Health Alterations - NUR241: Metformin Medication Report Analysis
VerifiedAdded on 2023/03/23
|1
|642
|62
Report
AI Summary
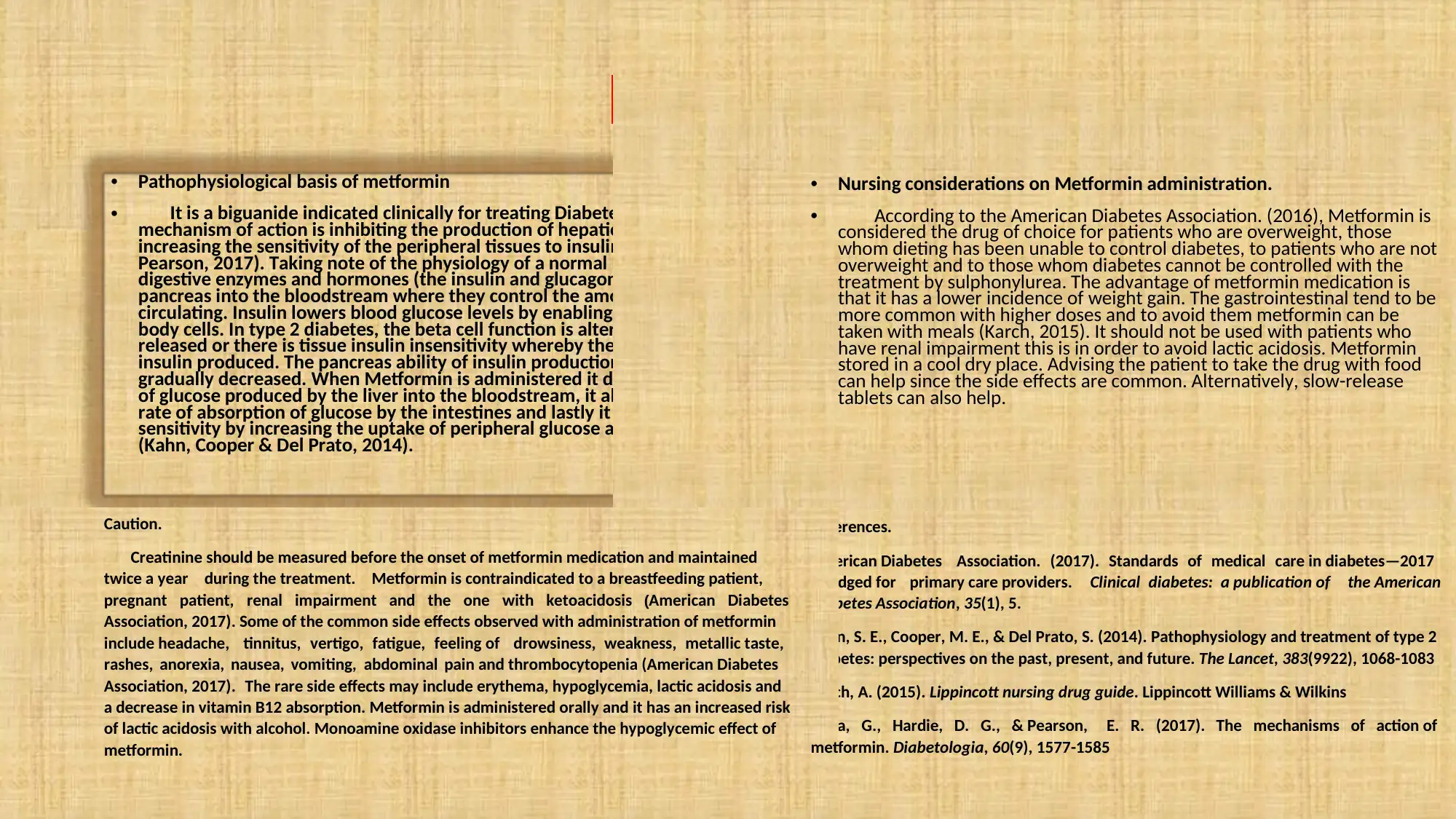
This report focuses on Metformin, a biguanide medication used to treat Type 2 Diabetes mellitus. It details the drug's mechanism of action, which includes inhibiting hepatic glucose production and increasing peripheral tissue sensitivity to insulin. The report explains the pathophysiology of Type 2 Diabetes, highlighting the role of insulin and glucagon in glucose regulation and the impact of beta-cell dysfunction and insulin resistance. It then examines how Metformin works to decrease glucose production by the liver, reduce glucose absorption in the intestines, and improve insulin sensitivity. The report also covers clinical applications of Metformin, including its consideration as a first-line treatment for overweight patients and those whose diabetes is not well-controlled by diet or other medications. It further addresses nursing considerations, such as contraindications (renal impairment, pregnancy, and breastfeeding), potential side effects (gastrointestinal issues, headache, and lactic acidosis), and patient education regarding administration (with meals) and monitoring (creatinine levels). References from the American Diabetes Association and other sources support the information provided.






![[object Object]](/_next/static/media/star-bottom.7253800d.svg)