Report on Mental Health Conditions, Treatment, and Nursing Care
VerifiedAdded on 2023/06/10
|10
|1508
|278
Report
AI Summary
This report provides a detailed overview of various mental health conditions, encompassing their respective treatments and nursing management strategies. The report delves into specific conditions such as psychosis, bipolar disorder, panic disorder, social phobia, PTSD, borderline personality disorder, schizophrenia, and dementia, outlining appropriate therapeutic interventions, including medication, psychotherapy, and rehabilitation. It emphasizes the crucial role of nurses in assessing patients, providing supportive care, and implementing evidence-based practices. The report also highlights the five principles of recovery in mental health, emphasizing individual uniqueness, real choices, attitudes and rights, dignity and respect, and partnership and communication. Furthermore, it addresses challenging behaviors, the impact of stigma, and person-centered care plans, offering insights into comprehensive mental health care. The report includes references to key research studies and guidelines, providing a valuable resource for healthcare professionals and students alike.
5.
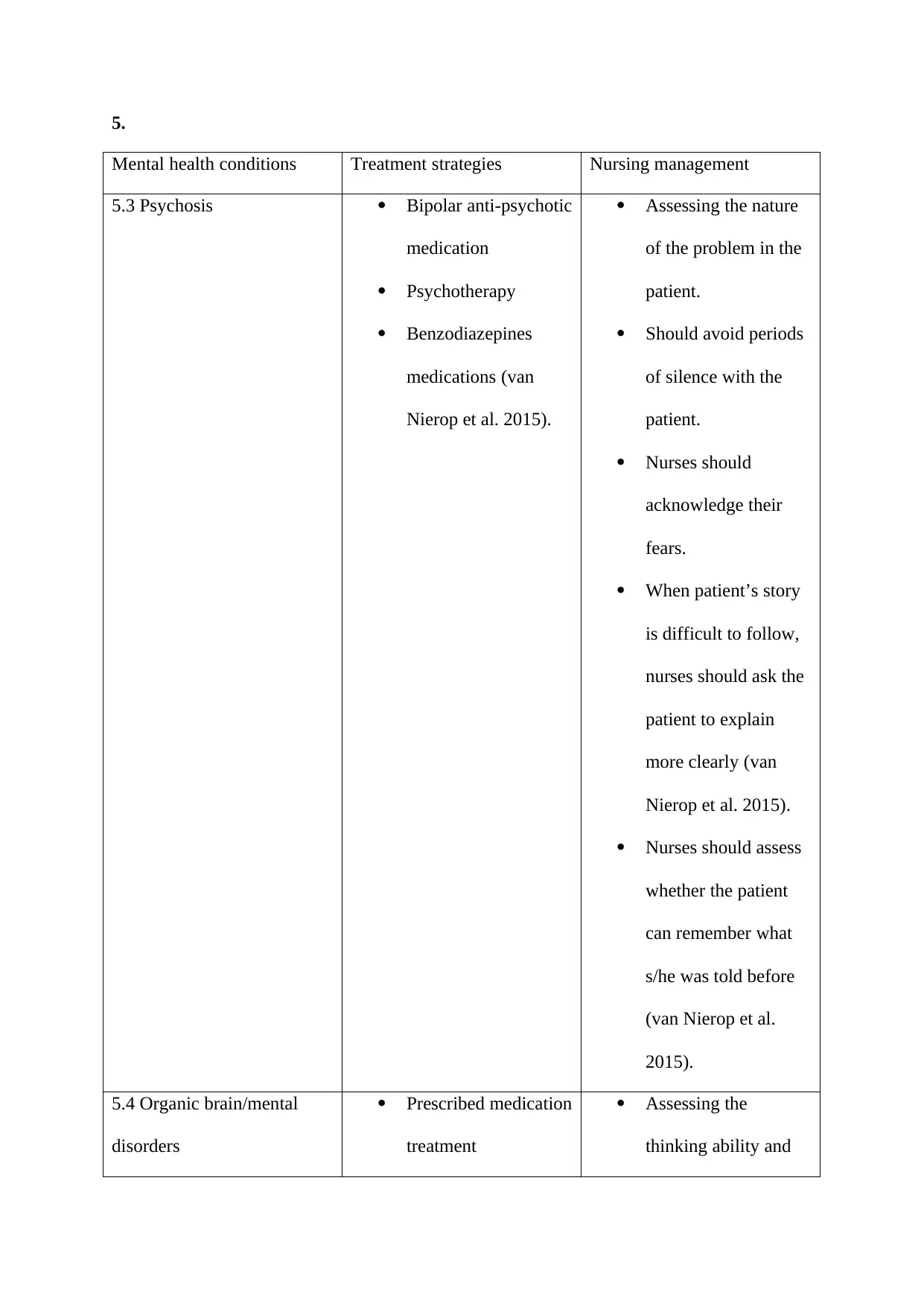
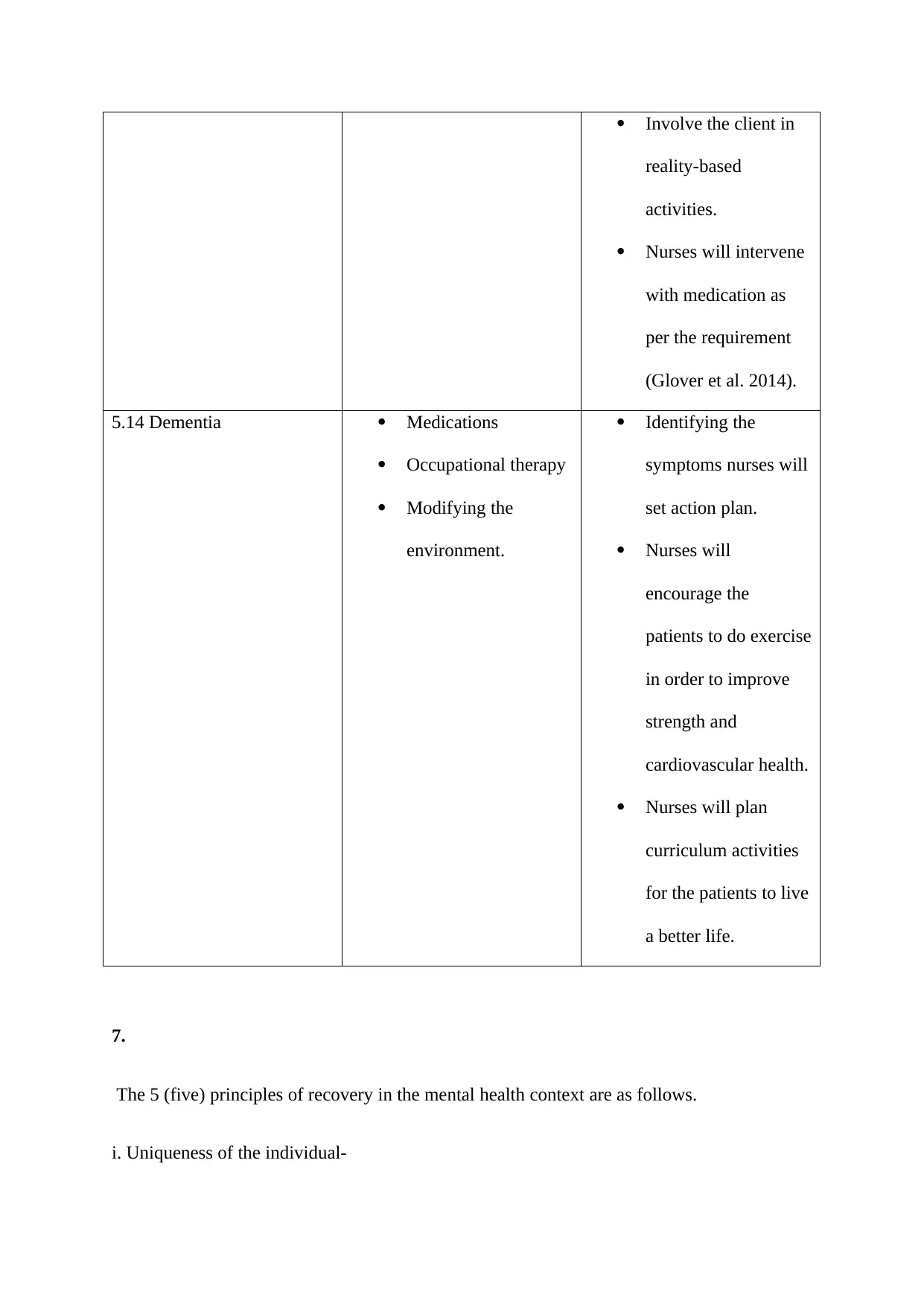
Mental health conditions Treatment strategies Nursing management
5.3 Psychosis Bipolar anti-psychotic
medication
Psychotherapy
Benzodiazepines
medications (van
Nierop et al. 2015).
Assessing the nature
of the problem in the
patient.
Should avoid periods
of silence with the
patient.
Nurses should
acknowledge their
fears.
When patient’s story
is difficult to follow,
nurses should ask the
patient to explain
more clearly (van
Nierop et al. 2015).
Nurses should assess
whether the patient
can remember what
s/he was told before
(van Nierop et al.
2015).
5.4 Organic brain/mental
disorders
Prescribed medication
treatment
Assessing the
thinking ability and
Mental health conditions Treatment strategies Nursing management
5.3 Psychosis Bipolar anti-psychotic
medication
Psychotherapy
Benzodiazepines
medications (van
Nierop et al. 2015).
Assessing the nature
of the problem in the
patient.
Should avoid periods
of silence with the
patient.
Nurses should
acknowledge their
fears.
When patient’s story
is difficult to follow,
nurses should ask the
patient to explain
more clearly (van
Nierop et al. 2015).
Nurses should assess
whether the patient
can remember what
s/he was told before
(van Nierop et al.
2015).
5.4 Organic brain/mental
disorders
Prescribed medication
treatment
Assessing the
thinking ability and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
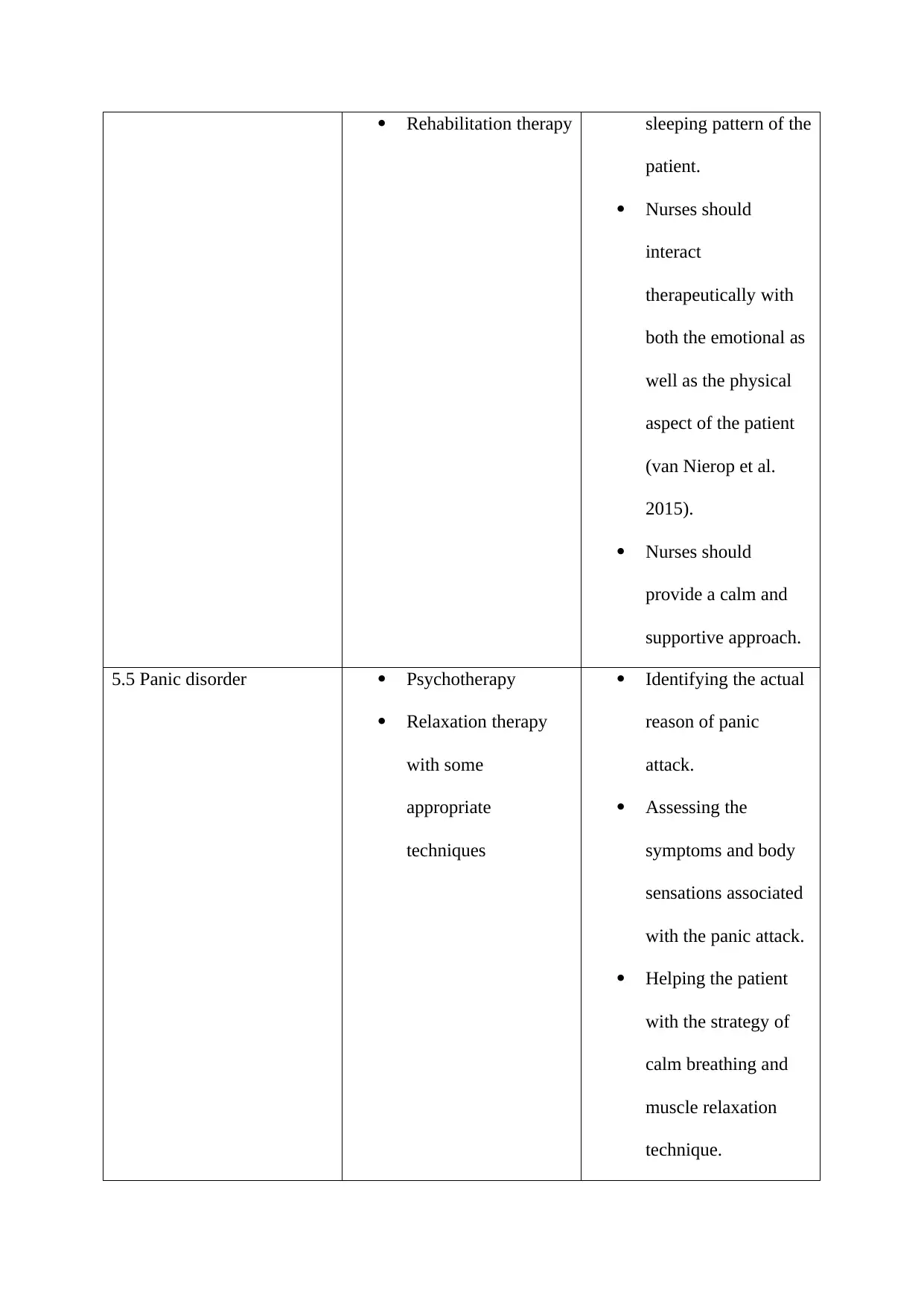
Rehabilitation therapy sleeping pattern of the
patient.
Nurses should
interact
therapeutically with
both the emotional as
well as the physical
aspect of the patient
(van Nierop et al.
2015).
Nurses should
provide a calm and
supportive approach.
5.5 Panic disorder Psychotherapy
Relaxation therapy
with some
appropriate
techniques
Identifying the actual
reason of panic
attack.
Assessing the
symptoms and body
sensations associated
with the panic attack.
Helping the patient
with the strategy of
calm breathing and
muscle relaxation
technique.
patient.
Nurses should
interact
therapeutically with
both the emotional as
well as the physical
aspect of the patient
(van Nierop et al.
2015).
Nurses should
provide a calm and
supportive approach.
5.5 Panic disorder Psychotherapy
Relaxation therapy
with some
appropriate
techniques
Identifying the actual
reason of panic
attack.
Assessing the
symptoms and body
sensations associated
with the panic attack.
Helping the patient
with the strategy of
calm breathing and
muscle relaxation
technique.
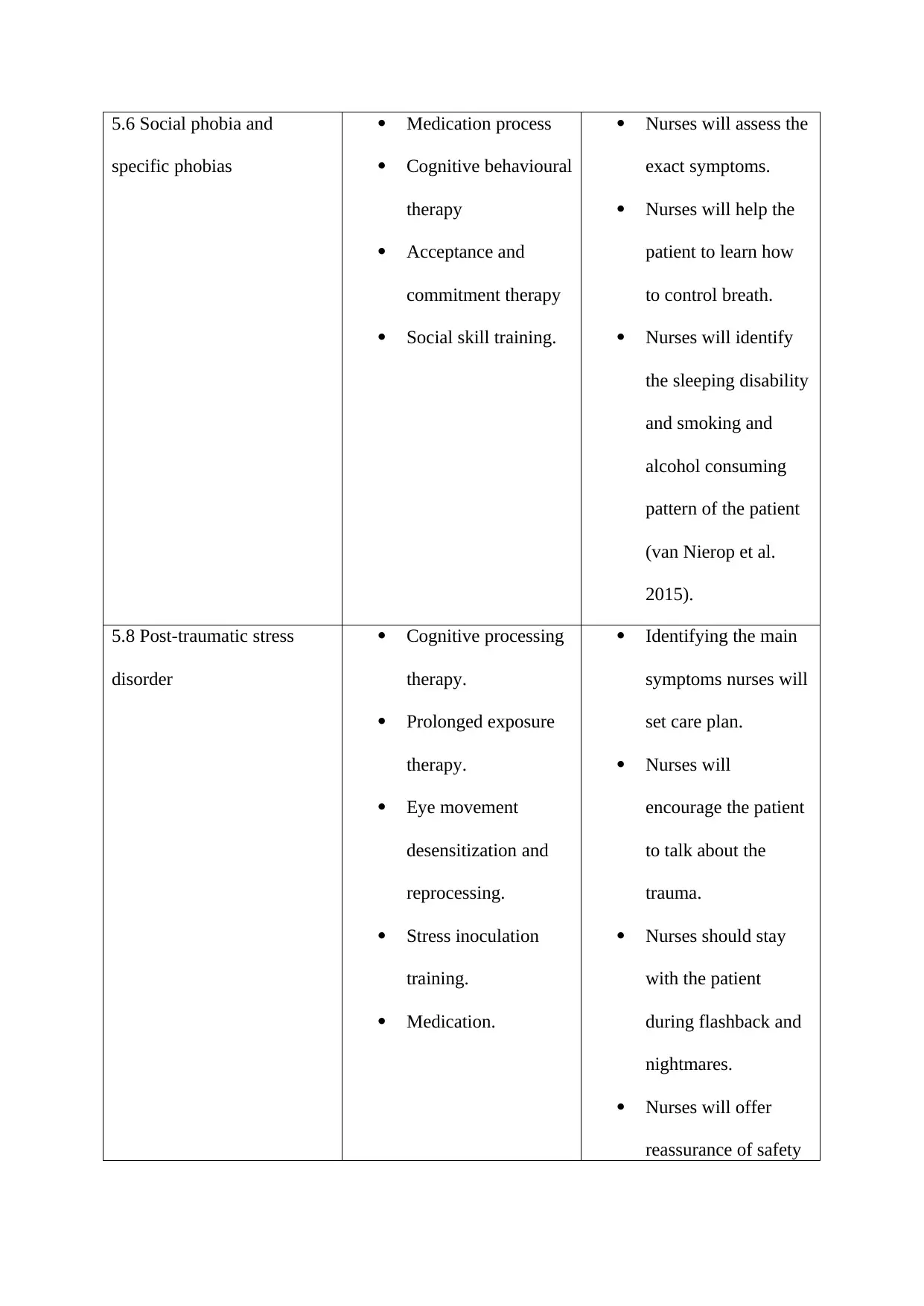
5.6 Social phobia and
specific phobias
Medication process
Cognitive behavioural
therapy
Acceptance and
commitment therapy
Social skill training.
Nurses will assess the
exact symptoms.
Nurses will help the
patient to learn how
to control breath.
Nurses will identify
the sleeping disability
and smoking and
alcohol consuming
pattern of the patient
(van Nierop et al.
2015).
5.8 Post-traumatic stress
disorder
Cognitive processing
therapy.
Prolonged exposure
therapy.
Eye movement
desensitization and
reprocessing.
Stress inoculation
training.
Medication.
Identifying the main
symptoms nurses will
set care plan.
Nurses will
encourage the patient
to talk about the
trauma.
Nurses should stay
with the patient
during flashback and
nightmares.
Nurses will offer
reassurance of safety
specific phobias
Medication process
Cognitive behavioural
therapy
Acceptance and
commitment therapy
Social skill training.
Nurses will assess the
exact symptoms.
Nurses will help the
patient to learn how
to control breath.
Nurses will identify
the sleeping disability
and smoking and
alcohol consuming
pattern of the patient
(van Nierop et al.
2015).
5.8 Post-traumatic stress
disorder
Cognitive processing
therapy.
Prolonged exposure
therapy.
Eye movement
desensitization and
reprocessing.
Stress inoculation
training.
Medication.
Identifying the main
symptoms nurses will
set care plan.
Nurses will
encourage the patient
to talk about the
trauma.
Nurses should stay
with the patient
during flashback and
nightmares.
Nurses will offer
reassurance of safety
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
and security.
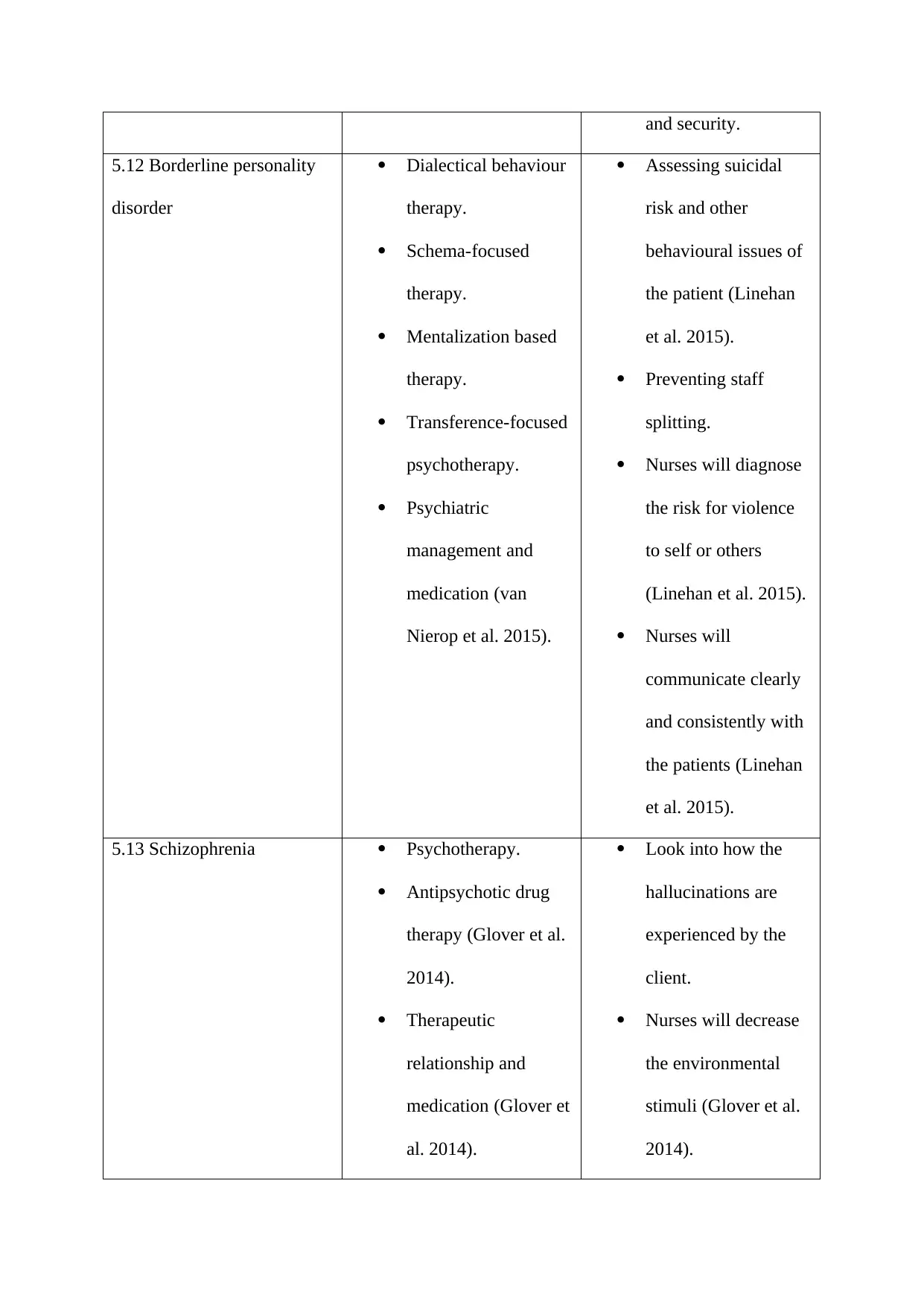
5.12 Borderline personality
disorder
Dialectical behaviour
therapy.
Schema-focused
therapy.
Mentalization based
therapy.
Transference-focused
psychotherapy.
Psychiatric
management and
medication (van
Nierop et al. 2015).
Assessing suicidal
risk and other
behavioural issues of
the patient (Linehan
et al. 2015).
Preventing staff
splitting.
Nurses will diagnose
the risk for violence
to self or others
(Linehan et al. 2015).
Nurses will
communicate clearly
and consistently with
the patients (Linehan
et al. 2015).
5.13 Schizophrenia Psychotherapy.
Antipsychotic drug
therapy (Glover et al.
2014).
Therapeutic
relationship and
medication (Glover et
al. 2014).
Look into how the
hallucinations are
experienced by the
client.
Nurses will decrease
the environmental
stimuli (Glover et al.
2014).
5.12 Borderline personality
disorder
Dialectical behaviour
therapy.
Schema-focused
therapy.
Mentalization based
therapy.
Transference-focused
psychotherapy.
Psychiatric
management and
medication (van
Nierop et al. 2015).
Assessing suicidal
risk and other
behavioural issues of
the patient (Linehan
et al. 2015).
Preventing staff
splitting.
Nurses will diagnose
the risk for violence
to self or others
(Linehan et al. 2015).
Nurses will
communicate clearly
and consistently with
the patients (Linehan
et al. 2015).
5.13 Schizophrenia Psychotherapy.
Antipsychotic drug
therapy (Glover et al.
2014).
Therapeutic
relationship and
medication (Glover et
al. 2014).
Look into how the
hallucinations are
experienced by the
client.
Nurses will decrease
the environmental
stimuli (Glover et al.
2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Involve the client in
reality-based
activities.
Nurses will intervene
with medication as
per the requirement
(Glover et al. 2014).
5.14 Dementia Medications
Occupational therapy
Modifying the
environment.
Identifying the
symptoms nurses will
set action plan.
Nurses will
encourage the
patients to do exercise
in order to improve
strength and
cardiovascular health.
Nurses will plan
curriculum activities
for the patients to live
a better life.
7.
The 5 (five) principles of recovery in the mental health context are as follows.
i. Uniqueness of the individual-
reality-based
activities.
Nurses will intervene
with medication as
per the requirement
(Glover et al. 2014).
5.14 Dementia Medications
Occupational therapy
Modifying the
environment.
Identifying the
symptoms nurses will
set action plan.
Nurses will
encourage the
patients to do exercise
in order to improve
strength and
cardiovascular health.
Nurses will plan
curriculum activities
for the patients to live
a better life.
7.
The 5 (five) principles of recovery in the mental health context are as follows.
i. Uniqueness of the individual-
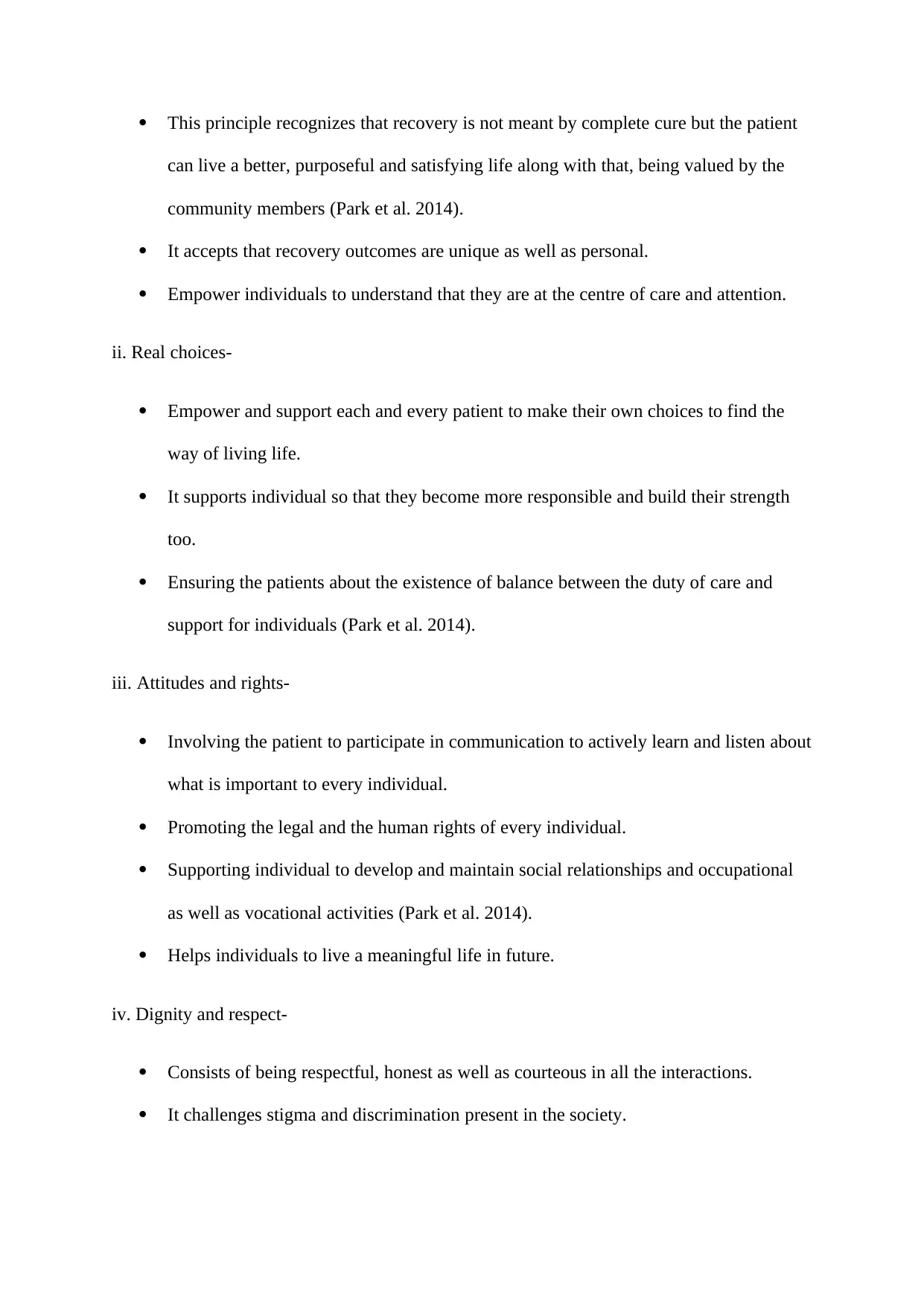
This principle recognizes that recovery is not meant by complete cure but the patient
can live a better, purposeful and satisfying life along with that, being valued by the
community members (Park et al. 2014).
It accepts that recovery outcomes are unique as well as personal.
Empower individuals to understand that they are at the centre of care and attention.
ii. Real choices-
Empower and support each and every patient to make their own choices to find the
way of living life.
It supports individual so that they become more responsible and build their strength
too.
Ensuring the patients about the existence of balance between the duty of care and
support for individuals (Park et al. 2014).
iii. Attitudes and rights-
Involving the patient to participate in communication to actively learn and listen about
what is important to every individual.
Promoting the legal and the human rights of every individual.
Supporting individual to develop and maintain social relationships and occupational
as well as vocational activities (Park et al. 2014).
Helps individuals to live a meaningful life in future.
iv. Dignity and respect-
Consists of being respectful, honest as well as courteous in all the interactions.
It challenges stigma and discrimination present in the society.
can live a better, purposeful and satisfying life along with that, being valued by the
community members (Park et al. 2014).
It accepts that recovery outcomes are unique as well as personal.
Empower individuals to understand that they are at the centre of care and attention.
ii. Real choices-
Empower and support each and every patient to make their own choices to find the
way of living life.
It supports individual so that they become more responsible and build their strength
too.
Ensuring the patients about the existence of balance between the duty of care and
support for individuals (Park et al. 2014).
iii. Attitudes and rights-
Involving the patient to participate in communication to actively learn and listen about
what is important to every individual.
Promoting the legal and the human rights of every individual.
Supporting individual to develop and maintain social relationships and occupational
as well as vocational activities (Park et al. 2014).
Helps individuals to live a meaningful life in future.
iv. Dignity and respect-
Consists of being respectful, honest as well as courteous in all the interactions.
It challenges stigma and discrimination present in the society.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Involves respect and sensitivity of every individual for their culture, beliefs as well as
values (Park et al. 2014).
v. Partnership and communication-
Involves working in partnership as well as in individuals.
Values the importance of communication to share relevant information for enabling
effective management (Park et al. 2014).
Involves working in realistic and positive cultures to set their goals, hopes and
aspirations.
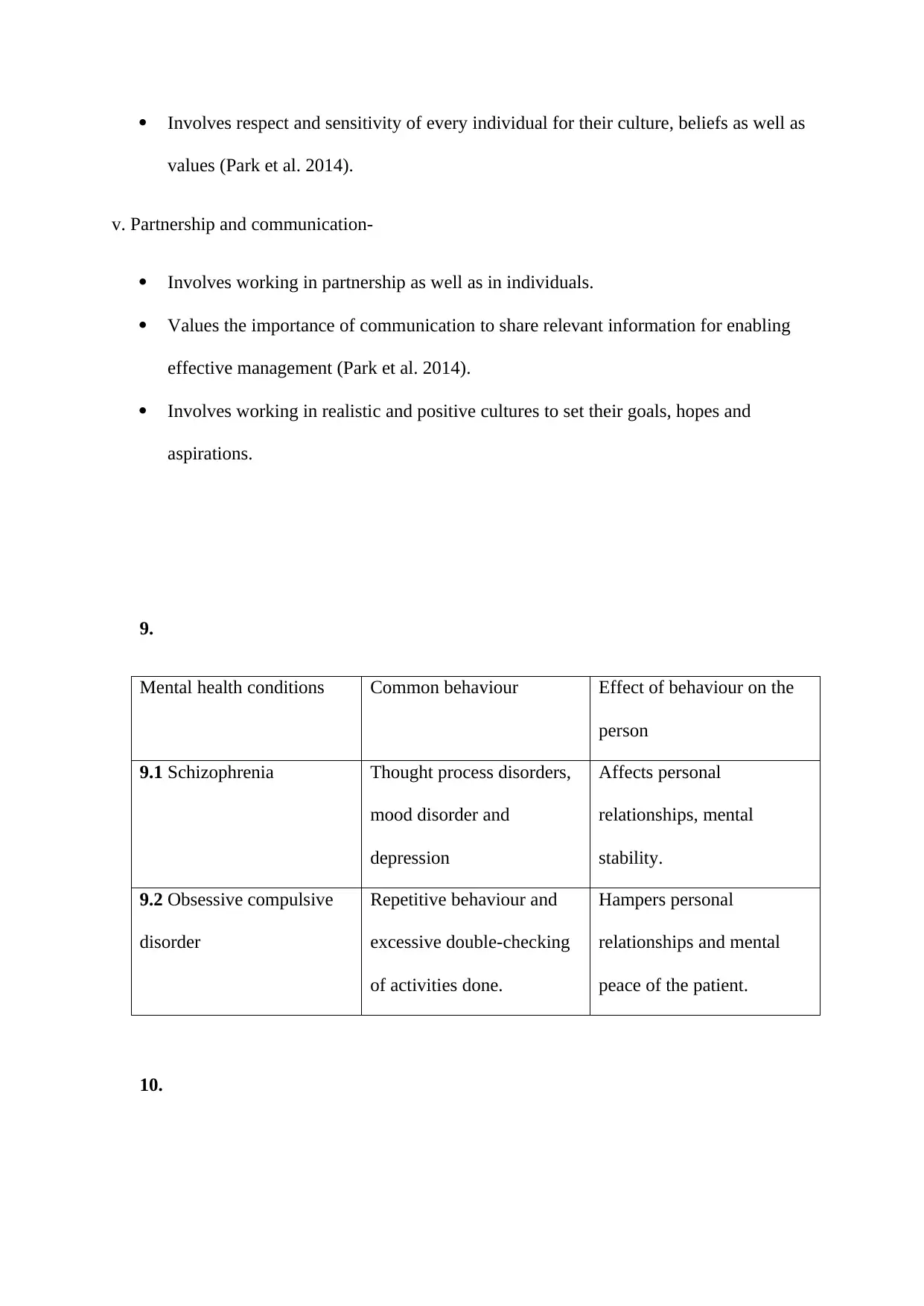
9.
Mental health conditions Common behaviour Effect of behaviour on the
person
9.1 Schizophrenia Thought process disorders,
mood disorder and
depression
Affects personal
relationships, mental
stability.
9.2 Obsessive compulsive
disorder
Repetitive behaviour and
excessive double-checking
of activities done.
Hampers personal
relationships and mental
peace of the patient.
10.
values (Park et al. 2014).
v. Partnership and communication-
Involves working in partnership as well as in individuals.
Values the importance of communication to share relevant information for enabling
effective management (Park et al. 2014).
Involves working in realistic and positive cultures to set their goals, hopes and
aspirations.
9.
Mental health conditions Common behaviour Effect of behaviour on the
person
9.1 Schizophrenia Thought process disorders,
mood disorder and
depression
Affects personal
relationships, mental
stability.
9.2 Obsessive compulsive
disorder
Repetitive behaviour and
excessive double-checking
of activities done.
Hampers personal
relationships and mental
peace of the patient.
10.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The effect of stigma includes the feeling of hopelessness, shame and isolation from the
society among the patients. In this disorder, patient becomes reluctant to ask for help or
treatment also. This affects the social and personal relationship. Even, due to such
disorder a person may not get employment and other opportunities in the society (Glover
et al. 2014). The patient also suffers from self-doubt and it affects their mental health in a
negative way.
12.1
Challenging behaviour is an aggressive behaviour of a patient in which verbal as well as
physical attack can occur. It is a common behavioural disorder among the dementia
patients. Dealing with such behaviour can be challenging for the nurses as well as other
health professionals (Sheehan et al. 2015).
12.2
Person centred care plan should be prepared in order to manage the challenging behaviour
of the dementia patient. Various types of sensory simulations such as hand massage can
help the patient. Music can soothe the patient and provide some relaxation (Sheehan et al.
2015).
society among the patients. In this disorder, patient becomes reluctant to ask for help or
treatment also. This affects the social and personal relationship. Even, due to such
disorder a person may not get employment and other opportunities in the society (Glover
et al. 2014). The patient also suffers from self-doubt and it affects their mental health in a
negative way.
12.1
Challenging behaviour is an aggressive behaviour of a patient in which verbal as well as
physical attack can occur. It is a common behavioural disorder among the dementia
patients. Dealing with such behaviour can be challenging for the nurses as well as other
health professionals (Sheehan et al. 2015).
12.2
Person centred care plan should be prepared in order to manage the challenging behaviour
of the dementia patient. Various types of sensory simulations such as hand massage can
help the patient. Music can soothe the patient and provide some relaxation (Sheehan et al.
2015).
References
Glover, G., Bernard, S., Branford, D., Holland, A. and Strydom, A., 2014. Use of
medication for challenging behaviour in people with intellectual disability. The British
Journal of Psychiatry, 205(1), pp.6-7.
Linehan, M.M., Korslund, K.E., Harned, M.S., Gallop, R.J., Lungu, A., Neacsiu, A.D.,
McDavid, J., Comtois, K.A. and Murray-Gregory, A.M., 2015. Dialectical behavior
therapy for high suicide risk in individuals with borderline personality disorder: a
randomized clinical trial and component analysis. JAMA psychiatry, 72(5), pp.475-482.
Park, M.M., Zafran, H., Stewart, J., Salsberg, J., Ells, C., Rouleau, S., Estein, O. and
Valente, T.W., 2014. Transforming mental health services: a participatory mixed methods
study to promote and evaluate the implementation of recovery-oriented
services. Implementation science, 9(1), p.119.
Sheehan, R., Hassiotis, A., Walters, K., Osborn, D., Strydom, A. and Horsfall, L., 2015.
Mental illness, challenging behaviour, and psychotropic drug prescribing in people with
intellectual disability: UK population based cohort study. Bmj, 351, p.h4326.
van Nierop, M., Viechtbauer, W., Gunther, N., Van Zelst, C., De Graaf, R., Ten Have,
M., Van Dorsselaer, S., Bak, M., van Winkel, R. and OUtcome of Psychosis (GROUP)
investigators, 2015. Childhood trauma is associated with a specific admixture of affective,
anxiety, and psychosis symptoms cutting across traditional diagnostic
boundaries. Psychological medicine, 45(6), pp.1277-1288.
Glover, G., Bernard, S., Branford, D., Holland, A. and Strydom, A., 2014. Use of
medication for challenging behaviour in people with intellectual disability. The British
Journal of Psychiatry, 205(1), pp.6-7.
Linehan, M.M., Korslund, K.E., Harned, M.S., Gallop, R.J., Lungu, A., Neacsiu, A.D.,
McDavid, J., Comtois, K.A. and Murray-Gregory, A.M., 2015. Dialectical behavior
therapy for high suicide risk in individuals with borderline personality disorder: a
randomized clinical trial and component analysis. JAMA psychiatry, 72(5), pp.475-482.
Park, M.M., Zafran, H., Stewart, J., Salsberg, J., Ells, C., Rouleau, S., Estein, O. and
Valente, T.W., 2014. Transforming mental health services: a participatory mixed methods
study to promote and evaluate the implementation of recovery-oriented
services. Implementation science, 9(1), p.119.
Sheehan, R., Hassiotis, A., Walters, K., Osborn, D., Strydom, A. and Horsfall, L., 2015.
Mental illness, challenging behaviour, and psychotropic drug prescribing in people with
intellectual disability: UK population based cohort study. Bmj, 351, p.h4326.
van Nierop, M., Viechtbauer, W., Gunther, N., Van Zelst, C., De Graaf, R., Ten Have,
M., Van Dorsselaer, S., Bak, M., van Winkel, R. and OUtcome of Psychosis (GROUP)
investigators, 2015. Childhood trauma is associated with a specific admixture of affective,
anxiety, and psychosis symptoms cutting across traditional diagnostic
boundaries. Psychological medicine, 45(6), pp.1277-1288.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





