Mental Health and Wellbeing: Analysis, Risks, and Care Planning
VerifiedAdded on 2023/04/21
|11
|2898
|165
Report
AI Summary
This report provides a comprehensive analysis of a mental health case involving a patient named Dimitrie, who is experiencing symptoms of schizophrenia, including auditory hallucinations. The report begins with a detailed Mental Status Examination (MSE), covering aspects such as appearance, behavior, affect, mood, speech, thought form, thought content, perception, cognition, and insight. Four key risks related to Dimitrie's condition are identified: worsening psychological health due to inconsistent medication and hallucinations, danger of harming others, risk of social isolation, and absence of mental peace. A nursing care plan is then developed to address the patient's schizophrenia, focusing on creating a calm environment, avoiding physical touch, and understanding the patient's delusions. Finally, the report critiques the nurse's interaction with the patient, highlighting both positive and negative elements of their therapeutic communication. Desklib offers similar solved assignments for students.

Running head: MENTAL HEALTH AND WELLBEING
MENTAL HEALTH AND WELLBEING
Name of the Student:
Name of the University:
Author note:
MENTAL HEALTH AND WELLBEING
Name of the Student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1MENTAL HEALTH AND WELLBEING
1) Mental Status Examination (MSE)-
Appearance: The patient Dimitrie appeared to be quite young with lean body
structure. He appeared physically healthy and well groomed; he was wearing a black
t-shirt with loose fitted shirt and a pant and had combed his hair. He had a habit of
biting his nails, which showed that he lacked good hygiene. Dimitrie had long black
hair with thin black moustache. He was wearing spectacles and had no notable
characteristics such as tattoos or piercing. Dimitrie was not sitting in a very poised
manner, instead was changing his body-posture quite frequently.
Behaviour: Dimitrie was very confused and not comfortable in front of the nurse, he
looked quite distressed. The nurse was trying to develop a good rapport with the
patient and was continuously asking him questions in order to understand his problem
and concern. Dimitrie was not responding to the nurse in an effective way due to his
mental health condition. He was responding in a haphazard way to the questions’ that
the nurse was asking him. He had poor psychometric skills, where he could not
control his mind and his emotions; hence, he lacked good coordination and balance.
He had a very confused attitude and his behaviour was quite complex due to his
health condition.
Affect: Dimitrie had a very restricted emotional response. He was not responding
effectively to the questions’ that the nurse was asking him. He had a delayed response
towards every question of the nurse and was not very open about his emotions. He
was very restricted and reserved and could not open up to the nurse. He lacked in
efficiently expressing his thoughts and feelings to the nurse and just answered her
questions with no clear outcome. Dimitrie was very confused regarding his thoughts
and responses. He was taking time to understand what exactly he has to say to the
nurse.
1) Mental Status Examination (MSE)-
Appearance: The patient Dimitrie appeared to be quite young with lean body
structure. He appeared physically healthy and well groomed; he was wearing a black
t-shirt with loose fitted shirt and a pant and had combed his hair. He had a habit of
biting his nails, which showed that he lacked good hygiene. Dimitrie had long black
hair with thin black moustache. He was wearing spectacles and had no notable
characteristics such as tattoos or piercing. Dimitrie was not sitting in a very poised
manner, instead was changing his body-posture quite frequently.
Behaviour: Dimitrie was very confused and not comfortable in front of the nurse, he
looked quite distressed. The nurse was trying to develop a good rapport with the
patient and was continuously asking him questions in order to understand his problem
and concern. Dimitrie was not responding to the nurse in an effective way due to his
mental health condition. He was responding in a haphazard way to the questions’ that
the nurse was asking him. He had poor psychometric skills, where he could not
control his mind and his emotions; hence, he lacked good coordination and balance.
He had a very confused attitude and his behaviour was quite complex due to his
health condition.
Affect: Dimitrie had a very restricted emotional response. He was not responding
effectively to the questions’ that the nurse was asking him. He had a delayed response
towards every question of the nurse and was not very open about his emotions. He
was very restricted and reserved and could not open up to the nurse. He lacked in
efficiently expressing his thoughts and feelings to the nurse and just answered her
questions with no clear outcome. Dimitrie was very confused regarding his thoughts
and responses. He was taking time to understand what exactly he has to say to the
nurse.
2MENTAL HEALTH AND WELLBEING
Mood: Dimitrie had a very fluctuating mood and response. He was feeling very
distressed and could not really open up with the nurse. He was facing a major problem
in controlling his mood as he was getting continuously distracted and disturbed by
some background noise that he could hear around him. His mood was fluctuating very
quickly and could not focus properly. Dimitrie could explain his problems to the nurse
but in a haphazard manner with no clear emotions. He lacked in explaining the depth
and intensity of his emotions to the nurse and could not convey his feelings properly.
Speech: Dimitrie was facing a major issue in speaking fluently. He was not replying
confidently to the questions’ asked by the nurse. His tone and volume of speaking was
very low and lacked confidence. Dimitrie was not very specific while speaking to the
nurse and was very slow and sluggish in responding and conveying his thoughts and
emotions to the nurse. His flow of speaking was very discontinuous and unclear. He
was taking time to complete his sentence and he was unclear with his words. Dimitrie
was taking a pause before speaking and in middle of his conversations and was
repeating words.
Thought Form: Dimitrie was unable to frame his ideas and thoughts properly. He was
very confused in expressing his thoughts and ideas. Dimitrie had a very vague
approach in framing his ideas together. Dimitrie had a weak association between his
thoughts and his mind and he lacked logical thought process. There was no continuity
in explaining his thoughts to the nurse and he was very unclear with his thought form.
Dimitrie was very restricted and blocked in explaining his thoughts and he kept on
pausing and getting distracted while responding about his feelings and thoughts to the
nurse.
Thought Content: Dimitrie was facing major delusion in explaining about his actual
thinking. He could not explain clearly to the nurse regarding what was exactly going
Mood: Dimitrie had a very fluctuating mood and response. He was feeling very
distressed and could not really open up with the nurse. He was facing a major problem
in controlling his mood as he was getting continuously distracted and disturbed by
some background noise that he could hear around him. His mood was fluctuating very
quickly and could not focus properly. Dimitrie could explain his problems to the nurse
but in a haphazard manner with no clear emotions. He lacked in explaining the depth
and intensity of his emotions to the nurse and could not convey his feelings properly.
Speech: Dimitrie was facing a major issue in speaking fluently. He was not replying
confidently to the questions’ asked by the nurse. His tone and volume of speaking was
very low and lacked confidence. Dimitrie was not very specific while speaking to the
nurse and was very slow and sluggish in responding and conveying his thoughts and
emotions to the nurse. His flow of speaking was very discontinuous and unclear. He
was taking time to complete his sentence and he was unclear with his words. Dimitrie
was taking a pause before speaking and in middle of his conversations and was
repeating words.
Thought Form: Dimitrie was unable to frame his ideas and thoughts properly. He was
very confused in expressing his thoughts and ideas. Dimitrie had a very vague
approach in framing his ideas together. Dimitrie had a weak association between his
thoughts and his mind and he lacked logical thought process. There was no continuity
in explaining his thoughts to the nurse and he was very unclear with his thought form.
Dimitrie was very restricted and blocked in explaining his thoughts and he kept on
pausing and getting distracted while responding about his feelings and thoughts to the
nurse.
Thought Content: Dimitrie was facing major delusion in explaining about his actual
thinking. He could not explain clearly to the nurse regarding what was exactly going
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3MENTAL HEALTH AND WELLBEING
in his mind. He lacked in providing any detailed information to the nurse and he was
only answering in a very reluctant manner with no clear idea and thought. The nurse
was continuously asking him questions to understand what exactly was going in his
mind but he lacked clear idea and perception about his thoughts. Dimitrie was not a
very social kind of a person and lack in speaking fluently, which made it difficult for
the people to understand what was exactly going in his mind and what was he exactly
thinking.
Perception: Dimitrie was facing an auditory hallucination that was continuously
distracting him and his thoughts. He could not complete his sentence and focus
properly as he was suffering from complete hallucination that was distracting his
peace of mind. Even while answering to the nurse he was very distressed and
distracted by those hallucinated voices.
Cognition and Intellectual Functioning: Dimitrie lacked proper concentration as some
hallucinated voices were distracting him. He could recall his memory and happenings
that took place in his life but was not at all confident. His calculation skill was good
as he could answer to the question of the nurse correctly but gain he lack confidence
and stated that those background voices were distracting him and not allowing him to
think effectively. Dimitrie had knowledge about what was happening around him but
his ability to concentrate or be attentive was very bad.
Insight and Judgement: Dimitrie was aware about his health condition and knew that
he was suffering from schizophrenia were he lost his ability to think and behave. He
was also aware that his friend bought him to the nurse for check-up, as his mental
health was getting bad day by day. When the doctor ask him that if he was aware of
his health condition he accepted that he was suffering from a mental health disorder
in his mind. He lacked in providing any detailed information to the nurse and he was
only answering in a very reluctant manner with no clear idea and thought. The nurse
was continuously asking him questions to understand what exactly was going in his
mind but he lacked clear idea and perception about his thoughts. Dimitrie was not a
very social kind of a person and lack in speaking fluently, which made it difficult for
the people to understand what was exactly going in his mind and what was he exactly
thinking.
Perception: Dimitrie was facing an auditory hallucination that was continuously
distracting him and his thoughts. He could not complete his sentence and focus
properly as he was suffering from complete hallucination that was distracting his
peace of mind. Even while answering to the nurse he was very distressed and
distracted by those hallucinated voices.
Cognition and Intellectual Functioning: Dimitrie lacked proper concentration as some
hallucinated voices were distracting him. He could recall his memory and happenings
that took place in his life but was not at all confident. His calculation skill was good
as he could answer to the question of the nurse correctly but gain he lack confidence
and stated that those background voices were distracting him and not allowing him to
think effectively. Dimitrie had knowledge about what was happening around him but
his ability to concentrate or be attentive was very bad.
Insight and Judgement: Dimitrie was aware about his health condition and knew that
he was suffering from schizophrenia were he lost his ability to think and behave. He
was also aware that his friend bought him to the nurse for check-up, as his mental
health was getting bad day by day. When the doctor ask him that if he was aware of
his health condition he accepted that he was suffering from a mental health disorder
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4MENTAL HEALTH AND WELLBEING
but he was not aware of the consequences that can occur due to his mental health
disorder.
but he was not aware of the consequences that can occur due to his mental health
disorder.
5MENTAL HEALTH AND WELLBEING
The four identified risk related to the client Dimitrie, interviewed in the video includes
the following:
Worsening of psychological health condition because of inconsistence to medicines
and auditory hallucination
As seen in the video, dimitrie was facing from long-term auditory hallucination stating
that random voices were distressing and distracting him, which disturbs his focus and
concentration (Ribe et al., 2015). When the nurse asked him that why did he discontinued his
medications in Japan, dimitrie replied that he was there for just 3 months and once his
medicines was over he was not concerned to buy his medicines as he could not understand
Japanese writing. This statement by dimitrie showed that he was inconsistent in taking his
medicines, which was effecting his health even more.
Danger of hurting or injuring others
It was noted and seen in the video that dimitrie tried to harm him and others. He
explained that he would never harm him even if the hallucinating voice asked him to do so
but will harm others who will try to attack him. Hence, it was predicted that he had self-
destructive factor in his conduct (Silverstein et al., 2015).
Risk of societal isolation
Dimitrie was at high risk of social seclusion, as his acquaintances lived in suburb and he
did not visit them very frequently. He also stated that he did not communicate much with his
family and friends and was mostly alone most of the time. Dimitrie also state that, as he was
not included in his family he was suffering from feeling of lowliness and danger of
depression, mental ill health and negative confidence (Giacco et al., 2016).
The four identified risk related to the client Dimitrie, interviewed in the video includes
the following:
Worsening of psychological health condition because of inconsistence to medicines
and auditory hallucination
As seen in the video, dimitrie was facing from long-term auditory hallucination stating
that random voices were distressing and distracting him, which disturbs his focus and
concentration (Ribe et al., 2015). When the nurse asked him that why did he discontinued his
medications in Japan, dimitrie replied that he was there for just 3 months and once his
medicines was over he was not concerned to buy his medicines as he could not understand
Japanese writing. This statement by dimitrie showed that he was inconsistent in taking his
medicines, which was effecting his health even more.
Danger of hurting or injuring others
It was noted and seen in the video that dimitrie tried to harm him and others. He
explained that he would never harm him even if the hallucinating voice asked him to do so
but will harm others who will try to attack him. Hence, it was predicted that he had self-
destructive factor in his conduct (Silverstein et al., 2015).
Risk of societal isolation
Dimitrie was at high risk of social seclusion, as his acquaintances lived in suburb and he
did not visit them very frequently. He also stated that he did not communicate much with his
family and friends and was mostly alone most of the time. Dimitrie also state that, as he was
not included in his family he was suffering from feeling of lowliness and danger of
depression, mental ill health and negative confidence (Giacco et al., 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6MENTAL HEALTH AND WELLBEING
Absence of mental peace
As dimitrie was hearing some hallucinated voices, he was continuously getting distracted
and diverted. He could not focus properly or could speak to anyone normally (Erickson,
Ruffle & Gold, 2016). His mental peace of mind was lost and as his health was further
deteriorating, he could face some major consequence in the future.
2) Nursing care plan:
The major risk or issue that the patient was suffering was schizophrenia, a condition
were the patient was hearing some background hallucinated voices, which was continuously
distracting him and effecting his mental health (Meehl, 2017). This mental health disorder
was getting worse day-by-day and required immediate concern.
The patient was suffering from major effects of schizophrenia, where he could not
control his thoughts and lost balance between his mind and thought activity. Dimitrie
mentioned that he used to always hear those voices and could not focus on anything; he also
stated that he was in danger of getting into depression, mental ill health and suffered negative
confidence, which were considered as the major impact of schizophrenia (Whalley et al.,
2015). He used to get distracted from his work and was secluded from family and friends.
The ultimate goal will be to develop an effective nursing care plan with proper
nursing intervention for schizophrenia to help dimitrie in recovering from his mental health
condition as soon as possible with effective care approach to distract him from hallucinated
voices that he used to listen and help him to lead a normal life (Bighelli et al., 2018).
The nursing intervention and rationale developed for the patient are described as
follows:
Absence of mental peace
As dimitrie was hearing some hallucinated voices, he was continuously getting distracted
and diverted. He could not focus properly or could speak to anyone normally (Erickson,
Ruffle & Gold, 2016). His mental peace of mind was lost and as his health was further
deteriorating, he could face some major consequence in the future.
2) Nursing care plan:
The major risk or issue that the patient was suffering was schizophrenia, a condition
were the patient was hearing some background hallucinated voices, which was continuously
distracting him and effecting his mental health (Meehl, 2017). This mental health disorder
was getting worse day-by-day and required immediate concern.
The patient was suffering from major effects of schizophrenia, where he could not
control his thoughts and lost balance between his mind and thought activity. Dimitrie
mentioned that he used to always hear those voices and could not focus on anything; he also
stated that he was in danger of getting into depression, mental ill health and suffered negative
confidence, which were considered as the major impact of schizophrenia (Whalley et al.,
2015). He used to get distracted from his work and was secluded from family and friends.
The ultimate goal will be to develop an effective nursing care plan with proper
nursing intervention for schizophrenia to help dimitrie in recovering from his mental health
condition as soon as possible with effective care approach to distract him from hallucinated
voices that he used to listen and help him to lead a normal life (Bighelli et al., 2018).
The nursing intervention and rationale developed for the patient are described as
follows:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7MENTAL HEALTH AND WELLBEING
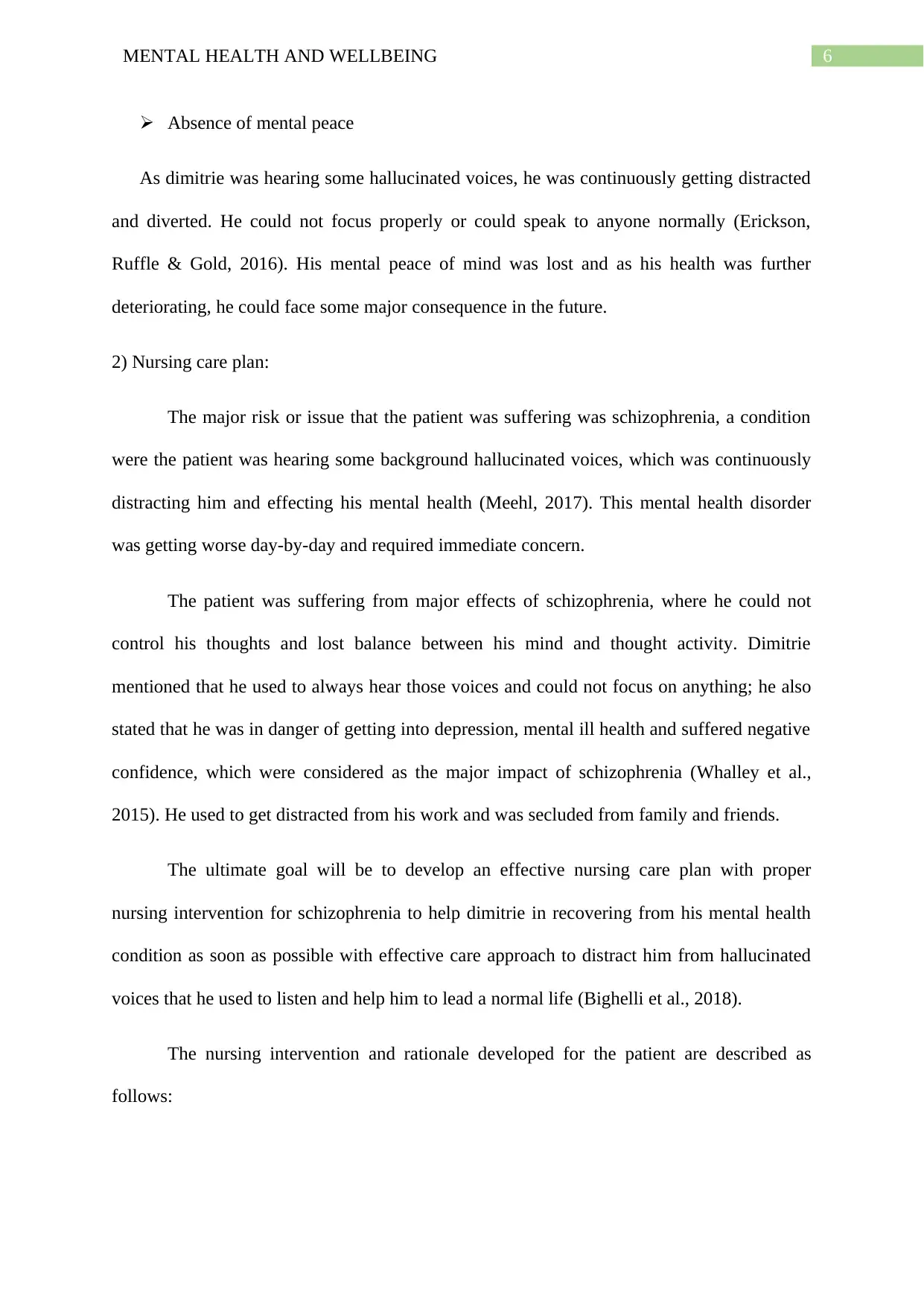
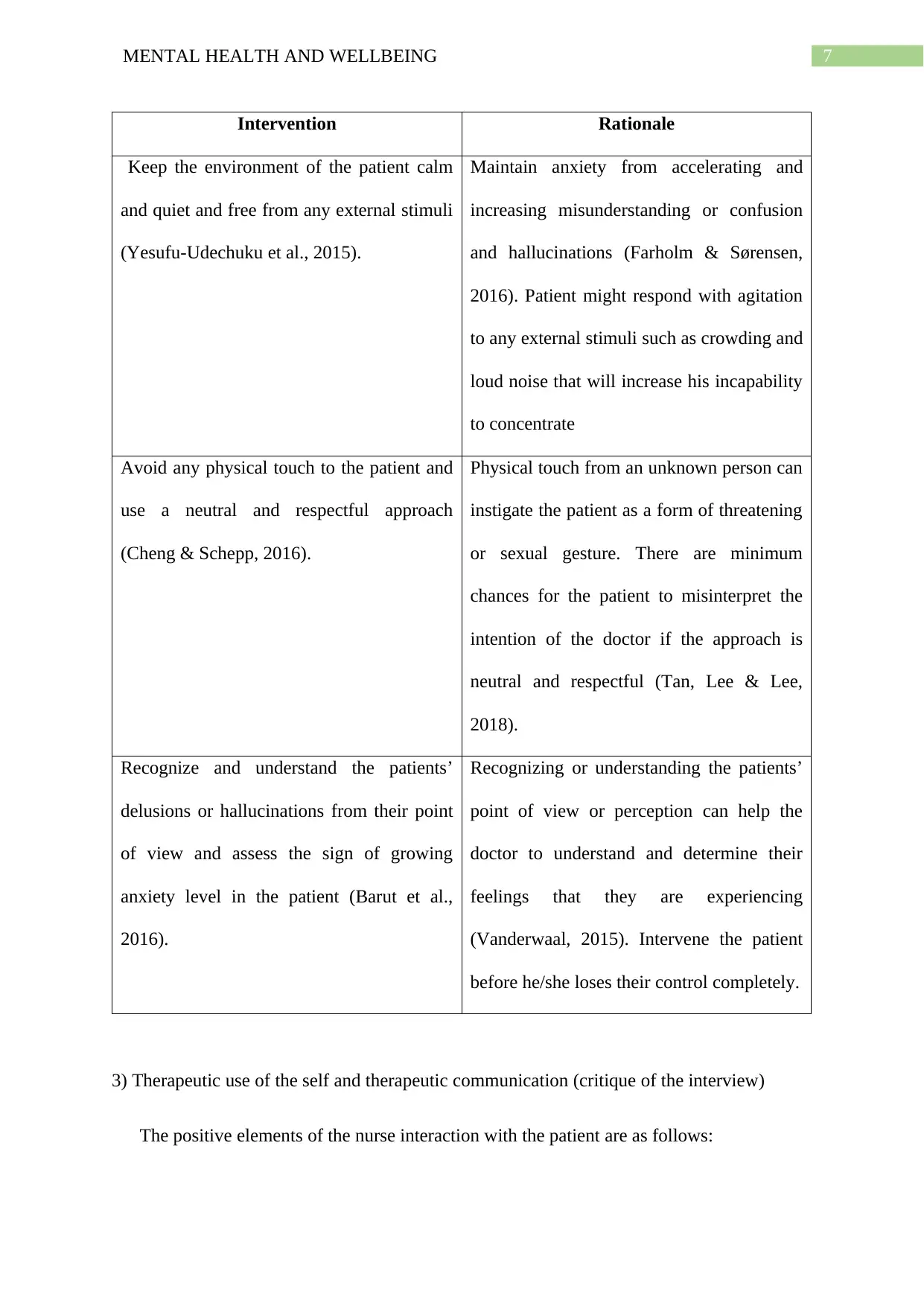
Intervention Rationale
Keep the environment of the patient calm
and quiet and free from any external stimuli
(Yesufu-Udechuku et al., 2015).
Maintain anxiety from accelerating and
increasing misunderstanding or confusion
and hallucinations (Farholm & Sørensen,
2016). Patient might respond with agitation
to any external stimuli such as crowding and
loud noise that will increase his incapability
to concentrate
Avoid any physical touch to the patient and
use a neutral and respectful approach
(Cheng & Schepp, 2016).
Physical touch from an unknown person can
instigate the patient as a form of threatening
or sexual gesture. There are minimum
chances for the patient to misinterpret the
intention of the doctor if the approach is
neutral and respectful (Tan, Lee & Lee,
2018).
Recognize and understand the patients’
delusions or hallucinations from their point
of view and assess the sign of growing
anxiety level in the patient (Barut et al.,
2016).
Recognizing or understanding the patients’
point of view or perception can help the
doctor to understand and determine their
feelings that they are experiencing
(Vanderwaal, 2015). Intervene the patient
before he/she loses their control completely.
3) Therapeutic use of the self and therapeutic communication (critique of the interview)
The positive elements of the nurse interaction with the patient are as follows:
Intervention Rationale
Keep the environment of the patient calm
and quiet and free from any external stimuli
(Yesufu-Udechuku et al., 2015).
Maintain anxiety from accelerating and
increasing misunderstanding or confusion
and hallucinations (Farholm & Sørensen,
2016). Patient might respond with agitation
to any external stimuli such as crowding and
loud noise that will increase his incapability
to concentrate
Avoid any physical touch to the patient and
use a neutral and respectful approach
(Cheng & Schepp, 2016).
Physical touch from an unknown person can
instigate the patient as a form of threatening
or sexual gesture. There are minimum
chances for the patient to misinterpret the
intention of the doctor if the approach is
neutral and respectful (Tan, Lee & Lee,
2018).
Recognize and understand the patients’
delusions or hallucinations from their point
of view and assess the sign of growing
anxiety level in the patient (Barut et al.,
2016).
Recognizing or understanding the patients’
point of view or perception can help the
doctor to understand and determine their
feelings that they are experiencing
(Vanderwaal, 2015). Intervene the patient
before he/she loses their control completely.
3) Therapeutic use of the self and therapeutic communication (critique of the interview)
The positive elements of the nurse interaction with the patient are as follows:
8MENTAL HEALTH AND WELLBEING
[1] The nurse could understand in detail about the auditory hallucinations and the
frequency of those hallucinations that the patient was suffering or going through as
the nurse herself witnessed the patient getting distracted by some hallucinating voices
while he was answering to her questions.
[2] The nurse understood that the patient was scared of living alone was affected more
when he is alone or not involved anywhere as the patient mentioned that he could not
sleep peacefully.
[3] The interaction between the nurse and patient allowed the nurse to understand that the
patient could remember everything and had no such memory loss issue as he could
remember the name of medicine and could easily finish the calculation that the nurse
asked him to do.
[4] The interaction helped the nurse to understand what exactly those hallucinated voices
were trying to say or communicate to the patient as the patient mentioned that those
voices were always criticizing him and he was scared of those voices. The nurse also
understood that the patient needed proper medication as the patient stated that
medication could help him to get out of this problem.
The negative elements of the nurse interaction with the patient are as follows:
[1] The patient was not responding and answering properly to the question’s’ that nurse
was asking him, he was responding only in bits and parts hence, the nurse had to take
huge efforts to communicate and understand the problem that the patient was
suffering.
[2] As the nurse was asking too many questions to the patient, he was getting irritated and
anxious of continuously listening to her.
[1] The nurse could understand in detail about the auditory hallucinations and the
frequency of those hallucinations that the patient was suffering or going through as
the nurse herself witnessed the patient getting distracted by some hallucinating voices
while he was answering to her questions.
[2] The nurse understood that the patient was scared of living alone was affected more
when he is alone or not involved anywhere as the patient mentioned that he could not
sleep peacefully.
[3] The interaction between the nurse and patient allowed the nurse to understand that the
patient could remember everything and had no such memory loss issue as he could
remember the name of medicine and could easily finish the calculation that the nurse
asked him to do.
[4] The interaction helped the nurse to understand what exactly those hallucinated voices
were trying to say or communicate to the patient as the patient mentioned that those
voices were always criticizing him and he was scared of those voices. The nurse also
understood that the patient needed proper medication as the patient stated that
medication could help him to get out of this problem.
The negative elements of the nurse interaction with the patient are as follows:
[1] The patient was not responding and answering properly to the question’s’ that nurse
was asking him, he was responding only in bits and parts hence, the nurse had to take
huge efforts to communicate and understand the problem that the patient was
suffering.
[2] As the nurse was asking too many questions to the patient, he was getting irritated and
anxious of continuously listening to her.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9MENTAL HEALTH AND WELLBEING
References
Barut, J. K., Dietrich, M. S., Zanoni, P. A., & Ridner, S. H. (2016). Sense of belonging and
hope in the lives of persons with schizophrenia. Archives of psychiatric nursing,
30(2), 178-184.
Bighelli, I., Salanti, G., Huhn, M., Schneider‐Thoma, J., Krause, M., Reitmeir, C., ... &
Furukawa, T. A. (2018). Psychological interventions to reduce positive symptoms in
schizophrenia: systematic review and network meta‐analysis. World psychiatry, 17(3),
316-329.
Cheng, S. C., & Schepp, K. G. (2016). Early intervention in schizophrenia: a literature
review. Archives of psychiatric nursing, 30(6), 774-781.
Erickson, M. A., Ruffle, A., & Gold, J. M. (2016). A meta-analysis of mismatch negativity in
schizophrenia: from clinical risk to disease specificity and progression. Biological
psychiatry, 79(12), 980-987.
Farholm, A., & Sørensen, M. (2016). Motivation for physical activity and exercise in severe
mental illness: A systematic review of intervention studies. International journal of
mental health nursing, 25(3), 194-205.
Giacco, D., Palumbo, C., Strappelli, N., Catapano, F., & Priebe, S. (2016). Social contacts
and loneliness in people with psychotic and mood disorders. Comprehensive
psychiatry, 66, 59-66.
Meehl, P. E. (2017). Schizotaxia, schizotypy, schizophrenia. In Schizophrenia (pp. 21-46).
Routledge.
Mental Health Assessment: Dimitrie. (2019). Retrieved from
https://www.youtube.com/watch?v=xgo8jvIJAQU&feature=youtu.be&app=desktop
References
Barut, J. K., Dietrich, M. S., Zanoni, P. A., & Ridner, S. H. (2016). Sense of belonging and
hope in the lives of persons with schizophrenia. Archives of psychiatric nursing,
30(2), 178-184.
Bighelli, I., Salanti, G., Huhn, M., Schneider‐Thoma, J., Krause, M., Reitmeir, C., ... &
Furukawa, T. A. (2018). Psychological interventions to reduce positive symptoms in
schizophrenia: systematic review and network meta‐analysis. World psychiatry, 17(3),
316-329.
Cheng, S. C., & Schepp, K. G. (2016). Early intervention in schizophrenia: a literature
review. Archives of psychiatric nursing, 30(6), 774-781.
Erickson, M. A., Ruffle, A., & Gold, J. M. (2016). A meta-analysis of mismatch negativity in
schizophrenia: from clinical risk to disease specificity and progression. Biological
psychiatry, 79(12), 980-987.
Farholm, A., & Sørensen, M. (2016). Motivation for physical activity and exercise in severe
mental illness: A systematic review of intervention studies. International journal of
mental health nursing, 25(3), 194-205.
Giacco, D., Palumbo, C., Strappelli, N., Catapano, F., & Priebe, S. (2016). Social contacts
and loneliness in people with psychotic and mood disorders. Comprehensive
psychiatry, 66, 59-66.
Meehl, P. E. (2017). Schizotaxia, schizotypy, schizophrenia. In Schizophrenia (pp. 21-46).
Routledge.
Mental Health Assessment: Dimitrie. (2019). Retrieved from
https://www.youtube.com/watch?v=xgo8jvIJAQU&feature=youtu.be&app=desktop
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10MENTAL HEALTH AND WELLBEING
Ribe, A. R., Laursen, T. M., Charles, M., Katon, W., Fenger-Grøn, M., Davydow, D., ... &
Vestergaard, M. (2015). Long-term risk of dementia in persons with schizophrenia: a
Danish population-based cohort study. JAMA psychiatry, 72(11), 1095-1101.
Silverstein, S. M., Del Pozzo, J., Roché, M., Boyle, D., & Miskimen, T. (2015).
Schizophrenia and violence: realities and recommendations. Crime psychology
review, 1(1), 21-42.
Tan, B. L., Lee, S. A., & Lee, J. (2018). Social cognitive interventions for people with
schizophrenia: a systematic review. Asian journal of psychiatry, 35, 115-131.
Vanderwaal, F. M. (2015). Impact of motivational interviewing on medication adherence in
schizophrenia. Issues in mental health nursing, 36(11), 900-904.
Whalley, H. C., Hall, L., Romaniuk, L., Macdonald, A., Lawrie, S. M., Sussmann, J. E., &
McIntosh, A. M. (2015). Impact of cross-disorder polygenic risk on frontal brain
activation with specific effect of schizophrenia risk. Schizophrenia research, 161(2-
3), 484-489.
Yesufu-Udechuku, A., Harrison, B., Mayo-Wilson, E., Young, N., Woodhams, P., Shiers, D.,
... & Kendall, T. (2015). Interventions to improve the experience of caring for people
with severe mental illness: systematic review and meta-analysis. The British Journal
of Psychiatry, 206(4), 268-274.
Ribe, A. R., Laursen, T. M., Charles, M., Katon, W., Fenger-Grøn, M., Davydow, D., ... &
Vestergaard, M. (2015). Long-term risk of dementia in persons with schizophrenia: a
Danish population-based cohort study. JAMA psychiatry, 72(11), 1095-1101.
Silverstein, S. M., Del Pozzo, J., Roché, M., Boyle, D., & Miskimen, T. (2015).
Schizophrenia and violence: realities and recommendations. Crime psychology
review, 1(1), 21-42.
Tan, B. L., Lee, S. A., & Lee, J. (2018). Social cognitive interventions for people with
schizophrenia: a systematic review. Asian journal of psychiatry, 35, 115-131.
Vanderwaal, F. M. (2015). Impact of motivational interviewing on medication adherence in
schizophrenia. Issues in mental health nursing, 36(11), 900-904.
Whalley, H. C., Hall, L., Romaniuk, L., Macdonald, A., Lawrie, S. M., Sussmann, J. E., &
McIntosh, A. M. (2015). Impact of cross-disorder polygenic risk on frontal brain
activation with specific effect of schizophrenia risk. Schizophrenia research, 161(2-
3), 484-489.
Yesufu-Udechuku, A., Harrison, B., Mayo-Wilson, E., Young, N., Woodhams, P., Shiers, D.,
... & Kendall, T. (2015). Interventions to improve the experience of caring for people
with severe mental illness: systematic review and meta-analysis. The British Journal
of Psychiatry, 206(4), 268-274.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





