital.
After interventions provided by the lactation consultation and support services, the
mother should be educated to maintain feeding 8-12 times each day and improve the
latching by Maria.
The lactation consultant will provide mother-daughter collaboration for improving the
latching in home setting.
Regular visits must be made to the lactation consultant in hospitals every occasionally
upto 3 times, along with other improved standards of care of unconjugated
hyperbilirubinemia (Walsh, 2015).
Proper breastfeeding helps in eliminating bilirubin from urine and stool. Signs of
improvement include having enough milk to wet 5-6 diapers each day, passing dark
colored stool and feeling satisfied upon breastfeeding (Bhutani et al., 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The implementation plan can be started with frequent visits and follow ups from
lactation expert and consultants on proper latching by baby, and frequent visits to
hospital to get baby’s health assessed in a month.
Meeting with pediatricians regularly, planning nurse home visits and newborn
nursery are important for tackling neonatal unconjugated hyperbilirubinemia in
Maria’s case.
7. According to Svetina (2014), there are 8 stages in Erikson's-Psychosocial-Development-
Theory from infancy to adulthood in psychosocial development, wherein people face
psychosocial crises and derive negative or positive traits in their personality which exists
throughout their life. The 8 stages are divided according to ages namely, 0-1.5years, 1.5-
3years, 3-5years, 5-12years, 12-18years, 18-40years, 40-65years, and above 65years. The
crises are trust-mistrust, autonomy-shame, initiative-guilt, industry-inferiority, identity-role
confusion, intimacy-isolation, generativity-stagnation and ego integrity-despair (Svetina,
2014).
Maria is in the first stage of trust-mistrust, wherein the basic virtue, which can develop in
her, is hope. During this stage as she is uncertain about her environment, she will trust people
when her gratifications are met and will mistrust people when her care is unpredictable,
inconsistent and unreliable. This is characterized by anxiety, insecurity and mistrust if her
care is not taken care of (Lerwick, 2013). As she suffers from unconjugated
hyperbilirubinemia, her senses are more pronounced than other babies are. If she is
hospitalized frequently, it will have an effect in her psychosocial development. If her
condition worsens she might have to get phototherapy which will increase her stay in
hospital. Here, her primary caregivers will be health-care professionals and nurses who will
deftly respond and meet all her physical requirements developing security and trust. Upon
comparison however, prolonged hospitalization may start to make her feel sicker than other
children, which will impact her way of self-visualizing herself (Olusanya, Osibanjo, &
Slusher, 2015).
8. Nursing diagnosis
lactation expert and consultants on proper latching by baby, and frequent visits to
hospital to get baby’s health assessed in a month.
Meeting with pediatricians regularly, planning nurse home visits and newborn
nursery are important for tackling neonatal unconjugated hyperbilirubinemia in
Maria’s case.
7. According to Svetina (2014), there are 8 stages in Erikson's-Psychosocial-Development-
Theory from infancy to adulthood in psychosocial development, wherein people face
psychosocial crises and derive negative or positive traits in their personality which exists
throughout their life. The 8 stages are divided according to ages namely, 0-1.5years, 1.5-
3years, 3-5years, 5-12years, 12-18years, 18-40years, 40-65years, and above 65years. The
crises are trust-mistrust, autonomy-shame, initiative-guilt, industry-inferiority, identity-role
confusion, intimacy-isolation, generativity-stagnation and ego integrity-despair (Svetina,
2014).
Maria is in the first stage of trust-mistrust, wherein the basic virtue, which can develop in
her, is hope. During this stage as she is uncertain about her environment, she will trust people
when her gratifications are met and will mistrust people when her care is unpredictable,
inconsistent and unreliable. This is characterized by anxiety, insecurity and mistrust if her
care is not taken care of (Lerwick, 2013). As she suffers from unconjugated
hyperbilirubinemia, her senses are more pronounced than other babies are. If she is
hospitalized frequently, it will have an effect in her psychosocial development. If her
condition worsens she might have to get phototherapy which will increase her stay in
hospital. Here, her primary caregivers will be health-care professionals and nurses who will
deftly respond and meet all her physical requirements developing security and trust. Upon
comparison however, prolonged hospitalization may start to make her feel sicker than other
children, which will impact her way of self-visualizing herself (Olusanya, Osibanjo, &
Slusher, 2015).
8. Nursing diagnosis
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
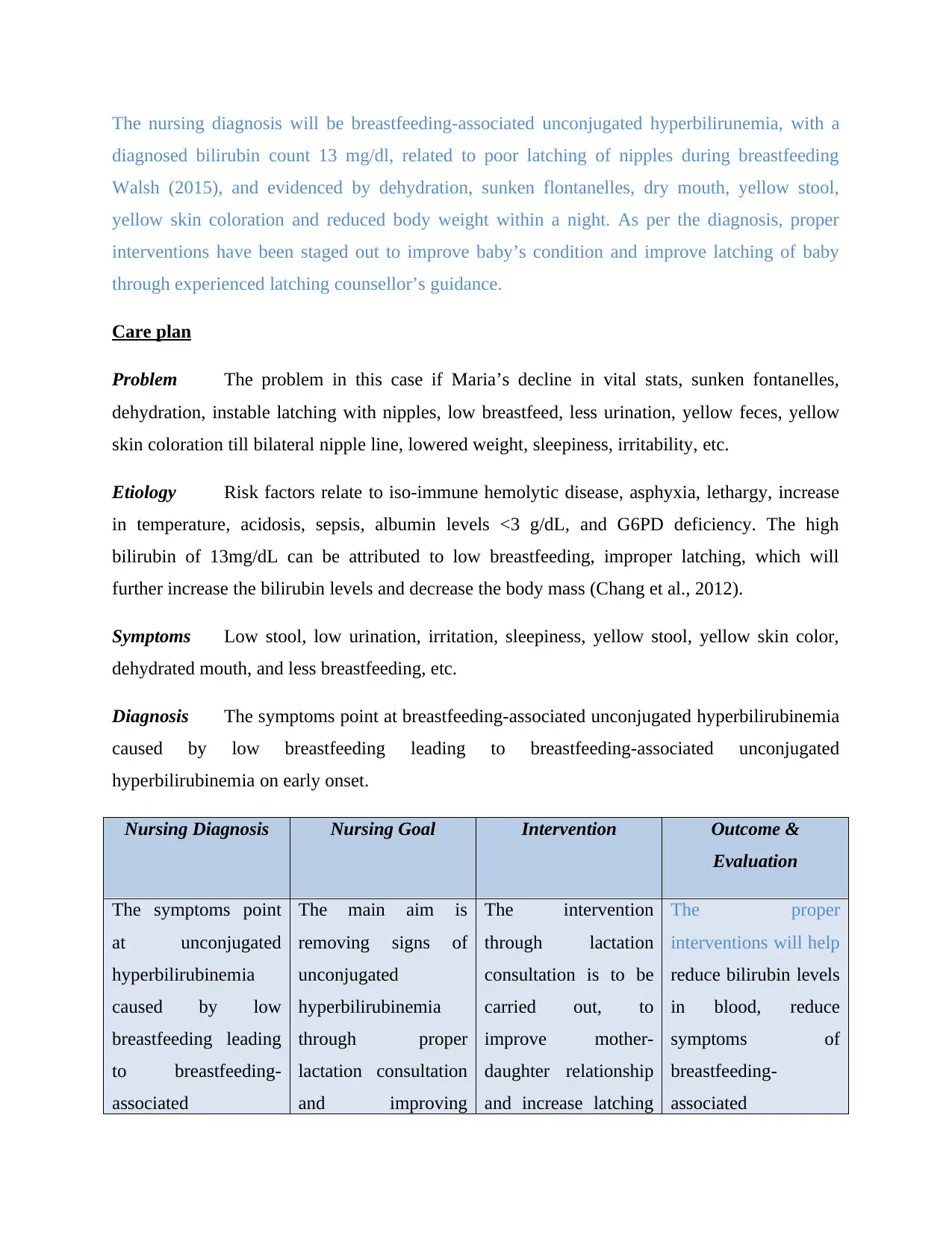
The nursing diagnosis will be breastfeeding-associated unconjugated hyperbilirunemia, with a
diagnosed bilirubin count 13 mg/dl, related to poor latching of nipples during breastfeeding
Walsh (2015), and evidenced by dehydration, sunken flontanelles, dry mouth, yellow stool,
yellow skin coloration and reduced body weight within a night. As per the diagnosis, proper
interventions have been staged out to improve baby’s condition and improve latching of baby
through experienced latching counsellor’s guidance.
Care plan
Problem The problem in this case if Maria’s decline in vital stats, sunken fontanelles,
dehydration, instable latching with nipples, low breastfeed, less urination, yellow feces, yellow
skin coloration till bilateral nipple line, lowered weight, sleepiness, irritability, etc.
Etiology Risk factors relate to iso-immune hemolytic disease, asphyxia, lethargy, increase
in temperature, acidosis, sepsis, albumin levels <3 g/dL, and G6PD deficiency. The high
bilirubin of 13mg/dL can be attributed to low breastfeeding, improper latching, which will
further increase the bilirubin levels and decrease the body mass (Chang et al., 2012).
Symptoms Low stool, low urination, irritation, sleepiness, yellow stool, yellow skin color,
dehydrated mouth, and less breastfeeding, etc.
Diagnosis The symptoms point at breastfeeding-associated unconjugated hyperbilirubinemia
caused by low breastfeeding leading to breastfeeding-associated unconjugated
hyperbilirubinemia on early onset.
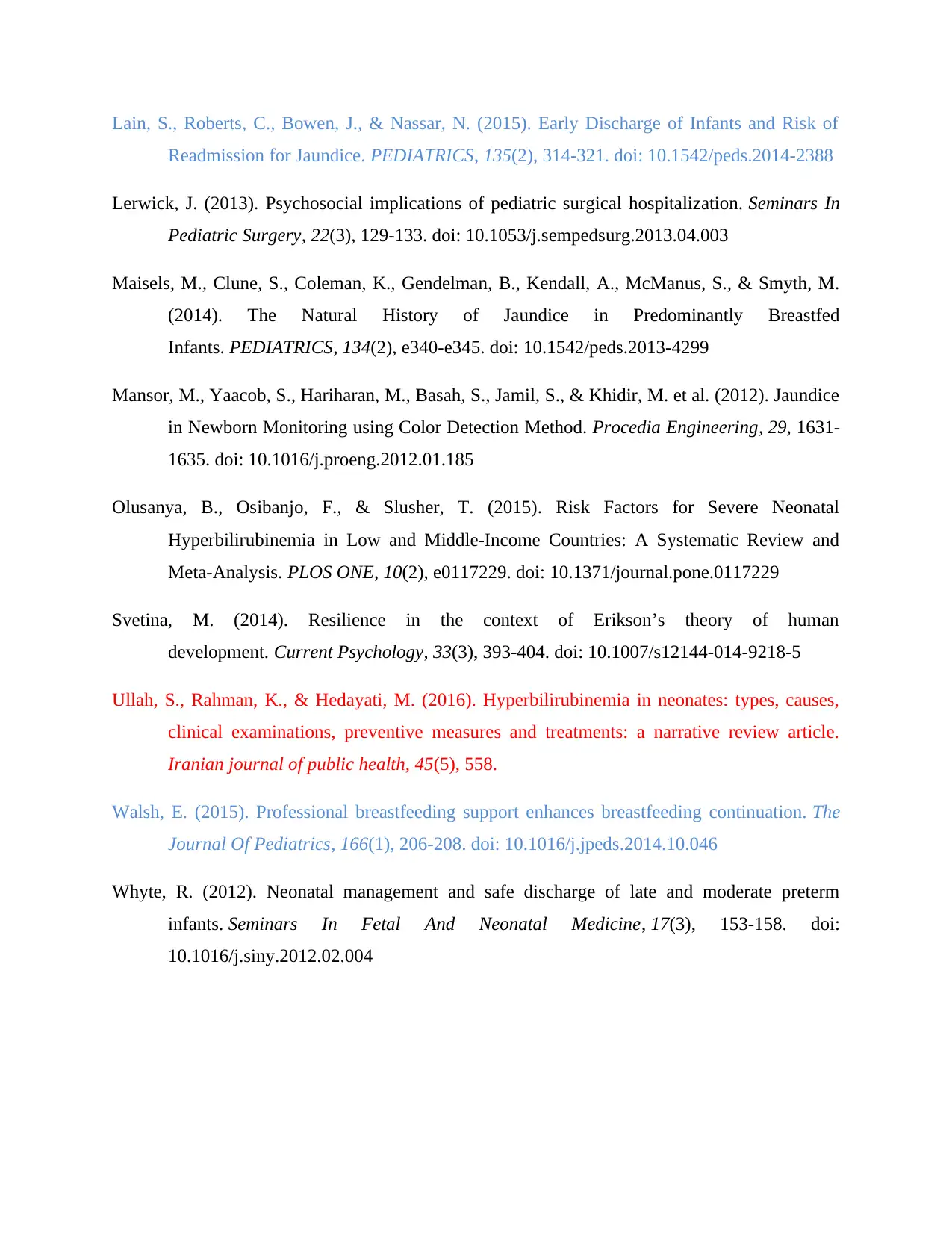
Nursing Diagnosis Nursing Goal Intervention Outcome &
Evaluation
The symptoms point
at unconjugated
hyperbilirubinemia
caused by low
breastfeeding leading
to breastfeeding-
associated
The main aim is
removing signs of
unconjugated
hyperbilirubinemia
through proper
lactation consultation
and improving
The intervention
through lactation
consultation is to be
carried out, to
improve mother-
daughter relationship
and increase latching
The proper
interventions will help
reduce bilirubin levels
in blood, reduce
symptoms of
breastfeeding-
associated
diagnosed bilirubin count 13 mg/dl, related to poor latching of nipples during breastfeeding
Walsh (2015), and evidenced by dehydration, sunken flontanelles, dry mouth, yellow stool,
yellow skin coloration and reduced body weight within a night. As per the diagnosis, proper
interventions have been staged out to improve baby’s condition and improve latching of baby
through experienced latching counsellor’s guidance.
Care plan
Problem The problem in this case if Maria’s decline in vital stats, sunken fontanelles,
dehydration, instable latching with nipples, low breastfeed, less urination, yellow feces, yellow
skin coloration till bilateral nipple line, lowered weight, sleepiness, irritability, etc.
Etiology Risk factors relate to iso-immune hemolytic disease, asphyxia, lethargy, increase
in temperature, acidosis, sepsis, albumin levels <3 g/dL, and G6PD deficiency. The high
bilirubin of 13mg/dL can be attributed to low breastfeeding, improper latching, which will
further increase the bilirubin levels and decrease the body mass (Chang et al., 2012).
Symptoms Low stool, low urination, irritation, sleepiness, yellow stool, yellow skin color,
dehydrated mouth, and less breastfeeding, etc.
Diagnosis The symptoms point at breastfeeding-associated unconjugated hyperbilirubinemia
caused by low breastfeeding leading to breastfeeding-associated unconjugated
hyperbilirubinemia on early onset.
Nursing Diagnosis Nursing Goal Intervention Outcome &
Evaluation
The symptoms point
at unconjugated
hyperbilirubinemia
caused by low
breastfeeding leading
to breastfeeding-
associated
The main aim is
removing signs of
unconjugated
hyperbilirubinemia
through proper
lactation consultation
and improving
The intervention
through lactation
consultation is to be
carried out, to
improve mother-
daughter relationship
and increase latching
The proper
interventions will help
reduce bilirubin levels
in blood, reduce
symptoms of
breastfeeding-
associated
unconjugated
hyperbilirubinemia on
early onset.
breastfeeding for
Maria, to flush out
excess bilirubin
storage in body.
to nipples, and
enhancing
feeding/day count to
10-12 times each day.
The intervention will
be carried through
graded steps by first
educating parents,
creating family-care
plans and involving
both father and
mother (Whyte,
2012). Proper
counseling and
intervention will
increase latching and
improve body weight,
decrease bilirubin in
blood
unconjugated
hyperbilirubinemia,
increase weight in
Maria and improve
breastfeeding to 10-12
times per day.
Evaluation of Maria is
to be done on out-
patient services, 3
times a month after
discharge. The time of
discharge will also be
postponed for a few
days, until
breastfeeding
improves and Weight
is controlled.
hyperbilirubinemia on
early onset.
breastfeeding for
Maria, to flush out
excess bilirubin
storage in body.
to nipples, and
enhancing
feeding/day count to
10-12 times each day.
The intervention will
be carried through
graded steps by first
educating parents,
creating family-care
plans and involving
both father and
mother (Whyte,
2012). Proper
counseling and
intervention will
increase latching and
improve body weight,
decrease bilirubin in
blood
unconjugated
hyperbilirubinemia,
increase weight in
Maria and improve
breastfeeding to 10-12
times per day.
Evaluation of Maria is
to be done on out-
patient services, 3
times a month after
discharge. The time of
discharge will also be
postponed for a few
days, until
breastfeeding
improves and Weight
is controlled.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

References
Amos, R., Jacob, H., & Leith, W. (2017). Jaundice in newborn babies under 28 days: NICE
guideline 2016 (CG98). Archives Of Disease In Childhood - Education & Practice
Edition, 102(4), 207-209. doi: 10.1136/archdischild-2016-311556
Bhutani, V. K., Srinivas, S., Castillo Cuadrado, M. E., Aby, J. L., Wong, R. J., & Stevenson, D.
K. (2016). Identification of neonatal haemolysis: an approach to predischarge
management of neonatal hyperbilirubinemia. Acta Paediatrica, 105(5), e189-e194.
Bhutani, V., Stark, A., Lazzeroni, L., Poland, R., Gourley, G., & Kazmierczak, S. et al. (2013).
Predischarge Screening for Severe Neonatal Hyperbilirubinemia Identifies Infants Who
Need Phototherapy. The Journal Of Pediatrics, 162(3), 477-482.e1. doi:
10.1016/j.jpeds.2012.08.022
Chang, R., Chou, H., Chang, Y., Chen, M., Chen, C., Hsieh, W., & Tsao, P. (2012). Weight Loss
Percentage Prediction of Subsequent Neonatal Hyperbilirubinemia in Exclusively
Breastfed Neonates. Pediatrics & Neonatology, 53(1), 41-44. doi:
10.1016/j.pedneo.2011.11.008
Davanzo, R., Cannioto, Z., Ronfani, L., Monasta, L., & Demarini, S. (2012). Breastfeeding and
Neonatal Weight Loss in Healthy Term Infants. Journal Of Human Lactation, 29(1), 45-
53. doi: 10.1177/0890334412444005
Hockenberry, M. J., & Wilson, D. (2013). Wong's Essentials of Pediatric Nursing9: Wong's
Essentials of Pediatric Nursing. Elsevier Health Sciences.
Hyperbilirubinemia management guidelines. (2019). Retrieved 3 October 2019, from
https://peditools.org/bili/index.php
La Lactancia Materna y la Ictericia - Asociación Americana del Embarazo. (2019). Retrieved 3
October 2019, from https://americanpregnancy.org/breastfeeding/breastfeeding-and-
jaundice/
Amos, R., Jacob, H., & Leith, W. (2017). Jaundice in newborn babies under 28 days: NICE
guideline 2016 (CG98). Archives Of Disease In Childhood - Education & Practice
Edition, 102(4), 207-209. doi: 10.1136/archdischild-2016-311556
Bhutani, V. K., Srinivas, S., Castillo Cuadrado, M. E., Aby, J. L., Wong, R. J., & Stevenson, D.
K. (2016). Identification of neonatal haemolysis: an approach to predischarge
management of neonatal hyperbilirubinemia. Acta Paediatrica, 105(5), e189-e194.
Bhutani, V., Stark, A., Lazzeroni, L., Poland, R., Gourley, G., & Kazmierczak, S. et al. (2013).
Predischarge Screening for Severe Neonatal Hyperbilirubinemia Identifies Infants Who
Need Phototherapy. The Journal Of Pediatrics, 162(3), 477-482.e1. doi:
10.1016/j.jpeds.2012.08.022
Chang, R., Chou, H., Chang, Y., Chen, M., Chen, C., Hsieh, W., & Tsao, P. (2012). Weight Loss
Percentage Prediction of Subsequent Neonatal Hyperbilirubinemia in Exclusively
Breastfed Neonates. Pediatrics & Neonatology, 53(1), 41-44. doi:
10.1016/j.pedneo.2011.11.008
Davanzo, R., Cannioto, Z., Ronfani, L., Monasta, L., & Demarini, S. (2012). Breastfeeding and
Neonatal Weight Loss in Healthy Term Infants. Journal Of Human Lactation, 29(1), 45-
53. doi: 10.1177/0890334412444005
Hockenberry, M. J., & Wilson, D. (2013). Wong's Essentials of Pediatric Nursing9: Wong's
Essentials of Pediatric Nursing. Elsevier Health Sciences.
Hyperbilirubinemia management guidelines. (2019). Retrieved 3 October 2019, from
https://peditools.org/bili/index.php
La Lactancia Materna y la Ictericia - Asociación Americana del Embarazo. (2019). Retrieved 3
October 2019, from https://americanpregnancy.org/breastfeeding/breastfeeding-and-
jaundice/
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Lain, S., Roberts, C., Bowen, J., & Nassar, N. (2015). Early Discharge of Infants and Risk of
Readmission for Jaundice. PEDIATRICS, 135(2), 314-321. doi: 10.1542/peds.2014-2388
Lerwick, J. (2013). Psychosocial implications of pediatric surgical hospitalization. Seminars In
Pediatric Surgery, 22(3), 129-133. doi: 10.1053/j.sempedsurg.2013.04.003
Maisels, M., Clune, S., Coleman, K., Gendelman, B., Kendall, A., McManus, S., & Smyth, M.
(2014). The Natural History of Jaundice in Predominantly Breastfed
Infants. PEDIATRICS, 134(2), e340-e345. doi: 10.1542/peds.2013-4299
Mansor, M., Yaacob, S., Hariharan, M., Basah, S., Jamil, S., & Khidir, M. et al. (2012). Jaundice
in Newborn Monitoring using Color Detection Method. Procedia Engineering, 29, 1631-
1635. doi: 10.1016/j.proeng.2012.01.185
Olusanya, B., Osibanjo, F., & Slusher, T. (2015). Risk Factors for Severe Neonatal
Hyperbilirubinemia in Low and Middle-Income Countries: A Systematic Review and
Meta-Analysis. PLOS ONE, 10(2), e0117229. doi: 10.1371/journal.pone.0117229
Svetina, M. (2014). Resilience in the context of Erikson’s theory of human
development. Current Psychology, 33(3), 393-404. doi: 10.1007/s12144-014-9218-5
Ullah, S., Rahman, K., & Hedayati, M. (2016). Hyperbilirubinemia in neonates: types, causes,
clinical examinations, preventive measures and treatments: a narrative review article.
Iranian journal of public health, 45(5), 558.
Walsh, E. (2015). Professional breastfeeding support enhances breastfeeding continuation. The
Journal Of Pediatrics, 166(1), 206-208. doi: 10.1016/j.jpeds.2014.10.046
Whyte, R. (2012). Neonatal management and safe discharge of late and moderate preterm
infants. Seminars In Fetal And Neonatal Medicine, 17(3), 153-158. doi:
10.1016/j.siny.2012.02.004
Readmission for Jaundice. PEDIATRICS, 135(2), 314-321. doi: 10.1542/peds.2014-2388
Lerwick, J. (2013). Psychosocial implications of pediatric surgical hospitalization. Seminars In
Pediatric Surgery, 22(3), 129-133. doi: 10.1053/j.sempedsurg.2013.04.003
Maisels, M., Clune, S., Coleman, K., Gendelman, B., Kendall, A., McManus, S., & Smyth, M.
(2014). The Natural History of Jaundice in Predominantly Breastfed
Infants. PEDIATRICS, 134(2), e340-e345. doi: 10.1542/peds.2013-4299
Mansor, M., Yaacob, S., Hariharan, M., Basah, S., Jamil, S., & Khidir, M. et al. (2012). Jaundice
in Newborn Monitoring using Color Detection Method. Procedia Engineering, 29, 1631-
1635. doi: 10.1016/j.proeng.2012.01.185
Olusanya, B., Osibanjo, F., & Slusher, T. (2015). Risk Factors for Severe Neonatal
Hyperbilirubinemia in Low and Middle-Income Countries: A Systematic Review and
Meta-Analysis. PLOS ONE, 10(2), e0117229. doi: 10.1371/journal.pone.0117229
Svetina, M. (2014). Resilience in the context of Erikson’s theory of human
development. Current Psychology, 33(3), 393-404. doi: 10.1007/s12144-014-9218-5
Ullah, S., Rahman, K., & Hedayati, M. (2016). Hyperbilirubinemia in neonates: types, causes,
clinical examinations, preventive measures and treatments: a narrative review article.
Iranian journal of public health, 45(5), 558.
Walsh, E. (2015). Professional breastfeeding support enhances breastfeeding continuation. The
Journal Of Pediatrics, 166(1), 206-208. doi: 10.1016/j.jpeds.2014.10.046
Whyte, R. (2012). Neonatal management and safe discharge of late and moderate preterm
infants. Seminars In Fetal And Neonatal Medicine, 17(3), 153-158. doi:
10.1016/j.siny.2012.02.004
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

