NRS83003 Mental Health: Alzheimer's Case Study - Diagnosis & Plan
VerifiedAdded on 2023/03/31
|9
|3895
|326
Case Study
AI Summary
This case study examines a 58-year-old male, Sam, diagnosed with early-onset Alzheimer's. The analysis covers the emergence and impact of his symptoms, including cognitive decline, apraxia, and apathy, which led to job loss and dependence on family. The diagnostic process involved neuropsychological testing and brain imaging, revealing atrophy and amyloid deposition. A bio-psycho-social formulation explores biological, psychological, and social factors influencing Sam's condition. The study concludes with a discussion of evidence-based treatment, including donepezil and memantine, along with behavioral therapies and the Progressively Lowered Stress Threshold model to improve Sam's quality of life. The treatment plan focuses on slowing the decline, managing symptoms, and providing support to maintain his independence and dignity, highlighting the importance of a holistic approach to Alzheimer's care. Desklib provides students access to such case studies and other resources.
1
Master in Health Care
Describe how and when symptoms emerged
The case study is of a 58 year old male patient named Sam. He complained of
progressive psychological decline which had begun 3 years before. Functioning as a
researcher, he committed calculation errors that made him leave his employment and
started filling in as a director of an organization. Be that as it may, his continuous
disturbance in ongoing memory debilitations hampered him from satisfying his
obligations, making him change occupations every now and again. Apraxia and apathy
had begun 2 years before his visit to the hospital, and unconsciousness to time and
individual was intensified to a degree which it made it difficult to drive every day
between his work and home. At the time of his visit to the facility, he had terminated his
professional activity. He also required incessant reminders from his family to look after
cleanliness and work. His sleep schedule had messed up caused him to wake up at
wee hours. He has also reported to talk to himself in the middle of the night.
Impact they have on the person’s functioning
The symptoms had left him imbalanced and unable to be accountable for the normal life
activities that he once carried on by himself. He also to leave his job and depend on his
family members and wait for them to give him cues. As a researcher he was required to
make intricate calculations and make detailed records of occurrences (Alzheimer’s,
2015). It was noticed that he made several mistakes in the calculations and unable to
manage his activities properly. The greatest impact was caused because of gradual
memory loss that made him severely bewildered as he was unable to recognise people
and even manage a healthy lifestyle. He also had diabetes and required to take
medicine for the issue but forgot to take them on time. In some cases, he administered
more doses than was necessary he was unable to keep tabs on it. As a result, his
metabolic health had also declined. His vision declined drastically and he often bumped
into furniture on his late-night activities.
Primary diagnosis
Sam has earlier visited two hospitals for a diagnosis but he was unable to receive help
that was able to manage the intensifying symptoms. In the last visit to the clinic he was
admitted to the psychiatric ward and neuropsychological test was run that showcased
severe impairment in his ability to recall something and recognition skills. Then
magnetic imaging tests were performed to see any abnormalities in the brain. Atrophy
and tissue breakdown were noticed in the medial temporal lobe and the cortes. These
were recognised as a sign of onset of dementia. In the next PET imaging test, the
presence of amyloid deposition was revealed. The above symptoms and reports from
tests suggested the onset of Alzheimer's.
Key symptoms associated with the diagnosis
The diagnosis was strengthened by the tissue breakdown noticed in the brain. However,
there were presence other physical symptoms that made the doctors run the specific
tests upon Sam. Even though Sam was able to keep his speech and verbal skills intact
he had problem in identifying people and even places that he had frequented before.
Master in Health Care
Describe how and when symptoms emerged
The case study is of a 58 year old male patient named Sam. He complained of
progressive psychological decline which had begun 3 years before. Functioning as a
researcher, he committed calculation errors that made him leave his employment and
started filling in as a director of an organization. Be that as it may, his continuous
disturbance in ongoing memory debilitations hampered him from satisfying his
obligations, making him change occupations every now and again. Apraxia and apathy
had begun 2 years before his visit to the hospital, and unconsciousness to time and
individual was intensified to a degree which it made it difficult to drive every day
between his work and home. At the time of his visit to the facility, he had terminated his
professional activity. He also required incessant reminders from his family to look after
cleanliness and work. His sleep schedule had messed up caused him to wake up at
wee hours. He has also reported to talk to himself in the middle of the night.
Impact they have on the person’s functioning
The symptoms had left him imbalanced and unable to be accountable for the normal life
activities that he once carried on by himself. He also to leave his job and depend on his
family members and wait for them to give him cues. As a researcher he was required to
make intricate calculations and make detailed records of occurrences (Alzheimer’s,
2015). It was noticed that he made several mistakes in the calculations and unable to
manage his activities properly. The greatest impact was caused because of gradual
memory loss that made him severely bewildered as he was unable to recognise people
and even manage a healthy lifestyle. He also had diabetes and required to take
medicine for the issue but forgot to take them on time. In some cases, he administered
more doses than was necessary he was unable to keep tabs on it. As a result, his
metabolic health had also declined. His vision declined drastically and he often bumped
into furniture on his late-night activities.
Primary diagnosis
Sam has earlier visited two hospitals for a diagnosis but he was unable to receive help
that was able to manage the intensifying symptoms. In the last visit to the clinic he was
admitted to the psychiatric ward and neuropsychological test was run that showcased
severe impairment in his ability to recall something and recognition skills. Then
magnetic imaging tests were performed to see any abnormalities in the brain. Atrophy
and tissue breakdown were noticed in the medial temporal lobe and the cortes. These
were recognised as a sign of onset of dementia. In the next PET imaging test, the
presence of amyloid deposition was revealed. The above symptoms and reports from
tests suggested the onset of Alzheimer's.
Key symptoms associated with the diagnosis
The diagnosis was strengthened by the tissue breakdown noticed in the brain. However,
there were presence other physical symptoms that made the doctors run the specific
tests upon Sam. Even though Sam was able to keep his speech and verbal skills intact
he had problem in identifying people and even places that he had frequented before.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Master in Health Care
His eyesight has degraded drastically and he often needed to see ophthalmologist
frequently. This was one of the reasons why his family asked to consult a neurologist.
Also, the physician opted for a scan or imaging test because it clearly hinted upon
tissue degradation in the brain which can be a reason for his failing eyesight. He was
also asked to present his as well as his patient history to see some congenital patterns
that has been prevalent in their genes. However, no such experience was seen in their
family history. The neuropsychological test was run when it was seen that the physical
symptoms were common to many other mental problems. These tests assess the
activity of the brain and is able to provide an accurate diagnosis.
Bio-psycho-social formulation
Biopsychosocial formulation is a technique through which physicians gain approach an
understanding of the patient’s condition by taking into account their biological,
psychological and social perspectives of the patient’s current situation (Frisoni et al.
2017). The biological factors include genetic and developmental factors that have
shaped Sam’s life. He lived a normal life until 3 years ago when he complained of a
psychological decline. He has never experienced such a situation in his developmental
years and was always able to manage himself. There is no report of drug or alcohol
addiction that may have explained his forgetfulness and imbalanced state. He has been
facing sleep disruption which is interfering with his daily schedule. He is also unable to
use any technology like the computer software used to make calculations in his
profession and cannot drive a car. Any activity that needs Sam to perform multiple
activities and be accountable for multiple results appears to be a great task to him.
The psychological factors include Sam’s cognitive style, his conflicts, self-image and
interpretation of the symptoms (Dubois et al. 2016). Sam finds himself to be confused
and struggling to manage things all the time. He also feels tired and unable to
concentrate on things that were once easy for him. He has been very focused on trying
to adapt and manage to these changes that seeking a doctor for help did not even occur
to him. It was his family who asked him to consult someone for his failing eyesight,
which eventually led him to seek out a neurologist. His bewildered and puzzled state
makes him very vulnerable. In one such episode when Sam was roaming two blocks
away from his home because he was unable to recognise the place and find his way
back home. He also cannot be trusted to drive or use heavy machinery and kitchen
wares. Sam lives a lonely life, as a result, he has many online acquaintances. This
could also be seen as a risk as he is susceptible to being scammed for money or
personal information (Liu et al. 2015). Since he was a key part of the research team, he
is also privy to some key data that makes him a target for other competitors trying to get
ahead in their research process. Sam being unable to recognise people sometimes
latches on to unknown people and believes them to be his acquaintances. The rejection
he faces is traumatic for him and he feels lonelier than he ever was. His family has
asked him to live with them, but he is adamant on trying to maintain his independent life.
Master in Health Care
His eyesight has degraded drastically and he often needed to see ophthalmologist
frequently. This was one of the reasons why his family asked to consult a neurologist.
Also, the physician opted for a scan or imaging test because it clearly hinted upon
tissue degradation in the brain which can be a reason for his failing eyesight. He was
also asked to present his as well as his patient history to see some congenital patterns
that has been prevalent in their genes. However, no such experience was seen in their
family history. The neuropsychological test was run when it was seen that the physical
symptoms were common to many other mental problems. These tests assess the
activity of the brain and is able to provide an accurate diagnosis.
Bio-psycho-social formulation
Biopsychosocial formulation is a technique through which physicians gain approach an
understanding of the patient’s condition by taking into account their biological,
psychological and social perspectives of the patient’s current situation (Frisoni et al.
2017). The biological factors include genetic and developmental factors that have
shaped Sam’s life. He lived a normal life until 3 years ago when he complained of a
psychological decline. He has never experienced such a situation in his developmental
years and was always able to manage himself. There is no report of drug or alcohol
addiction that may have explained his forgetfulness and imbalanced state. He has been
facing sleep disruption which is interfering with his daily schedule. He is also unable to
use any technology like the computer software used to make calculations in his
profession and cannot drive a car. Any activity that needs Sam to perform multiple
activities and be accountable for multiple results appears to be a great task to him.
The psychological factors include Sam’s cognitive style, his conflicts, self-image and
interpretation of the symptoms (Dubois et al. 2016). Sam finds himself to be confused
and struggling to manage things all the time. He also feels tired and unable to
concentrate on things that were once easy for him. He has been very focused on trying
to adapt and manage to these changes that seeking a doctor for help did not even occur
to him. It was his family who asked him to consult someone for his failing eyesight,
which eventually led him to seek out a neurologist. His bewildered and puzzled state
makes him very vulnerable. In one such episode when Sam was roaming two blocks
away from his home because he was unable to recognise the place and find his way
back home. He also cannot be trusted to drive or use heavy machinery and kitchen
wares. Sam lives a lonely life, as a result, he has many online acquaintances. This
could also be seen as a risk as he is susceptible to being scammed for money or
personal information (Liu et al. 2015). Since he was a key part of the research team, he
is also privy to some key data that makes him a target for other competitors trying to get
ahead in their research process. Sam being unable to recognise people sometimes
latches on to unknown people and believes them to be his acquaintances. The rejection
he faces is traumatic for him and he feels lonelier than he ever was. His family has
asked him to live with them, but he is adamant on trying to maintain his independent life.
3
Master in Health Care
The social perspective of his life accounts for the social relationships he has with
people. As mentioned earlier, Sam has always led a lonely life as he was too focused
with work. His most acquaintances were either common family friends or his co-
workers, He was described to be amiable and easy-going (Olsson et al. 2016). He
attended social events whenever called to them but did not show particular interest in
them or initiated them. Sam was very focused on his research and finding a
breakthrough in it. He was unable to come to terms with the loss of his position as a
researcher but tried to adapt to his new role as a manager. However, that role also
proved to be unfit. After leaving the job, his connection to the outer world was cut. He
felt lonely, rejected and separated.
Describe the ideal evidence-based treatment
Sam was diagnosed with early onset Alzheimer’s given his symptoms were mostly
similar to those of dementia. He was admitted to the psychiatric ward and was left after
ten days of stay. The physicians believed that his treatment will focus on a way to stop
the decline of his symptoms and to preserve his psychological and cognitive ability. He
was given a 5mg of donepezil. However, the dose was increased to 23mg when it was
seen that the symptoms were still continuously declining (Liu et al. 2015). The dose was
combined with 20mg of memantine. After this the symptoms and the decline in his
ability was slowed down. They asked Sam to accept the help of care provider who
would help him to manage his activities and also keep tabs on his condition. His mother
accepted the role of his care provider and Sam moved into their home. They were
requested to make monthly visits to the clinic to ensure that his condition did not decline
further.
Donepezil is used to treat symptoms of confusion, forgetfulness and other issues that
collectively defined as dementia (Ismail et al. 2016). There is no absolute cure to
Alzheimer’s and dementia symptoms can only be decreased in their intensity to prolong
the period of time Sam is able to maintain his cognitive skills for. The drug is an enzyme
blocker that preserves the balance in the brain. Memantine is also a similar drug that
blocks glutamate which is believed to be associated with dementia symptoms. The use
of these drugs often has some side effects like dizziness, constipation, headaches and
confusion (Viola & Klein, 2015). It can also cause hypertension, acute kidney failure and
stroke in extreme cases.
Other than medication, it is essential for Sam to be prepared with what is going to come
next. There is no cure for Alzheimer’s as a result, Sam’s condition is eventually going to
decline and he has to be able to accept and adapt to it (Vossel et al. 2016). The main
aim would be to ensure the quality of life to Sam and allows him to be as independent
as possible. He needs to be protected because of his vulnerable state and ensure his
body dignity and ability to consent is maintained.
It is often seen that due to lack of social stimulus, patients with dementia often fall prey
to depression or other psychological disorders (Barnes et al. 2015). It has been noted
that there is a connection between brain activity with mood of a person which further
Master in Health Care
The social perspective of his life accounts for the social relationships he has with
people. As mentioned earlier, Sam has always led a lonely life as he was too focused
with work. His most acquaintances were either common family friends or his co-
workers, He was described to be amiable and easy-going (Olsson et al. 2016). He
attended social events whenever called to them but did not show particular interest in
them or initiated them. Sam was very focused on his research and finding a
breakthrough in it. He was unable to come to terms with the loss of his position as a
researcher but tried to adapt to his new role as a manager. However, that role also
proved to be unfit. After leaving the job, his connection to the outer world was cut. He
felt lonely, rejected and separated.
Describe the ideal evidence-based treatment
Sam was diagnosed with early onset Alzheimer’s given his symptoms were mostly
similar to those of dementia. He was admitted to the psychiatric ward and was left after
ten days of stay. The physicians believed that his treatment will focus on a way to stop
the decline of his symptoms and to preserve his psychological and cognitive ability. He
was given a 5mg of donepezil. However, the dose was increased to 23mg when it was
seen that the symptoms were still continuously declining (Liu et al. 2015). The dose was
combined with 20mg of memantine. After this the symptoms and the decline in his
ability was slowed down. They asked Sam to accept the help of care provider who
would help him to manage his activities and also keep tabs on his condition. His mother
accepted the role of his care provider and Sam moved into their home. They were
requested to make monthly visits to the clinic to ensure that his condition did not decline
further.
Donepezil is used to treat symptoms of confusion, forgetfulness and other issues that
collectively defined as dementia (Ismail et al. 2016). There is no absolute cure to
Alzheimer’s and dementia symptoms can only be decreased in their intensity to prolong
the period of time Sam is able to maintain his cognitive skills for. The drug is an enzyme
blocker that preserves the balance in the brain. Memantine is also a similar drug that
blocks glutamate which is believed to be associated with dementia symptoms. The use
of these drugs often has some side effects like dizziness, constipation, headaches and
confusion (Viola & Klein, 2015). It can also cause hypertension, acute kidney failure and
stroke in extreme cases.
Other than medication, it is essential for Sam to be prepared with what is going to come
next. There is no cure for Alzheimer’s as a result, Sam’s condition is eventually going to
decline and he has to be able to accept and adapt to it (Vossel et al. 2016). The main
aim would be to ensure the quality of life to Sam and allows him to be as independent
as possible. He needs to be protected because of his vulnerable state and ensure his
body dignity and ability to consent is maintained.
It is often seen that due to lack of social stimulus, patients with dementia often fall prey
to depression or other psychological disorders (Barnes et al. 2015). It has been noted
that there is a connection between brain activity with mood of a person which further
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
Master in Health Care
dependent on the events and situations in his life. As a result, Sam’s treatment
approach needs to be included more treatment approaches other than just medication.
This may include behavioural therapy where his care provider is responsible for making
events or situations that are pleasurable for him. This would act as an opportunity to
stimulate Sam’s declining cognitive ability and also improve his mood. Research has
provided that these therapies are able to elicit better results than the prescribed
antipsychotic drugs. Moreover, the drugs are also associated with several side effects
which may impact the health condition (Alzheimer's Association, 2016). Often, the
patients hesitate to take such drugs as they feel that they lose their ability to control
their emotions and thoughts.
Care providers are aware that Alzheimer’s syndrome is not associated with
forgetfulness or lack of recognition. It is also followed by episodes of increased anger
and other challenging behaviours. The Progressively Lowered Stress Threshold model
can be used to reduce the occurrences of such events and provide better care and
quality of life to Sam. This model identifies probable stressors and tries to eliminate
them. It is identified that the challenging behaviour is induced by these stressors and
can be controlled if the stressors are eliminated (Cummings et al. 2016). Some
commonly identified stressors can be unmanaged pain or discomfort that Sam cannot
verbalise. Hunger, fatigue and feelings or failure, loneliness or unmet urges for love,
attention, friendship, purpose or success can also make a person restless. Since, they
are likely to be unable to communicate their feelings or their needs, it comes out in the
form of aggression or irritation.
Another treatment approach can provide cognitive stimulation to the patient so that they
are provided with an opportunity to use their receding ability (Wang et al. 2015).
However, it is to be ensured that the activity needs to be tailor made to their ability so
that they do not meet with failure. It has to be challenging enough that they are forced to
use their cognitive skills.
Write a collaborative mental health plan which describes
a. Measurable and attainable treatment goals Progression of dementia symptoms-
the first goal of the treatment is to slow down the progression of symptoms so that Sam
is able to maintain his cognitive ability for longer. The progression can be assessed by
running neuropsychological test. The tests can be run every 4 months and the desired
outcome can be seen after 2 months of regular doses (Rosenberg, Newgrange &
Lyketsos, 2015).
● Manage the side effects of the drugs- the Donepezil and Memantine are
associated with side effects like constipation, backache, headache and
sleepiness. This makes him more uncomfortable and also hesitant to take
medications (Winblad et al. 2016). The side effects noticed in the first month can
be managed through other medication and behavioural changes.
● Behavioural symptoms of Alzheimer’s- the drugs can work so much to reduce
the discomfort of an Alzheimer’s patient. However, Sam may still face difficulty in
Master in Health Care
dependent on the events and situations in his life. As a result, Sam’s treatment
approach needs to be included more treatment approaches other than just medication.
This may include behavioural therapy where his care provider is responsible for making
events or situations that are pleasurable for him. This would act as an opportunity to
stimulate Sam’s declining cognitive ability and also improve his mood. Research has
provided that these therapies are able to elicit better results than the prescribed
antipsychotic drugs. Moreover, the drugs are also associated with several side effects
which may impact the health condition (Alzheimer's Association, 2016). Often, the
patients hesitate to take such drugs as they feel that they lose their ability to control
their emotions and thoughts.
Care providers are aware that Alzheimer’s syndrome is not associated with
forgetfulness or lack of recognition. It is also followed by episodes of increased anger
and other challenging behaviours. The Progressively Lowered Stress Threshold model
can be used to reduce the occurrences of such events and provide better care and
quality of life to Sam. This model identifies probable stressors and tries to eliminate
them. It is identified that the challenging behaviour is induced by these stressors and
can be controlled if the stressors are eliminated (Cummings et al. 2016). Some
commonly identified stressors can be unmanaged pain or discomfort that Sam cannot
verbalise. Hunger, fatigue and feelings or failure, loneliness or unmet urges for love,
attention, friendship, purpose or success can also make a person restless. Since, they
are likely to be unable to communicate their feelings or their needs, it comes out in the
form of aggression or irritation.
Another treatment approach can provide cognitive stimulation to the patient so that they
are provided with an opportunity to use their receding ability (Wang et al. 2015).
However, it is to be ensured that the activity needs to be tailor made to their ability so
that they do not meet with failure. It has to be challenging enough that they are forced to
use their cognitive skills.
Write a collaborative mental health plan which describes
a. Measurable and attainable treatment goals Progression of dementia symptoms-
the first goal of the treatment is to slow down the progression of symptoms so that Sam
is able to maintain his cognitive ability for longer. The progression can be assessed by
running neuropsychological test. The tests can be run every 4 months and the desired
outcome can be seen after 2 months of regular doses (Rosenberg, Newgrange &
Lyketsos, 2015).
● Manage the side effects of the drugs- the Donepezil and Memantine are
associated with side effects like constipation, backache, headache and
sleepiness. This makes him more uncomfortable and also hesitant to take
medications (Winblad et al. 2016). The side effects noticed in the first month can
be managed through other medication and behavioural changes.
● Behavioural symptoms of Alzheimer’s- the drugs can work so much to reduce
the discomfort of an Alzheimer’s patient. However, Sam may still face difficulty in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Master in Health Care
communicating and managing his thoughts. He would not be able to focus on his
environment which may put him in vulnerable situations. It is essential to control
these behaviours through behavioural therapy (Zhao et al. 2016).
● Educating family members- Sam’s family will also have to adapt as Sam grows
heavily dependent on them. They would have to be aware of the stressors which
are likely to make him agitated. Moreover, there will be times when he feels
lonely and depressed (Hampel et al.2016). His family is required to emotionally
stimulate him and reserve his quality of life.
b. Recommended treatment (specify what treatment and by whom)
According to the National Institute of Ageing, Alzheimer’s is a complex disease, which
cannot be eliminated through the use of one particular drug. However, the drugs work
best when people are diagnosed at an early stage where Alzheimer’s is still on its onset.
As is seen in Sam’s case, he is still has maintained his speech skills which shows that
his condition is still not extreme. It is hoped that antipsychotic drugs are likely to be
effective and bring the required results (Knez et al. 2018).
The drugs prescribed to Sam are basically cholinesterase inhibitors that are able to
manage mild or moderate symptoms of Alzheimer’s. It is still unclear how these
inhibitors manage to suppress the symptoms. In Alzheimer’s the quantity of
acetylcholine is reduced more and more which causes the symptoms to degrade. The
cholinesterase inhibitors suppress the breakdown of these substances thus prolonging
the onset of the symptoms (Schmidt & Areberg, 2016). However, it is not able to provide
complete resolution.
There are three drugs that are prescribed: galantamine, rivastigmine and donepezil.
There is no research that compares the effect of these drugs and no such differences
have been noticed. However, it has been seen that some patients are likely to respond
to some drugs more than others (Kalaria, 2016). Also, the associated symptoms can be
less in one that the others. As Sam’s condition was not relieved by the use of donepezil,
he was also given memantine which is used to manage more severe symptoms. Sam
also needs to be given sleep aids such as zolpidem or zaleplon (Triccoet al. 2018).
These need to be administered with care and only when absolutely necessary. It is
advised that Sam care provider is kept responsible for storing and giving the doses.
c. Self-help / self-care activities
The care providers are required to engage Sam more and more into the care regime.
They are required to gain Sam’s consent before every treatment. They are required to
ensure that Sam is focused on his own self as well. He needs to establish a schedule or
routine which is supposed to bring order in his life. This will also make him more
comfortable and reduce the stressors (Schroeder, Joly-Amado, Gordon & Morgan,
2016). Exercise is essential to maintain bodily functions and also provide as a way to
ease out the energy. Sam may also indulge in mental stimulation like meditation or
yoga. He may take classes which will also add an activity to improve his quality of life.
d. Community resources the person may access to assist them
Master in Health Care
communicating and managing his thoughts. He would not be able to focus on his
environment which may put him in vulnerable situations. It is essential to control
these behaviours through behavioural therapy (Zhao et al. 2016).
● Educating family members- Sam’s family will also have to adapt as Sam grows
heavily dependent on them. They would have to be aware of the stressors which
are likely to make him agitated. Moreover, there will be times when he feels
lonely and depressed (Hampel et al.2016). His family is required to emotionally
stimulate him and reserve his quality of life.
b. Recommended treatment (specify what treatment and by whom)
According to the National Institute of Ageing, Alzheimer’s is a complex disease, which
cannot be eliminated through the use of one particular drug. However, the drugs work
best when people are diagnosed at an early stage where Alzheimer’s is still on its onset.
As is seen in Sam’s case, he is still has maintained his speech skills which shows that
his condition is still not extreme. It is hoped that antipsychotic drugs are likely to be
effective and bring the required results (Knez et al. 2018).
The drugs prescribed to Sam are basically cholinesterase inhibitors that are able to
manage mild or moderate symptoms of Alzheimer’s. It is still unclear how these
inhibitors manage to suppress the symptoms. In Alzheimer’s the quantity of
acetylcholine is reduced more and more which causes the symptoms to degrade. The
cholinesterase inhibitors suppress the breakdown of these substances thus prolonging
the onset of the symptoms (Schmidt & Areberg, 2016). However, it is not able to provide
complete resolution.
There are three drugs that are prescribed: galantamine, rivastigmine and donepezil.
There is no research that compares the effect of these drugs and no such differences
have been noticed. However, it has been seen that some patients are likely to respond
to some drugs more than others (Kalaria, 2016). Also, the associated symptoms can be
less in one that the others. As Sam’s condition was not relieved by the use of donepezil,
he was also given memantine which is used to manage more severe symptoms. Sam
also needs to be given sleep aids such as zolpidem or zaleplon (Triccoet al. 2018).
These need to be administered with care and only when absolutely necessary. It is
advised that Sam care provider is kept responsible for storing and giving the doses.
c. Self-help / self-care activities
The care providers are required to engage Sam more and more into the care regime.
They are required to gain Sam’s consent before every treatment. They are required to
ensure that Sam is focused on his own self as well. He needs to establish a schedule or
routine which is supposed to bring order in his life. This will also make him more
comfortable and reduce the stressors (Schroeder, Joly-Amado, Gordon & Morgan,
2016). Exercise is essential to maintain bodily functions and also provide as a way to
ease out the energy. Sam may also indulge in mental stimulation like meditation or
yoga. He may take classes which will also add an activity to improve his quality of life.
d. Community resources the person may access to assist them
6
Master in Health Care
Community resources may include easy access to facilities like medical care,
ambulance, food services, and other emergency services. Many communities often
have associations where people with dementia and Alzheimer’s can attend classes and
activities. The community gym can also include a secured section and separate slots for
people with dementia (Zheng, Fridkin & Youdim, 2015). The association or self-help
groups have a helpline number that can help them access immediate care. There is
also library section where people like Sam can indulge in some reading exercises that
are stimulating and within their level of competence.
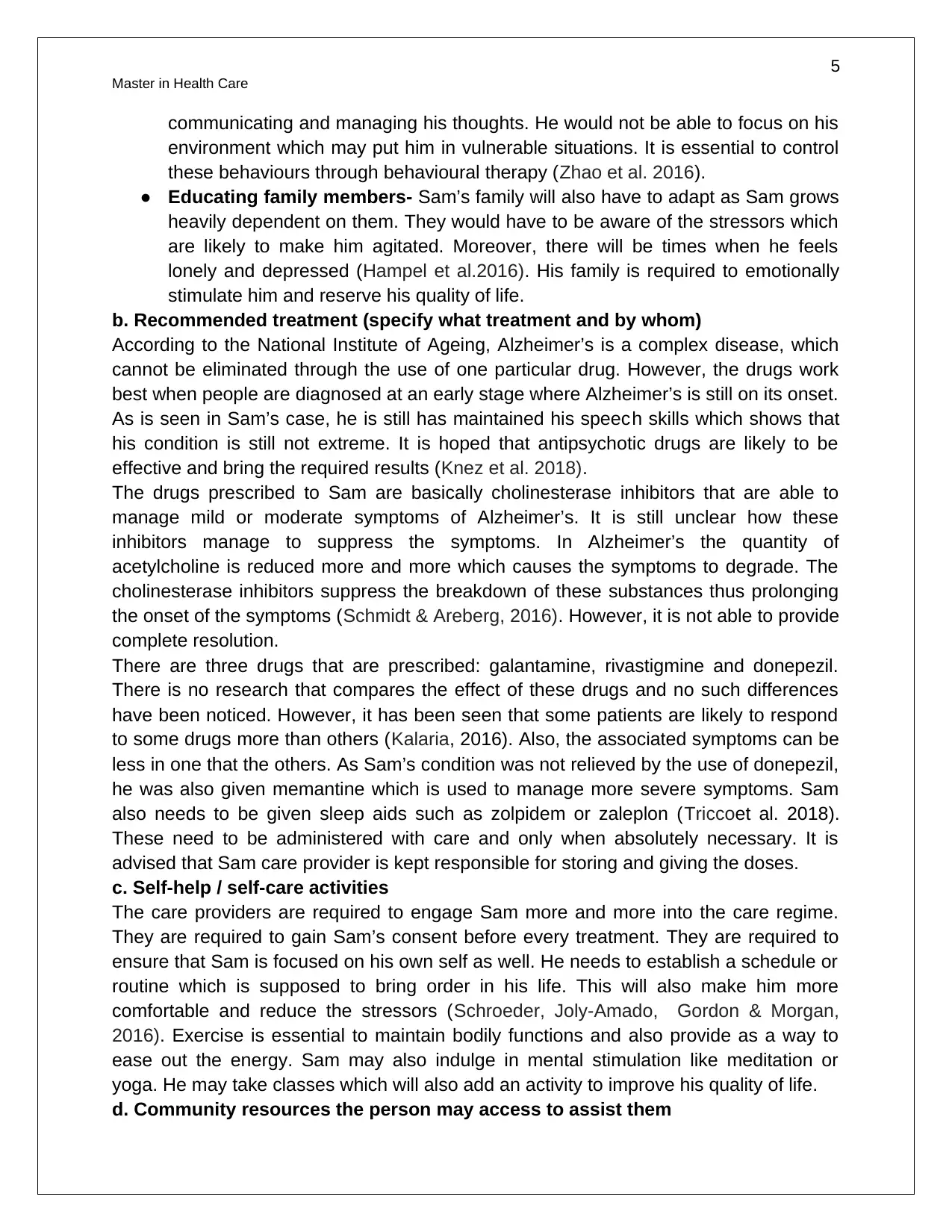
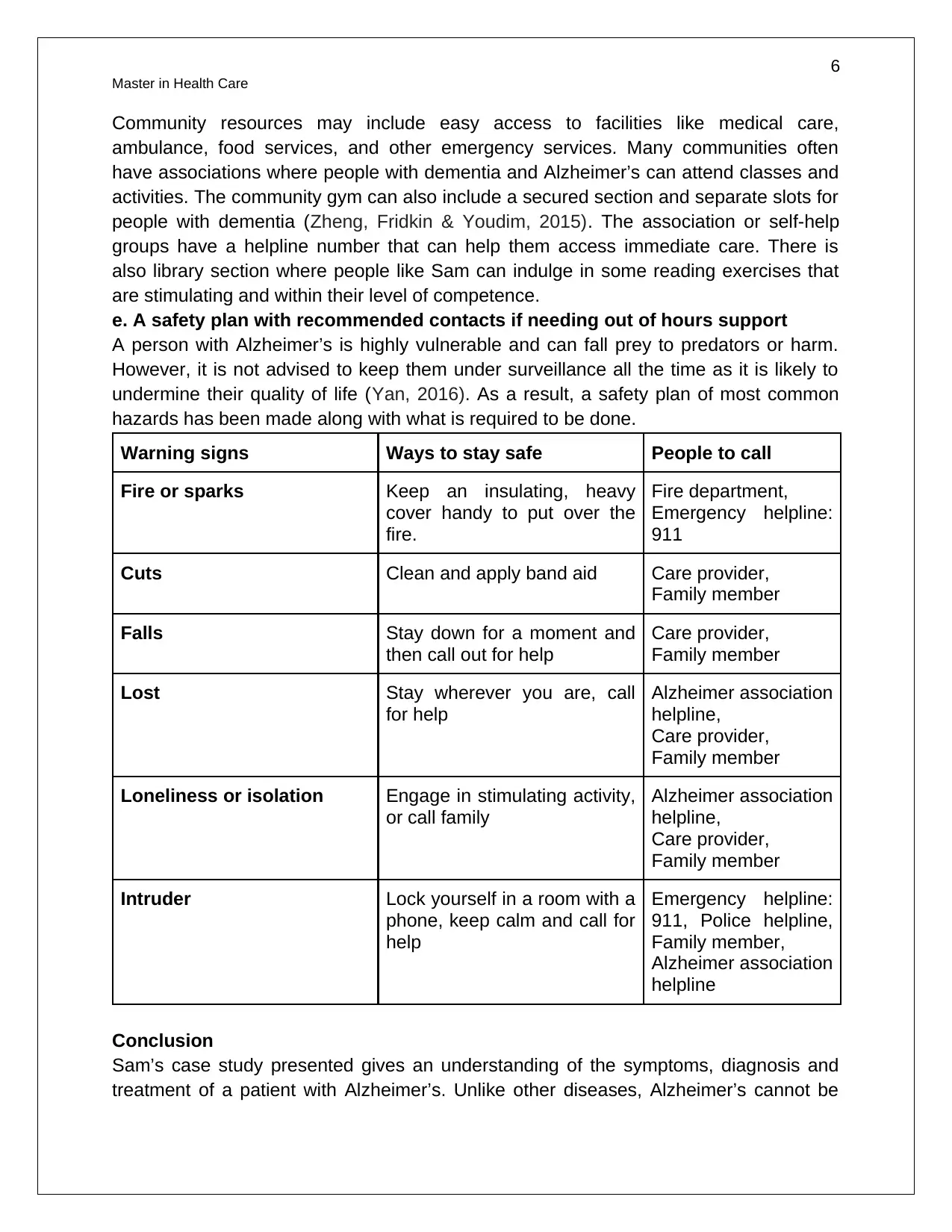
e. A safety plan with recommended contacts if needing out of hours support
A person with Alzheimer’s is highly vulnerable and can fall prey to predators or harm.
However, it is not advised to keep them under surveillance all the time as it is likely to
undermine their quality of life (Yan, 2016). As a result, a safety plan of most common
hazards has been made along with what is required to be done.
Warning signs Ways to stay safe People to call
Fire or sparks Keep an insulating, heavy
cover handy to put over the
fire.
Fire department,
Emergency helpline:
911
Cuts Clean and apply band aid Care provider,
Family member
Falls Stay down for a moment and
then call out for help
Care provider,
Family member
Lost Stay wherever you are, call
for help
Alzheimer association
helpline,
Care provider,
Family member
Loneliness or isolation Engage in stimulating activity,
or call family
Alzheimer association
helpline,
Care provider,
Family member
Intruder Lock yourself in a room with a
phone, keep calm and call for
help
Emergency helpline:
911, Police helpline,
Family member,
Alzheimer association
helpline
Conclusion
Sam’s case study presented gives an understanding of the symptoms, diagnosis and
treatment of a patient with Alzheimer’s. Unlike other diseases, Alzheimer’s cannot be
Master in Health Care
Community resources may include easy access to facilities like medical care,
ambulance, food services, and other emergency services. Many communities often
have associations where people with dementia and Alzheimer’s can attend classes and
activities. The community gym can also include a secured section and separate slots for
people with dementia (Zheng, Fridkin & Youdim, 2015). The association or self-help
groups have a helpline number that can help them access immediate care. There is
also library section where people like Sam can indulge in some reading exercises that
are stimulating and within their level of competence.
e. A safety plan with recommended contacts if needing out of hours support
A person with Alzheimer’s is highly vulnerable and can fall prey to predators or harm.
However, it is not advised to keep them under surveillance all the time as it is likely to
undermine their quality of life (Yan, 2016). As a result, a safety plan of most common
hazards has been made along with what is required to be done.
Warning signs Ways to stay safe People to call
Fire or sparks Keep an insulating, heavy
cover handy to put over the
fire.
Fire department,
Emergency helpline:
911
Cuts Clean and apply band aid Care provider,
Family member
Falls Stay down for a moment and
then call out for help
Care provider,
Family member
Lost Stay wherever you are, call
for help
Alzheimer association
helpline,
Care provider,
Family member
Loneliness or isolation Engage in stimulating activity,
or call family
Alzheimer association
helpline,
Care provider,
Family member
Intruder Lock yourself in a room with a
phone, keep calm and call for
help
Emergency helpline:
911, Police helpline,
Family member,
Alzheimer association
helpline
Conclusion
Sam’s case study presented gives an understanding of the symptoms, diagnosis and
treatment of a patient with Alzheimer’s. Unlike other diseases, Alzheimer’s cannot be
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
Master in Health Care
completely treated. The symptoms are likely to progress at a particular rate, even
medication is administered. As a result, it requires behavioural and lifestyle changes.
Also, the patient needs to adapt and come to terms with his condition. It is likely to bring
emotional pain, trauma and a feeling of separation. Patients need to be supported by
their family members during this time so that they are able to relieve their pain. The
treatment approach chosen for Sam is most suitable for his condition and has been
provided after proper assessment.
Master in Health Care
completely treated. The symptoms are likely to progress at a particular rate, even
medication is administered. As a result, it requires behavioural and lifestyle changes.
Also, the patient needs to adapt and come to terms with his condition. It is likely to bring
emotional pain, trauma and a feeling of separation. Patients need to be supported by
their family members during this time so that they are able to relieve their pain. The
treatment approach chosen for Sam is most suitable for his condition and has been
provided after proper assessment.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Master in Health Care
References
Alzheimer’s, A. (2015). 2015 Alzheimer's disease facts and figures. Alzheimer's &
dementia: the journal of the Alzheimer's Association, 11(3), 332.
Alzheimer's Association. (2016). 2016 Alzheimer's disease facts and figures.
Alzheimer's & Dementia, 12(4), 459-509.
Barnes, J., Dickerson, B. C., Frost, C., Jiskoot, L. C., Wolk, D., & van der Flier, W. M.
(2015). Alzheimer's disease first symptoms are age dependent: evidence from
the NACC dataset. Alzheimer's & dementia, 11(11), 1349-1357.
Cummings, J., Lai, T. J., Hemrungrojn, S., Mohandas, E., Yun Kim, S., Nair, G., &
Dash, A. (2016). Role of donepezil in the management of neuropsychiatric
symptoms in Alzheimer's disease and dementia with Lewy bodies. CNS
neuroscience & therapeutics, 22(3), 159-166.
Dubois, B., Padovani, A., Scheltens, P., Rossi, A., & Dell’Agnello, G. (2016). Timely
diagnosis for Alzheimer’s disease: a literature review on benefits and challenges.
Journal of Alzheimer's disease, 49(3), 617-631.
Frisoni, G. B., Boccardi, M., Barkhof, F., Blennow, K., Cappa, S., Chiotis, K., ... &
Hansson, O. (2017). Strategic roadmap for an early diagnosis of Alzheimer's
disease based on biomarkers. The Lancet Neurology, 16(8), 661-676.
Hampel, H. O. B. S., O’Bryant, S. E., Castrillo, J. I., Ritchie, C., Rojkova, K., Broich,
K., ... & Escott-Price, V. (2016). PRECISION MEDICINE-the golden gate for
detection, treatment and prevention of Alzheimer’s disease. The journal of
prevention of Alzheimer's disease, 3(4), 243.
Ismail, Z., Smith, E. E., Geda, Y., Sultzer, D., Brodaty, H., Smith, G., ... & Area, I. N. S.
P. I. (2016). Neuropsychiatric symptoms as early manifestations of emergent
dementia: provisional diagnostic criteria for mild behavioral impairment.
Alzheimer's & Dementia, 12(2), 195-202.
Kalaria, R. N. (2016). Neuropathological diagnosis of vascular cognitive impairment and
vascular dementia with implications for Alzheimer’s disease. Acta
neuropathologica, 131(5), 659-685.
Knez, D., Coquelle, N., Pišlar, A., Žakelj, S., Jukič, M., Sova, M., ... & Colletier, J. P.
(2018). Multi-target-directed ligands for treating Alzheimer's disease:
Butyrylcholinesterase inhibitors displaying antioxidant and neuroprotective
activities. European journal of medicinal chemistry, 156, 598-617.
Master in Health Care
References
Alzheimer’s, A. (2015). 2015 Alzheimer's disease facts and figures. Alzheimer's &
dementia: the journal of the Alzheimer's Association, 11(3), 332.
Alzheimer's Association. (2016). 2016 Alzheimer's disease facts and figures.
Alzheimer's & Dementia, 12(4), 459-509.
Barnes, J., Dickerson, B. C., Frost, C., Jiskoot, L. C., Wolk, D., & van der Flier, W. M.
(2015). Alzheimer's disease first symptoms are age dependent: evidence from
the NACC dataset. Alzheimer's & dementia, 11(11), 1349-1357.
Cummings, J., Lai, T. J., Hemrungrojn, S., Mohandas, E., Yun Kim, S., Nair, G., &
Dash, A. (2016). Role of donepezil in the management of neuropsychiatric
symptoms in Alzheimer's disease and dementia with Lewy bodies. CNS
neuroscience & therapeutics, 22(3), 159-166.
Dubois, B., Padovani, A., Scheltens, P., Rossi, A., & Dell’Agnello, G. (2016). Timely
diagnosis for Alzheimer’s disease: a literature review on benefits and challenges.
Journal of Alzheimer's disease, 49(3), 617-631.
Frisoni, G. B., Boccardi, M., Barkhof, F., Blennow, K., Cappa, S., Chiotis, K., ... &
Hansson, O. (2017). Strategic roadmap for an early diagnosis of Alzheimer's
disease based on biomarkers. The Lancet Neurology, 16(8), 661-676.
Hampel, H. O. B. S., O’Bryant, S. E., Castrillo, J. I., Ritchie, C., Rojkova, K., Broich,
K., ... & Escott-Price, V. (2016). PRECISION MEDICINE-the golden gate for
detection, treatment and prevention of Alzheimer’s disease. The journal of
prevention of Alzheimer's disease, 3(4), 243.
Ismail, Z., Smith, E. E., Geda, Y., Sultzer, D., Brodaty, H., Smith, G., ... & Area, I. N. S.
P. I. (2016). Neuropsychiatric symptoms as early manifestations of emergent
dementia: provisional diagnostic criteria for mild behavioral impairment.
Alzheimer's & Dementia, 12(2), 195-202.
Kalaria, R. N. (2016). Neuropathological diagnosis of vascular cognitive impairment and
vascular dementia with implications for Alzheimer’s disease. Acta
neuropathologica, 131(5), 659-685.
Knez, D., Coquelle, N., Pišlar, A., Žakelj, S., Jukič, M., Sova, M., ... & Colletier, J. P.
(2018). Multi-target-directed ligands for treating Alzheimer's disease:
Butyrylcholinesterase inhibitors displaying antioxidant and neuroprotective
activities. European journal of medicinal chemistry, 156, 598-617.
9
Master in Health Care
Liu, M., Zhang, D., Shen, D., & Alzheimer's Disease Neuroimaging Initiative. (2015).
View‐centralized multi‐atlas classification for Alzheimer's disease diagnosis.
Human brain mapping, 36(5), 1847-1865.
Liu, X., Hao, W., Qin, Y., Decker, Y., Wang, X., Burkart, M., ... & Liu, Y. (2015). Long-
term treatment with Ginkgo biloba extract EGb 761 improves symptoms and
pathology in a transgenic mouse model of Alzheimer’s disease. Brain, behavior,
and immunity, 46, 121-131.
Olsson, B., Lautner, R., Andreasson, U., Öhrfelt, A., Portelius, E., Bjerke, M., ... & Wu,
E. (2016). CSF and blood biomarkers for the diagnosis of Alzheimer's disease: a
systematic review and meta-analysis. The Lancet Neurology, 15(7), 673-684.
Rosenberg, P. B., Nowrangi, M. A., & Lyketsos, C. G. (2015). Neuropsychiatric
symptoms in Alzheimer's disease: what might be associated brain circuits?.
Molecular aspects of medicine, 43, 25-37.
Schmidt, E., & Areberg, J. (2016). U.S. Patent No. 9,375,418. Washington, DC: U.S.
Patent and Trademark Office.
Schroeder, S. K., Joly-Amado, A., Gordon, M. N., & Morgan, D. (2016). Tau-directed
immunotherapy: a promising strategy for treating Alzheimer’s disease and other
tauopathies. Journal of neuroimmune pharmacology, 11(1), 9-25.
Tricco, A. C., Ashoor, H. M., Soobiah, C., Rios, P., Veroniki, A. A., Hamid, J. S., ... &
Blondal, E. (2018). Comparative effectiveness and safety of cognitive enhancers
for treating Alzheimer's disease: systematic review and network metaanalysis.
Journal of the American Geriatrics Society, 66(1), 170-178.
Viola, K. L., & Klein, W. L. (2015). Amyloid β oligomers in Alzheimer’s disease
pathogenesis, treatment, and diagnosis. Acta neuropathologica, 129(2), 183-206.
Vossel, K. A., Ranasinghe, K. G., Beagle, A. J., Mizuiri, D., Honma, S. M., Dowling, A.
F., ... & Karydas, A. M. (2016). Incidence and impact of subclinical epileptiform
activity in Alzheimer's disease. Annals of neurology, 80(6), 858-870.
Wang, J., Yu, J. T., Wang, H. F., Meng, X. F., Wang, C., Tan, C. C., & Tan, L. (2015).
Pharmacological treatment of neuropsychiatric symptoms in Alzheimer's disease:
a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry, 86(1),
101-109.
Winblad, B., Amouyel, P., Andrieu, S., Ballard, C., Brayne, C., Brodaty, H., ... &
Fratiglioni, L. (2016). Defeating Alzheimer's disease and other dementias: a
priority for European science and society. The Lancet Neurology, 15(5), 455-532.
Yan, R. (2016). Stepping closer to treating Alzheimer’s disease patients with BACE1
inhibitor drugs. Translational neurodegeneration, 5(1), 13.
Zhao, Q. F., Tan, L., Wang, H. F., Jiang, T., Tan, M. S., Tan, L., ... & Yu, J. T. (2016).
The prevalence of neuropsychiatric symptoms in Alzheimer's disease: systematic
review and meta-analysis. Journal of affective disorders, 190, 264-271.
Zheng, H., Fridkin, M., & Youdim, M. (2015). New approaches to treating Alzheimer's
disease. Perspectives in medicinal chemistry, 7, PMC-S13210.
Master in Health Care
Liu, M., Zhang, D., Shen, D., & Alzheimer's Disease Neuroimaging Initiative. (2015).
View‐centralized multi‐atlas classification for Alzheimer's disease diagnosis.
Human brain mapping, 36(5), 1847-1865.
Liu, X., Hao, W., Qin, Y., Decker, Y., Wang, X., Burkart, M., ... & Liu, Y. (2015). Long-
term treatment with Ginkgo biloba extract EGb 761 improves symptoms and
pathology in a transgenic mouse model of Alzheimer’s disease. Brain, behavior,
and immunity, 46, 121-131.
Olsson, B., Lautner, R., Andreasson, U., Öhrfelt, A., Portelius, E., Bjerke, M., ... & Wu,
E. (2016). CSF and blood biomarkers for the diagnosis of Alzheimer's disease: a
systematic review and meta-analysis. The Lancet Neurology, 15(7), 673-684.
Rosenberg, P. B., Nowrangi, M. A., & Lyketsos, C. G. (2015). Neuropsychiatric
symptoms in Alzheimer's disease: what might be associated brain circuits?.
Molecular aspects of medicine, 43, 25-37.
Schmidt, E., & Areberg, J. (2016). U.S. Patent No. 9,375,418. Washington, DC: U.S.
Patent and Trademark Office.
Schroeder, S. K., Joly-Amado, A., Gordon, M. N., & Morgan, D. (2016). Tau-directed
immunotherapy: a promising strategy for treating Alzheimer’s disease and other
tauopathies. Journal of neuroimmune pharmacology, 11(1), 9-25.
Tricco, A. C., Ashoor, H. M., Soobiah, C., Rios, P., Veroniki, A. A., Hamid, J. S., ... &
Blondal, E. (2018). Comparative effectiveness and safety of cognitive enhancers
for treating Alzheimer's disease: systematic review and network metaanalysis.
Journal of the American Geriatrics Society, 66(1), 170-178.
Viola, K. L., & Klein, W. L. (2015). Amyloid β oligomers in Alzheimer’s disease
pathogenesis, treatment, and diagnosis. Acta neuropathologica, 129(2), 183-206.
Vossel, K. A., Ranasinghe, K. G., Beagle, A. J., Mizuiri, D., Honma, S. M., Dowling, A.
F., ... & Karydas, A. M. (2016). Incidence and impact of subclinical epileptiform
activity in Alzheimer's disease. Annals of neurology, 80(6), 858-870.
Wang, J., Yu, J. T., Wang, H. F., Meng, X. F., Wang, C., Tan, C. C., & Tan, L. (2015).
Pharmacological treatment of neuropsychiatric symptoms in Alzheimer's disease:
a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry, 86(1),
101-109.
Winblad, B., Amouyel, P., Andrieu, S., Ballard, C., Brayne, C., Brodaty, H., ... &
Fratiglioni, L. (2016). Defeating Alzheimer's disease and other dementias: a
priority for European science and society. The Lancet Neurology, 15(5), 455-532.
Yan, R. (2016). Stepping closer to treating Alzheimer’s disease patients with BACE1
inhibitor drugs. Translational neurodegeneration, 5(1), 13.
Zhao, Q. F., Tan, L., Wang, H. F., Jiang, T., Tan, M. S., Tan, L., ... & Yu, J. T. (2016).
The prevalence of neuropsychiatric symptoms in Alzheimer's disease: systematic
review and meta-analysis. Journal of affective disorders, 190, 264-271.
Zheng, H., Fridkin, M., & Youdim, M. (2015). New approaches to treating Alzheimer's
disease. Perspectives in medicinal chemistry, 7, PMC-S13210.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

