Ethical Practice in Mental Health and Addiction Support Work Report
VerifiedAdded on 2020/04/15
|14
|3088
|35
Report
AI Summary
This report delves into the ethical considerations within mental health and addiction support work. It addresses the ethical dilemma of privacy and confidentiality with mental health users, exploring decision-making processes that balance patient autonomy with the principles of justice, beneficence, and non-maleficence. The report examines the maintenance of boundaries according to wellness plans and organizational policies, and discusses ethical issues related to supervision. Furthermore, it analyzes ethical dilemmas surrounding consent with addiction service users, highlighting the application of utilitarianism in decision-making. The report also explores the importance of respecting patient autonomy, while adhering to organizational policies. The reflection section emphasizes the significance of ethical practices in patient care, focusing on the application of egalitarianism and the interconnectedness of beneficence and non-maleficence, to ensure patients receive quality care and improve their overall quality of life. The report references various academic sources to support its findings.

Running head: ETHICAL PRACTICE
ETHICAL PRACTICE IN MENTAL HEALTH & ADDICTION SUPPORT WORK
Name of the Student
Name of the University
Author Note
ETHICAL PRACTICE IN MENTAL HEALTH & ADDICTION SUPPORT WORK
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
ETHICAL PRACTICE
Table of Contents
Part: 1.........................................................................................................................................3
Mental Health Users:..............................................................................................................3
An ethical dilemma: Privacy..............................................................................................3
Decision making process....................................................................................................3
Maintenance of boundaries in accordance with the wellness plan.....................................4
Maintenance of boundaries in accordance with the organizational policies......................4
Discussion of ethical issues................................................................................................4
Ethical issues in accordance with organization policies....................................................5
Addiction Service Users.............................................................................................................5
An ethical dilemma: Consent.............................................................................................5
Maintenance of boundaries in accordance with the wellness plan.....................................6
Maintenance of boundaries in accordance with the organizational policies......................7
Discussion of ethical issues................................................................................................7
Ethical issues in accordance with organization policies....................................................8
Part 2..........................................................................................................................................9
Reflection...............................................................................................................................9
Reflection review...............................................................................................................9
Reflection on ethical practices: Self evaluation.................................................................9
References................................................................................................................................11
ETHICAL PRACTICE
Table of Contents
Part: 1.........................................................................................................................................3
Mental Health Users:..............................................................................................................3
An ethical dilemma: Privacy..............................................................................................3
Decision making process....................................................................................................3
Maintenance of boundaries in accordance with the wellness plan.....................................4
Maintenance of boundaries in accordance with the organizational policies......................4
Discussion of ethical issues................................................................................................4
Ethical issues in accordance with organization policies....................................................5
Addiction Service Users.............................................................................................................5
An ethical dilemma: Consent.............................................................................................5
Maintenance of boundaries in accordance with the wellness plan.....................................6
Maintenance of boundaries in accordance with the organizational policies......................7
Discussion of ethical issues................................................................................................7
Ethical issues in accordance with organization policies....................................................8
Part 2..........................................................................................................................................9
Reflection...............................................................................................................................9
Reflection review...............................................................................................................9
Reflection on ethical practices: Self evaluation.................................................................9
References................................................................................................................................11
2
ETHICAL PRACTICE
ETHICAL PRACTICE
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
ETHICAL PRACTICE
Part: 1
Mental Health Users:
An ethical dilemma: Privacy
The right of an individual towards confidentiality and privacy falls under the ethical
principle of autonomy. There are four types of privacy including physical privacy,
informational privacy, decisional privacy and proprietary privacy (Siriwardhana, Adikari,
Jayaweera & Sumathipala, 2013). Confidentiality is a right to restrict the disclosure of the
personal information. While providing mental healthcare to a Tangata Whai Ora mental
health patient, I faced ethical dilemma of privacy and confidentiality. The patient has
reported me certain information that is potentially harmful to himself or someone else and
thus I faced dilemma as a service worker in reporting the information. Moreover, a
psychiatric patient does not have a stable frame of mind for the information to be truthful. I
faced ethical dilemma in reporting that sensitive information to doctor because the patient
was not willing to share the same with the doctor. He has shared with me only out of sheer
trust and believed that I won't share the same information to anyone else.
Decision making process
In the domain of the disclosure of the information, patient's autonomy is at times
overridden by the ethical principal of justice and/or nonmaleficence, beneficence (DeKeyser
Ganz & Berkovitz, 2012). In the decision making process, what I took as a reference is,
information can be disclosed in the absence of the patient's information only when the person
are falling under a threat to themselves (non-maleficence) and when the information is in a
need for providing quality care (beneficence). In my case, the information shared by the
patients about his health status was misleading and has no connection with each other. This
ETHICAL PRACTICE
Part: 1
Mental Health Users:
An ethical dilemma: Privacy
The right of an individual towards confidentiality and privacy falls under the ethical
principle of autonomy. There are four types of privacy including physical privacy,
informational privacy, decisional privacy and proprietary privacy (Siriwardhana, Adikari,
Jayaweera & Sumathipala, 2013). Confidentiality is a right to restrict the disclosure of the
personal information. While providing mental healthcare to a Tangata Whai Ora mental
health patient, I faced ethical dilemma of privacy and confidentiality. The patient has
reported me certain information that is potentially harmful to himself or someone else and
thus I faced dilemma as a service worker in reporting the information. Moreover, a
psychiatric patient does not have a stable frame of mind for the information to be truthful. I
faced ethical dilemma in reporting that sensitive information to doctor because the patient
was not willing to share the same with the doctor. He has shared with me only out of sheer
trust and believed that I won't share the same information to anyone else.
Decision making process
In the domain of the disclosure of the information, patient's autonomy is at times
overridden by the ethical principal of justice and/or nonmaleficence, beneficence (DeKeyser
Ganz & Berkovitz, 2012). In the decision making process, what I took as a reference is,
information can be disclosed in the absence of the patient's information only when the person
are falling under a threat to themselves (non-maleficence) and when the information is in a
need for providing quality care (beneficence). In my case, the information shared by the
patients about his health status was misleading and has no connection with each other. This
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
ETHICAL PRACTICE
showed that the patient's was in a complex state of mind and was unable to recollect the
thoughts and hence I reported the same to the doctor via narrating his actual quotes. This I
need only for the continuity of care of the patient (beneficence) (DeKeyser Ganz &
Berkovitz, 2012).
Maintenance of boundaries in accordance with the wellness plan
According to the wellness plan, discussion of the issues in relation of the mental
health service seekers must be done with the knowledgeable staffs for delivery of care in a
safe manner (Arahura Charitable Trust, 2017). In this case, also the issues that are being
experienced by the Tangata Whai Ora disclosed to the doctors as they are most
knowledgeable person in the care model who will be successful in procuring quality care.
Maintenance of boundaries in accordance with the organizational policies
According to the organisational policies, all the staffs are legally restricted to respect
the confidentiality and privacy of the Tangata Whai Ora (Kidd, Butler & Harris, 2013). This
signifies that during the tenure of the work and even beyond the work hours they are required
to abide by the privacy policies. In order to remain within the boundary of the organisational
policies, I treated the patient with respect and did not discussed his details or personal issues
in front of the unauthorised person. What I did is I discussed his concerns with the doctors
and only for the betterment of his health. Doctors are the best person to provide quality care
to the patients via accessing their present condition. Since it is not possible for the doctors to
remain in touch with the patients 24X7, it is the duty of the associated service providers to
convey the information to the doctors.
Discussion of ethical issues
The ethical issue at supervision can be described under the light of the beneficence
and nonmaleficence. For the benefit of the patient, in order relief him from the mental
ETHICAL PRACTICE
showed that the patient's was in a complex state of mind and was unable to recollect the
thoughts and hence I reported the same to the doctor via narrating his actual quotes. This I
need only for the continuity of care of the patient (beneficence) (DeKeyser Ganz &
Berkovitz, 2012).
Maintenance of boundaries in accordance with the wellness plan
According to the wellness plan, discussion of the issues in relation of the mental
health service seekers must be done with the knowledgeable staffs for delivery of care in a
safe manner (Arahura Charitable Trust, 2017). In this case, also the issues that are being
experienced by the Tangata Whai Ora disclosed to the doctors as they are most
knowledgeable person in the care model who will be successful in procuring quality care.
Maintenance of boundaries in accordance with the organizational policies
According to the organisational policies, all the staffs are legally restricted to respect
the confidentiality and privacy of the Tangata Whai Ora (Kidd, Butler & Harris, 2013). This
signifies that during the tenure of the work and even beyond the work hours they are required
to abide by the privacy policies. In order to remain within the boundary of the organisational
policies, I treated the patient with respect and did not discussed his details or personal issues
in front of the unauthorised person. What I did is I discussed his concerns with the doctors
and only for the betterment of his health. Doctors are the best person to provide quality care
to the patients via accessing their present condition. Since it is not possible for the doctors to
remain in touch with the patients 24X7, it is the duty of the associated service providers to
convey the information to the doctors.
Discussion of ethical issues
The ethical issue at supervision can be described under the light of the beneficence
and nonmaleficence. For the benefit of the patient, in order relief him from the mental
5
ETHICAL PRACTICE
complexicities, it is the duty of the nurse to listen careful to very information or stories that is
being shared by the mental health patients. Moreover, the nurses are required to generate a
strong relationship based on trust with the patients so that they feel comfortable in sharing the
information. When it comes sharing the information to the patients to other healthcare
professionals who holds higher position in term of hierarchy, the ethical dilemma of
confidentiality or privacy can be breached on the grounds of nonmaleficence. The act of
nonmaleficence means no harm to the patients and here the nurse is only sharing data with
the doctors in order to prevent further mental harm to the patient (Kangasniemi, Vaismoradi,
Jasper & Turunen, 2013).
Ethical issues in accordance with organization policies
Organizational policies maintain a strict rule of privacy and confidentiality concern
when dealing with mental health patients. However, organization also assures quality care to
the patients. In the grounds of providing quality care, a nurse can share confidential data to
the doctors (included in the same health care team) in order to improve the therapy plan
(Kangasniemi, Vaismoradi, Jasper & Turunen, 2013).
Addiction Service Users
An ethical dilemma: Consent
The main ethical dilemma that is faced while providing support to the patients who
are suffering from certain kind of addiction (drug or alcohol) is, respecting patient’s
autonomy (Owonikoko, 2013). Principle of autonomy refers to the right of the individual to
determine the kind of activities they want or will to participate. The principal of autonomy
falls under the category of consent.
Decision making process
ETHICAL PRACTICE
complexicities, it is the duty of the nurse to listen careful to very information or stories that is
being shared by the mental health patients. Moreover, the nurses are required to generate a
strong relationship based on trust with the patients so that they feel comfortable in sharing the
information. When it comes sharing the information to the patients to other healthcare
professionals who holds higher position in term of hierarchy, the ethical dilemma of
confidentiality or privacy can be breached on the grounds of nonmaleficence. The act of
nonmaleficence means no harm to the patients and here the nurse is only sharing data with
the doctors in order to prevent further mental harm to the patient (Kangasniemi, Vaismoradi,
Jasper & Turunen, 2013).
Ethical issues in accordance with organization policies
Organizational policies maintain a strict rule of privacy and confidentiality concern
when dealing with mental health patients. However, organization also assures quality care to
the patients. In the grounds of providing quality care, a nurse can share confidential data to
the doctors (included in the same health care team) in order to improve the therapy plan
(Kangasniemi, Vaismoradi, Jasper & Turunen, 2013).
Addiction Service Users
An ethical dilemma: Consent
The main ethical dilemma that is faced while providing support to the patients who
are suffering from certain kind of addiction (drug or alcohol) is, respecting patient’s
autonomy (Owonikoko, 2013). Principle of autonomy refers to the right of the individual to
determine the kind of activities they want or will to participate. The principal of autonomy
falls under the category of consent.
Decision making process
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6
ETHICAL PRACTICE
The main decision making process that is being used for resolving the ethical
dilemma of autonomy while treating addicted patients is the theory of utilitarianism.
According to this theory, utility must always be encouraged as the sum of all the pleasures
from an action, minus any suffering of anyone involved in the action. So the principle of
utilitarianism always highlights the sum of well-being and ignores any negativity that may
arise while working in favour of the benefit (Grant, Kajii, Polak & Safra, 2012). I think, even
if the addicted (drug or alcohol) Tangata Whai Ora is refusing to give the consent to
participate in the addiction recovery service; the therapy can be applied beyond his or her
consent. This is because, participation in the addiction recovery therapy, will actually help
him or her to enter into a state of well-being. This quality of life will outnumber his or her
negative approach in providing the consent in the long run.
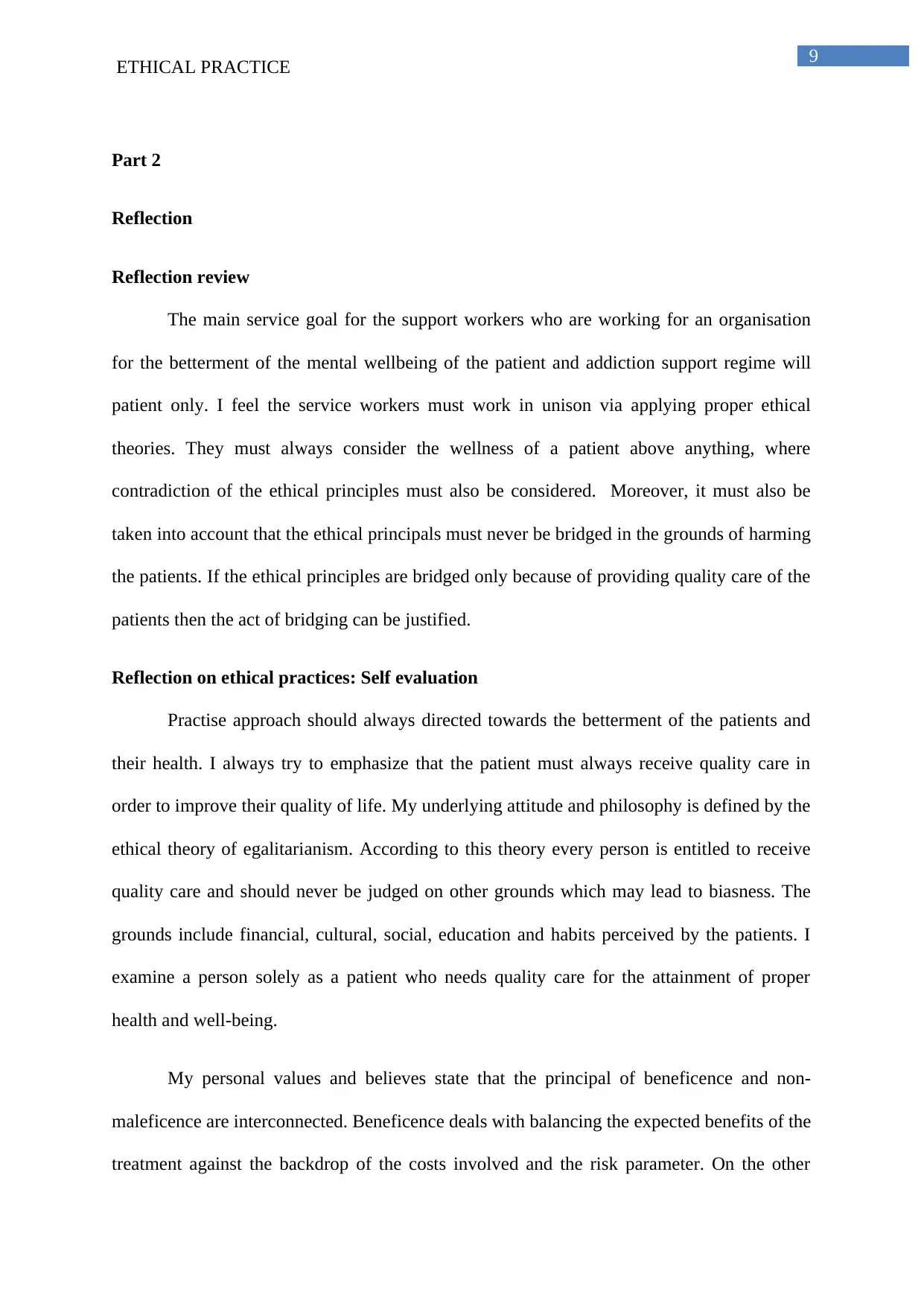
Maintenance of boundaries in accordance with the wellness plan
In order to maintain the boundary of the support worker role in accordance with the
organisational policies, I interacted with the Tangata whai Ora personally in order to know
the exact reasons behind why he is refusing to participate in the addiction control wellness
program (Holmes, 2012). What I elucidated that his concept of well-being is projected
towards four basic pillars of life, as discussed in picture below.
Figure: Four Dimensions of Wellbeing
ETHICAL PRACTICE
The main decision making process that is being used for resolving the ethical
dilemma of autonomy while treating addicted patients is the theory of utilitarianism.
According to this theory, utility must always be encouraged as the sum of all the pleasures
from an action, minus any suffering of anyone involved in the action. So the principle of
utilitarianism always highlights the sum of well-being and ignores any negativity that may
arise while working in favour of the benefit (Grant, Kajii, Polak & Safra, 2012). I think, even
if the addicted (drug or alcohol) Tangata Whai Ora is refusing to give the consent to
participate in the addiction recovery service; the therapy can be applied beyond his or her
consent. This is because, participation in the addiction recovery therapy, will actually help
him or her to enter into a state of well-being. This quality of life will outnumber his or her
negative approach in providing the consent in the long run.
Maintenance of boundaries in accordance with the wellness plan
In order to maintain the boundary of the support worker role in accordance with the
organisational policies, I interacted with the Tangata whai Ora personally in order to know
the exact reasons behind why he is refusing to participate in the addiction control wellness
program (Holmes, 2012). What I elucidated that his concept of well-being is projected
towards four basic pillars of life, as discussed in picture below.
Figure: Four Dimensions of Wellbeing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
ETHICAL PRACTICE
(Source: Hammell & Iwama, 2012)
After knowing the same, I tried to incline the effectiveness of the wellness programme
to each of the four dimensions in life. I also tried to explain him how addiction control
service will help him in stay under the good state of mental health, physical health and
spiritual health and all these health status will in turn promote the family health (Hoge et al.,
2-13). Thus via remaining within the boundaries of a support worker, I tried to earn the
consent of the patient for his participation in the wellness program, without bridging the
ethical theory of autonomy (consent).
Maintenance of boundaries in accordance with the organizational policies
As per the organizational policies, no patient can be forced or allowed to participate in
a wellness program beyond his or her consent (Grady, 2015). So in order to remain within the
boundaries of the organisational policies, I performed a counselling session with the patient.
The counselling session helped in the identification of the dilemma which the patient is
facing while participating in the wellness program. So via understanding the root of the
problem, I acted accordingly, made him understand the benefit of the wellness program on an
utilitarian approach and bridged the gap of autonomy (consent).
Discussion of ethical issues
The main ethical issues which are coming in supervision apart from the principal of
autonomy is, the theory of libertarianism. According to this theory, there must a freedom for
everything, like freedom of decision making, freedom of speech, freedom of gender equality
and so on. However, the theory of egalitarianism states that there must be equality for all
(Moreno-Ternero & Roemer, 2012). So under the light of the egalitarianism, the patient here
also deserves quality care but is unable to receive the same on the grounds of autonomy and
libertarianism. However, his concept of denial is not justified as he is unaware of the
ETHICAL PRACTICE
(Source: Hammell & Iwama, 2012)
After knowing the same, I tried to incline the effectiveness of the wellness programme
to each of the four dimensions in life. I also tried to explain him how addiction control
service will help him in stay under the good state of mental health, physical health and
spiritual health and all these health status will in turn promote the family health (Hoge et al.,
2-13). Thus via remaining within the boundaries of a support worker, I tried to earn the
consent of the patient for his participation in the wellness program, without bridging the
ethical theory of autonomy (consent).
Maintenance of boundaries in accordance with the organizational policies
As per the organizational policies, no patient can be forced or allowed to participate in
a wellness program beyond his or her consent (Grady, 2015). So in order to remain within the
boundaries of the organisational policies, I performed a counselling session with the patient.
The counselling session helped in the identification of the dilemma which the patient is
facing while participating in the wellness program. So via understanding the root of the
problem, I acted accordingly, made him understand the benefit of the wellness program on an
utilitarian approach and bridged the gap of autonomy (consent).
Discussion of ethical issues
The main ethical issues which are coming in supervision apart from the principal of
autonomy is, the theory of libertarianism. According to this theory, there must a freedom for
everything, like freedom of decision making, freedom of speech, freedom of gender equality
and so on. However, the theory of egalitarianism states that there must be equality for all
(Moreno-Ternero & Roemer, 2012). So under the light of the egalitarianism, the patient here
also deserves quality care but is unable to receive the same on the grounds of autonomy and
libertarianism. However, his concept of denial is not justified as he is unaware of the
8
ETHICAL PRACTICE
consequences of the addiction in his later stages of life so the counselling done during the
supervision is justified and will help the patient for fast recovery.
Ethical issues in accordance with organization policies
Organisational policies give importance of taking consent of patient at every stage of
the wellness and recovery therapy (Thiel, Bagdasarov, Harkrider, Johnson & Mumford,
2012). So in order to work in accordance with the organisational norms, the patient was
counselled in order to obtain the consent and progress the treatment in an ethically correct
manner
ETHICAL PRACTICE
consequences of the addiction in his later stages of life so the counselling done during the
supervision is justified and will help the patient for fast recovery.
Ethical issues in accordance with organization policies
Organisational policies give importance of taking consent of patient at every stage of
the wellness and recovery therapy (Thiel, Bagdasarov, Harkrider, Johnson & Mumford,
2012). So in order to work in accordance with the organisational norms, the patient was
counselled in order to obtain the consent and progress the treatment in an ethically correct
manner
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
ETHICAL PRACTICE
Part 2
Reflection
Reflection review
The main service goal for the support workers who are working for an organisation
for the betterment of the mental wellbeing of the patient and addiction support regime will
patient only. I feel the service workers must work in unison via applying proper ethical
theories. They must always consider the wellness of a patient above anything, where
contradiction of the ethical principles must also be considered. Moreover, it must also be
taken into account that the ethical principals must never be bridged in the grounds of harming
the patients. If the ethical principles are bridged only because of providing quality care of the
patients then the act of bridging can be justified.
Reflection on ethical practices: Self evaluation
Practise approach should always directed towards the betterment of the patients and
their health. I always try to emphasize that the patient must always receive quality care in
order to improve their quality of life. My underlying attitude and philosophy is defined by the
ethical theory of egalitarianism. According to this theory every person is entitled to receive
quality care and should never be judged on other grounds which may lead to biasness. The
grounds include financial, cultural, social, education and habits perceived by the patients. I
examine a person solely as a patient who needs quality care for the attainment of proper
health and well-being.
My personal values and believes state that the principal of beneficence and non-
maleficence are interconnected. Beneficence deals with balancing the expected benefits of the
treatment against the backdrop of the costs involved and the risk parameter. On the other
ETHICAL PRACTICE
Part 2
Reflection
Reflection review
The main service goal for the support workers who are working for an organisation
for the betterment of the mental wellbeing of the patient and addiction support regime will
patient only. I feel the service workers must work in unison via applying proper ethical
theories. They must always consider the wellness of a patient above anything, where
contradiction of the ethical principles must also be considered. Moreover, it must also be
taken into account that the ethical principals must never be bridged in the grounds of harming
the patients. If the ethical principles are bridged only because of providing quality care of the
patients then the act of bridging can be justified.
Reflection on ethical practices: Self evaluation
Practise approach should always directed towards the betterment of the patients and
their health. I always try to emphasize that the patient must always receive quality care in
order to improve their quality of life. My underlying attitude and philosophy is defined by the
ethical theory of egalitarianism. According to this theory every person is entitled to receive
quality care and should never be judged on other grounds which may lead to biasness. The
grounds include financial, cultural, social, education and habits perceived by the patients. I
examine a person solely as a patient who needs quality care for the attainment of proper
health and well-being.
My personal values and believes state that the principal of beneficence and non-
maleficence are interconnected. Beneficence deals with balancing the expected benefits of the
treatment against the backdrop of the costs involved and the risk parameter. On the other
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
ETHICAL PRACTICE
hand, non-maleficience means avoidance of harm. Several treatments involve certain degree
of harm; here the principle of non-maleficence would signify that the possible harm should
never be disproportionate to the expected benefit of the treatment. However, abiding the
principle of beneficence and non-maleficence may at times can cause harm to a person's
autonomy (in some circumstances) (Thiel, Bagdasarov, Harkrider, Johnson & Mumford,
2012). For example, it may be required to deliver treatment that is not expected to prevent the
development of a future, more serious health related problem. The overall course of the
treatment can be extremely unpleasant, uncomfortable or at times can be extremely painful.
However, this might cast comparatively less harm to the patient than that would occur
previously. So my self-evaluation tells me that my ethical mindset is more inclined towards
the ethical principal of beneficence and non-maleficence.
Patient's participation in the process of treatment decision, is the principal pillar of
health care. This can be related to the highest levels of patient's satisfaction, adherence to the
treatment and improved health outcomes. The level of patient's participation is the process of
treatment decisions in dependent on the intrapersonal (patient's characteristic) and
interpersonal (communication styles between the patient and the care provider) (Morse,
Salyers, Rollins, Monroe-DeVita & Pfahler, 2012). As per my evaluation, my communication
style is strong enough in modulating the patient’s mindset, while making the patient to
actively participate in the healthcare decision making.
ETHICAL PRACTICE
hand, non-maleficience means avoidance of harm. Several treatments involve certain degree
of harm; here the principle of non-maleficence would signify that the possible harm should
never be disproportionate to the expected benefit of the treatment. However, abiding the
principle of beneficence and non-maleficence may at times can cause harm to a person's
autonomy (in some circumstances) (Thiel, Bagdasarov, Harkrider, Johnson & Mumford,
2012). For example, it may be required to deliver treatment that is not expected to prevent the
development of a future, more serious health related problem. The overall course of the
treatment can be extremely unpleasant, uncomfortable or at times can be extremely painful.
However, this might cast comparatively less harm to the patient than that would occur
previously. So my self-evaluation tells me that my ethical mindset is more inclined towards
the ethical principal of beneficence and non-maleficence.
Patient's participation in the process of treatment decision, is the principal pillar of
health care. This can be related to the highest levels of patient's satisfaction, adherence to the
treatment and improved health outcomes. The level of patient's participation is the process of
treatment decisions in dependent on the intrapersonal (patient's characteristic) and
interpersonal (communication styles between the patient and the care provider) (Morse,
Salyers, Rollins, Monroe-DeVita & Pfahler, 2012). As per my evaluation, my communication
style is strong enough in modulating the patient’s mindset, while making the patient to
actively participate in the healthcare decision making.
11
ETHICAL PRACTICE
References
DeKeyser Ganz, F., & Berkovitz, K. (2012). Surgical nurses’ perceptions of ethical
dilemmas, moral distress and quality of care. Journal of advanced nursing, vol. 68(7),
pp. 1516-1525. 10.1111/j.1365-2648.2011.05897.x
Grady, C. (2015). Enduring and emerging challenges of informed consent. New England
Journal of Medicine, vol. (9), pp. 855-862. DOI: 10.1056/NEJMra1411250
Grant, S., Kajii, A., Polak, B., & Safra, Z. (2012). Equally-distributed equivalent utility, ex
post egalitarianism and utilitarianism. Journal of Economic Theory, vol. 147(4), pp.
1545-1571. https://doi.org/10.1016/j.jet.2011.04.001
Hammell, K. R. W., & Iwama, M. K. (2012). Well-being and occupational rights: An
imperative for critical occupational therapy. Scandinavian journal of occupational
therapy, vol. 19(5), pp. 385-394. http://dx.doi.org/10.3109/11038128.2011.611821
Hoge, M. A., Stuart, G. W., Morris, J., Flaherty, M. T., Paris Jr, M., & Goplerud, E. (2013).
Mental health and addiction workforce development: Federal leadership is needed to
address the growing crisis. Health Affairs, vol. 32(11), pp. 2005-2012.
https://doi.org/10.1377/hlthaff.2013.0541
Holmes, D. (2012). Prescription drug addiction: the treatment challenge. The Lancet, vol.
379(9810), pp. 17-18. DOI: http://dx.doi.org/10.1016/S0140-6736(12)60007-5
Kangasniemi, M., Vaismoradi, M., Jasper, M., & Turunen, H. (2013). Ethical issues in
patient safety: Implications for nursing management. Nursing ethics, vol. 20(8), pp.
904-916. https://doi.org/10.1177/0969733013484488
ETHICAL PRACTICE
References
DeKeyser Ganz, F., & Berkovitz, K. (2012). Surgical nurses’ perceptions of ethical
dilemmas, moral distress and quality of care. Journal of advanced nursing, vol. 68(7),
pp. 1516-1525. 10.1111/j.1365-2648.2011.05897.x
Grady, C. (2015). Enduring and emerging challenges of informed consent. New England
Journal of Medicine, vol. (9), pp. 855-862. DOI: 10.1056/NEJMra1411250
Grant, S., Kajii, A., Polak, B., & Safra, Z. (2012). Equally-distributed equivalent utility, ex
post egalitarianism and utilitarianism. Journal of Economic Theory, vol. 147(4), pp.
1545-1571. https://doi.org/10.1016/j.jet.2011.04.001
Hammell, K. R. W., & Iwama, M. K. (2012). Well-being and occupational rights: An
imperative for critical occupational therapy. Scandinavian journal of occupational
therapy, vol. 19(5), pp. 385-394. http://dx.doi.org/10.3109/11038128.2011.611821
Hoge, M. A., Stuart, G. W., Morris, J., Flaherty, M. T., Paris Jr, M., & Goplerud, E. (2013).
Mental health and addiction workforce development: Federal leadership is needed to
address the growing crisis. Health Affairs, vol. 32(11), pp. 2005-2012.
https://doi.org/10.1377/hlthaff.2013.0541
Holmes, D. (2012). Prescription drug addiction: the treatment challenge. The Lancet, vol.
379(9810), pp. 17-18. DOI: http://dx.doi.org/10.1016/S0140-6736(12)60007-5
Kangasniemi, M., Vaismoradi, M., Jasper, M., & Turunen, H. (2013). Ethical issues in
patient safety: Implications for nursing management. Nursing ethics, vol. 20(8), pp.
904-916. https://doi.org/10.1177/0969733013484488
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





