Comprehensive Report: Middle East Respiratory Syndrome (MERS) Overview
VerifiedAdded on 2020/05/04
|20
|5243
|67
Report
AI Summary
This report provides a comprehensive overview of Middle East Respiratory Syndrome (MERS), a respiratory illness originating in Saudi Arabia. It delves into the epidemiology of MERS, including transmission routes, risk factors, and clinical features, highlighting the role of the MERS coronavirus (MERS-CoV). The report discusses the interaction between the causative agent, host, and environmental factors in the development and spread of the condition, with a focus on the zoonotic transmission from dromedary camels. The report also examines the human-to-human transmission, especially in healthcare settings. It further explores the risk factors, including age, underlying health conditions, and healthcare worker exposure. The report concludes by discussing potential policy responses to control the spread of the virus and mitigate its impact on public health. The report also highlights the global impact of the disease, including outbreaks in countries outside the Middle East. The analysis underscores the importance of understanding MERS to develop effective prevention and control strategies.

Running head: MIDDLE EAST RESPIRATORY SYNDROME
MIDDLE EAST RESPIRATORY SYNDROME (MERS)
Name
Institution
MIDDLE EAST RESPIRATORY SYNDROME (MERS)
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MIDDLE EAST RESPIRATORY SYNDROME
Middle East Respiratory Syndrome (MERS)
Introduction
Middle East Respiratory Syndrome (MERS) is a respiratory syndrome that can be traced
back to Saudi Arabia in 2012. It was initially restricted to persons who were traveling within the
Middle East and/or their contacts, but later had a spill-over effect into other countries as
demonstrated by outbreaks in countries out of the Middle East block such as the Republic of
Korea (RoK), Austria, the Philippines, Thailand, France, Tunisia, Germany, Malaysia, Greece
and the United Kingdom (World Health Organization (WHO), 2017; NSW Government, 2017).
MERS is caused by Middle Eastern respiratory syndrome coronavirus (MERS-CoV). MERS is
not a national notifiable in Australia, but it is at least classified as a notifiable condition in some
parts of Australia, precisely South and Western Australia (Government of South Australia - SA
Health, n.d.) and the US (Centers for Disease Control and Prevention (CDC), 2015).
This paper is a discussion on MERS with focus on the role of agent, host and
environmental factors in the development and spread of the condition and the corresponding
potential policy responses to the same. This is achieved through discussions on three main
sections. The first section discusses the epidemiology, transmission routes, risk factors and
clinical features, while the second part is a discussion on the interaction between the causative
agent, host and environmental factors in the production of the illness in individuals, and the last
part discusses various responses towards the control of the spread of the virus.
Middle East Respiratory Syndrome (MERS)
Introduction
Middle East Respiratory Syndrome (MERS) is a respiratory syndrome that can be traced
back to Saudi Arabia in 2012. It was initially restricted to persons who were traveling within the
Middle East and/or their contacts, but later had a spill-over effect into other countries as
demonstrated by outbreaks in countries out of the Middle East block such as the Republic of
Korea (RoK), Austria, the Philippines, Thailand, France, Tunisia, Germany, Malaysia, Greece
and the United Kingdom (World Health Organization (WHO), 2017; NSW Government, 2017).
MERS is caused by Middle Eastern respiratory syndrome coronavirus (MERS-CoV). MERS is
not a national notifiable in Australia, but it is at least classified as a notifiable condition in some
parts of Australia, precisely South and Western Australia (Government of South Australia - SA
Health, n.d.) and the US (Centers for Disease Control and Prevention (CDC), 2015).
This paper is a discussion on MERS with focus on the role of agent, host and
environmental factors in the development and spread of the condition and the corresponding
potential policy responses to the same. This is achieved through discussions on three main
sections. The first section discusses the epidemiology, transmission routes, risk factors and
clinical features, while the second part is a discussion on the interaction between the causative
agent, host and environmental factors in the production of the illness in individuals, and the last
part discusses various responses towards the control of the spread of the virus.
MIDDLE EAST RESPIRATORY SYNDROME
Discussion
Epidemiology, Transmission Routes, Risk Factors and Clinical Features
Epidemiology
The MERS coronavirus belongs to the large and diverse family of coronaviruses which
are known to cause ill health to both humans and animals. Four strains of coronaviruses that
affect humans {human coronaviruses (hCoV)} are known to cause respiratory infections in
human, with severity ranging from mild to moderate. These hCoVs include the alpha-
coronaviruses hCoV-NL63 and hCoV-229E and betacoronaviruses hCoV-HKU and hCoV-OC43
(The Department of Health, 2014). In the class of beta-coronaviruses also lies the viruses causing
MERS-CoV and severe acute respiratory syndrome coronavirus (SARS-CoV). However,
according to The Australian Department of Health, these two viruses are genetically distinct
from each other (The Department of Health, 2014). The MERS coronavirus was only identified
in 2012 as a new variant of the coronavirus family that could lead to a rapid onset of severe
respiratory illness in humans (Zaki, van Boheemen, Bestebroer, Osterhaus, & Fouchier, 2012).
Most of MERS cases have been found to develop in persons presenting with other underlying
conditions which predispose them to respiratory infections. While MERS-CoV is distinct from
the SARS-CoV in humans, the MERS-CoV has some similarity to coronaviruses found in bats
(The Department of Health, 2014).
Up to date, all cases of MERS in humans have been in persons who have been residents
in or travellers to the countries in the Middle East or have had a close contact with persons
presenting with the infection in the same region. The disease has been predominantly reported in
in travellers or residents in the United Arab Emirates (UAE), Jordan, Qatar and the Kingdom of
Discussion
Epidemiology, Transmission Routes, Risk Factors and Clinical Features
Epidemiology
The MERS coronavirus belongs to the large and diverse family of coronaviruses which
are known to cause ill health to both humans and animals. Four strains of coronaviruses that
affect humans {human coronaviruses (hCoV)} are known to cause respiratory infections in
human, with severity ranging from mild to moderate. These hCoVs include the alpha-
coronaviruses hCoV-NL63 and hCoV-229E and betacoronaviruses hCoV-HKU and hCoV-OC43
(The Department of Health, 2014). In the class of beta-coronaviruses also lies the viruses causing
MERS-CoV and severe acute respiratory syndrome coronavirus (SARS-CoV). However,
according to The Australian Department of Health, these two viruses are genetically distinct
from each other (The Department of Health, 2014). The MERS coronavirus was only identified
in 2012 as a new variant of the coronavirus family that could lead to a rapid onset of severe
respiratory illness in humans (Zaki, van Boheemen, Bestebroer, Osterhaus, & Fouchier, 2012).
Most of MERS cases have been found to develop in persons presenting with other underlying
conditions which predispose them to respiratory infections. While MERS-CoV is distinct from
the SARS-CoV in humans, the MERS-CoV has some similarity to coronaviruses found in bats
(The Department of Health, 2014).
Up to date, all cases of MERS in humans have been in persons who have been residents
in or travellers to the countries in the Middle East or have had a close contact with persons
presenting with the infection in the same region. The disease has been predominantly reported in
in travellers or residents in the United Arab Emirates (UAE), Jordan, Qatar and the Kingdom of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MIDDLE EAST RESPIRATORY SYNDROME
Saudi Arabia (Who Mers-Cov Research Group., 2013). But as demonstrated in later years, the
infection is not just restricted to the Middle East as evidenced by the reported cases in countries,
not in the Middle East. This includes countries in Europe such as Italy, Germany, the United
Kingdom, France, Tunisia, Malaysia, South Korea, the Philippines, Thailand and Greece (NSW
Government, 2017). South Korea reported the largest outbreak in 2015, which was a multi-centre
hospital outbreak which was traced to a traveller from the Middle East (WHO, 2015; CDC,
2015). Notably, Australia has so far reported zero MERS-CoV cases. (NSW Government, 2017).
A MERS situation update by WHO for the months of January and February 2017 states that as of
the beginning of March 2017, a total of 1,916 laboratory confirmed cases of MERS have been
reported to WHO and a total of 702 persons have died, translating to a case-fatality rate of 36.6%
(WHO, 2017). According to the same update, a total of 27 countries worldwide have reported
MERS cases.
Transmission routes
The epidemiologic aspects of the MERS-CoV have not been adequately defined, but the
most recognized means of transmission is the human-to-human transmission of the virus, in
healthcare settings. However, just like other coronaviruses, the spread of the virus is thought to
occur through contact with an infected individual’s secretions. The exposure in healthcare
facilities could be justified by the 2015 outbreak in South Korea and Saudi Arabia, whose point
of introduction is always a single introduction of MERS, probably zoonotic (Al-Abdallat, et al.,
2014). According to the WHO, MERS-CoV is a zoonotic virus which enters the sphere of
humans through contact with infected dromedary camels in the Middle East (WHO, 2016). The
restriction that it is dromedary camels in the Arabian Peninsula can be supported by negative
findings of the virus in tested camels from other parts of the world (Chan, et al., 2015).
Saudi Arabia (Who Mers-Cov Research Group., 2013). But as demonstrated in later years, the
infection is not just restricted to the Middle East as evidenced by the reported cases in countries,
not in the Middle East. This includes countries in Europe such as Italy, Germany, the United
Kingdom, France, Tunisia, Malaysia, South Korea, the Philippines, Thailand and Greece (NSW
Government, 2017). South Korea reported the largest outbreak in 2015, which was a multi-centre
hospital outbreak which was traced to a traveller from the Middle East (WHO, 2015; CDC,
2015). Notably, Australia has so far reported zero MERS-CoV cases. (NSW Government, 2017).
A MERS situation update by WHO for the months of January and February 2017 states that as of
the beginning of March 2017, a total of 1,916 laboratory confirmed cases of MERS have been
reported to WHO and a total of 702 persons have died, translating to a case-fatality rate of 36.6%
(WHO, 2017). According to the same update, a total of 27 countries worldwide have reported
MERS cases.
Transmission routes
The epidemiologic aspects of the MERS-CoV have not been adequately defined, but the
most recognized means of transmission is the human-to-human transmission of the virus, in
healthcare settings. However, just like other coronaviruses, the spread of the virus is thought to
occur through contact with an infected individual’s secretions. The exposure in healthcare
facilities could be justified by the 2015 outbreak in South Korea and Saudi Arabia, whose point
of introduction is always a single introduction of MERS, probably zoonotic (Al-Abdallat, et al.,
2014). According to the WHO, MERS-CoV is a zoonotic virus which enters the sphere of
humans through contact with infected dromedary camels in the Middle East (WHO, 2016). The
restriction that it is dromedary camels in the Arabian Peninsula can be supported by negative
findings of the virus in tested camels from other parts of the world (Chan, et al., 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MIDDLE EAST RESPIRATORY SYNDROME
Studies have demonstrated strong indicators of both direct and indirect exposure to
camels to causing the infections. This hypothesis is supported by at least one group in which the
camels also tested seropositive (WHO, 2017). Outstandingly, a review of literature also indicates
cases where the infections resulted even in the absence of a history of prior exposure to other
animals. This perspective rather suggests the likelihood of the virus being introduced through
multiple channels as opposed to a single zoonotic case.
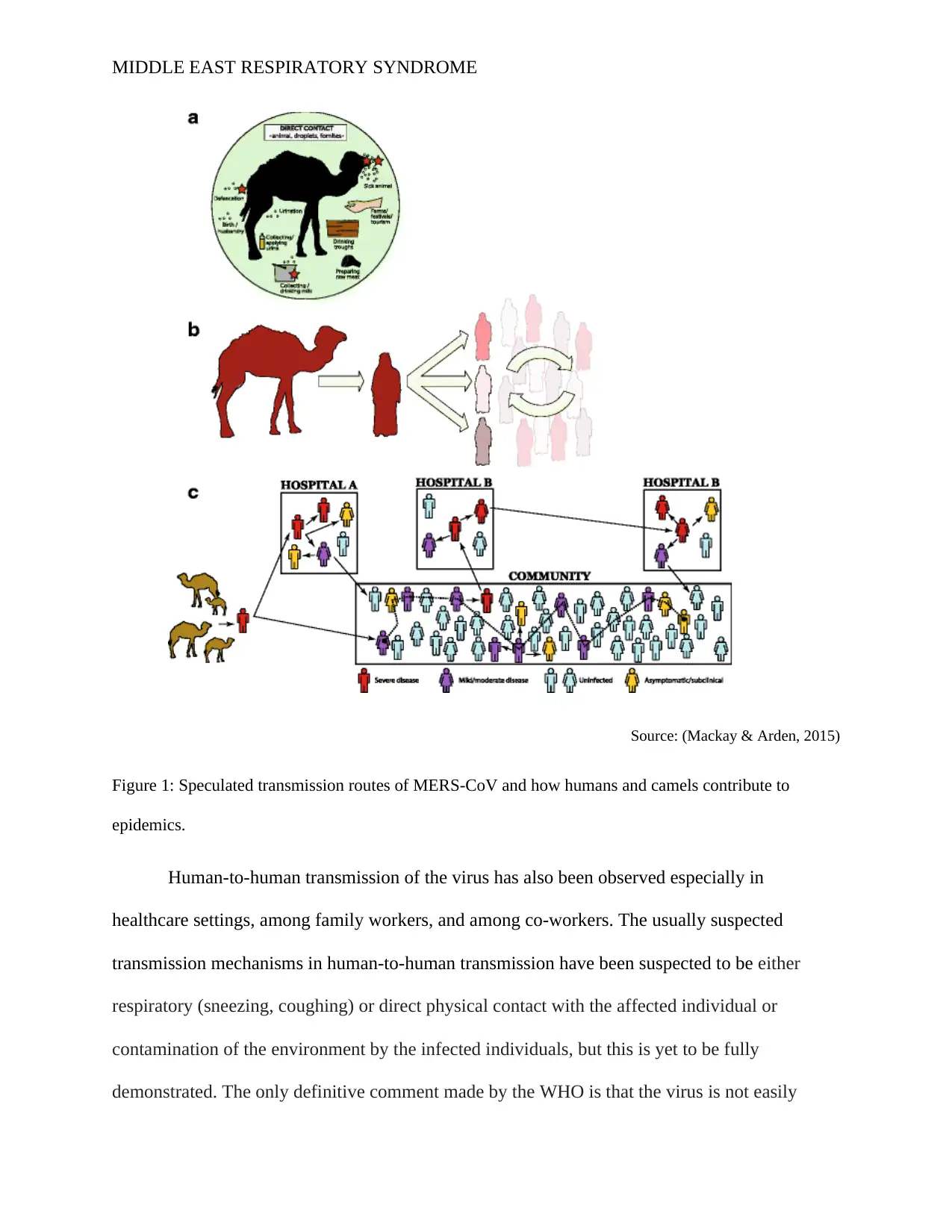
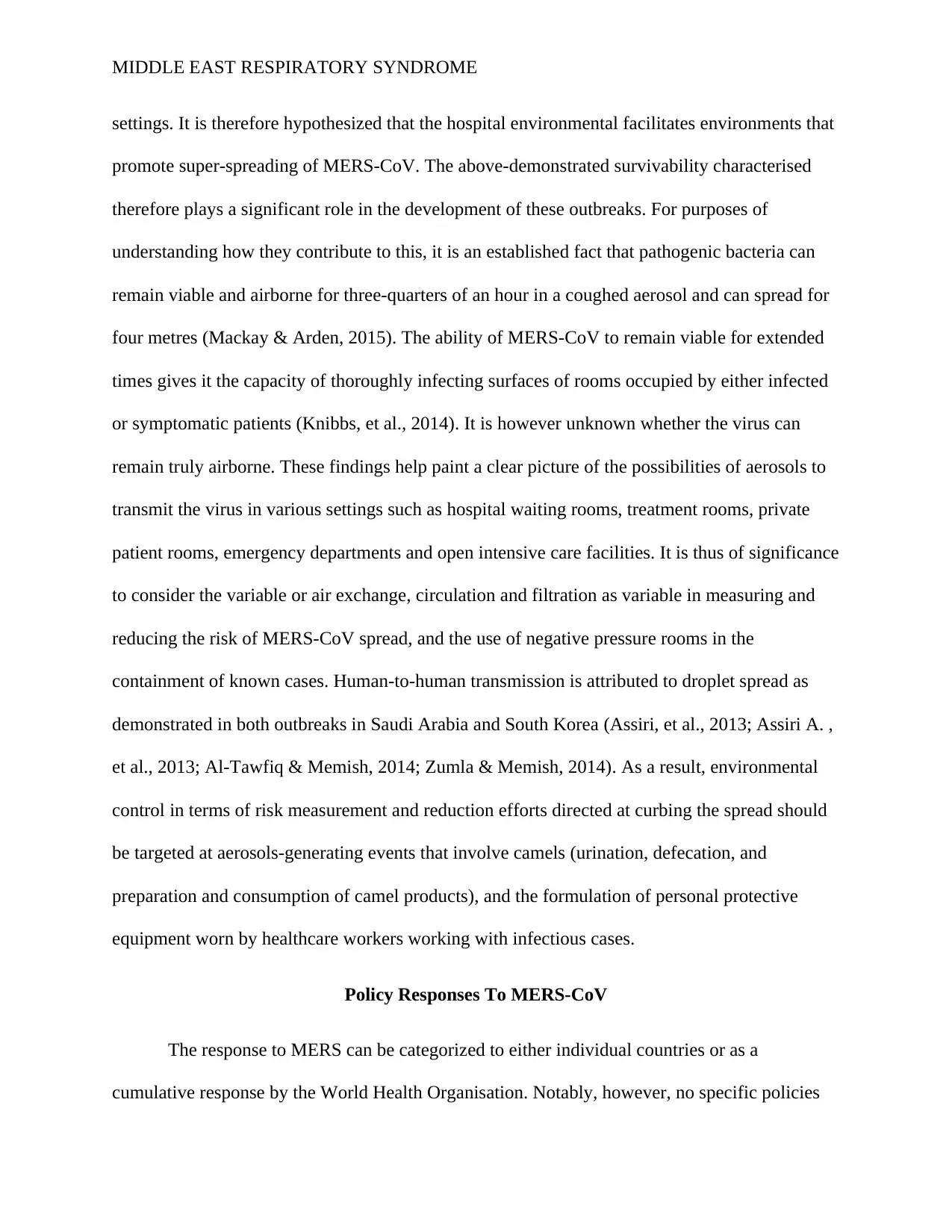
The primary hypothesis in the transmission and resulting outbreaks of MERS has been a
hypothesised link to some animals serving as either the reservoir or intermediate host(s), with
dromedary camels as the primary suspects. They are known to produce a significant amount of
MERS-CoV RNA in their lungs and the urinary tract (Khalafalla, et al., 2015). The droplet
transmission route is claimed to play a significant role in the transmission of the virus. The exact
source from which people acquire the virus from camels has not been clearly defined but it is
postulated that there is an intricate interplay of both animal and human behaviours as
demonstrated in the figure below.
Studies have demonstrated strong indicators of both direct and indirect exposure to
camels to causing the infections. This hypothesis is supported by at least one group in which the
camels also tested seropositive (WHO, 2017). Outstandingly, a review of literature also indicates
cases where the infections resulted even in the absence of a history of prior exposure to other
animals. This perspective rather suggests the likelihood of the virus being introduced through
multiple channels as opposed to a single zoonotic case.
The primary hypothesis in the transmission and resulting outbreaks of MERS has been a
hypothesised link to some animals serving as either the reservoir or intermediate host(s), with
dromedary camels as the primary suspects. They are known to produce a significant amount of
MERS-CoV RNA in their lungs and the urinary tract (Khalafalla, et al., 2015). The droplet
transmission route is claimed to play a significant role in the transmission of the virus. The exact
source from which people acquire the virus from camels has not been clearly defined but it is
postulated that there is an intricate interplay of both animal and human behaviours as
demonstrated in the figure below.
MIDDLE EAST RESPIRATORY SYNDROME
Source: (Mackay & Arden, 2015)
Figure 1: Speculated transmission routes of MERS-CoV and how humans and camels contribute to
epidemics.
Human-to-human transmission of the virus has also been observed especially in
healthcare settings, among family workers, and among co-workers. The usually suspected
transmission mechanisms in human-to-human transmission have been suspected to be either
respiratory (sneezing, coughing) or direct physical contact with the affected individual or
contamination of the environment by the infected individuals, but this is yet to be fully
demonstrated. The only definitive comment made by the WHO is that the virus is not easily
Source: (Mackay & Arden, 2015)
Figure 1: Speculated transmission routes of MERS-CoV and how humans and camels contribute to
epidemics.
Human-to-human transmission of the virus has also been observed especially in
healthcare settings, among family workers, and among co-workers. The usually suspected
transmission mechanisms in human-to-human transmission have been suspected to be either
respiratory (sneezing, coughing) or direct physical contact with the affected individual or
contamination of the environment by the infected individuals, but this is yet to be fully
demonstrated. The only definitive comment made by the WHO is that the virus is not easily
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MIDDLE EAST RESPIRATORY SYNDROME
transmitted from an individual to another unless there is close contact between the two, as
demonstrated in the provision of unprotected care to an infected patient (WHO, 2017). Cases of
human-to-human transmission have only been documented in the health care environment and
nowhere else.
Notably, the origins of MERS-CoV virus are yet to be fully understood, but analysis of
the virus genomes have demonstrated that the virus could have originated in bats and was
transmitted to dromedary camels during early ages.
Risk factors
The distribution of the disease among the already reported cases is demonstrated to be
skewed heavily to middle-aged persons and the elderly. The risk is heightened in persons who
are elderly, are immunocompromised, or present with other comorbidities (WHO, 2017). For
MERS associated with the health care environment, the risk for infection among healthcare
workers is magnified among those who have close contact with patients infected with the virus,
especially radiology technicians and nurses (Alraddadi, et al., 2016). In addition, according to the
same authors, health care workers with a history of smoking had 3 times increased risk for the
infection compared to non-smokers. This association further arouses the curiosity of the role that
smoking plays in the risk profile, unluckily, there is no literature addressing the same. This
requires further research.
Males aged above 60 years are also claimed to be at increased risk of contracting the
virus. The risk is further heightened if they suffer from underlying conditions such as renal
failure, hypertension, and diabetes (WHO, 2017). A twist to this association could rather suggest
that instead of a sex-specific difference in biologic susceptibility, males have exhibit social and
transmitted from an individual to another unless there is close contact between the two, as
demonstrated in the provision of unprotected care to an infected patient (WHO, 2017). Cases of
human-to-human transmission have only been documented in the health care environment and
nowhere else.
Notably, the origins of MERS-CoV virus are yet to be fully understood, but analysis of
the virus genomes have demonstrated that the virus could have originated in bats and was
transmitted to dromedary camels during early ages.
Risk factors
The distribution of the disease among the already reported cases is demonstrated to be
skewed heavily to middle-aged persons and the elderly. The risk is heightened in persons who
are elderly, are immunocompromised, or present with other comorbidities (WHO, 2017). For
MERS associated with the health care environment, the risk for infection among healthcare
workers is magnified among those who have close contact with patients infected with the virus,
especially radiology technicians and nurses (Alraddadi, et al., 2016). In addition, according to the
same authors, health care workers with a history of smoking had 3 times increased risk for the
infection compared to non-smokers. This association further arouses the curiosity of the role that
smoking plays in the risk profile, unluckily, there is no literature addressing the same. This
requires further research.
Males aged above 60 years are also claimed to be at increased risk of contracting the
virus. The risk is further heightened if they suffer from underlying conditions such as renal
failure, hypertension, and diabetes (WHO, 2017). A twist to this association could rather suggest
that instead of a sex-specific difference in biologic susceptibility, males have exhibit social and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MIDDLE EAST RESPIRATORY SYNDROME
behavioural factors which increase their exposure to the virus compared to females. This can be
supported by an observation by Mackay and Arden, (2015) in which males infected by MERS-
CoV present with a more severe disease compared to females of the same class.
Clinical picture
The mean incubation period for MERS-CoV has been determined to be 5 to 6 days, ranging from
2 to 16 days, with 13-14 days between when one person develops the diseases and spreads it to
another (Assiri, et al., 2013; Memish, Zumla, Al-Hakeem, Al-Rabeeah, & Stephens, 2013). For
cases with progressive illness, the median death is 11-13 days (Assiri, et al., 2013; Ki, 2015).
Early symptoms of the illness include fever, myalgia, chills and gastrointestinal symptoms,
which subsequently decline, only be substituted with more severe systemic and respiratory
syndrome, severe pneumonia with acute respiratory distress syndrome and multi-organ failure
(Kraaij-Dirkzwager, et al., 2014; Mailles, et al., 2013).
The Interaction Between The MERS-CoV, Host and Environmental Factors to Produce
MERS
Majority of camels in the Arabian Peninsula are dromedary camels and their contact with
humans ranges between little to close. This contact serves as the gateway to the transmission and
the corresponding outbreaks; hence it is significant to illustrate the interplay of the agent, the
reservoir and the environmental factors that predispose the host to the virus and consequential
development of the syndrome.
The human-camel contact is commonplace in the Arabian Peninsula and may result from
various ways (as illustrated in the figure above). Most of the countries in the Middle East (with
behavioural factors which increase their exposure to the virus compared to females. This can be
supported by an observation by Mackay and Arden, (2015) in which males infected by MERS-
CoV present with a more severe disease compared to females of the same class.
Clinical picture
The mean incubation period for MERS-CoV has been determined to be 5 to 6 days, ranging from
2 to 16 days, with 13-14 days between when one person develops the diseases and spreads it to
another (Assiri, et al., 2013; Memish, Zumla, Al-Hakeem, Al-Rabeeah, & Stephens, 2013). For
cases with progressive illness, the median death is 11-13 days (Assiri, et al., 2013; Ki, 2015).
Early symptoms of the illness include fever, myalgia, chills and gastrointestinal symptoms,
which subsequently decline, only be substituted with more severe systemic and respiratory
syndrome, severe pneumonia with acute respiratory distress syndrome and multi-organ failure
(Kraaij-Dirkzwager, et al., 2014; Mailles, et al., 2013).
The Interaction Between The MERS-CoV, Host and Environmental Factors to Produce
MERS
Majority of camels in the Arabian Peninsula are dromedary camels and their contact with
humans ranges between little to close. This contact serves as the gateway to the transmission and
the corresponding outbreaks; hence it is significant to illustrate the interplay of the agent, the
reservoir and the environmental factors that predispose the host to the virus and consequential
development of the syndrome.
The human-camel contact is commonplace in the Arabian Peninsula and may result from
various ways (as illustrated in the figure above). Most of the countries in the Middle East (with
MIDDLE EAST RESPIRATORY SYNDROME
special reference to Saudi Arabia due the fact that it has so far recorded the highest number of
cases), has several large well-attended festivals, parades, sales and races which feature
dromedary camels and also, these camels are bred and reared close to populated areas (Al-
Mukhtar & Estimo, 2014; Hemida, et al., 2015)127-128. In addition, inhabitants of these
countries have the tendency to consume milk and meat from camels after the Hajj pilgrimage
(Mackay & Arden, 2015). Notably, however, reports of infections of MERS-CoV are much
lower compared to the frequent habits of preparing, drinking, eating products from dromedary
camels. It is also established that some tribes in Saudi Arabia consume fresh unpasteurised milk
from dromedary camels, alongside their urine which is claimed to be having some health
benefits. It is however interesting to note that butchers make up a larger proportion of the local
occupations, and neither them nor any of the associated risk groups have ever been identified
among MERS cases (Mackay & Arden, 2015). A logical explanation to explain the same is that
there is a heightened likelihood to be a reporting issue and not just an unexplainable absence of
the illness. This association can be corroborated by evidence from a 2015 case-control study that
concluded that the onset of MERS is as a result of direct contact with dromedary camels and not
the ingestion of products from these animals (Alraddadi, et al., 2014). Some researchers hold a
different hypothesis that there is the likelihood of humans infecting dromedary camels, contrary
to the already established hypothesis. This divergent proposition has been instigated by
laboratory finding in which whenever cases of MERS have been reported, the camel population
is also found to have nasal colonisation of the virus alike. This hypothesis is however yet to be
studied and proven.
Camels often calve during the winter months that run between late October and late
February and this season may be characterised by an increased risk of spill-over of the virus to
special reference to Saudi Arabia due the fact that it has so far recorded the highest number of
cases), has several large well-attended festivals, parades, sales and races which feature
dromedary camels and also, these camels are bred and reared close to populated areas (Al-
Mukhtar & Estimo, 2014; Hemida, et al., 2015)127-128. In addition, inhabitants of these
countries have the tendency to consume milk and meat from camels after the Hajj pilgrimage
(Mackay & Arden, 2015). Notably, however, reports of infections of MERS-CoV are much
lower compared to the frequent habits of preparing, drinking, eating products from dromedary
camels. It is also established that some tribes in Saudi Arabia consume fresh unpasteurised milk
from dromedary camels, alongside their urine which is claimed to be having some health
benefits. It is however interesting to note that butchers make up a larger proportion of the local
occupations, and neither them nor any of the associated risk groups have ever been identified
among MERS cases (Mackay & Arden, 2015). A logical explanation to explain the same is that
there is a heightened likelihood to be a reporting issue and not just an unexplainable absence of
the illness. This association can be corroborated by evidence from a 2015 case-control study that
concluded that the onset of MERS is as a result of direct contact with dromedary camels and not
the ingestion of products from these animals (Alraddadi, et al., 2014). Some researchers hold a
different hypothesis that there is the likelihood of humans infecting dromedary camels, contrary
to the already established hypothesis. This divergent proposition has been instigated by
laboratory finding in which whenever cases of MERS have been reported, the camel population
is also found to have nasal colonisation of the virus alike. This hypothesis is however yet to be
studied and proven.
Camels often calve during the winter months that run between late October and late
February and this season may be characterised by an increased risk of spill-over of the virus to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MIDDLE EAST RESPIRATORY SYNDROME
humans because new infections are often likely to occur within the camel populations (Hemida,
et al., 2015). The role played by maternal camel antibody in delaying infection in the calves is
yet to be established (Memish, et al., 2013; Hemida, et al., 2015). Young camels have been
found to host active infection more often compared to their parents, and as a result of the
inclination to choose camels aged 5 years or older for sacrificial slaughter, and this is
accompanied with an insignificant risk of exposure to the virus. This conclusion draws reference
back to the fact that slaughterhouse workers stand out as a high-risk occupational group.
The survivability of MERS-CoV in the environment is also important towards
understanding the association between the various parameters leading to the development of the
illness. Laboratory experiments have demonstrated that adding the virus to milk from either a
camel, goat or cow, and storing it at low temperatures (4 degrees Celsius), the virus could still be
recovered at least seventy-two hours later, and if stored at 22 degrees Celsius (almost room
temperature), the virus could still survive up to 48 hours (van Doremalen, Bushmaker, &
Munster, 2013).
On the survivability of the virus in the environment in the absence of a milk medium, a
study by van Doremalen, Bushmaker, and Munster, (2013) was able to demonstrate that even at
high ambient temperatures (about 30 degrees Celsius) and low relative humidity (30%), the virus
still remains viable for up to 24 hours. This demonstrates quite a significant survivability rate
compared to other well-known and efficiently transmitted respiratory virus such as influenza A
virus which cannot be recovered even after four hours under the same conditions to those
survived by MERS-CoV (van Doremalen, Bushmaker, & Munster, 2013). However, the survival
of MERS-CoV is still said to be inferior compared to that of SARS-CoV (Chan, et al., 2011).
MERS outbreaks have been so far experienced in health care settings as opposed to community
humans because new infections are often likely to occur within the camel populations (Hemida,
et al., 2015). The role played by maternal camel antibody in delaying infection in the calves is
yet to be established (Memish, et al., 2013; Hemida, et al., 2015). Young camels have been
found to host active infection more often compared to their parents, and as a result of the
inclination to choose camels aged 5 years or older for sacrificial slaughter, and this is
accompanied with an insignificant risk of exposure to the virus. This conclusion draws reference
back to the fact that slaughterhouse workers stand out as a high-risk occupational group.
The survivability of MERS-CoV in the environment is also important towards
understanding the association between the various parameters leading to the development of the
illness. Laboratory experiments have demonstrated that adding the virus to milk from either a
camel, goat or cow, and storing it at low temperatures (4 degrees Celsius), the virus could still be
recovered at least seventy-two hours later, and if stored at 22 degrees Celsius (almost room
temperature), the virus could still survive up to 48 hours (van Doremalen, Bushmaker, &
Munster, 2013).
On the survivability of the virus in the environment in the absence of a milk medium, a
study by van Doremalen, Bushmaker, and Munster, (2013) was able to demonstrate that even at
high ambient temperatures (about 30 degrees Celsius) and low relative humidity (30%), the virus
still remains viable for up to 24 hours. This demonstrates quite a significant survivability rate
compared to other well-known and efficiently transmitted respiratory virus such as influenza A
virus which cannot be recovered even after four hours under the same conditions to those
survived by MERS-CoV (van Doremalen, Bushmaker, & Munster, 2013). However, the survival
of MERS-CoV is still said to be inferior compared to that of SARS-CoV (Chan, et al., 2011).
MERS outbreaks have been so far experienced in health care settings as opposed to community
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MIDDLE EAST RESPIRATORY SYNDROME
settings. It is therefore hypothesized that the hospital environmental facilitates environments that
promote super-spreading of MERS-CoV. The above-demonstrated survivability characterised
therefore plays a significant role in the development of these outbreaks. For purposes of
understanding how they contribute to this, it is an established fact that pathogenic bacteria can
remain viable and airborne for three-quarters of an hour in a coughed aerosol and can spread for
four metres (Mackay & Arden, 2015). The ability of MERS-CoV to remain viable for extended
times gives it the capacity of thoroughly infecting surfaces of rooms occupied by either infected
or symptomatic patients (Knibbs, et al., 2014). It is however unknown whether the virus can
remain truly airborne. These findings help paint a clear picture of the possibilities of aerosols to
transmit the virus in various settings such as hospital waiting rooms, treatment rooms, private
patient rooms, emergency departments and open intensive care facilities. It is thus of significance
to consider the variable or air exchange, circulation and filtration as variable in measuring and
reducing the risk of MERS-CoV spread, and the use of negative pressure rooms in the
containment of known cases. Human-to-human transmission is attributed to droplet spread as
demonstrated in both outbreaks in Saudi Arabia and South Korea (Assiri, et al., 2013; Assiri A. ,
et al., 2013; Al-Tawfiq & Memish, 2014; Zumla & Memish, 2014). As a result, environmental
control in terms of risk measurement and reduction efforts directed at curbing the spread should
be targeted at aerosols-generating events that involve camels (urination, defecation, and
preparation and consumption of camel products), and the formulation of personal protective
equipment worn by healthcare workers working with infectious cases.
Policy Responses To MERS-CoV
The response to MERS can be categorized to either individual countries or as a
cumulative response by the World Health Organisation. Notably, however, no specific policies
settings. It is therefore hypothesized that the hospital environmental facilitates environments that
promote super-spreading of MERS-CoV. The above-demonstrated survivability characterised
therefore plays a significant role in the development of these outbreaks. For purposes of
understanding how they contribute to this, it is an established fact that pathogenic bacteria can
remain viable and airborne for three-quarters of an hour in a coughed aerosol and can spread for
four metres (Mackay & Arden, 2015). The ability of MERS-CoV to remain viable for extended
times gives it the capacity of thoroughly infecting surfaces of rooms occupied by either infected
or symptomatic patients (Knibbs, et al., 2014). It is however unknown whether the virus can
remain truly airborne. These findings help paint a clear picture of the possibilities of aerosols to
transmit the virus in various settings such as hospital waiting rooms, treatment rooms, private
patient rooms, emergency departments and open intensive care facilities. It is thus of significance
to consider the variable or air exchange, circulation and filtration as variable in measuring and
reducing the risk of MERS-CoV spread, and the use of negative pressure rooms in the
containment of known cases. Human-to-human transmission is attributed to droplet spread as
demonstrated in both outbreaks in Saudi Arabia and South Korea (Assiri, et al., 2013; Assiri A. ,
et al., 2013; Al-Tawfiq & Memish, 2014; Zumla & Memish, 2014). As a result, environmental
control in terms of risk measurement and reduction efforts directed at curbing the spread should
be targeted at aerosols-generating events that involve camels (urination, defecation, and
preparation and consumption of camel products), and the formulation of personal protective
equipment worn by healthcare workers working with infectious cases.
Policy Responses To MERS-CoV
The response to MERS can be categorized to either individual countries or as a
cumulative response by the World Health Organisation. Notably, however, no specific policies
MIDDLE EAST RESPIRATORY SYNDROME
have been designed to control the virus, but rather various guidelines are available for the control
of the same. For instance, the Saudi Arabian Ministry of health has responded with both
outbreak control policies touching on notification of suspected cases, risk assessment,
investigation procedures and treatment protocols. WHO has likewise taken various steps and also
projected steps to be undertaken later on.
WHO works with various countries, and has notably worked with CDC to develop
policies aimed at improving the efficiency of surveillance (Banerjee, Rawat, & Subudhi, 2015),
and the Saudi Arabian Ministry of Health (MoH) to develop specific guideline for the control
and prevention of infections by the virus for both health care workers, patients and their family
members contained under the Scientific Advisory Board’s Infection Prevention and Control
Guidelines for Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Infection (Saudi
Arabia Ministry of Health, 2014; Scientific Advisory Board, 2015). Neither CDC nor Saudi
Arabia MoH has prescribed specific guidelines for the control of the agent, but have rather made
recommendations for quarantine measures for infected individuals and have also prescribed
guidelines to be followed before the infected person resumes regular activities following
recovery. Both the CDC, Saudi Arabian MoH and various agencies from most countries
(Australia included) have also prescribed guidelines for airport staff on the management of
suspected MERS cases, and likewise developed advisories and precautionary statements for
travellers into and out of the countries.
The WHO Director-General convened the International Health Regulations (IHR)
Emergency Committee on MERS which is chaired by Australia’s Chief Medical Officer (The
Department of Health, 2016). In the case of Australia, the country’s Communicable Diseases
Network Australia has also developed a national guideline for the public health management of
have been designed to control the virus, but rather various guidelines are available for the control
of the same. For instance, the Saudi Arabian Ministry of health has responded with both
outbreak control policies touching on notification of suspected cases, risk assessment,
investigation procedures and treatment protocols. WHO has likewise taken various steps and also
projected steps to be undertaken later on.
WHO works with various countries, and has notably worked with CDC to develop
policies aimed at improving the efficiency of surveillance (Banerjee, Rawat, & Subudhi, 2015),
and the Saudi Arabian Ministry of Health (MoH) to develop specific guideline for the control
and prevention of infections by the virus for both health care workers, patients and their family
members contained under the Scientific Advisory Board’s Infection Prevention and Control
Guidelines for Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Infection (Saudi
Arabia Ministry of Health, 2014; Scientific Advisory Board, 2015). Neither CDC nor Saudi
Arabia MoH has prescribed specific guidelines for the control of the agent, but have rather made
recommendations for quarantine measures for infected individuals and have also prescribed
guidelines to be followed before the infected person resumes regular activities following
recovery. Both the CDC, Saudi Arabian MoH and various agencies from most countries
(Australia included) have also prescribed guidelines for airport staff on the management of
suspected MERS cases, and likewise developed advisories and precautionary statements for
travellers into and out of the countries.
The WHO Director-General convened the International Health Regulations (IHR)
Emergency Committee on MERS which is chaired by Australia’s Chief Medical Officer (The
Department of Health, 2016). In the case of Australia, the country’s Communicable Diseases
Network Australia has also developed a national guideline for the public health management of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





