Mental Status Examination, Risk Assessment, and Care Plan Report
VerifiedAdded on 2022/08/19
|8
|3278
|14
Report
AI Summary
This report presents a Mental Status Examination (MSE) of a client, modeled after NSW HEALTH guidelines, based on a video interview. The MSE covers the client's appearance, behavior, affect, mood, speech, thought form, thought content, perception, cognition, insight, and judgment, revealing symptoms such as auditory hallucinations and mild depression. The report identifies four key risks: severe depressive symptoms, suicide ideation, potential for violent behavior, and self-harm. A care plan is then developed, prioritizing the risk of suicide ideation. The care plan includes interventions such as collaboration with a general practitioner for Olanzapine administration, referral for Cognitive Behavioral Therapy (CBT), and family therapy, with rationales provided for each intervention. The report also analyzes the interviewer's positive interactions with the client, highlighting active listening, empathy, and obtaining consent, and provides a critique of the interaction.
Mental status examination: modelled from NSW HEALTH documents
The following are the key components and findings which were observed and documented with
respect to the Mental State Examination (MSE) of the interviewed client (NSW Government, 2019):
APPEARANCE: From the interview, the client’s appearance can be presumed to well-groomed with
no signs of any dishevelment. However, with regards to the eye contact, a number of instances
would be observed where the client seemed distracted from his surroundings with greater emphasis
on turning behind towards the ‘voice’, rather than maintaining eye contact with the mental health
professional. However, the client was also observed to be cooperative and demonstrated eagerness
to answer all questions asked by the mental health professional.
BEHAVIOUR: While the client did not demonstrate any form of overactivity or restlessness and
seemed calmed when interacting with the mental health professional. However, several instances
were recorded where the client seemed to distracted himself from his surroundings and begin
talking to himself. This was in response to the ‘voices’ who the client claimed to keep critiquing him
when enquired by the mental health professional. The client also did not demonstrate any
overactive or retarded motor activity but was seemingly found to be agitated when he heard voices,
as evident from his distracted gaze and elevated tone of voice.
AFFECT: From the interview it can be observed that the client’s emotional response seemed to be
restricted and flattened to some extent as observed in several instances where he seemed to lose
track of the question or took time to remember the date. There were however bouts of reactivity
when the client was observed to talk to himself in response to hearing his auditory hallucinations.
MOOD: The client’s mood was found to be mildly depressed as observed from his responses that the
auditory hallucinations have been criticising his capabilities. From the client’s own perceptions, it can
be observed that feelings and emotions of depression and agitation are of significant intensity,
duration and fluctuations as observed from his responses that he had been experiencing these
hallucinations several times in the past and also during sleeping.
SPEECH: The client’s speech demonstrated low tone, quantity and volume and a monotonous
without any form of variation and with long pauses before answering any questions. However,
several instances of erratic speech were observed in the form of the client raising his tone, volume
and rate of speech during every period when he claimed to experience auditory hallucinations.
Several instances of distracted demeanour coupled with long drawn pauses and short periods of
poverty of speech were some of unusual characteristics observed.
THOUGHT FORM: Based on the client’s responses in the view, his thoughts seemed to be logical and
concrete and was comprehendible with significant associations, congruent associations between
each responses. However, instances of vague thoughts were demonstrated in instances when the
client unpredictable overlooked the health professional and sought to respond to the ‘voices’ or the
auditory hallucinations which he was experiencing. Despite the prevalence of logical and congruent
responses, each response of the client were preceded by a brief period of poverty of speech where
he felt distracted and lost insight of the questions.
THOUGHT CONTENT: From the interview it can be observed that the client’s thoughts are easily
understandable and coherent, as he shared his recent vacation and his prospects of writing a novel.
However, it can be observed that the client has recently been experiencing auditory hallucinations in
the form of ‘voices’ which have resurfaced as a result of absence of medication. While the client did
not demonstrate any form of anti-social urges there was an instance where the client claimed his
The following are the key components and findings which were observed and documented with
respect to the Mental State Examination (MSE) of the interviewed client (NSW Government, 2019):
APPEARANCE: From the interview, the client’s appearance can be presumed to well-groomed with
no signs of any dishevelment. However, with regards to the eye contact, a number of instances
would be observed where the client seemed distracted from his surroundings with greater emphasis
on turning behind towards the ‘voice’, rather than maintaining eye contact with the mental health
professional. However, the client was also observed to be cooperative and demonstrated eagerness
to answer all questions asked by the mental health professional.
BEHAVIOUR: While the client did not demonstrate any form of overactivity or restlessness and
seemed calmed when interacting with the mental health professional. However, several instances
were recorded where the client seemed to distracted himself from his surroundings and begin
talking to himself. This was in response to the ‘voices’ who the client claimed to keep critiquing him
when enquired by the mental health professional. The client also did not demonstrate any
overactive or retarded motor activity but was seemingly found to be agitated when he heard voices,
as evident from his distracted gaze and elevated tone of voice.
AFFECT: From the interview it can be observed that the client’s emotional response seemed to be
restricted and flattened to some extent as observed in several instances where he seemed to lose
track of the question or took time to remember the date. There were however bouts of reactivity
when the client was observed to talk to himself in response to hearing his auditory hallucinations.
MOOD: The client’s mood was found to be mildly depressed as observed from his responses that the
auditory hallucinations have been criticising his capabilities. From the client’s own perceptions, it can
be observed that feelings and emotions of depression and agitation are of significant intensity,
duration and fluctuations as observed from his responses that he had been experiencing these
hallucinations several times in the past and also during sleeping.
SPEECH: The client’s speech demonstrated low tone, quantity and volume and a monotonous
without any form of variation and with long pauses before answering any questions. However,
several instances of erratic speech were observed in the form of the client raising his tone, volume
and rate of speech during every period when he claimed to experience auditory hallucinations.
Several instances of distracted demeanour coupled with long drawn pauses and short periods of
poverty of speech were some of unusual characteristics observed.
THOUGHT FORM: Based on the client’s responses in the view, his thoughts seemed to be logical and
concrete and was comprehendible with significant associations, congruent associations between
each responses. However, instances of vague thoughts were demonstrated in instances when the
client unpredictable overlooked the health professional and sought to respond to the ‘voices’ or the
auditory hallucinations which he was experiencing. Despite the prevalence of logical and congruent
responses, each response of the client were preceded by a brief period of poverty of speech where
he felt distracted and lost insight of the questions.
THOUGHT CONTENT: From the interview it can be observed that the client’s thoughts are easily
understandable and coherent, as he shared his recent vacation and his prospects of writing a novel.
However, it can be observed that the client has recently been experiencing auditory hallucinations in
the form of ‘voices’ which have resurfaced as a result of absence of medication. While the client did
not demonstrate any form of anti-social urges there was an instance where the client claimed his
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ability to defend himself since anyone can harm him. Additionally, the client demonstrated several
instances of rebuking or responding to the voices which were ‘critical’ of him, thus raising concerns
of possible delusions of paranoia or feelings of lack of self-esteem.
PERCEPTION: From the interview, it was evident that the client is currently experiencing several
instances of auditory hallucinations especially in response to withdrawal of the medication
Olanzapine. This was experienced by the client in the form of ‘voices’ which claimed to severely
critique him, as observed in the clients responses during instances where he shared regarding his
ability to finish the novel, his prospects as a writer, his current circle of friends and his skills of
arithmetic.
COGNITION & INTELLECTUAL FUNCTIONING: In terms of orientation, the client was seemingly
distracted as observed in his inability to recall the question being asked to him. The client was
however well oriented in terms of his memory and present experiences as observed from his ability
to recall his recent vacation, his friend circle, his presence in the mental health settings and his
ability to plan the writing of his novel. The client’s concentration was however disrupted during
several instances as he responded to his hallucinations. However, his ability to calculate and engage
in abstract reasoning was delayed but commendable as observed in his calculations as well his claims
that he may be harmed by the mental health professional, the need to be hospitalised and wish to
not worry his mother regarding his illness.
INSIGHT & JUDGEMENT: The client demonstrated commendable levels of insight with regards to his
problem, as observed in his acceptance that he required help, was in need of medications and may
require hospitalisation. The client’s judgement seemed slightly impaired as observed in erratic
responses where at one time he expressed his ability to write the novel and defend himself and at
another time responding to the voices regarding completion of his novel, self-critiquing his math
skills and claiming that even the healthcare professional may harm him.
(15 marks)
Identify 4 risks (5 marks). Refer to risk template for various types of risks.
From the above observations recorded in the MSE, the concerned client may be at risk of the
following:
From the interview it can be implied that the client is at risk of acquiring severe depressive
symptoms due to auditory hallucinations. It has been evidenced that prolonged
preoccupation with auditory hallucinations are likely to increase the risk of symptoms of
depression in the concerned individual, such as: impaired levels of concentration, loss of
self-esteem and associated slowing with regards to activity and thought process. Indeed, the
client indeed demonstrated the several instances of distraction, low mood, excessive self-
criticism and decreased sense of self-esteem (Chiang et al., 2018).
The client is likely at risk of suicide and feelings of suicide ideation. It has been evidenced
that individuals with auditory hallucinations as well as symptoms of depression are at risk of
experiencing low levels of self-esteem, optimism and self-worth, which in turn, can increase
their risk of suicide (Slotema et al., 2017).
The client is likely to be at risk of engaging in violent behaviour and harm others, as evident
from the claims that the voices are critical of him along with the client’s statement that he
can defend himself since there is a possibility that the mental healthcare professional can
harm him. It has been evidenced that individuals with auditory hallucinations are at risk of
instances of rebuking or responding to the voices which were ‘critical’ of him, thus raising concerns
of possible delusions of paranoia or feelings of lack of self-esteem.
PERCEPTION: From the interview, it was evident that the client is currently experiencing several
instances of auditory hallucinations especially in response to withdrawal of the medication
Olanzapine. This was experienced by the client in the form of ‘voices’ which claimed to severely
critique him, as observed in the clients responses during instances where he shared regarding his
ability to finish the novel, his prospects as a writer, his current circle of friends and his skills of
arithmetic.
COGNITION & INTELLECTUAL FUNCTIONING: In terms of orientation, the client was seemingly
distracted as observed in his inability to recall the question being asked to him. The client was
however well oriented in terms of his memory and present experiences as observed from his ability
to recall his recent vacation, his friend circle, his presence in the mental health settings and his
ability to plan the writing of his novel. The client’s concentration was however disrupted during
several instances as he responded to his hallucinations. However, his ability to calculate and engage
in abstract reasoning was delayed but commendable as observed in his calculations as well his claims
that he may be harmed by the mental health professional, the need to be hospitalised and wish to
not worry his mother regarding his illness.
INSIGHT & JUDGEMENT: The client demonstrated commendable levels of insight with regards to his
problem, as observed in his acceptance that he required help, was in need of medications and may
require hospitalisation. The client’s judgement seemed slightly impaired as observed in erratic
responses where at one time he expressed his ability to write the novel and defend himself and at
another time responding to the voices regarding completion of his novel, self-critiquing his math
skills and claiming that even the healthcare professional may harm him.
(15 marks)
Identify 4 risks (5 marks). Refer to risk template for various types of risks.
From the above observations recorded in the MSE, the concerned client may be at risk of the
following:
From the interview it can be implied that the client is at risk of acquiring severe depressive
symptoms due to auditory hallucinations. It has been evidenced that prolonged
preoccupation with auditory hallucinations are likely to increase the risk of symptoms of
depression in the concerned individual, such as: impaired levels of concentration, loss of
self-esteem and associated slowing with regards to activity and thought process. Indeed, the
client indeed demonstrated the several instances of distraction, low mood, excessive self-
criticism and decreased sense of self-esteem (Chiang et al., 2018).
The client is likely at risk of suicide and feelings of suicide ideation. It has been evidenced
that individuals with auditory hallucinations as well as symptoms of depression are at risk of
experiencing low levels of self-esteem, optimism and self-worth, which in turn, can increase
their risk of suicide (Slotema et al., 2017).
The client is likely to be at risk of engaging in violent behaviour and harm others, as evident
from the claims that the voices are critical of him along with the client’s statement that he
can defend himself since there is a possibility that the mental healthcare professional can
harm him. It has been evidenced that individuals with auditory hallucinations are at risk of
acquiring delusions of mistrust and paranoia, which in turn can increase the risk of harming
and being violent towards others (Ullrich et al., 2018).
The client is likely at risk of harming and inflicting injuries upon himself. It has been
evidenced that individuals with auditory hallucinations due to their possible risk of mistrust
and delusions of paranoia are likely to be self-critical and as a result harm themselves
(Dugré, Guay & Dumais, 2018).
Care plan: Modelled on clinical modules information NSW HEALTH
(20 marks)
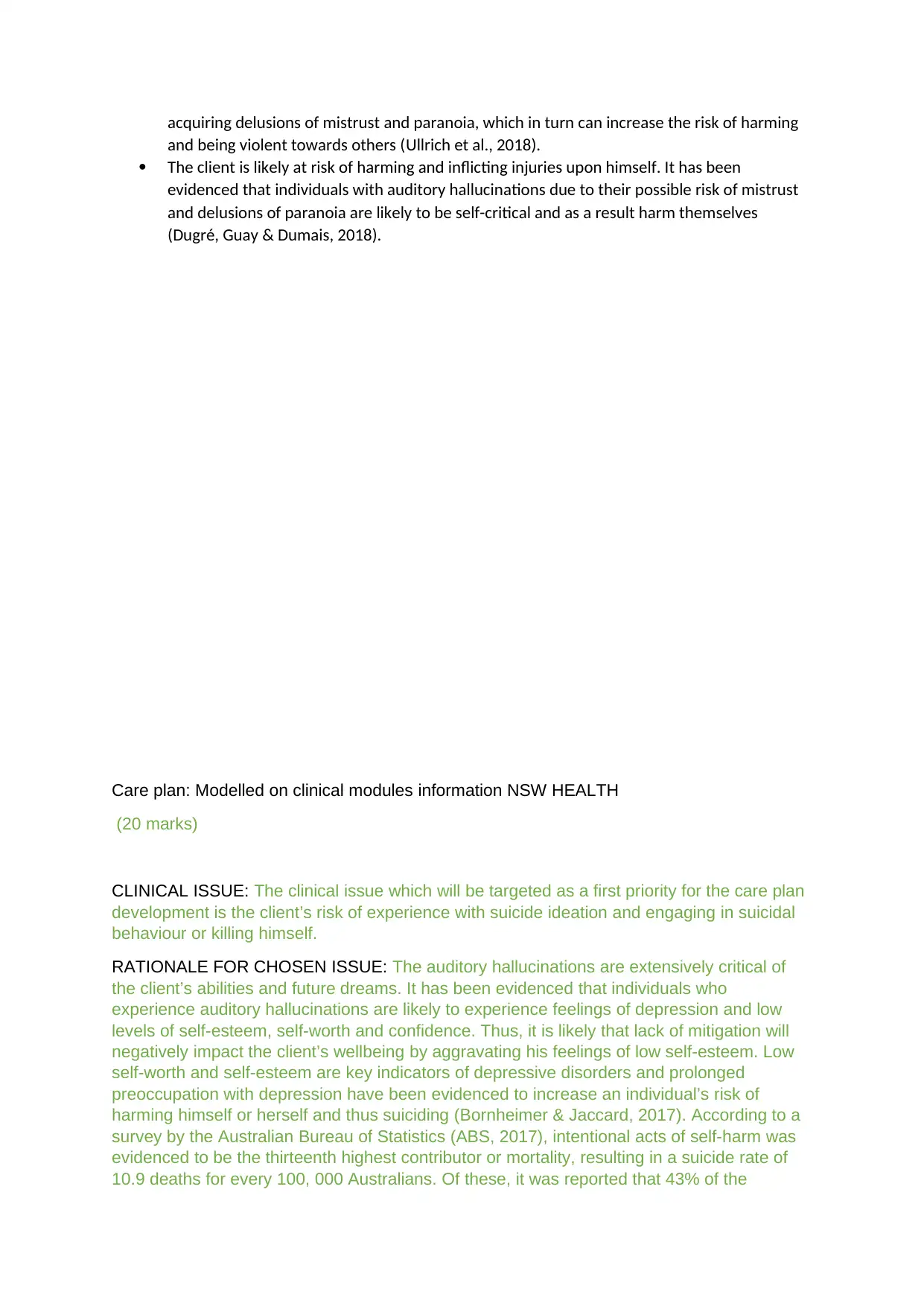
CLINICAL ISSUE: The clinical issue which will be targeted as a first priority for the care plan
development is the client’s risk of experience with suicide ideation and engaging in suicidal
behaviour or killing himself.
RATIONALE FOR CHOSEN ISSUE: The auditory hallucinations are extensively critical of
the client’s abilities and future dreams. It has been evidenced that individuals who
experience auditory hallucinations are likely to experience feelings of depression and low
levels of self-esteem, self-worth and confidence. Thus, it is likely that lack of mitigation will
negatively impact the client’s wellbeing by aggravating his feelings of low self-esteem. Low
self-worth and self-esteem are key indicators of depressive disorders and prolonged
preoccupation with depression have been evidenced to increase an individual’s risk of
harming himself or herself and thus suiciding (Bornheimer & Jaccard, 2017). According to a
survey by the Australian Bureau of Statistics (ABS, 2017), intentional acts of self-harm was
evidenced to be the thirteenth highest contributor or mortality, resulting in a suicide rate of
10.9 deaths for every 100, 000 Australians. Of these, it was reported that 43% of the
and being violent towards others (Ullrich et al., 2018).
The client is likely at risk of harming and inflicting injuries upon himself. It has been
evidenced that individuals with auditory hallucinations due to their possible risk of mistrust
and delusions of paranoia are likely to be self-critical and as a result harm themselves
(Dugré, Guay & Dumais, 2018).
Care plan: Modelled on clinical modules information NSW HEALTH
(20 marks)
CLINICAL ISSUE: The clinical issue which will be targeted as a first priority for the care plan
development is the client’s risk of experience with suicide ideation and engaging in suicidal
behaviour or killing himself.
RATIONALE FOR CHOSEN ISSUE: The auditory hallucinations are extensively critical of
the client’s abilities and future dreams. It has been evidenced that individuals who
experience auditory hallucinations are likely to experience feelings of depression and low
levels of self-esteem, self-worth and confidence. Thus, it is likely that lack of mitigation will
negatively impact the client’s wellbeing by aggravating his feelings of low self-esteem. Low
self-worth and self-esteem are key indicators of depressive disorders and prolonged
preoccupation with depression have been evidenced to increase an individual’s risk of
harming himself or herself and thus suiciding (Bornheimer & Jaccard, 2017). According to a
survey by the Australian Bureau of Statistics (ABS, 2017), intentional acts of self-harm was
evidenced to be the thirteenth highest contributor or mortality, resulting in a suicide rate of
10.9 deaths for every 100, 000 Australians. Of these, it was reported that 43% of the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
individual were already inflicted with depression. There is thus a need to address the issue
of suicide in the client on a priority basis.
GOAL/S: The goal of the care plant is to achieve a positive health outcomes in the client, in
the form of reducing the risk of self-harm and suicide ideation, reduced engagement in
negative self-perception and an increased sense of self-esteem.
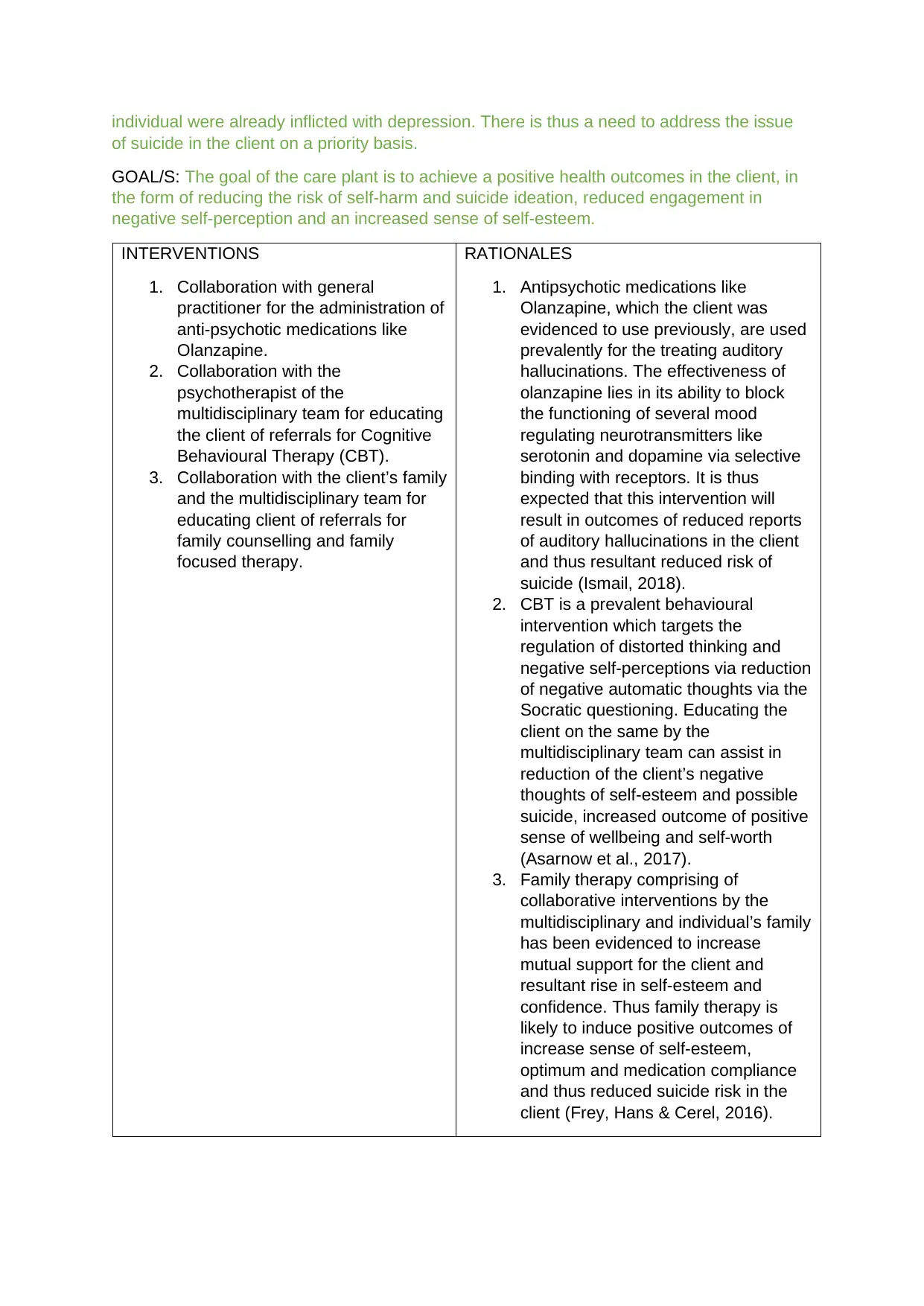
INTERVENTIONS
1. Collaboration with general
practitioner for the administration of
anti-psychotic medications like
Olanzapine.
2. Collaboration with the
psychotherapist of the
multidisciplinary team for educating
the client of referrals for Cognitive
Behavioural Therapy (CBT).
3. Collaboration with the client’s family
and the multidisciplinary team for
educating client of referrals for
family counselling and family
focused therapy.
RATIONALES
1. Antipsychotic medications like
Olanzapine, which the client was
evidenced to use previously, are used
prevalently for the treating auditory
hallucinations. The effectiveness of
olanzapine lies in its ability to block
the functioning of several mood
regulating neurotransmitters like
serotonin and dopamine via selective
binding with receptors. It is thus
expected that this intervention will
result in outcomes of reduced reports
of auditory hallucinations in the client
and thus resultant reduced risk of
suicide (Ismail, 2018).
2. CBT is a prevalent behavioural
intervention which targets the
regulation of distorted thinking and
negative self-perceptions via reduction
of negative automatic thoughts via the
Socratic questioning. Educating the
client on the same by the
multidisciplinary team can assist in
reduction of the client’s negative
thoughts of self-esteem and possible
suicide, increased outcome of positive
sense of wellbeing and self-worth
(Asarnow et al., 2017).
3. Family therapy comprising of
collaborative interventions by the
multidisciplinary and individual’s family
has been evidenced to increase
mutual support for the client and
resultant rise in self-esteem and
confidence. Thus family therapy is
likely to induce positive outcomes of
increase sense of self-esteem,
optimum and medication compliance
and thus reduced suicide risk in the
client (Frey, Hans & Cerel, 2016).
of suicide in the client on a priority basis.
GOAL/S: The goal of the care plant is to achieve a positive health outcomes in the client, in
the form of reducing the risk of self-harm and suicide ideation, reduced engagement in
negative self-perception and an increased sense of self-esteem.
INTERVENTIONS
1. Collaboration with general
practitioner for the administration of
anti-psychotic medications like
Olanzapine.
2. Collaboration with the
psychotherapist of the
multidisciplinary team for educating
the client of referrals for Cognitive
Behavioural Therapy (CBT).
3. Collaboration with the client’s family
and the multidisciplinary team for
educating client of referrals for
family counselling and family
focused therapy.
RATIONALES
1. Antipsychotic medications like
Olanzapine, which the client was
evidenced to use previously, are used
prevalently for the treating auditory
hallucinations. The effectiveness of
olanzapine lies in its ability to block
the functioning of several mood
regulating neurotransmitters like
serotonin and dopamine via selective
binding with receptors. It is thus
expected that this intervention will
result in outcomes of reduced reports
of auditory hallucinations in the client
and thus resultant reduced risk of
suicide (Ismail, 2018).
2. CBT is a prevalent behavioural
intervention which targets the
regulation of distorted thinking and
negative self-perceptions via reduction
of negative automatic thoughts via the
Socratic questioning. Educating the
client on the same by the
multidisciplinary team can assist in
reduction of the client’s negative
thoughts of self-esteem and possible
suicide, increased outcome of positive
sense of wellbeing and self-worth
(Asarnow et al., 2017).
3. Family therapy comprising of
collaborative interventions by the
multidisciplinary and individual’s family
has been evidenced to increase
mutual support for the client and
resultant rise in self-esteem and
confidence. Thus family therapy is
likely to induce positive outcomes of
increase sense of self-esteem,
optimum and medication compliance
and thus reduced suicide risk in the
client (Frey, Hans & Cerel, 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACTIVITY 3
The following were the four positive interactions which were observed during the interview:
1. It was observed that the interviewer engaged in patient and active listening, as
observed in the moments of silence she engaged when the client took a lot of time to
respond as well as actively engaging in listening to the client as he continued to
demonstrate his slowed speech, distractions and response to the voices which he
was hearing. It has been evidenced that skills of interpersonal communication such
as patience and active listening facilitate positive therapeutic relationships with the
client. This is because active listening from the interviewer, paves the way for
positive perceptions where the client will feel that his or her concerns are being
listened to with concern, which in turn will contribute to development of positive
rapport (Moosvi & Garbutt, 2020).
2. The interviewer engaged in empathy – the act of placing oneself in someone else’s
condition. It was observed that the interviewer empathized with the client regarding
how distressing the hallucinations may be. Empathy enhances interviewee-
interviewer interaction since it makes the client feel that his or her thoughts are valid
and are of importance to others as well (Outlaw & Rushing, 2018).
3. The third positive aspect of the interaction was the interviewer obtaining consent from
the client before proceeding, as was observed in her enquiry regarding whether the
client was comfortable with hospitalization and that his information may be shared
within the multidisciplinary team. Obtaining informed consent demonstrates ethical
compliance to autonomy and patient centeredness. It additionally enhances client
compliance since the client is likely feel that he or she is being dignified and
respected as a person (Kilpatrick, Elliott & Fry, 2019).
4. The interviewer used of open ended questioning to the client. This was observed in
the form of the interviewer asking subjective questions such as those related to the
client’s current experiences, mood and connections with family. Engaging in open
ended questioning as compared to close ended questioning is useful for positive
therapeutic communication since it encourages the client to share his or her
experiences in detail, which otherwise may not be possible to cover by restrictive,
close ended questions (Maame Kissiwaa Amoah et al., 2018).
The following two negative aspects were observed in the interaction:
1. The interviewer was observed to engage in a form of non-verbal communication, by
shaking hands with the client. While such gestures are demonstrative of the positive
rapport and sense of compassion and affection, gestures like handshakes may not
always be perceived well by individuals. Without appropriate consent, individuals
may perceive contact gestures as signs of impoliteness and rudeness (Green et al.,
2020).
2. The second negative aspect was absence on elaboration and education by the
interviewer to the interviewee on the rationale behind the interventions
The following were the four positive interactions which were observed during the interview:
1. It was observed that the interviewer engaged in patient and active listening, as
observed in the moments of silence she engaged when the client took a lot of time to
respond as well as actively engaging in listening to the client as he continued to
demonstrate his slowed speech, distractions and response to the voices which he
was hearing. It has been evidenced that skills of interpersonal communication such
as patience and active listening facilitate positive therapeutic relationships with the
client. This is because active listening from the interviewer, paves the way for
positive perceptions where the client will feel that his or her concerns are being
listened to with concern, which in turn will contribute to development of positive
rapport (Moosvi & Garbutt, 2020).
2. The interviewer engaged in empathy – the act of placing oneself in someone else’s
condition. It was observed that the interviewer empathized with the client regarding
how distressing the hallucinations may be. Empathy enhances interviewee-
interviewer interaction since it makes the client feel that his or her thoughts are valid
and are of importance to others as well (Outlaw & Rushing, 2018).
3. The third positive aspect of the interaction was the interviewer obtaining consent from
the client before proceeding, as was observed in her enquiry regarding whether the
client was comfortable with hospitalization and that his information may be shared
within the multidisciplinary team. Obtaining informed consent demonstrates ethical
compliance to autonomy and patient centeredness. It additionally enhances client
compliance since the client is likely feel that he or she is being dignified and
respected as a person (Kilpatrick, Elliott & Fry, 2019).
4. The interviewer used of open ended questioning to the client. This was observed in
the form of the interviewer asking subjective questions such as those related to the
client’s current experiences, mood and connections with family. Engaging in open
ended questioning as compared to close ended questioning is useful for positive
therapeutic communication since it encourages the client to share his or her
experiences in detail, which otherwise may not be possible to cover by restrictive,
close ended questions (Maame Kissiwaa Amoah et al., 2018).
The following two negative aspects were observed in the interaction:
1. The interviewer was observed to engage in a form of non-verbal communication, by
shaking hands with the client. While such gestures are demonstrative of the positive
rapport and sense of compassion and affection, gestures like handshakes may not
always be perceived well by individuals. Without appropriate consent, individuals
may perceive contact gestures as signs of impoliteness and rudeness (Green et al.,
2020).
2. The second negative aspect was absence on elaboration and education by the
interviewer to the interviewee on the rationale behind the interventions

recommended. This is because lack of adequate health literacy is one of the
strongest causes of non-compliance by clients towards treatment (Penneçot et al.,
2020).
strongest causes of non-compliance by clients towards treatment (Penneçot et al.,
2020).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References and academic writing (5 marks).
ABS. (2017). 3303.0 - Causes of Death, Australia, 2017. Retrieved 18 March 2020, from
https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/3303.0~2017~Main
%20Features~Intentional%20self-harm,%20key%20characteristics~3.
Asarnow, J. R., Hughes, J. L., Babeva, K. N., & Sugar, C. A. (2017). Cognitive-behavioral family
treatment for suicide attempt prevention: a randomized controlled trial. Journal of the
American Academy of Child & Adolescent Psychiatry, 56(6), 506-514.
Bornheimer, L. A., & Jaccard, J. (2017). Symptoms of depression, positive symptoms of psychosis,
and suicidal ideation among adults diagnosed with schizophrenia within the clinical
antipsychotic trials of intervention effectiveness. Archives of Suicide Research, 21(4), 633-
645.
Chiang, Y. H., Beckstead, J. W., Lo, S. C., & Yang, C. Y. (2018). Association of auditory hallucination
and anxiety symptoms with depressive symptoms in patients with schizophrenia: a three-
month follow-up. Archives of psychiatric nursing, 32(4), 585-590.
Dugré, J. R., Guay, J. P., & Dumais, A. (2018). Risk factors of compliance with self-harm command
hallucinations in individuals with affective and non-affective psychosis. Schizophrenia
research, 195, 115-121.
Frey, L. M., Hans, J. D., & Cerel, J. (2016). Suicide disclosure in suicide attempt survivors: Does family
reaction moderate or mediate disclosure's effect on depression?. Suicide and Life
‐
Threatening Behavior, 46(1), 96-105.
Green, C., Vandall-Walker, V., Rysdale, L., Stevens, M., Feldmann, H., Tymura, S., & Stojkovic, K.
(2020). You Can’t Touch… or Can You? Dietitians’ Perceptions of Expressive Touch in Client
Encounters. Canadian Journal of Dietetic Practice and Research, 81, 1-8.
Ismail, M. F. (2018). A Rare Case of Alcohol-Induced Psychotic Disorder (Alcoholic Hallucinosis)
Responding to Olanzapine. Malaysian Journal of Psychiatry, 27(2), 35-37.
Kilpatrick, J., Elliott, R., & Fry, M. (2019). Health professionals’ understanding of person-centred
communication for risk prevention conversations: an exploratory study. Contemporary
nurse, 1-12.
Maame Kissiwaa Amoah, V., Anokye, R., Boakye, D. S., & Gyamfi, N. (2018). Perceived barriers to
effective therapeutic communication among nurses and patients at Kumasi South
Hospital. Cogent Medicine, 5(1), 1459341.
Moosvi, K., & Garbutt, S. (2020). Shifting Strategies: Using Film to Improve Therapeutic
Communication and Nursing Education. Nursing education perspectives, 41(2), 134-135.
NSW Government. (2019). Mental Health Clinical Documentation Guidelines. Retrieved 18 March
2020, from https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2014_002.pdf.
Outlaw, K., & Rushing, D. S. (2018). Increasing Empathy in Mental Health Nursing Using Simulation
and Reflective Journaling. Journal of Nursing Education, 57(12), 766-766.
Penneçot, C., Gagnayre, R., Ammirati, C., Bertin, É., Capelle, D., Cheraitia, E., ... & Derambure, P.
(2020). Consensus Recommendations for the Use of Simulation in Therapeutic Patient
Education. Simulation in Healthcare, 15(1), 30-38.
ABS. (2017). 3303.0 - Causes of Death, Australia, 2017. Retrieved 18 March 2020, from
https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/3303.0~2017~Main
%20Features~Intentional%20self-harm,%20key%20characteristics~3.
Asarnow, J. R., Hughes, J. L., Babeva, K. N., & Sugar, C. A. (2017). Cognitive-behavioral family
treatment for suicide attempt prevention: a randomized controlled trial. Journal of the
American Academy of Child & Adolescent Psychiatry, 56(6), 506-514.
Bornheimer, L. A., & Jaccard, J. (2017). Symptoms of depression, positive symptoms of psychosis,
and suicidal ideation among adults diagnosed with schizophrenia within the clinical
antipsychotic trials of intervention effectiveness. Archives of Suicide Research, 21(4), 633-
645.
Chiang, Y. H., Beckstead, J. W., Lo, S. C., & Yang, C. Y. (2018). Association of auditory hallucination
and anxiety symptoms with depressive symptoms in patients with schizophrenia: a three-
month follow-up. Archives of psychiatric nursing, 32(4), 585-590.
Dugré, J. R., Guay, J. P., & Dumais, A. (2018). Risk factors of compliance with self-harm command
hallucinations in individuals with affective and non-affective psychosis. Schizophrenia
research, 195, 115-121.
Frey, L. M., Hans, J. D., & Cerel, J. (2016). Suicide disclosure in suicide attempt survivors: Does family
reaction moderate or mediate disclosure's effect on depression?. Suicide and Life
‐
Threatening Behavior, 46(1), 96-105.
Green, C., Vandall-Walker, V., Rysdale, L., Stevens, M., Feldmann, H., Tymura, S., & Stojkovic, K.
(2020). You Can’t Touch… or Can You? Dietitians’ Perceptions of Expressive Touch in Client
Encounters. Canadian Journal of Dietetic Practice and Research, 81, 1-8.
Ismail, M. F. (2018). A Rare Case of Alcohol-Induced Psychotic Disorder (Alcoholic Hallucinosis)
Responding to Olanzapine. Malaysian Journal of Psychiatry, 27(2), 35-37.
Kilpatrick, J., Elliott, R., & Fry, M. (2019). Health professionals’ understanding of person-centred
communication for risk prevention conversations: an exploratory study. Contemporary
nurse, 1-12.
Maame Kissiwaa Amoah, V., Anokye, R., Boakye, D. S., & Gyamfi, N. (2018). Perceived barriers to
effective therapeutic communication among nurses and patients at Kumasi South
Hospital. Cogent Medicine, 5(1), 1459341.
Moosvi, K., & Garbutt, S. (2020). Shifting Strategies: Using Film to Improve Therapeutic
Communication and Nursing Education. Nursing education perspectives, 41(2), 134-135.
NSW Government. (2019). Mental Health Clinical Documentation Guidelines. Retrieved 18 March
2020, from https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2014_002.pdf.
Outlaw, K., & Rushing, D. S. (2018). Increasing Empathy in Mental Health Nursing Using Simulation
and Reflective Journaling. Journal of Nursing Education, 57(12), 766-766.
Penneçot, C., Gagnayre, R., Ammirati, C., Bertin, É., Capelle, D., Cheraitia, E., ... & Derambure, P.
(2020). Consensus Recommendations for the Use of Simulation in Therapeutic Patient
Education. Simulation in Healthcare, 15(1), 30-38.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Slotema, C. W., Niemantsverdriet, M. B. A., Blom, J. D., van der Gaag, M., Hoek, H. W., & Sommer, I.
E. C. (2017). Suicidality and hospitalisation in patients with borderline personality disorder
who experience auditory verbal hallucinations. European psychiatry, 41, 47-52.
Ullrich, S., Keers, R., Shaw, J., Doyle, M., & Coid, J. W. (2018). Acting on delusions: the role of
negative affect in the pathway towards serious violence. The Journal of Forensic Psychiatry &
Psychology, 29(5), 691-704.
E. C. (2017). Suicidality and hospitalisation in patients with borderline personality disorder
who experience auditory verbal hallucinations. European psychiatry, 41, 47-52.
Ullrich, S., Keers, R., Shaw, J., Doyle, M., & Coid, J. W. (2018). Acting on delusions: the role of
negative affect in the pathway towards serious violence. The Journal of Forensic Psychiatry &
Psychology, 29(5), 691-704.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





