University Case Study: Mental Health & Inquiry-Based Learning
VerifiedAdded on 2023/06/05
|5
|883
|81
Case Study
AI Summary
This case study delves into a patient's mental health issues, employing an inquiry-based learning approach to understand and address the challenges. The study focuses on physical and behavioral changes, including mood swings, restlessness, and sleep disturbances, indicative of potential bipolar disorder. It emphasizes the importance of assessing food-drug interactions and caffeine intake. Key traits are identified to mitigate relapse through treatment adherence, sleep management, and cognitive behavioral therapy. The study poses critical questions about cognitive behavioral mechanisms and coping strategies, highlighting the need for a comprehensive and supportive environment to enhance the patient's treatment process. References to various scholarly articles support the assessment and proposed interventions.
University
Assignment
Student name
Tutor
Assignment
Student name
Tutor
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mental Health Case study Assesment
2
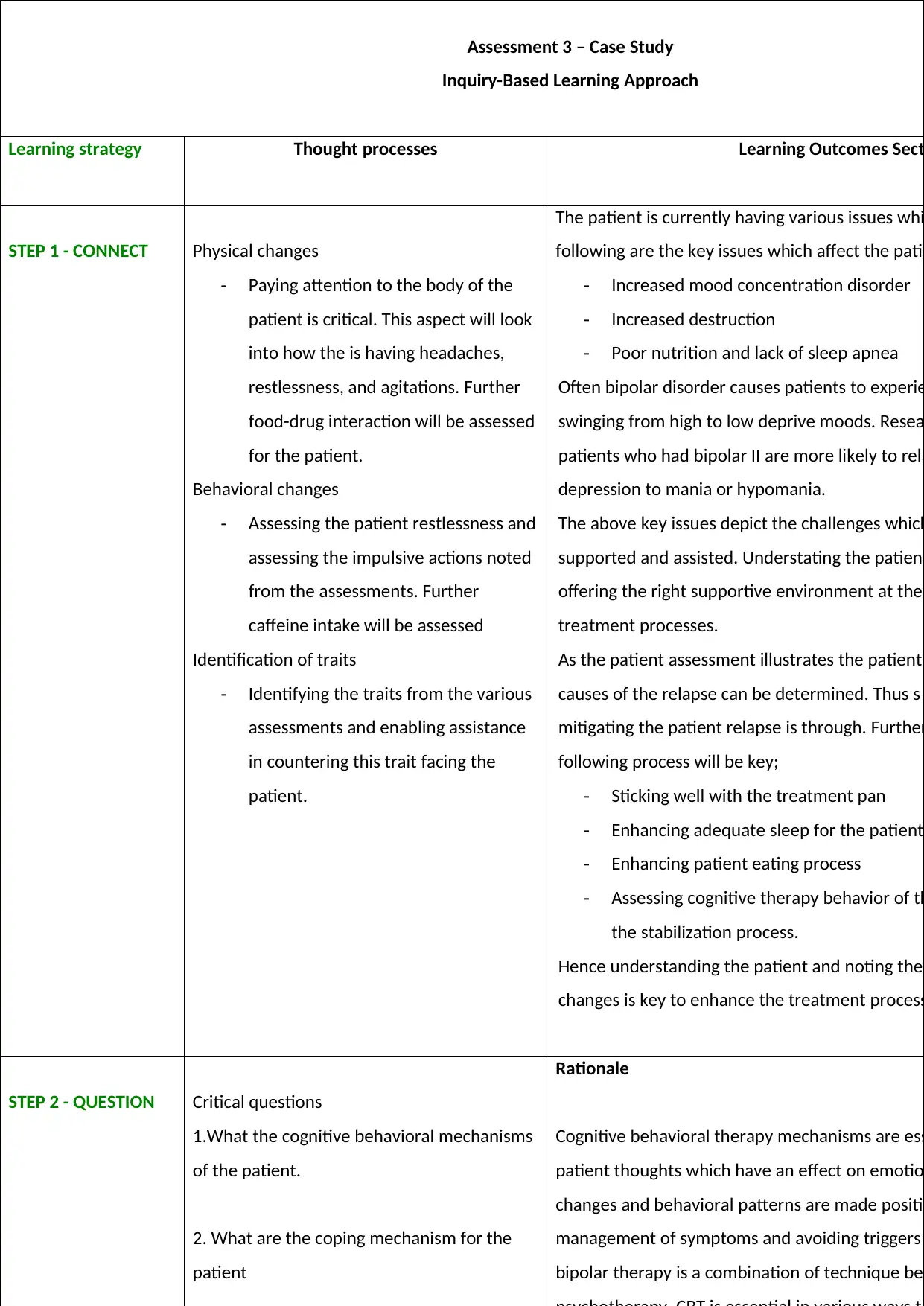
Assessment 3 – Case Study
Inquiry-Based Learning Approach
Learning strategy Thought processes Learning Outcomes Secti
STEP 1 - CONNECT Physical changes
- Paying attention to the body of the
patient is critical. This aspect will look
into how the is having headaches,
restlessness, and agitations. Further
food-drug interaction will be assessed
for the patient.
Behavioral changes
- Assessing the patient restlessness and
assessing the impulsive actions noted
from the assessments. Further
caffeine intake will be assessed
Identification of traits
- Identifying the traits from the various
assessments and enabling assistance
in countering this trait facing the
patient.
The patient is currently having various issues whi
following are the key issues which affect the patie
- Increased mood concentration disorder
- Increased destruction
- Poor nutrition and lack of sleep apnea
Often bipolar disorder causes patients to experie
swinging from high to low deprive moods. Resea
patients who had bipolar II are more likely to rela
depression to mania or hypomania.
The above key issues depict the challenges which
supported and assisted. Understating the patient
offering the right supportive environment at the
treatment processes.
As the patient assessment illustrates the patient
causes of the relapse can be determined. Thus s
mitigating the patient relapse is through. Further
following process will be key;
- Sticking well with the treatment pan
- Enhancing adequate sleep for the patient
- Enhancing patient eating process
- Assessing cognitive therapy behavior of th
the stabilization process.
Hence understanding the patient and noting the
changes is key to enhance the treatment process
STEP 2 - QUESTION Critical questions
1.What the cognitive behavioral mechanisms
of the patient.
2. What are the coping mechanism for the
patient
Rationale
Cognitive behavioral therapy mechanisms are ess
patient thoughts which have an effect on emotio
changes and behavioral patterns are made positiv
management of symptoms and avoiding triggers
bipolar therapy is a combination of technique bet
2
Assessment 3 – Case Study
Inquiry-Based Learning Approach
Learning strategy Thought processes Learning Outcomes Secti
STEP 1 - CONNECT Physical changes
- Paying attention to the body of the
patient is critical. This aspect will look
into how the is having headaches,
restlessness, and agitations. Further
food-drug interaction will be assessed
for the patient.
Behavioral changes
- Assessing the patient restlessness and
assessing the impulsive actions noted
from the assessments. Further
caffeine intake will be assessed
Identification of traits
- Identifying the traits from the various
assessments and enabling assistance
in countering this trait facing the
patient.
The patient is currently having various issues whi
following are the key issues which affect the patie
- Increased mood concentration disorder
- Increased destruction
- Poor nutrition and lack of sleep apnea
Often bipolar disorder causes patients to experie
swinging from high to low deprive moods. Resea
patients who had bipolar II are more likely to rela
depression to mania or hypomania.
The above key issues depict the challenges which
supported and assisted. Understating the patient
offering the right supportive environment at the
treatment processes.
As the patient assessment illustrates the patient
causes of the relapse can be determined. Thus s
mitigating the patient relapse is through. Further
following process will be key;
- Sticking well with the treatment pan
- Enhancing adequate sleep for the patient
- Enhancing patient eating process
- Assessing cognitive therapy behavior of th
the stabilization process.
Hence understanding the patient and noting the
changes is key to enhance the treatment process
STEP 2 - QUESTION Critical questions
1.What the cognitive behavioral mechanisms
of the patient.
2. What are the coping mechanism for the
patient
Rationale
Cognitive behavioral therapy mechanisms are ess
patient thoughts which have an effect on emotio
changes and behavioral patterns are made positiv
management of symptoms and avoiding triggers
bipolar therapy is a combination of technique bet

Mental Health Case study Assesment
3
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Mental Health Case study Assesment
4
References
Blixen, C., Perzynski, A.T., Bukach, A., Howland, M. and Sajatovic, M., 2016. Patients’ perceptions of barriers
to self-managing bipolar disorder: A qualitative study. International Journal of Social Psychiatry, 62(7),
pp.635-645
Collins, E., Tranter, S. and Irvine, F., 2012. The physical health of the seriously mentally ill: an overview of
the literature. Journal of Psychiatric and Mental Health Nursing, 19(7), pp.638-646.
DSM-5 American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders.
Arlington: American Psychiatric Publishing.
Goossens, P.J.J., Kupka, R.W., Beentjes, T.A.A., and van Achterberg, T., 2010. Recognizing prodromes of
manic or depressive recurrence in outpatients with bipolar disorder: A cross-sectional study. International
journal of nursing studies, 47(10), pp.1201-1207.
Jann, M.W., 2014. Diagnosis and treatment of bipolar disorders in adults: a review of the evidence on
pharmacologic treatments. American health & drug benefits, 7(9), p.489.
Jesus, E.D.S., Marques, L.R., Assis, L.C.F., Alves, T.B., Freitas, G.F.D. and Oguisso, T., 2010.
Prejudice in nursing: perception of nurses educated in different decades. Revista da Escola de
Enfermagem da USP, 44(1), pp.166-173.
Krans, B. & Cherney, K. (2016). The history of bipolar disorder. Retrieved from
ht1p://www.healthline.com /health/bipolar-disorder /history-bit
Rowland, J.E., Hamilton, M.K., Lino, B.J., Ly, P., Denny, K., Hwang, E.J., Mitchell, P.B., Carr, V.J. and Green,
M.J., 2013. Cognitive regulation of negative affect in schizophrenia and bipolar disorder. Psychiatry
research, 208(1), pp.21-28.
Salloum, I.M., 2014. A person-centered approach to diagnosis and care for Bipolar Disorder and Alcoholism.
International Journal of Person Centered Medicine, 3(3), pp.198-204.
Salvatore, P., Tohen, M., Khalsa, H.M.K., Baethge, C., Tondo, L. and Baldessarini, R.J., 2007. Longitudinal
research on bipolar disorders. Epidemiology and Psychiatric Sciences, 16(2), pp.109-117.
Schulze, T.G., Detera-Wadleigh, S.D., Akula, N., Gupta, A., Kassem, L., Steele, J., Pearl, J., Strohmaier, J.,
Breuer, R., Schwarz, M. and Propping, P., 2009. Two variants in Ankyrin 3 (ANK3) are independent genetic
risk factors for bipolar disorder. Molecular psychiatry, 14(5), p.487.
4
References
Blixen, C., Perzynski, A.T., Bukach, A., Howland, M. and Sajatovic, M., 2016. Patients’ perceptions of barriers
to self-managing bipolar disorder: A qualitative study. International Journal of Social Psychiatry, 62(7),
pp.635-645
Collins, E., Tranter, S. and Irvine, F., 2012. The physical health of the seriously mentally ill: an overview of
the literature. Journal of Psychiatric and Mental Health Nursing, 19(7), pp.638-646.
DSM-5 American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders.
Arlington: American Psychiatric Publishing.
Goossens, P.J.J., Kupka, R.W., Beentjes, T.A.A., and van Achterberg, T., 2010. Recognizing prodromes of
manic or depressive recurrence in outpatients with bipolar disorder: A cross-sectional study. International
journal of nursing studies, 47(10), pp.1201-1207.
Jann, M.W., 2014. Diagnosis and treatment of bipolar disorders in adults: a review of the evidence on
pharmacologic treatments. American health & drug benefits, 7(9), p.489.
Jesus, E.D.S., Marques, L.R., Assis, L.C.F., Alves, T.B., Freitas, G.F.D. and Oguisso, T., 2010.
Prejudice in nursing: perception of nurses educated in different decades. Revista da Escola de
Enfermagem da USP, 44(1), pp.166-173.
Krans, B. & Cherney, K. (2016). The history of bipolar disorder. Retrieved from
ht1p://www.healthline.com /health/bipolar-disorder /history-bit
Rowland, J.E., Hamilton, M.K., Lino, B.J., Ly, P., Denny, K., Hwang, E.J., Mitchell, P.B., Carr, V.J. and Green,
M.J., 2013. Cognitive regulation of negative affect in schizophrenia and bipolar disorder. Psychiatry
research, 208(1), pp.21-28.
Salloum, I.M., 2014. A person-centered approach to diagnosis and care for Bipolar Disorder and Alcoholism.
International Journal of Person Centered Medicine, 3(3), pp.198-204.
Salvatore, P., Tohen, M., Khalsa, H.M.K., Baethge, C., Tondo, L. and Baldessarini, R.J., 2007. Longitudinal
research on bipolar disorders. Epidemiology and Psychiatric Sciences, 16(2), pp.109-117.
Schulze, T.G., Detera-Wadleigh, S.D., Akula, N., Gupta, A., Kassem, L., Steele, J., Pearl, J., Strohmaier, J.,
Breuer, R., Schwarz, M. and Propping, P., 2009. Two variants in Ankyrin 3 (ANK3) are independent genetic
risk factors for bipolar disorder. Molecular psychiatry, 14(5), p.487.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mental Health Case study Assesment
5
Swartz, H.A. and Swanson, J., 2014. Psychotherapy for bipolar disorder in adults: a review of the evidence.
Focus, 12(3), pp.251-266.
5
Swartz, H.A. and Swanson, J., 2014. Psychotherapy for bipolar disorder in adults: a review of the evidence.
Focus, 12(3), pp.251-266.
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





