University Mental Health Project: Staff Training and Patient Care
VerifiedAdded on 2021/10/13
|11
|2500
|40
Project
AI Summary
This project addresses the stigmatization and ill-treatment of mentally ill patients by healthcare staff, a significant issue in mental health facilities. The project explores current systems, highlighting the ineffectiveness of existing practices due to factors like lack of awareness, burnout, and inadequate training. The proposed solution involves an integrative education, training, and awareness program for junior mental health nursing staff, focusing on handling challenging behaviors, compassionate communication, and stress management through mindfulness. The project aligns with clinical governance principles, emphasizing clinical effectiveness, risk management, and patient involvement. The effectiveness of the intervention will be evaluated over six months through practice improvements, manager feedback, and patient satisfaction surveys. The project aims to provide evidence-based interventions to improve the quality of care and patient outcomes, and the results will determine the potential for wider implementation.

Running head: PROJECT ON MENTAL HEALTH
Project on mental health
Name of the student:
Name of the university:
Author note:
Project on mental health
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
PROJECT ON MENTAL HEALTH
Table of Contents
Introduction and description of the issue...................................................................................2
Current systems and practices and its ineffectiveness:..............................................................2
Clinical governance:...................................................................................................................3
Proposed solution:......................................................................................................................4
Evaluating the effectiveness:......................................................................................................5
Conclusion:................................................................................................................................6
References:.................................................................................................................................7
Appendix:...................................................................................................................................9
PROJECT ON MENTAL HEALTH
Table of Contents
Introduction and description of the issue...................................................................................2
Current systems and practices and its ineffectiveness:..............................................................2
Clinical governance:...................................................................................................................3
Proposed solution:......................................................................................................................4
Evaluating the effectiveness:......................................................................................................5
Conclusion:................................................................................................................................6
References:.................................................................................................................................7
Appendix:...................................................................................................................................9
2
PROJECT ON MENTAL HEALTH
Introduction and description of the issue:
Mental illness has been subjected to stigmatization and discrimination since
decades in the past, and even though the innovative transition and modernization of the
society and the health care industry has helped in mental illnesses acquiring the status of a
disease, there is still a considerable stigma associated with the mental illness and people that
suffer from it. As discussed by Malla, Joober and Garcia (2015), the stigma associated with
mental health still operates in the society, and although it is internalized by the individuals,
the stigmatization is attributed by the health care professions itself. The impact of
stigmatization and discrimination on the mentally ill patients committed by the mental health
care staff itself can lead to various negative outcomes for the patients, including lack of
responsiveness, loss of help-seeking behaviour, aggression and irritation, and can even lead
to violence by provocation due to the ill-treatment or behaviour (Michaels et al., 2017). This
project will aim to explore the reasons behind the ill-treatment of mental health staff to
patients, the relation with lack of education and awareness, and propose intervention
strategies to improve practice with respect to clinical governance framework. Current systems
and practices and its ineffectiveness:
Kopera et al. (2015) stated that there is still a prevalence of more significant barriers
to availing mental health care than physical health care in society. Elaborating further, 70%
of the mentally ill young adults and adults do not access care services due to the fear of
stigma, especially for conditions such as depression, anxiety disorders and paranoia. The
researchers are of the opinion that the impact of lack of knowledge and awareness regarding
the mental illnesses are the most important contributing factors to the stigmatizing behaviours
of the mental health staff, especially for the remote areas. In many cases, the extreme
workload and burnout of the mental health staff can also be considered as potent contributing
factors to the inadequate and stigmatizing behaviour of the staff to mentally ill unstable staff.
PROJECT ON MENTAL HEALTH
Introduction and description of the issue:
Mental illness has been subjected to stigmatization and discrimination since
decades in the past, and even though the innovative transition and modernization of the
society and the health care industry has helped in mental illnesses acquiring the status of a
disease, there is still a considerable stigma associated with the mental illness and people that
suffer from it. As discussed by Malla, Joober and Garcia (2015), the stigma associated with
mental health still operates in the society, and although it is internalized by the individuals,
the stigmatization is attributed by the health care professions itself. The impact of
stigmatization and discrimination on the mentally ill patients committed by the mental health
care staff itself can lead to various negative outcomes for the patients, including lack of
responsiveness, loss of help-seeking behaviour, aggression and irritation, and can even lead
to violence by provocation due to the ill-treatment or behaviour (Michaels et al., 2017). This
project will aim to explore the reasons behind the ill-treatment of mental health staff to
patients, the relation with lack of education and awareness, and propose intervention
strategies to improve practice with respect to clinical governance framework. Current systems
and practices and its ineffectiveness:
Kopera et al. (2015) stated that there is still a prevalence of more significant barriers
to availing mental health care than physical health care in society. Elaborating further, 70%
of the mentally ill young adults and adults do not access care services due to the fear of
stigma, especially for conditions such as depression, anxiety disorders and paranoia. The
researchers are of the opinion that the impact of lack of knowledge and awareness regarding
the mental illnesses are the most important contributing factors to the stigmatizing behaviours
of the mental health staff, especially for the remote areas. In many cases, the extreme
workload and burnout of the mental health staff can also be considered as potent contributing
factors to the inadequate and stigmatizing behaviour of the staff to mentally ill unstable staff.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
PROJECT ON MENTAL HEALTH
Elaborating more, the staffing shortage situation of the mental health care sector is
alarming, with respect to the nurse to patient ratio. The burnout and emotional exhaustion due
to working multiple shifts and handling more mentally ill patients than a nurse can handle
often has a deep impact on the behaviour and responsiveness of the staff (Henderson et al.,
2014). The impact of the burnout ranges from depression, aggression, depersonalization and
low personal achievement, which in turn has been reported to affect the behaviour, nature and
professional competence of the staff as well. Although, the lack of education and awareness
on handling mentally ill patients cannot be ignored in this context. First and foremost, the
staff often lacks applicative practice knowledge regarding handling mentally ill patients,
especially with challenging behaviour. Many research studies have mentioned that the
specialist mental nursing staff is a rather expensive and overstretched resource, which cannot
be accessed for minor causes. As a result, the staff that handles mental health emergencies
lack specialist expertise and knowledge in handling patients. Moreover, the gap between
theoretical and practice knowledge and expertise in the entry level mental health staff in such
cases develop more stigmatizing attitude. Hence, undoubtedly, there is need for education
and training to the mental health staff on both patient handling, compassionate approach, and
dealing with burnout (Ellis, 2017).
Clinical governance:
Clinical governance is a systematic framework which facilitates the completion of
improvement of the care practices and maintenance of the continuous cycle of improvement.
Clinical governance has the purpose to ensure that the consumers or patients can get safe and
effective care services through integrated corporate and clinical governance systems. Within
the context of mental health, the aspect of clinical governance is associated with clinical risk
management, improving care, and incorporating consumer perspective to enhance care. There
are seven pillars to the clinical governance, clinical effectiveness, risk management, patient
PROJECT ON MENTAL HEALTH
Elaborating more, the staffing shortage situation of the mental health care sector is
alarming, with respect to the nurse to patient ratio. The burnout and emotional exhaustion due
to working multiple shifts and handling more mentally ill patients than a nurse can handle
often has a deep impact on the behaviour and responsiveness of the staff (Henderson et al.,
2014). The impact of the burnout ranges from depression, aggression, depersonalization and
low personal achievement, which in turn has been reported to affect the behaviour, nature and
professional competence of the staff as well. Although, the lack of education and awareness
on handling mentally ill patients cannot be ignored in this context. First and foremost, the
staff often lacks applicative practice knowledge regarding handling mentally ill patients,
especially with challenging behaviour. Many research studies have mentioned that the
specialist mental nursing staff is a rather expensive and overstretched resource, which cannot
be accessed for minor causes. As a result, the staff that handles mental health emergencies
lack specialist expertise and knowledge in handling patients. Moreover, the gap between
theoretical and practice knowledge and expertise in the entry level mental health staff in such
cases develop more stigmatizing attitude. Hence, undoubtedly, there is need for education
and training to the mental health staff on both patient handling, compassionate approach, and
dealing with burnout (Ellis, 2017).
Clinical governance:
Clinical governance is a systematic framework which facilitates the completion of
improvement of the care practices and maintenance of the continuous cycle of improvement.
Clinical governance has the purpose to ensure that the consumers or patients can get safe and
effective care services through integrated corporate and clinical governance systems. Within
the context of mental health, the aspect of clinical governance is associated with clinical risk
management, improving care, and incorporating consumer perspective to enhance care. There
are seven pillars to the clinical governance, clinical effectiveness, risk management, patient
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
PROJECT ON MENTAL HEALTH
experience and involvement, communication, resource effectiveness, strategic effectiveness,
and learning effectiveness. In this case, the most applicable principles to clinical governance
that can be employed to the project includes clinical effectiveness, risk management, and
patient experience and involvement (Van Zwanenberg & Edwards, 2018).
Elaborating further, clinical effectiveness is associated with improving the care
practices in accordance with the evidence based practice festering optimal clinical
effectiveness of the outcome. In this case, the stigmatization and ill treatment of the mentally
ill patients by the inadequately trained and over-timing mental health staff requires evidence
based interventions that can address the root of the issue and bring forth optimal and
clinically effective results (Leroux, 2018). Similarly, the impact of the stigmatization and ill
treatment has been reported to affect patient safety and has even resulted in considerable
harm and injury for the patients. The mistreatment in the facility has also been a great impact
on the emotional and psychological health of the patients as well. Overall, this is a major
clinical risk with the intervention proposed in the project will attempt to address. Lastly,
consumer voice is an integral component of the clinical governance framework, in this case
as well, the grievances and preferences of the patients and their families need to be
acknowledged and incorporated while designing the interventions to train and educate the
staff.
Proposed solution:
The solution proposed for addressing this alarming public health priority includes an
integrative and interactive education, training and awareness program for the junior mental
health nursing staff. As discussed by Yanos et al. (2015), the lack of awareness and practical
application based training in the nursing staff regarding how to deal with mentally ill patients,
especially with unstable and difficult to contain behaviour. Hence the first strategy will be to
arrange a training program for the junior mental health nurses in our facility and provide
PROJECT ON MENTAL HEALTH
experience and involvement, communication, resource effectiveness, strategic effectiveness,
and learning effectiveness. In this case, the most applicable principles to clinical governance
that can be employed to the project includes clinical effectiveness, risk management, and
patient experience and involvement (Van Zwanenberg & Edwards, 2018).
Elaborating further, clinical effectiveness is associated with improving the care
practices in accordance with the evidence based practice festering optimal clinical
effectiveness of the outcome. In this case, the stigmatization and ill treatment of the mentally
ill patients by the inadequately trained and over-timing mental health staff requires evidence
based interventions that can address the root of the issue and bring forth optimal and
clinically effective results (Leroux, 2018). Similarly, the impact of the stigmatization and ill
treatment has been reported to affect patient safety and has even resulted in considerable
harm and injury for the patients. The mistreatment in the facility has also been a great impact
on the emotional and psychological health of the patients as well. Overall, this is a major
clinical risk with the intervention proposed in the project will attempt to address. Lastly,
consumer voice is an integral component of the clinical governance framework, in this case
as well, the grievances and preferences of the patients and their families need to be
acknowledged and incorporated while designing the interventions to train and educate the
staff.
Proposed solution:
The solution proposed for addressing this alarming public health priority includes an
integrative and interactive education, training and awareness program for the junior mental
health nursing staff. As discussed by Yanos et al. (2015), the lack of awareness and practical
application based training in the nursing staff regarding how to deal with mentally ill patients,
especially with unstable and difficult to contain behaviour. Hence the first strategy will be to
arrange a training program for the junior mental health nurses in our facility and provide
5
PROJECT ON MENTAL HEALTH
them interactive seminar based education and training on handling mental patients with
challenging behaviour (Thornicroft et al., 2016).
Secondly, the lack of understanding on compassionate and empathetic verbal and
nonverbal communication training and practice protocol in active therapeutic engagement
with such patients had been identified as a key challenge for the nurses. In this case as well,
training workshops designed specifically in a bi-monthly manner for the selected nurses will
be the second strategy of the program. Thirdly, the nurses often lack understanding on how to
overcome stress, emotional exhaustion, and burnout; they often do not know how to avoid
letting the depersonalizing impact of the exhaustion affecting professional competence and
patient care. Hence, the third phase of the intervention program will be mindfulness based
therapy training to help the selected staff learn and use the non-pharmacological technique to
cope with stress and enhance professional competence (Corrigan, Druss & Perlick, 2014).
Evaluating the effectiveness:
The project will take place for 6 consecutive months and the education workshops
will continue simultaneously with the regular shifts of the nurses so that the patient care is not
affected in any manner. The sessions will be arranged taking the aid of the nurse managers
and shift allocators to help the nurses participate after the shift hours and each session will be
of 30 minutes. The evaluation parameters for the project will be based on the practice
improvement of the nurses in the units, feedback from the nurse manager on performance
improvement, and the feedback shared by the patient and their families with respect to their
satisfaction. Monthly audits will be performed to ensure that the rate of practice improvement
and the end results of each audit will be added to the final audits after the completion of the
entire program. The data will be statistically analysed and the interpretation will be done by
the project management community.
PROJECT ON MENTAL HEALTH
them interactive seminar based education and training on handling mental patients with
challenging behaviour (Thornicroft et al., 2016).
Secondly, the lack of understanding on compassionate and empathetic verbal and
nonverbal communication training and practice protocol in active therapeutic engagement
with such patients had been identified as a key challenge for the nurses. In this case as well,
training workshops designed specifically in a bi-monthly manner for the selected nurses will
be the second strategy of the program. Thirdly, the nurses often lack understanding on how to
overcome stress, emotional exhaustion, and burnout; they often do not know how to avoid
letting the depersonalizing impact of the exhaustion affecting professional competence and
patient care. Hence, the third phase of the intervention program will be mindfulness based
therapy training to help the selected staff learn and use the non-pharmacological technique to
cope with stress and enhance professional competence (Corrigan, Druss & Perlick, 2014).
Evaluating the effectiveness:
The project will take place for 6 consecutive months and the education workshops
will continue simultaneously with the regular shifts of the nurses so that the patient care is not
affected in any manner. The sessions will be arranged taking the aid of the nurse managers
and shift allocators to help the nurses participate after the shift hours and each session will be
of 30 minutes. The evaluation parameters for the project will be based on the practice
improvement of the nurses in the units, feedback from the nurse manager on performance
improvement, and the feedback shared by the patient and their families with respect to their
satisfaction. Monthly audits will be performed to ensure that the rate of practice improvement
and the end results of each audit will be added to the final audits after the completion of the
entire program. The data will be statistically analysed and the interpretation will be done by
the project management community.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
PROJECT ON MENTAL HEALTH
Conclusion:
On a concluding note, the project addresses a grave practice issue which is one of the
fundamental contributor to the reduced consumer satisfaction in the mental health facilities.
The interventions proposed are in accordance and respond to the most applicable pillars of
clinical governance and are designed with respect to best practice evidences. The evaluation
of the project will provide data on whether the intervention had been successful or not, and
based on the results, whether the project should be replicated on a large scale will be
determined.
PROJECT ON MENTAL HEALTH
Conclusion:
On a concluding note, the project addresses a grave practice issue which is one of the
fundamental contributor to the reduced consumer satisfaction in the mental health facilities.
The interventions proposed are in accordance and respond to the most applicable pillars of
clinical governance and are designed with respect to best practice evidences. The evaluation
of the project will provide data on whether the intervention had been successful or not, and
based on the results, whether the project should be replicated on a large scale will be
determined.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
PROJECT ON MENTAL HEALTH
References:
Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The impact of mental illness stigma
on seeking and participating in mental health care. Psychological Science in the
Public Interest, 15(2), 37-70.
Ellis, R. (2017). Heritage and Stigma. Co-producing and communicating the histories of
mental health and learning disability. Medical humanities, 43(2), 92-98.
Henderson, C., Noblett, J., Parke, H., Clement, S., Caffrey, A., Gale-Grant, O., ... &
Thornicroft, G. (2014). Mental health-related stigma in health care and mental health-
care settings. The Lancet Psychiatry, 1(6), 467-482.
Kopera, M., Suszek, H., Bonar, E., Myszka, M., Gmaj, B., Ilgen, M., & Wojnar, M. (2015).
Evaluating explicit and implicit stigma of mental illness in mental health
professionals and medical students. Community mental health journal, 51(5), 628-
634.
Malla, A., Joober, R., & Garcia, A. (2015). “Mental illness is like any other medical illness”:
a critical examination of the statement and its impact on patient care and
society. Journal of psychiatry & neuroscience: JPN, 40(3), 147.
Michaels, P. J., López, M., Rüsch, N., & Corrigan, P. W. (2017). Constructs and concepts
comprising the stigma of mental illness. Psychology, Society, & Education, 4(2), 183-
194.
Thornicroft, G., Mehta, N., Clement, S., Evans-Lacko, S., Doherty, M., Rose, D., ... &
Henderson, C. (2016). Evidence for effective interventions to reduce mental-health-
related stigma and discrimination. The Lancet, 387(10023), 1123-1132.
PROJECT ON MENTAL HEALTH
References:
Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The impact of mental illness stigma
on seeking and participating in mental health care. Psychological Science in the
Public Interest, 15(2), 37-70.
Ellis, R. (2017). Heritage and Stigma. Co-producing and communicating the histories of
mental health and learning disability. Medical humanities, 43(2), 92-98.
Henderson, C., Noblett, J., Parke, H., Clement, S., Caffrey, A., Gale-Grant, O., ... &
Thornicroft, G. (2014). Mental health-related stigma in health care and mental health-
care settings. The Lancet Psychiatry, 1(6), 467-482.
Kopera, M., Suszek, H., Bonar, E., Myszka, M., Gmaj, B., Ilgen, M., & Wojnar, M. (2015).
Evaluating explicit and implicit stigma of mental illness in mental health
professionals and medical students. Community mental health journal, 51(5), 628-
634.
Malla, A., Joober, R., & Garcia, A. (2015). “Mental illness is like any other medical illness”:
a critical examination of the statement and its impact on patient care and
society. Journal of psychiatry & neuroscience: JPN, 40(3), 147.
Michaels, P. J., López, M., Rüsch, N., & Corrigan, P. W. (2017). Constructs and concepts
comprising the stigma of mental illness. Psychology, Society, & Education, 4(2), 183-
194.
Thornicroft, G., Mehta, N., Clement, S., Evans-Lacko, S., Doherty, M., Rose, D., ... &
Henderson, C. (2016). Evidence for effective interventions to reduce mental-health-
related stigma and discrimination. The Lancet, 387(10023), 1123-1132.

8
PROJECT ON MENTAL HEALTH
Yanos, P. T., Lucksted, A., Drapalski, A. L., Roe, D., & Lysaker, P. (2015). Interventions
targeting mental health self-stigma: A review and comparison. Psychiatric
rehabilitation journal, 38(2), 171.
Van Zwanenberg, T., & Edwards, C. (2018). Clinical governance in primary care. In Clinical
Governance in Primary Care (pp. 17-30). CRC Press.
Leroux, P. (2018). Clinical Effectiveness in Psychotherapy and Mental Health: Strategies
and Resources for the Effective Clinical Governance. Routledge.
PROJECT ON MENTAL HEALTH
Yanos, P. T., Lucksted, A., Drapalski, A. L., Roe, D., & Lysaker, P. (2015). Interventions
targeting mental health self-stigma: A review and comparison. Psychiatric
rehabilitation journal, 38(2), 171.
Van Zwanenberg, T., & Edwards, C. (2018). Clinical governance in primary care. In Clinical
Governance in Primary Care (pp. 17-30). CRC Press.
Leroux, P. (2018). Clinical Effectiveness in Psychotherapy and Mental Health: Strategies
and Resources for the Effective Clinical Governance. Routledge.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
PROJECT ON MENTAL HEALTH
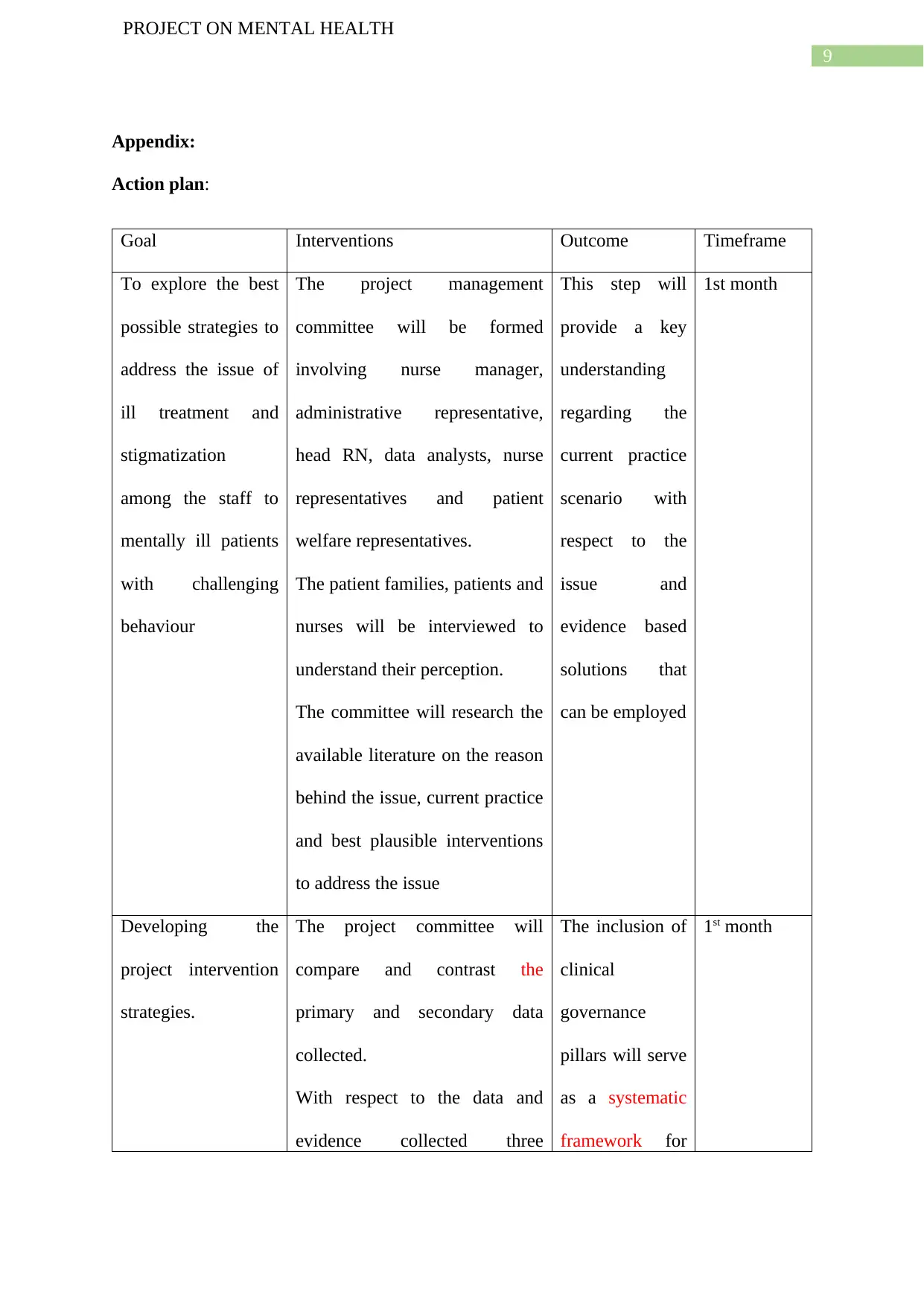
Appendix:
Action plan:
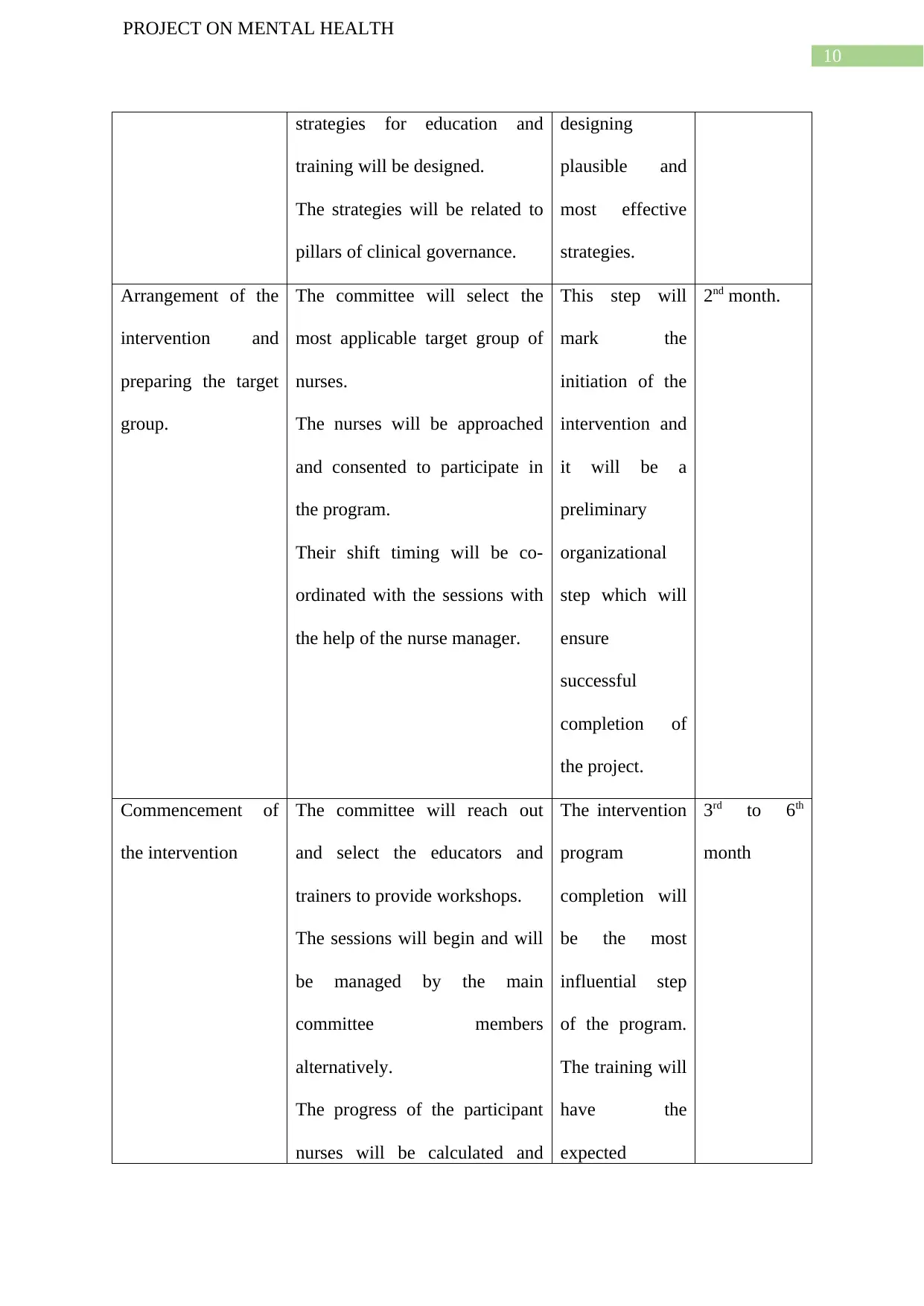
Goal Interventions Outcome Timeframe
To explore the best
possible strategies to
address the issue of
ill treatment and
stigmatization
among the staff to
mentally ill patients
with challenging
behaviour
The project management
committee will be formed
involving nurse manager,
administrative representative,
head RN, data analysts, nurse
representatives and patient
welfare representatives.
The patient families, patients and
nurses will be interviewed to
understand their perception.
The committee will research the
available literature on the reason
behind the issue, current practice
and best plausible interventions
to address the issue
This step will
provide a key
understanding
regarding the
current practice
scenario with
respect to the
issue and
evidence based
solutions that
can be employed
1st month
Developing the
project intervention
strategies.
The project committee will
compare and contrast the
primary and secondary data
collected.
With respect to the data and
evidence collected three
The inclusion of
clinical
governance
pillars will serve
as a systematic
framework for
1st month
PROJECT ON MENTAL HEALTH
Appendix:
Action plan:
Goal Interventions Outcome Timeframe
To explore the best
possible strategies to
address the issue of
ill treatment and
stigmatization
among the staff to
mentally ill patients
with challenging
behaviour
The project management
committee will be formed
involving nurse manager,
administrative representative,
head RN, data analysts, nurse
representatives and patient
welfare representatives.
The patient families, patients and
nurses will be interviewed to
understand their perception.
The committee will research the
available literature on the reason
behind the issue, current practice
and best plausible interventions
to address the issue
This step will
provide a key
understanding
regarding the
current practice
scenario with
respect to the
issue and
evidence based
solutions that
can be employed
1st month
Developing the
project intervention
strategies.
The project committee will
compare and contrast the
primary and secondary data
collected.
With respect to the data and
evidence collected three
The inclusion of
clinical
governance
pillars will serve
as a systematic
framework for
1st month
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
PROJECT ON MENTAL HEALTH
strategies for education and
training will be designed.
The strategies will be related to
pillars of clinical governance.
designing
plausible and
most effective
strategies.
Arrangement of the
intervention and
preparing the target
group.
The committee will select the
most applicable target group of
nurses.
The nurses will be approached
and consented to participate in
the program.
Their shift timing will be co-
ordinated with the sessions with
the help of the nurse manager.
This step will
mark the
initiation of the
intervention and
it will be a
preliminary
organizational
step which will
ensure
successful
completion of
the project.
2nd month.
Commencement of
the intervention
The committee will reach out
and select the educators and
trainers to provide workshops.
The sessions will begin and will
be managed by the main
committee members
alternatively.
The progress of the participant
nurses will be calculated and
The intervention
program
completion will
be the most
influential step
of the program.
The training will
have the
expected
3rd to 6th
month
PROJECT ON MENTAL HEALTH
strategies for education and
training will be designed.
The strategies will be related to
pillars of clinical governance.
designing
plausible and
most effective
strategies.
Arrangement of the
intervention and
preparing the target
group.
The committee will select the
most applicable target group of
nurses.
The nurses will be approached
and consented to participate in
the program.
Their shift timing will be co-
ordinated with the sessions with
the help of the nurse manager.
This step will
mark the
initiation of the
intervention and
it will be a
preliminary
organizational
step which will
ensure
successful
completion of
the project.
2nd month.
Commencement of
the intervention
The committee will reach out
and select the educators and
trainers to provide workshops.
The sessions will begin and will
be managed by the main
committee members
alternatively.
The progress of the participant
nurses will be calculated and
The intervention
program
completion will
be the most
influential step
of the program.
The training will
have the
expected
3rd to 6th
month
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





