MD4: A Case Study of Neurological Disorder Diagnosis & Management
VerifiedAdded on 2023/06/09
|7
|2092
|348
Case Study
AI Summary
This case study presents a 60-year-old Native American female presenting with symptoms indicative of a neurological disorder, including fever, headache, neck stiffness, and confusion. The initial assessment includes a review of systems, vital signs, and patient history, with further investigation involving lab tests such as CBC, CMP, and lumbar puncture. Differential diagnoses considered are tick bite meningitis, encephalitis, and dengue fever. The analysis focuses on tick bite meningitis, detailing its pathophysiology, symptoms, and treatment options, including antibiotics and supportive care. The case study concludes with a follow-up plan to monitor the patient's response to treatment and adjust management accordingly. The study emphasizes the importance of prompt diagnosis and appropriate management in neurological disorders.
MD4 – Neurological Disorders
Use as much room as you need to formulate a complete answer.
General Information:
CONTEXT:
60 yo Native American female who actively participates in crossfit, running and biking. She has no significant
health issues. She presented to the ER with complaints of rapid onset fever, headaches, neck pain and
stiffness, malaise, myalgias, anorexia and confusion.
On assessment:
Section 1: Observations: ROS (Review of systems):
GENERAL: 60 yo Native American, ill appearing female. Unable to answer questions due to confusion, her
husband relays PMH.
SKIN: Pale, diaphoretic.
LUNGS: Clear to ausculatation
CARDIOVASCULAR: Heart rate regular, S1S2 intact w/out murmurs, rubs or gallops. No jugular venous
distention
ABDOMEN: Soft, nontender, nondistended, normal bowel sounds
MUSCULOSKELETAL: Nuchal rigidity, flaccid muscles
NEUROLOGICAL: confused mental status with altered consciousness, Coarse tremor, upper extremity
myoclonus, positive Kernig sign
VS: BP 96/56, pulse98, Temp 38.4C, RR 24
More information from the patient (relayed by husband):
- Have you had any exposures? Anyone else in the family with similar symptoms? Any recent trips?
- No one else in the family has been ill.
- We recently hiked on the Appalachian Trail for 2 weeks, we returned a week ago. Up until now she’s
always been healthy and active.
- How long has she been sick?
- She started feeling achy and ‘like she was coming down with something’ a couple of days ago.
- Then she developed the fever which got worse yesterday. Then she just started getting worse with
confusion and twitching and complaining of severe headaches.
- Any difficulty breathing, chest pain?
- Not that she is complaining of.
- Any nausea/ vomiting?
- She was complaining of feeling nauseous when this first started but no vomiting. Probably because she
doesn’t feel like eating.
- Current Medications
Use as much room as you need to formulate a complete answer.
General Information:
CONTEXT:
60 yo Native American female who actively participates in crossfit, running and biking. She has no significant
health issues. She presented to the ER with complaints of rapid onset fever, headaches, neck pain and
stiffness, malaise, myalgias, anorexia and confusion.
On assessment:
Section 1: Observations: ROS (Review of systems):
GENERAL: 60 yo Native American, ill appearing female. Unable to answer questions due to confusion, her
husband relays PMH.
SKIN: Pale, diaphoretic.
LUNGS: Clear to ausculatation
CARDIOVASCULAR: Heart rate regular, S1S2 intact w/out murmurs, rubs or gallops. No jugular venous
distention
ABDOMEN: Soft, nontender, nondistended, normal bowel sounds
MUSCULOSKELETAL: Nuchal rigidity, flaccid muscles
NEUROLOGICAL: confused mental status with altered consciousness, Coarse tremor, upper extremity
myoclonus, positive Kernig sign
VS: BP 96/56, pulse98, Temp 38.4C, RR 24
More information from the patient (relayed by husband):
- Have you had any exposures? Anyone else in the family with similar symptoms? Any recent trips?
- No one else in the family has been ill.
- We recently hiked on the Appalachian Trail for 2 weeks, we returned a week ago. Up until now she’s
always been healthy and active.
- How long has she been sick?
- She started feeling achy and ‘like she was coming down with something’ a couple of days ago.
- Then she developed the fever which got worse yesterday. Then she just started getting worse with
confusion and twitching and complaining of severe headaches.
- Any difficulty breathing, chest pain?
- Not that she is complaining of.
- Any nausea/ vomiting?
- She was complaining of feeling nauseous when this first started but no vomiting. Probably because she
doesn’t feel like eating.
- Current Medications
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
- Tylenol for fever and aches. She also takes a multivitamin and calcium supplement. But really nothing
else.
- Insect bites, tick bites?
- We pulled off a couple of ticks during the trip, and of course, there were mosquitoes everywhere.
- Did you drink stream water during the hiking trip?
- We’re very careful with that. We did fill our canteens from a stream but used purifying tablets.
Knowing this information, what 5 specific questions would you ask? (5 points)
1. Does she pose allergy to any food or drugs?
2. Does she report about sore throat?
3. Does she face sleepiness or any difficulty in waking?
4. Any past brain or spinal cord injury?
5. Any skin rashes?
Section 2 Labs (2 parts): Part 1 - (10 pts)
How will you continue your work-up? Here explain what each test is and in this case what you are looking for.
More Patient Information:
Labs: CBC w differential, CMP (Comprehensive Metabolic Panel), Sedimentation rate (assesses for
inflammation), stool cultures of OVA and Parasites
Imaging: MRI of head and spine, lumbar puncture
Lab results:
HGB 15.0
WBC 3.2
Normal Neutrophils, lymphocytes
Sodium 146 Normal range 135-145
Potassium 4.2 Normal range 3.5-5.2
Chloride 110 Normal range 98-107
Bicarbonate 22 Normal range 22-28
Creatinine 1.1 Normal range 0.6-1.1
BUN 28 Normal range 8-24
ALT 20Normal range 7-45
AST 40Normal range 8-43
Stool cultures were negative
else.
- Insect bites, tick bites?
- We pulled off a couple of ticks during the trip, and of course, there were mosquitoes everywhere.
- Did you drink stream water during the hiking trip?
- We’re very careful with that. We did fill our canteens from a stream but used purifying tablets.
Knowing this information, what 5 specific questions would you ask? (5 points)
1. Does she pose allergy to any food or drugs?
2. Does she report about sore throat?
3. Does she face sleepiness or any difficulty in waking?
4. Any past brain or spinal cord injury?
5. Any skin rashes?
Section 2 Labs (2 parts): Part 1 - (10 pts)
How will you continue your work-up? Here explain what each test is and in this case what you are looking for.
More Patient Information:
Labs: CBC w differential, CMP (Comprehensive Metabolic Panel), Sedimentation rate (assesses for
inflammation), stool cultures of OVA and Parasites
Imaging: MRI of head and spine, lumbar puncture
Lab results:
HGB 15.0
WBC 3.2
Normal Neutrophils, lymphocytes
Sodium 146 Normal range 135-145
Potassium 4.2 Normal range 3.5-5.2
Chloride 110 Normal range 98-107
Bicarbonate 22 Normal range 22-28
Creatinine 1.1 Normal range 0.6-1.1
BUN 28 Normal range 8-24
ALT 20Normal range 7-45
AST 40Normal range 8-43
Stool cultures were negative
MRI was negative for acute process
Lumbar puncture: Demonstrates elevated protein, moderate pleocytosis with predominance of neutrophils.
Cytologic exam shows plasmacytoid lymphocytes
In order to continue the work-up several important tests are required. As I am looking for imbalance in the
platelets, RBC and WBC counts a blood test is required. In this case Complete Blood Count would be helpful as
it provides the potential number of white blood cells, red blood cells and platelets with differential count and
measures the amount of hemoglobin. Further I am looking for disorder elated to metabolism, thus
comprehensive metabolic panel test is required as it provides current status of metabolism and informs about
the level of blood glucose and proteins. I also want to know if the patient is facing any inflammation. In this
regards Erythrocyte sedimentation rate or ESR test is required. As the patient’s husband has mentioned that
they were exposed to couple of ticks during their trip I am looking for any parasite infection and stool of OVA
and parasite examination would help me in this case, because the test helps to determine whether any
parasite infection has occurred in the digestive tract or not. As the patient is suffering from headache and
confused mental status it is required to identify any past injury, thus MRI of brain and spinal cord is required.
As the symptoms of the patient are indicating the consequence of meningitis or encephalitis, I would like to
conduct lumbar puncture to confirm the presence of such disease.
Part 2 - List your findings so far (10 points):
It has been found in the assessment that the patient is suffering from fever, nausea, headache, stiffness, neck pain,
malaise, myalgias, anorexia and confusion. Pale and diaphoretic skin has been found. Musculoskeletal
assessment has indicated nuchal rigidity and flaccid muscle. Confused mental status, positive Kernig sign,
coarse tremor and upper extremity myoclonus has been found in the neurological assessment. The blood
pressure of the patient is 96/56 which is low. Pulse rate is 98. Body temperature 38.4C and respiratory rate is
24. The lab report has indicated that the metabolism is normal, WBC count is 3 and hemoglobin count is 15.
The MRI and stool report is negative. However, the lumbar puncture has demonstrated elevated protein,
moderate pleocytosis with predominance of neutrophils. The cytologic exam has shown plasmacytoid
lymphocytes.
Section 3 Diagnoses: Short list of possible ailments. 15 points.
What is your short list of 3 diagnoses with a rationale why you chose those. The rationale should show a direct
relationship to the findings and ROS:
With the symptoms of nausea, headache, stiffness, neck pain, Kernig sign and confused mind the possible
three diagnoses are listed below.
1. Tick bite Meningitis: Excessive headache with nausea and high fever, stiffness, confusion and positive kernig
and lumber puncture test has lead to diagnose of meningitis. The information provided by the patient’s
husband regarding their exposure to ticks during the trip has indicated that the patient may be suffering from
tick bite meningitis.
Lumbar puncture: Demonstrates elevated protein, moderate pleocytosis with predominance of neutrophils.
Cytologic exam shows plasmacytoid lymphocytes
In order to continue the work-up several important tests are required. As I am looking for imbalance in the
platelets, RBC and WBC counts a blood test is required. In this case Complete Blood Count would be helpful as
it provides the potential number of white blood cells, red blood cells and platelets with differential count and
measures the amount of hemoglobin. Further I am looking for disorder elated to metabolism, thus
comprehensive metabolic panel test is required as it provides current status of metabolism and informs about
the level of blood glucose and proteins. I also want to know if the patient is facing any inflammation. In this
regards Erythrocyte sedimentation rate or ESR test is required. As the patient’s husband has mentioned that
they were exposed to couple of ticks during their trip I am looking for any parasite infection and stool of OVA
and parasite examination would help me in this case, because the test helps to determine whether any
parasite infection has occurred in the digestive tract or not. As the patient is suffering from headache and
confused mental status it is required to identify any past injury, thus MRI of brain and spinal cord is required.
As the symptoms of the patient are indicating the consequence of meningitis or encephalitis, I would like to
conduct lumbar puncture to confirm the presence of such disease.
Part 2 - List your findings so far (10 points):
It has been found in the assessment that the patient is suffering from fever, nausea, headache, stiffness, neck pain,
malaise, myalgias, anorexia and confusion. Pale and diaphoretic skin has been found. Musculoskeletal
assessment has indicated nuchal rigidity and flaccid muscle. Confused mental status, positive Kernig sign,
coarse tremor and upper extremity myoclonus has been found in the neurological assessment. The blood
pressure of the patient is 96/56 which is low. Pulse rate is 98. Body temperature 38.4C and respiratory rate is
24. The lab report has indicated that the metabolism is normal, WBC count is 3 and hemoglobin count is 15.
The MRI and stool report is negative. However, the lumbar puncture has demonstrated elevated protein,
moderate pleocytosis with predominance of neutrophils. The cytologic exam has shown plasmacytoid
lymphocytes.
Section 3 Diagnoses: Short list of possible ailments. 15 points.
What is your short list of 3 diagnoses with a rationale why you chose those. The rationale should show a direct
relationship to the findings and ROS:
With the symptoms of nausea, headache, stiffness, neck pain, Kernig sign and confused mind the possible
three diagnoses are listed below.
1. Tick bite Meningitis: Excessive headache with nausea and high fever, stiffness, confusion and positive kernig
and lumber puncture test has lead to diagnose of meningitis. The information provided by the patient’s
husband regarding their exposure to ticks during the trip has indicated that the patient may be suffering from
tick bite meningitis.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2. Encephalitis: Nausea, headache, fever, poor feeding or problem with eating, confusion, unconsciousness
and positive lumbar puncture report has lead to the diagnose of encephalitis (Venkatesan et al. 2013).
3. Dengue: Sudden fever, headache, nausea and most importantly the presence of plasmocytoid lymphocytes
has lead to diagnose of dengue (Borges, Castro and Fonseca 2013).
Section 4 Plan: Follow up tests/studies – 15 points
This section is important because you will chose THE MOST LIKELY DIAGNOSIS IN YOUR OPINION and follow up
with that one diagnosis only. These tests should be specific in nature and allow you to determine whether or
not the patient has that particular problem/disease.
In this particular case I would like to following up with tick bite meningitis. As I am dealing with nausea,
headache, confusion, stiffness, high fever, neck pain, coarse tremor, upper extremity myoclonus and positive
Kernig sign and as the patient’s husband has mentioned that they were exposed to couple of ticks during their
trip I would like to follow up with Complete blood count test which provides potential WBC, RBC and platelets
count. Furthermore, I would like to follow up Lumbar puncture test to confirm tick bite meningitis.
Section 5 Pathophysiology: 25 points.Most important section - Even if your diagnosis is not the actual one,
as long as you have a good explanation for the ONE you chose, you WILL GET FULL CREDIT. You need to
describe how the disorder/disease you chose going forward MAKE the person feel sick, what the treatment
is, how the treatment will counteract the disorder and how it will affect the symptoms the patient
manifests. See example for understanding the depth of detail with respect to this question.
Meningitis is defined as the inflammation of the meninges, the membrane surrounding brain. The disease is
mainly caused by the bacterial or viral infection. The bacterial meningitis may be caused by Pneumococcal or
Meningococcal bacteria and viruses responsible for meningitis include Enterovirus. In some cases it may be
caused by environmental exposure to parasites and immunocompromised state. The consequence of
meningitis may lead to leads to life threatening issue thus it is important to provide immediate medical care in
order to prevent serious complications (Pyrgos et al. 2013).
and positive lumbar puncture report has lead to the diagnose of encephalitis (Venkatesan et al. 2013).
3. Dengue: Sudden fever, headache, nausea and most importantly the presence of plasmocytoid lymphocytes
has lead to diagnose of dengue (Borges, Castro and Fonseca 2013).
Section 4 Plan: Follow up tests/studies – 15 points
This section is important because you will chose THE MOST LIKELY DIAGNOSIS IN YOUR OPINION and follow up
with that one diagnosis only. These tests should be specific in nature and allow you to determine whether or
not the patient has that particular problem/disease.
In this particular case I would like to following up with tick bite meningitis. As I am dealing with nausea,
headache, confusion, stiffness, high fever, neck pain, coarse tremor, upper extremity myoclonus and positive
Kernig sign and as the patient’s husband has mentioned that they were exposed to couple of ticks during their
trip I would like to follow up with Complete blood count test which provides potential WBC, RBC and platelets
count. Furthermore, I would like to follow up Lumbar puncture test to confirm tick bite meningitis.
Section 5 Pathophysiology: 25 points.Most important section - Even if your diagnosis is not the actual one,
as long as you have a good explanation for the ONE you chose, you WILL GET FULL CREDIT. You need to
describe how the disorder/disease you chose going forward MAKE the person feel sick, what the treatment
is, how the treatment will counteract the disorder and how it will affect the symptoms the patient
manifests. See example for understanding the depth of detail with respect to this question.
Meningitis is defined as the inflammation of the meninges, the membrane surrounding brain. The disease is
mainly caused by the bacterial or viral infection. The bacterial meningitis may be caused by Pneumococcal or
Meningococcal bacteria and viruses responsible for meningitis include Enterovirus. In some cases it may be
caused by environmental exposure to parasites and immunocompromised state. The consequence of
meningitis may lead to leads to life threatening issue thus it is important to provide immediate medical care in
order to prevent serious complications (Pyrgos et al. 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
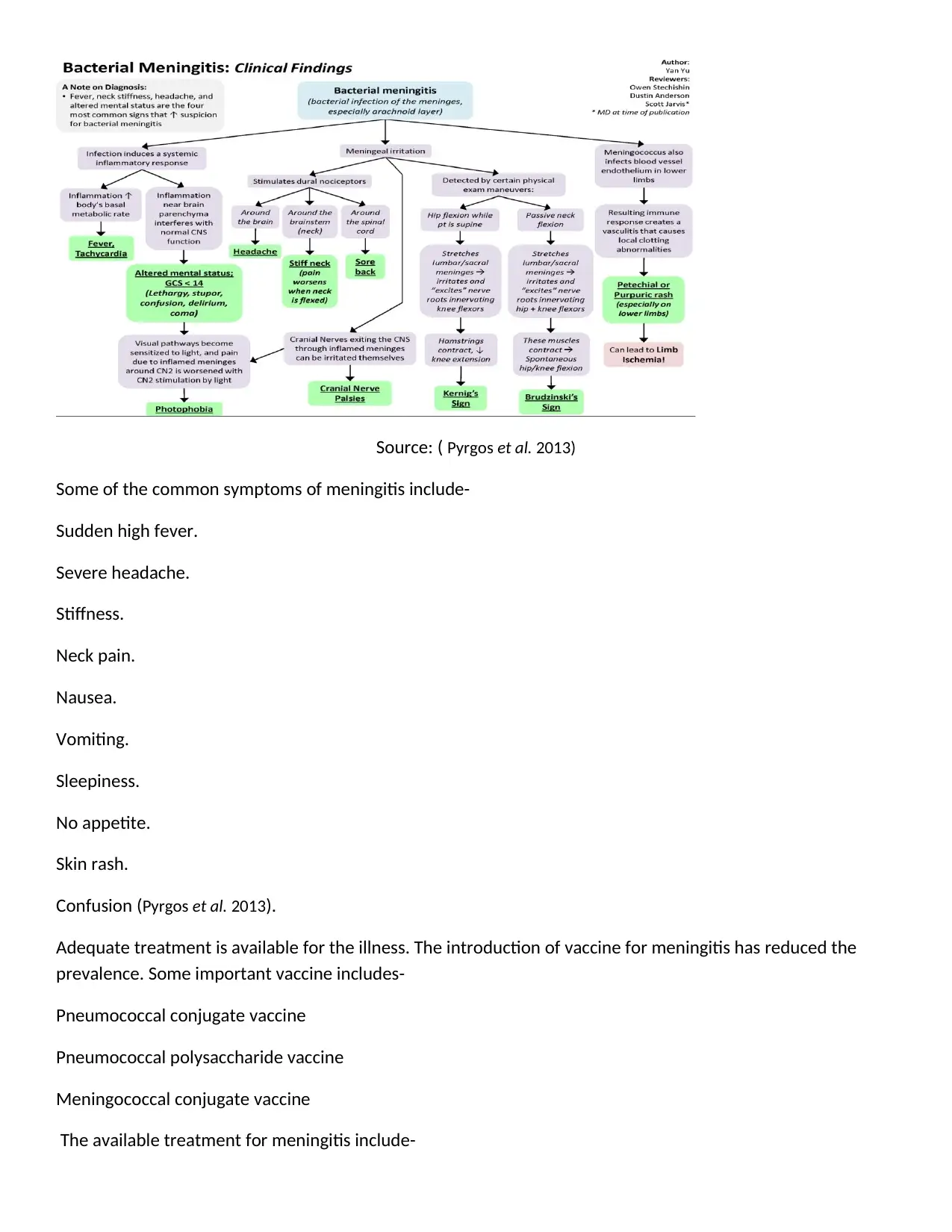
Source: ( Pyrgos et al. 2013)
Some of the common symptoms of meningitis include-
Sudden high fever.
Severe headache.
Stiffness.
Neck pain.
Nausea.
Vomiting.
Sleepiness.
No appetite.
Skin rash.
Confusion (Pyrgos et al. 2013).
Adequate treatment is available for the illness. The introduction of vaccine for meningitis has reduced the
prevalence. Some important vaccine includes-
Pneumococcal conjugate vaccine
Pneumococcal polysaccharide vaccine
Meningococcal conjugate vaccine
The available treatment for meningitis include-
Some of the common symptoms of meningitis include-
Sudden high fever.
Severe headache.
Stiffness.
Neck pain.
Nausea.
Vomiting.
Sleepiness.
No appetite.
Skin rash.
Confusion (Pyrgos et al. 2013).
Adequate treatment is available for the illness. The introduction of vaccine for meningitis has reduced the
prevalence. Some important vaccine includes-
Pneumococcal conjugate vaccine
Pneumococcal polysaccharide vaccine
Meningococcal conjugate vaccine
The available treatment for meningitis include-
Intravenous antibiotics.
Intake plenty of fluids.
Proper medication for fever and pain.
Bed rest.
Cefotaxime is used to treat documented or suspected bacterial meningitis (Musa et al. 2013).
With the immunization and proper treatment meningitis could be cured and the patient could live healthy life
and maintain well-being in an effective manner.
Section 6 – Follow-up – 5 points
In this section, you describe different things you would look for and ask about in a follow up appointment with
the patient. You will be responsible for determining how the patient is responding.
The further follow up appointment are as follows-
Fixed appointment after 1 week in order to understand the health condition of the patient after providing treatment and
adequate medication and identify whether the treatment is appropriate for the patient or not. Follow up appointment
after 2 weeks for another complete blood count and lumber puncture test to monitor the health condition. Further
treatment would be determined based o the result of the tests.
Intake plenty of fluids.
Proper medication for fever and pain.
Bed rest.
Cefotaxime is used to treat documented or suspected bacterial meningitis (Musa et al. 2013).
With the immunization and proper treatment meningitis could be cured and the patient could live healthy life
and maintain well-being in an effective manner.
Section 6 – Follow-up – 5 points
In this section, you describe different things you would look for and ask about in a follow up appointment with
the patient. You will be responsible for determining how the patient is responding.
The further follow up appointment are as follows-
Fixed appointment after 1 week in order to understand the health condition of the patient after providing treatment and
adequate medication and identify whether the treatment is appropriate for the patient or not. Follow up appointment
after 2 weeks for another complete blood count and lumber puncture test to monitor the health condition. Further
treatment would be determined based o the result of the tests.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References:
Borges, M.C., Castro, L.A. and Fonseca, B.A.L.D., 2013. Chloroquine use improves dengue-related symptoms. Memórias
do Instituto Oswaldo Cruz, 108(5), pp.596-599.
Musa, S.H., Basri, M., Masoumi, H.R.F., Karjiban, R.A., Malek, E.A., Basri, H. and Shamsuddin, A.F., 2013. Formulation
optimization of palm kernel oil esters nanoemulsion-loaded with chloramphenicol suitable for meningitis
treatment. Colloids and Surfaces B: Biointerfaces, 112, pp.113-119.
Pyrgos, V., Seitz, A.E., Steiner, C.A., Prevots, D.R. and Williamson, P.R., 2013. Epidemiology of cryptococcal meningitis in
the US: 1997–2009. PloS one, 8(2), p.e56269.
Venkatesan, A., Tunkel, A.R., Bloch, K.C., Lauring, A.S., Sejvar, J., Bitnun, A., Stahl, J.P., Mailles, A., Drebot, M., Rupprecht,
C.E. and Yoder, J., 2013. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of
the international encephalitis consortium. Clinical Infectious Diseases, 57(8), pp.1114-1128.
Borges, M.C., Castro, L.A. and Fonseca, B.A.L.D., 2013. Chloroquine use improves dengue-related symptoms. Memórias
do Instituto Oswaldo Cruz, 108(5), pp.596-599.
Musa, S.H., Basri, M., Masoumi, H.R.F., Karjiban, R.A., Malek, E.A., Basri, H. and Shamsuddin, A.F., 2013. Formulation
optimization of palm kernel oil esters nanoemulsion-loaded with chloramphenicol suitable for meningitis
treatment. Colloids and Surfaces B: Biointerfaces, 112, pp.113-119.
Pyrgos, V., Seitz, A.E., Steiner, C.A., Prevots, D.R. and Williamson, P.R., 2013. Epidemiology of cryptococcal meningitis in
the US: 1997–2009. PloS one, 8(2), p.e56269.
Venkatesan, A., Tunkel, A.R., Bloch, K.C., Lauring, A.S., Sejvar, J., Bitnun, A., Stahl, J.P., Mailles, A., Drebot, M., Rupprecht,
C.E. and Yoder, J., 2013. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of
the international encephalitis consortium. Clinical Infectious Diseases, 57(8), pp.1114-1128.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.