Case Study Report: Meningitis Caused by Streptococcus and Neisseria
VerifiedAdded on 2022/10/19
|9
|2187
|445
Case Study
AI Summary
This case study report examines the case of an 80-year-old immunosuppressed woman diagnosed with meningitis caused by a combination of Streptococcus and Neisseria bacteria. The report details the patient's symptoms, diagnostic tests (including CSF analysis), and treatment with Ceftriaxone. It analyzes the effectiveness of the treatment, the significance of the patient's immunosuppressed state, and the implications of the bacterial combination. Recommendations are made for future management, emphasizing the importance of early diagnosis and appropriate antibiotic selection. The report also reflects on the potential for evidence-based medicine and suggests directions for further research, highlighting the significance of the case in understanding meningitis caused by these specific bacteria and the risk factors involved, such as old age and immunosuppression. The study emphasizes the need for prompt lumbar puncture and evaluation of cerebrospinal fluid for definitive analysis, especially in patients with symptoms related to meningitis.

CASE STUDY REPORT 1
Case Study Report
Case Study Report
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASE STUDY REPORT 2
Case Study Report
1. Introduction
Meningitis is a disorder that is linked by the inflammation of the membrane that surrounds
the brain and the spinal cord (Sloan and Parris, 2014). The swelling of meninges normally leads
to symptoms such as fever, stiff neck and headache. In most cases, meningitis is brought about
by a viral disease yet on rare occasion induced by bacteria, fungal and parasitic infection.
Furthermore, no cases have been reported about meningitis induced by the combination of
Streptococcus and Neisseria bacteria. Streptococcus is a bacterium that is normally found in skin,
oropharynx, genital tract and intestinal system whereas Neisseria subflava is found in the upper
respiratory system of the human body system. They are both benign bacteria, and on the rare
occasion, they cause infections of the CNS (Lucas, Brouwer and Beek, 2016). The current case
study follows a case of meningitis which is as a result of the combination of Streptococcus and
Neisseria bacteria. The report involves a 80-year-old woman who was admitted with complains
of disturbances of consciousness.
The main aim of this case report is to critically analyze and evaluate the current case study
while concentrating on the signs and symptoms, diagnosis, therapy, and follow up (Fukumoto, et
al., 2018). Furthermore, the report provides recommendations concerning the future management
of meningitis based on current research. Besides, the report provides directions for extension of
the current case report and reflects on the case studies the potential for implementation in
evidence-based medicine.
Case Study Report
1. Introduction
Meningitis is a disorder that is linked by the inflammation of the membrane that surrounds
the brain and the spinal cord (Sloan and Parris, 2014). The swelling of meninges normally leads
to symptoms such as fever, stiff neck and headache. In most cases, meningitis is brought about
by a viral disease yet on rare occasion induced by bacteria, fungal and parasitic infection.
Furthermore, no cases have been reported about meningitis induced by the combination of
Streptococcus and Neisseria bacteria. Streptococcus is a bacterium that is normally found in skin,
oropharynx, genital tract and intestinal system whereas Neisseria subflava is found in the upper
respiratory system of the human body system. They are both benign bacteria, and on the rare
occasion, they cause infections of the CNS (Lucas, Brouwer and Beek, 2016). The current case
study follows a case of meningitis which is as a result of the combination of Streptococcus and
Neisseria bacteria. The report involves a 80-year-old woman who was admitted with complains
of disturbances of consciousness.
The main aim of this case report is to critically analyze and evaluate the current case study
while concentrating on the signs and symptoms, diagnosis, therapy, and follow up (Fukumoto, et
al., 2018). Furthermore, the report provides recommendations concerning the future management
of meningitis based on current research. Besides, the report provides directions for extension of
the current case report and reflects on the case studies the potential for implementation in
evidence-based medicine.
CASE STUDY REPORT 3
2. Case study analysis and evaluation
The woman had a history of rheumatoid arthritis as she was old aged. The condition was
being controlled with methotrexate every week, tacrolimus and prednisolone every day. The
patient has also suffered from type 11 Diabetes which was being controlled by oral medications.
The lady's glycated hemoglobin level was 7.8 percent and had a dental embed which had been
expelled before the affirmation. She had been treated with medications which were halted seven
days before the confirmation (Fukumoto, et al., 2018).
The physical appraisal indicated she had a temperature of 36.6 degrees. She appeared to be
sleepy with a Glasgow unconsciousness score of twelve. Her neurological appraisal uncovered
cranial nerves in the left conjugate deviation other than her engine capacity is unblemished. Her
profound ligament reflexes were hyperactive in the entirety of her appendages. No ataxia, no
neurotic reflexes or sensory disorder were distinguished. The lady has a solid stiff neck with no
kernig's signs.
The lab tests for the lady uncovered that she had a white platelet check of 13,400/ul. Her C-
responsive protein level was 5.6 mg/dl. At the point when her lumbar cut was played done, her
underlying cerebrospinal fluid pressure was 130mm water and had a cell tally of 40/ul, CSF cell
count was 40/ul with elevated levels of protein and decreased the level of blood glucose. When
put under brain magnetic resonance imaging, no parenchymal issues were noted.
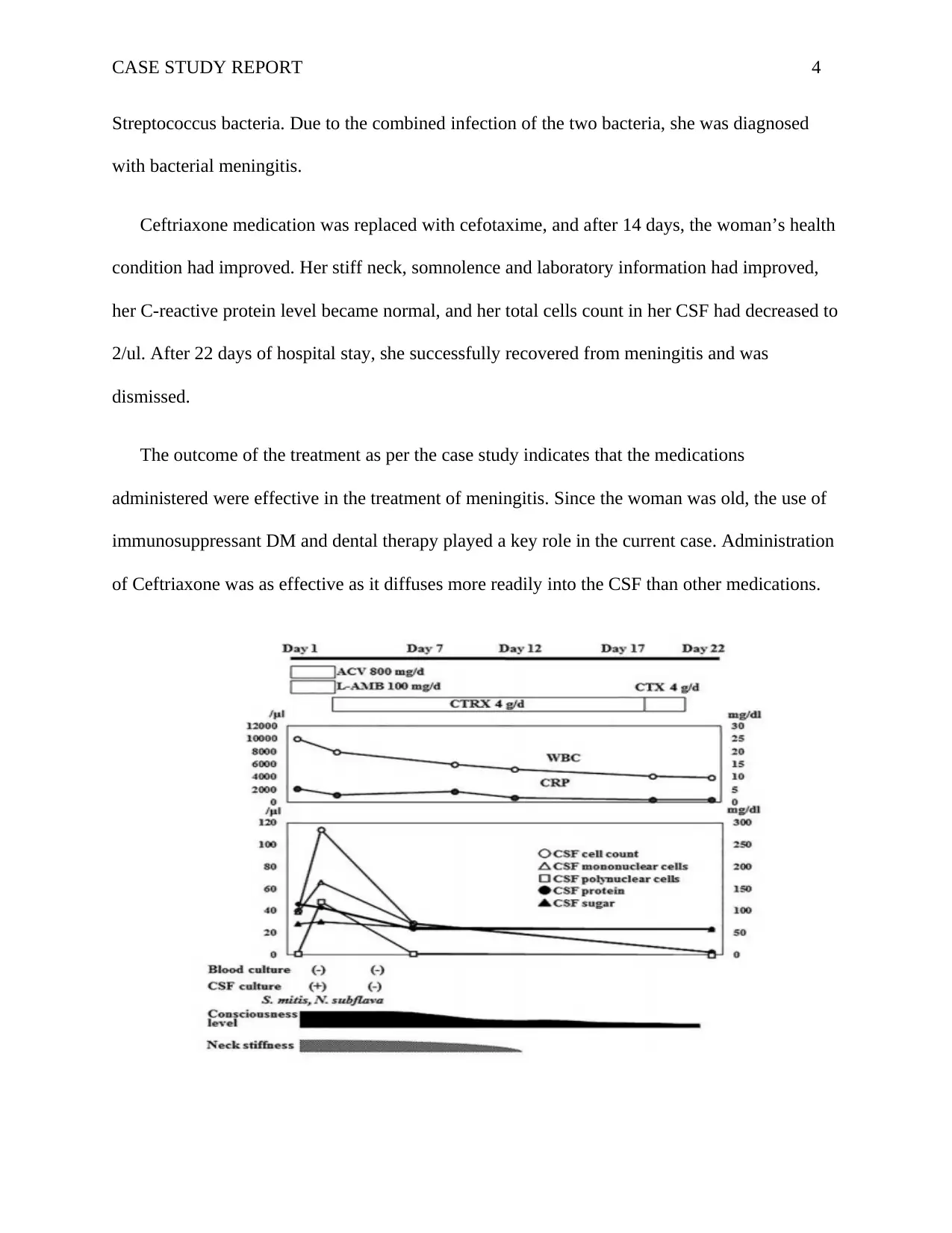
She was first administered with acyclovir and amphotericin medication which acted as an
empirical treatment for fungal and viral meningitis. After three days of hospital stay, the patient’s
CSF cultures become positive for Neisseria and Streptococcus bacteria. As a result of the tests,
the earlier medication was replaced with Ceftriaxone. Her CSF culture disclosed Neisseria and
2. Case study analysis and evaluation
The woman had a history of rheumatoid arthritis as she was old aged. The condition was
being controlled with methotrexate every week, tacrolimus and prednisolone every day. The
patient has also suffered from type 11 Diabetes which was being controlled by oral medications.
The lady's glycated hemoglobin level was 7.8 percent and had a dental embed which had been
expelled before the affirmation. She had been treated with medications which were halted seven
days before the confirmation (Fukumoto, et al., 2018).
The physical appraisal indicated she had a temperature of 36.6 degrees. She appeared to be
sleepy with a Glasgow unconsciousness score of twelve. Her neurological appraisal uncovered
cranial nerves in the left conjugate deviation other than her engine capacity is unblemished. Her
profound ligament reflexes were hyperactive in the entirety of her appendages. No ataxia, no
neurotic reflexes or sensory disorder were distinguished. The lady has a solid stiff neck with no
kernig's signs.
The lab tests for the lady uncovered that she had a white platelet check of 13,400/ul. Her C-
responsive protein level was 5.6 mg/dl. At the point when her lumbar cut was played done, her
underlying cerebrospinal fluid pressure was 130mm water and had a cell tally of 40/ul, CSF cell
count was 40/ul with elevated levels of protein and decreased the level of blood glucose. When
put under brain magnetic resonance imaging, no parenchymal issues were noted.
She was first administered with acyclovir and amphotericin medication which acted as an
empirical treatment for fungal and viral meningitis. After three days of hospital stay, the patient’s
CSF cultures become positive for Neisseria and Streptococcus bacteria. As a result of the tests,
the earlier medication was replaced with Ceftriaxone. Her CSF culture disclosed Neisseria and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CASE STUDY REPORT 4
Streptococcus bacteria. Due to the combined infection of the two bacteria, she was diagnosed
with bacterial meningitis.
Ceftriaxone medication was replaced with cefotaxime, and after 14 days, the woman’s health
condition had improved. Her stiff neck, somnolence and laboratory information had improved,
her C-reactive protein level became normal, and her total cells count in her CSF had decreased to
2/ul. After 22 days of hospital stay, she successfully recovered from meningitis and was
dismissed.
The outcome of the treatment as per the case study indicates that the medications
administered were effective in the treatment of meningitis. Since the woman was old, the use of
immunosuppressant DM and dental therapy played a key role in the current case. Administration
of Ceftriaxone was as effective as it diffuses more readily into the CSF than other medications.
Streptococcus bacteria. Due to the combined infection of the two bacteria, she was diagnosed
with bacterial meningitis.
Ceftriaxone medication was replaced with cefotaxime, and after 14 days, the woman’s health
condition had improved. Her stiff neck, somnolence and laboratory information had improved,
her C-reactive protein level became normal, and her total cells count in her CSF had decreased to
2/ul. After 22 days of hospital stay, she successfully recovered from meningitis and was
dismissed.
The outcome of the treatment as per the case study indicates that the medications
administered were effective in the treatment of meningitis. Since the woman was old, the use of
immunosuppressant DM and dental therapy played a key role in the current case. Administration
of Ceftriaxone was as effective as it diffuses more readily into the CSF than other medications.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASE STUDY REPORT 5
The current case study is important addition to the current body of literature on meningitis
and its causes. The case demonstrates that it is possible for an immunosuppressed patient to
develop meningitis as a result of the combination of Streptococcus and Neisseria bacteria both
which are natural inhabitants of mucous membranes (Fukumoto, et al., 2018). The case
represents the best reported case of meningitis that is as a result of a combination of benign
bacteria thus it opens door for further research and exploration.
3. Recommendation
Streptococcus is a bacterium that is normally found in skin, oropharynx, genital tract and
intestinal system on the other hand Neisseria subflava is found in mucous that is contained in the
upper respiratory system. They are both natural inhabitants of the mucous membrane thus
referred to as benign bacteria.
Many cases including the current case has been reported on meningitis that is caused by the
combination of the two natural inhabitants. As evidenced from (Brouwer et al., 2012), a serious
case of penicillin resistant Streptococcus caused meningitis to a six year old child who had
history of acute lymphoblastic leukemia. Also, another case was reported of 36 year old male
who had suffered from meningitis and septicemia induced by Neisseria subflava. This case
demonstrates that Streptococcus and Neisseria microbes may all be more principle purposes
behind meningitis than it is regularly fathomed. This demonstrates the requirement for
acknowledgment that S. furthermore, N.subflava both natural occupants can be pathogenic and
cause meningitis ( Hagiya and Otsuka, 2014).
The present case includes a case of elderly immunosuppressed patient. It involves a 80 year
woman who is immunosuppressed in that, she has disturbances of consciousness, a history of
The current case study is important addition to the current body of literature on meningitis
and its causes. The case demonstrates that it is possible for an immunosuppressed patient to
develop meningitis as a result of the combination of Streptococcus and Neisseria bacteria both
which are natural inhabitants of mucous membranes (Fukumoto, et al., 2018). The case
represents the best reported case of meningitis that is as a result of a combination of benign
bacteria thus it opens door for further research and exploration.
3. Recommendation
Streptococcus is a bacterium that is normally found in skin, oropharynx, genital tract and
intestinal system on the other hand Neisseria subflava is found in mucous that is contained in the
upper respiratory system. They are both natural inhabitants of the mucous membrane thus
referred to as benign bacteria.
Many cases including the current case has been reported on meningitis that is caused by the
combination of the two natural inhabitants. As evidenced from (Brouwer et al., 2012), a serious
case of penicillin resistant Streptococcus caused meningitis to a six year old child who had
history of acute lymphoblastic leukemia. Also, another case was reported of 36 year old male
who had suffered from meningitis and septicemia induced by Neisseria subflava. This case
demonstrates that Streptococcus and Neisseria microbes may all be more principle purposes
behind meningitis than it is regularly fathomed. This demonstrates the requirement for
acknowledgment that S. furthermore, N.subflava both natural occupants can be pathogenic and
cause meningitis ( Hagiya and Otsuka, 2014).
The present case includes a case of elderly immunosuppressed patient. It involves a 80 year
woman who is immunosuppressed in that, she has disturbances of consciousness, a history of
CASE STUDY REPORT 6
rheumatoid arthritis and previously she had suffered from type 11 diabetes. This indicates that
older and immunosuppressed people are at a high risk of suffering from meningitis that is
induced by Streptococcus and Neisseria (Glimåker et al., 2015). Therefore, it is high
recommended for older and immunosuppressed individuals to be diagnosed and be prevented
from such illness.
Also the decision of antibiotic that is used for the treatment of meningitis matters thus the
initial treatment has to be empirical (Nigrovic et al., 2013). Besides, the chosen antibiotic has to
have a bactericidal activity in the CSF as addressed in the current case. Furthermore, due to the
poor performance of clinical signs and manifestations that can help specialists to preclude
meningitis, all patients with present side effects that are connected to meningitis ought to
undergo prompt lumbar puncture and evaluation of cerebrospinal fluid for definitive analysis
(Fukumoto et al., 2018).
The case should also recommend for prevention of risk factors for patients to undergo lumbar
puncture. This is because many health care issues have been reported for patients who have
undergone lumbar Puncture. Some of the risk factors include immunosuppression, respiratory
abnormalities, seizure and altered mental status (McIntyre, et al., 2012).
4. Reflection on evidence-based medicine
The present case has the potential to be utilized in evidence-based medicine (Fukumoto, et
al., 2018). This is because the case is well documented with all medical history, laboratory tests
as well as diagnostic tests. As a result, the current case scenario has offered valuable insight into
optimal potential to provide valuable knowledge for the elderly immunosuppressed patient.
Furthermore, the case study provides valuable knowledge about the efficacy of various therapy
rheumatoid arthritis and previously she had suffered from type 11 diabetes. This indicates that
older and immunosuppressed people are at a high risk of suffering from meningitis that is
induced by Streptococcus and Neisseria (Glimåker et al., 2015). Therefore, it is high
recommended for older and immunosuppressed individuals to be diagnosed and be prevented
from such illness.
Also the decision of antibiotic that is used for the treatment of meningitis matters thus the
initial treatment has to be empirical (Nigrovic et al., 2013). Besides, the chosen antibiotic has to
have a bactericidal activity in the CSF as addressed in the current case. Furthermore, due to the
poor performance of clinical signs and manifestations that can help specialists to preclude
meningitis, all patients with present side effects that are connected to meningitis ought to
undergo prompt lumbar puncture and evaluation of cerebrospinal fluid for definitive analysis
(Fukumoto et al., 2018).
The case should also recommend for prevention of risk factors for patients to undergo lumbar
puncture. This is because many health care issues have been reported for patients who have
undergone lumbar Puncture. Some of the risk factors include immunosuppression, respiratory
abnormalities, seizure and altered mental status (McIntyre, et al., 2012).
4. Reflection on evidence-based medicine
The present case has the potential to be utilized in evidence-based medicine (Fukumoto, et
al., 2018). This is because the case is well documented with all medical history, laboratory tests
as well as diagnostic tests. As a result, the current case scenario has offered valuable insight into
optimal potential to provide valuable knowledge for the elderly immunosuppressed patient.
Furthermore, the case study provides valuable knowledge about the efficacy of various therapy
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CASE STUDY REPORT 7
and diagnostic approaches that can be utilized to treat patients with meningitis that is induced by
Streptococcus and Neisseria bacteria. Therefore, the current case study holds great potential to be
used in evidence-based medicine if extended to a case series comparing and contrasting various
cases.
5. Conclusion
The case study presents a 80-year-old woman who is immunosuppressed. She is diagnosed
with meningitis that is initiated by Streptococcus and Neisseria bacteria. Meningitis is a disorder
that is attributed by an inflammation of the membrane that surrounds the brain and the spinal
cord (Nakao et al., 2014). The inflammation of meninges normally leads to symptoms such as
fever, stiff neck and headache. In most cases, meningitis is induced by a viral infection but only
in rare cases that bacteria, fungal and parasitic infection have been reported. Streptococcus is a
bacterium that is normally found in skin, oropharynx, genital tract and intestinal system whereas
Neisseria subflava is found in the upper respiratory system of the human body system (Entesari
et al., 2014).
As confirmed from the case, Streptococcus and Neisseria bacteria, a natural inhabitant can be
the infective agent of meningitis. The risk factors for meningitis that is induced by Streptococcus
and Neisseria bacteria may include old age, dental treatment and immunosuppressive treatment
(Ali et al., 2016). A future study should be recommended to determine if these risk factors are
definite causes of meningitis that is induced by Neisseria and Streptococcus bacteria. In
conclusion, the present case had the potential for use in evidence-based medicine as it calls
attention to meningitis that is induced by natural inhabitant and highlights some of the risk
factors that may induce the illness.
and diagnostic approaches that can be utilized to treat patients with meningitis that is induced by
Streptococcus and Neisseria bacteria. Therefore, the current case study holds great potential to be
used in evidence-based medicine if extended to a case series comparing and contrasting various
cases.
5. Conclusion
The case study presents a 80-year-old woman who is immunosuppressed. She is diagnosed
with meningitis that is initiated by Streptococcus and Neisseria bacteria. Meningitis is a disorder
that is attributed by an inflammation of the membrane that surrounds the brain and the spinal
cord (Nakao et al., 2014). The inflammation of meninges normally leads to symptoms such as
fever, stiff neck and headache. In most cases, meningitis is induced by a viral infection but only
in rare cases that bacteria, fungal and parasitic infection have been reported. Streptococcus is a
bacterium that is normally found in skin, oropharynx, genital tract and intestinal system whereas
Neisseria subflava is found in the upper respiratory system of the human body system (Entesari
et al., 2014).
As confirmed from the case, Streptococcus and Neisseria bacteria, a natural inhabitant can be
the infective agent of meningitis. The risk factors for meningitis that is induced by Streptococcus
and Neisseria bacteria may include old age, dental treatment and immunosuppressive treatment
(Ali et al., 2016). A future study should be recommended to determine if these risk factors are
definite causes of meningitis that is induced by Neisseria and Streptococcus bacteria. In
conclusion, the present case had the potential for use in evidence-based medicine as it calls
attention to meningitis that is induced by natural inhabitant and highlights some of the risk
factors that may induce the illness.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASE STUDY REPORT 8
References
Ali, O., Aseffa, A., Omer, A.B., Lema, T., Demissie, T.M., Tekletsion, Y., Worku, A., Xabher,
H.G., Yamuah, L., Boukary, R.M. and Collard, J.M., 2016. Household transmission of Neisseria
meningitidis in the African meningitis belt: a longitudinal cohort study. The Lancet Global
Health, 4(12), pp.e989-e995.
Brouwer, M.C., Thwaites, G.E., Tunkel, A.R. and van de Beek, D., 2012. Dilemmas in the
diagnosis of acute community-acquired bacterial meningitis. The Lancet, 380(9854), pp.1684-
1692.
Entesari, D., Bagherirad, M., Quan, D. and Athan, E., 2014. Iatrogenic meningitis caused by
Neisseria sicca/subflava after intrathecal contrast injection, Australia. Emerging infectious
diseases, 20(6), p.1023.
Fukumoto, K., Manabe, Y., Fujiwara, S., Omote, Y., Narai, H., Yamada, H., Saito, T. and Abe,
K., 2018. Meningitis due to a Combination of Streptococcus mitis and Neisseria subflava: A
Case Report. Case reports in neurology, 10(2), pp.177-180.
Glimåker, M., Johansson, B., Grindborg, Ö., Bottai, M., Lindquist, L. and Sjölin, J., 2015. Adult
bacterial meningitis: earlier treatment and improved outcome following guideline revision
promoting prompt lumbar puncture. Clinical Infectious Diseases, 60(8), pp.1162-1169.
Hagiya, H. and Otsuka, F., 2014. Actinomyces meyeri meningitis: the need for anaerobic
cerebrospinal fluid cultures. Internal Medicine, 53(1), pp.67-71
Lucas, M.J., Brouwer, M.C. and Beek, D., 2016. Neurological sequelae of bacterial
meningitis. Journal of Infection, 73(1), pp.18-27.
References
Ali, O., Aseffa, A., Omer, A.B., Lema, T., Demissie, T.M., Tekletsion, Y., Worku, A., Xabher,
H.G., Yamuah, L., Boukary, R.M. and Collard, J.M., 2016. Household transmission of Neisseria
meningitidis in the African meningitis belt: a longitudinal cohort study. The Lancet Global
Health, 4(12), pp.e989-e995.
Brouwer, M.C., Thwaites, G.E., Tunkel, A.R. and van de Beek, D., 2012. Dilemmas in the
diagnosis of acute community-acquired bacterial meningitis. The Lancet, 380(9854), pp.1684-
1692.
Entesari, D., Bagherirad, M., Quan, D. and Athan, E., 2014. Iatrogenic meningitis caused by
Neisseria sicca/subflava after intrathecal contrast injection, Australia. Emerging infectious
diseases, 20(6), p.1023.
Fukumoto, K., Manabe, Y., Fujiwara, S., Omote, Y., Narai, H., Yamada, H., Saito, T. and Abe,
K., 2018. Meningitis due to a Combination of Streptococcus mitis and Neisseria subflava: A
Case Report. Case reports in neurology, 10(2), pp.177-180.
Glimåker, M., Johansson, B., Grindborg, Ö., Bottai, M., Lindquist, L. and Sjölin, J., 2015. Adult
bacterial meningitis: earlier treatment and improved outcome following guideline revision
promoting prompt lumbar puncture. Clinical Infectious Diseases, 60(8), pp.1162-1169.
Hagiya, H. and Otsuka, F., 2014. Actinomyces meyeri meningitis: the need for anaerobic
cerebrospinal fluid cultures. Internal Medicine, 53(1), pp.67-71
Lucas, M.J., Brouwer, M.C. and Beek, D., 2016. Neurological sequelae of bacterial
meningitis. Journal of Infection, 73(1), pp.18-27.
CASE STUDY REPORT 9
McIntyre, P.B., O'Brien, K.L., Greenwood, B. and Van De Beek, D., 2012. Effect of vaccines on
bacterial meningitis worldwide. The Lancet, 380(9854), pp.1703-1711.
Nakao, J.H., Jafri, F.N., Shah, K. and Newman, D.H., 2014. Jolt accentuation of headache and
other clinical signs: poor predictors of meningitis in adults. The American journal of emergency
medicine, 32(1), pp.24-28.
Nigrovic, L.E., Fine, A.M., Monuteaux, M.C., Shah, S.S. and Neuman, M.I., 2013. Trends in the
management of viral meningitis at United States children’s hospitals. Pediatrics, 131(4), pp.670-
676.
Sloan, D.J. and Parris, V., 2014. Cryptococcal meningitis: epidemiology and therapeutic
options. Clinical epidemiology, 6, p.169.
McIntyre, P.B., O'Brien, K.L., Greenwood, B. and Van De Beek, D., 2012. Effect of vaccines on
bacterial meningitis worldwide. The Lancet, 380(9854), pp.1703-1711.
Nakao, J.H., Jafri, F.N., Shah, K. and Newman, D.H., 2014. Jolt accentuation of headache and
other clinical signs: poor predictors of meningitis in adults. The American journal of emergency
medicine, 32(1), pp.24-28.
Nigrovic, L.E., Fine, A.M., Monuteaux, M.C., Shah, S.S. and Neuman, M.I., 2013. Trends in the
management of viral meningitis at United States children’s hospitals. Pediatrics, 131(4), pp.670-
676.
Sloan, D.J. and Parris, V., 2014. Cryptococcal meningitis: epidemiology and therapeutic
options. Clinical epidemiology, 6, p.169.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
