Developing a Recovery-Focused Care Plan for Katie: Mental Health
VerifiedAdded on 2023/06/15
|10
|2528
|129
Report
AI Summary
This report presents a recovery-focused care plan for Katie, a patient diagnosed with paranoid schizophrenia, anxiety disorder, and hypertension. The plan outlines specific goals, interventions, and evaluation methods for each condition, emphasizing effective communication, anxiety reduction, and blood pressure management. It also references current literature and guidelines, including the DSM-5 and the Mental Health Act 1983, to inform clinical decision-making. The plan details strategies for medication adherence, relaxation techniques, and lifestyle modifications, all tailored to Katie's individual needs and preferences. The report concludes by highlighting the importance of a holistic approach that considers Katie's mental and physical well-being, ensuring a comprehensive and effective care strategy. Desklib provides similar solved assignments and resources for students.
Mental health Nursing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Introduction...........................................................................................................................................2
Main Body.............................................................................................................................................2
The recovery focused plan for Katie..................................................................................................2
Current prevailing literature and guidelines to inform critical thinking.............................................5
References:............................................................................................................................................9
Introduction...........................................................................................................................................2
Main Body.............................................................................................................................................2
The recovery focused plan for Katie..................................................................................................2
Current prevailing literature and guidelines to inform critical thinking.............................................5
References:............................................................................................................................................9
Introduction
Mental health nursing is a specialised field of healthcare practice which is involved in
the individual care with mental disorders to help them in recovery and improving the quality
of their life. This is also known as psychiatric nursing. The nurses in mental health have
advance skills and knowledge of assessment, treatment and diagnosis of various psychiatric
disorders which assist them in providing their specialised care to users of service (Kumar and
Nayar, 2021). Mental health nurses work alongside the other health care professionals in
medical teams in a medical centres with an objective of providing the optimal clinical results
for the patient.
The report will aim to inform the in-depth critical formulation of recovery focused
care plan of provided case. The report will focus to provide care plan with themes on which
plan ill prioritise. Literature and guidelines to inform clinical thinking will also be provided.
Main Body
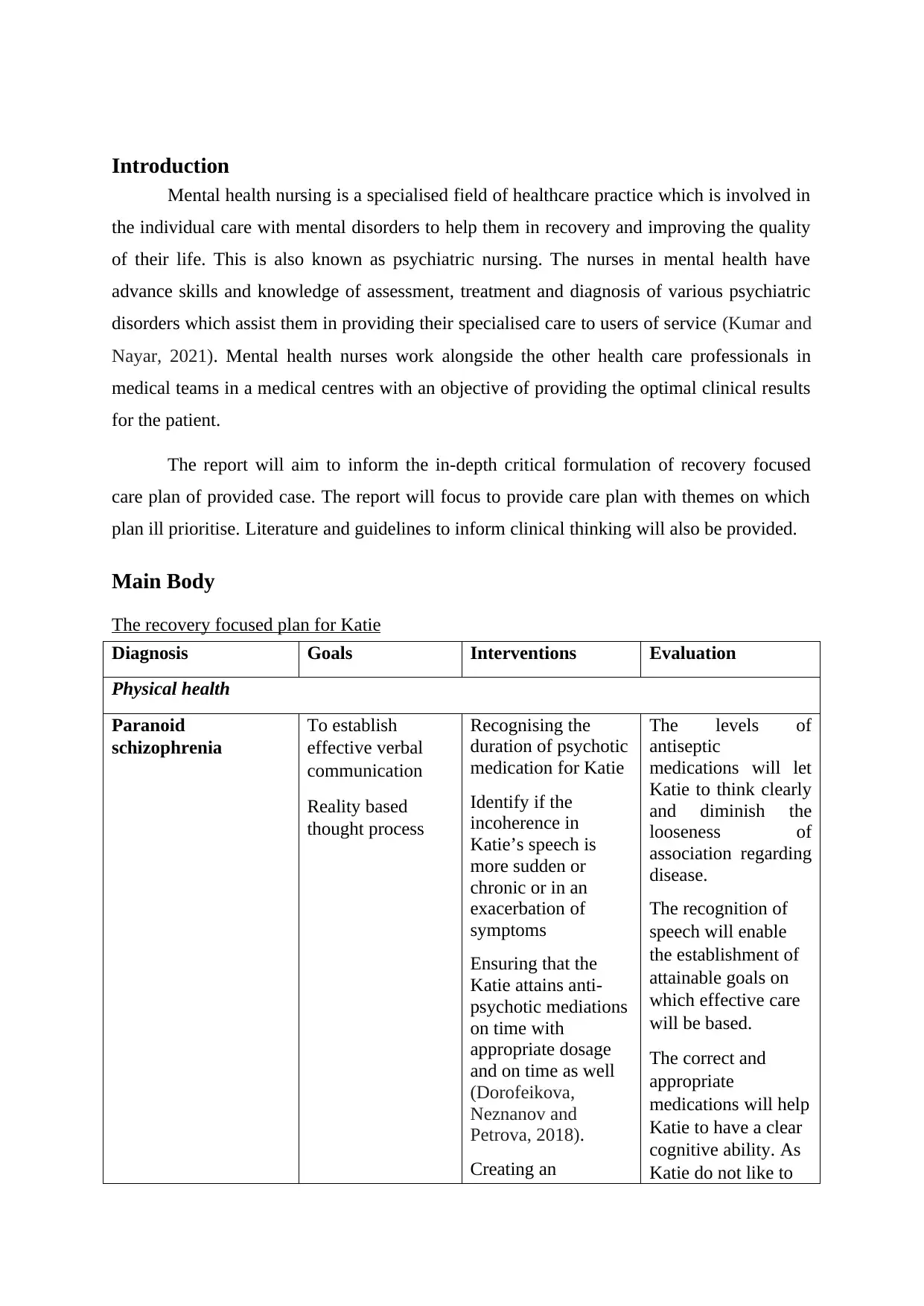
The recovery focused plan for Katie
Diagnosis Goals Interventions Evaluation
Physical health
Paranoid
schizophrenia
To establish
effective verbal
communication
Reality based
thought process
Recognising the
duration of psychotic
medication for Katie
Identify if the
incoherence in
Katie’s speech is
more sudden or
chronic or in an
exacerbation of
symptoms
Ensuring that the
Katie attains anti-
psychotic mediations
on time with
appropriate dosage
and on time as well
(Dorofeikova,
Neznanov and
Petrova, 2018).
Creating an
The levels of
antiseptic
medications will let
Katie to think clearly
and diminish the
looseness of
association regarding
disease.
The recognition of
speech will enable
the establishment of
attainable goals on
which effective care
will be based.
The correct and
appropriate
medications will help
Katie to have a clear
cognitive ability. As
Katie do not like to
Mental health nursing is a specialised field of healthcare practice which is involved in
the individual care with mental disorders to help them in recovery and improving the quality
of their life. This is also known as psychiatric nursing. The nurses in mental health have
advance skills and knowledge of assessment, treatment and diagnosis of various psychiatric
disorders which assist them in providing their specialised care to users of service (Kumar and
Nayar, 2021). Mental health nurses work alongside the other health care professionals in
medical teams in a medical centres with an objective of providing the optimal clinical results
for the patient.
The report will aim to inform the in-depth critical formulation of recovery focused
care plan of provided case. The report will focus to provide care plan with themes on which
plan ill prioritise. Literature and guidelines to inform clinical thinking will also be provided.
Main Body
The recovery focused plan for Katie
Diagnosis Goals Interventions Evaluation
Physical health
Paranoid
schizophrenia
To establish
effective verbal
communication
Reality based
thought process
Recognising the
duration of psychotic
medication for Katie
Identify if the
incoherence in
Katie’s speech is
more sudden or
chronic or in an
exacerbation of
symptoms
Ensuring that the
Katie attains anti-
psychotic mediations
on time with
appropriate dosage
and on time as well
(Dorofeikova,
Neznanov and
Petrova, 2018).
Creating an
The levels of
antiseptic
medications will let
Katie to think clearly
and diminish the
looseness of
association regarding
disease.
The recognition of
speech will enable
the establishment of
attainable goals on
which effective care
will be based.
The correct and
appropriate
medications will help
Katie to have a clear
cognitive ability. As
Katie do not like to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
environment which is
quiet and calm
take medicines, it
will be good to make
her take her
medications in front
of nurse.
Creating a calm
environment will
help Katie in
preventing
confusions
(Krzystanek, Krysta
and Skałacka, 2017).
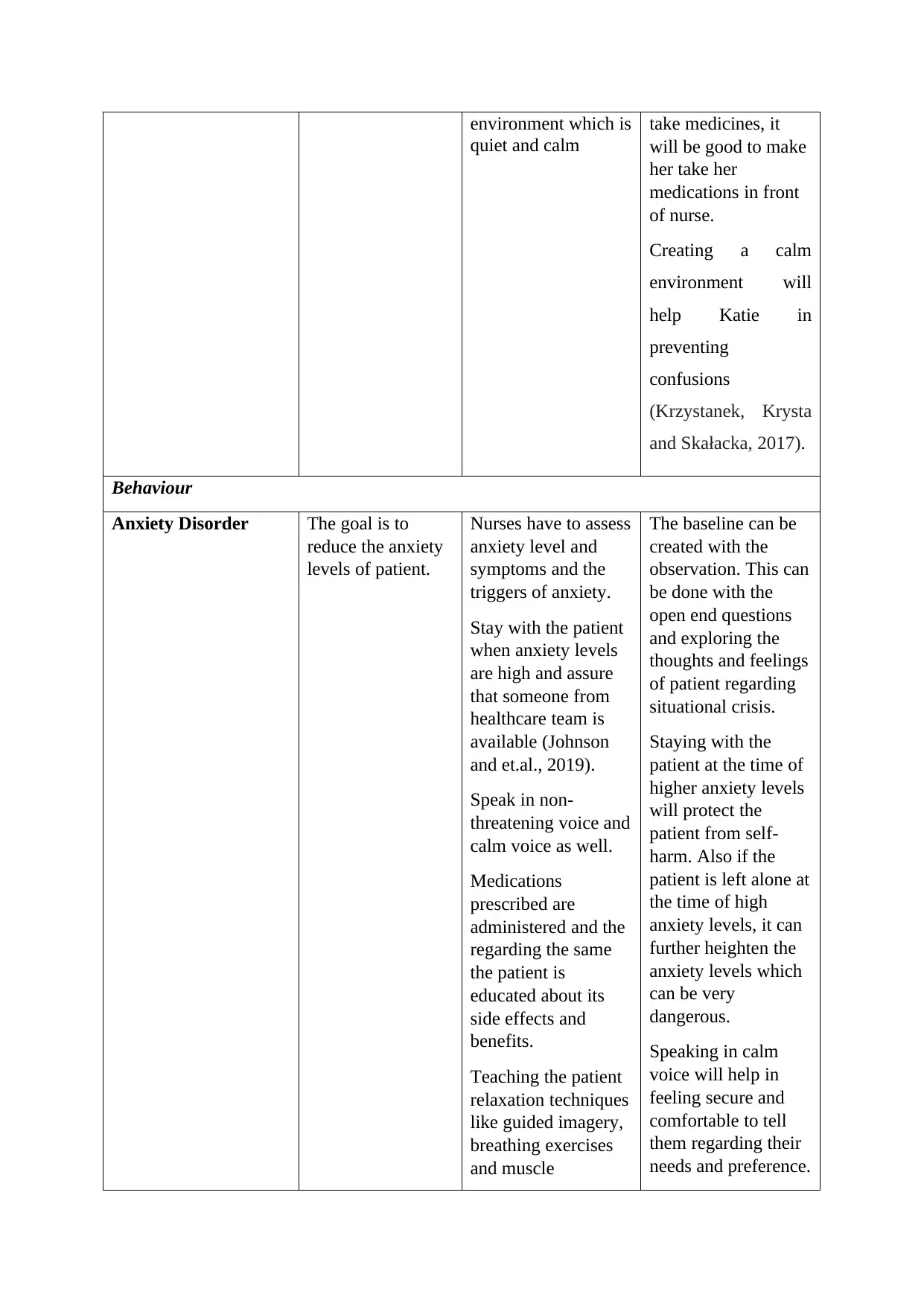
Behaviour
Anxiety Disorder The goal is to
reduce the anxiety
levels of patient.
Nurses have to assess
anxiety level and
symptoms and the
triggers of anxiety.
Stay with the patient
when anxiety levels
are high and assure
that someone from
healthcare team is
available (Johnson
and et.al., 2019).
Speak in non-
threatening voice and
calm voice as well.
Medications
prescribed are
administered and the
regarding the same
the patient is
educated about its
side effects and
benefits.
Teaching the patient
relaxation techniques
like guided imagery,
breathing exercises
and muscle
The baseline can be
created with the
observation. This can
be done with the
open end questions
and exploring the
thoughts and feelings
of patient regarding
situational crisis.
Staying with the
patient at the time of
higher anxiety levels
will protect the
patient from self-
harm. Also if the
patient is left alone at
the time of high
anxiety levels, it can
further heighten the
anxiety levels which
can be very
dangerous.
Speaking in calm
voice will help in
feeling secure and
comfortable to tell
them regarding their
needs and preference.
quiet and calm
take medicines, it
will be good to make
her take her
medications in front
of nurse.
Creating a calm
environment will
help Katie in
preventing
confusions
(Krzystanek, Krysta
and Skałacka, 2017).
Behaviour
Anxiety Disorder The goal is to
reduce the anxiety
levels of patient.
Nurses have to assess
anxiety level and
symptoms and the
triggers of anxiety.
Stay with the patient
when anxiety levels
are high and assure
that someone from
healthcare team is
available (Johnson
and et.al., 2019).
Speak in non-
threatening voice and
calm voice as well.
Medications
prescribed are
administered and the
regarding the same
the patient is
educated about its
side effects and
benefits.
Teaching the patient
relaxation techniques
like guided imagery,
breathing exercises
and muscle
The baseline can be
created with the
observation. This can
be done with the
open end questions
and exploring the
thoughts and feelings
of patient regarding
situational crisis.
Staying with the
patient at the time of
higher anxiety levels
will protect the
patient from self-
harm. Also if the
patient is left alone at
the time of high
anxiety levels, it can
further heighten the
anxiety levels which
can be very
dangerous.
Speaking in calm
voice will help in
feeling secure and
comfortable to tell
them regarding their
needs and preference.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
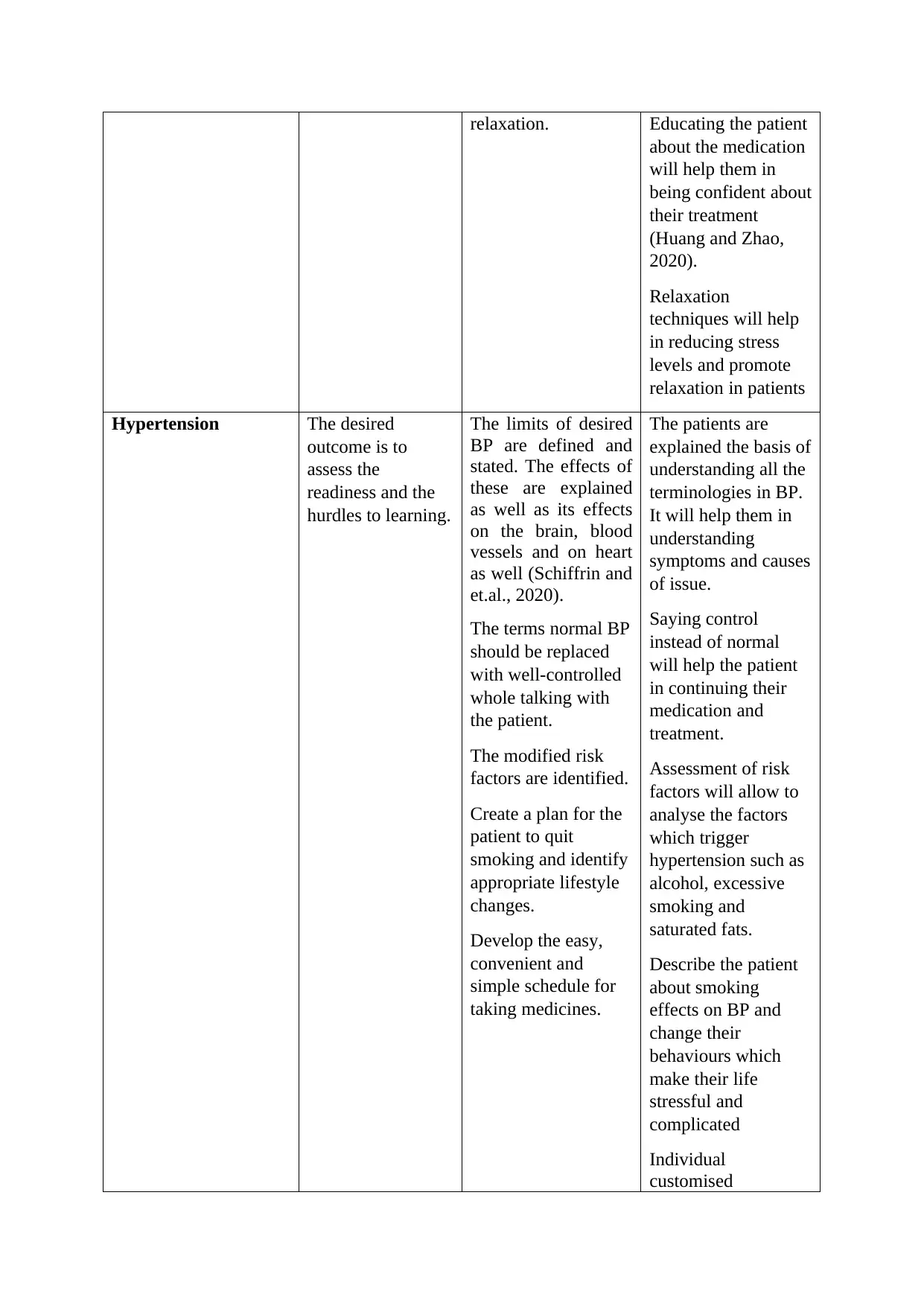
relaxation. Educating the patient
about the medication
will help them in
being confident about
their treatment
(Huang and Zhao,
2020).
Relaxation
techniques will help
in reducing stress
levels and promote
relaxation in patients
Hypertension The desired
outcome is to
assess the
readiness and the
hurdles to learning.
The limits of desired
BP are defined and
stated. The effects of
these are explained
as well as its effects
on the brain, blood
vessels and on heart
as well (Schiffrin and
et.al., 2020).
The terms normal BP
should be replaced
with well-controlled
whole talking with
the patient.
The modified risk
factors are identified.
Create a plan for the
patient to quit
smoking and identify
appropriate lifestyle
changes.
Develop the easy,
convenient and
simple schedule for
taking medicines.
The patients are
explained the basis of
understanding all the
terminologies in BP.
It will help them in
understanding
symptoms and causes
of issue.
Saying control
instead of normal
will help the patient
in continuing their
medication and
treatment.
Assessment of risk
factors will allow to
analyse the factors
which trigger
hypertension such as
alcohol, excessive
smoking and
saturated fats.
Describe the patient
about smoking
effects on BP and
change their
behaviours which
make their life
stressful and
complicated
Individual
customised
about the medication
will help them in
being confident about
their treatment
(Huang and Zhao,
2020).
Relaxation
techniques will help
in reducing stress
levels and promote
relaxation in patients
Hypertension The desired
outcome is to
assess the
readiness and the
hurdles to learning.
The limits of desired
BP are defined and
stated. The effects of
these are explained
as well as its effects
on the brain, blood
vessels and on heart
as well (Schiffrin and
et.al., 2020).
The terms normal BP
should be replaced
with well-controlled
whole talking with
the patient.
The modified risk
factors are identified.
Create a plan for the
patient to quit
smoking and identify
appropriate lifestyle
changes.
Develop the easy,
convenient and
simple schedule for
taking medicines.
The patients are
explained the basis of
understanding all the
terminologies in BP.
It will help them in
understanding
symptoms and causes
of issue.
Saying control
instead of normal
will help the patient
in continuing their
medication and
treatment.
Assessment of risk
factors will allow to
analyse the factors
which trigger
hypertension such as
alcohol, excessive
smoking and
saturated fats.
Describe the patient
about smoking
effects on BP and
change their
behaviours which
make their life
stressful and
complicated
Individual
customised
medication plans will
help in taking the
medications as per
their needs and
personal habits
(Mills, Stefanescu
and He, 2020).
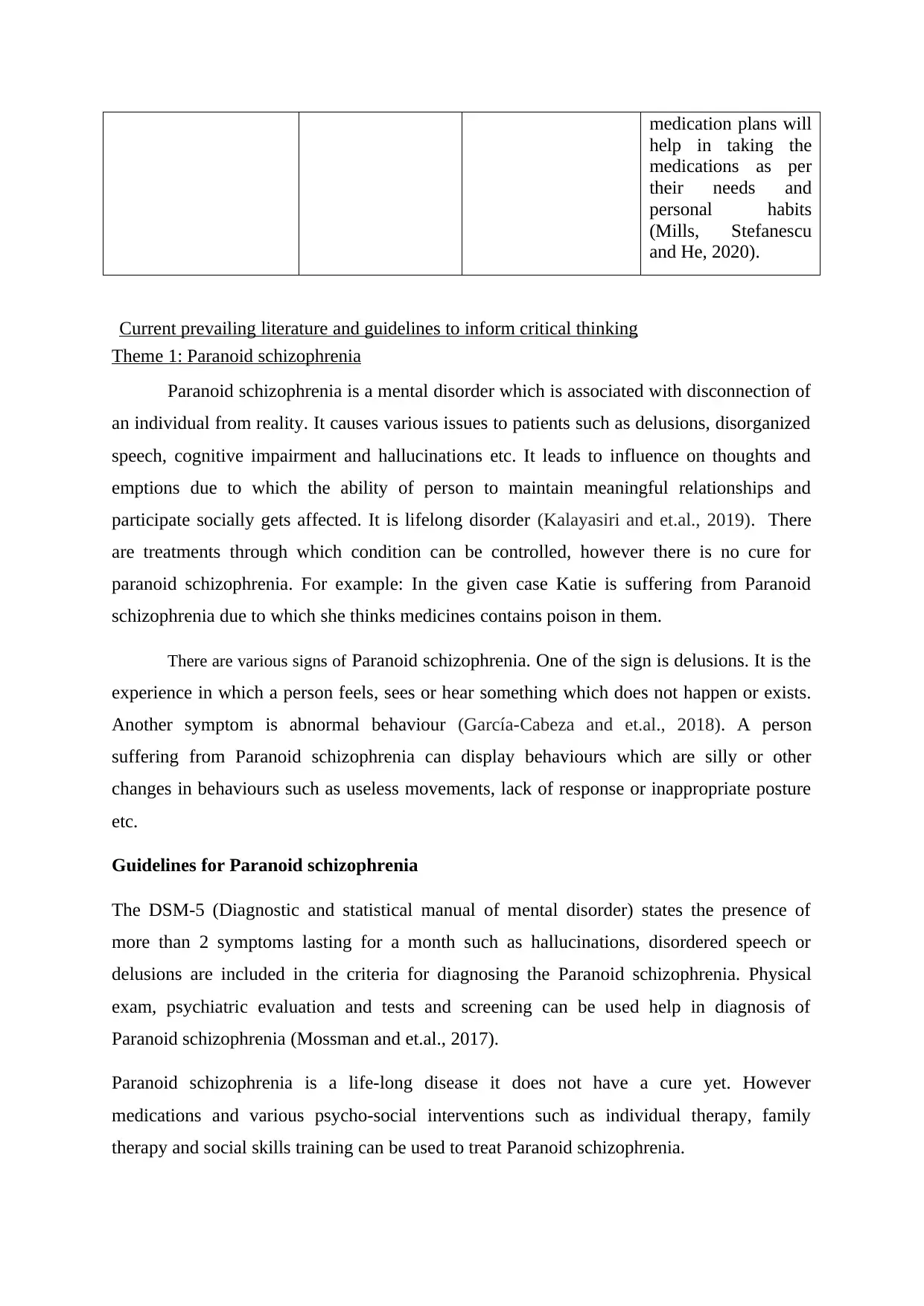
Current prevailing literature and guidelines to inform critical thinking
Theme 1: Paranoid schizophrenia
Paranoid schizophrenia is a mental disorder which is associated with disconnection of
an individual from reality. It causes various issues to patients such as delusions, disorganized
speech, cognitive impairment and hallucinations etc. It leads to influence on thoughts and
emptions due to which the ability of person to maintain meaningful relationships and
participate socially gets affected. It is lifelong disorder (Kalayasiri and et.al., 2019). There
are treatments through which condition can be controlled, however there is no cure for
paranoid schizophrenia. For example: In the given case Katie is suffering from Paranoid
schizophrenia due to which she thinks medicines contains poison in them.
There are various signs of Paranoid schizophrenia. One of the sign is delusions. It is the
experience in which a person feels, sees or hear something which does not happen or exists.
Another symptom is abnormal behaviour (García-Cabeza and et.al., 2018). A person
suffering from Paranoid schizophrenia can display behaviours which are silly or other
changes in behaviours such as useless movements, lack of response or inappropriate posture
etc.
Guidelines for Paranoid schizophrenia
The DSM-5 (Diagnostic and statistical manual of mental disorder) states the presence of
more than 2 symptoms lasting for a month such as hallucinations, disordered speech or
delusions are included in the criteria for diagnosing the Paranoid schizophrenia. Physical
exam, psychiatric evaluation and tests and screening can be used help in diagnosis of
Paranoid schizophrenia (Mossman and et.al., 2017).
Paranoid schizophrenia is a life-long disease it does not have a cure yet. However
medications and various psycho-social interventions such as individual therapy, family
therapy and social skills training can be used to treat Paranoid schizophrenia.
help in taking the
medications as per
their needs and
personal habits
(Mills, Stefanescu
and He, 2020).
Current prevailing literature and guidelines to inform critical thinking
Theme 1: Paranoid schizophrenia
Paranoid schizophrenia is a mental disorder which is associated with disconnection of
an individual from reality. It causes various issues to patients such as delusions, disorganized
speech, cognitive impairment and hallucinations etc. It leads to influence on thoughts and
emptions due to which the ability of person to maintain meaningful relationships and
participate socially gets affected. It is lifelong disorder (Kalayasiri and et.al., 2019). There
are treatments through which condition can be controlled, however there is no cure for
paranoid schizophrenia. For example: In the given case Katie is suffering from Paranoid
schizophrenia due to which she thinks medicines contains poison in them.
There are various signs of Paranoid schizophrenia. One of the sign is delusions. It is the
experience in which a person feels, sees or hear something which does not happen or exists.
Another symptom is abnormal behaviour (García-Cabeza and et.al., 2018). A person
suffering from Paranoid schizophrenia can display behaviours which are silly or other
changes in behaviours such as useless movements, lack of response or inappropriate posture
etc.
Guidelines for Paranoid schizophrenia
The DSM-5 (Diagnostic and statistical manual of mental disorder) states the presence of
more than 2 symptoms lasting for a month such as hallucinations, disordered speech or
delusions are included in the criteria for diagnosing the Paranoid schizophrenia. Physical
exam, psychiatric evaluation and tests and screening can be used help in diagnosis of
Paranoid schizophrenia (Mossman and et.al., 2017).
Paranoid schizophrenia is a life-long disease it does not have a cure yet. However
medications and various psycho-social interventions such as individual therapy, family
therapy and social skills training can be used to treat Paranoid schizophrenia.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
APA guidelines recommend that the initial assessment of a patient should involve the risk of
evaluation, their goals and preferences and treatment of patients with psychotic disorder. The
psychiatric symptoms and trauma history of patient is also assessed as well with the
assessment tobacco use, substance use, physical health and cultural factors assessment
(Rodebaugh and et.al., 2018). The APA also suggests that the mental examination, risk of
suicide, aggressive behaviours and cognitive assessment.
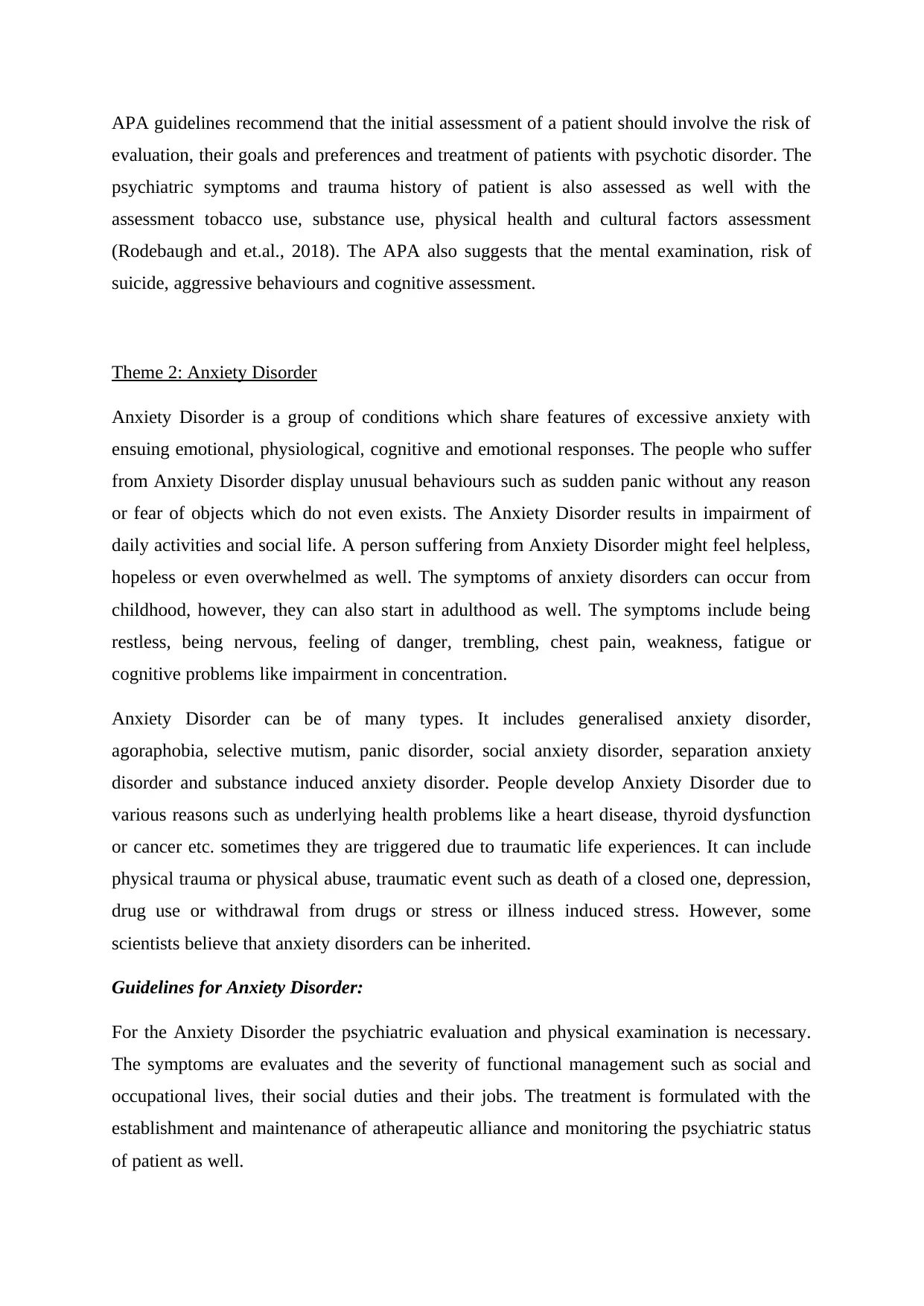
Theme 2: Anxiety Disorder
Anxiety Disorder is a group of conditions which share features of excessive anxiety with
ensuing emotional, physiological, cognitive and emotional responses. The people who suffer
from Anxiety Disorder display unusual behaviours such as sudden panic without any reason
or fear of objects which do not even exists. The Anxiety Disorder results in impairment of
daily activities and social life. A person suffering from Anxiety Disorder might feel helpless,
hopeless or even overwhelmed as well. The symptoms of anxiety disorders can occur from
childhood, however, they can also start in adulthood as well. The symptoms include being
restless, being nervous, feeling of danger, trembling, chest pain, weakness, fatigue or
cognitive problems like impairment in concentration.
Anxiety Disorder can be of many types. It includes generalised anxiety disorder,
agoraphobia, selective mutism, panic disorder, social anxiety disorder, separation anxiety
disorder and substance induced anxiety disorder. People develop Anxiety Disorder due to
various reasons such as underlying health problems like a heart disease, thyroid dysfunction
or cancer etc. sometimes they are triggered due to traumatic life experiences. It can include
physical trauma or physical abuse, traumatic event such as death of a closed one, depression,
drug use or withdrawal from drugs or stress or illness induced stress. However, some
scientists believe that anxiety disorders can be inherited.
Guidelines for Anxiety Disorder:
For the Anxiety Disorder the psychiatric evaluation and physical examination is necessary.
The symptoms are evaluates and the severity of functional management such as social and
occupational lives, their social duties and their jobs. The treatment is formulated with the
establishment and maintenance of atherapeutic alliance and monitoring the psychiatric status
of patient as well.
evaluation, their goals and preferences and treatment of patients with psychotic disorder. The
psychiatric symptoms and trauma history of patient is also assessed as well with the
assessment tobacco use, substance use, physical health and cultural factors assessment
(Rodebaugh and et.al., 2018). The APA also suggests that the mental examination, risk of
suicide, aggressive behaviours and cognitive assessment.
Theme 2: Anxiety Disorder
Anxiety Disorder is a group of conditions which share features of excessive anxiety with
ensuing emotional, physiological, cognitive and emotional responses. The people who suffer
from Anxiety Disorder display unusual behaviours such as sudden panic without any reason
or fear of objects which do not even exists. The Anxiety Disorder results in impairment of
daily activities and social life. A person suffering from Anxiety Disorder might feel helpless,
hopeless or even overwhelmed as well. The symptoms of anxiety disorders can occur from
childhood, however, they can also start in adulthood as well. The symptoms include being
restless, being nervous, feeling of danger, trembling, chest pain, weakness, fatigue or
cognitive problems like impairment in concentration.
Anxiety Disorder can be of many types. It includes generalised anxiety disorder,
agoraphobia, selective mutism, panic disorder, social anxiety disorder, separation anxiety
disorder and substance induced anxiety disorder. People develop Anxiety Disorder due to
various reasons such as underlying health problems like a heart disease, thyroid dysfunction
or cancer etc. sometimes they are triggered due to traumatic life experiences. It can include
physical trauma or physical abuse, traumatic event such as death of a closed one, depression,
drug use or withdrawal from drugs or stress or illness induced stress. However, some
scientists believe that anxiety disorders can be inherited.
Guidelines for Anxiety Disorder:
For the Anxiety Disorder the psychiatric evaluation and physical examination is necessary.
The symptoms are evaluates and the severity of functional management such as social and
occupational lives, their social duties and their jobs. The treatment is formulated with the
establishment and maintenance of atherapeutic alliance and monitoring the psychiatric status
of patient as well.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Theme 3: Hypertension
Hypertension is the term which is used for high Blood pressures in medical terms. In
hypertension is categorised essential or primary or sometimes as secondary as per identified
or pathological condition like renal disease or aldosteronism. There are various levels of
hypertension such as normal blood pressure, prehypertension, Stage-1 hypertension and
stage-2 hypertension. Hyper tension are very dangerous as it can make hard for the heart to
pump blood to the body that lead to increased risk of heart failure and hardening of arteries
(Wang and et.al., 2018).
As there is not an exact cause of hypertension but some other causes are identified such as
being overweight, smoking habits, high salted diet and genetic as well. The primary cause of
hyper tension makes about most of the hypertension and the secondary hypertension can
make high blood pressure an identifiable cause.
There are various people how do not realise they have hypertension as the symptoms cannot
be identified. However some most common symptoms of hypertension such as buzzing of
ears, fatigue, nose bleeding, blurred vision, chest pain, difficulty in breathing and fatigue as
well. If a person is diagnosed with high blood pressure, it becomes important to follow an
appropriate nursing diagnosis and a nursing care plan for hypertension. It can help in
reducing the effects of hypertension and also maintain the quality of life high of the patient.
Guidelines for treatment:
Mental Health Act, 1983
The act states the legislation which covers treatment, rights of people and assessment of
people with mental disorders. In the act the people which are detained needs urgent treatment.
For a mental health disorder or at a risk to themselves or as well others. The government have
made some temporary changes in the Act due to coronavirus.
The advice for carers and families is also provided in the Act. The act states that the
people who are detained have to stay in hospital or in a mental health tribunal. The act
provides right to visit and those arrangements depends upon hospitals (Glover-Thomas,
2018). The doctors can discuss the treatment of plan with the relatives of patients. The
hospital accommodations of the patient should be gender appropriate and age appropriate.
Hypertension is the term which is used for high Blood pressures in medical terms. In
hypertension is categorised essential or primary or sometimes as secondary as per identified
or pathological condition like renal disease or aldosteronism. There are various levels of
hypertension such as normal blood pressure, prehypertension, Stage-1 hypertension and
stage-2 hypertension. Hyper tension are very dangerous as it can make hard for the heart to
pump blood to the body that lead to increased risk of heart failure and hardening of arteries
(Wang and et.al., 2018).
As there is not an exact cause of hypertension but some other causes are identified such as
being overweight, smoking habits, high salted diet and genetic as well. The primary cause of
hyper tension makes about most of the hypertension and the secondary hypertension can
make high blood pressure an identifiable cause.
There are various people how do not realise they have hypertension as the symptoms cannot
be identified. However some most common symptoms of hypertension such as buzzing of
ears, fatigue, nose bleeding, blurred vision, chest pain, difficulty in breathing and fatigue as
well. If a person is diagnosed with high blood pressure, it becomes important to follow an
appropriate nursing diagnosis and a nursing care plan for hypertension. It can help in
reducing the effects of hypertension and also maintain the quality of life high of the patient.
Guidelines for treatment:
Mental Health Act, 1983
The act states the legislation which covers treatment, rights of people and assessment of
people with mental disorders. In the act the people which are detained needs urgent treatment.
For a mental health disorder or at a risk to themselves or as well others. The government have
made some temporary changes in the Act due to coronavirus.
The advice for carers and families is also provided in the Act. The act states that the
people who are detained have to stay in hospital or in a mental health tribunal. The act
provides right to visit and those arrangements depends upon hospitals (Glover-Thomas,
2018). The doctors can discuss the treatment of plan with the relatives of patients. The
hospital accommodations of the patient should be gender appropriate and age appropriate.
The patients have the right to raise concerns and their worries with the nurses and doctors. In
the case of Katie, Section-3 of Mental Health Act is applicable. It states that the patient can
be admitted to hospital and detain them there for the time period. The act states that the
hospitals must provide the treatment on the basis of degree of nature, protection and safety of
patient and available appropriate medical treatment (Solanki, 2020).
the case of Katie, Section-3 of Mental Health Act is applicable. It states that the patient can
be admitted to hospital and detain them there for the time period. The act states that the
hospitals must provide the treatment on the basis of degree of nature, protection and safety of
patient and available appropriate medical treatment (Solanki, 2020).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References:
Books and journals:
Dorofeikova, M., Neznanov, N. and Petrova, N., 2018. Cognitive deficit in patients with
paranoid schizophrenia: its clinical and laboratory correlates. Psychiatry
research. 262. pp.542-548.
García-Cabeza, I. and et.al., 2018. Adherence, insight and disability in paranoid
schizophrenia. Psychiatry research. 270. pp.274-280.
Glover-Thomas, N., 2018. Decision-Making Behaviour under the Mental Health Act 1983
and Its Impact on Mental Health Tribunals: An English Perspective. Laws, 7(2), p.12.
Huang, Y. and Zhao, N., 2020. Generalized anxiety disorder, depressive symptoms and sleep
quality during COVID-19 outbreak in China: a web-based cross-sectional
survey. Psychiatry research. 288. p.112954.
Johnson, S.U. and et.al., 2019. Psychometric properties of the general anxiety disorder 7-item
(GAD-7) scale in a heterogeneous psychiatric sample. Frontiers in psychology. 10.
p.1713.
Kalayasiri, R. and et.al., 2019. Paranoid schizophrenia and methamphetamine-induced
paranoia are both characterized by a similar LINE-1 partial methylation profile, which
is more pronounced in paranoid schizophrenia. Schizophrenia research. 208. pp.221-
227.
Krzystanek, M., Krysta, K. and Skałacka, K., 2017. Treatment compliance in the long-term
paranoid schizophrenia telemedicine study. Journal of technology in behavioral
science. 2(2). pp.84-87.
Kumar, A. and Nayar, K.R., 2021. COVID 19 and its mental health consequences. Journal of
Mental Health. 30(1). pp.1-2.
Mills, K.T., Stefanescu, A. and He, J., 2020. The global epidemiology of
hypertension. Nature Reviews Nephrology. 16(4). pp.223-237.
Mossman, S.A. and et.al., 2017. The generalized anxiety disorder 7-item (GAD-7) scale in
adolescents with generalized anxiety disorder: Signal detection and validation. Annals
of clinical psychiatry: official journal of the American Academy of Clinical
Psychiatrists. 29(4). p.227.
Rodebaugh, T.L. and et.al., 2018. Does centrality in a cross-sectional network suggest
intervention targets for social anxiety disorder?. Journal of consulting and clinical
psychology. 86(10). p.831.
Schiffrin, E.L. and et.al., 2020. Hypertension and COVID-19. American journal of
hypertension. 33(5). pp.373-374.
Solanki, J., 2020. Experiences of adults from a Black Minority Ethnic (BME) background
who have been detained as inpatients under the Mental Health Act (1983) (Doctoral
dissertation, University of Essex).
Wang, Z. and et.al., 2018. Status of hypertension in China: results from the China
hypertension survey, 2012–2015. Circulation. 137(22). pp.2344-2356.
Books and journals:
Dorofeikova, M., Neznanov, N. and Petrova, N., 2018. Cognitive deficit in patients with
paranoid schizophrenia: its clinical and laboratory correlates. Psychiatry
research. 262. pp.542-548.
García-Cabeza, I. and et.al., 2018. Adherence, insight and disability in paranoid
schizophrenia. Psychiatry research. 270. pp.274-280.
Glover-Thomas, N., 2018. Decision-Making Behaviour under the Mental Health Act 1983
and Its Impact on Mental Health Tribunals: An English Perspective. Laws, 7(2), p.12.
Huang, Y. and Zhao, N., 2020. Generalized anxiety disorder, depressive symptoms and sleep
quality during COVID-19 outbreak in China: a web-based cross-sectional
survey. Psychiatry research. 288. p.112954.
Johnson, S.U. and et.al., 2019. Psychometric properties of the general anxiety disorder 7-item
(GAD-7) scale in a heterogeneous psychiatric sample. Frontiers in psychology. 10.
p.1713.
Kalayasiri, R. and et.al., 2019. Paranoid schizophrenia and methamphetamine-induced
paranoia are both characterized by a similar LINE-1 partial methylation profile, which
is more pronounced in paranoid schizophrenia. Schizophrenia research. 208. pp.221-
227.
Krzystanek, M., Krysta, K. and Skałacka, K., 2017. Treatment compliance in the long-term
paranoid schizophrenia telemedicine study. Journal of technology in behavioral
science. 2(2). pp.84-87.
Kumar, A. and Nayar, K.R., 2021. COVID 19 and its mental health consequences. Journal of
Mental Health. 30(1). pp.1-2.
Mills, K.T., Stefanescu, A. and He, J., 2020. The global epidemiology of
hypertension. Nature Reviews Nephrology. 16(4). pp.223-237.
Mossman, S.A. and et.al., 2017. The generalized anxiety disorder 7-item (GAD-7) scale in
adolescents with generalized anxiety disorder: Signal detection and validation. Annals
of clinical psychiatry: official journal of the American Academy of Clinical
Psychiatrists. 29(4). p.227.
Rodebaugh, T.L. and et.al., 2018. Does centrality in a cross-sectional network suggest
intervention targets for social anxiety disorder?. Journal of consulting and clinical
psychology. 86(10). p.831.
Schiffrin, E.L. and et.al., 2020. Hypertension and COVID-19. American journal of
hypertension. 33(5). pp.373-374.
Solanki, J., 2020. Experiences of adults from a Black Minority Ethnic (BME) background
who have been detained as inpatients under the Mental Health Act (1983) (Doctoral
dissertation, University of Essex).
Wang, Z. and et.al., 2018. Status of hypertension in China: results from the China
hypertension survey, 2012–2015. Circulation. 137(22). pp.2344-2356.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





