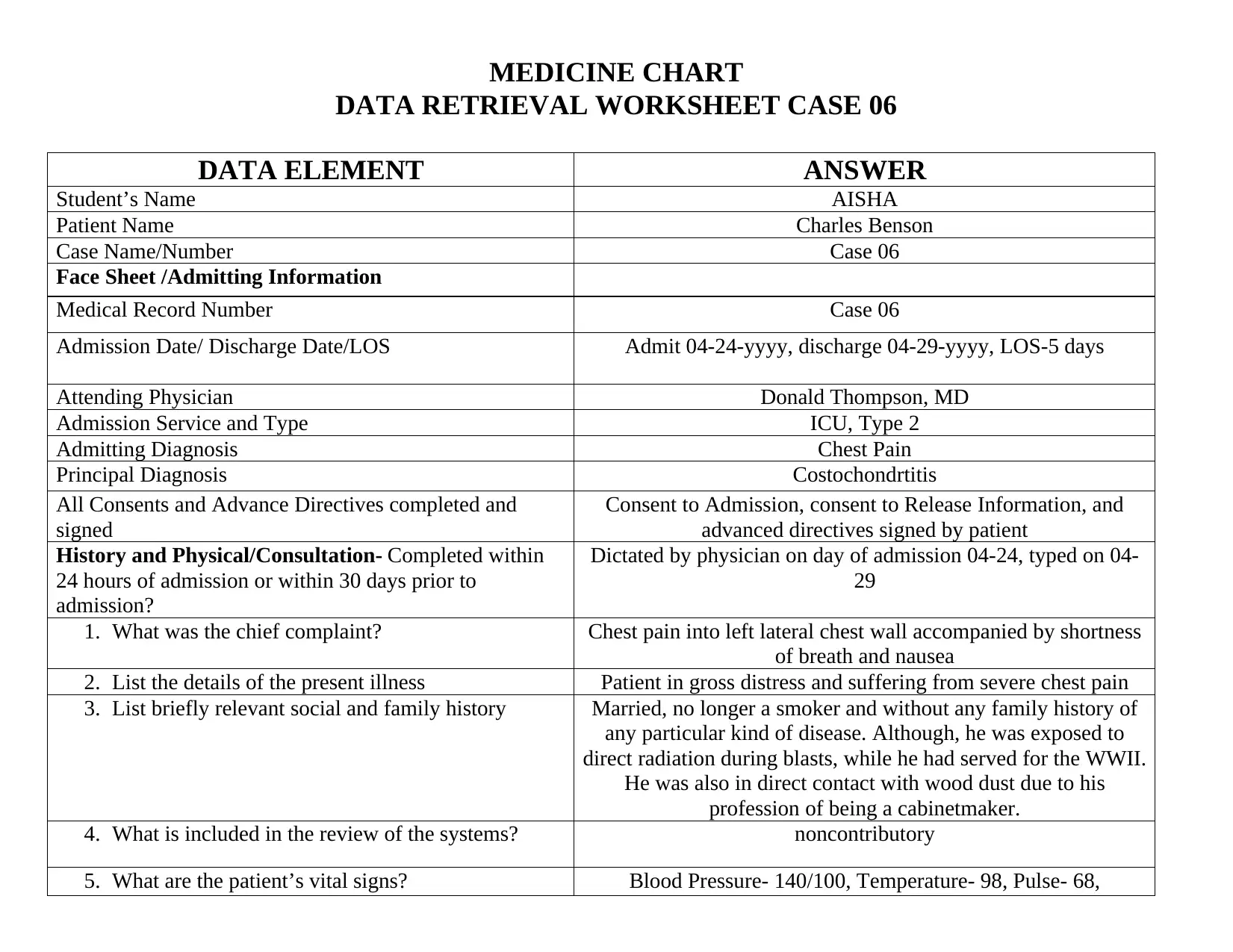
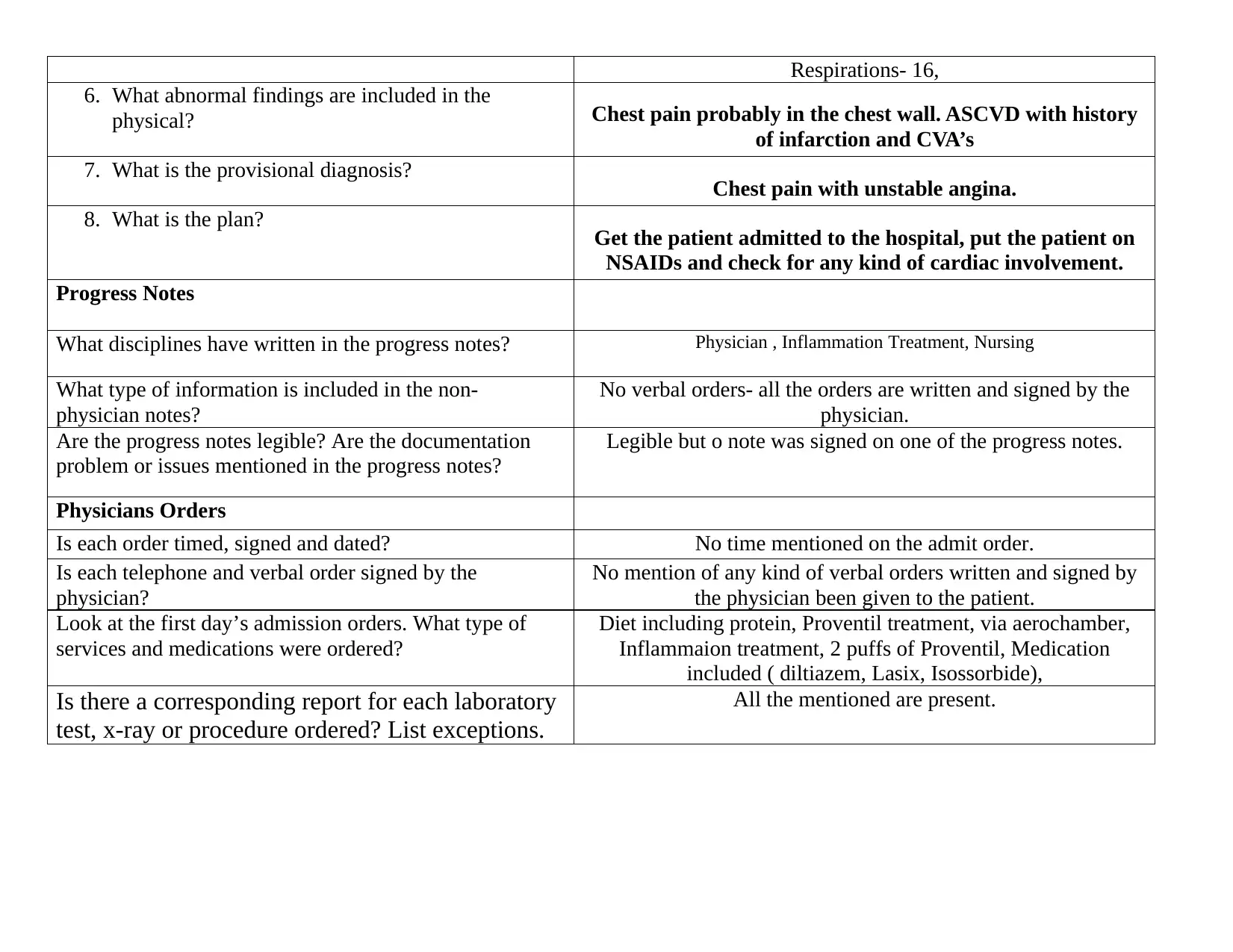
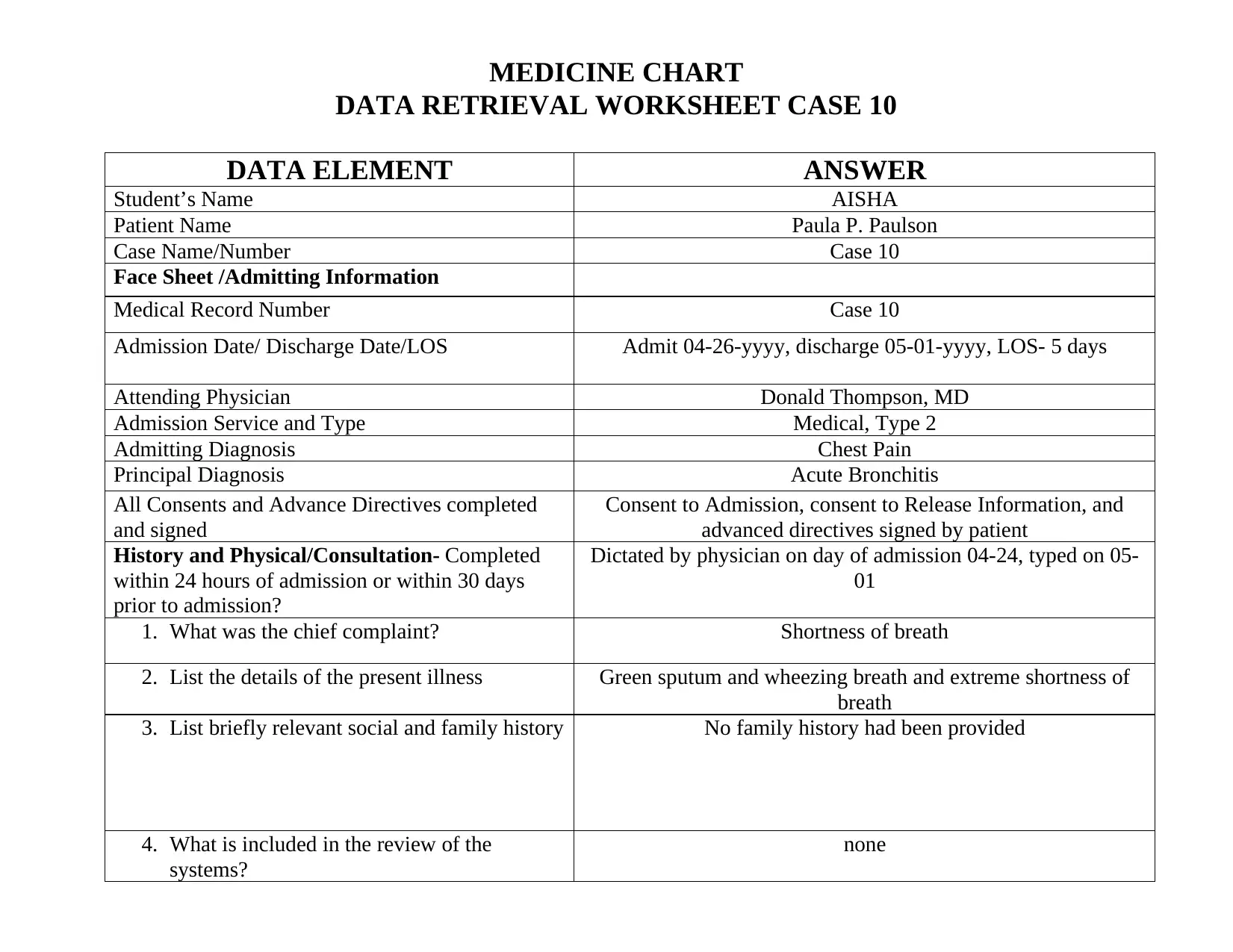
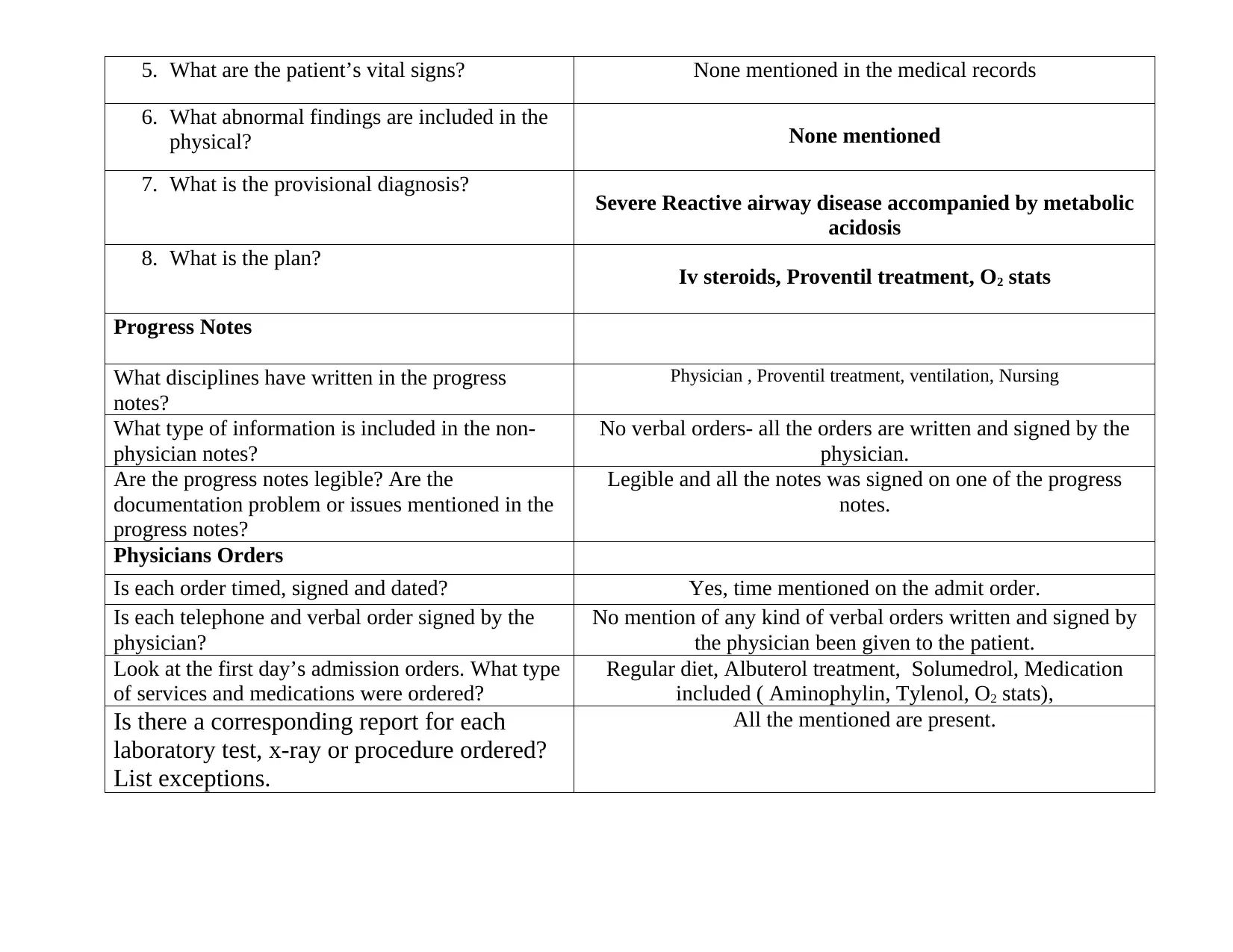
Medical Chart Data Retrieval Worksheet: Cases 06 and 10 Evaluation
VerifiedAdded on 2022/08/08
|5
|1033
|16
Homework Assignment
AI Summary
This assignment presents a detailed medical chart data retrieval worksheet, focusing on Cases 06 and 10. The worksheet requires the student to extract and analyze critical information from the provided medical records, adhering to specific guidelines. The student, Aisha, is tasked with identifying key data elements across various sections of the medical chart, including face sheets, history and physical reports, progress notes, and physician's orders. The analysis includes assessing the completeness and accuracy of documentation, calculating length of stay, identifying diagnoses, and evaluating the presence of necessary consents and directives. The assignment also requires an assessment of the completeness and compliance of physician orders, including timing, signatures, and corresponding reports. The assignment utilizes guidelines from Shanholtzer, Chapter 6 and web-based resources to ensure a thorough analysis. The student is also required to identify any documentation issues and non-compliance with established guidelines. This exercise aims to enhance the student's ability to interpret medical documentation and apply chart analysis principles.
1 out of 5








![[object Object]](/_next/static/media/star-bottom.7253800d.svg)