NU3163: Psychoeducation Proposal for Bipolar Disorder Treatment
VerifiedAdded on 2023/06/10
|37
|10904
|259
Report
AI Summary
This report presents a proposal for implementing psychoeducation as a therapeutic intervention by nursing professionals for patients with bipolar disorder in a psychiatric ward. It begins by highlighting the rationale for the project, emphasizing the prevalence and challenges of bipolar disorder, including high rates of suicide, self-harm, and addiction. The proposal outlines the project's aims, which focus on utilizing psychoeducation to effectively manage bipolar disorder symptoms and associated comorbidities. A narrative literature review, employing databases like MEDLINE, CINAHL, and PubMed, supports the effectiveness of psychoeducation in improving medication adherence, reducing relapse rates, and enhancing the overall quality of life for patients. The report also addresses change management strategies necessary for successful implementation within nursing practice, concluding with recommendations for operationalizing the intervention.

Running head: BSC MENTAL HEALTH NURSING
NU3163 Toolkit for professional registration
Name of the Student
Name of the University
Author Note
NU3163 Toolkit for professional registration
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1BSC MENTAL HEALTH NURSING
Table of Contents
1.0 Full Dissertation title............................................................................................................2
2.0 Key words............................................................................................................................2
3.0 Rationale/need for the project..............................................................................................2
4.0 Project Methodology............................................................................................................4
4.0.1 Aims..............................................................................................................................4
4.0.2 Literature search strategy..............................................................................................4
4.0.3 Literature review...........................................................................................................5
5.0 Change management..........................................................................................................14
5.0.1 Project initiation..........................................................................................................16
6.0 Conclusion..........................................................................................................................21
References................................................................................................................................22
Appendix..................................................................................................................................34
Table of Contents
1.0 Full Dissertation title............................................................................................................2
2.0 Key words............................................................................................................................2
3.0 Rationale/need for the project..............................................................................................2
4.0 Project Methodology............................................................................................................4
4.0.1 Aims..............................................................................................................................4
4.0.2 Literature search strategy..............................................................................................4
4.0.3 Literature review...........................................................................................................5
5.0 Change management..........................................................................................................14
5.0.1 Project initiation..........................................................................................................16
6.0 Conclusion..........................................................................................................................21
References................................................................................................................................22
Appendix..................................................................................................................................34
2BSC MENTAL HEALTH NURSING
1.0 Full Dissertation title
A proposal to introduce psychoeducation approaches for implementation by nursing
professionals to treat patients suffering from bipolar disorder. The proposal will be
implemented in the psychiatric ward.
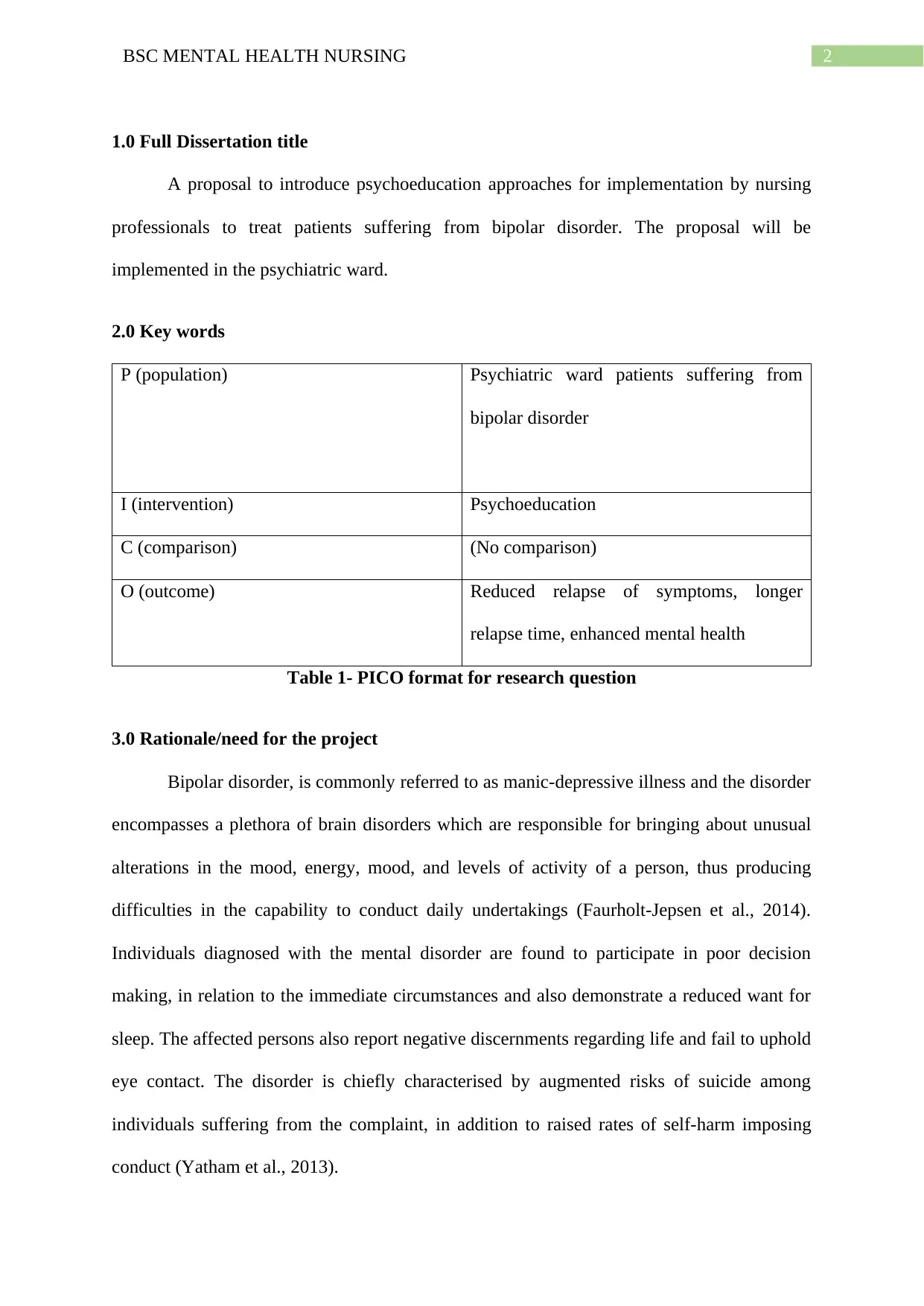
2.0 Key words
P (population) Psychiatric ward patients suffering from
bipolar disorder
I (intervention) Psychoeducation
C (comparison) (No comparison)
O (outcome) Reduced relapse of symptoms, longer
relapse time, enhanced mental health
Table 1- PICO format for research question
3.0 Rationale/need for the project
Bipolar disorder, is commonly referred to as manic-depressive illness and the disorder
encompasses a plethora of brain disorders which are responsible for bringing about unusual
alterations in the mood, energy, mood, and levels of activity of a person, thus producing
difficulties in the capability to conduct daily undertakings (Faurholt-Jepsen et al., 2014).
Individuals diagnosed with the mental disorder are found to participate in poor decision
making, in relation to the immediate circumstances and also demonstrate a reduced want for
sleep. The affected persons also report negative discernments regarding life and fail to uphold
eye contact. The disorder is chiefly characterised by augmented risks of suicide among
individuals suffering from the complaint, in addition to raised rates of self-harm imposing
conduct (Yatham et al., 2013).
1.0 Full Dissertation title
A proposal to introduce psychoeducation approaches for implementation by nursing
professionals to treat patients suffering from bipolar disorder. The proposal will be
implemented in the psychiatric ward.
2.0 Key words
P (population) Psychiatric ward patients suffering from
bipolar disorder
I (intervention) Psychoeducation
C (comparison) (No comparison)
O (outcome) Reduced relapse of symptoms, longer
relapse time, enhanced mental health
Table 1- PICO format for research question
3.0 Rationale/need for the project
Bipolar disorder, is commonly referred to as manic-depressive illness and the disorder
encompasses a plethora of brain disorders which are responsible for bringing about unusual
alterations in the mood, energy, mood, and levels of activity of a person, thus producing
difficulties in the capability to conduct daily undertakings (Faurholt-Jepsen et al., 2014).
Individuals diagnosed with the mental disorder are found to participate in poor decision
making, in relation to the immediate circumstances and also demonstrate a reduced want for
sleep. The affected persons also report negative discernments regarding life and fail to uphold
eye contact. The disorder is chiefly characterised by augmented risks of suicide among
individuals suffering from the complaint, in addition to raised rates of self-harm imposing
conduct (Yatham et al., 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3BSC MENTAL HEALTH NURSING
There were an estimated 4 million cases of mood disorders that also comprised of
bipolar disorder among people living in the UK in 2013. Furthermore, the youth were also
found at an increased likelihood of suffering from bipolar disorder, when compared to their
older counterparts in 2014. While 3-4% of young people aged 16-24 years showed a positive
screening for the mental illness, only 0.4% of older adults aged 65-74 years reported the same
(Mental health foundation, 2015).
While the lifetime prevalence of bipolar disorder in the UK population is 1-2%, it
takes approximately 10.5 years for an affected person to obtain the correct health diagnosis
for the condition (Bipolar UK, 2018). Addiction is a major problem among people suffering
from bipolar disorder. Most patients diagnosed with the mental illness report attempts of self-
medication for reducing the severity of depression and often resort to the use of drugs and
alcohol, with the aim of promoting sleep. Mixed mood episodes that are primarily
characterised by the incidence of both hypomanic or manic and depressive symptoms, in
association with a rapid change of the symptom types, are being progressively recognised as
more prevalent among people diagnosed with bipolar disorder (Phillips & Kupfer, 2013).
Furthermore, there are several medications that are used for treating people suffering
from bipolar disorder. These medications are prescribed with the intent of reducing the
depressive and maniac symptoms (Bourne et al., 2013). Although valproic acid, lithium, and
lamotrigine are commonly used under such circumstances, it often becomes difficult for
nursing professionals and psychiatrists to determine the correct combination of medications
that would prove effective (Malhi, Adams & Berk, 2010). Patients suffering from bipolar
disorder also report an increased susceptibility to a plethora of other social and physical
problems (Piterman, Jones, & Castle, 2010). While the psychological comorbidities most
commonly assume the form of anxiety symptoms that get superimposed on depression or
hypomania, there is a need to detect the exact difference between them. Physical
There were an estimated 4 million cases of mood disorders that also comprised of
bipolar disorder among people living in the UK in 2013. Furthermore, the youth were also
found at an increased likelihood of suffering from bipolar disorder, when compared to their
older counterparts in 2014. While 3-4% of young people aged 16-24 years showed a positive
screening for the mental illness, only 0.4% of older adults aged 65-74 years reported the same
(Mental health foundation, 2015).
While the lifetime prevalence of bipolar disorder in the UK population is 1-2%, it
takes approximately 10.5 years for an affected person to obtain the correct health diagnosis
for the condition (Bipolar UK, 2018). Addiction is a major problem among people suffering
from bipolar disorder. Most patients diagnosed with the mental illness report attempts of self-
medication for reducing the severity of depression and often resort to the use of drugs and
alcohol, with the aim of promoting sleep. Mixed mood episodes that are primarily
characterised by the incidence of both hypomanic or manic and depressive symptoms, in
association with a rapid change of the symptom types, are being progressively recognised as
more prevalent among people diagnosed with bipolar disorder (Phillips & Kupfer, 2013).
Furthermore, there are several medications that are used for treating people suffering
from bipolar disorder. These medications are prescribed with the intent of reducing the
depressive and maniac symptoms (Bourne et al., 2013). Although valproic acid, lithium, and
lamotrigine are commonly used under such circumstances, it often becomes difficult for
nursing professionals and psychiatrists to determine the correct combination of medications
that would prove effective (Malhi, Adams & Berk, 2010). Patients suffering from bipolar
disorder also report an increased susceptibility to a plethora of other social and physical
problems (Piterman, Jones, & Castle, 2010). While the psychological comorbidities most
commonly assume the form of anxiety symptoms that get superimposed on depression or
hypomania, there is a need to detect the exact difference between them. Physical
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4BSC MENTAL HEALTH NURSING
comorbidities also express in the form of cardiovascular complications, poor diet, obesity,
and hyperlipidaemia (Amann, Radua, Wunsch, König & Simhandl, 2017). Thus, it is
essential for the healthcare professionals to adapt to the use of other non-pharmacological
approaches as well for management of bipolar disorder symptoms among patients admitted to
a psychiatric ward. Thus, the proposal aims at implementing psychoeducation, an evidence-
based therapeutic intervention by nursing professionals for educating the people seeking
treatment for bipolar disorder, and effectively managing their illness and other comorbidities.
4.0 Project Methodology
4.0.1 Aims
The project will aim to implement a change strategy that focuses on psychoeducation
as an effective therapeutic tool that can be used by nursing professionals in a psychiatric ward
for the management of bipolar disorder symptoms among admitted patients. The change
management strategies will also be followed by recommendations that can help in operation
of the intervention in nursing practice.
4.0.2 Literature search strategy
The strategy used in this dissertation focuses on a narrative literature review that is
based upon previous findings, pertinent to the research question. Some keywords and search
phrases that were used along with specific boolean operators were ‘AND’ and ‘OR’. These
helped in either broadening or narrowing down the search results and facilitated extraction of
relevant scholarly pieces of literature (McGowan et al., 2016). Three electronic databases
namely, MEDLINE, CINAHL, and PubMed were used for the data extraction. Input of the
search terms were accompanied by addition of filters and limiters that narrowed down the
emphasis of the search, thus ensuring that the exploration was restricted in accordance to the
research question (Aromataris & Riitano, 2014) (refer to appendix). The Appraisal Skills
comorbidities also express in the form of cardiovascular complications, poor diet, obesity,
and hyperlipidaemia (Amann, Radua, Wunsch, König & Simhandl, 2017). Thus, it is
essential for the healthcare professionals to adapt to the use of other non-pharmacological
approaches as well for management of bipolar disorder symptoms among patients admitted to
a psychiatric ward. Thus, the proposal aims at implementing psychoeducation, an evidence-
based therapeutic intervention by nursing professionals for educating the people seeking
treatment for bipolar disorder, and effectively managing their illness and other comorbidities.
4.0 Project Methodology
4.0.1 Aims
The project will aim to implement a change strategy that focuses on psychoeducation
as an effective therapeutic tool that can be used by nursing professionals in a psychiatric ward
for the management of bipolar disorder symptoms among admitted patients. The change
management strategies will also be followed by recommendations that can help in operation
of the intervention in nursing practice.
4.0.2 Literature search strategy
The strategy used in this dissertation focuses on a narrative literature review that is
based upon previous findings, pertinent to the research question. Some keywords and search
phrases that were used along with specific boolean operators were ‘AND’ and ‘OR’. These
helped in either broadening or narrowing down the search results and facilitated extraction of
relevant scholarly pieces of literature (McGowan et al., 2016). Three electronic databases
namely, MEDLINE, CINAHL, and PubMed were used for the data extraction. Input of the
search terms were accompanied by addition of filters and limiters that narrowed down the
emphasis of the search, thus ensuring that the exploration was restricted in accordance to the
research question (Aromataris & Riitano, 2014) (refer to appendix). The Appraisal Skills
5BSC MENTAL HEALTH NURSING
Programme checklist (CASP) was also used to review the articles, with the aim of obtaining
appropriate and evidence-based literature on psychoeducation in mental health practice.
4.0.3 Literature review
Psychoeducation is defined as the procedure that encompasses the delivery of
education and pertinent information to people who seek or receive appropriate mental health
services (Chan, Yip, Tso, Cheng & Tam, 2009). This is usually required by individuals
diagnosed with different mental health condition and their family members. Zhao, Sampson,
Xia and Jayaram (2015) define psychoeducation as the education of a person who has been
diagnosed with a psychiatric disorder regarding the presenting complaints, symptoms,
prognosis and treatment of the illness. They also elaborated on the fact that brief
psychoeducation for any mental illness reports significant reduction in the relapse of the
illness in medium term, and also promotes medication compliance among the affected people
in short term. The statements are consistent with other articles that illustrated the importance
of psychoeducation in improving the compliance to schizophrenia symptoms and health
outcomes, without bringing about any noteworthy onset of adverse health effects (Bäuml et
al., 2016).
In other words, psychoeducation have been found beneficial in improving the
adherence to prescribed treatment regimen and also motivates the mentally ill patients to
accept the recommended maintenance therapy, as per the healthcare guidelines. The
information that is offered to patients seeking psychoeducation support often range from
educating the patients on the potential benefits of the prescribed medication to enhancing
their adherence, to complex, intensive interventions that cover all information related to drugs
and the illness. There often exists a considerable overlap between specific psychotherapies
Programme checklist (CASP) was also used to review the articles, with the aim of obtaining
appropriate and evidence-based literature on psychoeducation in mental health practice.
4.0.3 Literature review
Psychoeducation is defined as the procedure that encompasses the delivery of
education and pertinent information to people who seek or receive appropriate mental health
services (Chan, Yip, Tso, Cheng & Tam, 2009). This is usually required by individuals
diagnosed with different mental health condition and their family members. Zhao, Sampson,
Xia and Jayaram (2015) define psychoeducation as the education of a person who has been
diagnosed with a psychiatric disorder regarding the presenting complaints, symptoms,
prognosis and treatment of the illness. They also elaborated on the fact that brief
psychoeducation for any mental illness reports significant reduction in the relapse of the
illness in medium term, and also promotes medication compliance among the affected people
in short term. The statements are consistent with other articles that illustrated the importance
of psychoeducation in improving the compliance to schizophrenia symptoms and health
outcomes, without bringing about any noteworthy onset of adverse health effects (Bäuml et
al., 2016).
In other words, psychoeducation have been found beneficial in improving the
adherence to prescribed treatment regimen and also motivates the mentally ill patients to
accept the recommended maintenance therapy, as per the healthcare guidelines. The
information that is offered to patients seeking psychoeducation support often range from
educating the patients on the potential benefits of the prescribed medication to enhancing
their adherence, to complex, intensive interventions that cover all information related to drugs
and the illness. There often exists a considerable overlap between specific psychotherapies
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6BSC MENTAL HEALTH NURSING
such as, interpersonal and social rhythm therapy (IPSRT), cognitive behavioural therapy
(CBT), and family-focused therapy (FFT) and psychoeducation (Lefley, 2009). D’Souza et
al. (2010) conducted a randomised controlled trial to determine the impacts of
psychoeducation program on the relapse rates of bipolar disorder among patients. Findings of
the RCT suggested that the intervention group participants showed reduced likelihood of
relapse symptoms and also had a longer relapse time (11 weeks), in comparison to the
treatment-as-usual group. Although the sample size was small, further improvements were
also associated with a reduction in the maniac symptoms and improved adherence to
medications, thus suggesting the utility of psychoeducation in bipolar disorder management.
However, Bond and Anderson (2015) argued that individual psychoeducation
programs were not much beneficial in preventing bipolar disorder relapse. Upon conducting a
systematic review of randomised controlled trials, the findings suggested that
psychoeducation was effective in averting any reversion of symptoms (n = 7; OR: 1.98–2.75;
number needed to treat (NNT): 5–7) and hypomanic or manic recurrence (n = 8; OR: 1.68–
2.52; NNT: 6–8). Showing consistency with previous findings, psychoeducation was found to
improve the short‐term medication knowledge and medication adherence. However, failure of
the psychoeducation interventions in preventing bipolar associated depressive symptom
relapse explained the presence of heterogeneity in the individual interventions.
Nonetheless, the interventions that focus on psychoeducation were found operational
in bringing about statistically momentous enhancement in the compliance to medications
among bipolar disorder patients in another RCT (P = 0.008). Upon subjecting patients to 50
minutes of psychoeducation sessions, lower cases of hospital admissions and disorder relapse
were also found in the intervention group, compared to the control group (P = 0.000)
(Javadpour, Hedayati, Dehbozorgi & Azizi, 2013). These were in contrast to the findings
presented by de Azevedo Cardoso et al. (2014) who conducted an RCT for assessing the
such as, interpersonal and social rhythm therapy (IPSRT), cognitive behavioural therapy
(CBT), and family-focused therapy (FFT) and psychoeducation (Lefley, 2009). D’Souza et
al. (2010) conducted a randomised controlled trial to determine the impacts of
psychoeducation program on the relapse rates of bipolar disorder among patients. Findings of
the RCT suggested that the intervention group participants showed reduced likelihood of
relapse symptoms and also had a longer relapse time (11 weeks), in comparison to the
treatment-as-usual group. Although the sample size was small, further improvements were
also associated with a reduction in the maniac symptoms and improved adherence to
medications, thus suggesting the utility of psychoeducation in bipolar disorder management.
However, Bond and Anderson (2015) argued that individual psychoeducation
programs were not much beneficial in preventing bipolar disorder relapse. Upon conducting a
systematic review of randomised controlled trials, the findings suggested that
psychoeducation was effective in averting any reversion of symptoms (n = 7; OR: 1.98–2.75;
number needed to treat (NNT): 5–7) and hypomanic or manic recurrence (n = 8; OR: 1.68–
2.52; NNT: 6–8). Showing consistency with previous findings, psychoeducation was found to
improve the short‐term medication knowledge and medication adherence. However, failure of
the psychoeducation interventions in preventing bipolar associated depressive symptom
relapse explained the presence of heterogeneity in the individual interventions.
Nonetheless, the interventions that focus on psychoeducation were found operational
in bringing about statistically momentous enhancement in the compliance to medications
among bipolar disorder patients in another RCT (P = 0.008). Upon subjecting patients to 50
minutes of psychoeducation sessions, lower cases of hospital admissions and disorder relapse
were also found in the intervention group, compared to the control group (P = 0.000)
(Javadpour, Hedayati, Dehbozorgi & Azizi, 2013). These were in contrast to the findings
presented by de Azevedo Cardoso et al. (2014) who conducted an RCT for assessing the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7BSC MENTAL HEALTH NURSING
effects of brief psychoeducation on bipolar disorder. While there was no statistically
significant difference in the quality of life of patients subjected to psychoeducation and
medication, and the usual care group, the improvement persisted during 6-month follow-up
period, thus establishing the fact that psychoeducation in addition to pharmacological
intervention might prove effective in enhancing quality of life of bipolar disorder patients.
In the words of Gumus, Buzlu and Cakir (2015) individual psychoeducation program
do not prove helpful in reducing recurrence rates of bipolar disorder and its comorbid
psychological symptoms. Although recurrence rate among patients in the experimental study
was 18.9% in intervention group, in comparison to 34.1% in the control group, failure to
achieve a statistical significance between the both made the researchers conclude that
although individual psychoeducation sessions produce positive impacts, they are ineffective
in the prevention of relapse. Besides, it was reinforced by other researchers that
psychoeducation programs in addition to pharmacotherapy are a potential treatment option
that can improve global functioning and medication adherence of bipolar disorder patients.
Increase in medication adherence score of the psycho-educational group from 6.27(0.88) to
7.92(1.38) provided evidence for the worth of psychoeducation as an intervention in mental
health settings (Bahredar, Farid, Ghanizadeh & Birashk, 2014).
Rahmani, Ebrahimi, Ranjbar, Razavi and Asghari (2016) also recommended the
implementation of interventions that focused on psychoeducation in clinical settings by
psychiatric nurses. Significant increase in the mean scores related to medication adherence in
the experimental group than the control group established the fact that educating the patients
on the benefits of the prescribed medications are a good strategy for increasing their
compliance, thus managing the bipolar disorder symptoms. Psychoeducation was confirmed
as the key component of collaborative models related to treatment of mental disorder that
campaigns the rights of all patients being informed about the proposed plan of treatment plan.
effects of brief psychoeducation on bipolar disorder. While there was no statistically
significant difference in the quality of life of patients subjected to psychoeducation and
medication, and the usual care group, the improvement persisted during 6-month follow-up
period, thus establishing the fact that psychoeducation in addition to pharmacological
intervention might prove effective in enhancing quality of life of bipolar disorder patients.
In the words of Gumus, Buzlu and Cakir (2015) individual psychoeducation program
do not prove helpful in reducing recurrence rates of bipolar disorder and its comorbid
psychological symptoms. Although recurrence rate among patients in the experimental study
was 18.9% in intervention group, in comparison to 34.1% in the control group, failure to
achieve a statistical significance between the both made the researchers conclude that
although individual psychoeducation sessions produce positive impacts, they are ineffective
in the prevention of relapse. Besides, it was reinforced by other researchers that
psychoeducation programs in addition to pharmacotherapy are a potential treatment option
that can improve global functioning and medication adherence of bipolar disorder patients.
Increase in medication adherence score of the psycho-educational group from 6.27(0.88) to
7.92(1.38) provided evidence for the worth of psychoeducation as an intervention in mental
health settings (Bahredar, Farid, Ghanizadeh & Birashk, 2014).
Rahmani, Ebrahimi, Ranjbar, Razavi and Asghari (2016) also recommended the
implementation of interventions that focused on psychoeducation in clinical settings by
psychiatric nurses. Significant increase in the mean scores related to medication adherence in
the experimental group than the control group established the fact that educating the patients
on the benefits of the prescribed medications are a good strategy for increasing their
compliance, thus managing the bipolar disorder symptoms. Psychoeducation was confirmed
as the key component of collaborative models related to treatment of mental disorder that
campaigns the rights of all patients being informed about the proposed plan of treatment plan.
8BSC MENTAL HEALTH NURSING
Increase in treatment adherence rate of patients in intervention group from 40.0% (14
patients/pre-test) to 86.7% (26 patients/post-test) established the benefits of six-week
psychoeducation programs on adherence improvement (Eker & Harkın, 2012).
In the words of Husain et al. (2017) a pilot study confirmed the feasibility and
acceptability of psychoeducation intervention in the treatment of bipolar disorder patients by
enhancing their mood and knowledge attitudes. Improved patient satisfaction (ES = 1.41),
greater medication adherence (MMAS-4: ES = 0.81), enhanced measures related to quality of
life (EQ-5D: ES ⇒ 0.88) and improved knowledge towards mania (YMRS: ES = 1.18),
bipolar (BKAQ: ES = 0.68), and depression (BDI: ES = 1.17) helped in establishing the value
of culturally adapted bipolar psychoeducation programmes (CaPE). These were consistent
with findings presented by Chen et al. (2018) who conducted a qualitative study with the
intent of understanding the impact of group psychoeducation on perception of inpatients after
remission of manic episode in bipolar I disorder. Some of the common themes that emerged
from the results were namely, (1) increased patient engagement, (2) recommendation of the
intervention to others, (3) learning environment, (4) facilitators, (5) time, (6) class-taught
versus discussion, and (7) suggestions, among others. It was found that psychoeducation
made the patients more confident, enhanced self-acceptance of the mental disorder, helped
the patients understand the side effects, and also prevented relapse. Similar findings were
reported in another RCT where the patients were subjected to eight group‐based
psychoeducation sessions in the intervention group. Psychoeducation proved beneficial in
management of bipolar disorder by reducing the mania recurrence, showing lower
hospitalisation rates, and bringing about changes in depression scores, global functioning and
mania (Chen et al., 2018).
Soo et al. (2018) conducted a systematic review with the aim of summarising the
effectiveness of psychoeducation and its four modalities (individual, internet- based, group,
Increase in treatment adherence rate of patients in intervention group from 40.0% (14
patients/pre-test) to 86.7% (26 patients/post-test) established the benefits of six-week
psychoeducation programs on adherence improvement (Eker & Harkın, 2012).
In the words of Husain et al. (2017) a pilot study confirmed the feasibility and
acceptability of psychoeducation intervention in the treatment of bipolar disorder patients by
enhancing their mood and knowledge attitudes. Improved patient satisfaction (ES = 1.41),
greater medication adherence (MMAS-4: ES = 0.81), enhanced measures related to quality of
life (EQ-5D: ES ⇒ 0.88) and improved knowledge towards mania (YMRS: ES = 1.18),
bipolar (BKAQ: ES = 0.68), and depression (BDI: ES = 1.17) helped in establishing the value
of culturally adapted bipolar psychoeducation programmes (CaPE). These were consistent
with findings presented by Chen et al. (2018) who conducted a qualitative study with the
intent of understanding the impact of group psychoeducation on perception of inpatients after
remission of manic episode in bipolar I disorder. Some of the common themes that emerged
from the results were namely, (1) increased patient engagement, (2) recommendation of the
intervention to others, (3) learning environment, (4) facilitators, (5) time, (6) class-taught
versus discussion, and (7) suggestions, among others. It was found that psychoeducation
made the patients more confident, enhanced self-acceptance of the mental disorder, helped
the patients understand the side effects, and also prevented relapse. Similar findings were
reported in another RCT where the patients were subjected to eight group‐based
psychoeducation sessions in the intervention group. Psychoeducation proved beneficial in
management of bipolar disorder by reducing the mania recurrence, showing lower
hospitalisation rates, and bringing about changes in depression scores, global functioning and
mania (Chen et al., 2018).
Soo et al. (2018) conducted a systematic review with the aim of summarising the
effectiveness of psychoeducation and its four modalities (individual, internet- based, group,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9BSC MENTAL HEALTH NURSING
family) upon bipolar disorder patients and found that the intervention played a major role in
reducing illness recurrences, decreasing the duration and number of hospitalizations,
increasing time to relapse of illness, enhancing treatment adherence, and reducing stigma
related to mental illnesses. However, Gumus (2017) argued that individual psycho-education
proved ineffective in bringing about an improvement in global functioning and quality of life
of bipolar disorder patients. Nonetheless, the intervention was successful in improving
participation of patients in social activities (T = 2.011; P = 0.048) and taking the initiative for
self-management of condition (T =2.093; P = 0.040). The effectiveness of psychoeducation
programs were also not consistent with the findings presented in another trial where the
intervention was related to constraints in rate of participation among patients and a sense of
motivation among them (Cakir, Bensusan, Akca & Yazici, 2009).
Batista, Baes and Juruena (2011) opined that psychoeducation based interventions had
the potential of significantly improving the treatment adherence, clinical course, and
psychosocial functioning of all bipolar patients. It also decreased the number of recurrences
and relapses per patient and augmented the time to manic, depressive, mixed, and hypomanic
recurrences. The length and instances of hospitalizations were also lower among patients
subjected to the intervention. This was consistent with results of another RCT where
psychoeducation reduced percentages of mood relapse (χ2=6.53; p=0.011) and increased the
relapse free time periods experienced by bipolar disorder patients (log‐rank χ2=4.04;
p=0.044). This helped the authors conclude that group based psychoeducation intervention
for caregivers of bipolar patients can be considered as an useful adjunct to typical treatment
for patients in dropping the risk of relapses, particularly hypomania and mania, in bipolar
disorder (Reinares et al., 2009).
However, Zaretsky, Lancee, Miller, Harris and Parikh (2008) contended that
following optimisation of pharmacological treatment, longer duration of adjunctive CBT was
family) upon bipolar disorder patients and found that the intervention played a major role in
reducing illness recurrences, decreasing the duration and number of hospitalizations,
increasing time to relapse of illness, enhancing treatment adherence, and reducing stigma
related to mental illnesses. However, Gumus (2017) argued that individual psycho-education
proved ineffective in bringing about an improvement in global functioning and quality of life
of bipolar disorder patients. Nonetheless, the intervention was successful in improving
participation of patients in social activities (T = 2.011; P = 0.048) and taking the initiative for
self-management of condition (T =2.093; P = 0.040). The effectiveness of psychoeducation
programs were also not consistent with the findings presented in another trial where the
intervention was related to constraints in rate of participation among patients and a sense of
motivation among them (Cakir, Bensusan, Akca & Yazici, 2009).
Batista, Baes and Juruena (2011) opined that psychoeducation based interventions had
the potential of significantly improving the treatment adherence, clinical course, and
psychosocial functioning of all bipolar patients. It also decreased the number of recurrences
and relapses per patient and augmented the time to manic, depressive, mixed, and hypomanic
recurrences. The length and instances of hospitalizations were also lower among patients
subjected to the intervention. This was consistent with results of another RCT where
psychoeducation reduced percentages of mood relapse (χ2=6.53; p=0.011) and increased the
relapse free time periods experienced by bipolar disorder patients (log‐rank χ2=4.04;
p=0.044). This helped the authors conclude that group based psychoeducation intervention
for caregivers of bipolar patients can be considered as an useful adjunct to typical treatment
for patients in dropping the risk of relapses, particularly hypomania and mania, in bipolar
disorder (Reinares et al., 2009).
However, Zaretsky, Lancee, Miller, Harris and Parikh (2008) contended that
following optimisation of pharmacological treatment, longer duration of adjunctive CBT was
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10BSC MENTAL HEALTH NURSING
found to deliver supplementary benefits over short-term psychoeducation programs for
management and treatment of bipolar disorder. Findings from another cluster feasibility
randomised trial that comprised of community mental health programs (hourly sessions of
psychoeducation) suggested that the intervention was an effective approach in preventing
relapse of bipolar disorder symptoms and also improved the occupational and social
functioning among the patients (regression coefficient 0.68, 95% CI 0.05–1.32) (Lobban et
al., 2010). Morriss et al. (2016) suggested that although structured group psychoeducation
was not able to prove its clinically effectiveness, when compared to parallel intensive un-
structured peer support programs, the former was better acceptable and helped in enhancing
the outcomes among participants by reducing their bipolar episodes. The findings reported
higher attendance in the psychoeducation groups, in comparison to peer support (median 14
sessions vs nine sessions; p=0·026). Furthermore, only 58% participants subjected to
psychoeducation experienced relapse of next episode of bipolar disorder, compared to 65% in
the other group.
According to Kallestad, Wullum, Scott, Stiles and Morken (2016) bipolar disorder
patients who were subjected to group psychoeducation (GP) demonstrated lengthier survival
times when compared to individual psychoeducation (IP), over a period of 27 months
(p<0.05). GP cases associated with harmful substance abuse comorbidity reported shortest
survival time, while those without the comorbidity survived more (p=0.02). Significant
lessening in hospital admissions upon implementation of the group based intervention also
proved the efficacy of psychoeducation in bipolar disorder management (p=0.04).
BalancingMySwing, a nursing based psychoeducation program was also found to improve the
adherence to medications among Taiwanese Han-Chinese bipolar II disorder patients. Owing
to the fact that medication adherence is considered crucial for long-term management of
mental illness management, and non-adherence can pose major challenges while treating
found to deliver supplementary benefits over short-term psychoeducation programs for
management and treatment of bipolar disorder. Findings from another cluster feasibility
randomised trial that comprised of community mental health programs (hourly sessions of
psychoeducation) suggested that the intervention was an effective approach in preventing
relapse of bipolar disorder symptoms and also improved the occupational and social
functioning among the patients (regression coefficient 0.68, 95% CI 0.05–1.32) (Lobban et
al., 2010). Morriss et al. (2016) suggested that although structured group psychoeducation
was not able to prove its clinically effectiveness, when compared to parallel intensive un-
structured peer support programs, the former was better acceptable and helped in enhancing
the outcomes among participants by reducing their bipolar episodes. The findings reported
higher attendance in the psychoeducation groups, in comparison to peer support (median 14
sessions vs nine sessions; p=0·026). Furthermore, only 58% participants subjected to
psychoeducation experienced relapse of next episode of bipolar disorder, compared to 65% in
the other group.
According to Kallestad, Wullum, Scott, Stiles and Morken (2016) bipolar disorder
patients who were subjected to group psychoeducation (GP) demonstrated lengthier survival
times when compared to individual psychoeducation (IP), over a period of 27 months
(p<0.05). GP cases associated with harmful substance abuse comorbidity reported shortest
survival time, while those without the comorbidity survived more (p=0.02). Significant
lessening in hospital admissions upon implementation of the group based intervention also
proved the efficacy of psychoeducation in bipolar disorder management (p=0.04).
BalancingMySwing, a nursing based psychoeducation program was also found to improve the
adherence to medications among Taiwanese Han-Chinese bipolar II disorder patients. Owing
to the fact that medication adherence is considered crucial for long-term management of
mental illness management, and non-adherence can pose major challenges while treating
11BSC MENTAL HEALTH NURSING
bipolar disorder patients, the results helped the authors to establish the efficacy and worth of
the nurse-led psychoeducation program (Lin, Berk & Hsu, 2017).
In the words of George, Sharma and Nair (2013) significant improvements were
observed in a randomised controlled trial among the patients suffering from bipolar disorder
who were placed in the intervention group that comprised of four sessions of
psychoeducation. Substantial enhancement of attitude and knowledge scores among the
investigational group, compared to the control group (p =0.001) established the worth of the
psychoeducation program. Although not noteworthy, differences were also observed in the
adherence to intervention between the two groups (p = 0.111). Thus, the results confirmed the
fact that psychoeducation based intervention concomitant with pharmacotherapy acted as an
easy, cost-effective and feasible intervention for enhancing treatment adherence among
bipolar disorder patients.
Pakpour et al. (2017) also conducted a study where patients with bipolar
disorder were randomised to an intervention group that encompassed five sessions of
psychoeducation and motivational interviewing, together with their family members. Patients
in the intervention group demonstrated enhancement in adherence to medications (baseline
score: 6.03; score at the sixth month: 9.55) when compared to those in the usual care group.
Furthermore, those subjected to psychoeducation and motivational interviewing sessions
were able to manifest improvement in all scores related to their secondary outcomes as well.
This confirmed the effectiveness of psychoeducation approaches on functional and clinical
outcomes of bipolar disorder patients. Parallel to the aforementioned findings,
psychoeducation was found to exert long-term prophylactic impacts on bipolar disorder
affected individuals in another RCT. Patients who had been administered the
psychoeducation program manifested longer time to recurrence for bipolar disorder (log
rank=9.953, P<0.002). The intervention group also reported lesser instances of disease
bipolar disorder patients, the results helped the authors to establish the efficacy and worth of
the nurse-led psychoeducation program (Lin, Berk & Hsu, 2017).
In the words of George, Sharma and Nair (2013) significant improvements were
observed in a randomised controlled trial among the patients suffering from bipolar disorder
who were placed in the intervention group that comprised of four sessions of
psychoeducation. Substantial enhancement of attitude and knowledge scores among the
investigational group, compared to the control group (p =0.001) established the worth of the
psychoeducation program. Although not noteworthy, differences were also observed in the
adherence to intervention between the two groups (p = 0.111). Thus, the results confirmed the
fact that psychoeducation based intervention concomitant with pharmacotherapy acted as an
easy, cost-effective and feasible intervention for enhancing treatment adherence among
bipolar disorder patients.
Pakpour et al. (2017) also conducted a study where patients with bipolar
disorder were randomised to an intervention group that encompassed five sessions of
psychoeducation and motivational interviewing, together with their family members. Patients
in the intervention group demonstrated enhancement in adherence to medications (baseline
score: 6.03; score at the sixth month: 9.55) when compared to those in the usual care group.
Furthermore, those subjected to psychoeducation and motivational interviewing sessions
were able to manifest improvement in all scores related to their secondary outcomes as well.
This confirmed the effectiveness of psychoeducation approaches on functional and clinical
outcomes of bipolar disorder patients. Parallel to the aforementioned findings,
psychoeducation was found to exert long-term prophylactic impacts on bipolar disorder
affected individuals in another RCT. Patients who had been administered the
psychoeducation program manifested longer time to recurrence for bipolar disorder (log
rank=9.953, P<0.002). The intervention group also reported lesser instances of disease
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 37
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





