Motivational Interviewing Training with Simulation for Opioid Abuse
VerifiedAdded on 2022/09/03
|9
|7385
|40
Report
AI Summary
This research article investigates the effectiveness of motivational interviewing (MI) training, incorporating didactic lectures, role-playing exercises, and standardized patient (SP) simulation, on the learning outcomes of Doctor of Nursing Practice (DNP) students. The study, employing a one-group pretest-posttest design, aimed to enhance students' knowledge and confidence in managing prescription opioid abuse among older adults. Findings revealed significant improvements in both knowledge and confidence levels post-training. The study highlights the potential of MI training with SP simulation to improve care for older adults who misuse opioids, addressing a critical healthcare issue. The research underscores the importance of integrating MI into healthcare curricula to equip future providers with effective behavioral intervention skills.
Perspect Psychiatr Care.2019;55:681-689. wileyonlinelibrary.com/journal/ppc © 2019 Wiley Periodicals,Inc. | 681
Received:24 September 2018| Revised: 14 April 2019| Accepted:5 May 2019
DOI: 10.1111/ppc.12402
O R I G I N A L A R T I C L E
Motivational interviewing training with standardized patient
simulation for prescription opioid abuse among older adults
Yu‐Ping Chang PhD,RN, FGSA, FAAN 1 | Jade Cassalia DNP,FNP‐C2 |
Molli Warunek DNP,FNP‐C1 | Yvonne Scherer EdD,RN1
1School of Nursing,The State University of
New York,University at Buffalo,Buffalo,New
York
2Newark‐Wayne Community Hospital,
Rochester,New York
Correspondence
Yu‐Ping Chang PhD,RN, FGSA,FAAN, School
of Nursing,The State University of New York,
University at Buffalo,Buffalo,3435 Main
Street,Wende Hall Rm 301C,Buffalo,NY
14214.
Email:yc73@buffalo.edu
Funding information
Health Foundation for Western and Central
New York
Abstract
Purpose:This study aimed to examine the effect of motivationalinterviewing (MI)
education on the doctorate of nursing practice (DNP) students’learning outcomes.
Design and methods:This study used a one‐group with preposttestdesign.The
sample consisted of31 DNP students who received an MI training,including a
didactic lecture,role‐playing exercise,and standardized patient simulation.
Findings: Findings indicated a significantincrease in students’knowledge and
confidence regarding MI at both posttests compared with baseline.
Practice implications: Findings suggested that MI training with standardized patient
simulation demonstrated preliminary promising effects on DNP students’knowledge
and confidence in MI techniques to manage prescription opioid abuse among older
adults. This study showed the potential to enhance the care of older adults who abuse
opioids to address this problem in practice.
K E Y W O R D S
chronic pain,motivationalinterviewing,older adults,prescription opioid misuse,standardized
patient simulation
1 | INTRODUCTION
Prescription opioids are a common strategy for managing chronic
pain in older adults.1 The use of these medications in the older adult
population has increased nine‐fold between the years of1995 to
2010.2 It has been found that 92% of older adults that were
prescribed opioids had been on them for a period of5 years or
more.3 Opioids are being used more frequently and for longer
periods of time to treat patients experiencing chronic pain.4 As the
use of opioids has increased, there has been a corresponding increase
in their misuse or abuse.5 In 2012, 2.9 million older adults in America
reported nonmedical use of their prescription drugs.6 In addition, the
rates of older adults being admitted into facilities for treatment of
prescription drug abuse has increased from 0.7% to 3.5% between
the years of 1992 to 2005.3 As the population of older adults
increases,especially with the aging of baby boomers,it is expected
that providers will be faced with increased incidences of chronic pain.
Inevitably,this will lead to increased prescription opioid use by the
older adult population, thereby increasing the potential for misuse or
abuse.7
The question raised by this growing problem is how to properly
intervene in older adults with chronic pain who misuse or abuse their
prescription opioids?Currently, there is limited information on
effective interventionsfor substance use disorder(SUD) among
older adults.However,there are severalavailable evidence‐based
practice approaches for the treatment ofSUD within the general
population.One approach is the use of motivationalinterviewing
(MI). MI is a patient‐centered,semi‐directive cognitive behavioral
method that focuses on enhancing intrinsic motivation,and auton-
omy to change behavior.8 Clinicians help patients identify problem
behaviors,resolve ambivalence,determine and enhance motivation,
and aid in problem‐solving and goalsetting.9 MI has been demon-
strated to be effective in patient health behavior outcomes, including
substance abuse.8,9 There are studies that support the efficacy of MI
on behavior change among older adults to address a variety of health
care issues including physical activity, general health, smoking
Received:24 September 2018| Revised: 14 April 2019| Accepted:5 May 2019
DOI: 10.1111/ppc.12402
O R I G I N A L A R T I C L E
Motivational interviewing training with standardized patient
simulation for prescription opioid abuse among older adults
Yu‐Ping Chang PhD,RN, FGSA, FAAN 1 | Jade Cassalia DNP,FNP‐C2 |
Molli Warunek DNP,FNP‐C1 | Yvonne Scherer EdD,RN1
1School of Nursing,The State University of
New York,University at Buffalo,Buffalo,New
York
2Newark‐Wayne Community Hospital,
Rochester,New York
Correspondence
Yu‐Ping Chang PhD,RN, FGSA,FAAN, School
of Nursing,The State University of New York,
University at Buffalo,Buffalo,3435 Main
Street,Wende Hall Rm 301C,Buffalo,NY
14214.
Email:yc73@buffalo.edu
Funding information
Health Foundation for Western and Central
New York
Abstract
Purpose:This study aimed to examine the effect of motivationalinterviewing (MI)
education on the doctorate of nursing practice (DNP) students’learning outcomes.
Design and methods:This study used a one‐group with preposttestdesign.The
sample consisted of31 DNP students who received an MI training,including a
didactic lecture,role‐playing exercise,and standardized patient simulation.
Findings: Findings indicated a significantincrease in students’knowledge and
confidence regarding MI at both posttests compared with baseline.
Practice implications: Findings suggested that MI training with standardized patient
simulation demonstrated preliminary promising effects on DNP students’knowledge
and confidence in MI techniques to manage prescription opioid abuse among older
adults. This study showed the potential to enhance the care of older adults who abuse
opioids to address this problem in practice.
K E Y W O R D S
chronic pain,motivationalinterviewing,older adults,prescription opioid misuse,standardized
patient simulation
1 | INTRODUCTION
Prescription opioids are a common strategy for managing chronic
pain in older adults.1 The use of these medications in the older adult
population has increased nine‐fold between the years of1995 to
2010.2 It has been found that 92% of older adults that were
prescribed opioids had been on them for a period of5 years or
more.3 Opioids are being used more frequently and for longer
periods of time to treat patients experiencing chronic pain.4 As the
use of opioids has increased, there has been a corresponding increase
in their misuse or abuse.5 In 2012, 2.9 million older adults in America
reported nonmedical use of their prescription drugs.6 In addition, the
rates of older adults being admitted into facilities for treatment of
prescription drug abuse has increased from 0.7% to 3.5% between
the years of 1992 to 2005.3 As the population of older adults
increases,especially with the aging of baby boomers,it is expected
that providers will be faced with increased incidences of chronic pain.
Inevitably,this will lead to increased prescription opioid use by the
older adult population, thereby increasing the potential for misuse or
abuse.7
The question raised by this growing problem is how to properly
intervene in older adults with chronic pain who misuse or abuse their
prescription opioids?Currently, there is limited information on
effective interventionsfor substance use disorder(SUD) among
older adults.However,there are severalavailable evidence‐based
practice approaches for the treatment ofSUD within the general
population.One approach is the use of motivationalinterviewing
(MI). MI is a patient‐centered,semi‐directive cognitive behavioral
method that focuses on enhancing intrinsic motivation,and auton-
omy to change behavior.8 Clinicians help patients identify problem
behaviors,resolve ambivalence,determine and enhance motivation,
and aid in problem‐solving and goalsetting.9 MI has been demon-
strated to be effective in patient health behavior outcomes, including
substance abuse.8,9 There are studies that support the efficacy of MI
on behavior change among older adults to address a variety of health
care issues including physical activity, general health, smoking
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
cessation,diet, weight loss,and cardiovascular risk factors.10 One
study on hazardous drinking among the older adult population found
that MI had a significant impact on decreasing the number of drinks
per day, the total number of drinks overall, as well as increasing days
of abstinence when compared with standard care.11
2 | CURRENT ISSUE ON BEHAVIORAL
INTERVENTION TRAINING AMONG
HEALTH CARE PROVIDERS
Without adequate mentaland behavioralhealth services to treat
older adults who are misusing or abusing their prescription opioids,
the burden falls to other health care providers,such as primary care
providers.Currently,MI has not been adequately incorporated into
the educational curriculum of health care providers, preventing them
from gaining enough knowledge and skill to perform this intervention
when they begin practicing.It has also been noted that older adults
are less likely to seek help for their substance use,12 partially due to
perceived stigma.Utilizing MI techniques within the primary care
setting might increase older adults’motivation to seek treatments.
As a counseling approach that can be utilized by any health care
providers,including primary care,MI could be a feasible solution to
overcoming barriers for providing intervention to older adults with a
SUD.The utilization of MI would allow any health care provider who
is a part of the patient’s care, the ability to promote behavior change.
In addition,MI has been found to be useful in situations where there
is limited contact with patients and can be performed in as little as
one to two sessions.13 MI also has the potentialto be used as a
preventative measure for prescription opioid misuse or abuse for
individuals with chronic pain issues.A pilot study found that the use
of MI decreased the risk of prescription opioid abuse in older adults
with chronic pain,as well as decreased the risk of alcohol abuse for
those that drank.14
2.1 | Motivational interviewing training
With the lack of educational preparation on behavioral interventions
and the inadequate numbers of trained mentalhealth providers,an
argument can be made that it is important for future health care
providers to be educated on the use ofMI. With proper training,
health care providers can be more competent in addressing issues
among older adults with chronic pain who are misusing or abusing
their prescription opioids. Multiple studies have focused on
incorporating MI education into the curricula ofdifferent health
care disciplines.The most frequently studied discipline is medical
education.15-17 These studies indicated that a formalized MI
education helped to increase medical student’s behavioral counseling
skills and supported that MI education should be a part of an
educationalcurriculum for future providers in an effort to better
prepare them to address behavior modification in their future patient
population.Yet, such integration and evaluation of MI education in
nursing education is lacking.
2.2 | Standardized patient simulations
With the understanding that MI education is important,the question
arises as to how to educate future health care providers in this
technique.A number of studies on MI education with medical
students utilized standardizedpatients (SP) as an educational
intervention and assessmenttool.15-17 Research supports the use
of SP as an educational strategy that has been found to be effective
in improving student’s knowledge,psychomotor skills,and commu-
nication skills when used in the fields of medical and nursing
education.18 A meta‐analysis on the efficacy of SP in nursing
education found that SP had a significant positive effect on students’
cognitive (knowledge,critical thinking, communication,problem‐
solving),affective (learning motivation,self‐efficacy,learning satis-
faction), and psychomotor (clinical competencies) learning domains.19
SP used in mental health education provides an increased benefit of
allowing students to be able to assess nonverbalcues that patients
exhibit such as body and facial expression. Nonverbal communication
can provide information that may be useful in evaluating and
developing a plan of care for patients.20
With approximately two‐thirdsof Americansbeing seen by
advanced practice nurses (APNs)for their health care needs,the
potential for APNs to make a significant contribution toward
addressing the needs of older adults who are misusing or abusing
their prescription opioids is clearly evident. This supports the
argumentfor the need to educate APNs on MI so they will be
equipped with the appropriate skills and knowledge needed to utilize
this behavioral intervention.However,there is a lack of research on
MI education for APN students.This study aimed to evaluate an MI
educationalintervention through the use of didactic and SP
simulations on the doctorate of nursing practice (DNP) students to
address prescription opioid abuse in the older adult population living
with chronic pain.
3 | METHOD
3.1 | Design and sample
This study utilized a one‐group pretest‐posttest design with a
convenience sampling.The outcome variables included confi-
dence,knowledge,and skills regarding the use of MI.The sample
consisted of 31 students who were enrolled in the baccalaureate
of nursing (BSN) to the doctorate of nursing practice program
(DNP) of a University. The MI educational intervention was
integrated into the advanced health assessment course.The MI
education included a didactic lecture,a role‐playing exercise,and
SP simulation.All students enrolled in the course were required
to complete this activity.The students were given a choice as to
whether or not they wanted to complete the pre‐ and posttests.
Completion of the pre‐ and posttests were indicative of informed
consent that the data could be used for research purposes.An
explanation of how this data would be used was provided to the
students before the implementation ofthe study. The didactic
682 | CHANG ET AL.
study on hazardous drinking among the older adult population found
that MI had a significant impact on decreasing the number of drinks
per day, the total number of drinks overall, as well as increasing days
of abstinence when compared with standard care.11
2 | CURRENT ISSUE ON BEHAVIORAL
INTERVENTION TRAINING AMONG
HEALTH CARE PROVIDERS
Without adequate mentaland behavioralhealth services to treat
older adults who are misusing or abusing their prescription opioids,
the burden falls to other health care providers,such as primary care
providers.Currently,MI has not been adequately incorporated into
the educational curriculum of health care providers, preventing them
from gaining enough knowledge and skill to perform this intervention
when they begin practicing.It has also been noted that older adults
are less likely to seek help for their substance use,12 partially due to
perceived stigma.Utilizing MI techniques within the primary care
setting might increase older adults’motivation to seek treatments.
As a counseling approach that can be utilized by any health care
providers,including primary care,MI could be a feasible solution to
overcoming barriers for providing intervention to older adults with a
SUD.The utilization of MI would allow any health care provider who
is a part of the patient’s care, the ability to promote behavior change.
In addition,MI has been found to be useful in situations where there
is limited contact with patients and can be performed in as little as
one to two sessions.13 MI also has the potentialto be used as a
preventative measure for prescription opioid misuse or abuse for
individuals with chronic pain issues.A pilot study found that the use
of MI decreased the risk of prescription opioid abuse in older adults
with chronic pain,as well as decreased the risk of alcohol abuse for
those that drank.14
2.1 | Motivational interviewing training
With the lack of educational preparation on behavioral interventions
and the inadequate numbers of trained mentalhealth providers,an
argument can be made that it is important for future health care
providers to be educated on the use ofMI. With proper training,
health care providers can be more competent in addressing issues
among older adults with chronic pain who are misusing or abusing
their prescription opioids. Multiple studies have focused on
incorporating MI education into the curricula ofdifferent health
care disciplines.The most frequently studied discipline is medical
education.15-17 These studies indicated that a formalized MI
education helped to increase medical student’s behavioral counseling
skills and supported that MI education should be a part of an
educationalcurriculum for future providers in an effort to better
prepare them to address behavior modification in their future patient
population.Yet, such integration and evaluation of MI education in
nursing education is lacking.
2.2 | Standardized patient simulations
With the understanding that MI education is important,the question
arises as to how to educate future health care providers in this
technique.A number of studies on MI education with medical
students utilized standardizedpatients (SP) as an educational
intervention and assessmenttool.15-17 Research supports the use
of SP as an educational strategy that has been found to be effective
in improving student’s knowledge,psychomotor skills,and commu-
nication skills when used in the fields of medical and nursing
education.18 A meta‐analysis on the efficacy of SP in nursing
education found that SP had a significant positive effect on students’
cognitive (knowledge,critical thinking, communication,problem‐
solving),affective (learning motivation,self‐efficacy,learning satis-
faction), and psychomotor (clinical competencies) learning domains.19
SP used in mental health education provides an increased benefit of
allowing students to be able to assess nonverbalcues that patients
exhibit such as body and facial expression. Nonverbal communication
can provide information that may be useful in evaluating and
developing a plan of care for patients.20
With approximately two‐thirdsof Americansbeing seen by
advanced practice nurses (APNs)for their health care needs,the
potential for APNs to make a significant contribution toward
addressing the needs of older adults who are misusing or abusing
their prescription opioids is clearly evident. This supports the
argumentfor the need to educate APNs on MI so they will be
equipped with the appropriate skills and knowledge needed to utilize
this behavioral intervention.However,there is a lack of research on
MI education for APN students.This study aimed to evaluate an MI
educationalintervention through the use of didactic and SP
simulations on the doctorate of nursing practice (DNP) students to
address prescription opioid abuse in the older adult population living
with chronic pain.
3 | METHOD
3.1 | Design and sample
This study utilized a one‐group pretest‐posttest design with a
convenience sampling.The outcome variables included confi-
dence,knowledge,and skills regarding the use of MI.The sample
consisted of 31 students who were enrolled in the baccalaureate
of nursing (BSN) to the doctorate of nursing practice program
(DNP) of a University. The MI educational intervention was
integrated into the advanced health assessment course.The MI
education included a didactic lecture,a role‐playing exercise,and
SP simulation.All students enrolled in the course were required
to complete this activity.The students were given a choice as to
whether or not they wanted to complete the pre‐ and posttests.
Completion of the pre‐ and posttests were indicative of informed
consent that the data could be used for research purposes.An
explanation of how this data would be used was provided to the
students before the implementation ofthe study. The didactic
682 | CHANG ET AL.
lecture and the role‐playing exercise occurred in a classroom
setting and the SP simulation took place within the simulation
center of the University.Approval for this study was obtained by
the University’s InstitutionalReview Board.
3.2 | Didactic lecture and role play
The MI lecture and role‐playing scenario were developed by two
experts who have experience in utilizing MI in research,education,
and clinicalpractice.Materials used for the didactic lecture were
taken in part from the Motivational Interviewing Network of
Trainers,an organization designed to promote research and training
of MI. Other materials were obtained from a thorough review of the
current literature on MI training. The didactic lecture includes
content on MI principles,spirit, core skills,techniques,and clinical
applications,as well as barriers to helping patientschange.The
lecture used the example of an older adult who took more
prescription opioids than prescribed.A role‐playing scenario utilizing
that example was demonstrated to students by the research team.
The students were then given similar scenarios and performed role‐
playing by taking turns,acting as both the patient and practitioner.
The research team and course instructorwere available to help
students with MI skills and techniques,provide immediate feedback,
and answer any questions.
3.3 | Simulation preparation and implementation
3.3.1 | Preparation
The SP scenario was developed by an expert panelof psychiatric‐
mental health professionals,family nursing practitioners,MI experts,
addiction researchers, experienced educators, and simulation faculty.
The SP simulation involved an older adult patient who was asking for
an early refillof prescription opioid medication that he took for his
chronic pain.The patient had been misusing his opioids by taking
more than prescribed to help with pain and other symptoms.The
patient in the scenario was a recent widower who was becoming
increasingly depressed and was also drinking in excess.He had risk
factors of socialisolation,limited mobility,and unmanaged pain.An
MI lecture was provided to 11 SP who were experienced professional
actors in simulation.A training section was held to promote SP’s
understanding of MIeducation,as well as the simulation scenario.
SP’s training involved a 2‐hour training session that covered topics
including project overview; read‐through and clarification of scenar-
io; role‐playing;trouble‐shooting;appropriate attire and demeanor
(eg body language,disposition,etc) during simulation;a tour of
simulation rooms;and what type of education students were given.
The SPs were expected to study the training materialfor 4 hours
after the training session before the simulation. The SPs also received
a lecture on the basic concepts of MI.A brief meeting with SPs was
held directly before the simulation for a brief review of the training
materials and to answer any questions.
Students were given a briefreview of the simulation process
before the simulation took place.Studentswere encouraged to
review training materials as described in the didactic and role‐play
section.Students were given a PowerPoint lecture on the simulation
process including the SP,space,time duration,and procedure.A
discussion was also held with students to help them understand the
simulation process,expectations,and to address any questions or
concerns.
3.3.2 | Implementation
Students were given 10 minutesto review a door chart that
contained pertinentpatient information thatwould simulate the
type of information a “real‐life” provider may have before a patient
encounter. The door chart contained instructions for students to help
guide them through the simulation.The instructions were very
detailed,as the participants in the study were the first year DNP
students who had not yet taken their clinicalpracticum course,nor
had any prior experience with SP simulation.After the 10‐minute
review, students were prompted to enter the patient room and begin
the encounter.The encounter was limited to 30 minutes.After the
students finished their encounter,they were asked to wait outside
the patient’s door.Then as a group,they were taken to a computer
lab to complete their simulation evaluation.After all, students
completed their evaluation,they were taken into a conference room
for debriefing.Debriefing was facilitated by the research staff and
included reflection and discussion regarding the simulation scenario,
the educationalintervention,and the simulation process.Students
were asked questions such as: what could be done better with regard
to the simulation experience? What aspects of MIwere you most
successfulat demonstratingor would like to strengthen? And
whether or not a participation in the simulation experience helped
better prepare you for implementing MI into your clinicalpractice.
The debriefing session provided an opportunity forstudentsto
critique and reflect on their performance and facilitate learning by
recognizing the knowledge and skills they demonstrated vs those
they did not.This allowed for students to transform and assimilate
new knowledge by utilizing reflective observation to create abstract
conceptualization.
3.4 | Measures
3.4.1 | Motivational interviewing knowledge and
attitude test
Motivationalinterviewing knowledge and attitude test (MIKAT) is a
measurement tool that assesses MI knowledge and beliefs consistent
with the spirit of MI. The tool is useful for measuring changes in
attitudes and knowledge regarding MIbefore and after an educa-
tionalintervention.The MIKAT is a quiz consisting of 19 questions:
10 true‐false questions about addiction myths; four questions about
MI‐consistent attitudes and assumptions;and five questions about
counseling behaviors consistentwith an MI approach.Scoring is
based upon calculating the number of correct answers given by the
subject then dividing by 19 (the totalnumber ofcorrect answers
possible). Scoring is divided into subcomponentsthat include
CHANG ET AL. | 683
setting and the SP simulation took place within the simulation
center of the University.Approval for this study was obtained by
the University’s InstitutionalReview Board.
3.2 | Didactic lecture and role play
The MI lecture and role‐playing scenario were developed by two
experts who have experience in utilizing MI in research,education,
and clinicalpractice.Materials used for the didactic lecture were
taken in part from the Motivational Interviewing Network of
Trainers,an organization designed to promote research and training
of MI. Other materials were obtained from a thorough review of the
current literature on MI training. The didactic lecture includes
content on MI principles,spirit, core skills,techniques,and clinical
applications,as well as barriers to helping patientschange.The
lecture used the example of an older adult who took more
prescription opioids than prescribed.A role‐playing scenario utilizing
that example was demonstrated to students by the research team.
The students were then given similar scenarios and performed role‐
playing by taking turns,acting as both the patient and practitioner.
The research team and course instructorwere available to help
students with MI skills and techniques,provide immediate feedback,
and answer any questions.
3.3 | Simulation preparation and implementation
3.3.1 | Preparation
The SP scenario was developed by an expert panelof psychiatric‐
mental health professionals,family nursing practitioners,MI experts,
addiction researchers, experienced educators, and simulation faculty.
The SP simulation involved an older adult patient who was asking for
an early refillof prescription opioid medication that he took for his
chronic pain.The patient had been misusing his opioids by taking
more than prescribed to help with pain and other symptoms.The
patient in the scenario was a recent widower who was becoming
increasingly depressed and was also drinking in excess.He had risk
factors of socialisolation,limited mobility,and unmanaged pain.An
MI lecture was provided to 11 SP who were experienced professional
actors in simulation.A training section was held to promote SP’s
understanding of MIeducation,as well as the simulation scenario.
SP’s training involved a 2‐hour training session that covered topics
including project overview; read‐through and clarification of scenar-
io; role‐playing;trouble‐shooting;appropriate attire and demeanor
(eg body language,disposition,etc) during simulation;a tour of
simulation rooms;and what type of education students were given.
The SPs were expected to study the training materialfor 4 hours
after the training session before the simulation. The SPs also received
a lecture on the basic concepts of MI.A brief meeting with SPs was
held directly before the simulation for a brief review of the training
materials and to answer any questions.
Students were given a briefreview of the simulation process
before the simulation took place.Studentswere encouraged to
review training materials as described in the didactic and role‐play
section.Students were given a PowerPoint lecture on the simulation
process including the SP,space,time duration,and procedure.A
discussion was also held with students to help them understand the
simulation process,expectations,and to address any questions or
concerns.
3.3.2 | Implementation
Students were given 10 minutesto review a door chart that
contained pertinentpatient information thatwould simulate the
type of information a “real‐life” provider may have before a patient
encounter. The door chart contained instructions for students to help
guide them through the simulation.The instructions were very
detailed,as the participants in the study were the first year DNP
students who had not yet taken their clinicalpracticum course,nor
had any prior experience with SP simulation.After the 10‐minute
review, students were prompted to enter the patient room and begin
the encounter.The encounter was limited to 30 minutes.After the
students finished their encounter,they were asked to wait outside
the patient’s door.Then as a group,they were taken to a computer
lab to complete their simulation evaluation.After all, students
completed their evaluation,they were taken into a conference room
for debriefing.Debriefing was facilitated by the research staff and
included reflection and discussion regarding the simulation scenario,
the educationalintervention,and the simulation process.Students
were asked questions such as: what could be done better with regard
to the simulation experience? What aspects of MIwere you most
successfulat demonstratingor would like to strengthen? And
whether or not a participation in the simulation experience helped
better prepare you for implementing MI into your clinicalpractice.
The debriefing session provided an opportunity forstudentsto
critique and reflect on their performance and facilitate learning by
recognizing the knowledge and skills they demonstrated vs those
they did not.This allowed for students to transform and assimilate
new knowledge by utilizing reflective observation to create abstract
conceptualization.
3.4 | Measures
3.4.1 | Motivational interviewing knowledge and
attitude test
Motivationalinterviewing knowledge and attitude test (MIKAT) is a
measurement tool that assesses MI knowledge and beliefs consistent
with the spirit of MI. The tool is useful for measuring changes in
attitudes and knowledge regarding MIbefore and after an educa-
tionalintervention.The MIKAT is a quiz consisting of 19 questions:
10 true‐false questions about addiction myths; four questions about
MI‐consistent attitudes and assumptions;and five questions about
counseling behaviors consistentwith an MI approach.Scoring is
based upon calculating the number of correct answers given by the
subject then dividing by 19 (the totalnumber ofcorrect answers
possible). Scoring is divided into subcomponentsthat include
CHANG ET AL. | 683
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
attitudes consistent with MI, SA myths identified, behaviors
consistent with MI (prescribed behaviors),and behaviors not
consistent with MI (proscribed behaviors).21 Internalconsistency of
the toolhas been documented with a Cronbach’s α of 0.84.22
3.4.2 | Motivational interviewing confidence scale
Because there is no established toolmeasuring confidence for MI,the
research team developed this tool to assess the student’s confidence in
understanding and performing MI.The development ofthis tool was
through a review of literature by a group of clinicians and educators who
have expertise in motivational interviewing.The tool was also reviewed
by a panel of researchers and clinicians for content validity. A total of 10
questions were developed to measure how confident students are in
their ability to use MI techniques including express empathy; elicit/evoke
change talk; engage in reflective listening; assess the stage of change; use
the readiness to change ruler,and apply MI in clinical practice.The tool
utilizesa five‐pointLikert scale thatrangesfrom one, being “very
confident”,to five,being “very not confident”.
3.4.3 | Behavior change counseling index
Behavior change counseling index (BECCI) is a tool assessing skills in MI
counseling and has been widely utilized in previous studies.BECCI
includes 11 items that measure the counselor’s MI skills using a five‐point
scale with zero beings “did notdemonstrate atall” and four being
“demonstrated with a greatextent.”The tool aims to focus on the
counselor’s behavior and attitude rather than patient response. While the
internalconsistency is low,this toolhas demonstrated high inter‐rater
reliability with a moderate levelof reliability across time,as wellas a
moderatesensitivityto observe the change in the interviewer’s
performance.23 Score is reported as a mean score (totalscore for all
11 items/11).The tool also assesses how often the counselor spoke,
whether it is “more than half the time”, “about half the time”, or “less than
half the time.” The MI counseling is collaborative and the patient is an
active and engaged participant.The counselor uses MI skills to explore
the patient’s feelings about behavior changes and encourage them to
make their own decisions about change by verbally expressing their
feelings and attitudes. Ideally, the counselor should be speaking less than
50% of the time.
3.5 | Demographic survey
The data collected included:age; sex; race; enrollmentstatus;
specialty enrolled in;employment status;years of working experi-
ence;type of nursing experience; current employment setting; work
experience with substance abuse;graduate‐levelcourse content on
substance abuse;and previous education on MI.
3.6 | Data analysis
Data analysis was conducted using the StatisticalPackage for the
SocialSciences (SPSS)software,version 24 (SPSS Inc,Chicago,IL).
Descriptive statistics including mean,range,standard deviation,and
percentage were used to describe the demographic data,as wellas
outcomes regarding MI skills obtained from the BECCI.A one way
repeated analysis of variance was utilized to examine the effect of
the MI education outcome variables,including MI confidence,
knowledge,and attitudes across three‐time points.
4 | RESULTS
All 31 students completed the preintervention and poststandardized
patient assessments.Twenty‐eightparticipantswere female and
three were male.Ages ranged from 21 to 42,with a mean age of 27.
Twenty‐five participants reported full‐time student status while six
reported a part‐time status.Amongst participants,45.2% of them
were in the family nurse practitioner program,19.4% in the adult
nurse practitionerprogram,and 35.5% in the psychiatric nurse
practitioner program. Most participants reported being used full‐time
(54.8%),41.9% reported being used part‐time,and 3.2% reported
being unemployed.Years of nursing experience ranged from 1 to
17 years, with the majority falling in the 1 year of nursing experience
(35.5%),and the second highest being 2 years of experience (22.6%).
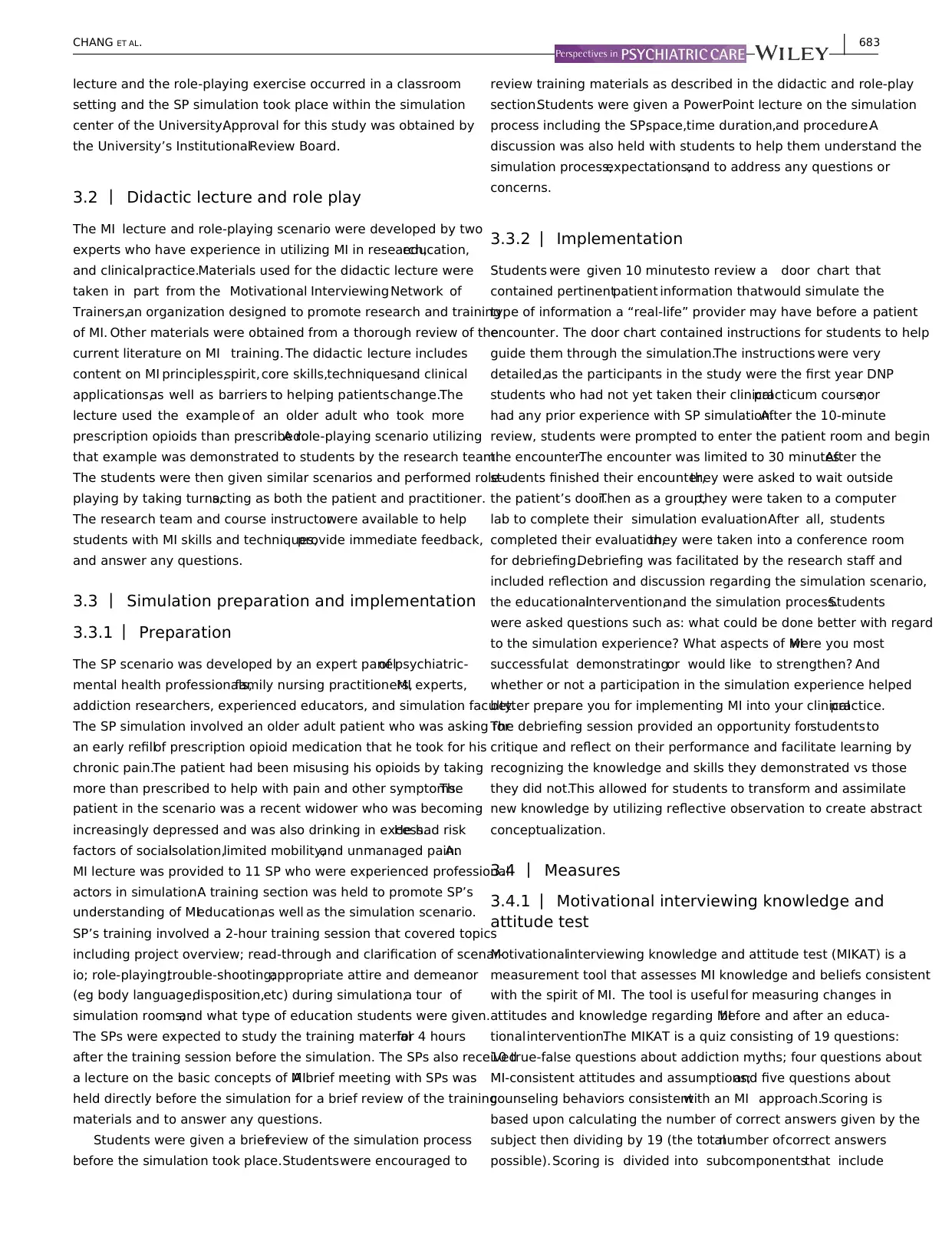
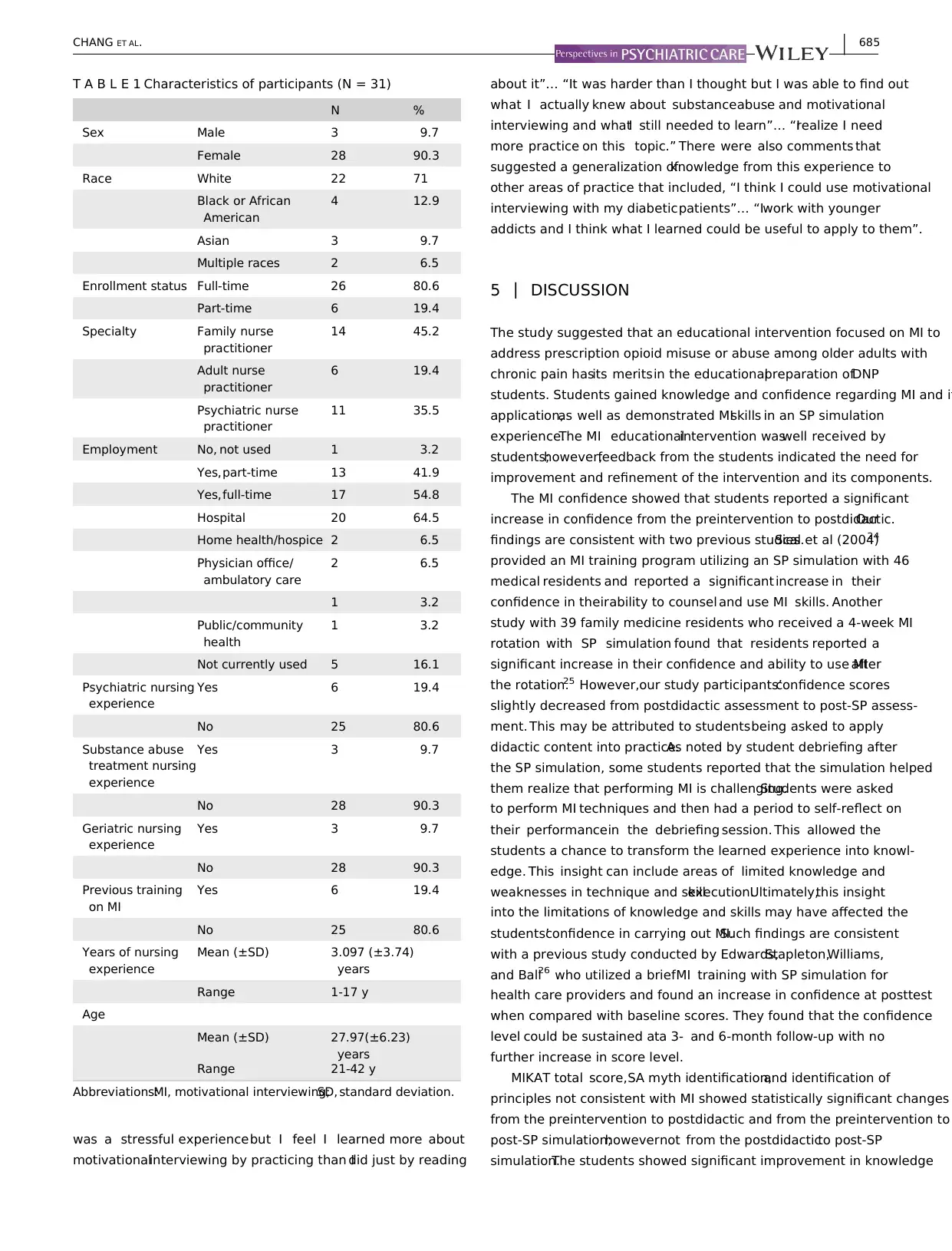
Demographic characteristics are summarized in Table 1.
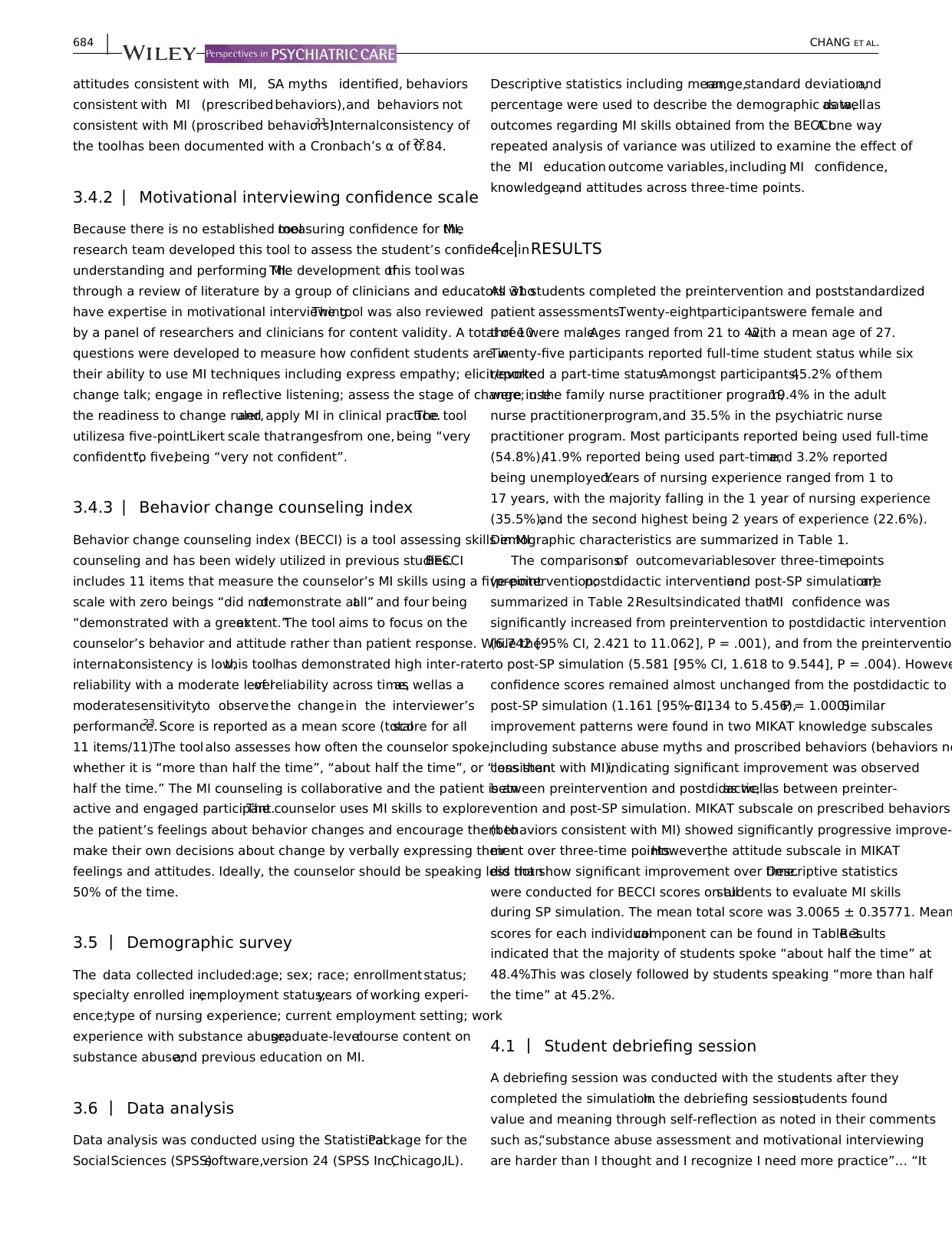
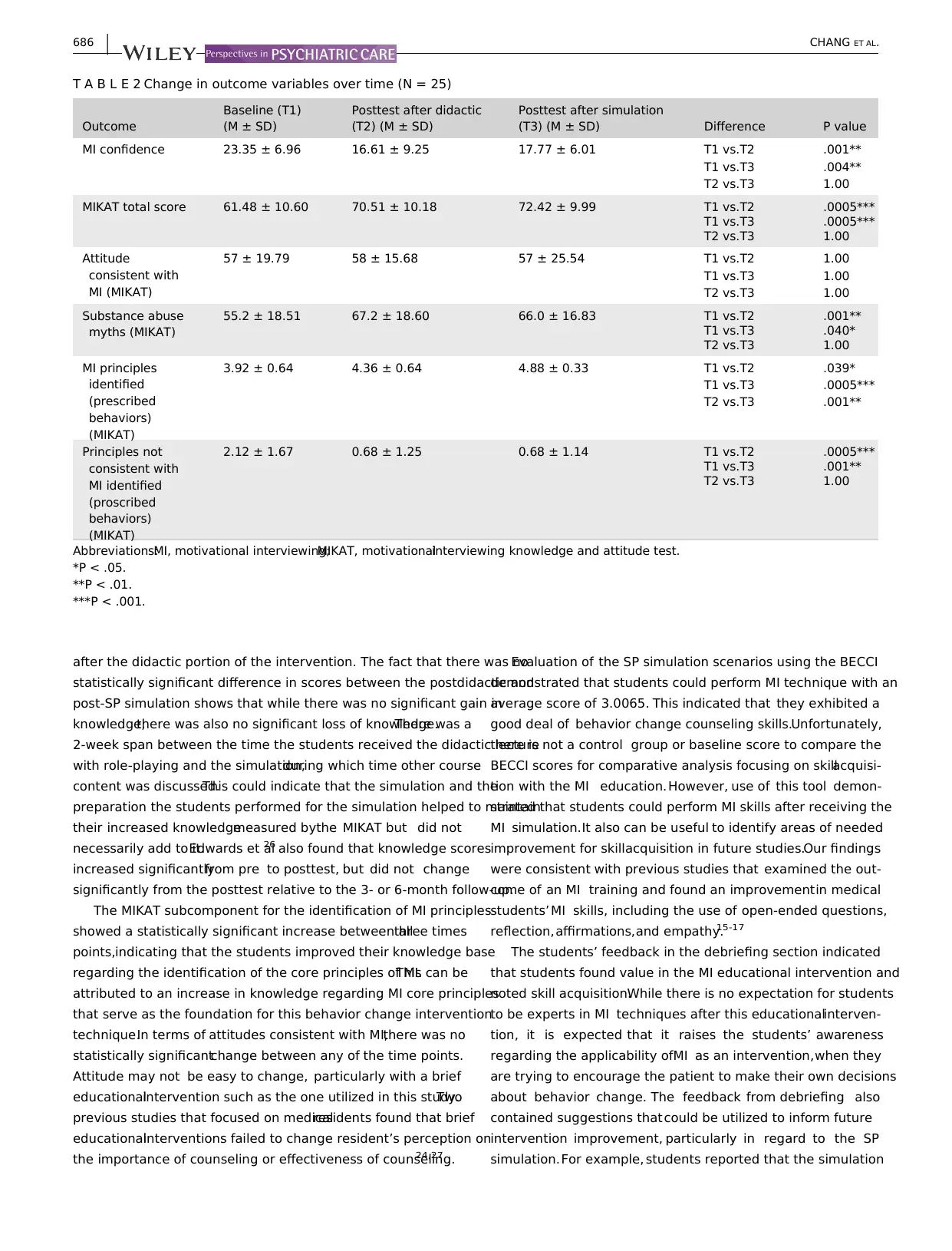
The comparisonsof outcomevariablesover three‐timepoints
(preintervention;postdidactic intervention;and post‐SP simulation)are
summarized in Table 2.Resultsindicated thatMI confidence was
significantly increased from preintervention to postdidactic intervention
(6.742 [95% CI, 2.421 to 11.062], P = .001), and from the preinterventio
to post‐SP simulation (5.581 [95% CI, 1.618 to 9.544], P = .004). Howeve
confidence scores remained almost unchanged from the postdidactic to
post‐SP simulation (1.161 [95% CI,−3.134 to 5.456),P = 1.000).Similar
improvement patterns were found in two MIKAT knowledge subscales
including substance abuse myths and proscribed behaviors (behaviors no
consistent with MI),indicating significant improvement was observed
between preintervention and postdidactic,as wellas between preinter-
vention and post‐SP simulation. MIKAT subscale on prescribed behaviors
(behaviors consistent with MI) showed significantly progressive improve-
ment over three‐time points.However,the attitude subscale in MIKAT
did not show significant improvement over time.Descriptive statistics
were conducted for BECCI scores on allstudents to evaluate MI skills
during SP simulation. The mean total score was 3.0065 ± 0.35771. Mean
scores for each individualcomponent can be found in Table 3.Results
indicated that the majority of students spoke “about half the time” at
48.4%.This was closely followed by students speaking “more than half
the time” at 45.2%.
4.1 | Student debriefing session
A debriefing session was conducted with the students after they
completed the simulation.In the debriefing session,students found
value and meaning through self‐reflection as noted in their comments
such as,“substance abuse assessment and motivational interviewing
are harder than I thought and I recognize I need more practice”… “It
684 | CHANG ET AL.
consistent with MI (prescribed behaviors),and behaviors not
consistent with MI (proscribed behaviors).21 Internalconsistency of
the toolhas been documented with a Cronbach’s α of 0.84.22
3.4.2 | Motivational interviewing confidence scale
Because there is no established toolmeasuring confidence for MI,the
research team developed this tool to assess the student’s confidence in
understanding and performing MI.The development ofthis tool was
through a review of literature by a group of clinicians and educators who
have expertise in motivational interviewing.The tool was also reviewed
by a panel of researchers and clinicians for content validity. A total of 10
questions were developed to measure how confident students are in
their ability to use MI techniques including express empathy; elicit/evoke
change talk; engage in reflective listening; assess the stage of change; use
the readiness to change ruler,and apply MI in clinical practice.The tool
utilizesa five‐pointLikert scale thatrangesfrom one, being “very
confident”,to five,being “very not confident”.
3.4.3 | Behavior change counseling index
Behavior change counseling index (BECCI) is a tool assessing skills in MI
counseling and has been widely utilized in previous studies.BECCI
includes 11 items that measure the counselor’s MI skills using a five‐point
scale with zero beings “did notdemonstrate atall” and four being
“demonstrated with a greatextent.”The tool aims to focus on the
counselor’s behavior and attitude rather than patient response. While the
internalconsistency is low,this toolhas demonstrated high inter‐rater
reliability with a moderate levelof reliability across time,as wellas a
moderatesensitivityto observe the change in the interviewer’s
performance.23 Score is reported as a mean score (totalscore for all
11 items/11).The tool also assesses how often the counselor spoke,
whether it is “more than half the time”, “about half the time”, or “less than
half the time.” The MI counseling is collaborative and the patient is an
active and engaged participant.The counselor uses MI skills to explore
the patient’s feelings about behavior changes and encourage them to
make their own decisions about change by verbally expressing their
feelings and attitudes. Ideally, the counselor should be speaking less than
50% of the time.
3.5 | Demographic survey
The data collected included:age; sex; race; enrollmentstatus;
specialty enrolled in;employment status;years of working experi-
ence;type of nursing experience; current employment setting; work
experience with substance abuse;graduate‐levelcourse content on
substance abuse;and previous education on MI.
3.6 | Data analysis
Data analysis was conducted using the StatisticalPackage for the
SocialSciences (SPSS)software,version 24 (SPSS Inc,Chicago,IL).
Descriptive statistics including mean,range,standard deviation,and
percentage were used to describe the demographic data,as wellas
outcomes regarding MI skills obtained from the BECCI.A one way
repeated analysis of variance was utilized to examine the effect of
the MI education outcome variables,including MI confidence,
knowledge,and attitudes across three‐time points.
4 | RESULTS
All 31 students completed the preintervention and poststandardized
patient assessments.Twenty‐eightparticipantswere female and
three were male.Ages ranged from 21 to 42,with a mean age of 27.
Twenty‐five participants reported full‐time student status while six
reported a part‐time status.Amongst participants,45.2% of them
were in the family nurse practitioner program,19.4% in the adult
nurse practitionerprogram,and 35.5% in the psychiatric nurse
practitioner program. Most participants reported being used full‐time
(54.8%),41.9% reported being used part‐time,and 3.2% reported
being unemployed.Years of nursing experience ranged from 1 to
17 years, with the majority falling in the 1 year of nursing experience
(35.5%),and the second highest being 2 years of experience (22.6%).
Demographic characteristics are summarized in Table 1.
The comparisonsof outcomevariablesover three‐timepoints
(preintervention;postdidactic intervention;and post‐SP simulation)are
summarized in Table 2.Resultsindicated thatMI confidence was
significantly increased from preintervention to postdidactic intervention
(6.742 [95% CI, 2.421 to 11.062], P = .001), and from the preinterventio
to post‐SP simulation (5.581 [95% CI, 1.618 to 9.544], P = .004). Howeve
confidence scores remained almost unchanged from the postdidactic to
post‐SP simulation (1.161 [95% CI,−3.134 to 5.456),P = 1.000).Similar
improvement patterns were found in two MIKAT knowledge subscales
including substance abuse myths and proscribed behaviors (behaviors no
consistent with MI),indicating significant improvement was observed
between preintervention and postdidactic,as wellas between preinter-
vention and post‐SP simulation. MIKAT subscale on prescribed behaviors
(behaviors consistent with MI) showed significantly progressive improve-
ment over three‐time points.However,the attitude subscale in MIKAT
did not show significant improvement over time.Descriptive statistics
were conducted for BECCI scores on allstudents to evaluate MI skills
during SP simulation. The mean total score was 3.0065 ± 0.35771. Mean
scores for each individualcomponent can be found in Table 3.Results
indicated that the majority of students spoke “about half the time” at
48.4%.This was closely followed by students speaking “more than half
the time” at 45.2%.
4.1 | Student debriefing session
A debriefing session was conducted with the students after they
completed the simulation.In the debriefing session,students found
value and meaning through self‐reflection as noted in their comments
such as,“substance abuse assessment and motivational interviewing
are harder than I thought and I recognize I need more practice”… “It
684 | CHANG ET AL.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
was a stressful experiencebut I feel I learned more about
motivationalinterviewing by practicing than Idid just by reading
about it”… “It was harder than I thought but I was able to find out
what I actually knew about substanceabuse and motivational
interviewing and whatI still needed to learn”… “Irealize I need
more practice on this topic.” There were also comments that
suggested a generalization ofknowledge from this experience to
other areas of practice that included, “I think I could use motivational
interviewing with my diabeticpatients”… “Iwork with younger
addicts and I think what I learned could be useful to apply to them”.
5 | DISCUSSION
The study suggested that an educational intervention focused on MI to
address prescription opioid misuse or abuse among older adults with
chronic pain hasits meritsin the educationalpreparation ofDNP
students. Students gained knowledge and confidence regarding MI and it
application,as well as demonstrated MIskills in an SP simulation
experience.The MI educationalintervention waswell received by
students;however,feedback from the students indicated the need for
improvement and refinement of the intervention and its components.
The MI confidence showed that students reported a significant
increase in confidence from the preintervention to postdidactic.Our
findings are consistent with two previous studies.Scal et al (2004)24
provided an MI training program utilizing an SP simulation with 46
medical residents and reported a significant increase in their
confidence in theirability to counsel and use MI skills. Another
study with 39 family medicine residents who received a 4‐week MI
rotation with SP simulation found that residents reported a
significant increase in their confidence and ability to use MIafter
the rotation.25 However,our study participants’confidence scores
slightly decreased from postdidactic assessment to post‐SP assess-
ment. This may be attributed to studentsbeing asked to apply
didactic content into practice.As noted by student debriefing after
the SP simulation, some students reported that the simulation helped
them realize that performing MI is challenging.Students were asked
to perform MI techniques and then had a period to self‐reflect on
their performancein the debriefing session. This allowed the
students a chance to transform the learned experience into knowl-
edge. This insight can include areas of limited knowledge and
weaknesses in technique and skillexecution.Ultimately,this insight
into the limitations of knowledge and skills may have affected the
students’confidence in carrying out MI.Such findings are consistent
with a previous study conducted by Edwards,Stapleton,Williams,
and Ball26 who utilized a briefMI training with SP simulation for
health care providers and found an increase in confidence at posttest
when compared with baseline scores. They found that the confidence
level could be sustained ata 3‐ and 6‐month follow‐up with no
further increase in score level.
MIKAT total score,SA myth identification,and identification of
principles not consistent with MI showed statistically significant changes
from the preintervention to postdidactic and from the preintervention to
post‐SP simulation;howevernot from the postdidacticto post‐SP
simulation.The students showed significant improvement in knowledge
T A B L E 1 Characteristics of participants (N = 31)
N %
Sex Male 3 9.7
Female 28 90.3
Race White 22 71
Black or African
American
4 12.9
Asian 3 9.7
Multiple races 2 6.5
Enrollment status Full‐time 26 80.6
Part‐time 6 19.4
Specialty Family nurse
practitioner
14 45.2
Adult nurse
practitioner
6 19.4
Psychiatric nurse
practitioner
11 35.5
Employment No, not used 1 3.2
Yes,part‐time 13 41.9
Yes,full‐time 17 54.8
Hospital 20 64.5
Home health/hospice 2 6.5
Physician office/
ambulatory care
2 6.5
1 3.2
Public/community
health
1 3.2
Not currently used 5 16.1
Psychiatric nursing
experience
Yes 6 19.4
No 25 80.6
Substance abuse
treatment nursing
experience
Yes 3 9.7
No 28 90.3
Geriatric nursing
experience
Yes 3 9.7
No 28 90.3
Previous training
on MI
Yes 6 19.4
No 25 80.6
Years of nursing
experience
Mean (±SD) 3.097 (±3.74)
years
Range 1‐17 y
Age
Mean (±SD) 27.97(±6.23)
years
Range 21‐42 y
Abbreviations:MI, motivational interviewing;SD, standard deviation.
CHANG ET AL. | 685
motivationalinterviewing by practicing than Idid just by reading
about it”… “It was harder than I thought but I was able to find out
what I actually knew about substanceabuse and motivational
interviewing and whatI still needed to learn”… “Irealize I need
more practice on this topic.” There were also comments that
suggested a generalization ofknowledge from this experience to
other areas of practice that included, “I think I could use motivational
interviewing with my diabeticpatients”… “Iwork with younger
addicts and I think what I learned could be useful to apply to them”.
5 | DISCUSSION
The study suggested that an educational intervention focused on MI to
address prescription opioid misuse or abuse among older adults with
chronic pain hasits meritsin the educationalpreparation ofDNP
students. Students gained knowledge and confidence regarding MI and it
application,as well as demonstrated MIskills in an SP simulation
experience.The MI educationalintervention waswell received by
students;however,feedback from the students indicated the need for
improvement and refinement of the intervention and its components.
The MI confidence showed that students reported a significant
increase in confidence from the preintervention to postdidactic.Our
findings are consistent with two previous studies.Scal et al (2004)24
provided an MI training program utilizing an SP simulation with 46
medical residents and reported a significant increase in their
confidence in theirability to counsel and use MI skills. Another
study with 39 family medicine residents who received a 4‐week MI
rotation with SP simulation found that residents reported a
significant increase in their confidence and ability to use MIafter
the rotation.25 However,our study participants’confidence scores
slightly decreased from postdidactic assessment to post‐SP assess-
ment. This may be attributed to studentsbeing asked to apply
didactic content into practice.As noted by student debriefing after
the SP simulation, some students reported that the simulation helped
them realize that performing MI is challenging.Students were asked
to perform MI techniques and then had a period to self‐reflect on
their performancein the debriefing session. This allowed the
students a chance to transform the learned experience into knowl-
edge. This insight can include areas of limited knowledge and
weaknesses in technique and skillexecution.Ultimately,this insight
into the limitations of knowledge and skills may have affected the
students’confidence in carrying out MI.Such findings are consistent
with a previous study conducted by Edwards,Stapleton,Williams,
and Ball26 who utilized a briefMI training with SP simulation for
health care providers and found an increase in confidence at posttest
when compared with baseline scores. They found that the confidence
level could be sustained ata 3‐ and 6‐month follow‐up with no
further increase in score level.
MIKAT total score,SA myth identification,and identification of
principles not consistent with MI showed statistically significant changes
from the preintervention to postdidactic and from the preintervention to
post‐SP simulation;howevernot from the postdidacticto post‐SP
simulation.The students showed significant improvement in knowledge
T A B L E 1 Characteristics of participants (N = 31)
N %
Sex Male 3 9.7
Female 28 90.3
Race White 22 71
Black or African
American
4 12.9
Asian 3 9.7
Multiple races 2 6.5
Enrollment status Full‐time 26 80.6
Part‐time 6 19.4
Specialty Family nurse
practitioner
14 45.2
Adult nurse
practitioner
6 19.4
Psychiatric nurse
practitioner
11 35.5
Employment No, not used 1 3.2
Yes,part‐time 13 41.9
Yes,full‐time 17 54.8
Hospital 20 64.5
Home health/hospice 2 6.5
Physician office/
ambulatory care
2 6.5
1 3.2
Public/community
health
1 3.2
Not currently used 5 16.1
Psychiatric nursing
experience
Yes 6 19.4
No 25 80.6
Substance abuse
treatment nursing
experience
Yes 3 9.7
No 28 90.3
Geriatric nursing
experience
Yes 3 9.7
No 28 90.3
Previous training
on MI
Yes 6 19.4
No 25 80.6
Years of nursing
experience
Mean (±SD) 3.097 (±3.74)
years
Range 1‐17 y
Age
Mean (±SD) 27.97(±6.23)
years
Range 21‐42 y
Abbreviations:MI, motivational interviewing;SD, standard deviation.
CHANG ET AL. | 685
after the didactic portion of the intervention. The fact that there was no
statistically significant difference in scores between the postdidactic and
post‐SP simulation shows that while there was no significant gain in
knowledge,there was also no significant loss of knowledge.There was a
2‐week span between the time the students received the didactic lecture
with role‐playing and the simulation,during which time other course
content was discussed.This could indicate that the simulation and the
preparation the students performed for the simulation helped to maintain
their increased knowledgemeasured bythe MIKAT but did not
necessarily add to it.Edwards et al26 also found that knowledge scores
increased significantlyfrom pre to posttest, but did not change
significantly from the posttest relative to the 3‐ or 6‐month follow‐up.
The MIKAT subcomponent for the identification of MI principles
showed a statistically significant increase between allthree times
points,indicating that the students improved their knowledge base
regarding the identification of the core principles of MI.This can be
attributed to an increase in knowledge regarding MI core principles
that serve as the foundation for this behavior change intervention
technique.In terms of attitudes consistent with MI,there was no
statistically significantchange between any of the time points.
Attitude may not be easy to change, particularly with a brief
educationalintervention such as the one utilized in this study.Two
previous studies that focused on medicalresidents found that brief
educationalinterventions failed to change resident’s perception on
the importance of counseling or effectiveness of counseling.24,27
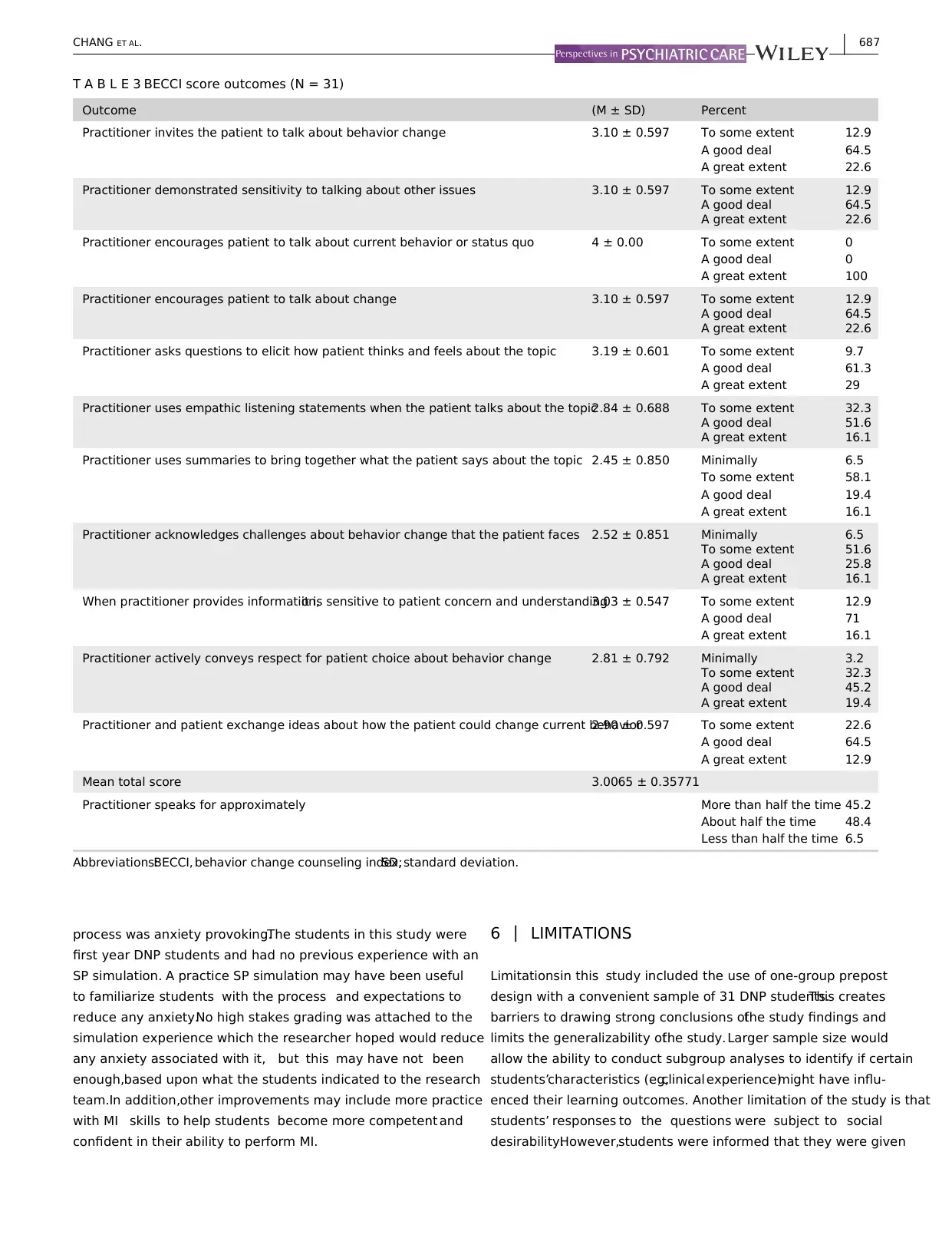
Evaluation of the SP simulation scenarios using the BECCI
demonstrated that students could perform MI technique with an
average score of 3.0065. This indicated that they exhibited a
good deal of behavior change counseling skills.Unfortunately,
there is not a control group or baseline score to compare the
BECCI scores for comparative analysis focusing on skillacquisi-
tion with the MI education. However, use of this tool demon-
strated that students could perform MI skills after receiving the
MI simulation.It also can be useful to identify areas of needed
improvement for skillacquisition in future studies.Our findings
were consistent with previous studies that examined the out-
come of an MI training and found an improvementin medical
students’ MI skills, including the use of open‐ended questions,
reflection,affirmations,and empathy.15-17
The students’ feedback in the debriefing section indicated
that students found value in the MI educational intervention and
noted skill acquisition.While there is no expectation for students
to be experts in MI techniques after this educationalinterven-
tion, it is expected that it raises the students’ awareness
regarding the applicability ofMI as an intervention,when they
are trying to encourage the patient to make their own decisions
about behavior change. The feedback from debriefing also
contained suggestions that could be utilized to inform future
intervention improvement, particularly in regard to the SP
simulation.For example, students reported that the simulation
T A B L E 2 Change in outcome variables over time (N = 25)
Outcome
Baseline (T1)
(M ± SD)
Posttest after didactic
(T2) (M ± SD)
Posttest after simulation
(T3) (M ± SD) Difference P value
MI confidence 23.35 ± 6.96 16.61 ± 9.25 17.77 ± 6.01 T1 vs.T2 .001**
T1 vs.T3 .004**
T2 vs.T3 1.00
MIKAT total score 61.48 ± 10.60 70.51 ± 10.18 72.42 ± 9.99 T1 vs.T2 .0005***
T1 vs.T3 .0005***
T2 vs.T3 1.00
Attitude
consistent with
MI (MIKAT)
57 ± 19.79 58 ± 15.68 57 ± 25.54 T1 vs.T2 1.00
T1 vs.T3 1.00
T2 vs.T3 1.00
Substance abuse
myths (MIKAT)
55.2 ± 18.51 67.2 ± 18.60 66.0 ± 16.83 T1 vs.T2 .001**
T1 vs.T3 .040*
T2 vs.T3 1.00
MI principles
identified
(prescribed
behaviors)
(MIKAT)
3.92 ± 0.64 4.36 ± 0.64 4.88 ± 0.33 T1 vs.T2 .039*
T1 vs.T3 .0005***
T2 vs.T3 .001**
Principles not
consistent with
MI identified
(proscribed
behaviors)
(MIKAT)
2.12 ± 1.67 0.68 ± 1.25 0.68 ± 1.14 T1 vs.T2 .0005***
T1 vs.T3 .001**
T2 vs.T3 1.00
Abbreviations:MI, motivational interviewing;MIKAT, motivationalinterviewing knowledge and attitude test.
*P < .05.
**P < .01.
***P < .001.
686 | CHANG ET AL.
statistically significant difference in scores between the postdidactic and
post‐SP simulation shows that while there was no significant gain in
knowledge,there was also no significant loss of knowledge.There was a
2‐week span between the time the students received the didactic lecture
with role‐playing and the simulation,during which time other course
content was discussed.This could indicate that the simulation and the
preparation the students performed for the simulation helped to maintain
their increased knowledgemeasured bythe MIKAT but did not
necessarily add to it.Edwards et al26 also found that knowledge scores
increased significantlyfrom pre to posttest, but did not change
significantly from the posttest relative to the 3‐ or 6‐month follow‐up.
The MIKAT subcomponent for the identification of MI principles
showed a statistically significant increase between allthree times
points,indicating that the students improved their knowledge base
regarding the identification of the core principles of MI.This can be
attributed to an increase in knowledge regarding MI core principles
that serve as the foundation for this behavior change intervention
technique.In terms of attitudes consistent with MI,there was no
statistically significantchange between any of the time points.
Attitude may not be easy to change, particularly with a brief
educationalintervention such as the one utilized in this study.Two
previous studies that focused on medicalresidents found that brief
educationalinterventions failed to change resident’s perception on
the importance of counseling or effectiveness of counseling.24,27
Evaluation of the SP simulation scenarios using the BECCI
demonstrated that students could perform MI technique with an
average score of 3.0065. This indicated that they exhibited a
good deal of behavior change counseling skills.Unfortunately,
there is not a control group or baseline score to compare the
BECCI scores for comparative analysis focusing on skillacquisi-
tion with the MI education. However, use of this tool demon-
strated that students could perform MI skills after receiving the
MI simulation.It also can be useful to identify areas of needed
improvement for skillacquisition in future studies.Our findings
were consistent with previous studies that examined the out-
come of an MI training and found an improvementin medical
students’ MI skills, including the use of open‐ended questions,
reflection,affirmations,and empathy.15-17
The students’ feedback in the debriefing section indicated
that students found value in the MI educational intervention and
noted skill acquisition.While there is no expectation for students
to be experts in MI techniques after this educationalinterven-
tion, it is expected that it raises the students’ awareness
regarding the applicability ofMI as an intervention,when they
are trying to encourage the patient to make their own decisions
about behavior change. The feedback from debriefing also
contained suggestions that could be utilized to inform future
intervention improvement, particularly in regard to the SP
simulation.For example, students reported that the simulation
T A B L E 2 Change in outcome variables over time (N = 25)
Outcome
Baseline (T1)
(M ± SD)
Posttest after didactic
(T2) (M ± SD)
Posttest after simulation
(T3) (M ± SD) Difference P value
MI confidence 23.35 ± 6.96 16.61 ± 9.25 17.77 ± 6.01 T1 vs.T2 .001**
T1 vs.T3 .004**
T2 vs.T3 1.00
MIKAT total score 61.48 ± 10.60 70.51 ± 10.18 72.42 ± 9.99 T1 vs.T2 .0005***
T1 vs.T3 .0005***
T2 vs.T3 1.00
Attitude
consistent with
MI (MIKAT)
57 ± 19.79 58 ± 15.68 57 ± 25.54 T1 vs.T2 1.00
T1 vs.T3 1.00
T2 vs.T3 1.00
Substance abuse
myths (MIKAT)
55.2 ± 18.51 67.2 ± 18.60 66.0 ± 16.83 T1 vs.T2 .001**
T1 vs.T3 .040*
T2 vs.T3 1.00
MI principles
identified
(prescribed
behaviors)
(MIKAT)
3.92 ± 0.64 4.36 ± 0.64 4.88 ± 0.33 T1 vs.T2 .039*
T1 vs.T3 .0005***
T2 vs.T3 .001**
Principles not
consistent with
MI identified
(proscribed
behaviors)
(MIKAT)
2.12 ± 1.67 0.68 ± 1.25 0.68 ± 1.14 T1 vs.T2 .0005***
T1 vs.T3 .001**
T2 vs.T3 1.00
Abbreviations:MI, motivational interviewing;MIKAT, motivationalinterviewing knowledge and attitude test.
*P < .05.
**P < .01.
***P < .001.
686 | CHANG ET AL.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
process was anxiety provoking.The students in this study were
first year DNP students and had no previous experience with an
SP simulation. A practice SP simulation may have been useful
to familiarize students with the process and expectations to
reduce any anxiety.No high stakes grading was attached to the
simulation experience which the researcher hoped would reduce
any anxiety associated with it, but this may have not been
enough,based upon what the students indicated to the research
team.In addition,other improvements may include more practice
with MI skills to help students become more competent and
confident in their ability to perform MI.
6 | LIMITATIONS
Limitationsin this study included the use of one‐group prepost
design with a convenient sample of 31 DNP students.This creates
barriers to drawing strong conclusions ofthe study findings and
limits the generalizability ofthe study.Larger sample size would
allow the ability to conduct subgroup analyses to identify if certain
students’characteristics (eg,clinical experience)might have influ-
enced their learning outcomes. Another limitation of the study is that
students’ responses to the questions were subject to social
desirability.However,students were informed that they were given
T A B L E 3 BECCI score outcomes (N = 31)
Outcome (M ± SD) Percent
Practitioner invites the patient to talk about behavior change 3.10 ± 0.597 To some extent 12.9
A good deal 64.5
A great extent 22.6
Practitioner demonstrated sensitivity to talking about other issues 3.10 ± 0.597 To some extent 12.9
A good deal 64.5
A great extent 22.6
Practitioner encourages patient to talk about current behavior or status quo 4 ± 0.00 To some extent 0
A good deal 0
A great extent 100
Practitioner encourages patient to talk about change 3.10 ± 0.597 To some extent 12.9
A good deal 64.5
A great extent 22.6
Practitioner asks questions to elicit how patient thinks and feels about the topic 3.19 ± 0.601 To some extent 9.7
A good deal 61.3
A great extent 29
Practitioner uses empathic listening statements when the patient talks about the topic2.84 ± 0.688 To some extent 32.3
A good deal 51.6
A great extent 16.1
Practitioner uses summaries to bring together what the patient says about the topic 2.45 ± 0.850 Minimally 6.5
To some extent 58.1
A good deal 19.4
A great extent 16.1
Practitioner acknowledges challenges about behavior change that the patient faces 2.52 ± 0.851 Minimally 6.5
To some extent 51.6
A good deal 25.8
A great extent 16.1
When practitioner provides information,it is sensitive to patient concern and understanding3.03 ± 0.547 To some extent 12.9
A good deal 71
A great extent 16.1
Practitioner actively conveys respect for patient choice about behavior change 2.81 ± 0.792 Minimally 3.2
To some extent 32.3
A good deal 45.2
A great extent 19.4
Practitioner and patient exchange ideas about how the patient could change current behavior2.90 ± 0.597 To some extent 22.6
A good deal 64.5
A great extent 12.9
Mean total score 3.0065 ± 0.35771
Practitioner speaks for approximately More than half the time 45.2
About half the time 48.4
Less than half the time 6.5
Abbreviations:BECCI, behavior change counseling index;SD, standard deviation.
CHANG ET AL. | 687
first year DNP students and had no previous experience with an
SP simulation. A practice SP simulation may have been useful
to familiarize students with the process and expectations to
reduce any anxiety.No high stakes grading was attached to the
simulation experience which the researcher hoped would reduce
any anxiety associated with it, but this may have not been
enough,based upon what the students indicated to the research
team.In addition,other improvements may include more practice
with MI skills to help students become more competent and
confident in their ability to perform MI.
6 | LIMITATIONS
Limitationsin this study included the use of one‐group prepost
design with a convenient sample of 31 DNP students.This creates
barriers to drawing strong conclusions ofthe study findings and
limits the generalizability ofthe study.Larger sample size would
allow the ability to conduct subgroup analyses to identify if certain
students’characteristics (eg,clinical experience)might have influ-
enced their learning outcomes. Another limitation of the study is that
students’ responses to the questions were subject to social
desirability.However,students were informed that they were given
T A B L E 3 BECCI score outcomes (N = 31)
Outcome (M ± SD) Percent
Practitioner invites the patient to talk about behavior change 3.10 ± 0.597 To some extent 12.9
A good deal 64.5
A great extent 22.6
Practitioner demonstrated sensitivity to talking about other issues 3.10 ± 0.597 To some extent 12.9
A good deal 64.5
A great extent 22.6
Practitioner encourages patient to talk about current behavior or status quo 4 ± 0.00 To some extent 0
A good deal 0
A great extent 100
Practitioner encourages patient to talk about change 3.10 ± 0.597 To some extent 12.9
A good deal 64.5
A great extent 22.6
Practitioner asks questions to elicit how patient thinks and feels about the topic 3.19 ± 0.601 To some extent 9.7
A good deal 61.3
A great extent 29
Practitioner uses empathic listening statements when the patient talks about the topic2.84 ± 0.688 To some extent 32.3
A good deal 51.6
A great extent 16.1
Practitioner uses summaries to bring together what the patient says about the topic 2.45 ± 0.850 Minimally 6.5
To some extent 58.1
A good deal 19.4
A great extent 16.1
Practitioner acknowledges challenges about behavior change that the patient faces 2.52 ± 0.851 Minimally 6.5
To some extent 51.6
A good deal 25.8
A great extent 16.1
When practitioner provides information,it is sensitive to patient concern and understanding3.03 ± 0.547 To some extent 12.9
A good deal 71
A great extent 16.1
Practitioner actively conveys respect for patient choice about behavior change 2.81 ± 0.792 Minimally 3.2
To some extent 32.3
A good deal 45.2
A great extent 19.4
Practitioner and patient exchange ideas about how the patient could change current behavior2.90 ± 0.597 To some extent 22.6
A good deal 64.5
A great extent 12.9
Mean total score 3.0065 ± 0.35771
Practitioner speaks for approximately More than half the time 45.2
About half the time 48.4
Less than half the time 6.5
Abbreviations:BECCI, behavior change counseling index;SD, standard deviation.
CHANG ET AL. | 687
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
full credit for the SP simulation if they participated and put forth a
good effort. This also helped to reduce social desirability bias. Finally,
our study did not examine students’ knowledge and attitudes toward
older adults with opioid abuse as outcomes of MItraining.Future
research should incorporate knowledge and attitude measures as
training outcomes.
7 | CONCLUSION
This study demonstrated that an MIeducation can successfully
be implemented into a DNP curriculum with promising results in
improving student’s knowledge and confidence, as well as
demonstrating skill acquisition. This study showed that the SP
simulation is a promising format to educate students on
behavioral interventions like MI, by allowing them to interact
with a real patient in a safe and supervised setting.Even with the
limitations of the study, there were valuable findings that
supported the implementation of MI education for DNP students.
ACKNOWLEDGMENT
The study was funded by the Health Foundation for Western and
Central New York (grant no.870‐12).
CONFLICT OF INTERESTS
The authors declared that there is no conflict of interest.
ORCID
Yu‐Ping Chang http://orcid.org/0000-0003-2328-6876
REFERENCES
1. Chang YP,Compton P.Opioid misuse/abuse and quality persistent pain
management in older adults.J Gerontol Nurs.2016;42(12):21‐30.https://
doi.org/10.3928/00989134‐20161110‐06
2. Olfson M,Wang S,Iza M, Crystal S,Blanco C.National trends in the
office‐based prescription ofschedule II opioids.J Clin Psychiatry.
2013;74(9):932‐939.https://doi.org/10.4088/JCP.13m08349
3. Kalapatapu R,Sullivan M.Prescription use disorder in older adults.
Am J Addict. 2010;19(6):515‐522.https://doi.org/10.1111/j.1521‐
0391.2010.00080.x
4. Chang YP, Compton P. Management ofchronic pain with chronic
opioid therapy in patients with substance use disorders.Addict Sci
Clin Pract.2013;8(1):21.https://doi.org/10.1186/1940‐0640‐8‐21
5. Franklin GM.Opioids for chronic noncancer pain: a position paper of
the American academy of neurology.Neurology.2014;83(14):1277‐
1284.https://doi.org/10.1212/WNL.0000000000000839
6. Substance Abuse and MentalHealth Service Administration (2013).
Results from the 2012 national survey on drug use and health: summary
of national findings.Retrieved from http://www.samhsa.gov/data/
NSDUH/2012summnatfinddettables/nationalfindings/
NSDUHresults2012.htm
7. Chang YP. Factors Associated with Prescription Opioid Misuse in
Adults Aged 50 or Older.Nurs Outlook.2018;66(2):112‐120.https://
doi.org/10.1016/j.outlook.2017.10.007
8. Smedslund G,Berg R, Hammerstrom K,et al. Motivationalinter-
viewing for substance abuse.Cochrane Database Syst Rev.2011;11(5).
https://doi.org/10.1002/14651858.CD008063.pub2
9. Dunhill D, Schmidt S, Klein R. Motivational interviewing interventions
in graduate medicaleducation:a systematic review ofevidence.J
Grad Med Educ.2014;6(2):222‐236.https://doi.org/10.4300/JGME‐
D‐13‐00124.1
10. Cummings S,Cooper R,McClure K.Motivationalinterviewing to affect
behavioralchange in older adults.Res Soc Work Pract.2009;19(2):195‐
204.https://doi.org/10.1177/1049731508320216
11. Blow FC,Bartels SJ,Brockmann LM,Van Citters AD.Evidence‐based
practices for preventing substance abuse and mentalhealth problems in
older adults.Rockville,MD: Substance Abuse and MentalHealth
Services Administration,Older American SubstanceAbuse and
Mental Health TechnicalAssistance Center;2005.
12. Han B, Gfroerer J, Colliver J, Penne M. Substance abuse disorder among
older adults in the United States in 2020.Addiction.2009;104(1):88‐96.
https://doi.org/10.1111/j.1360‐0443.2008.02411.x
13. Miller WR, Rollnick S.MotivationalInterviewing:Preparing people for
change.2nd ed.New York,NY: The Guildford Press;2002.
14. Chang YP,Compton P,Almeter P,Fox C. The effect ofmotivational
interviewing on prescription opioid adherence among older adults with
chronic pain.Perspect Psychiatr Care. 2015;51(3):211‐219. https://doi.org/
10.1111/ppc.12082
15. Haeseler F,Fortin A,Pfeiffer C,Walters C,Martino S.Assessment of
a motivationalinterviewing curriculum for year 3 medicalstudents
using a standardized patient case.Patient Educ Couns.2011;84(1):27‐
30. https://doi.org/10.1016/j.pec.2010.10.029
16. Childers J, Bost J, Kraemer K,et al. Giving residents tools to talk
about behavior change: a motivationalinterviewing curriculum
description and evaluation.Patient Educ Couns.2012;89(2):281‐287.
https://doi.org/10.1016/j.pec.2012.08.001
17. Daeppen J,Fortini C,Bertholet N,et al.Training medical students to
conduct motivationalinterviewing:a randomized controlled trial.
PatientEduc Couns.2012;87(3):313‐318.https://doi.org/10.1016/j.
pec.2011.12.005
18. May W, Park J, Lee K. A ten‐year review of the literature
on the use of standardized patients in teaching and learning.
Medical Teaching.2009;31(6):487‐492.https://doi.org/10.1080/
01421590802530898
19. Oh P, Jeon K, Koh M. The effects ofsimulation‐based learning using
standardized patients in nursing students:a meta‐analysis.Nurse Educ
Today.2015;35(5):e6‐e15.https://doi.org/10.1016/j.nedt.2015.01.019
20. Doolen J,Giddings M,Johnson M,Guizado de Nathan G,Badia L.An
evaluation of mental health simulation with standardized patient.Int
J Nurs Educ Scholarsh.2014;11(1):55‐62.https://doi.org/10.1515/
ijnes‐2013‐0075
21. LeffingwellT. MotivationalInterviewingKnowledgeand Attitude
Test (MIKAT) for evaluation oftraining outcomes.MINUET.2006;
13:10‐11.
22. Doran N, Hohman M, Koutsenok I. Motivational interviewing training
in juvenile corrections: a comparison of outside experts and internal
trainers. Legal and CriminologicalPsychology.2011;18(2):262‐273.
https://doi.org/10.1111/j.2044‐8333.2011.02036.x
23. Lane C,Huws‐Thomas M,Hood K, Rollnick S,Edwards K,Robling
M. Measuring adaptations of motivational interviewing: the
developmentand validation of the behavior change counseling
index (BECCI). Patient Educ Couns.2005;56(2):166‐173.https://
doi.org/10.1016/j.pec.2004.01.003
24. Scal P, Hennrikus D, Ehrlich L, Ireland M, Borowsky I. Preparing residents
to counselabout smoking.Clin Pediatr.2004;43(8):703‐708.https://doi.
org/10.1177/000992280404300803
688 | CHANG ET AL.
good effort. This also helped to reduce social desirability bias. Finally,
our study did not examine students’ knowledge and attitudes toward
older adults with opioid abuse as outcomes of MItraining.Future
research should incorporate knowledge and attitude measures as
training outcomes.
7 | CONCLUSION
This study demonstrated that an MIeducation can successfully
be implemented into a DNP curriculum with promising results in
improving student’s knowledge and confidence, as well as
demonstrating skill acquisition. This study showed that the SP
simulation is a promising format to educate students on
behavioral interventions like MI, by allowing them to interact
with a real patient in a safe and supervised setting.Even with the
limitations of the study, there were valuable findings that
supported the implementation of MI education for DNP students.
ACKNOWLEDGMENT
The study was funded by the Health Foundation for Western and
Central New York (grant no.870‐12).
CONFLICT OF INTERESTS
The authors declared that there is no conflict of interest.
ORCID
Yu‐Ping Chang http://orcid.org/0000-0003-2328-6876
REFERENCES
1. Chang YP,Compton P.Opioid misuse/abuse and quality persistent pain
management in older adults.J Gerontol Nurs.2016;42(12):21‐30.https://
doi.org/10.3928/00989134‐20161110‐06
2. Olfson M,Wang S,Iza M, Crystal S,Blanco C.National trends in the
office‐based prescription ofschedule II opioids.J Clin Psychiatry.
2013;74(9):932‐939.https://doi.org/10.4088/JCP.13m08349
3. Kalapatapu R,Sullivan M.Prescription use disorder in older adults.
Am J Addict. 2010;19(6):515‐522.https://doi.org/10.1111/j.1521‐
0391.2010.00080.x
4. Chang YP, Compton P. Management ofchronic pain with chronic
opioid therapy in patients with substance use disorders.Addict Sci
Clin Pract.2013;8(1):21.https://doi.org/10.1186/1940‐0640‐8‐21
5. Franklin GM.Opioids for chronic noncancer pain: a position paper of
the American academy of neurology.Neurology.2014;83(14):1277‐
1284.https://doi.org/10.1212/WNL.0000000000000839
6. Substance Abuse and MentalHealth Service Administration (2013).
Results from the 2012 national survey on drug use and health: summary
of national findings.Retrieved from http://www.samhsa.gov/data/
NSDUH/2012summnatfinddettables/nationalfindings/
NSDUHresults2012.htm
7. Chang YP. Factors Associated with Prescription Opioid Misuse in
Adults Aged 50 or Older.Nurs Outlook.2018;66(2):112‐120.https://
doi.org/10.1016/j.outlook.2017.10.007
8. Smedslund G,Berg R, Hammerstrom K,et al. Motivationalinter-
viewing for substance abuse.Cochrane Database Syst Rev.2011;11(5).
https://doi.org/10.1002/14651858.CD008063.pub2
9. Dunhill D, Schmidt S, Klein R. Motivational interviewing interventions
in graduate medicaleducation:a systematic review ofevidence.J
Grad Med Educ.2014;6(2):222‐236.https://doi.org/10.4300/JGME‐
D‐13‐00124.1
10. Cummings S,Cooper R,McClure K.Motivationalinterviewing to affect
behavioralchange in older adults.Res Soc Work Pract.2009;19(2):195‐
204.https://doi.org/10.1177/1049731508320216
11. Blow FC,Bartels SJ,Brockmann LM,Van Citters AD.Evidence‐based
practices for preventing substance abuse and mentalhealth problems in
older adults.Rockville,MD: Substance Abuse and MentalHealth
Services Administration,Older American SubstanceAbuse and
Mental Health TechnicalAssistance Center;2005.
12. Han B, Gfroerer J, Colliver J, Penne M. Substance abuse disorder among
older adults in the United States in 2020.Addiction.2009;104(1):88‐96.
https://doi.org/10.1111/j.1360‐0443.2008.02411.x
13. Miller WR, Rollnick S.MotivationalInterviewing:Preparing people for
change.2nd ed.New York,NY: The Guildford Press;2002.
14. Chang YP,Compton P,Almeter P,Fox C. The effect ofmotivational
interviewing on prescription opioid adherence among older adults with
chronic pain.Perspect Psychiatr Care. 2015;51(3):211‐219. https://doi.org/
10.1111/ppc.12082
15. Haeseler F,Fortin A,Pfeiffer C,Walters C,Martino S.Assessment of
a motivationalinterviewing curriculum for year 3 medicalstudents
using a standardized patient case.Patient Educ Couns.2011;84(1):27‐
30. https://doi.org/10.1016/j.pec.2010.10.029
16. Childers J, Bost J, Kraemer K,et al. Giving residents tools to talk
about behavior change: a motivationalinterviewing curriculum
description and evaluation.Patient Educ Couns.2012;89(2):281‐287.
https://doi.org/10.1016/j.pec.2012.08.001
17. Daeppen J,Fortini C,Bertholet N,et al.Training medical students to
conduct motivationalinterviewing:a randomized controlled trial.
PatientEduc Couns.2012;87(3):313‐318.https://doi.org/10.1016/j.
pec.2011.12.005
18. May W, Park J, Lee K. A ten‐year review of the literature
on the use of standardized patients in teaching and learning.
Medical Teaching.2009;31(6):487‐492.https://doi.org/10.1080/
01421590802530898
19. Oh P, Jeon K, Koh M. The effects ofsimulation‐based learning using
standardized patients in nursing students:a meta‐analysis.Nurse Educ
Today.2015;35(5):e6‐e15.https://doi.org/10.1016/j.nedt.2015.01.019
20. Doolen J,Giddings M,Johnson M,Guizado de Nathan G,Badia L.An
evaluation of mental health simulation with standardized patient.Int
J Nurs Educ Scholarsh.2014;11(1):55‐62.https://doi.org/10.1515/
ijnes‐2013‐0075
21. LeffingwellT. MotivationalInterviewingKnowledgeand Attitude
Test (MIKAT) for evaluation oftraining outcomes.MINUET.2006;
13:10‐11.
22. Doran N, Hohman M, Koutsenok I. Motivational interviewing training
in juvenile corrections: a comparison of outside experts and internal
trainers. Legal and CriminologicalPsychology.2011;18(2):262‐273.
https://doi.org/10.1111/j.2044‐8333.2011.02036.x
23. Lane C,Huws‐Thomas M,Hood K, Rollnick S,Edwards K,Robling
M. Measuring adaptations of motivational interviewing: the
developmentand validation of the behavior change counseling
index (BECCI). Patient Educ Couns.2005;56(2):166‐173.https://
doi.org/10.1016/j.pec.2004.01.003
24. Scal P, Hennrikus D, Ehrlich L, Ireland M, Borowsky I. Preparing residents
to counselabout smoking.Clin Pediatr.2004;43(8):703‐708.https://doi.
org/10.1177/000992280404300803
688 | CHANG ET AL.

25. Triana A,Olson M,Trevino D.A new paradigm for teaching behavior
change:implications for residency training in family medicine and
psychiatry.BMC Med Educ.2012;12(1):64.https://doi.org/10.1186/
1472‐6920‐12‐64
26. Edwards E, Stapleton P, Williams K, Ball L. Building
skills, knowledge, and confidence in eating and exercise beh-
avior change:brief motivationalinterviewing training for health-
care providers.Patient Educ Couns.2015;98(5):674‐676.https://
doi.org/10.1016/j.pec.2015.02.006
27. Johns T, Lawrence E, Martini L, Dunn G, Thompson Z,
Zwygart K. Smoking cessation in family medicine:effect of an
area health education center training program. J Grad Med
Educ. 2010;2(2):283‐288. https://doi.org/10.4300/JGME‐D‐10‐
00043.1
How to cite this article: Chang Y‐P,Cassalia J,Warunek M,
Scherer Y.Motivationalinterviewing training with
standardized patient simulation for prescription opioid abuse
among older adults. Perspect Psychiatr Care. 2019;55:681‐689.
https://doi.org/10.1111/ppc.12402
CHANG ET AL. | 689
change:implications for residency training in family medicine and
psychiatry.BMC Med Educ.2012;12(1):64.https://doi.org/10.1186/
1472‐6920‐12‐64
26. Edwards E, Stapleton P, Williams K, Ball L. Building
skills, knowledge, and confidence in eating and exercise beh-
avior change:brief motivationalinterviewing training for health-
care providers.Patient Educ Couns.2015;98(5):674‐676.https://
doi.org/10.1016/j.pec.2015.02.006
27. Johns T, Lawrence E, Martini L, Dunn G, Thompson Z,
Zwygart K. Smoking cessation in family medicine:effect of an
area health education center training program. J Grad Med
Educ. 2010;2(2):283‐288. https://doi.org/10.4300/JGME‐D‐10‐
00043.1
How to cite this article: Chang Y‐P,Cassalia J,Warunek M,
Scherer Y.Motivationalinterviewing training with
standardized patient simulation for prescription opioid abuse
among older adults. Perspect Psychiatr Care. 2019;55:681‐689.
https://doi.org/10.1111/ppc.12402
CHANG ET AL. | 689
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.