Measles Epidemiology: Incidence, Vaccination and Prevention Study
VerifiedAdded on 2022/11/19
|18
|4166
|219
Homework Assignment
AI Summary
This assignment provides a comprehensive analysis of measles, focusing on its epidemiology, pathogenesis, prevention, and vaccination strategies. The study begins by examining the incidence of measles in Australia over a 10-year period, including data on monthly cases, state-wise distribution, age demographics, and vaccination status. The assignment then compares these statistics with those of several countries in the Western Pacific region. The pathogenesis of measles is explored, detailing the virus's entry points, replication process, and potential complications, including neurological effects. The assignment also addresses prevention strategies, with an emphasis on herd immunity and the significance of rubella vaccination. The study concludes with a discussion on vaccination, examining the MMR vaccine's side effects, and the importance of individual choices within the context of public health and safety. The assignment is a detailed analysis of measles, incorporating statistical data, scientific understanding, and ethical considerations.

Running Head: A DETAILED STUDY ON DISEASES AND THE POPULATION IT
AFFECTS
A detailed study on diseases and the population it affects
Name of the Student:
Name of the University:
Author Note:
AFFECTS
A detailed study on diseases and the population it affects
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
Answer 1:
No. of cases by month in Australia:
(Australian Government Department of Health 2019)
Jan Feb Ma
r
Ap
r
Ma
y
Jun
e
Jul
y
Au
g
Se
p
Oct No
v
De
c
Annua
l total
201
0
1 11 2 4 5 7 4 17 9 3 2 5 70
201
1
21 29 29 16 9 6 12 16 6 5 31 14 194
201
2
3 2 4 10 9 12 26 42 61 21 6 3 199
201
3
3 5 2 3 7 7 4 21 19 44 26 17 158
201
4
78 61 36 14 23 34 32 22 3 17 5 14 339
201
5
10 6 11 9 5 5 3 7 9 0 4 5 74
201
6
6 15 16 10 5 4 6 1 7 7 6 16 99
201
7
9 7 25 7 4 0 2 4 14 7 0 2 81
201
8
3 2 30 10 4 2 6 20 4 3 7 12 103
201
9
25 20 45 23 15 3 15 1 0 0 0 0 14
Answer 1:
No. of cases by month in Australia:
(Australian Government Department of Health 2019)
Jan Feb Ma
r
Ap
r
Ma
y
Jun
e
Jul
y
Au
g
Se
p
Oct No
v
De
c
Annua
l total
201
0
1 11 2 4 5 7 4 17 9 3 2 5 70
201
1
21 29 29 16 9 6 12 16 6 5 31 14 194
201
2
3 2 4 10 9 12 26 42 61 21 6 3 199
201
3
3 5 2 3 7 7 4 21 19 44 26 17 158
201
4
78 61 36 14 23 34 32 22 3 17 5 14 339
201
5
10 6 11 9 5 5 3 7 9 0 4 5 74
201
6
6 15 16 10 5 4 6 1 7 7 6 16 99
201
7
9 7 25 7 4 0 2 4 14 7 0 2 81
201
8
3 2 30 10 4 2 6 20 4 3 7 12 103
201
9
25 20 45 23 15 3 15 1 0 0 0 0 14
2A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
0
10
20
30
40
50
60
70
80
90
Graphical repr esentati on of the
prevalence of m easles in Australia
Jan Feb Mar Apr May June July Aug Sep Oct Nov Dec
years
Incidence of the disease
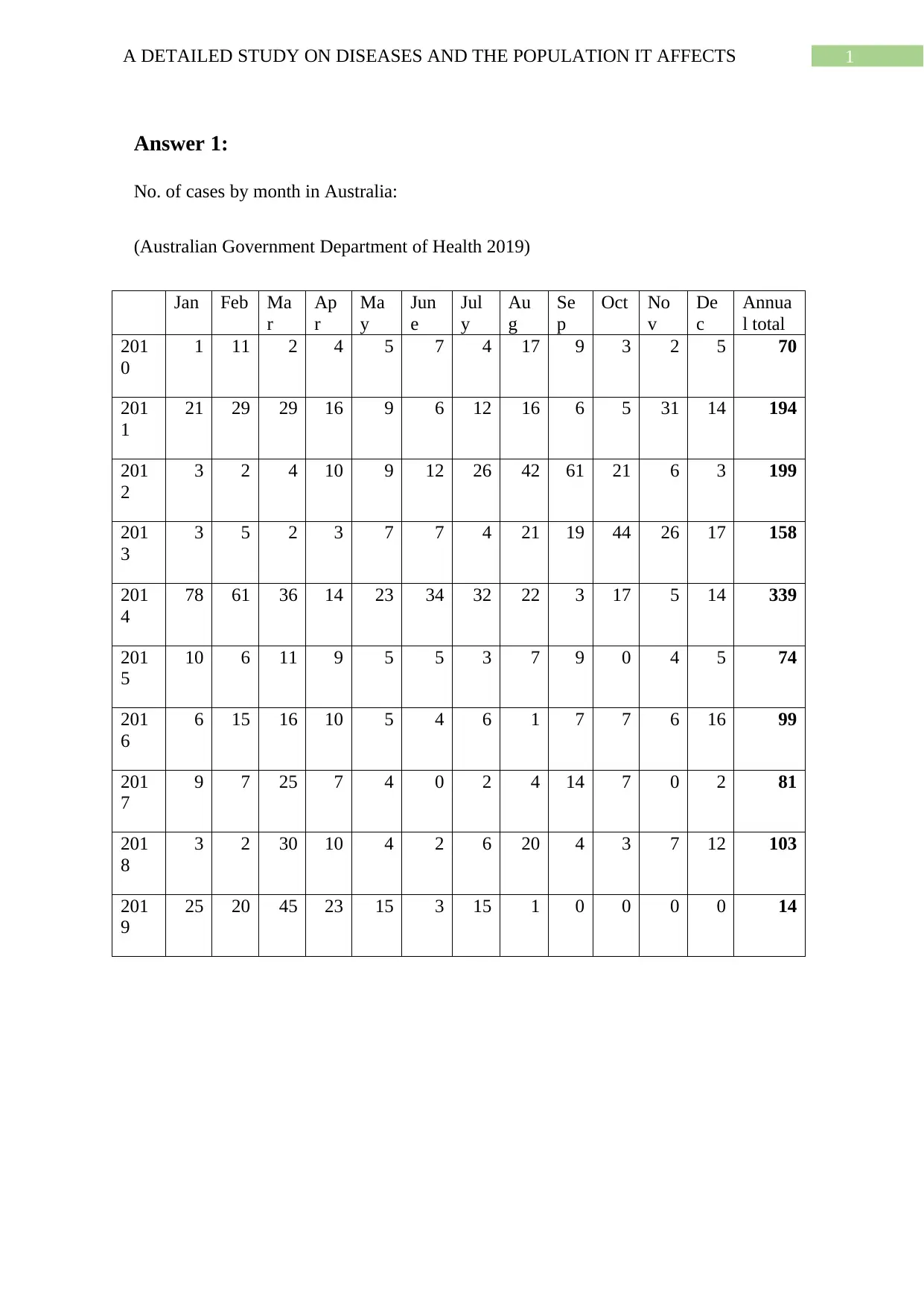
Based on the statistical data provided it shows that the incidence of the disease increased
since 2011 to 2014 but it dropped post that exception being 2018 and 2019 also seems
comparatively higher.
No. of cases by state in Australia:
(Australian Government Department of Health 2019)
Year ACT NSW NT QLD SA TAS VIC WA Aust
2010 1 25 2 14 2 0 15 11 70
2011 21 90 5 18 4 0 39 17 194
2012 0 170 2 4 6 0 11 6 199
2013 1 34 0 52 16 0 41 14 158
2014 7 67 52 72 16 5 77 43 339
2015 2 9 0 21 4 0 30 8 74
2016 2 18 0 15 11 3 39 11 99
2017 2 30 2 8 1 0 21 17 81
2018 3 19 0 14 2 1 26 38 103
2019 2 37 29 22 4 1 29 23 147
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
0
10
20
30
40
50
60
70
80
90
Graphical repr esentati on of the
prevalence of m easles in Australia
Jan Feb Mar Apr May June July Aug Sep Oct Nov Dec
years
Incidence of the disease
Based on the statistical data provided it shows that the incidence of the disease increased
since 2011 to 2014 but it dropped post that exception being 2018 and 2019 also seems
comparatively higher.
No. of cases by state in Australia:
(Australian Government Department of Health 2019)
Year ACT NSW NT QLD SA TAS VIC WA Aust
2010 1 25 2 14 2 0 15 11 70
2011 21 90 5 18 4 0 39 17 194
2012 0 170 2 4 6 0 11 6 199
2013 1 34 0 52 16 0 41 14 158
2014 7 67 52 72 16 5 77 43 339
2015 2 9 0 21 4 0 30 8 74
2016 2 18 0 15 11 3 39 11 99
2017 2 30 2 8 1 0 21 17 81
2018 3 19 0 14 2 1 26 38 103
2019 2 37 29 22 4 1 29 23 147
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
0
50
100
150
200
250
300
350
400
Prevalence of Measles in different states of Australia every
year
ACT NSW NT QLD SA TAS VIC WA Aust
Year
Incidence of the disease
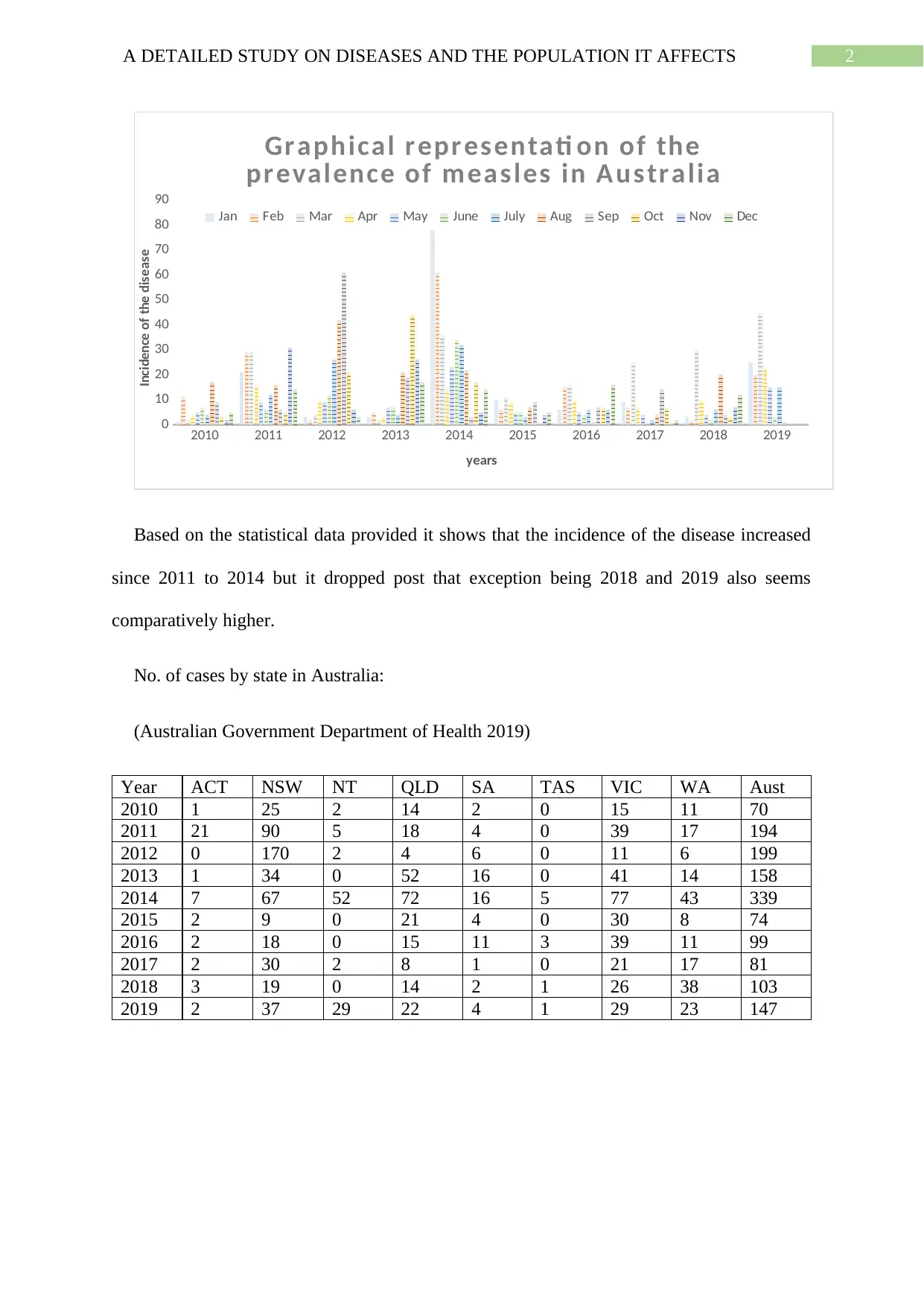
The Australian Capital Territory and Tasmania is least affected with the disease based on
the provided data and the Aust state has the highest prevalence of the disease. New South
Wales, Western Australia and Victoria are moderately affected by the disease.
No. cases by age distribution in Australia:
(Australian Government Department of Health 2019)
Age (in years) Males Females Total cases
00-04 12 6 18
05-09 2 0 2
10-14 5 3 8
15-19 8 8 16
20-24 16 9 25
25-29 15 7 22
30-34 10 3 13
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
0
50
100
150
200
250
300
350
400
Prevalence of Measles in different states of Australia every
year
ACT NSW NT QLD SA TAS VIC WA Aust
Year
Incidence of the disease
The Australian Capital Territory and Tasmania is least affected with the disease based on
the provided data and the Aust state has the highest prevalence of the disease. New South
Wales, Western Australia and Victoria are moderately affected by the disease.
No. cases by age distribution in Australia:
(Australian Government Department of Health 2019)
Age (in years) Males Females Total cases
00-04 12 6 18
05-09 2 0 2
10-14 5 3 8
15-19 8 8 16
20-24 16 9 25
25-29 15 7 22
30-34 10 3 13
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
35-39 11 2 13
40-44 10 5 15
45-49 7 4 11
50-54 2 1 3
55-59 0 1 1
60-64 0 0 0
65-69 0 0 0
70-74 0 0 0
75-79 0 0 0
80-84 0 0 0
85+ 0 0 0
Unknown 0 0 0
Total 98 49 147
00-04
05 to 09
10 to 14
15-19
20-24
25-29
30-34
35-39
40-44
45-49
50-54
55-59
60-64
65-69
70-74
75-79
80-84
85+
Unknown
0
2
4
6
8
10
12
14
16
18
Age Distribution of the Disease
Prevalence
Prevalence of disease
35-39 11 2 13
40-44 10 5 15
45-49 7 4 11
50-54 2 1 3
55-59 0 1 1
60-64 0 0 0
65-69 0 0 0
70-74 0 0 0
75-79 0 0 0
80-84 0 0 0
85+ 0 0 0
Unknown 0 0 0
Total 98 49 147
00-04
05 to 09
10 to 14
15-19
20-24
25-29
30-34
35-39
40-44
45-49
50-54
55-59
60-64
65-69
70-74
75-79
80-84
85+
Unknown
0
2
4
6
8
10
12
14
16
18
Age Distribution of the Disease
Prevalence
Prevalence of disease
5A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
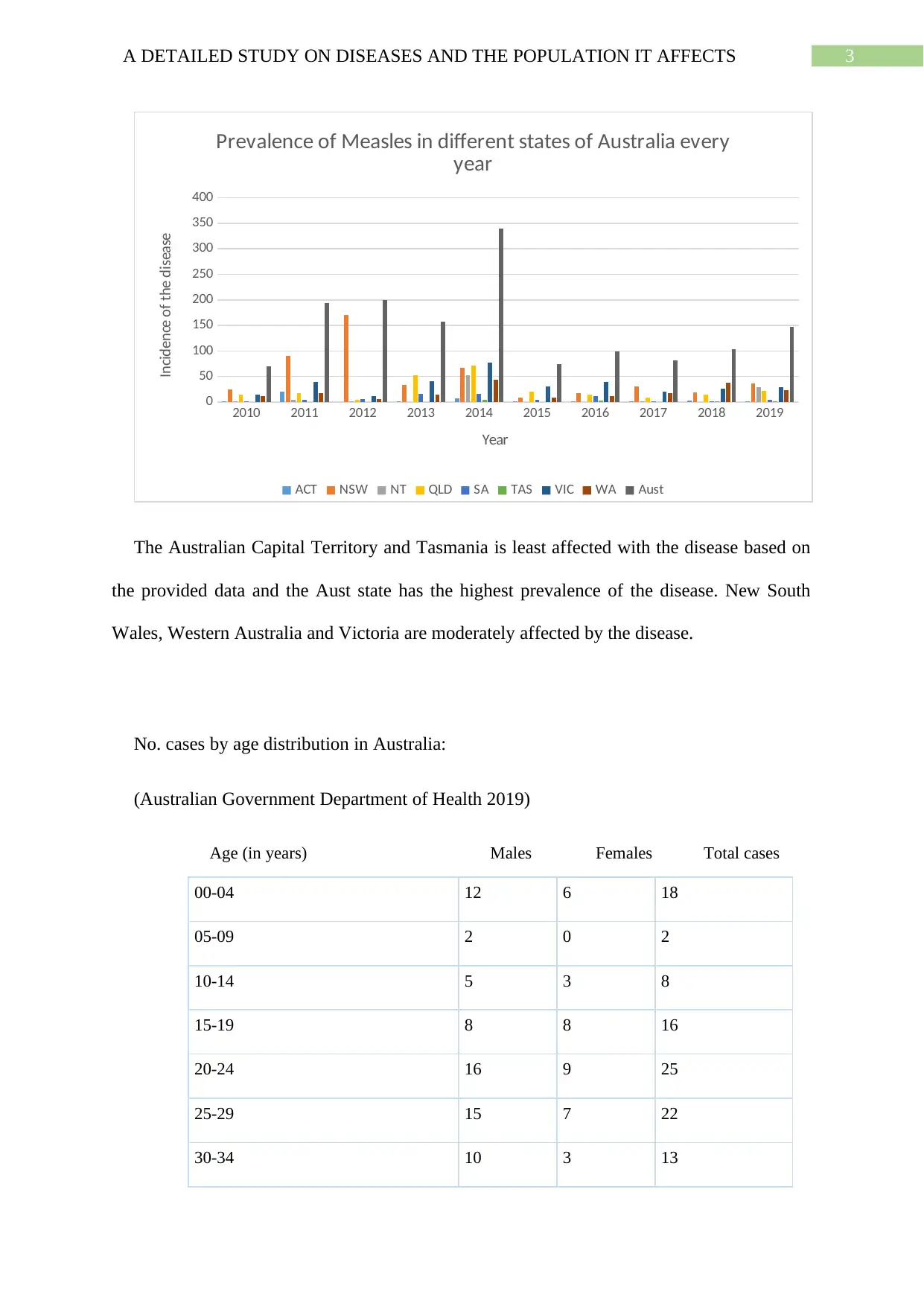
From the graph it is evident that the males are more affected by measles than females and
majorly affects the middle aged group of the age 24 to 45. Incidence of the disease is not
observed among the elders.
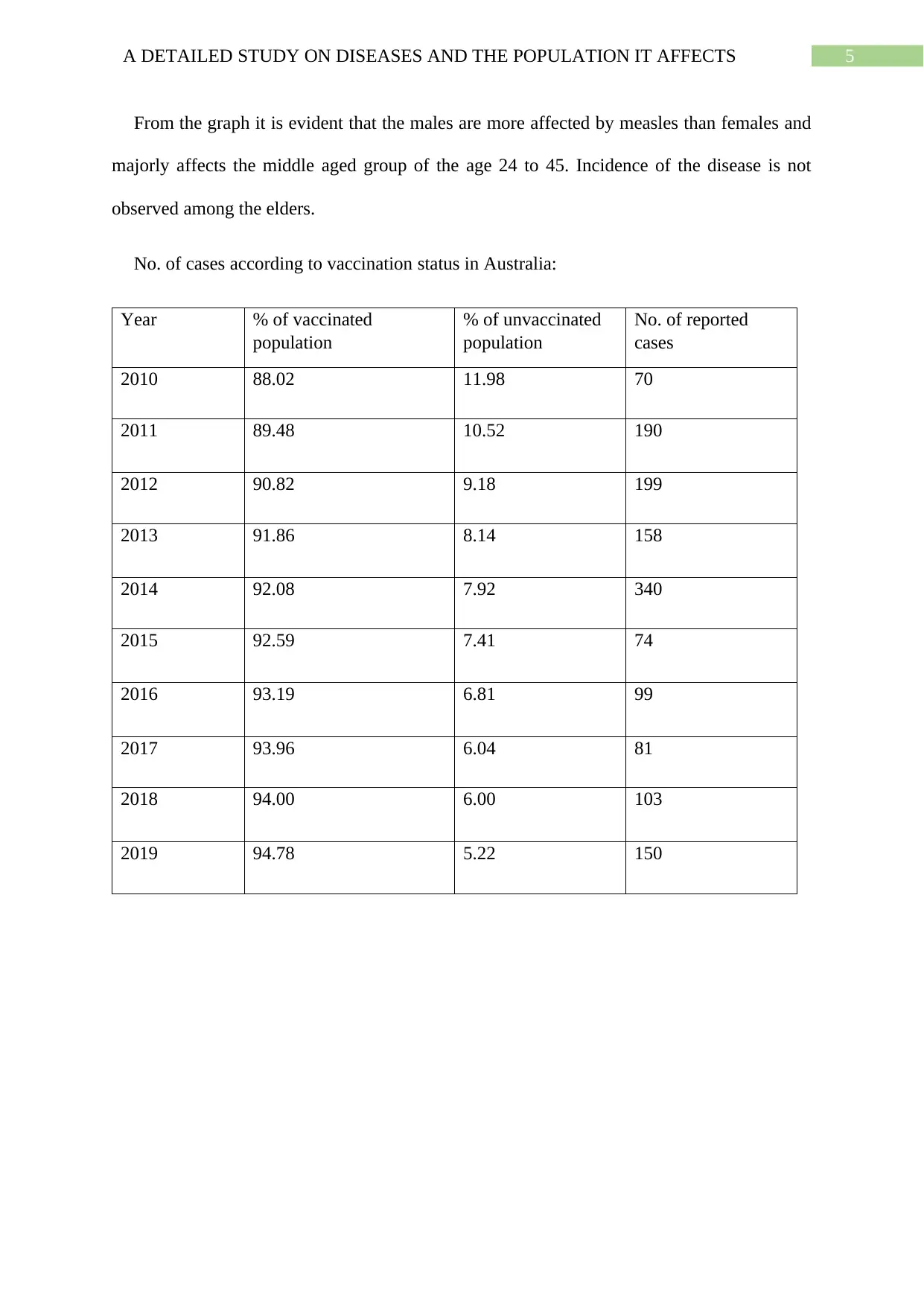
No. of cases according to vaccination status in Australia:
Year % of vaccinated
population
% of unvaccinated
population
No. of reported
cases
2010 88.02 11.98 70
2011 89.48 10.52 190
2012 90.82 9.18 199
2013 91.86 8.14 158
2014 92.08 7.92 340
2015 92.59 7.41 74
2016 93.19 6.81 99
2017 93.96 6.04 81
2018 94.00 6.00 103
2019 94.78 5.22 150
From the graph it is evident that the males are more affected by measles than females and
majorly affects the middle aged group of the age 24 to 45. Incidence of the disease is not
observed among the elders.
No. of cases according to vaccination status in Australia:
Year % of vaccinated
population
% of unvaccinated
population
No. of reported
cases
2010 88.02 11.98 70
2011 89.48 10.52 190
2012 90.82 9.18 199
2013 91.86 8.14 158
2014 92.08 7.92 340
2015 92.59 7.41 74
2016 93.19 6.81 99
2017 93.96 6.04 81
2018 94.00 6.00 103
2019 94.78 5.22 150
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
0
50
100
150
200
250
300
350
400
Graphical representati on of the disease post
vaccinati on
Incidence of the disease
The data proves that the measles virus is resistant to the measles vaccine that is being
administered. This is because even after the majority of the population are getting immunized
the prevalence of the disease is not decreasing and thus even the vaccinated individuals are
susceptible to the disease.
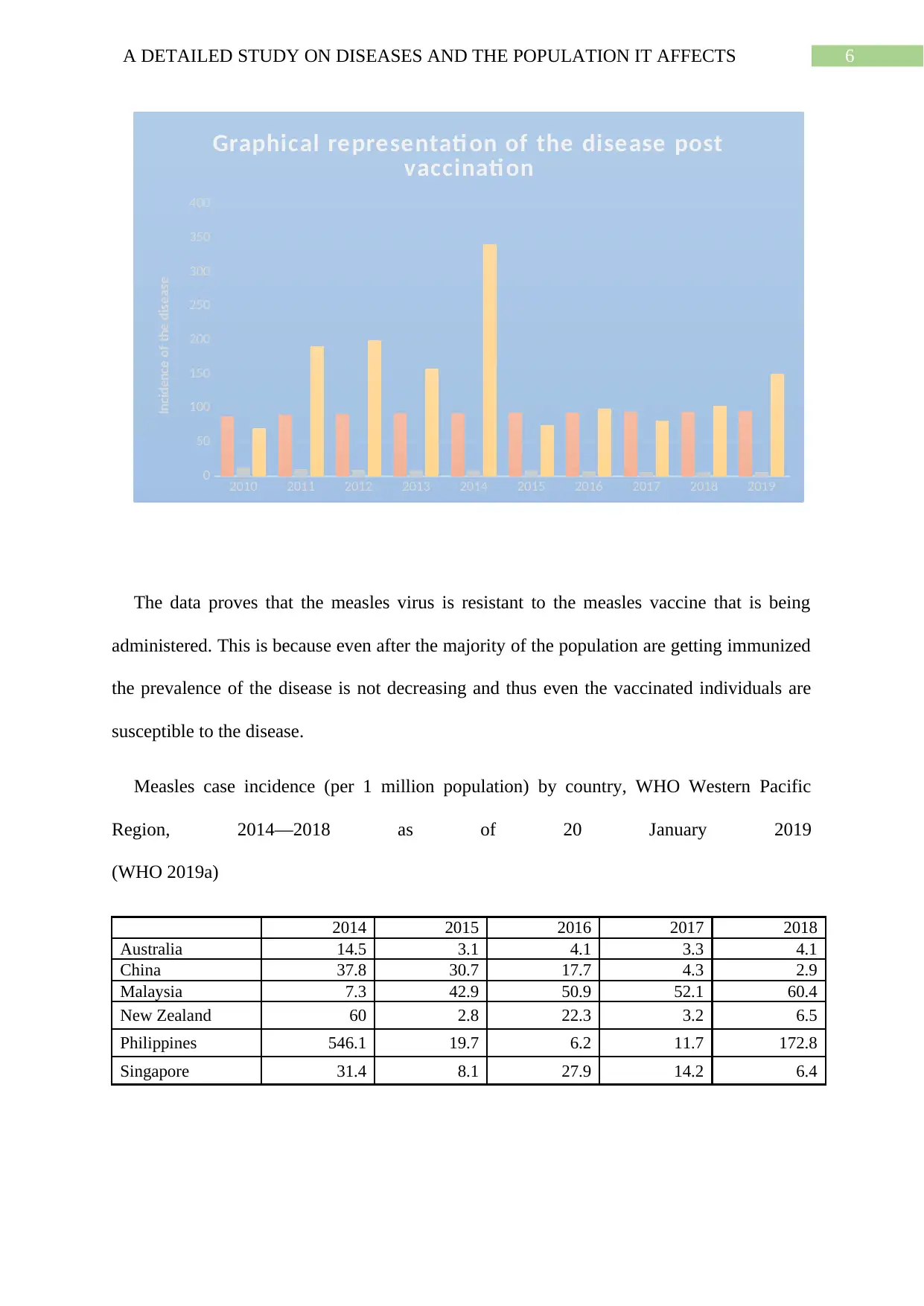
Measles case incidence (per 1 million population) by country, WHO Western Pacific
Region, 2014—2018 as of 20 January 2019
(WHO 2019a)
2014 2015 2016 2017 2018
Australia 14.5 3.1 4.1 3.3 4.1
China 37.8 30.7 17.7 4.3 2.9
Malaysia 7.3 42.9 50.9 52.1 60.4
New Zealand 60 2.8 22.3 3.2 6.5
Philippines 546.1 19.7 6.2 11.7 172.8
Singapore 31.4 8.1 27.9 14.2 6.4
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
0
50
100
150
200
250
300
350
400
Graphical representati on of the disease post
vaccinati on
Incidence of the disease
The data proves that the measles virus is resistant to the measles vaccine that is being
administered. This is because even after the majority of the population are getting immunized
the prevalence of the disease is not decreasing and thus even the vaccinated individuals are
susceptible to the disease.
Measles case incidence (per 1 million population) by country, WHO Western Pacific
Region, 2014—2018 as of 20 January 2019
(WHO 2019a)
2014 2015 2016 2017 2018
Australia 14.5 3.1 4.1 3.3 4.1
China 37.8 30.7 17.7 4.3 2.9
Malaysia 7.3 42.9 50.9 52.1 60.4
New Zealand 60 2.8 22.3 3.2 6.5
Philippines 546.1 19.7 6.2 11.7 172.8
Singapore 31.4 8.1 27.9 14.2 6.4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
Australia China Malaysia New Zealand Philippines Singapore
0
100
200
300
400
500
600
Comparative study of the incidence of measles in the
Western countries
Incidence of Measles
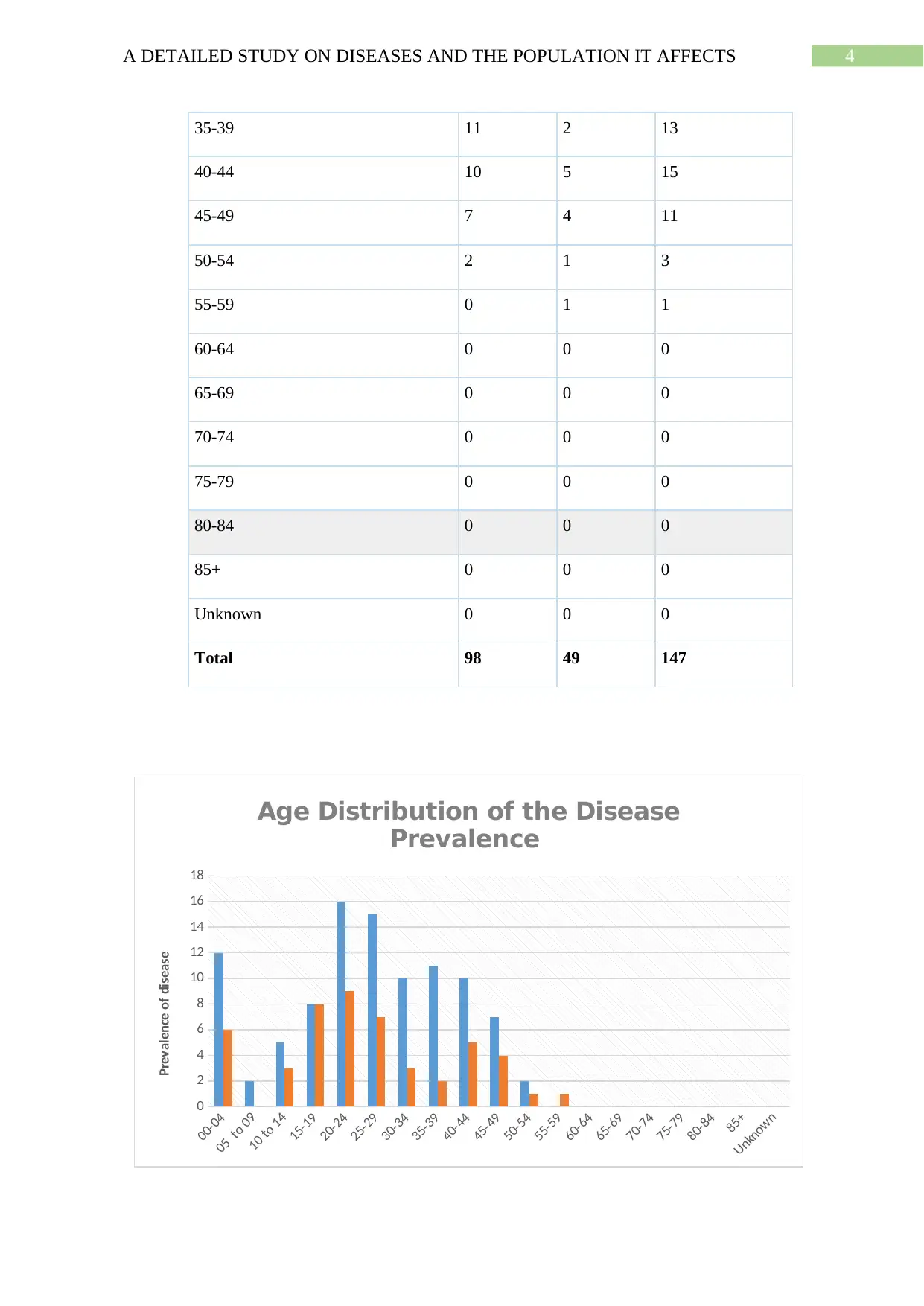
Based on the above graphical details it is evident that the prevalence of the disease was
highest in Philippines majorly affected in the year 2014 and 2018. The prevalence of the
disease is comparatively lesser in Australia that in the other countries based on the statistical
data provided.
Answer 2:
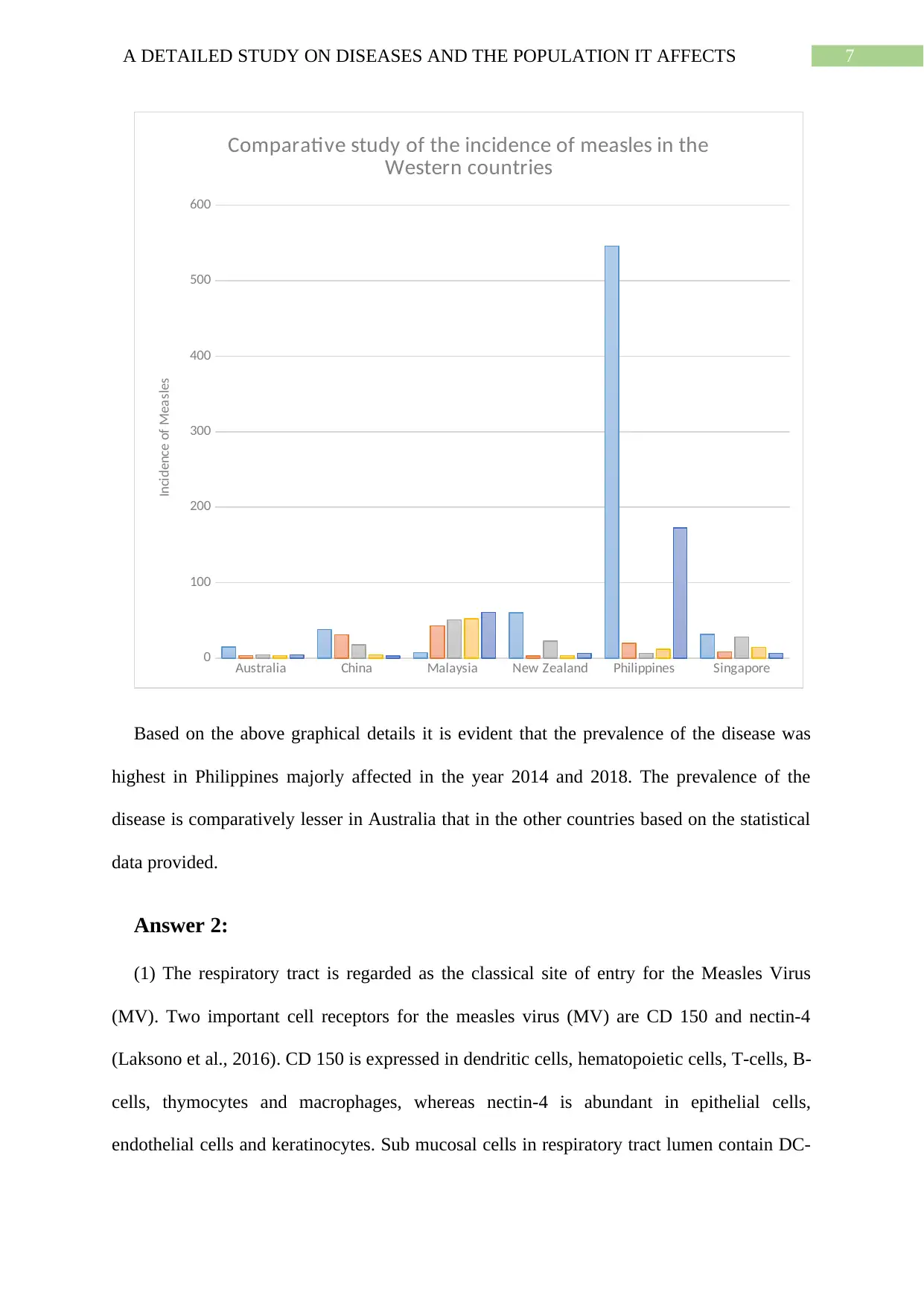
(1) The respiratory tract is regarded as the classical site of entry for the Measles Virus
(MV). Two important cell receptors for the measles virus (MV) are CD 150 and nectin-4
(Laksono et al., 2016). CD 150 is expressed in dendritic cells, hematopoietic cells, T-cells, B-
cells, thymocytes and macrophages, whereas nectin-4 is abundant in epithelial cells,
endothelial cells and keratinocytes. Sub mucosal cells in respiratory tract lumen contain DC-
Australia China Malaysia New Zealand Philippines Singapore
0
100
200
300
400
500
600
Comparative study of the incidence of measles in the
Western countries
Incidence of Measles
Based on the above graphical details it is evident that the prevalence of the disease was
highest in Philippines majorly affected in the year 2014 and 2018. The prevalence of the
disease is comparatively lesser in Australia that in the other countries based on the statistical
data provided.
Answer 2:
(1) The respiratory tract is regarded as the classical site of entry for the Measles Virus
(MV). Two important cell receptors for the measles virus (MV) are CD 150 and nectin-4
(Laksono et al., 2016). CD 150 is expressed in dendritic cells, hematopoietic cells, T-cells, B-
cells, thymocytes and macrophages, whereas nectin-4 is abundant in epithelial cells,
endothelial cells and keratinocytes. Sub mucosal cells in respiratory tract lumen contain DC-
8A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
SIGN, another cellular receptor for MV (Wang et al., 2014). Another route of entry is
through infection of lymphoid or myeloid cells of the conjunctiva. After infection, the virus
spreads in the body primarily through the thymus and bone marrow, and secondarily through
the spleen, lymph nodes and tonsils, affecting the liver, kidney, GI tract and skin through CD
150 immune cells (de Vries et al. 2012) (Ludlow et al., 2015). Clinically, the disease course
begins with the appearance of Koplik’s spots on the buccal mucosa that culminate in a few
days into a maculopapular skin rash. The third stage of disease is transmission which takes
place through large respiratory droplets from the patient’s sneeze/cough or small aerosol
droplets, both of which remain airborne for a couple of hours, especially in poorly ventilated,
humid areas (Nali et al., 2016). Inhaling contaminated air or touching infected surfaces can
cause disease. MV is transmissible 4 days before and after the appearance of skin rashes.
Fig 1: Pathogenesis of Measles virus (Ludlow et al., 2015)
(2) Most cases of measles may resolve without causing major complications. However, the
blood-brain barrier or the lymphatic vessels in the brain may allow CNS infection to occur.
The most common of these neurological complications is ADEM (Acute disseminated
SIGN, another cellular receptor for MV (Wang et al., 2014). Another route of entry is
through infection of lymphoid or myeloid cells of the conjunctiva. After infection, the virus
spreads in the body primarily through the thymus and bone marrow, and secondarily through
the spleen, lymph nodes and tonsils, affecting the liver, kidney, GI tract and skin through CD
150 immune cells (de Vries et al. 2012) (Ludlow et al., 2015). Clinically, the disease course
begins with the appearance of Koplik’s spots on the buccal mucosa that culminate in a few
days into a maculopapular skin rash. The third stage of disease is transmission which takes
place through large respiratory droplets from the patient’s sneeze/cough or small aerosol
droplets, both of which remain airborne for a couple of hours, especially in poorly ventilated,
humid areas (Nali et al., 2016). Inhaling contaminated air or touching infected surfaces can
cause disease. MV is transmissible 4 days before and after the appearance of skin rashes.
Fig 1: Pathogenesis of Measles virus (Ludlow et al., 2015)
(2) Most cases of measles may resolve without causing major complications. However, the
blood-brain barrier or the lymphatic vessels in the brain may allow CNS infection to occur.
The most common of these neurological complications is ADEM (Acute disseminated
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
encephalomyelitis), an autoimmune response generated on the basis of structural similarity
between myelin and MV proteins (Wender 2011). The resultant demyelination manifests as
ataxia, sensory and motor loss, and altered mental status that lead to death (15% fatality rate)
(Bale Jr, 2014). Within a year of acute infection or live virus vaccination, immune-
compromised patients or infants may acquire MIBE (Measles inclusion body encephalitis).
The symptoms of focal seizures, altered mental status, and loss of hearing or vision may
culminate in coma followed by death. The rarest complication is SSPE (Subacute sclerosing
pan encephalitis) (Guler, Kucukkoc & Iscan, 2015). Years after a normal resolution of
measles, symptoms appear as altered behaviour, declining school performance, myoclonic
seizure and ataxia that prove to be fatal in 1-3 years (Laksono et al. 2016). The case fatality
rate in Australia is low due to effective vaccination and disease management. Only 3 deaths
were reported from 1996-2016 (AIHW 2018).
(3) Young children who have not been vaccinated against measles are at the highest risk of
infection as well as its complications (CDC, 2019). Pregnant women who have not been
vaccinated are also at risk. People who received vaccination but did not develop immunity to
the disease are also vulnerable to infection (WHO 2019b). People in proximity of patients in
closed, poorly ventilated environments are at risk because this disease is highly transmissible
through inhalation of contaminated air or direct contact with infected surfaces (Maltezou and
Wicker, 2013). Once a person has acquired the disease, he or she develops lifelong immunity
to it. Adults without a history of measles and without vaccination can be considered
susceptible because their bodies have not developed immunity either way (Gostin, 2015).
Answer 3:
(1) Herd immunity is a condition in which majority of the population has acquired
resistance to the spread of a contagious disease by receiving vaccination and successfully
encephalomyelitis), an autoimmune response generated on the basis of structural similarity
between myelin and MV proteins (Wender 2011). The resultant demyelination manifests as
ataxia, sensory and motor loss, and altered mental status that lead to death (15% fatality rate)
(Bale Jr, 2014). Within a year of acute infection or live virus vaccination, immune-
compromised patients or infants may acquire MIBE (Measles inclusion body encephalitis).
The symptoms of focal seizures, altered mental status, and loss of hearing or vision may
culminate in coma followed by death. The rarest complication is SSPE (Subacute sclerosing
pan encephalitis) (Guler, Kucukkoc & Iscan, 2015). Years after a normal resolution of
measles, symptoms appear as altered behaviour, declining school performance, myoclonic
seizure and ataxia that prove to be fatal in 1-3 years (Laksono et al. 2016). The case fatality
rate in Australia is low due to effective vaccination and disease management. Only 3 deaths
were reported from 1996-2016 (AIHW 2018).
(3) Young children who have not been vaccinated against measles are at the highest risk of
infection as well as its complications (CDC, 2019). Pregnant women who have not been
vaccinated are also at risk. People who received vaccination but did not develop immunity to
the disease are also vulnerable to infection (WHO 2019b). People in proximity of patients in
closed, poorly ventilated environments are at risk because this disease is highly transmissible
through inhalation of contaminated air or direct contact with infected surfaces (Maltezou and
Wicker, 2013). Once a person has acquired the disease, he or she develops lifelong immunity
to it. Adults without a history of measles and without vaccination can be considered
susceptible because their bodies have not developed immunity either way (Gostin, 2015).
Answer 3:
(1) Herd immunity is a condition in which majority of the population has acquired
resistance to the spread of a contagious disease by receiving vaccination and successfully
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
developing immunity to it (Fine, Eames & Heymann 2011). This concept is of maximum
significance to those who cannot receive the vaccine because of allergies or weak immune
systems; they rely on the immunised state of those around them to confer protection upon
them Farrugia and Quinti, 2019). If herd immunity drops, there definitely is risk of an
outbreak (Plans Rubio, 2019). This is because measles is a highly contagious disease. Most
susceptible to it are non-immunized infants, pregnant women, people who have not
developed immunity despite receiving vaccination as well as other immuno-compromised
patients. When most people in a community are not vaccinated and therefore not immune to
the disease, even a few people contracting it will expose huge risk to those around them
because the disease spreads by inhalation of droplets or aerosols as well as by direct contact
with infected surfaces. Also notable is the fact that there exists no particular treatment for
measles; one can only manage the symptoms (Holland and Zachary, 2014). Therefore, efforts
must be put in to achieve community level immunity by vaccination.
(2) Rubella is a contagious viral disease which can be transmitted from an expectant
mother to her child. It may cause miscarriage or Congenital Rubella Syndrome (CRS) in the
foetus. These defects include eye diseases (retinitis, glaucoma, and cataracts), hearing loss,
congenital heart defect, bone disease, microcephaly, diabetes and mental retardation (McLean
2013). Rubella can be avoided by the administration of a vaccine. However, this vaccine
must not be administered during pregnancy. It can be given either at least one month before
pregnancy or upon completion or termination of pregnancy (Prymula et al., 2014). Either
way, the defects the baby might have inherited from an infected mother cannot be reversed.
Therefore, it is extremely important that females be vaccinated against rubella because
otherwise, they must plan their pregnancy keeping in mind the administration of a vaccine or
put their baby at risk (Demicheli et al., 2013). It is important for males to also be immunised
because rubella can be transmitted sexually to their partners. If a woman is not vaccinated or
developing immunity to it (Fine, Eames & Heymann 2011). This concept is of maximum
significance to those who cannot receive the vaccine because of allergies or weak immune
systems; they rely on the immunised state of those around them to confer protection upon
them Farrugia and Quinti, 2019). If herd immunity drops, there definitely is risk of an
outbreak (Plans Rubio, 2019). This is because measles is a highly contagious disease. Most
susceptible to it are non-immunized infants, pregnant women, people who have not
developed immunity despite receiving vaccination as well as other immuno-compromised
patients. When most people in a community are not vaccinated and therefore not immune to
the disease, even a few people contracting it will expose huge risk to those around them
because the disease spreads by inhalation of droplets or aerosols as well as by direct contact
with infected surfaces. Also notable is the fact that there exists no particular treatment for
measles; one can only manage the symptoms (Holland and Zachary, 2014). Therefore, efforts
must be put in to achieve community level immunity by vaccination.
(2) Rubella is a contagious viral disease which can be transmitted from an expectant
mother to her child. It may cause miscarriage or Congenital Rubella Syndrome (CRS) in the
foetus. These defects include eye diseases (retinitis, glaucoma, and cataracts), hearing loss,
congenital heart defect, bone disease, microcephaly, diabetes and mental retardation (McLean
2013). Rubella can be avoided by the administration of a vaccine. However, this vaccine
must not be administered during pregnancy. It can be given either at least one month before
pregnancy or upon completion or termination of pregnancy (Prymula et al., 2014). Either
way, the defects the baby might have inherited from an infected mother cannot be reversed.
Therefore, it is extremely important that females be vaccinated against rubella because
otherwise, they must plan their pregnancy keeping in mind the administration of a vaccine or
put their baby at risk (Demicheli et al., 2013). It is important for males to also be immunised
because rubella can be transmitted sexually to their partners. If a woman is not vaccinated or
11A DETAILED STUDY ON DISEASES AND THE POPULATION IT AFFECTS
has not developed immunity to rubella, her infected partner puts her and her baby at risk
(Lambert et al., 2015). He also puts the general community at risk, so vaccination must be
ensured for everyone.
(3) The MMR vaccine has several side effects ranging in severity. Firstly, some soreness,
itching, redness, burning or swelling may occur at the site of injection for 1-2 days. Around 7
to 10 days after vaccination, the recipient might experience fever (above 39.4 °C), light red
rash, runny nose, puffy eyes, cough, lethargy or drowsiness and salivary gland swelling.
Some rare side effects include febrile convulsions, temporary stiffness and joint pain,
bruising or bleeding from a temporarily low platelet count. Thrombocytopenia is very rare.
Anaphylaxis (serious allergic reaction) occurs in less than 1 in a million cases (Gowda et al.,
2013).
Autism is a neurodevelopmental disorder with a genetic basis and is not a side effect of the
vaccine. Research has been conducted and even children with autistic siblings did not get
autism because of the vaccine (DeStefano & Shimabukuro 2019).
Answer 4:
(1) It is important to respect the individuality of others, letting them decide what they want
for their children and family without any external compulsion. Respecting would mean
letting people choose, and not judging or discriminating them on the basis of their choices.
However, there is a limit to which this freedom can be allowed (Racine et al., 2013). When
the question is of public safety with respect to a contagious disease, it does not remain an
individual decision. Respect and regard for those around you demands that decisions be taken
keeping in mind the safety and stability of all parties involved, namely other families or the
community, healthcare providers and government authorities. Valuing the health and well-
being of others would signify true respect for them (Minkoff, 2014).
has not developed immunity to rubella, her infected partner puts her and her baby at risk
(Lambert et al., 2015). He also puts the general community at risk, so vaccination must be
ensured for everyone.
(3) The MMR vaccine has several side effects ranging in severity. Firstly, some soreness,
itching, redness, burning or swelling may occur at the site of injection for 1-2 days. Around 7
to 10 days after vaccination, the recipient might experience fever (above 39.4 °C), light red
rash, runny nose, puffy eyes, cough, lethargy or drowsiness and salivary gland swelling.
Some rare side effects include febrile convulsions, temporary stiffness and joint pain,
bruising or bleeding from a temporarily low platelet count. Thrombocytopenia is very rare.
Anaphylaxis (serious allergic reaction) occurs in less than 1 in a million cases (Gowda et al.,
2013).
Autism is a neurodevelopmental disorder with a genetic basis and is not a side effect of the
vaccine. Research has been conducted and even children with autistic siblings did not get
autism because of the vaccine (DeStefano & Shimabukuro 2019).
Answer 4:
(1) It is important to respect the individuality of others, letting them decide what they want
for their children and family without any external compulsion. Respecting would mean
letting people choose, and not judging or discriminating them on the basis of their choices.
However, there is a limit to which this freedom can be allowed (Racine et al., 2013). When
the question is of public safety with respect to a contagious disease, it does not remain an
individual decision. Respect and regard for those around you demands that decisions be taken
keeping in mind the safety and stability of all parties involved, namely other families or the
community, healthcare providers and government authorities. Valuing the health and well-
being of others would signify true respect for them (Minkoff, 2014).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





