Clinical Information System Design for Medication Adherence (2019)
VerifiedAdded on 2022/11/14
|14
|3394
|131
Project
AI Summary
This report proposes a Clinical Information System (CIS), specifically a digital adherence system (DAS), to address the global challenge of medication non-adherence. The system is designed as a mobile application to remind patients to take their medications and record adherence, leveraging technologies like SMS and integrating with existing healthcare information systems such as My Health Record. The report details the problem statement, discussing factors contributing to non-adherence and limitations of current strategies. It outlines the system's design, including data sharing capabilities and benefits for clinicians, caregivers, and patients, such as improved patient care and reduced costs. Ethical considerations, including data privacy and security measures, are also addressed. The report emphasizes the importance of data integration, interoperability, and the use of appropriate clinical terminology to improve healthcare outcomes. The DAS application aims to enhance medication adherence through digital observation, automated reminders, and data-driven insights. This comprehensive approach aims to improve the quality of care and patient outcomes in the Australian healthcare context.

HEALTH INFORMATICS 1
Health Informatics
Student Name
Institution
Date
Health Informatics
Student Name
Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

HEALTH INFORMATICS 2
Table of Contents
Introduction................................................................................................................................3
Problem Statement.....................................................................................................................3
Digital Observation of Medication Adherence..........................................................................5
Data sharing among the different Healthcare Information Systems..........................................5
System Design............................................................................................................................6
Benefits of DAS to Clinicians, Caregivers, and Patients...........................................................7
Ethical, Security and Privacy Considerations in Collecting, Storing and Communicating Data
....................................................................................................................................................7
Conclusion..................................................................................................................................8
Reference List..........................................................................................................................10
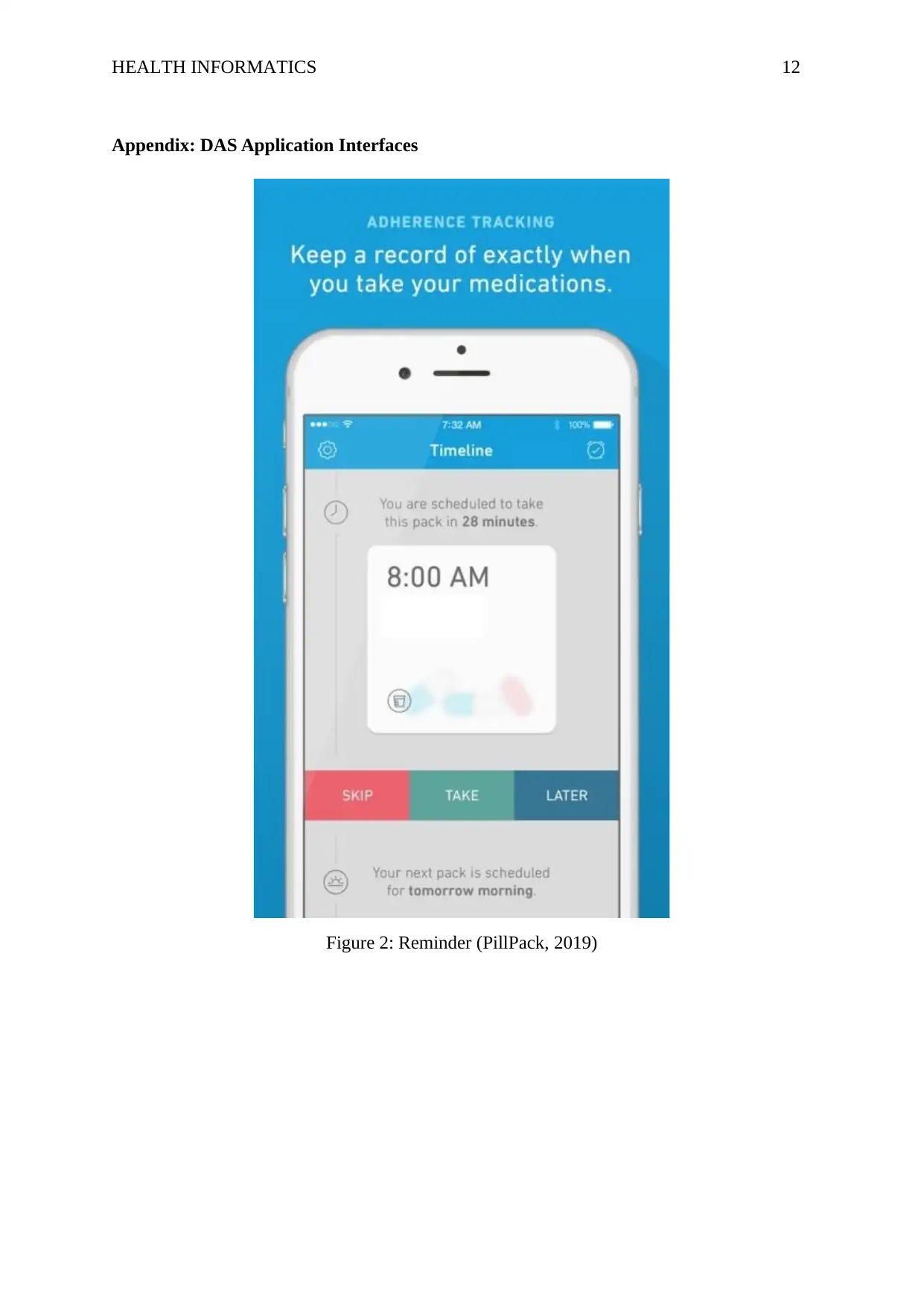
Appendix: DAS Application Interfaces...................................................................................12
Table of Contents
Introduction................................................................................................................................3
Problem Statement.....................................................................................................................3
Digital Observation of Medication Adherence..........................................................................5
Data sharing among the different Healthcare Information Systems..........................................5
System Design............................................................................................................................6
Benefits of DAS to Clinicians, Caregivers, and Patients...........................................................7
Ethical, Security and Privacy Considerations in Collecting, Storing and Communicating Data
....................................................................................................................................................7
Conclusion..................................................................................................................................8
Reference List..........................................................................................................................10
Appendix: DAS Application Interfaces...................................................................................12
HEALTH INFORMATICS 3
Introduction
Adherence in clinical setup refers to collaborative, voluntary, and active engagement
of the patient in a mutually aggregable behavior and actions aimed at achieving positive
therapeutic outcome (Ahmed et al., 2018). In essence, the patient has the choice and that the
healthcare providers and the patients create a mutual medical regimen and treatment goals.
From the above description, medication adherence, therefore, refers to the behavior that the
patient exhibits in continuously taking the prescribed medicine in the right dosage for the
specific time mentioned by the healthcare provider.
There is a rising concern among the healthcare stakeholders including clinicians,
caregivers, and medical providers on the aspect of medication adherence because of the
increasing rate of nonadherence or medical prescriptions which has resulted in adverse effects
and increased cost of medication and care (Ho, Bryson and Rumsfeld, 2012). According to a
recent study conducted by WHO, the rate of medication nonadherence is increasing across
the world (Brown and Bussell, 2011). There is need to have a collaborative partnership with
patients in order to achieve long-term results and therapeutic objectives unlike other quality
mechanisms that are controlled directly by healthcare providers such as giving prescriptions
during discharge.
Currently, in a routine clinical practice, measuring patient’s medication adherence and
the use of various intervention strategies to enhance adherence has still proven to be less
effective. As a result, medication adherence has been referred by many as the next frontier in
improving the quality of healthcare and has become one of the key research topics in clinical
medicine. The goal of this report is to propose a clinical information system that will be able
to address the current challenges in medication adherence.
Problem Statement
Non-adherence to medical prescriptions has become a normal behavior among many
patients. According to research conducted by Chappell (2015), approximately 30% of the
patients do not fill medication sheets after discharge, as a result it is difficult to keep tract and
ascertain that the patient has taken his/her medication. There is a rapid decline in adherence
to prescribed medication among the patient during the early stages after discharge (Mitchell,
Introduction
Adherence in clinical setup refers to collaborative, voluntary, and active engagement
of the patient in a mutually aggregable behavior and actions aimed at achieving positive
therapeutic outcome (Ahmed et al., 2018). In essence, the patient has the choice and that the
healthcare providers and the patients create a mutual medical regimen and treatment goals.
From the above description, medication adherence, therefore, refers to the behavior that the
patient exhibits in continuously taking the prescribed medicine in the right dosage for the
specific time mentioned by the healthcare provider.
There is a rising concern among the healthcare stakeholders including clinicians,
caregivers, and medical providers on the aspect of medication adherence because of the
increasing rate of nonadherence or medical prescriptions which has resulted in adverse effects
and increased cost of medication and care (Ho, Bryson and Rumsfeld, 2012). According to a
recent study conducted by WHO, the rate of medication nonadherence is increasing across
the world (Brown and Bussell, 2011). There is need to have a collaborative partnership with
patients in order to achieve long-term results and therapeutic objectives unlike other quality
mechanisms that are controlled directly by healthcare providers such as giving prescriptions
during discharge.
Currently, in a routine clinical practice, measuring patient’s medication adherence and
the use of various intervention strategies to enhance adherence has still proven to be less
effective. As a result, medication adherence has been referred by many as the next frontier in
improving the quality of healthcare and has become one of the key research topics in clinical
medicine. The goal of this report is to propose a clinical information system that will be able
to address the current challenges in medication adherence.
Problem Statement
Non-adherence to medical prescriptions has become a normal behavior among many
patients. According to research conducted by Chappell (2015), approximately 30% of the
patients do not fill medication sheets after discharge, as a result it is difficult to keep tract and
ascertain that the patient has taken his/her medication. There is a rapid decline in adherence
to prescribed medication among the patient during the early stages after discharge (Mitchell,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH INFORMATICS 4
Chong and Lim, 2016). Even though the period of transition between outpatient environment
and hospital environment seems to be specifically a high-risk period.
The causative elements of medication non-adherence are complicated and entails
several aspects such as healthcare related issues (poor user-experience, lack of counselling),
therapy related issued (toxicities), structural issues (medication costs, distance from the
clinic), and psychological problems (stigma, depression, drug abuse) (Car et al., 2017). In
order to address this challenge, healthcare providers came up with a strategy, directly
observed therapy (DOT), which was established to minimize medication non adherence.
Nevertheless, this strategy has been less effective and have received resistance from some
stakeholders because of the fact that it may impinge on the autonomy of the patient and has
less chances of enhancing the treatment results as compared to other strategies like self-
administered therapy (Kvarnström, Airaksinen and Liira, 2018).
As a result, clinicians have identified the need to have a clinical information system
that will help in addressing the problem of medication no-adherence (Kini and Ho, 2018).
This has been attributed to the growth and advancement of technology that has made it
possible to access records and medical services from the phone. Developing a clinical
information system, in this case the system will be referred to as digital adherence system
(DAS), may help and improve medication adherence across the globe. The information
system will support several platforms ranging from ingestible sensors, digital pillboxes, to
short message services (SMS). The information system will be designed as a mobile phone
application that will automatically remind the patient to take medication and fill in the
medication sheet on the application acknowledging that he/she has taken the medicine.
According to a study done by Krousel-Wood et al. (2010), many stakeholders have
high hopes that DAS will have a positive impact on medication adherence. This is because,
the system will be designed to be user specific, that is the user logs in with the provided
credentials and will be able to track his/her prescriptions. Also, the healthcare providers will
be able to monitor if the patients are taking their prescriptions, and if not, it will be easier to
identify the specific patient and take the necessary action to ensure that they are able to
adhere to the prescribed medicine and medication duration. The application/information
system will utilize cellular networks and other infrastructure to carryout a number of
functions including tracing dosing history, observing the doses taken digitally, and reminding
Chong and Lim, 2016). Even though the period of transition between outpatient environment
and hospital environment seems to be specifically a high-risk period.
The causative elements of medication non-adherence are complicated and entails
several aspects such as healthcare related issues (poor user-experience, lack of counselling),
therapy related issued (toxicities), structural issues (medication costs, distance from the
clinic), and psychological problems (stigma, depression, drug abuse) (Car et al., 2017). In
order to address this challenge, healthcare providers came up with a strategy, directly
observed therapy (DOT), which was established to minimize medication non adherence.
Nevertheless, this strategy has been less effective and have received resistance from some
stakeholders because of the fact that it may impinge on the autonomy of the patient and has
less chances of enhancing the treatment results as compared to other strategies like self-
administered therapy (Kvarnström, Airaksinen and Liira, 2018).
As a result, clinicians have identified the need to have a clinical information system
that will help in addressing the problem of medication no-adherence (Kini and Ho, 2018).
This has been attributed to the growth and advancement of technology that has made it
possible to access records and medical services from the phone. Developing a clinical
information system, in this case the system will be referred to as digital adherence system
(DAS), may help and improve medication adherence across the globe. The information
system will support several platforms ranging from ingestible sensors, digital pillboxes, to
short message services (SMS). The information system will be designed as a mobile phone
application that will automatically remind the patient to take medication and fill in the
medication sheet on the application acknowledging that he/she has taken the medicine.
According to a study done by Krousel-Wood et al. (2010), many stakeholders have
high hopes that DAS will have a positive impact on medication adherence. This is because,
the system will be designed to be user specific, that is the user logs in with the provided
credentials and will be able to track his/her prescriptions. Also, the healthcare providers will
be able to monitor if the patients are taking their prescriptions, and if not, it will be easier to
identify the specific patient and take the necessary action to ensure that they are able to
adhere to the prescribed medicine and medication duration. The application/information
system will utilize cellular networks and other infrastructure to carryout a number of
functions including tracing dosing history, observing the doses taken digitally, and reminding
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH INFORMATICS 5
the patients to take the medication. The data collected will be very useful for the healthcare
providers to determine and address the issues of medication non-adherence.
Digital Observation of Medication Adherence
The system will be expected to record, track, and observe dose-taking which is
particularly an important objective of the system. However, some stakeholders have argued
that monitoring and tracking patients regarding taking doses is an invasion of privacy but,
however, the system is intended to remind the patient on the different time that he/she should
take the medication over a specific period of time. Implementing DAS will reduce the risk of
healthcare providers mis-recording information accidentally and minimizes the efforts that a
patient needs to put in adhering to medication schedule. However, one of the setbacks
associated with DAS is that, the patient might fill in the medication sheet on the app but have
not actually taken the prescription. However, according to Yap, Thirumoorthy and Kwan
(2015), there is a 2% likelihood of such an event occurring which is still a smaller percentage
but with time it will reduce.
Electronic data from the various pharmacies have been used to measure medication
adherence using the frequency of patients obtaining refills. Nevertheless, this strategy is still
ineffective because the data collected from the pharmacies are insufficient because many of
the pharmacies lack electronic records showing patient refill patterns. As such, the digital
adherence system will come in handy in solving such limitations.
Data sharing among the different Healthcare Information Systems
The clinical information system, DAS, will be able to integrate with other electronic
systems such as My Health record, Hospital systems, GP Clinics, and Pathology systems by
integrating a shared database. DAS application will be able to pull the various data from the
different healthcare information system such as getting the medical history from My Health
Record and using the information generated to make more informed decision on prescriptions
(Ahrq.gov, 2018). The health messaging standard can be integrated into the DAS application
to offer messaging alerts to the patients when medication time arrives. Healthcare system is
made up of different private and public data collection system which are utilized by various
the patients to take the medication. The data collected will be very useful for the healthcare
providers to determine and address the issues of medication non-adherence.
Digital Observation of Medication Adherence
The system will be expected to record, track, and observe dose-taking which is
particularly an important objective of the system. However, some stakeholders have argued
that monitoring and tracking patients regarding taking doses is an invasion of privacy but,
however, the system is intended to remind the patient on the different time that he/she should
take the medication over a specific period of time. Implementing DAS will reduce the risk of
healthcare providers mis-recording information accidentally and minimizes the efforts that a
patient needs to put in adhering to medication schedule. However, one of the setbacks
associated with DAS is that, the patient might fill in the medication sheet on the app but have
not actually taken the prescription. However, according to Yap, Thirumoorthy and Kwan
(2015), there is a 2% likelihood of such an event occurring which is still a smaller percentage
but with time it will reduce.
Electronic data from the various pharmacies have been used to measure medication
adherence using the frequency of patients obtaining refills. Nevertheless, this strategy is still
ineffective because the data collected from the pharmacies are insufficient because many of
the pharmacies lack electronic records showing patient refill patterns. As such, the digital
adherence system will come in handy in solving such limitations.
Data sharing among the different Healthcare Information Systems
The clinical information system, DAS, will be able to integrate with other electronic
systems such as My Health record, Hospital systems, GP Clinics, and Pathology systems by
integrating a shared database. DAS application will be able to pull the various data from the
different healthcare information system such as getting the medical history from My Health
Record and using the information generated to make more informed decision on prescriptions
(Ahrq.gov, 2018). The health messaging standard can be integrated into the DAS application
to offer messaging alerts to the patients when medication time arrives. Healthcare system is
made up of different private and public data collection system which are utilized by various
HEALTH INFORMATICS 6
sectors and industries including health plans, physicians, hospitals among others to make
decisions (Quinn et al., 2018).
Many authors have focused on the need to have a standard interoperability functions
among the health information systems. There is a possibility of having one database that can
be shared by these systems to facilitate integration and more common understanding of the
healthcare trends and medication adherence among the patients. In addition, the standard
should facilitate sharing and access to healthcare data from different databases. There are a
number of techniques that can be implemented to promote interoperability and integration
among the healthcare systems including S and I Framework, ONC eHealth-Exchange which
offer interoperability functions of healthcare information system which allows both private
and public stakeholders to share data. As a result, there is need to have a standard to govern
and guide data transmission and sharing among the stakeholders. My Health Record, Hospital
systems, GP Clinics, and Pathology systems can be integrated to support medication
adherence for better healthcare and improved quality of life. Community and individual
resilience, and emergency preparedness.
However, it is important to note that integrating data across the different healthcare
information system is a complex process and requires sufficient knowledge, expertise, and
experience (Larson, 2018). Comprehensive healthcare information comes from a variety of
sources which need to be cleaned and filtered for accuracy, relevance, and redundancy.
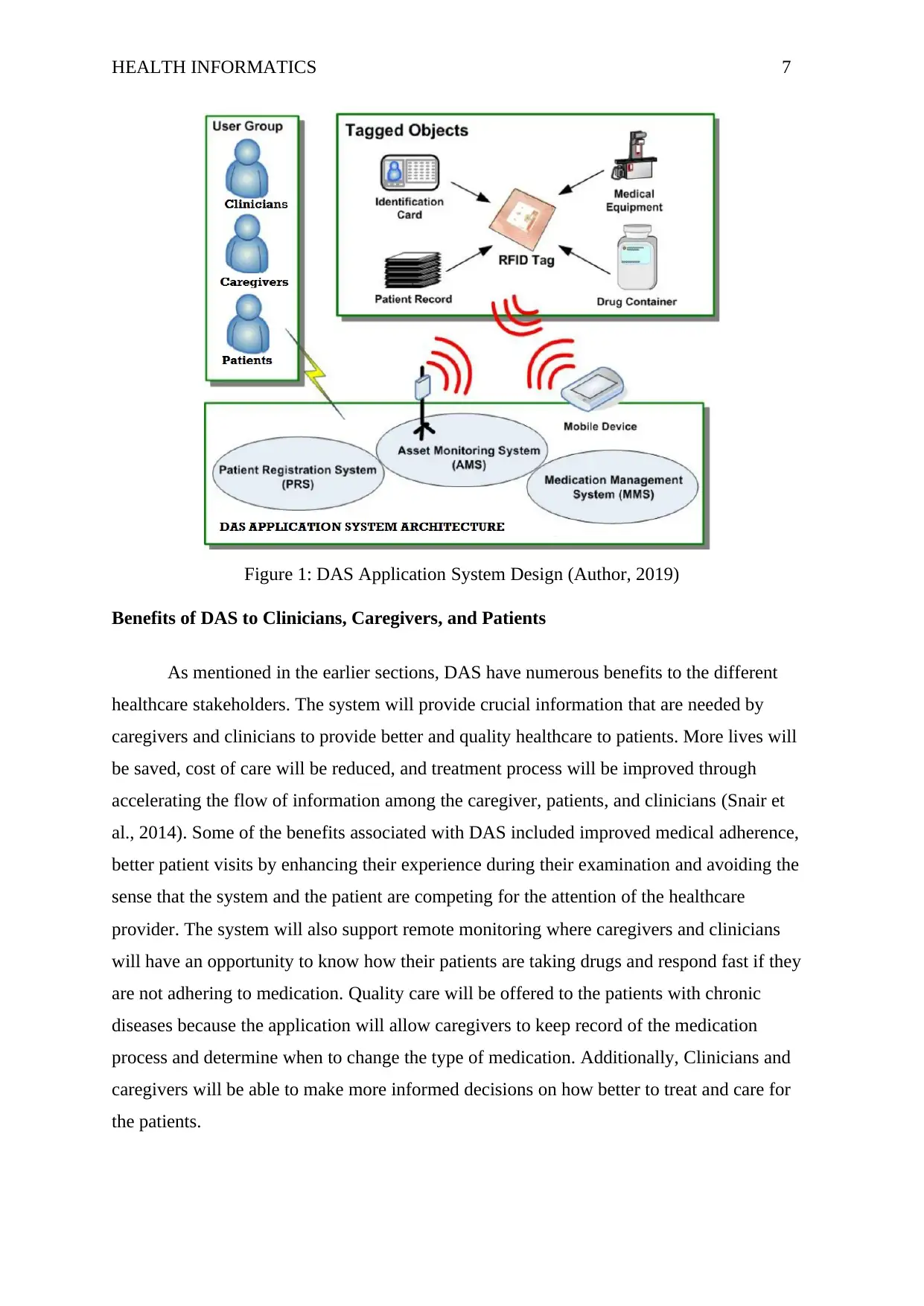
System Design
The following diagram represents DAS application design and how it will interact
with the different elements within associated with the clinical information system.
sectors and industries including health plans, physicians, hospitals among others to make
decisions (Quinn et al., 2018).
Many authors have focused on the need to have a standard interoperability functions
among the health information systems. There is a possibility of having one database that can
be shared by these systems to facilitate integration and more common understanding of the
healthcare trends and medication adherence among the patients. In addition, the standard
should facilitate sharing and access to healthcare data from different databases. There are a
number of techniques that can be implemented to promote interoperability and integration
among the healthcare systems including S and I Framework, ONC eHealth-Exchange which
offer interoperability functions of healthcare information system which allows both private
and public stakeholders to share data. As a result, there is need to have a standard to govern
and guide data transmission and sharing among the stakeholders. My Health Record, Hospital
systems, GP Clinics, and Pathology systems can be integrated to support medication
adherence for better healthcare and improved quality of life. Community and individual
resilience, and emergency preparedness.
However, it is important to note that integrating data across the different healthcare
information system is a complex process and requires sufficient knowledge, expertise, and
experience (Larson, 2018). Comprehensive healthcare information comes from a variety of
sources which need to be cleaned and filtered for accuracy, relevance, and redundancy.
System Design
The following diagram represents DAS application design and how it will interact
with the different elements within associated with the clinical information system.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH INFORMATICS 7
Figure 1: DAS Application System Design (Author, 2019)
Benefits of DAS to Clinicians, Caregivers, and Patients
As mentioned in the earlier sections, DAS have numerous benefits to the different
healthcare stakeholders. The system will provide crucial information that are needed by
caregivers and clinicians to provide better and quality healthcare to patients. More lives will
be saved, cost of care will be reduced, and treatment process will be improved through
accelerating the flow of information among the caregiver, patients, and clinicians (Snair et
al., 2014). Some of the benefits associated with DAS included improved medical adherence,
better patient visits by enhancing their experience during their examination and avoiding the
sense that the system and the patient are competing for the attention of the healthcare
provider. The system will also support remote monitoring where caregivers and clinicians
will have an opportunity to know how their patients are taking drugs and respond fast if they
are not adhering to medication. Quality care will be offered to the patients with chronic
diseases because the application will allow caregivers to keep record of the medication
process and determine when to change the type of medication. Additionally, Clinicians and
caregivers will be able to make more informed decisions on how better to treat and care for
the patients.
Figure 1: DAS Application System Design (Author, 2019)
Benefits of DAS to Clinicians, Caregivers, and Patients
As mentioned in the earlier sections, DAS have numerous benefits to the different
healthcare stakeholders. The system will provide crucial information that are needed by
caregivers and clinicians to provide better and quality healthcare to patients. More lives will
be saved, cost of care will be reduced, and treatment process will be improved through
accelerating the flow of information among the caregiver, patients, and clinicians (Snair et
al., 2014). Some of the benefits associated with DAS included improved medical adherence,
better patient visits by enhancing their experience during their examination and avoiding the
sense that the system and the patient are competing for the attention of the healthcare
provider. The system will also support remote monitoring where caregivers and clinicians
will have an opportunity to know how their patients are taking drugs and respond fast if they
are not adhering to medication. Quality care will be offered to the patients with chronic
diseases because the application will allow caregivers to keep record of the medication
process and determine when to change the type of medication. Additionally, Clinicians and
caregivers will be able to make more informed decisions on how better to treat and care for
the patients.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH INFORMATICS 8
Ethical, Security and Privacy Considerations in Collecting, Storing and Communicating
Data
There are several ethical concerns regarding collection, storage, and use of the data
over the Das application (Harman, Flite and Bond, 2012). Some of the key issues include
confidentiality and privacy (Nate, 2018). Privacy in medical terms refers to right to be alone.
Patients have the right to keep their information from being shared with other people. In this
digital era, digital system is facing numerous threats that are being invented everyday
targeting healthcare information systems. As such, DAS should be able to ensure security of
the data that is collected or shared to ensure privacy and confidentiality of the patients and the
clinicians. No data should be shared without authorization from the appropriate agencies and
with consent from the affected patients (Thorlby et al., 2011). Healthcare information is
considered private and confidential under Australian law and even international laws.
Information that will be associated with DAS application include laboratory results,
treatments notes, diagnoses, and identification data which are stored in various formats in the
DAS application. The key to ensuring confidentiality of patient data is ensuring that only
authorized persons are allowed to access the data. This can be achieved through access
control which involves limiting the people who can access or see the information.
Information security refers to preserving availability, integrity, confidentiality, and
privacy of patient information (Alice, 2017). Information security involved establishing
guidelines that is aimed at securing the data in accordance with Health Information
Technology for Economic and Clinical Health (HITECH) Act and Health Insurance
Portability and Accountability Act (HIPAA) which demands so (Ross, 2018). The rising
concerns regarding the security of clinical information is as a result of increased use of
electronic devices to access electronic health information. Several security mechanisms will
be implemented in DAS application to ensure that the integrity and privacy of patient
information is maintained. Some of the security measures that will be implemented in DAS
application include: evaluation of compliance of healthcare providers and partners, educating
healthcare staff on best practices, data encryption, access control, data usage controls,
monitoring application usage through logging, securing mobile devices, using off-site data
backups, carrying out regular risks’ assessments, and mitigating connected device risks.
Conclusion
Ethical, Security and Privacy Considerations in Collecting, Storing and Communicating
Data
There are several ethical concerns regarding collection, storage, and use of the data
over the Das application (Harman, Flite and Bond, 2012). Some of the key issues include
confidentiality and privacy (Nate, 2018). Privacy in medical terms refers to right to be alone.
Patients have the right to keep their information from being shared with other people. In this
digital era, digital system is facing numerous threats that are being invented everyday
targeting healthcare information systems. As such, DAS should be able to ensure security of
the data that is collected or shared to ensure privacy and confidentiality of the patients and the
clinicians. No data should be shared without authorization from the appropriate agencies and
with consent from the affected patients (Thorlby et al., 2011). Healthcare information is
considered private and confidential under Australian law and even international laws.
Information that will be associated with DAS application include laboratory results,
treatments notes, diagnoses, and identification data which are stored in various formats in the
DAS application. The key to ensuring confidentiality of patient data is ensuring that only
authorized persons are allowed to access the data. This can be achieved through access
control which involves limiting the people who can access or see the information.
Information security refers to preserving availability, integrity, confidentiality, and
privacy of patient information (Alice, 2017). Information security involved establishing
guidelines that is aimed at securing the data in accordance with Health Information
Technology for Economic and Clinical Health (HITECH) Act and Health Insurance
Portability and Accountability Act (HIPAA) which demands so (Ross, 2018). The rising
concerns regarding the security of clinical information is as a result of increased use of
electronic devices to access electronic health information. Several security mechanisms will
be implemented in DAS application to ensure that the integrity and privacy of patient
information is maintained. Some of the security measures that will be implemented in DAS
application include: evaluation of compliance of healthcare providers and partners, educating
healthcare staff on best practices, data encryption, access control, data usage controls,
monitoring application usage through logging, securing mobile devices, using off-site data
backups, carrying out regular risks’ assessments, and mitigating connected device risks.
Conclusion
HEALTH INFORMATICS 9
In conclusion, the rate of medication nonadherence is increasing around the world and
this has got the attention of clinicians. This has been attributed to lack of collaborative
framework that bring the patients, clinicians, and caregivers together. As such, there is need
to have a collaborative partnership with patients in order to achieve long-term results and
therapeutic objectives unlike other quality mechanisms that are controlled directly by
healthcare providers such as giving prescriptions during discharge. Clinicians have identified
the need to have a clinical information system that will help in addressing the problem of
medication no-adherence. This has been attributed to the growth and advancement of
technology that has made it possible to access records and medical services from the phone.
The system will be expected to record, track, and observe dose-taking which is
particularly an important objective of the system. DAS application will be able to pull the
various data from the different healthcare information system such as getting the medical
history from My Health Record and using the information generated to make more informed
decision on prescriptions. The system will also support remote monitoring where caregivers
and clinicians will have an opportunity to know how their patients are taking drugs and
respond fast if they are not adhering to medication.
In conclusion, the rate of medication nonadherence is increasing around the world and
this has got the attention of clinicians. This has been attributed to lack of collaborative
framework that bring the patients, clinicians, and caregivers together. As such, there is need
to have a collaborative partnership with patients in order to achieve long-term results and
therapeutic objectives unlike other quality mechanisms that are controlled directly by
healthcare providers such as giving prescriptions during discharge. Clinicians have identified
the need to have a clinical information system that will help in addressing the problem of
medication no-adherence. This has been attributed to the growth and advancement of
technology that has made it possible to access records and medical services from the phone.
The system will be expected to record, track, and observe dose-taking which is
particularly an important objective of the system. DAS application will be able to pull the
various data from the different healthcare information system such as getting the medical
history from My Health Record and using the information generated to make more informed
decision on prescriptions. The system will also support remote monitoring where caregivers
and clinicians will have an opportunity to know how their patients are taking drugs and
respond fast if they are not adhering to medication.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH INFORMATICS 10
Reference List
Ahmed, I., Ahmad, N., Ali, S., Ali, S., George, A., Saleem Danish, H., Uppal, E., Soo, J.,
Mobasheri, M., King, D., Cox, B. and Darzi, A. (2018). Medication Adherence Apps: Review
and Content Analysis. JMIR mHealth and uHealth, 6(3), p.e62.
Ahrq.gov, A. (2018). 5. Improving Data Collection across the Health Care System | Agency
for Healthcare Research & Quality. [online] Ahrq.gov. Available at:
https://www.ahrq.gov/research/findings/final-reports/iomracereport/reldata5.html [Accessed
24 May 2019].
Alice, L. (2017). The 10 Data Security Measures you must take for your business - Wimi.
[online] Wimi. Available at: https://www.wimi-teamwork.com/blog/10-data-security-
measures/ [Accessed 24 May 2019].
Brown, M. and Bussell, J. (2011). Medication Adherence: WHO Cares?. Mayo Clinic
Proceedings, 86(4), pp.304-314.
Car, J., Tan, W., Huang, Z., Sloot, P. and Franklin, B. (2017). eHealth in the future of
medications management: personalisation, monitoring and adherence. BMC Medicine, 15(1).
Chappell, F. (2015). Medication adherence remains a challenge. Prescriber, 26(12), pp.31-
34.
Harman, L., Flite, C. and Bond, K. (2012). Electronic Health Records: Privacy,
Confidentiality, and Security. Virtual Mentor, 14(9), pp.712-719.
Ho, P., Bryson, C. and Rumsfeld, J. (2012). Medication Adherence. Circulation, 119(23),
pp.3028-3035.
Kini, V. and Ho, P. (2018). Interventions to Improve Medication Adherence. JAMA, 320(23),
p.2461.
Krousel-Wood, M., Muntner, P., Joyce, C., Islam, T., Stanley, E., Holt, E., Morisky, D., He,
J. and Webber, L. (2010). Adverse Effects of Complementary and Alternative Medicine on
Antihypertensive Medication Adherence: Findings from the Cohort Study of Medication
Adherence Among Older Adults. Journal of the American Geriatrics Society, 58(1), pp.54-
61.
Reference List
Ahmed, I., Ahmad, N., Ali, S., Ali, S., George, A., Saleem Danish, H., Uppal, E., Soo, J.,
Mobasheri, M., King, D., Cox, B. and Darzi, A. (2018). Medication Adherence Apps: Review
and Content Analysis. JMIR mHealth and uHealth, 6(3), p.e62.
Ahrq.gov, A. (2018). 5. Improving Data Collection across the Health Care System | Agency
for Healthcare Research & Quality. [online] Ahrq.gov. Available at:
https://www.ahrq.gov/research/findings/final-reports/iomracereport/reldata5.html [Accessed
24 May 2019].
Alice, L. (2017). The 10 Data Security Measures you must take for your business - Wimi.
[online] Wimi. Available at: https://www.wimi-teamwork.com/blog/10-data-security-
measures/ [Accessed 24 May 2019].
Brown, M. and Bussell, J. (2011). Medication Adherence: WHO Cares?. Mayo Clinic
Proceedings, 86(4), pp.304-314.
Car, J., Tan, W., Huang, Z., Sloot, P. and Franklin, B. (2017). eHealth in the future of
medications management: personalisation, monitoring and adherence. BMC Medicine, 15(1).
Chappell, F. (2015). Medication adherence remains a challenge. Prescriber, 26(12), pp.31-
34.
Harman, L., Flite, C. and Bond, K. (2012). Electronic Health Records: Privacy,
Confidentiality, and Security. Virtual Mentor, 14(9), pp.712-719.
Ho, P., Bryson, C. and Rumsfeld, J. (2012). Medication Adherence. Circulation, 119(23),
pp.3028-3035.
Kini, V. and Ho, P. (2018). Interventions to Improve Medication Adherence. JAMA, 320(23),
p.2461.
Krousel-Wood, M., Muntner, P., Joyce, C., Islam, T., Stanley, E., Holt, E., Morisky, D., He,
J. and Webber, L. (2010). Adverse Effects of Complementary and Alternative Medicine on
Antihypertensive Medication Adherence: Findings from the Cohort Study of Medication
Adherence Among Older Adults. Journal of the American Geriatrics Society, 58(1), pp.54-
61.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH INFORMATICS 11
Kvarnström, K., Airaksinen, M. and Liira, H. (2018). Barriers and facilitators to medication
adherence: a qualitative study with general practitioners. BMJ Open, 8(1), p.e015332.
Larson, A. (2018). How Data Sharing and Integrated Information Systems Can Improve
Government Performance. [online] Scholars Strategy Network. Available at:
https://scholars.org/brief/how-data-sharing-and-integrated-information-systems-can-improve-
government-performance [Accessed 24 May 2019].
Mitchell, B., Chong, C. and Lim, W. (2016). Medication adherence 1 month after hospital
discharge in medical inpatients. Internal Medicine Journal, 46(2), pp.185-192.
Nate, L. (2018). Healthcare Cybersecurity: Tips for Securing Private Health Data. [online]
Digital Guardian. Available at: https://digitalguardian.com/blog/healthcare-cybersecurity-
tips-securing-private-health-data [Accessed 24 May 2019].
PillPack, P. (2019). Are you human, bot or alien? | mobile9. [online] Gallery.mobile9.com.
Available at: https://gallery.mobile9.com/asf/ixfawldg9sam/pillpack-medication-reminders/
[Accessed 24 May 2019].
Quinn, M., Forman, J., Harrod, M., Winter, S., Fowler, K., Krein, S., Gupta, A., Saint, S.,
Singh, H. and Chopra, V. (2018). Electronic health records, communication, and data
sharing: challenges and opportunities for improving the diagnostic process. Diagnosis, 0(0).
Ross, S. (2018). 5 Ways to Improve Patient Data Security. [online] The Doctor Weighs In.
Available at: https://thedoctorweighsin.com/patient-data-security/ [Accessed 24 May 2019].
Snair, M., Wizemann, T., Eckert, B. and Altevogt, B. (2014). The impacts of the Affordable
Care Act on preparedness resources and programs. Washington (DC): National Academies
Press.
Thorlby, R., Jorgensen, S., Siegel, B. And Ayanian, J. (2011). How Health Care
Organizations Are Using Data on Patients’ Race and Ethnicity to Improve Quality of
Care. Milbank Quarterly, 89(2), pp.226-255.
Yap, A., Thirumoorthy, T. and Kwan, Y. (2015). Systematic review of the barriers affecting
medication adherence in older adults. Geriatrics & Gerontology International, 16(10),
pp.1093-1101.
Kvarnström, K., Airaksinen, M. and Liira, H. (2018). Barriers and facilitators to medication
adherence: a qualitative study with general practitioners. BMJ Open, 8(1), p.e015332.
Larson, A. (2018). How Data Sharing and Integrated Information Systems Can Improve
Government Performance. [online] Scholars Strategy Network. Available at:
https://scholars.org/brief/how-data-sharing-and-integrated-information-systems-can-improve-
government-performance [Accessed 24 May 2019].
Mitchell, B., Chong, C. and Lim, W. (2016). Medication adherence 1 month after hospital
discharge in medical inpatients. Internal Medicine Journal, 46(2), pp.185-192.
Nate, L. (2018). Healthcare Cybersecurity: Tips for Securing Private Health Data. [online]
Digital Guardian. Available at: https://digitalguardian.com/blog/healthcare-cybersecurity-
tips-securing-private-health-data [Accessed 24 May 2019].
PillPack, P. (2019). Are you human, bot or alien? | mobile9. [online] Gallery.mobile9.com.
Available at: https://gallery.mobile9.com/asf/ixfawldg9sam/pillpack-medication-reminders/
[Accessed 24 May 2019].
Quinn, M., Forman, J., Harrod, M., Winter, S., Fowler, K., Krein, S., Gupta, A., Saint, S.,
Singh, H. and Chopra, V. (2018). Electronic health records, communication, and data
sharing: challenges and opportunities for improving the diagnostic process. Diagnosis, 0(0).
Ross, S. (2018). 5 Ways to Improve Patient Data Security. [online] The Doctor Weighs In.
Available at: https://thedoctorweighsin.com/patient-data-security/ [Accessed 24 May 2019].
Snair, M., Wizemann, T., Eckert, B. and Altevogt, B. (2014). The impacts of the Affordable
Care Act on preparedness resources and programs. Washington (DC): National Academies
Press.
Thorlby, R., Jorgensen, S., Siegel, B. And Ayanian, J. (2011). How Health Care
Organizations Are Using Data on Patients’ Race and Ethnicity to Improve Quality of
Care. Milbank Quarterly, 89(2), pp.226-255.
Yap, A., Thirumoorthy, T. and Kwan, Y. (2015). Systematic review of the barriers affecting
medication adherence in older adults. Geriatrics & Gerontology International, 16(10),
pp.1093-1101.
HEALTH INFORMATICS 12
Appendix: DAS Application Interfaces
Figure 2: Reminder (PillPack, 2019)
Appendix: DAS Application Interfaces
Figure 2: Reminder (PillPack, 2019)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





