Mental Health Nursing Case Study: Managing John Gray's Depression
VerifiedAdded on 2020/02/19
|10
|2283
|1060
Case Study
AI Summary
This case study examines the mental health nursing care of Mr. John Gray, a 28-year-old male experiencing major depression due to the stress of a drought affecting his family farm and a recent suicide attempt. The assignment details the application of the Levett-Jones clinical reasoning cycle to assess, plan, and evaluate the patient's care. The case study outlines the patient's history, including symptoms of depression, social isolation, and physical signs of self-harm. It identifies key nursing issues, such as suicide risk, depression, and social isolation, and establishes goals for intervention. The nursing care plan includes interventions like anxiety reduction, suicide prevention measures, and strategies to address social isolation, including motivational sessions, environmental modifications, and family involvement. The evaluation of outcomes focuses on improvements in the patient's self-confidence, reduced anxiety, and increased social engagement. The author reflects on the importance of patient-centered care and the effectiveness of the clinical reasoning cycle in developing an appropriate treatment plan.

Running Head: MENTAL HEALTH NURSING
Mental Health Nursing
Name of the Student
Name of the University
Author Note
Mental Health Nursing
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1MENTAL HEALTH NURSING
Introduction
Several aspects of daily life hamper the psychological, emotional, and social well-being
of an individual. The effect may be mild to severe mental disorders such as obsessive-
compulsive disorder, schizophrenia, anxiety, and depression that severely affect behaviour and
thought. The paper deals with the case study of John Gray who is suffering from major
depression. The paper presents the management of the patient using the Levett-Jone’s clinical
reasoning cycle. This framework is effective to plan and evaluate the person-centred care
appropriate for individual patient.
Patient details
Mr. John Gray (Male, 28) lives in Brisbane. He is expected by his family to take over the
family farm, as he is son of grazier. John is depressed due to longstanding drought that affected
his farm. He had attempted suicide and is presented to hospital a week ago.
Patient information
The data collected from the John’s handover informs of major depression and increased
social isolation evident from disorientation and signs of withdrawal. He is not taking breakfast
and skipped lunch as well. He slept with empty stomach. John’s vital signs as per the assessment
data shows blood pressure 125/75, pulse rate 66, respiration rate 18. Physical examination
reports of bruising and broken skin on his legs and arms. Around his neck a rope burned mark
is prominent that indicates his suicide attempt. His current medications include Multivit I and
Vitamin B Co I daily, Venlafaxine 75mg BD.
Introduction
Several aspects of daily life hamper the psychological, emotional, and social well-being
of an individual. The effect may be mild to severe mental disorders such as obsessive-
compulsive disorder, schizophrenia, anxiety, and depression that severely affect behaviour and
thought. The paper deals with the case study of John Gray who is suffering from major
depression. The paper presents the management of the patient using the Levett-Jone’s clinical
reasoning cycle. This framework is effective to plan and evaluate the person-centred care
appropriate for individual patient.
Patient details
Mr. John Gray (Male, 28) lives in Brisbane. He is expected by his family to take over the
family farm, as he is son of grazier. John is depressed due to longstanding drought that affected
his farm. He had attempted suicide and is presented to hospital a week ago.
Patient information
The data collected from the John’s handover informs of major depression and increased
social isolation evident from disorientation and signs of withdrawal. He is not taking breakfast
and skipped lunch as well. He slept with empty stomach. John’s vital signs as per the assessment
data shows blood pressure 125/75, pulse rate 66, respiration rate 18. Physical examination
reports of bruising and broken skin on his legs and arms. Around his neck a rope burned mark
is prominent that indicates his suicide attempt. His current medications include Multivit I and
Vitamin B Co I daily, Venlafaxine 75mg BD.
2MENTAL HEALTH NURSING
Processing information- collection of cues
Collecting the patient cues is the next step of clinical reasoning cycle. In addition to the
case details, I have collected more information by interacting with communicated with John and
his family. To gain broad perspective on the Johm’s mental condition it is necessary to identify
the risk factors for suicide and level of depression. Thus, collection of patient cues is necessary.
Depression is the mental illness where a person loses interest to live. It is manifested as low self-
confidence and self-esteem and ultimately an urge to commit suicide (Goesling et al., 2013).
Depressions occur due to overwhelming crisis, where a person is unable to cope up. In this case
is John is unable to cope up with drought and failure to fulfil farm’s responsibility. He is worried
about future. Thus, he is withdrawing from social engagement may be due to feeling of guilt and
shame. John is not involving in any communication and tends to be demonstrated. It can be
interpreted as loss of interest and hope in life (Chu et al., 2015).
Identification of issues of nursing priority
After collecting the patient cues, I have identified the primary issues of the case. Firstly,
John is worried about future. It is increasing his stress and anxiety. His thinking is of anxious
pattern that may be due to longstanding drought and failure to fulfil family responsibility. He
may be stressed thinking about the way to revive family’s farm. During depression people have
tendency to engage in self-criticism and decrease communication an interaction with people
(Cummins et al., 2015). Feeling of worthlessness is another risk factor for depression and
suicide. This risk factor triggers impulsive thoughts and impairs concentration. It causes
indecisiveness and self-harm behavior. According to Freud aggression, anger and negative
feelings result from loss of objects. Loss of farm, lack of social support and deception are
environmental triggers of depression and suicide in John (Cummins et al., 2015). Thus, it is
Processing information- collection of cues
Collecting the patient cues is the next step of clinical reasoning cycle. In addition to the
case details, I have collected more information by interacting with communicated with John and
his family. To gain broad perspective on the Johm’s mental condition it is necessary to identify
the risk factors for suicide and level of depression. Thus, collection of patient cues is necessary.
Depression is the mental illness where a person loses interest to live. It is manifested as low self-
confidence and self-esteem and ultimately an urge to commit suicide (Goesling et al., 2013).
Depressions occur due to overwhelming crisis, where a person is unable to cope up. In this case
is John is unable to cope up with drought and failure to fulfil farm’s responsibility. He is worried
about future. Thus, he is withdrawing from social engagement may be due to feeling of guilt and
shame. John is not involving in any communication and tends to be demonstrated. It can be
interpreted as loss of interest and hope in life (Chu et al., 2015).
Identification of issues of nursing priority
After collecting the patient cues, I have identified the primary issues of the case. Firstly,
John is worried about future. It is increasing his stress and anxiety. His thinking is of anxious
pattern that may be due to longstanding drought and failure to fulfil family responsibility. He
may be stressed thinking about the way to revive family’s farm. During depression people have
tendency to engage in self-criticism and decrease communication an interaction with people
(Cummins et al., 2015). Feeling of worthlessness is another risk factor for depression and
suicide. This risk factor triggers impulsive thoughts and impairs concentration. It causes
indecisiveness and self-harm behavior. According to Freud aggression, anger and negative
feelings result from loss of objects. Loss of farm, lack of social support and deception are
environmental triggers of depression and suicide in John (Cummins et al., 2015). Thus, it is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3MENTAL HEALTH NURSING
important for mental health nurse to maintain the patient safety. It is necessary to minimizing
self-harm and ensure positive outcomes by safe medication. It is necessary to eliminate the
feeling of hopelessness in John so that he can resume his daily activities so that he can eat, read,
and interact with people normally.
Thus, the three priority nursing areas are-
Depression and low self esteem
Suicide risk and self harm tendency
Increased Social isolation, and disorientation
Other nursing issues considered are-
Feeling of worthlessness
Loss of hope in life
Anxiety
Nutrition- Skipping breakfast and dinner
Need of increasing adherence to medication
Cure physical injury
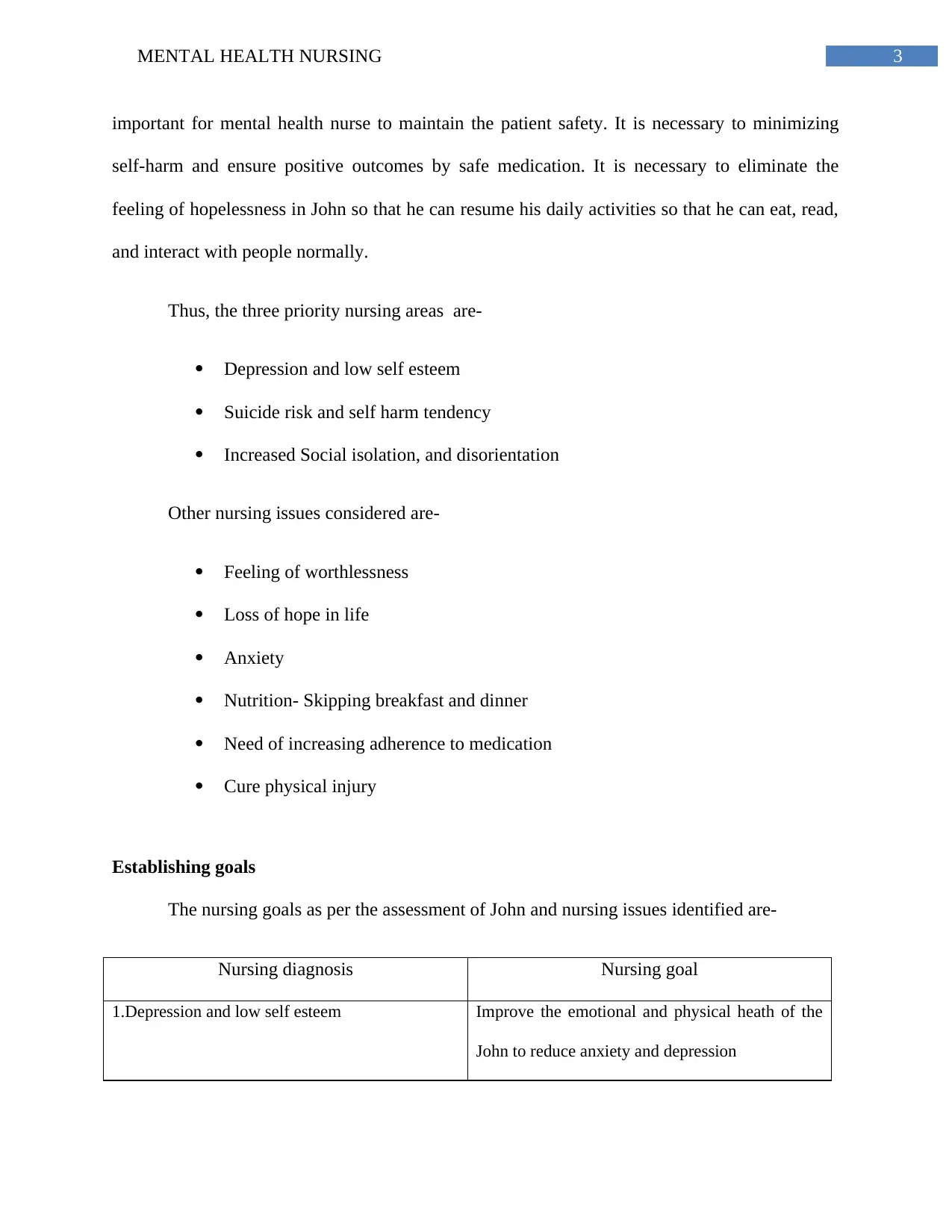
Establishing goals
The nursing goals as per the assessment of John and nursing issues identified are-
Nursing diagnosis Nursing goal
1.Depression and low self esteem Improve the emotional and physical heath of the
John to reduce anxiety and depression
important for mental health nurse to maintain the patient safety. It is necessary to minimizing
self-harm and ensure positive outcomes by safe medication. It is necessary to eliminate the
feeling of hopelessness in John so that he can resume his daily activities so that he can eat, read,
and interact with people normally.
Thus, the three priority nursing areas are-
Depression and low self esteem
Suicide risk and self harm tendency
Increased Social isolation, and disorientation
Other nursing issues considered are-
Feeling of worthlessness
Loss of hope in life
Anxiety
Nutrition- Skipping breakfast and dinner
Need of increasing adherence to medication
Cure physical injury
Establishing goals
The nursing goals as per the assessment of John and nursing issues identified are-
Nursing diagnosis Nursing goal
1.Depression and low self esteem Improve the emotional and physical heath of the
John to reduce anxiety and depression
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4MENTAL HEALTH NURSING
(Gordon, 2014)
2.Sucide risk and self harm Assessment of the environment to prevent self-
injury of patient. Assessment of the environment
include identifying for objects such as ligature
point, belt, knife and any other object that can
help in self harm. The goal is to Monitor the
mental status of the patient regularly to modify
the risk factors (Smith et al., 2015)
3. Increased Social isolation Increase communication and interaction with
patient to help verbalise thoughts and reduce
withdrawl and disorientation in-patient.
(Moorhead et al., 2014)
Nursing care plan for John
Nursing interventions and Rationale
The first nursing intervention classification is Anxiety reduction- The nursing
interventions for anxiety reduction are establishing therapeutic relationship with client. John can
be assisted to verbalise his feelings and voice out expression only by building strong rapport
with him (Adams & Iseler, 2014). Further patient centred care will be provided to foster
positive psychological balance in John. John will feel important and feel connected if he
receives empathy (Forbes & Watt, 2015). Motivational sessions will be arranged for John to
trigger positivity and increase courage to overcome fear and worthlessness (Robson et al., 2013).
(Gordon, 2014)
2.Sucide risk and self harm Assessment of the environment to prevent self-
injury of patient. Assessment of the environment
include identifying for objects such as ligature
point, belt, knife and any other object that can
help in self harm. The goal is to Monitor the
mental status of the patient regularly to modify
the risk factors (Smith et al., 2015)
3. Increased Social isolation Increase communication and interaction with
patient to help verbalise thoughts and reduce
withdrawl and disorientation in-patient.
(Moorhead et al., 2014)
Nursing care plan for John
Nursing interventions and Rationale
The first nursing intervention classification is Anxiety reduction- The nursing
interventions for anxiety reduction are establishing therapeutic relationship with client. John can
be assisted to verbalise his feelings and voice out expression only by building strong rapport
with him (Adams & Iseler, 2014). Further patient centred care will be provided to foster
positive psychological balance in John. John will feel important and feel connected if he
receives empathy (Forbes & Watt, 2015). Motivational sessions will be arranged for John to
trigger positivity and increase courage to overcome fear and worthlessness (Robson et al., 2013).
5MENTAL HEALTH NURSING
The second intervention is suicide prevention- The intervention to prevent suicide
involves modifying patient’s environment. Providing positive environment will prevent self-
harm behaviour. Removal of sharp objects and anything that can assist John to self-harm is the
part of the intervention (Happell & Gaskin 2013). Referral to mental health counselling in case is
John is evident of suicidal intent. Counselling will help control distorted and impulsive thoughts
in John. Further John will be provided health education. The health education is provided to
increase adherence to medication and have proper diet as John is presently at risk of
malnutrition. Health education create awareness on the consequences of depression and how it
stimulates one to attempt suicide (Seo et al., 2015).
The third nursing intervention is crisis intervention and decrease social isolation- In
order to enhance coping skills in John, his parents and family members will be involved. This
will reinforce his self-esteem. Further, John will be involved in physical activity in-group where
he can interact with other people of his age. Involving John in jogging, swimming, walking,
whichever enhances mood will promote social connectedness. Depression, anxiety and social
isolation can be minimised by physical activities like exercise (Storm & Edwards, 2013). John’s
parents will be referred to crisis intervention agencies to receive help on current situation.
Resolving crisis will prevent social withdrawl in client and promote willingness to eat, talk and
live (France, 2015).
Evaluation of outcomes
The following outcomes indicate improvement in the John’s condition in regards to the
priority nursing areas.
Patient demonstrates increase in self-confidence and relaxed state of mind.
The second intervention is suicide prevention- The intervention to prevent suicide
involves modifying patient’s environment. Providing positive environment will prevent self-
harm behaviour. Removal of sharp objects and anything that can assist John to self-harm is the
part of the intervention (Happell & Gaskin 2013). Referral to mental health counselling in case is
John is evident of suicidal intent. Counselling will help control distorted and impulsive thoughts
in John. Further John will be provided health education. The health education is provided to
increase adherence to medication and have proper diet as John is presently at risk of
malnutrition. Health education create awareness on the consequences of depression and how it
stimulates one to attempt suicide (Seo et al., 2015).
The third nursing intervention is crisis intervention and decrease social isolation- In
order to enhance coping skills in John, his parents and family members will be involved. This
will reinforce his self-esteem. Further, John will be involved in physical activity in-group where
he can interact with other people of his age. Involving John in jogging, swimming, walking,
whichever enhances mood will promote social connectedness. Depression, anxiety and social
isolation can be minimised by physical activities like exercise (Storm & Edwards, 2013). John’s
parents will be referred to crisis intervention agencies to receive help on current situation.
Resolving crisis will prevent social withdrawl in client and promote willingness to eat, talk and
live (France, 2015).
Evaluation of outcomes
The following outcomes indicate improvement in the John’s condition in regards to the
priority nursing areas.
Patient demonstrates increase in self-confidence and relaxed state of mind.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6MENTAL HEALTH NURSING
John will show reduced anxiety in 2 weeks
John will talk about feelings and express his anger or frustration
Reduce the risk of suicide indicated by- reduced patient’s ability to accelerate risk, i.e,
John does not harm self
Increase in communication skills of patient, physical activity and engagement in daily
activities indicate social engagement
Reflection
I have realised from my experience with John’s case that patient centred care is
fundamental aspect of the mental health care. Patients feel comfortable and respected when
information is provided to them effectively. Using the clinical reasoning cycle was effective in
developing care plan that is appropriate for John. I was able to design care plan appropriate to
reduce depression and suicidal tendencies treatment plan for depression and anxiety.
Demonstrating self-awareness is important while establishing the therapeutic relationship with
patient. Establishment of interpersonal relations assisted in John’s assessment. The clinical
reasoning framework helped me to think and analyse the cause of depression an current thinking
pattern of John. It improved my critical thinking skills to collect information from patient with
high level of psychological distress. I was able to assist John to believe in himself and foster a
sense of control over his situation by giving support and empathy. It improved the overall care
process and increased the verbal expression of the client. Involving his family, encouraged him
to recover and helped in decision-making. I maintained the respect and dignity of the client as
well as of his family members. I can conclude that up skilling is an essential part of nursing. I
need to strengthen my professional skills even more to assist patients with mental health
disorder.
John will show reduced anxiety in 2 weeks
John will talk about feelings and express his anger or frustration
Reduce the risk of suicide indicated by- reduced patient’s ability to accelerate risk, i.e,
John does not harm self
Increase in communication skills of patient, physical activity and engagement in daily
activities indicate social engagement
Reflection
I have realised from my experience with John’s case that patient centred care is
fundamental aspect of the mental health care. Patients feel comfortable and respected when
information is provided to them effectively. Using the clinical reasoning cycle was effective in
developing care plan that is appropriate for John. I was able to design care plan appropriate to
reduce depression and suicidal tendencies treatment plan for depression and anxiety.
Demonstrating self-awareness is important while establishing the therapeutic relationship with
patient. Establishment of interpersonal relations assisted in John’s assessment. The clinical
reasoning framework helped me to think and analyse the cause of depression an current thinking
pattern of John. It improved my critical thinking skills to collect information from patient with
high level of psychological distress. I was able to assist John to believe in himself and foster a
sense of control over his situation by giving support and empathy. It improved the overall care
process and increased the verbal expression of the client. Involving his family, encouraged him
to recover and helped in decision-making. I maintained the respect and dignity of the client as
well as of his family members. I can conclude that up skilling is an essential part of nursing. I
need to strengthen my professional skills even more to assist patients with mental health
disorder.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7MENTAL HEALTH NURSING
8MENTAL HEALTH NURSING
References
Adams, K. L., & Iseler, J. I. (2014). The relationship of bedside nurses' emotional intelligence
with quality of care. Journal of nursing care quality,29(2), 174-181.
Bolton, J. M., Gunnell, D., & Turecki, G. (2015). Suicide risk assessment and intervention in
people with mental illness. BMJ, 351, h4978.
Chu, C., Klein, K. M., Buchman‐Schmitt, J. M., Hom, M. A., Hagan, C. R., & Joiner, T. E.
(2015). Routinized assessment of suicide risk in clinical practice: an empirically informed
update. Journal of clinical psychology, 71(12), 1186-1200.
Cummins, N., Scherer, S., Krajewski, J., Schnieder, S., Epps, J., & Quatieri, T. F. (2015). A
review of depression and suicide risk assessment using speech analysis. Speech
Communication, 71, 10-49.
El‐Jawahri, A. R., Traeger, L. N., Kuzmuk, K., Eusebio, J. R., Vandusen, H. B., Shin, J. A., ... &
Jackson, V. A. (2015). Quality of life and mood of patients and family caregivers during
hospitalization for hematopoietic stem cell transplantation. Cancer, 121(6), 951-959.
Forbes, H., & Watt, E. (2015). Jarvis's Physical Examination and Health Assessment. Elsevier
Health Sciences.
France, K. (2015). Crisis intervention: A handbook of immediate person-to-person help. Charles
C Thomas Publisher.
Goesling, J., Clauw, D. J., & Hassett, A. L. (2013). Pain and depression: an integrative review of
neurobiological and psychological factors. Current psychiatry reports, 15(12), 421.
References
Adams, K. L., & Iseler, J. I. (2014). The relationship of bedside nurses' emotional intelligence
with quality of care. Journal of nursing care quality,29(2), 174-181.
Bolton, J. M., Gunnell, D., & Turecki, G. (2015). Suicide risk assessment and intervention in
people with mental illness. BMJ, 351, h4978.
Chu, C., Klein, K. M., Buchman‐Schmitt, J. M., Hom, M. A., Hagan, C. R., & Joiner, T. E.
(2015). Routinized assessment of suicide risk in clinical practice: an empirically informed
update. Journal of clinical psychology, 71(12), 1186-1200.
Cummins, N., Scherer, S., Krajewski, J., Schnieder, S., Epps, J., & Quatieri, T. F. (2015). A
review of depression and suicide risk assessment using speech analysis. Speech
Communication, 71, 10-49.
El‐Jawahri, A. R., Traeger, L. N., Kuzmuk, K., Eusebio, J. R., Vandusen, H. B., Shin, J. A., ... &
Jackson, V. A. (2015). Quality of life and mood of patients and family caregivers during
hospitalization for hematopoietic stem cell transplantation. Cancer, 121(6), 951-959.
Forbes, H., & Watt, E. (2015). Jarvis's Physical Examination and Health Assessment. Elsevier
Health Sciences.
France, K. (2015). Crisis intervention: A handbook of immediate person-to-person help. Charles
C Thomas Publisher.
Goesling, J., Clauw, D. J., & Hassett, A. L. (2013). Pain and depression: an integrative review of
neurobiological and psychological factors. Current psychiatry reports, 15(12), 421.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9MENTAL HEALTH NURSING
Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
Happell, B., & Gaskin, C. J. (2013). The attitudes of undergraduate nursing students towards
mental health nursing: A systematic review. Journal of Clinical Nursing, 22(1-2), 148-
158.
Moorhead, S., Johnson, M., Maas, M. L., & Swanson, E. (2014). Nursing Outcomes
Classification (NOC)-E-Book: Measurement of Health Outcomes. Elsevier Health
Sciences.
Robson, D., Haddad, M., Gray, R., & Gournay, K. (2013). Mental health nursing and physical
health care: A cross‐sectional study of nurses' attitudes, practice, and perceived training
needs for the physical health care of people with severe mental illness. International
Journal of Mental Health Nursing, 22(5), 409-417.
Seo, M., Kang, H. S., Lee, Y. J., & Chae, S. M. (2015). Narrative therapy with an emotional
approach for people with depression: Improved symptom and cognitive‐emotional
outcomes. Journal of psychiatric and mental health nursing, 22(6), 379-389.
Smith, M. J., Bouch, J., Bradstreet, S., Lakey, T., Nightingale, A., & O'Connor, R. C. (2015).
Health services, suicide, and self-harm: patient distress and system anxiety. The Lancet
Psychiatry, 2(3), 275-280.
Storm, M., & Edwards, A. (2013). Models of user involvement in the mental health context:
intentions and implementation challenges. Psychiatric Quarterly, 84(3), 313-327.
Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
Happell, B., & Gaskin, C. J. (2013). The attitudes of undergraduate nursing students towards
mental health nursing: A systematic review. Journal of Clinical Nursing, 22(1-2), 148-
158.
Moorhead, S., Johnson, M., Maas, M. L., & Swanson, E. (2014). Nursing Outcomes
Classification (NOC)-E-Book: Measurement of Health Outcomes. Elsevier Health
Sciences.
Robson, D., Haddad, M., Gray, R., & Gournay, K. (2013). Mental health nursing and physical
health care: A cross‐sectional study of nurses' attitudes, practice, and perceived training
needs for the physical health care of people with severe mental illness. International
Journal of Mental Health Nursing, 22(5), 409-417.
Seo, M., Kang, H. S., Lee, Y. J., & Chae, S. M. (2015). Narrative therapy with an emotional
approach for people with depression: Improved symptom and cognitive‐emotional
outcomes. Journal of psychiatric and mental health nursing, 22(6), 379-389.
Smith, M. J., Bouch, J., Bradstreet, S., Lakey, T., Nightingale, A., & O'Connor, R. C. (2015).
Health services, suicide, and self-harm: patient distress and system anxiety. The Lancet
Psychiatry, 2(3), 275-280.
Storm, M., & Edwards, A. (2013). Models of user involvement in the mental health context:
intentions and implementation challenges. Psychiatric Quarterly, 84(3), 313-327.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





