NURS2006 Supplementary Assessment: Medication Error Project Report
VerifiedAdded on 2020/06/06
|12
|5338
|55
Report
AI Summary
This report presents a clinical practice improvement project focused on reducing and preventing medication errors by nurses in acute care settings. The project's aim is to analyze medication errors, identify their causes, and implement interventions for improvement. The report highlights the significance of the issue, emphasizing the impact of medication errors on patient safety, healthcare costs, and the healthcare team. Clinical governance is discussed as a crucial framework for improving care quality. Key stakeholders, including healthcare professionals, service users, and leaders, are identified. The cause and effect (fishbone) diagram is selected as the CPI tool to analyze the root causes of medication errors. The report proposes interventions like the Clinical Decision Support System (CDSS) to enhance medication safety and improve patient outcomes. The report emphasizes the importance of staff awareness and responsibility in creating a safer patient environment.

NURS2006 SUPPLEMENTARY ASSESSMENT
Clinical Practice Improvement Project Report
Aim of the project is “To analyse the issue of medication errors, their possible causes and
bring improvement in the practice of medication administration implementing suitable
interventions”.
Background and Evidence that the issue is worth solving:
A medication error is defined as a preventable event that leads to patient harm due to
inappropriate medication which is in the control of heath care professionals or the patient
himself. Administration of medication is a complex process that involves multiple steps
including prescribing, transcribing, dispensing and administering drugs. It is considered to
play an important role in patient safety. Error can occur at any step and may place the
patient’s life at risk. Medication errors are considered to be the most common health
threatening mistakes and considerably affect the patient care. Overwork and systemic issues
may lead to medication errors (Keers and et.al., 2013). Though these may be caused by all the
members of healthcare team, however, medications errors by nurses is more common. This is
because majority of medical orders are executed by the nurses. Also, a considerable portion
of their time is spent by the nurses for administering medications in the hospital. Both
developed and developing countries have high rates of nursing medication errors. In
Australia, there are approximately 230, 000 medication related hospital admissions per year
(Roughead and et.al., 2016). The country incurs an annual cost of AU$1.2 billion due to
medication related hospital admissions.
Deaths as a result of medication errors are not only tragic for the patients and families,
but also for the healthcare staff that is responsible. Medication error is a serious concern as it
leads to adverse outcomes in the form of increased duration of hospitalization, increased
mortality and increased medical expenses (Flynn and et.al. 2012). Medication errors not only
costs the nation in the form of monetary aspects, but these also costs in terms of loss of trust
on healthcare services. This eventually stems patient dissatisfaction and degrades the morale
NURS2006 Supplementary Assessment for Semester Two, 2017. 1
Clinical Practice Improvement Project Report
Aim of the project is “To analyse the issue of medication errors, their possible causes and
bring improvement in the practice of medication administration implementing suitable
interventions”.
Background and Evidence that the issue is worth solving:
A medication error is defined as a preventable event that leads to patient harm due to
inappropriate medication which is in the control of heath care professionals or the patient
himself. Administration of medication is a complex process that involves multiple steps
including prescribing, transcribing, dispensing and administering drugs. It is considered to
play an important role in patient safety. Error can occur at any step and may place the
patient’s life at risk. Medication errors are considered to be the most common health
threatening mistakes and considerably affect the patient care. Overwork and systemic issues
may lead to medication errors (Keers and et.al., 2013). Though these may be caused by all the
members of healthcare team, however, medications errors by nurses is more common. This is
because majority of medical orders are executed by the nurses. Also, a considerable portion
of their time is spent by the nurses for administering medications in the hospital. Both
developed and developing countries have high rates of nursing medication errors. In
Australia, there are approximately 230, 000 medication related hospital admissions per year
(Roughead and et.al., 2016). The country incurs an annual cost of AU$1.2 billion due to
medication related hospital admissions.
Deaths as a result of medication errors are not only tragic for the patients and families,
but also for the healthcare staff that is responsible. Medication error is a serious concern as it
leads to adverse outcomes in the form of increased duration of hospitalization, increased
mortality and increased medical expenses (Flynn and et.al. 2012). Medication errors not only
costs the nation in the form of monetary aspects, but these also costs in terms of loss of trust
on healthcare services. This eventually stems patient dissatisfaction and degrades the morale
NURS2006 Supplementary Assessment for Semester Two, 2017. 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

of nurses as well as other healthcare staff.
There are different types of medication errors that can occurs in a care setting. These
include prescription of an incorrect dosage of a medicine, incorrect documentation of the
medication history of a person at the time of admission, administration of wrong medicine,
omission of a therapy when it was needed, administration of medicine even when the person
has a history of allergy, administration of a medicine which interacts with other medicines
etc. (Sarvadikar, Prescott and Williams, 2010) According to NSW public hospital system,
there has been an increase in the number of medication errors which resulted in patient’s
death (Alexander, 2016). In the year 2013- 14, out of 53 sentinel events, 12 were related to
death of a patient due to administration of wrong drugs. Acute care settings encompass a
range of clinical health care functions that provide short term treatment to a patient for severe
injury or for a medical condition that requires urgent attention. Medication errors by nurses in
acute care settings imply delayed patient complications and hospital stays which could have
been prevented.
The study conducted by Lopez and et.al. (2012) studied various interventions for
reducing medication errors in hospitalized adults. The study described medication error by
nurse as an adverse event and highlighted the burden of medication errors and adverse events
as serious concern for healthcare services.
Thus above evidence indicates that the issue of medication errors by nurses in acute care
settings requires attention and is worth solving.
Relevance of Clinical Governance to your project
Clinical governance refers to a system which makes the health care organizations
accountable for safeguarding high standards of care and bringing improvements in the quality
of their services (Wilson and Harrison, 2002). This also includes creation of an environment
which is characterized by promotion of excellence in clinical care. Considering the present
project on Clinical practice improvement regarding the issue of medication errors by nurses,
clinical governance is extremely relevant. This is because it covers those activities that hep
the healthcare organizations sustain as well as improve high standards of patient care. High
standards of care imply that the health care staff have a duty to maintain quality and safety of
NURS2006 Supplementary Assessment for Semester Two, 2017. 2
There are different types of medication errors that can occurs in a care setting. These
include prescription of an incorrect dosage of a medicine, incorrect documentation of the
medication history of a person at the time of admission, administration of wrong medicine,
omission of a therapy when it was needed, administration of medicine even when the person
has a history of allergy, administration of a medicine which interacts with other medicines
etc. (Sarvadikar, Prescott and Williams, 2010) According to NSW public hospital system,
there has been an increase in the number of medication errors which resulted in patient’s
death (Alexander, 2016). In the year 2013- 14, out of 53 sentinel events, 12 were related to
death of a patient due to administration of wrong drugs. Acute care settings encompass a
range of clinical health care functions that provide short term treatment to a patient for severe
injury or for a medical condition that requires urgent attention. Medication errors by nurses in
acute care settings imply delayed patient complications and hospital stays which could have
been prevented.
The study conducted by Lopez and et.al. (2012) studied various interventions for
reducing medication errors in hospitalized adults. The study described medication error by
nurse as an adverse event and highlighted the burden of medication errors and adverse events
as serious concern for healthcare services.
Thus above evidence indicates that the issue of medication errors by nurses in acute care
settings requires attention and is worth solving.
Relevance of Clinical Governance to your project
Clinical governance refers to a system which makes the health care organizations
accountable for safeguarding high standards of care and bringing improvements in the quality
of their services (Wilson and Harrison, 2002). This also includes creation of an environment
which is characterized by promotion of excellence in clinical care. Considering the present
project on Clinical practice improvement regarding the issue of medication errors by nurses,
clinical governance is extremely relevant. This is because it covers those activities that hep
the healthcare organizations sustain as well as improve high standards of patient care. High
standards of care imply that the health care staff have a duty to maintain quality and safety of
NURS2006 Supplementary Assessment for Semester Two, 2017. 2
care. This eventually includes the aspects related to medication safety.
Clinical governance comprises of the following seven pillars:
Risk management
Staffing and staff management
Service users, carers and public involvement
Clinical audit,
Education and training
Clinical information
Clinical effectiveness
The above-mentioned pillars of clinical governance are closely related to fostering quality
and safety within the healthcare organizations (Clinical Governance, 2017). These also
enhance the relevance of clinical governance to the current project of clinical practice
improvement. The present project aims at bringing improvement in the practice of medication
administration by nurses within acute care settings to reduce and prevent the issue of
medication errors. This can be well achieved with clinical governance and its seven pillars.
This is because these not only involve the healthcare staff aspects but also focus on
involvement of service users and public (Treiber and Jones, 2010). Hence, the issue of
medication errors can be analysed from different perspectives with the help of clinical
governance. In addition to this, clinical governance also involves clinical information, clinical
effectiveness and clinical audit which would help in reducing the issue of medication errors.
Furthermore, clinical governance pillars related to education and training and risk
management provide a platform through which steps can be taken to ensure prevention of
medication errors. Hence, clinical governance has significant relevance to this project.
Key Stakeholders:
The present clinical practice improvement project regarding the issue of medication error will
comprise of the following stakeholders:
Health care professionals: These form an important group of stakeholders who can
be associated with the CPI project. They can be involved in the project by assigning
NURS2006 Supplementary Assessment for Semester Two, 2017. 3
Clinical governance comprises of the following seven pillars:
Risk management
Staffing and staff management
Service users, carers and public involvement
Clinical audit,
Education and training
Clinical information
Clinical effectiveness
The above-mentioned pillars of clinical governance are closely related to fostering quality
and safety within the healthcare organizations (Clinical Governance, 2017). These also
enhance the relevance of clinical governance to the current project of clinical practice
improvement. The present project aims at bringing improvement in the practice of medication
administration by nurses within acute care settings to reduce and prevent the issue of
medication errors. This can be well achieved with clinical governance and its seven pillars.
This is because these not only involve the healthcare staff aspects but also focus on
involvement of service users and public (Treiber and Jones, 2010). Hence, the issue of
medication errors can be analysed from different perspectives with the help of clinical
governance. In addition to this, clinical governance also involves clinical information, clinical
effectiveness and clinical audit which would help in reducing the issue of medication errors.
Furthermore, clinical governance pillars related to education and training and risk
management provide a platform through which steps can be taken to ensure prevention of
medication errors. Hence, clinical governance has significant relevance to this project.
Key Stakeholders:
The present clinical practice improvement project regarding the issue of medication error will
comprise of the following stakeholders:
Health care professionals: These form an important group of stakeholders who can
be associated with the CPI project. They can be involved in the project by assigning
NURS2006 Supplementary Assessment for Semester Two, 2017. 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

them the responsibility of risk assessment to be conducted within the acute care
setting. Managerial roles can also be assigned to the health care professionals who can
assess potential areas of risk related to medication error. As the health care
professional are closely related to patient as well as the nurses and other staff, they are
aware about the aspects that need to be taken care of while bringing practice
improvement for reducing medication errors by nurses (Choo, Hutchinson and
Bucknall, 2010). Hence, an important role will be played by them in the project.
Service users and families: These are another group of stakeholders for the project.
They can be involved by obtaining feedback from them regarding the quality of care
being delivered at the care setting. Their opinions will provide information regarding
loopholes in care which may be corrected to reduce and prevent medication errors.
Healthcare leaders: These will play an important role in the project by using clear
communication techniques which will allow free flow of discussions to all levels of
the organizations (Bayazidi and et.al., 2012). Hence, leaders will play a significant
role in bringing the change within the acute care settings.
External healthcare stakeholders: These include the accrediting, regulatory and
licensing bodies which will provide insights to the various healthcare organization to
make sure that the relevant safety standards are being followed by them.
CPI Tool:
There are various interventions for improving medication safety in acute care settings.
For the present CPI project, the tool of cause and effect diagrams will be used for reducing
and preventing medication error by nurses in acute care settings. Cause and effect diagrams
are also known as fish bone diagram. These help in visually analysing a problem or the root
causes of a condition. With the help of these diagrams, the team member are able to separate
the content of a problem from its history (Wilson and Harrison, 2002). The tool comprises of
stating the problem, categorization of the process, brainstorming about the contributing
factors, analysing deeper causes and testing for root causes.
Fish bone analysis is a tool that helps in identifying all the possible causes for a
problem. It thus, seeks to determine the root cause of the problem from a systemic
perspective (Gold and et.al., 2014). Use of this tool will involve a group of staff, who are the
NURS2006 Supplementary Assessment for Semester Two, 2017. 4
setting. Managerial roles can also be assigned to the health care professionals who can
assess potential areas of risk related to medication error. As the health care
professional are closely related to patient as well as the nurses and other staff, they are
aware about the aspects that need to be taken care of while bringing practice
improvement for reducing medication errors by nurses (Choo, Hutchinson and
Bucknall, 2010). Hence, an important role will be played by them in the project.
Service users and families: These are another group of stakeholders for the project.
They can be involved by obtaining feedback from them regarding the quality of care
being delivered at the care setting. Their opinions will provide information regarding
loopholes in care which may be corrected to reduce and prevent medication errors.
Healthcare leaders: These will play an important role in the project by using clear
communication techniques which will allow free flow of discussions to all levels of
the organizations (Bayazidi and et.al., 2012). Hence, leaders will play a significant
role in bringing the change within the acute care settings.
External healthcare stakeholders: These include the accrediting, regulatory and
licensing bodies which will provide insights to the various healthcare organization to
make sure that the relevant safety standards are being followed by them.
CPI Tool:
There are various interventions for improving medication safety in acute care settings.
For the present CPI project, the tool of cause and effect diagrams will be used for reducing
and preventing medication error by nurses in acute care settings. Cause and effect diagrams
are also known as fish bone diagram. These help in visually analysing a problem or the root
causes of a condition. With the help of these diagrams, the team member are able to separate
the content of a problem from its history (Wilson and Harrison, 2002). The tool comprises of
stating the problem, categorization of the process, brainstorming about the contributing
factors, analysing deeper causes and testing for root causes.
Fish bone analysis is a tool that helps in identifying all the possible causes for a
problem. It thus, seeks to determine the root cause of the problem from a systemic
perspective (Gold and et.al., 2014). Use of this tool will involve a group of staff, who are the
NURS2006 Supplementary Assessment for Semester Two, 2017. 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
key stakeholders in the project, to work together and evoke the possible causes behind the
issue. Following this the main causes will be further explored to identify sub- causes of the
issue. In this way, Root causes to the problem will be identified on the basis of which a
striong actuion plan could be prepared.
Addressing the aim with CPI tool
The present project is a clinical practice improvement project and aims to reduce and
prevent medication errors by nurses working in acute care settings. Fish bone diagrams will
allow in- depth analysis of the issue of medication errors by nurses. This tool will provide
insights to all the people associated with the issues. Hence, it will allow for the development
of a collaborative solution. Moreover, use of this tool will help in minimizing the adverse
events related to medication errors as it will provide retrospective views of incident. The
cause and effect diagrams will also help in developing the awareness of the staff regarding
their responsibility and professional duty. This will lead towards a safer patient environment.
With the help of Fish bone diagram, this project will get a template for separating and
categorizing possible causes of a problem. Thus the health care team addressing the issue of
medication errors in acute care settings will be able to focus on the content of problem. They
will be able to analyse the root cause of the issue which will not only helps in reducing
medication errors but also preventing them.
The tool of fishbone diagram will also help in implementing the various interventions
for reducing and preventing medication errors. This is because, as it will make the healthcare
staff realize their duty and responsibility, it will enable them to understand the need for the
implementation of intervention.
Summary of proposed intervention:
NURS2006 Supplementary Assessment for Semester Two, 2017. 5
issue. Following this the main causes will be further explored to identify sub- causes of the
issue. In this way, Root causes to the problem will be identified on the basis of which a
striong actuion plan could be prepared.
Addressing the aim with CPI tool
The present project is a clinical practice improvement project and aims to reduce and
prevent medication errors by nurses working in acute care settings. Fish bone diagrams will
allow in- depth analysis of the issue of medication errors by nurses. This tool will provide
insights to all the people associated with the issues. Hence, it will allow for the development
of a collaborative solution. Moreover, use of this tool will help in minimizing the adverse
events related to medication errors as it will provide retrospective views of incident. The
cause and effect diagrams will also help in developing the awareness of the staff regarding
their responsibility and professional duty. This will lead towards a safer patient environment.
With the help of Fish bone diagram, this project will get a template for separating and
categorizing possible causes of a problem. Thus the health care team addressing the issue of
medication errors in acute care settings will be able to focus on the content of problem. They
will be able to analyse the root cause of the issue which will not only helps in reducing
medication errors but also preventing them.
The tool of fishbone diagram will also help in implementing the various interventions
for reducing and preventing medication errors. This is because, as it will make the healthcare
staff realize their duty and responsibility, it will enable them to understand the need for the
implementation of intervention.
Summary of proposed intervention:
NURS2006 Supplementary Assessment for Semester Two, 2017. 5
Proposed interventions
Clinical Decision Support System (CDSS)
Clinical Decision Support System is a system of health information technology which
helps physicians and other health professionals by providing them clinical decision support
(Lopez and et.al., 2012). It therefore assists them with clinical decision making. These
systems perform the work of forming links between health observations and health
knowledge which has influence on health choices made by clinicians. CDSS are active
knowledge systems which make use of more than two items of patient data for generating
advice. It thus uses knowledge management is a manner that relevant clinical advice is
received for delivering care to the patient. The study by Lopez and et.al. (2012) also
mentioned CDSS as an intervention that can be used for reducing medication errors.
CDSS will serve as an effective intervention in reducing and preventing medication errors
by nurses in acute care settings. These improve the process of care and have the potential to
consistently improve the patient outcomes (Musen, Middleton and Greenes, 2014). CDS
provides medication alerts and reminders which will positively impact the process of care.
The following features of CDSS will be useful in achieving the aim of reducing and
preventing medication errors by nurses:
Drug allergy checking: This is an important medication safety feature of CDSS
which will present a reminder the moment when the medication that is ordered by the
provider has a risk of developing documented allergy in the patient (Bright and et.al.,
2012). This will thus alert the nurses and prevent potential patient harm.
Basic dosing guidance: CDSS has multiple mechanisms which provides support to
improve medication dosing. This will help in reducing variability in initial dosing thus
preventing patient harm.
Formulary decision support: CDSS also provides guidance to the health care
professionals and nurses regarding formulary options. Formularies are known be
clinically effective and safe drug therapy (Musen, Middleton and Greenes, 2014).
Education and training
This is another intervention for reducing and preventing medication errors by nurses.
NURS2006 Supplementary Assessment for Semester Two, 2017. 6
Clinical Decision Support System (CDSS)
Clinical Decision Support System is a system of health information technology which
helps physicians and other health professionals by providing them clinical decision support
(Lopez and et.al., 2012). It therefore assists them with clinical decision making. These
systems perform the work of forming links between health observations and health
knowledge which has influence on health choices made by clinicians. CDSS are active
knowledge systems which make use of more than two items of patient data for generating
advice. It thus uses knowledge management is a manner that relevant clinical advice is
received for delivering care to the patient. The study by Lopez and et.al. (2012) also
mentioned CDSS as an intervention that can be used for reducing medication errors.
CDSS will serve as an effective intervention in reducing and preventing medication errors
by nurses in acute care settings. These improve the process of care and have the potential to
consistently improve the patient outcomes (Musen, Middleton and Greenes, 2014). CDS
provides medication alerts and reminders which will positively impact the process of care.
The following features of CDSS will be useful in achieving the aim of reducing and
preventing medication errors by nurses:
Drug allergy checking: This is an important medication safety feature of CDSS
which will present a reminder the moment when the medication that is ordered by the
provider has a risk of developing documented allergy in the patient (Bright and et.al.,
2012). This will thus alert the nurses and prevent potential patient harm.
Basic dosing guidance: CDSS has multiple mechanisms which provides support to
improve medication dosing. This will help in reducing variability in initial dosing thus
preventing patient harm.
Formulary decision support: CDSS also provides guidance to the health care
professionals and nurses regarding formulary options. Formularies are known be
clinically effective and safe drug therapy (Musen, Middleton and Greenes, 2014).
Education and training
This is another intervention for reducing and preventing medication errors by nurses.
NURS2006 Supplementary Assessment for Semester Two, 2017. 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The errors are caused by nurses even when the appropriate doses have been prescribed by the
doctors. Medications are either not administered on time or are completely omitted. This
indicates towards the loophole that exists around the practice environment and may be
associated with other factors. According to Lopez and et.al. (2012), education and training is
among one of the interventions which can be used for reducing medication errors in
healthcare settings. From this it can be analysed that this intervention can be used for the
present CPI project. The intervention will cover a holistic plan for guiding and educating the
nurses on the protocols to be followed during administration of medication. It will basically
focus on developing a culture of patient safety by inculcating values in nurses regarding
importance of patient safety in the form of safe administration of drugs. The training will
focus on teaching the nurses about the possible errors that are generally caused while
administering medications so that these can be prevented in future.
Project outline
The present project is a clinical practice improvement project to reduce and prevent
medication errors by nurses. The purpose of the project is to analyse the issue of medication
errors, their possible causes and bring improvement in the practice of medication
administration by implementation of suitable interventions. The project aims at practice
improvement so that patient safety culture is enhanced.
Relevance to clinical practice
The project is relevant to clinical practice as it will lead to adoption of a better and
safe practice of administering medication to patients so that medication errors could be
reduced. Administering medications is one of the most important and critical duties of nurses
(Roughead and et.al., 2016). This is because, errors during this phase may result in serious
consequences for the patient. There has been a growing reliance on medication therapy which
places the patients receiving medication at risk if a medication error occurs. Hence, the
intervention if relevant to the clinical practice as nurses may not be authorized to implement
structural changes, but they can be trained and educated to take precautions for preventing
medication errors.
Barriers to implementation:
NURS2006 Supplementary Assessment for Semester Two, 2017. 7
doctors. Medications are either not administered on time or are completely omitted. This
indicates towards the loophole that exists around the practice environment and may be
associated with other factors. According to Lopez and et.al. (2012), education and training is
among one of the interventions which can be used for reducing medication errors in
healthcare settings. From this it can be analysed that this intervention can be used for the
present CPI project. The intervention will cover a holistic plan for guiding and educating the
nurses on the protocols to be followed during administration of medication. It will basically
focus on developing a culture of patient safety by inculcating values in nurses regarding
importance of patient safety in the form of safe administration of drugs. The training will
focus on teaching the nurses about the possible errors that are generally caused while
administering medications so that these can be prevented in future.
Project outline
The present project is a clinical practice improvement project to reduce and prevent
medication errors by nurses. The purpose of the project is to analyse the issue of medication
errors, their possible causes and bring improvement in the practice of medication
administration by implementation of suitable interventions. The project aims at practice
improvement so that patient safety culture is enhanced.
Relevance to clinical practice
The project is relevant to clinical practice as it will lead to adoption of a better and
safe practice of administering medication to patients so that medication errors could be
reduced. Administering medications is one of the most important and critical duties of nurses
(Roughead and et.al., 2016). This is because, errors during this phase may result in serious
consequences for the patient. There has been a growing reliance on medication therapy which
places the patients receiving medication at risk if a medication error occurs. Hence, the
intervention if relevant to the clinical practice as nurses may not be authorized to implement
structural changes, but they can be trained and educated to take precautions for preventing
medication errors.
Barriers to implementation:
NURS2006 Supplementary Assessment for Semester Two, 2017. 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The implementation of the proposed intervention may face several barriers as discussed
below:
Concerns regarding negative consequences: Though a clear and compelling
mechanism is provided by the IT systems for reduction of medication errors but their
potential negative consequences raise concerns which act as barriers in
implementation (Bright and et.al., 2012). These concerns are associated with the staff
who will be required to perform new work due to CDSS. This can further lead to
workflow issues as well as generation of new errors. However, the problem can be
overcome by redefining the roles and responsibilities of clinicians and nurses. This
will help in managing the new work generated by CDSS along with eliminating the
possibility of generation of new errors.
Incorporation into clinical processes: To prevent medication errors, it is important
that CDSS is incorporated into the clinical processes and workflow. This corresponds
to the socio- technical environment of the clinical workplace. However, the issue can
be overcome by re-designing the work processes. Further, training can be imparted to
the healthcare professionals so that functionality of the system is maintained and it is
incorporated into the workflow.
Nurses’ knowledge: Effective implementation of CDS needs to consider the factor of
staff’ knowledge regarding it (Greenes, 2011). Lack of knowledge will likely make it
difficult to implement the proposed intervention. This barrier can be overcome with
the help of training sessions to work with a CDSS.
Nurses’ attitude: This is an important factor which may act as a barrier to
implementation of the interventions. Implementing CDSS and education and training
will require the staff to devote extra time and energy towards them. They will have
extra work due to CDSS initially which could later be adjusted and balanced. Also,
education and training will require their additional time. As the nurses already have a
number of responsibilities and duties, they may not have positive attitude towards
adoption of these interventions. Lack of positive attitude of the nurses will act as a
barrier to effective implementation of the proposed interventions (Sanghera, Franklin
and Dhillon, 2007). This barrier can be overcome by appropriate change management
NURS2006 Supplementary Assessment for Semester Two, 2017. 8
below:
Concerns regarding negative consequences: Though a clear and compelling
mechanism is provided by the IT systems for reduction of medication errors but their
potential negative consequences raise concerns which act as barriers in
implementation (Bright and et.al., 2012). These concerns are associated with the staff
who will be required to perform new work due to CDSS. This can further lead to
workflow issues as well as generation of new errors. However, the problem can be
overcome by redefining the roles and responsibilities of clinicians and nurses. This
will help in managing the new work generated by CDSS along with eliminating the
possibility of generation of new errors.
Incorporation into clinical processes: To prevent medication errors, it is important
that CDSS is incorporated into the clinical processes and workflow. This corresponds
to the socio- technical environment of the clinical workplace. However, the issue can
be overcome by re-designing the work processes. Further, training can be imparted to
the healthcare professionals so that functionality of the system is maintained and it is
incorporated into the workflow.
Nurses’ knowledge: Effective implementation of CDS needs to consider the factor of
staff’ knowledge regarding it (Greenes, 2011). Lack of knowledge will likely make it
difficult to implement the proposed intervention. This barrier can be overcome with
the help of training sessions to work with a CDSS.
Nurses’ attitude: This is an important factor which may act as a barrier to
implementation of the interventions. Implementing CDSS and education and training
will require the staff to devote extra time and energy towards them. They will have
extra work due to CDSS initially which could later be adjusted and balanced. Also,
education and training will require their additional time. As the nurses already have a
number of responsibilities and duties, they may not have positive attitude towards
adoption of these interventions. Lack of positive attitude of the nurses will act as a
barrier to effective implementation of the proposed interventions (Sanghera, Franklin
and Dhillon, 2007). This barrier can be overcome by appropriate change management
NURS2006 Supplementary Assessment for Semester Two, 2017. 8
principles and practices. Raising the awareness of nurses towards the issue of
medication error and its consequences will also help in dealing with the barrier of
negative attitude. This is because it will help in changing their perception
Lack of resources: Both implementation of CDSS as well as education and training
programs will requires resources in the form of time and money (Musen, Middleton
and Greenes, 2014). It is important to note that all the acute care settings may not
have the financial resources available for implementing a CDSS or an education and
training program. Also, there may be lack of resources in the form of time. This factor
will act as a barrier to implementation. The barrier can be minimized by government
funding to the acute care settings that lack the required resources. Also, government
aided training programs can be organized.
Clinical outcomes: The impact of CDSS on clinical outcomes is still not clear which
raises a question on its implementation acceptance by the staff. The barrier can be
minimized by testing and evaluating the proposed interventions.
Resistance from staff: The implementation of proposed interventions may face the
barrier in the form of resistance form the staff. Adoption of CDS system and
education and training would require redefining the roles and redesigning the work
processes in order to incorporate the system into the workflow. This change may face
resistance from the staff as they may have become comfortable in particular roles and
may find it difficult to adjust to new roles, responsibilities and job processes.
Therefore, they may resist to its implementation. However, the barrier can be
overcome by utilizing appropriate change management processes. Change
management agent can be employed for assimilating the change within the acute care
settings.
Evaluation of the project:
The present CPI project is about bringing improvement in the clinical practice by
reducing and preventing medication errors by nurses in acute care setting. It intends to use the
proposed interventions of implementation of CDSS and education and training programs for
the issue of medication errors by nurses. The project will involve the use of fish bone
diagram as the clinical practice improvement tool. This will assist in analysing the root
NURS2006 Supplementary Assessment for Semester Two, 2017. 9
medication error and its consequences will also help in dealing with the barrier of
negative attitude. This is because it will help in changing their perception
Lack of resources: Both implementation of CDSS as well as education and training
programs will requires resources in the form of time and money (Musen, Middleton
and Greenes, 2014). It is important to note that all the acute care settings may not
have the financial resources available for implementing a CDSS or an education and
training program. Also, there may be lack of resources in the form of time. This factor
will act as a barrier to implementation. The barrier can be minimized by government
funding to the acute care settings that lack the required resources. Also, government
aided training programs can be organized.
Clinical outcomes: The impact of CDSS on clinical outcomes is still not clear which
raises a question on its implementation acceptance by the staff. The barrier can be
minimized by testing and evaluating the proposed interventions.
Resistance from staff: The implementation of proposed interventions may face the
barrier in the form of resistance form the staff. Adoption of CDS system and
education and training would require redefining the roles and redesigning the work
processes in order to incorporate the system into the workflow. This change may face
resistance from the staff as they may have become comfortable in particular roles and
may find it difficult to adjust to new roles, responsibilities and job processes.
Therefore, they may resist to its implementation. However, the barrier can be
overcome by utilizing appropriate change management processes. Change
management agent can be employed for assimilating the change within the acute care
settings.
Evaluation of the project:
The present CPI project is about bringing improvement in the clinical practice by
reducing and preventing medication errors by nurses in acute care setting. It intends to use the
proposed interventions of implementation of CDSS and education and training programs for
the issue of medication errors by nurses. The project will involve the use of fish bone
diagram as the clinical practice improvement tool. This will assist in analysing the root
NURS2006 Supplementary Assessment for Semester Two, 2017. 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
causes of the issue of medication error and draw a concrete action plan based on it. The
project can be evaluated by obtaining feedback from the management of the acute care
setting. The feedback will help in gaining information about the extent to which the
medication administration is abiding by the prescribed standards. Further, organizational
records can be used for identifying if there have been any incidents of medication errors.
Feedback can also be obtained from the service users. These methods will help in evaluating
the project from different perspectives.
REFERENCES
Journal and books
Bayazidi, S. and et.al., 2012. Medication error reporting rate and its barriers and facilitators
among nurses. Journal of caring sciences. 1(4). p.231.
Bright, T.J. and et.al., 2012. Effect of clinical decision-support systemsa systematic
review. Annals of internal medicine, 157(1), pp.29-43.
Choo, J., Hutchinson, A. and Bucknall, T., 2010. Nurses' role in medication safety. Journal of
nursing management. 18(7). pp.853-861.
Flynn, L. and et.al. 2012. Nurses’ practice environments, error interception practices, and
inpatient medication errors. Journal of Nursing Scholarship. 44(2). pp.180-186.
Gold, J. and et.al., 2014. A quality improvement study using fishbone analysis and an electronic
medical records intervention to improve care for children with asthma. American Journal
of Medical Quality. 29(1). pp.70-77.
Greenes, R.A. ed., 2011. Clinical decision support: the road ahead. Academic Press.
Keers, R. N. and et.al., 2013. Causes of medication administration errors in hospitals: a
systematic review of quantitative and qualitative evidence. Drug Safety. 36(11). pp.1-45-
1067.
Lopez, AS and et.al., 2012. Interventions for reducing medication errors in hospitalised adults
(Intervention Protocol) The Cochrane Collaboration. The Cochrane Library. 7.
Musen, M.A., Middleton, B. and Greenes, R.A., 2014. Clinical decision-support systems.
In Biomedical informatics (pp. 643-674). Springer London.
Roughead, E. E. and et.al., 2016. The extent of medication errors and adverse drug reactions
throughout the patient journey in acute care in Australia. International Journal of
Evidence-Based Healthcare. 14(3). pp.113-122.
Sanghera, I. S., Franklin, B. D. and Dhillon, S. 2007. The attitudes and beliefs of healthcare
professionals on the causes and reporting of medication errors in a UK Intensive care unit.
Anaesthesia. 62(1). pp.53-61.
NURS2006 Supplementary Assessment for Semester Two, 2017. 10
project can be evaluated by obtaining feedback from the management of the acute care
setting. The feedback will help in gaining information about the extent to which the
medication administration is abiding by the prescribed standards. Further, organizational
records can be used for identifying if there have been any incidents of medication errors.
Feedback can also be obtained from the service users. These methods will help in evaluating
the project from different perspectives.
REFERENCES
Journal and books
Bayazidi, S. and et.al., 2012. Medication error reporting rate and its barriers and facilitators
among nurses. Journal of caring sciences. 1(4). p.231.
Bright, T.J. and et.al., 2012. Effect of clinical decision-support systemsa systematic
review. Annals of internal medicine, 157(1), pp.29-43.
Choo, J., Hutchinson, A. and Bucknall, T., 2010. Nurses' role in medication safety. Journal of
nursing management. 18(7). pp.853-861.
Flynn, L. and et.al. 2012. Nurses’ practice environments, error interception practices, and
inpatient medication errors. Journal of Nursing Scholarship. 44(2). pp.180-186.
Gold, J. and et.al., 2014. A quality improvement study using fishbone analysis and an electronic
medical records intervention to improve care for children with asthma. American Journal
of Medical Quality. 29(1). pp.70-77.
Greenes, R.A. ed., 2011. Clinical decision support: the road ahead. Academic Press.
Keers, R. N. and et.al., 2013. Causes of medication administration errors in hospitals: a
systematic review of quantitative and qualitative evidence. Drug Safety. 36(11). pp.1-45-
1067.
Lopez, AS and et.al., 2012. Interventions for reducing medication errors in hospitalised adults
(Intervention Protocol) The Cochrane Collaboration. The Cochrane Library. 7.
Musen, M.A., Middleton, B. and Greenes, R.A., 2014. Clinical decision-support systems.
In Biomedical informatics (pp. 643-674). Springer London.
Roughead, E. E. and et.al., 2016. The extent of medication errors and adverse drug reactions
throughout the patient journey in acute care in Australia. International Journal of
Evidence-Based Healthcare. 14(3). pp.113-122.
Sanghera, I. S., Franklin, B. D. and Dhillon, S. 2007. The attitudes and beliefs of healthcare
professionals on the causes and reporting of medication errors in a UK Intensive care unit.
Anaesthesia. 62(1). pp.53-61.
NURS2006 Supplementary Assessment for Semester Two, 2017. 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Sarvadikar, A., Prescott, G. and Williams, D., 2010. Attitudes to reporting medication error
among differing healthcare professionals. European journal of clinical
pharmacology. 66(8). pp.843-853.
Treiber, L. A. and Jones, J. H., 2010. Devastatingly human: an analysis of registered nurses’
medication error accounts. Qualitative Health Research. 20(10). pp.1327-1342.
Wilson, R. M. and Harrison, B. T., 2002. What is clinical practice improvement?. Internal
Medicine Journal. 32(9/10). pp. 460-464.
Online
Alexander, H., 2016. NSW public hospitals record rise in medication errors, surgical errors,
inpatient suicides. [Online]. Available through:
<http://www.smh.com.au/national/health/nsw-public-hospitals-record-rise-in-medication-
errors-surgical-errors-inpatient-suicides-20160203-gmksyi.html>
Clinical Governance. 2017. [Online]. Available through:
<https://www.cumbriapartnership.nhs.uk/health-professionals/clinical-governance>
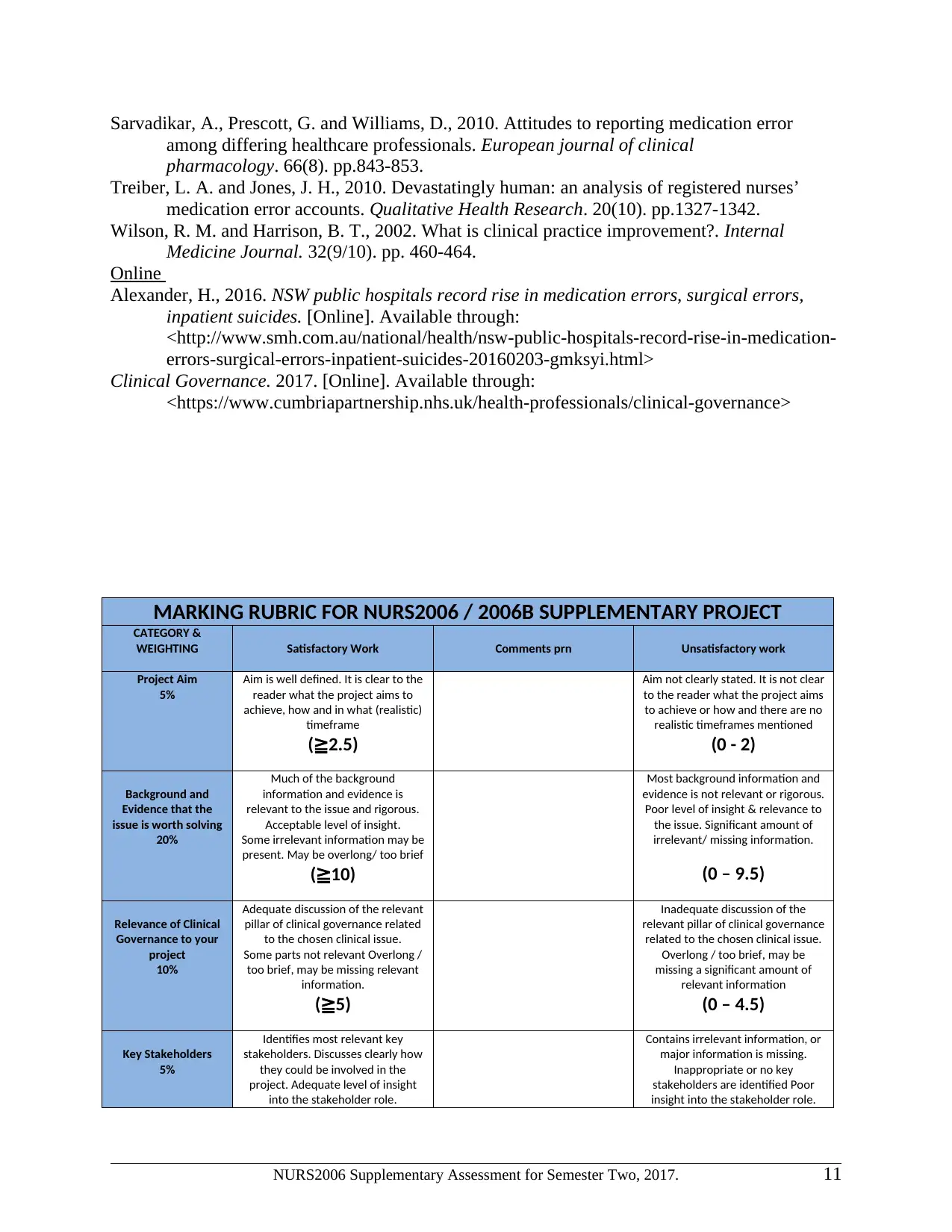
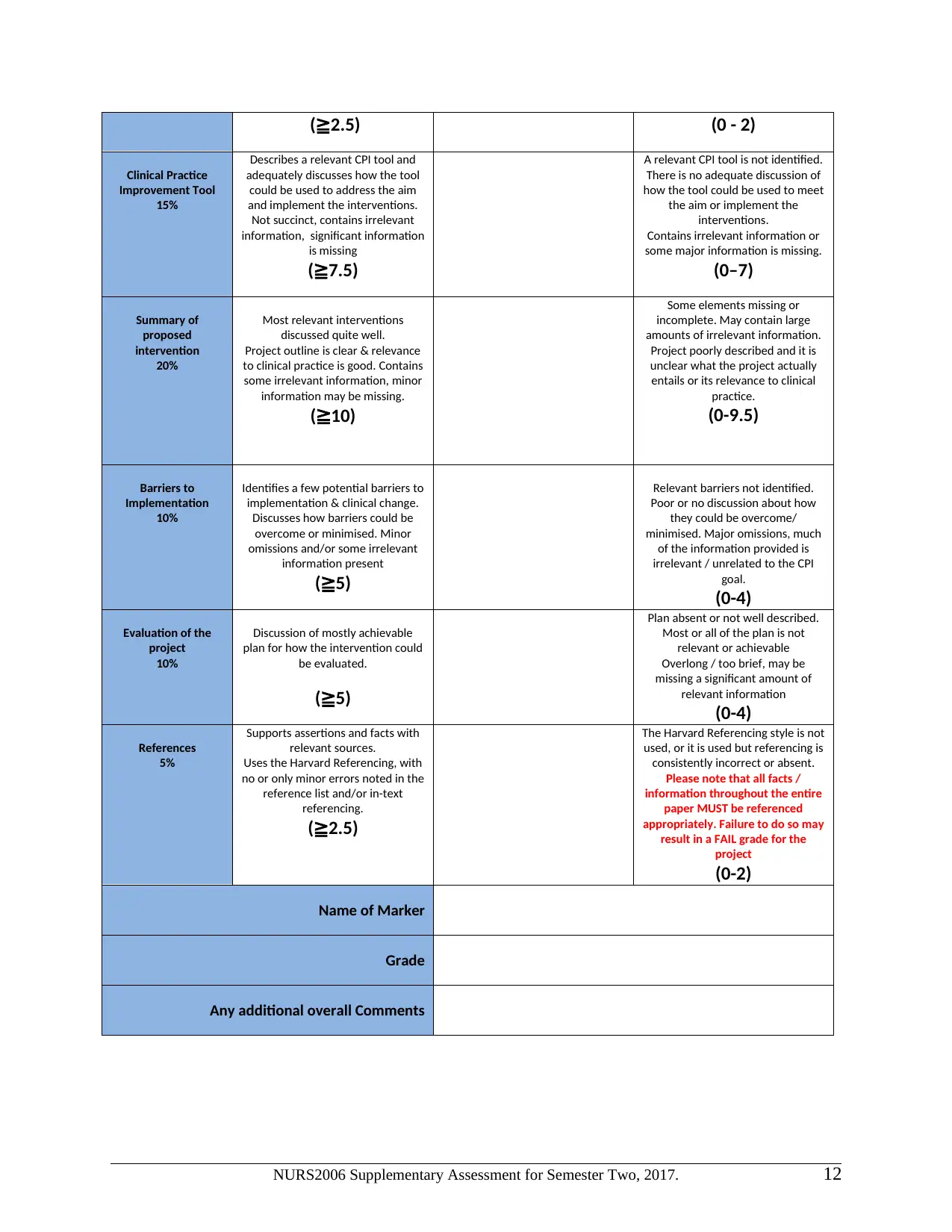
MARKING RUBRIC FOR NURS2006 / 2006B SUPPLEMENTARY PROJECT
CATEGORY &
WEIGHTING Satisfactory Work Comments prn Unsatisfactory work
Project Aim
5%
Aim is well defined. It is clear to the
reader what the project aims to
achieve, how and in what (realistic)
timeframe
(≧2.5)
Aim not clearly stated. It is not clear
to the reader what the project aims
to achieve or how and there are no
realistic timeframes mentioned
(0 - 2)
Background and
Evidence that the
issue is worth solving
20%
Much of the background
information and evidence is
relevant to the issue and rigorous.
Acceptable level of insight.
Some irrelevant information may be
present. May be overlong/ too brief
(≧10)
Most background information and
evidence is not relevant or rigorous.
Poor level of insight & relevance to
the issue. Significant amount of
irrelevant/ missing information.
(0 – 9.5)
Relevance of Clinical
Governance to your
project
10%
Adequate discussion of the relevant
pillar of clinical governance related
to the chosen clinical issue.
Some parts not relevant Overlong /
too brief, may be missing relevant
information.
(≧5)
Inadequate discussion of the
relevant pillar of clinical governance
related to the chosen clinical issue.
Overlong / too brief, may be
missing a significant amount of
relevant information
(0 – 4.5)
Key Stakeholders
5%
Identifies most relevant key
stakeholders. Discusses clearly how
they could be involved in the
project. Adequate level of insight
into the stakeholder role.
Contains irrelevant information, or
major information is missing.
Inappropriate or no key
stakeholders are identified Poor
insight into the stakeholder role.
NURS2006 Supplementary Assessment for Semester Two, 2017. 11
among differing healthcare professionals. European journal of clinical
pharmacology. 66(8). pp.843-853.
Treiber, L. A. and Jones, J. H., 2010. Devastatingly human: an analysis of registered nurses’
medication error accounts. Qualitative Health Research. 20(10). pp.1327-1342.
Wilson, R. M. and Harrison, B. T., 2002. What is clinical practice improvement?. Internal
Medicine Journal. 32(9/10). pp. 460-464.
Online
Alexander, H., 2016. NSW public hospitals record rise in medication errors, surgical errors,
inpatient suicides. [Online]. Available through:
<http://www.smh.com.au/national/health/nsw-public-hospitals-record-rise-in-medication-
errors-surgical-errors-inpatient-suicides-20160203-gmksyi.html>
Clinical Governance. 2017. [Online]. Available through:
<https://www.cumbriapartnership.nhs.uk/health-professionals/clinical-governance>
MARKING RUBRIC FOR NURS2006 / 2006B SUPPLEMENTARY PROJECT
CATEGORY &
WEIGHTING Satisfactory Work Comments prn Unsatisfactory work
Project Aim
5%
Aim is well defined. It is clear to the
reader what the project aims to
achieve, how and in what (realistic)
timeframe
(≧2.5)
Aim not clearly stated. It is not clear
to the reader what the project aims
to achieve or how and there are no
realistic timeframes mentioned
(0 - 2)
Background and
Evidence that the
issue is worth solving
20%
Much of the background
information and evidence is
relevant to the issue and rigorous.
Acceptable level of insight.
Some irrelevant information may be
present. May be overlong/ too brief
(≧10)
Most background information and
evidence is not relevant or rigorous.
Poor level of insight & relevance to
the issue. Significant amount of
irrelevant/ missing information.
(0 – 9.5)
Relevance of Clinical
Governance to your
project
10%
Adequate discussion of the relevant
pillar of clinical governance related
to the chosen clinical issue.
Some parts not relevant Overlong /
too brief, may be missing relevant
information.
(≧5)
Inadequate discussion of the
relevant pillar of clinical governance
related to the chosen clinical issue.
Overlong / too brief, may be
missing a significant amount of
relevant information
(0 – 4.5)
Key Stakeholders
5%
Identifies most relevant key
stakeholders. Discusses clearly how
they could be involved in the
project. Adequate level of insight
into the stakeholder role.
Contains irrelevant information, or
major information is missing.
Inappropriate or no key
stakeholders are identified Poor
insight into the stakeholder role.
NURS2006 Supplementary Assessment for Semester Two, 2017. 11
(≧2.5) (0 - 2)
Clinical Practice
Improvement Tool
15%
Describes a relevant CPI tool and
adequately discusses how the tool
could be used to address the aim
and implement the interventions.
Not succinct, contains irrelevant
information, significant information
is missing
(≧7.5)
A relevant CPI tool is not identified.
There is no adequate discussion of
how the tool could be used to meet
the aim or implement the
interventions.
Contains irrelevant information or
some major information is missing.
(0–7)
Summary of
proposed
intervention
20%
Most relevant interventions
discussed quite well.
Project outline is clear & relevance
to clinical practice is good. Contains
some irrelevant information, minor
information may be missing.
(≧10)
Some elements missing or
incomplete. May contain large
amounts of irrelevant information.
Project poorly described and it is
unclear what the project actually
entails or its relevance to clinical
practice.
(0-9.5)
Barriers to
Implementation
10%
Identifies a few potential barriers to
implementation & clinical change.
Discusses how barriers could be
overcome or minimised. Minor
omissions and/or some irrelevant
information present
(≧5)
Relevant barriers not identified.
Poor or no discussion about how
they could be overcome/
minimised. Major omissions, much
of the information provided is
irrelevant / unrelated to the CPI
goal.
(0-4)
Evaluation of the
project
10%
Discussion of mostly achievable
plan for how the intervention could
be evaluated.
(≧5)
Plan absent or not well described.
Most or all of the plan is not
relevant or achievable
Overlong / too brief, may be
missing a significant amount of
relevant information
(0-4)
References
5%
Supports assertions and facts with
relevant sources.
Uses the Harvard Referencing, with
no or only minor errors noted in the
reference list and/or in-text
referencing.
(≧2.5)
The Harvard Referencing style is not
used, or it is used but referencing is
consistently incorrect or absent.
Please note that all facts /
information throughout the entire
paper MUST be referenced
appropriately. Failure to do so may
result in a FAIL grade for the
project
(0-2)
Name of Marker
Grade
Any additional overall Comments
NURS2006 Supplementary Assessment for Semester Two, 2017. 12
Clinical Practice
Improvement Tool
15%
Describes a relevant CPI tool and
adequately discusses how the tool
could be used to address the aim
and implement the interventions.
Not succinct, contains irrelevant
information, significant information
is missing
(≧7.5)
A relevant CPI tool is not identified.
There is no adequate discussion of
how the tool could be used to meet
the aim or implement the
interventions.
Contains irrelevant information or
some major information is missing.
(0–7)
Summary of
proposed
intervention
20%
Most relevant interventions
discussed quite well.
Project outline is clear & relevance
to clinical practice is good. Contains
some irrelevant information, minor
information may be missing.
(≧10)
Some elements missing or
incomplete. May contain large
amounts of irrelevant information.
Project poorly described and it is
unclear what the project actually
entails or its relevance to clinical
practice.
(0-9.5)
Barriers to
Implementation
10%
Identifies a few potential barriers to
implementation & clinical change.
Discusses how barriers could be
overcome or minimised. Minor
omissions and/or some irrelevant
information present
(≧5)
Relevant barriers not identified.
Poor or no discussion about how
they could be overcome/
minimised. Major omissions, much
of the information provided is
irrelevant / unrelated to the CPI
goal.
(0-4)
Evaluation of the
project
10%
Discussion of mostly achievable
plan for how the intervention could
be evaluated.
(≧5)
Plan absent or not well described.
Most or all of the plan is not
relevant or achievable
Overlong / too brief, may be
missing a significant amount of
relevant information
(0-4)
References
5%
Supports assertions and facts with
relevant sources.
Uses the Harvard Referencing, with
no or only minor errors noted in the
reference list and/or in-text
referencing.
(≧2.5)
The Harvard Referencing style is not
used, or it is used but referencing is
consistently incorrect or absent.
Please note that all facts /
information throughout the entire
paper MUST be referenced
appropriately. Failure to do so may
result in a FAIL grade for the
project
(0-2)
Name of Marker
Grade
Any additional overall Comments
NURS2006 Supplementary Assessment for Semester Two, 2017. 12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





