Biological Paradigm in Mental Health: A Comprehensive Overview
VerifiedAdded on 2020/02/24
|10
|2464
|132
Essay
AI Summary
This essay provides a comprehensive overview of the biological paradigm in mental health, examining how biological processes influence the development and treatment of mental illnesses. It begins by defining the biological paradigm and its core tenets, emphasizing the roles of brain chemistry, brain structure, and genetics in shaping behavior. The essay then explores low-prevalence disorders like schizophrenia and psychotic disorders, discussing their impact and the challenges in screening and intervention. It also delves into co-morbidity, examining the co-occurrence of mental health disorders and substance abuse within the framework of the biological paradigm. The essay further discusses various interventions based on this paradigm, including pharmacological treatments and other therapies aimed at altering brain function. Finally, it addresses the concept of recovery, highlighting how the biological paradigm informs strategies to manage depression and promote overall well-being. The essay concludes by summarizing the key points and emphasizing the significance of the biological paradigm in understanding and treating mental health conditions.

Running head: MENTAL HEALTH PRACTICE 1
Mental Health Practice
Name:
Institution:
Mental Health Practice
Name:
Institution:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mental Health Practice 2
Introduction
This paper aims to explain the biological paradigm which is one of the theoretical models
of mental illness. The biological paradigm proposes that the abnormal behavior may arise due to
the changes in the biological processes. These processes are the brain chemistry disparity, the
chaotic growth of the structures of the brain, and heredity. This paradigm holds that the human
behavior and personality are related, and they are discussed based on the structures of the brain,
tendencies in genetics, and the processes in biochemistry (Nusslock, Young & Damme, 2014).
Clearly, this paradigm outlines that the biological makeup of a person determines how best the
human being is understood. Various scholars within the paradigm make some assumptions that
the genes carry the personality traits and the temperament of a human being. The assumptions
impacts how human beings respond to the surrounding and also, the interactions with the other
persons (Gradin, Pérez, MacFarlane, Cavin, Waiter, Engelmann & Steele, 2015). The thinkers
also assume that the hereditary tendencies have the behavioral disparities which are explained
via the changes in some regions such as the neurological functioning and the brain structures. In
simple words, the individual attitudes result in the biochemical and genetic makeup of an
individual. The scholars reveal that the temperamental dispositions are continuous through the
life of an individual. Clearly, the dispositions in the biological paradigm do not have an impact
on the individual personality but they impact the relationship between an individual and other
things. However, the biological paradigm indicates that an individual draws the traits to the
surrounding which reacts accordingly.
Low Prevalence Disorder
Introduction
This paper aims to explain the biological paradigm which is one of the theoretical models
of mental illness. The biological paradigm proposes that the abnormal behavior may arise due to
the changes in the biological processes. These processes are the brain chemistry disparity, the
chaotic growth of the structures of the brain, and heredity. This paradigm holds that the human
behavior and personality are related, and they are discussed based on the structures of the brain,
tendencies in genetics, and the processes in biochemistry (Nusslock, Young & Damme, 2014).
Clearly, this paradigm outlines that the biological makeup of a person determines how best the
human being is understood. Various scholars within the paradigm make some assumptions that
the genes carry the personality traits and the temperament of a human being. The assumptions
impacts how human beings respond to the surrounding and also, the interactions with the other
persons (Gradin, Pérez, MacFarlane, Cavin, Waiter, Engelmann & Steele, 2015). The thinkers
also assume that the hereditary tendencies have the behavioral disparities which are explained
via the changes in some regions such as the neurological functioning and the brain structures. In
simple words, the individual attitudes result in the biochemical and genetic makeup of an
individual. The scholars reveal that the temperamental dispositions are continuous through the
life of an individual. Clearly, the dispositions in the biological paradigm do not have an impact
on the individual personality but they impact the relationship between an individual and other
things. However, the biological paradigm indicates that an individual draws the traits to the
surrounding which reacts accordingly.
Low Prevalence Disorder
Mental Health Practice 3
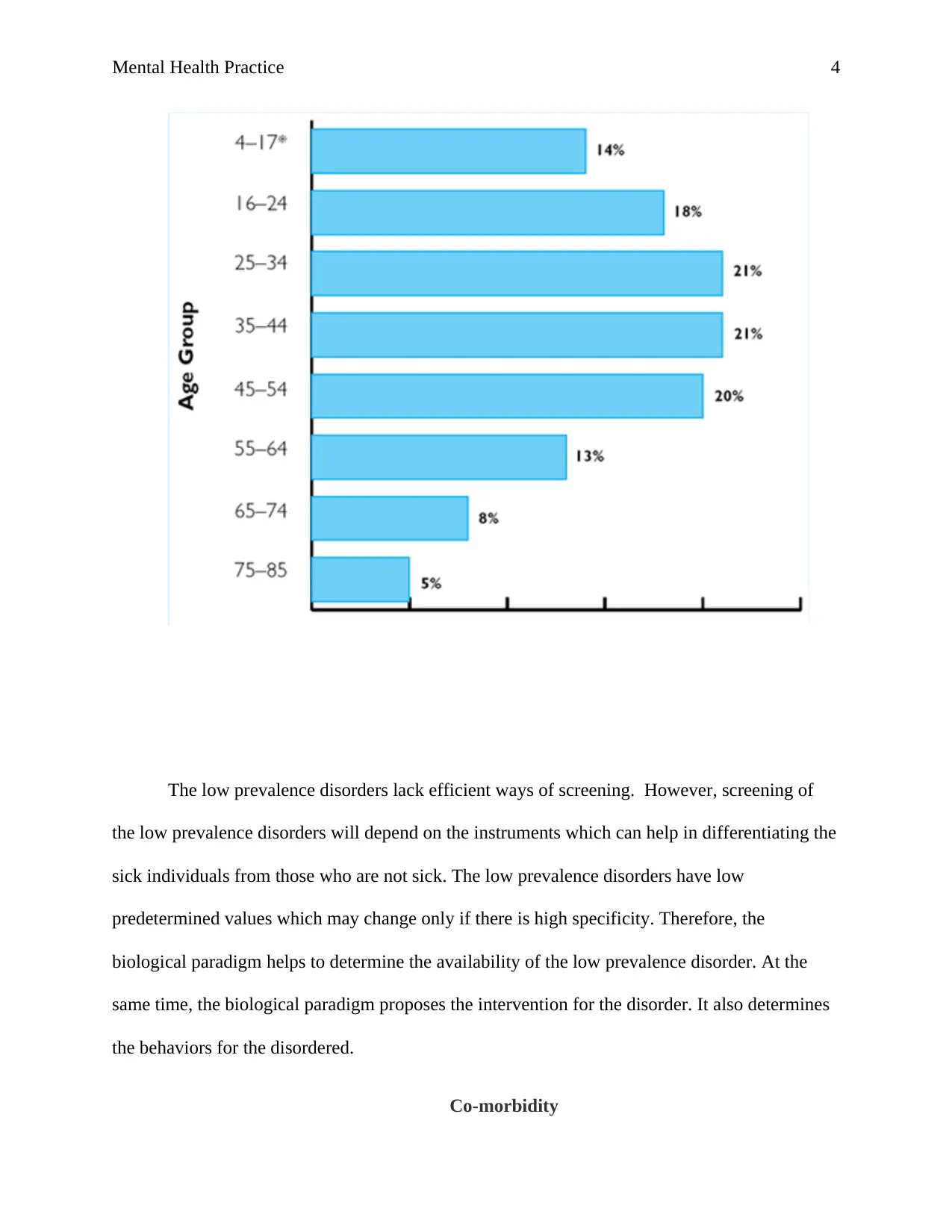
In the case of mental illness, it includes a low prevalence of various disorders. For
example, schizophrenia and the other psychoses impact one to two percent of the adults in the
population who were not part of the ABS survey conducted in 2007. The low prevalence disorder
is not common though the few affected people require services for a long time which causes the
Australian government to spend more in the mental health facilities (Wesseloo, Kamperman,
Munk-Olsen, Pop, Kushner & Bergink, 2015). The low prevalence accounts for around eighty
percent of Australian expenditure. Mental illness depends on the duration, intensity, and the
degree of the disability caused by the disorder. It is evident that fifty percent of the Australians
suffer from the psychotic disorder and Schizophrenia. Mainly, the Schizophrenia and the
psychotic disorders impact the individuals who experience anxiety and depression issues
(Laurens, Luo, Matheson, Carr, Raudino, Harris & Green, 2015). Various studies indicate that
about forty percent prisoners suffer from the psychotic disorder and Schizophrenia. Clearly, the
economic costs are high in many nations since they have to cater for the sick individuals. The
graph below shows the prevalence of the Schizophrenia and psychotic disorders in Australia
based on different ages.
In the case of mental illness, it includes a low prevalence of various disorders. For
example, schizophrenia and the other psychoses impact one to two percent of the adults in the
population who were not part of the ABS survey conducted in 2007. The low prevalence disorder
is not common though the few affected people require services for a long time which causes the
Australian government to spend more in the mental health facilities (Wesseloo, Kamperman,
Munk-Olsen, Pop, Kushner & Bergink, 2015). The low prevalence accounts for around eighty
percent of Australian expenditure. Mental illness depends on the duration, intensity, and the
degree of the disability caused by the disorder. It is evident that fifty percent of the Australians
suffer from the psychotic disorder and Schizophrenia. Mainly, the Schizophrenia and the
psychotic disorders impact the individuals who experience anxiety and depression issues
(Laurens, Luo, Matheson, Carr, Raudino, Harris & Green, 2015). Various studies indicate that
about forty percent prisoners suffer from the psychotic disorder and Schizophrenia. Clearly, the
economic costs are high in many nations since they have to cater for the sick individuals. The
graph below shows the prevalence of the Schizophrenia and psychotic disorders in Australia
based on different ages.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Mental Health Practice 4
The low prevalence disorders lack efficient ways of screening. However, screening of
the low prevalence disorders will depend on the instruments which can help in differentiating the
sick individuals from those who are not sick. The low prevalence disorders have low
predetermined values which may change only if there is high specificity. Therefore, the
biological paradigm helps to determine the availability of the low prevalence disorder. At the
same time, the biological paradigm proposes the intervention for the disorder. It also determines
the behaviors for the disordered.
Co-morbidity
The low prevalence disorders lack efficient ways of screening. However, screening of
the low prevalence disorders will depend on the instruments which can help in differentiating the
sick individuals from those who are not sick. The low prevalence disorders have low
predetermined values which may change only if there is high specificity. Therefore, the
biological paradigm helps to determine the availability of the low prevalence disorder. At the
same time, the biological paradigm proposes the intervention for the disorder. It also determines
the behaviors for the disordered.
Co-morbidity
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mental Health Practice 5
Co-morbid mental health/AOD issues refer to the co-occurrence of a single or several
diseases within a person. Also, it is referred to as the co-occurrence of disorders due to drug use,
or Schizophrenia. Therefore, for this paper, Co-morbidity will be discussed in a broad way under
the biological paradigm in the consideration of mental illness and drug abuse in various ways.
For individuals with low prevalence disorders, for instance, Schizophrenia, they experience
various challenges which impact even their families. Basing on the biological paradigm, the
illnesses co-occur with personalities, drug abuse, affective, and anxiety (Singer, Szalai, Briest,
Brown, Dietz, Einenkel & Löbner, 2013). The co-morbidities are widespread and they have
significant implications on the public health and to the society and people. Co-morbidity occurs
in a different pattern which is viewed by the specialists in mental health. Based on the biological
paradigm, the mental health disorders occur due to several reasons as outlined in this paper. First,
the arbitrary division of illnesses such as anxiety may cause co-morbidity. Other types of drugs
may impact mental illness such as the psychotics, hence increasing the risks associated with the
use of substance disorders. Co-morbidity matters since it is more of a rule and it cannot be
ignored when discussing the mental disorders (Kwako, Schwandt, Sells, Ramchandani, Hommer,
George & Heilig, 2015). Also, the characteristics of an illness under study can be mistaken if the
co-morbidity is ignored. Co-morbidity assists in understanding the co-occurrence hence
respective protection is provided. For instance, the biological paradigm outlines that self-
medication with drugs and alcohol for issues like affective and the anxiety disorders can be
identified through co-morbidity. Individuals suffering from co-morbidity do not respond well to
the treatment and hence the condition may worsen with time. It is evident that the treatment for
issues such as Schizophrenia does not respond effectively. Therefore, co-morbidity correlates
with the biological paradigm and hence it is an important issue to be discussed in this paper.
Co-morbid mental health/AOD issues refer to the co-occurrence of a single or several
diseases within a person. Also, it is referred to as the co-occurrence of disorders due to drug use,
or Schizophrenia. Therefore, for this paper, Co-morbidity will be discussed in a broad way under
the biological paradigm in the consideration of mental illness and drug abuse in various ways.
For individuals with low prevalence disorders, for instance, Schizophrenia, they experience
various challenges which impact even their families. Basing on the biological paradigm, the
illnesses co-occur with personalities, drug abuse, affective, and anxiety (Singer, Szalai, Briest,
Brown, Dietz, Einenkel & Löbner, 2013). The co-morbidities are widespread and they have
significant implications on the public health and to the society and people. Co-morbidity occurs
in a different pattern which is viewed by the specialists in mental health. Based on the biological
paradigm, the mental health disorders occur due to several reasons as outlined in this paper. First,
the arbitrary division of illnesses such as anxiety may cause co-morbidity. Other types of drugs
may impact mental illness such as the psychotics, hence increasing the risks associated with the
use of substance disorders. Co-morbidity matters since it is more of a rule and it cannot be
ignored when discussing the mental disorders (Kwako, Schwandt, Sells, Ramchandani, Hommer,
George & Heilig, 2015). Also, the characteristics of an illness under study can be mistaken if the
co-morbidity is ignored. Co-morbidity assists in understanding the co-occurrence hence
respective protection is provided. For instance, the biological paradigm outlines that self-
medication with drugs and alcohol for issues like affective and the anxiety disorders can be
identified through co-morbidity. Individuals suffering from co-morbidity do not respond well to
the treatment and hence the condition may worsen with time. It is evident that the treatment for
issues such as Schizophrenia does not respond effectively. Therefore, co-morbidity correlates
with the biological paradigm and hence it is an important issue to be discussed in this paper.
Mental Health Practice 6
Interventions
The unusual behavior reflects the biological mechanism as suggested by the biological
paradigm, especially within the brain. The biological paradigm aims to change the brain
psychology. This is because drugs change the synaptic level of the neurotransmitter. Also,
surgery is conducted to eliminate the brain tissues. The seizures are induced to change the
functioning of the brain such as the ECT (Alden, Cucurull-Sanchez, Larminie, Coles, Kullberg,
Evans & Timmis, 2017). Scholars propose that the biological paradigm give an opportunity for
research, a teaching framework, and a design for action in the world of health care. It outlines the
experiments in the animal study, the function of the past, early, and modern life experiences to
change the perception of various diseases in the presence of predisposition in genetics. This
model outlines the family system called the FSGI which deals with the genetic diseases (Lett,
Voineskos, Kennedy, Levine & Daskalakis, 2014). It helps to solve the psychological problems
of the genetic conditions for the families and sick persons. It also offers a biological framework
for clinical research as well as practice. The knowledge in families about the risk of the disorders
may help in minimizing the risks. The biological processes may be incorporated to prevent the
lags in the research behind the technological advances to help individuals the neurobiological
substrate (Butcher, Mineka & Hooley, 2013). The decisions made on how and whether to add the
variables in biology in the research for interventions is determined by the biological
vulnerabilities and the risk factors. The evidence-based interventions are also employed in the
treatment for the mental illness. They include the dialectical behavior therapy which aims to
minimize the tendencies which are not effective based on the clarifications of significant genetic
elements.
Recovery
Interventions
The unusual behavior reflects the biological mechanism as suggested by the biological
paradigm, especially within the brain. The biological paradigm aims to change the brain
psychology. This is because drugs change the synaptic level of the neurotransmitter. Also,
surgery is conducted to eliminate the brain tissues. The seizures are induced to change the
functioning of the brain such as the ECT (Alden, Cucurull-Sanchez, Larminie, Coles, Kullberg,
Evans & Timmis, 2017). Scholars propose that the biological paradigm give an opportunity for
research, a teaching framework, and a design for action in the world of health care. It outlines the
experiments in the animal study, the function of the past, early, and modern life experiences to
change the perception of various diseases in the presence of predisposition in genetics. This
model outlines the family system called the FSGI which deals with the genetic diseases (Lett,
Voineskos, Kennedy, Levine & Daskalakis, 2014). It helps to solve the psychological problems
of the genetic conditions for the families and sick persons. It also offers a biological framework
for clinical research as well as practice. The knowledge in families about the risk of the disorders
may help in minimizing the risks. The biological processes may be incorporated to prevent the
lags in the research behind the technological advances to help individuals the neurobiological
substrate (Butcher, Mineka & Hooley, 2013). The decisions made on how and whether to add the
variables in biology in the research for interventions is determined by the biological
vulnerabilities and the risk factors. The evidence-based interventions are also employed in the
treatment for the mental illness. They include the dialectical behavior therapy which aims to
minimize the tendencies which are not effective based on the clarifications of significant genetic
elements.
Recovery
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Mental Health Practice 7
Based on the biological paradigm, recovery is defined as the individual journey where
hope, security, copings, supportive relationship, as well as meaning, are developed. Therefore, it
involves the growth of purpose and meaning within an individual from the impacts of the mental
disorders. The recovery elements discussed are connectedness, hope, and identity (Bird, 2015).
To start with connectedness, it involves where other people believe in the recovery of other
persons. Therefore, the professionals in mental health may help to foster hope as well as the
relationships established between the family members and friends. Hope is the individual
willingness to persevere challenges (Dopke & Batscha, 2014). Through identity in recovery,
individuals accept themselves and also acquire a sense of belonging. They withstand feelings of
anger and loss. Scholars propose that the biological paradigm helps in recovery since it helps
individuals manage depression within the brain. Through the biological paradigm, Schizophrenia
is connected to genes such as the brain abnormalities which are considered in recovery. It holds
that the human activities are triggered by the activities of the brain. This is because every action
intended by an individual comes from the brain. Therefore, the elements of recovery originate
from the brain.
Conclusion
In conclusion, this paper reviews the biological paradigm and explains the low
prevalence disorder, the co-morbidity in mental health, interventions, and recovery. In the case
of the low prevalence disorder, Schizophrenia and the psychotic disorders are considered. The
biological paradigm outlines that the abnormal behavior occurs due to various reasons. For
instance, if the receptors are less in the postsynaptic neuron membrane the abnormal behavior
may occur. In addition, if there are many neurotransmitters which cause changes in the
transmitter's re-uptake. Co-morbid mental health/AOD issues are discussed in this paper
Based on the biological paradigm, recovery is defined as the individual journey where
hope, security, copings, supportive relationship, as well as meaning, are developed. Therefore, it
involves the growth of purpose and meaning within an individual from the impacts of the mental
disorders. The recovery elements discussed are connectedness, hope, and identity (Bird, 2015).
To start with connectedness, it involves where other people believe in the recovery of other
persons. Therefore, the professionals in mental health may help to foster hope as well as the
relationships established between the family members and friends. Hope is the individual
willingness to persevere challenges (Dopke & Batscha, 2014). Through identity in recovery,
individuals accept themselves and also acquire a sense of belonging. They withstand feelings of
anger and loss. Scholars propose that the biological paradigm helps in recovery since it helps
individuals manage depression within the brain. Through the biological paradigm, Schizophrenia
is connected to genes such as the brain abnormalities which are considered in recovery. It holds
that the human activities are triggered by the activities of the brain. This is because every action
intended by an individual comes from the brain. Therefore, the elements of recovery originate
from the brain.
Conclusion
In conclusion, this paper reviews the biological paradigm and explains the low
prevalence disorder, the co-morbidity in mental health, interventions, and recovery. In the case
of the low prevalence disorder, Schizophrenia and the psychotic disorders are considered. The
biological paradigm outlines that the abnormal behavior occurs due to various reasons. For
instance, if the receptors are less in the postsynaptic neuron membrane the abnormal behavior
may occur. In addition, if there are many neurotransmitters which cause changes in the
transmitter's re-uptake. Co-morbid mental health/AOD issues are discussed in this paper
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mental Health Practice 8
which refers to the co-occurrence of a single or several diseases within a person. Based on the
biological paradigm, co-morbidity is viewed as the illnesses co-occur with personalities, drug
abuse, affective, and anxiety. At the same time, the interventions are discussed where the
biological mechanism and processes in the treatment of mental illness are outlined (Ringen,
Engh, Birkenaes, Dieset & Andreassen, 2014). Biological approaches have been applied for the
treatment of mental treatment. Clearly, the interventions have an impact on the brain physiology.
The biological paradigm suggests through recovery, individuals manage depression within the
brain. This is because all the elements of recovery such as connectedness, hope, and meaning
originate from the brain.
which refers to the co-occurrence of a single or several diseases within a person. Based on the
biological paradigm, co-morbidity is viewed as the illnesses co-occur with personalities, drug
abuse, affective, and anxiety. At the same time, the interventions are discussed where the
biological mechanism and processes in the treatment of mental illness are outlined (Ringen,
Engh, Birkenaes, Dieset & Andreassen, 2014). Biological approaches have been applied for the
treatment of mental treatment. Clearly, the interventions have an impact on the brain physiology.
The biological paradigm suggests through recovery, individuals manage depression within the
brain. This is because all the elements of recovery such as connectedness, hope, and meaning
originate from the brain.
Mental Health Practice 9
References
Alden, K. J., Cucurull-Sanchez, L., Larminie, C., Coles, M. C., Kullberg, M. C., Evans, S. K., &
Timmis, J. I. (2017). ASPASIA: A toolkit for evaluating the effects of biological
interventions on SBML model behavior. PLoS Computational Biology.
Bird, V. (2015). Supporting the recovery of black individuals who use community mental health
services (Doctoral dissertation, Institute of Psychiatry, Psychology and Neuroscience).
Butcher, J. N., Mineka, S., & Hooley, J. M. (2013). Abnormal psychology. Pearson Education
India.
Dopke, C. A., & Batscha, C. L. (2014). Cognitive-Behavioral Therapy for Individuals with
Schizophrenia: A Recovery Approach. American Journal of Psychiatric
Rehabilitation, 17(1), 44-71.
Gradin, V. B., Pérez, A., MacFarlane, J. A., Cavin, I., Waiter, G., Engelmann, J., ... & Steele, J.
D. (2015). Abnormal brain responses to social fairness in depression: an fMRI study
using the Ultimatum Game. Psychological medicine, 45(6), 1241-1251.
Kwako, L. E., Schwandt, M. L., Sells, J. R., Ramchandani, V. A., Hommer, D. W., George, D.
T., ... & Heilig, M. (2015). Methods for inducing alcohol craving in individuals with co‐
morbid alcohol dependence and posttraumatic stress disorder: behavioral and
physiological outcomes. Addiction biology, 20(4), 733-746.
Laurens, K. R., Luo, L., Matheson, S. L., Carr, V. J., Raudino, A., Harris, F., & Green, M. J.
(2015). Common or distinct pathways to psychosis? A systematic review of evidence
References
Alden, K. J., Cucurull-Sanchez, L., Larminie, C., Coles, M. C., Kullberg, M. C., Evans, S. K., &
Timmis, J. I. (2017). ASPASIA: A toolkit for evaluating the effects of biological
interventions on SBML model behavior. PLoS Computational Biology.
Bird, V. (2015). Supporting the recovery of black individuals who use community mental health
services (Doctoral dissertation, Institute of Psychiatry, Psychology and Neuroscience).
Butcher, J. N., Mineka, S., & Hooley, J. M. (2013). Abnormal psychology. Pearson Education
India.
Dopke, C. A., & Batscha, C. L. (2014). Cognitive-Behavioral Therapy for Individuals with
Schizophrenia: A Recovery Approach. American Journal of Psychiatric
Rehabilitation, 17(1), 44-71.
Gradin, V. B., Pérez, A., MacFarlane, J. A., Cavin, I., Waiter, G., Engelmann, J., ... & Steele, J.
D. (2015). Abnormal brain responses to social fairness in depression: an fMRI study
using the Ultimatum Game. Psychological medicine, 45(6), 1241-1251.
Kwako, L. E., Schwandt, M. L., Sells, J. R., Ramchandani, V. A., Hommer, D. W., George, D.
T., ... & Heilig, M. (2015). Methods for inducing alcohol craving in individuals with co‐
morbid alcohol dependence and posttraumatic stress disorder: behavioral and
physiological outcomes. Addiction biology, 20(4), 733-746.
Laurens, K. R., Luo, L., Matheson, S. L., Carr, V. J., Raudino, A., Harris, F., & Green, M. J.
(2015). Common or distinct pathways to psychosis? A systematic review of evidence
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Mental Health Practice 10
from prospective studies for developmental risk factors and antecedents of the
schizophrenia spectrum disorders and affective psychoses. BMC psychiatry, 15(1), 205.
Lett, T. A., Voineskos, A. N., Kennedy, J. L., Levine, B., & Daskalakis, Z. J. (2014). Treating
working memory deficits in schizophrenia: a review of the neurobiology. Biological
psychiatry, 75(5), 361-370.
Nusslock, R., Young, C. B., & Damme, K. S. (2014). Elevated reward-related neural activation
as a unique biological marker of bipolar disorder: assessment and treatment
implications. Behaviour research and therapy, 62, 74-87.
Ringen, P. A., Engh, J. A., Birkenaes, A. B., Dieset, I., & Andreassen, O. A. (2014). Increased
mortality in schizophrenia due to cardiovascular disease–a non-systematic review of
epidemiology, possible causes, and interventions. Frontiers in psychiatry, 5.
Singer, S., Szalai, C., Briest, S., Brown, A., Dietz, A., Einenkel, J., ... & Löbner, M. (2013). Co‐
morbid mental health conditions in cancer patients at working age–prevalence, risk
profiles, and care uptake. Psycho
‐Oncology, 22(10), 2291-2297.
Wesseloo, R., Kamperman, A. M., Munk-Olsen, T., Pop, V. J., Kushner, S. A., & Bergink, V.
(2015). Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a
systematic review and meta-analysis. American Journal of Psychiatry, 173(2), 117-127.
from prospective studies for developmental risk factors and antecedents of the
schizophrenia spectrum disorders and affective psychoses. BMC psychiatry, 15(1), 205.
Lett, T. A., Voineskos, A. N., Kennedy, J. L., Levine, B., & Daskalakis, Z. J. (2014). Treating
working memory deficits in schizophrenia: a review of the neurobiology. Biological
psychiatry, 75(5), 361-370.
Nusslock, R., Young, C. B., & Damme, K. S. (2014). Elevated reward-related neural activation
as a unique biological marker of bipolar disorder: assessment and treatment
implications. Behaviour research and therapy, 62, 74-87.
Ringen, P. A., Engh, J. A., Birkenaes, A. B., Dieset, I., & Andreassen, O. A. (2014). Increased
mortality in schizophrenia due to cardiovascular disease–a non-systematic review of
epidemiology, possible causes, and interventions. Frontiers in psychiatry, 5.
Singer, S., Szalai, C., Briest, S., Brown, A., Dietz, A., Einenkel, J., ... & Löbner, M. (2013). Co‐
morbid mental health conditions in cancer patients at working age–prevalence, risk
profiles, and care uptake. Psycho
‐Oncology, 22(10), 2291-2297.
Wesseloo, R., Kamperman, A. M., Munk-Olsen, T., Pop, V. J., Kushner, S. A., & Bergink, V.
(2015). Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a
systematic review and meta-analysis. American Journal of Psychiatry, 173(2), 117-127.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




