Challenges and Opportunities of Free Flaps in Nepal: A Review
VerifiedAdded on 2022/11/25
|7
|5423
|291
Report
AI Summary
This report presents a retrospective cohort study analyzing the first 108 free flap cases performed in Nepal, focusing on the challenges and opportunities within a developing country setting. The study, conducted at Public Health Concern Trust–NEPAL hospitals, reviews patient demographics, indications for surgery (including tumor, trauma, and burns), types of flaps used (radial artery forearm, anterolateral thigh, and free fibular flaps being the most common), hospital stays, complications, and the impact of microsurgery teaching workshops. The findings reveal a flap success rate of approximately 90%, highlighting the feasibility of reconstructive microsurgery with persistent technical support and training programs. The study underscores the importance of such initiatives in improving access to reconstructive services and achieving positive outcomes in resource-limited environments.
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/327340729
Review of the First 108 Free Flaps at Public Health Concern Trust–NEPAL
Hospitals: Challenges and Opportunities in Developing Countries
Article in Annals of Plastic Surgery · August 2018
DOI: 10.1097/SAP.0000000000001583
CITATIONS
0
READS
40
11 authors, including:
Some of the authors of this publication are also working on these related projects:
MicrosurgeryView project
burn surgeryView project
Kiran Nakarmi
Kirtipur Hospital
18PUBLICATIONS19CITATIONS
SEE PROFILE
Bishal Karki
Kathmandu Model Hospital
12PUBLICATIONS30CITATIONS
SEE PROFILE
Review of the First 108 Free Flaps at Public Health Concern Trust–NEPAL
Hospitals: Challenges and Opportunities in Developing Countries
Article in Annals of Plastic Surgery · August 2018
DOI: 10.1097/SAP.0000000000001583
CITATIONS
0
READS
40
11 authors, including:
Some of the authors of this publication are also working on these related projects:
MicrosurgeryView project
burn surgeryView project
Kiran Nakarmi
Kirtipur Hospital
18PUBLICATIONS19CITATIONS
SEE PROFILE
Bishal Karki
Kathmandu Model Hospital
12PUBLICATIONS30CITATIONS
SEE PROFILE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Review of the First 108 Free Flaps at Public Health Conce
Trust–NEPAL Hospitals
Challenges and Opportunities in Developing Countries
Kiran K. Nakarmi, MCh,* Danielle H. Rochlin, MD,† Surendra J. Basnet, MS,* Pramila Sha
Bishal Karki, MCh,* Mangal G. Magar, FCPS,* Krishna K. Nagarkoti, MBBS,*
Pradeep K. Rajbhandari, MD,‡ Devendra Maharjan, MD,‡
Susan S. Prajapati, MD,‡ and Shankar M. Rai, MS*
Background: Free tissue transfer is one of the most important and essential
techniques in reconstructive surgery. The underlying complexity, steep learning
curve, high cost, and fear of failure make it very difficult to establish as a regular
service in developing countries such as Nepal.
Methods: A retrospective cohort study design was used to analyze the challenges
with and opportunities for reconstructive surgery in Nepal. Medical records were
reviewed for patient demographics, indications, types of free flaps, hospital stay,
complications, and involvement of a microsurgery teaching workshop.
Results: A total of 16 microsurgical workshops were carried out by 3 interna-
tional organizations over the study period (2007–2017). Altogether 108 free flaps
in 103 subjects were reviewed during the study period at different hospitals of the
Public Health Concern Trust–NEPAL (phect-NEPAL) and National Trauma Cen-
ter. Of 103 patients, 60 were males and 43 were females with an average age of
34.5 years (range, 8–73 years). The most common indications for microsurgical
reconstruction were tumor, trauma, and burns. Radial artery forearm flap, antero-
lateral thigh flap, and free fibular flap were the most common types of flaps. Ten
different types of flaps were performed. Four cases needed more than 1 flap; one
of them needed 3 flaps. Flap success rate approached 90%. Four patients died in
the hospital postoperatively.
Conclusion: Reconstructive microsurgery is challenging in Nepal and more gen-
erally in developing settings. However, persistent technical support such as train-
ing and workshops can make it feasible.
Key Words: developing country, free flap, microsurgery workshop, Nepal,
reconstructive surgery
(Ann Plast Surg 2018;00: 00–00)
Surgicalconditions constitute 28% to 32% ofglobaldisability-
adjusted life-years.1 Five billion people lack access to basic surgical
services, largely in developing countries.2 Plastic surgery as a specialty
is still in its infancy in the developing world, and there are much fewer
plastic surgeons in these countries.3,4 In addition,conditions thatre-
quire plastic surgical intervention disproportionately affect people from
lower social stratum. As a result, developing countries are often reliant
on plastic surgery teams from outside countries.5,6
In humanitarian plastic surgical initiatives, there has b
from supporting missions to building care centers,which prioritizes
sustainability and builds quantity, capacity, and availability
health care systems through education or financial support.7,8Develop-
ing health care infrastructure involves empowering medical
proving education,training in-country personnel,and constructing
new units,such as cleft centers.9,10Supporting localsurgeons in the
care of their indigent patients is the most cost-effective and
method of increasing access to care.11
Apart from occasional finger and limb replants, regular
surgery has not been a common practice in Nepal. Interplas
and New Zealand (IAN)first visited Kathmandu ModelHospital
(KMH) in 2007 in orderto strengthen microsurgery servicesin
Nepal.Besides this,several regular educationaltrips have been con-
ducted at KMH and later at Kirtipur Hospital with the help of
tions such as the British Foundation for InternationalReconstructive
Surgery and Training (BFIRST) and ReSurge International (RThe
purpose of this study was to review the Nepalese experienc
crosurgical free flap reconstruction in order to demonstrate
of such teaching workshops on access to reconstructive serv
free flap outcomes in Nepal.
METHODS
With institutional review board approval, a retrospectiv
view was performed of all subjects undergoing microsurgica
reconstruction from April2007 to August2017.All cases were per-
formed at KMH and Kirtipur Hospital, working under the umb
Public Health Concern Trust–NEPAL (phect-NEPAL),exceptfor 4
cases at the National Trauma Center. Sixteen microsurgery
were held during the study period.InterplastAustralia and New
Zealand conducted 10 microsurgery workshops, almost onc
with the exception of 3 workshops in 2008 and none in 2013
2016.ReSurge Internationalheld 4 workshops,1 each in 2015 and
2016 and 2 in 2017. The British Foundation for International
structive Surgery and Training held workshops after the ear
2015 and again in 2017.
During workshops, local and visiting surgeons evaluate
together. Local surgeons were encouraged to make diagnos
apeutic plans.Preoperative evaluation included routine hemato
biochemistry, and kidney and liver function tests, in addition
type and cross match, viral markers, chest x-ray, and electr
for patients older than 40 years or younger if indicated. Ima
orthopantomogram,computed tomography scan,or magnetic reso-
nance imaging scan) was done in indicated cases.Angiography was
not performed routinely.
All the surgeries were done under general anesthesia e
cases that had only epidural anesthesia. All the lower extrem
ceived indwelling epidural catheterization for postoperative
Received May 2, 2018, and accepted for publication, after revision June 7, 2018.
From the *Departmentof Burns,Plastic and Reconstructive Surgery,phect-
NEPAL, Kirtipur Hospital,Kathmandu,Nepal;†Division of Plastic and
Reconstructive Surgery,Stanford University Schoolof Medicine,Stanford,
CA; ‡Department of Anesthesiology and Critical Care,phect-NEPAL,Kirtipur
Hospital, Kathmandu, Nepal.
Conflicts of interest and sources of funding: none declared.
Reprints: Kiran K. Nakarmi, MCh, Department of Burns, Plastic and Reconstructive
Surgery, phect-NEPAL, Kirtipur Hospital, Dev Dhoka, Kirtipur,
Kathmandu, Nepal. E-mail: kknakarmi@yahoo.com.
Copyright © 2018 Wolters Kluwer Health, Inc. All rights reserved.
ISSN: 0148-7043/18/0000–0000
DOI: 10.1097/SAP.0000000000001583
MICROSURGERY
Annals of Plastic Surgery• Volume 00, Number 00, Month 2018 www.annalsplasticsurgery.com1
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Trust–NEPAL Hospitals
Challenges and Opportunities in Developing Countries
Kiran K. Nakarmi, MCh,* Danielle H. Rochlin, MD,† Surendra J. Basnet, MS,* Pramila Sha
Bishal Karki, MCh,* Mangal G. Magar, FCPS,* Krishna K. Nagarkoti, MBBS,*
Pradeep K. Rajbhandari, MD,‡ Devendra Maharjan, MD,‡
Susan S. Prajapati, MD,‡ and Shankar M. Rai, MS*
Background: Free tissue transfer is one of the most important and essential
techniques in reconstructive surgery. The underlying complexity, steep learning
curve, high cost, and fear of failure make it very difficult to establish as a regular
service in developing countries such as Nepal.
Methods: A retrospective cohort study design was used to analyze the challenges
with and opportunities for reconstructive surgery in Nepal. Medical records were
reviewed for patient demographics, indications, types of free flaps, hospital stay,
complications, and involvement of a microsurgery teaching workshop.
Results: A total of 16 microsurgical workshops were carried out by 3 interna-
tional organizations over the study period (2007–2017). Altogether 108 free flaps
in 103 subjects were reviewed during the study period at different hospitals of the
Public Health Concern Trust–NEPAL (phect-NEPAL) and National Trauma Cen-
ter. Of 103 patients, 60 were males and 43 were females with an average age of
34.5 years (range, 8–73 years). The most common indications for microsurgical
reconstruction were tumor, trauma, and burns. Radial artery forearm flap, antero-
lateral thigh flap, and free fibular flap were the most common types of flaps. Ten
different types of flaps were performed. Four cases needed more than 1 flap; one
of them needed 3 flaps. Flap success rate approached 90%. Four patients died in
the hospital postoperatively.
Conclusion: Reconstructive microsurgery is challenging in Nepal and more gen-
erally in developing settings. However, persistent technical support such as train-
ing and workshops can make it feasible.
Key Words: developing country, free flap, microsurgery workshop, Nepal,
reconstructive surgery
(Ann Plast Surg 2018;00: 00–00)
Surgicalconditions constitute 28% to 32% ofglobaldisability-
adjusted life-years.1 Five billion people lack access to basic surgical
services, largely in developing countries.2 Plastic surgery as a specialty
is still in its infancy in the developing world, and there are much fewer
plastic surgeons in these countries.3,4 In addition,conditions thatre-
quire plastic surgical intervention disproportionately affect people from
lower social stratum. As a result, developing countries are often reliant
on plastic surgery teams from outside countries.5,6
In humanitarian plastic surgical initiatives, there has b
from supporting missions to building care centers,which prioritizes
sustainability and builds quantity, capacity, and availability
health care systems through education or financial support.7,8Develop-
ing health care infrastructure involves empowering medical
proving education,training in-country personnel,and constructing
new units,such as cleft centers.9,10Supporting localsurgeons in the
care of their indigent patients is the most cost-effective and
method of increasing access to care.11
Apart from occasional finger and limb replants, regular
surgery has not been a common practice in Nepal. Interplas
and New Zealand (IAN)first visited Kathmandu ModelHospital
(KMH) in 2007 in orderto strengthen microsurgery servicesin
Nepal.Besides this,several regular educationaltrips have been con-
ducted at KMH and later at Kirtipur Hospital with the help of
tions such as the British Foundation for InternationalReconstructive
Surgery and Training (BFIRST) and ReSurge International (RThe
purpose of this study was to review the Nepalese experienc
crosurgical free flap reconstruction in order to demonstrate
of such teaching workshops on access to reconstructive serv
free flap outcomes in Nepal.
METHODS
With institutional review board approval, a retrospectiv
view was performed of all subjects undergoing microsurgica
reconstruction from April2007 to August2017.All cases were per-
formed at KMH and Kirtipur Hospital, working under the umb
Public Health Concern Trust–NEPAL (phect-NEPAL),exceptfor 4
cases at the National Trauma Center. Sixteen microsurgery
were held during the study period.InterplastAustralia and New
Zealand conducted 10 microsurgery workshops, almost onc
with the exception of 3 workshops in 2008 and none in 2013
2016.ReSurge Internationalheld 4 workshops,1 each in 2015 and
2016 and 2 in 2017. The British Foundation for International
structive Surgery and Training held workshops after the ear
2015 and again in 2017.
During workshops, local and visiting surgeons evaluate
together. Local surgeons were encouraged to make diagnos
apeutic plans.Preoperative evaluation included routine hemato
biochemistry, and kidney and liver function tests, in addition
type and cross match, viral markers, chest x-ray, and electr
for patients older than 40 years or younger if indicated. Ima
orthopantomogram,computed tomography scan,or magnetic reso-
nance imaging scan) was done in indicated cases.Angiography was
not performed routinely.
All the surgeries were done under general anesthesia e
cases that had only epidural anesthesia. All the lower extrem
ceived indwelling epidural catheterization for postoperative
Received May 2, 2018, and accepted for publication, after revision June 7, 2018.
From the *Departmentof Burns,Plastic and Reconstructive Surgery,phect-
NEPAL, Kirtipur Hospital,Kathmandu,Nepal;†Division of Plastic and
Reconstructive Surgery,Stanford University Schoolof Medicine,Stanford,
CA; ‡Department of Anesthesiology and Critical Care,phect-NEPAL,Kirtipur
Hospital, Kathmandu, Nepal.
Conflicts of interest and sources of funding: none declared.
Reprints: Kiran K. Nakarmi, MCh, Department of Burns, Plastic and Reconstructive
Surgery, phect-NEPAL, Kirtipur Hospital, Dev Dhoka, Kirtipur,
Kathmandu, Nepal. E-mail: kknakarmi@yahoo.com.
Copyright © 2018 Wolters Kluwer Health, Inc. All rights reserved.
ISSN: 0148-7043/18/0000–0000
DOI: 10.1097/SAP.0000000000001583
MICROSURGERY
Annals of Plastic Surgery• Volume 00, Number 00, Month 2018 www.annalsplasticsurgery.com1
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
During workshops, flap dissection and donor site preparation were each
performed by a team consisting of a local and visiting surgeons in order
to optimize focused learning; both local surgeons then participated in
flap in-setting and microanastomosis.Surgeries priorto May 2008
and those done at National Trauma Center were performed with operat-
ing loupes. The remaining flaps were performed with operating micro-
scopes.Postoperatively,patients remained intubated overnightif the
surgery lasted for 12 hours or longer or if there were issues with venti-
lation.Patients were generally transferred to the postoperative ward
(which is a step-down unit with a 4:1 patient-to-nurse ratio) or to the in-
tensive care unit if they were intubated. Flaps were monitored by clini-
cal examination and Dopplerevery 15 minutes for2 hours,every
30 minutes for the next 2 hours, and then every 2 hours for the next
2 days. Flap monitoring was subsequently done every 6 hours until dis-
charge. Feeding was started after 24 hours of flap observation, except
for cases of oral surgery in which feeding via nasogastric tube was per-
formed until oral feeding after the fifth postoperative day. Most of the
oral cancer patients received temporary tracheostomy that was typically
removed by 1 week after a plugging trial. Patients were given 2500 IU
of heparin intravenously twice daily for 5 days and low-dose aspirin for
a month. Discharge criteria included no further need for flap monitor-
ing, resolved flap swelling, tracheostomy and nasogastric tube removed,
adequate oral intake, and independent patient mobility.
RESULTS
Demographics
A total of 108 free flaps in 103 patients were reviewed. Males
outnumbered females (Table 1). The average age was 34.5 years (range,
8–73 years),with patients mostfrequently in the 16- to 30-year age
group (39.8%).
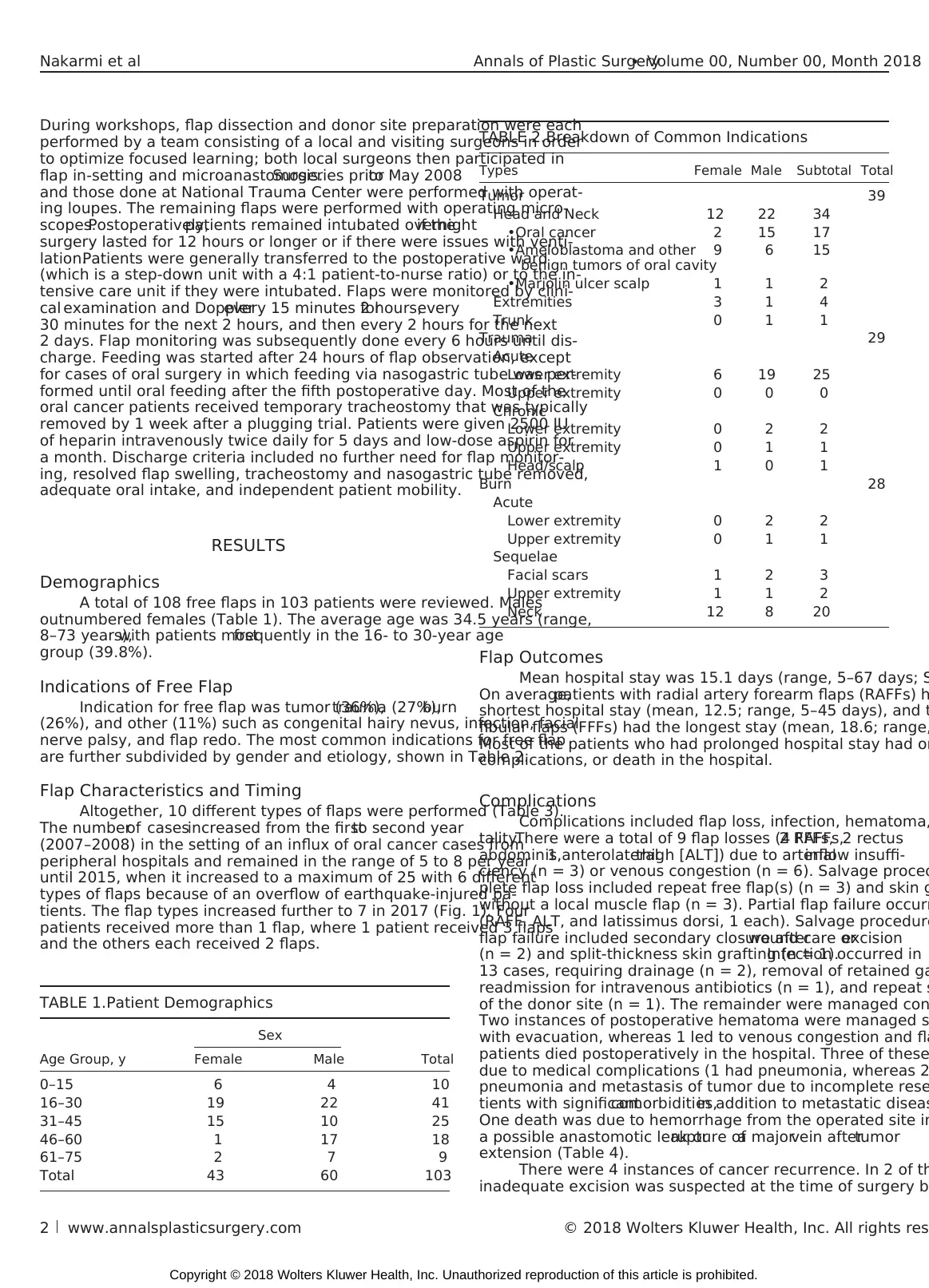
Indications of Free Flap
Indication for free flap was tumor (36%),trauma (27%),burn
(26%), and other (11%) such as congenital hairy nevus, infection, facial
nerve palsy, and flap redo. The most common indications for free flap
are further subdivided by gender and etiology, shown in Table 2.
Flap Characteristics and Timing
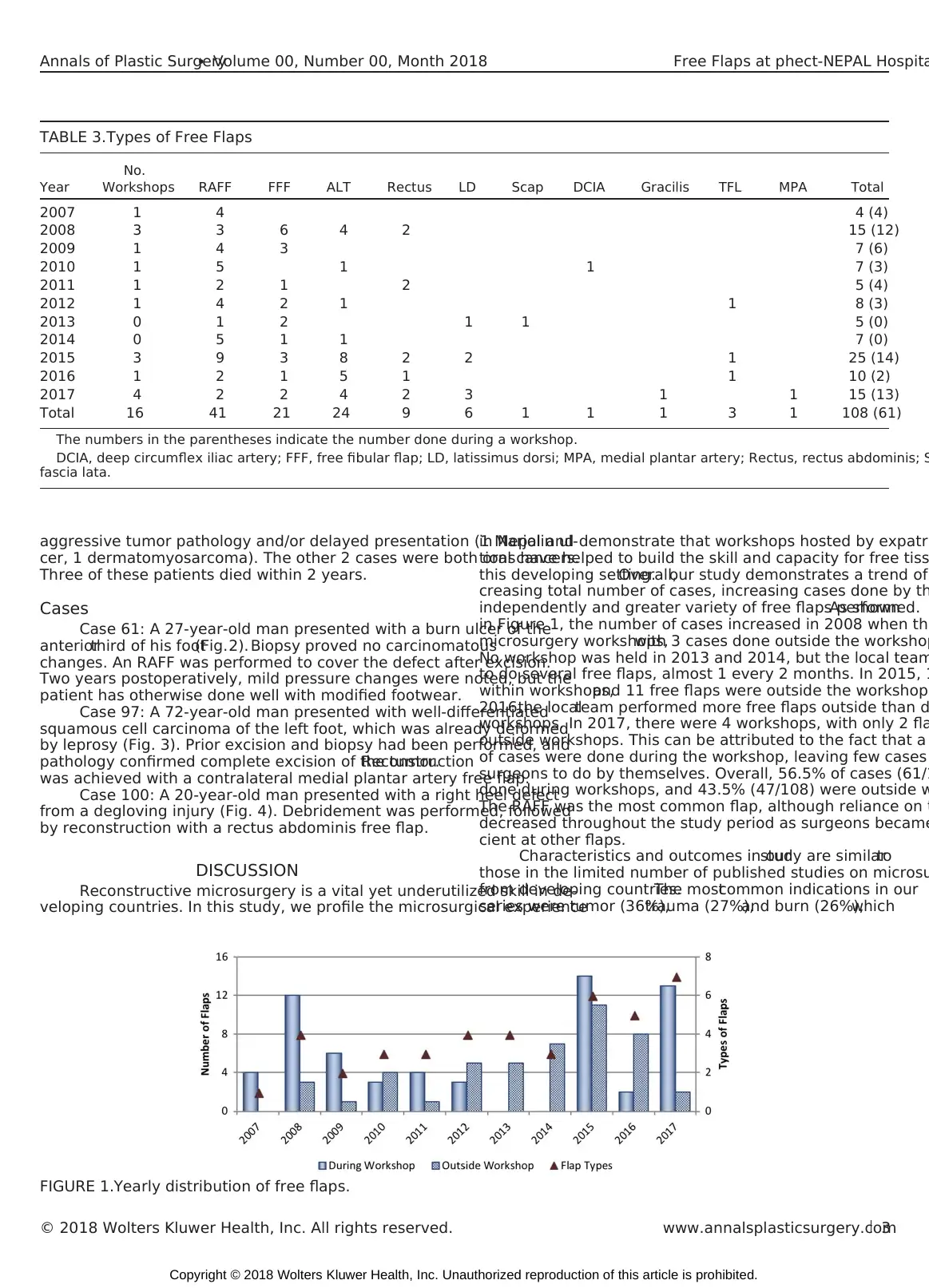
Altogether, 10 different types of flaps were performed (Table 3).
The numberof casesincreased from the firstto second year
(2007–2008) in the setting of an influx of oral cancer cases from
peripheral hospitals and remained in the range of 5 to 8 per year
until 2015, when it increased to a maximum of 25 with 6 different
types of flaps because of an overflow of earthquake-injured pa-
tients. The flap types increased further to 7 in 2017 (Fig. 1). Four
patients received more than 1 flap, where 1 patient received 3 flaps
and the others each received 2 flaps.
Flap Outcomes
Mean hospital stay was 15.1 days (range, 5–67 days; S
On average,patients with radial artery forearm flaps (RAFFs) h
shortest hospital stay (mean, 12.5; range, 5–45 days), and t
fibular flaps (FFFs) had the longest stay (mean, 18.6; range,
Most of the patients who had prolonged hospital stay had or
complications, or death in the hospital.
Complications
Complications included flap loss, infection, hematoma,
tality.There were a total of 9 flap losses (4 FFFs,2 RAFFs,2 rectus
abdominis,1 anterolateralthigh [ALT]) due to arterialinflow insuffi-
ciency (n = 3) or venous congestion (n = 6). Salvage proced
plete flap loss included repeat free flap(s) (n = 3) and skin g
without a local muscle flap (n = 3). Partial flap failure occurr
(RAFF, ALT, and latissimus dorsi, 1 each). Salvage procedure
flap failure included secondary closure afterwound care orexcision
(n = 2) and split-thickness skin grafting (n = 1).Infection occurred in
13 cases, requiring drainage (n = 2), removal of retained ga
readmission for intravenous antibiotics (n = 1), and repeat s
of the donor site (n = 1). The remainder were managed con
Two instances of postoperative hematoma were managed s
with evacuation, whereas 1 led to venous congestion and fla
patients died postoperatively in the hospital. Three of these
due to medical complications (1 had pneumonia, whereas 2
pneumonia and metastasis of tumor due to incomplete rese
tients with significantcomorbidities,in addition to metastatic diseas
One death was due to hemorrhage from the operated site in
a possible anastomotic leak orrupture ofa majorvein aftertumor
extension (Table 4).
There were 4 instances of cancer recurrence. In 2 of th
inadequate excision was suspected at the time of surgery b
TABLE 1.Patient Demographics
Sex
Age Group, y Female Male Total
0–15 6 4 10
16–30 19 22 41
31–45 15 10 25
46–60 1 17 18
61–75 2 7 9
Total 43 60 103
TABLE 2.Breakdown of Common Indications
Types Female Male Subtotal Total
Tumor 39
Head and Neck 12 22 34
•Oral cancer 2 15 17
•Ameloblastoma and other
benign tumors of oral cavity
9 6 15
•Marjolin ulcer scalp 1 1 2
Extremities 3 1 4
Trunk 0 1 1
Trauma 29
Acute
Lower extremity 6 19 25
Upper extremity 0 0 0
Chronic
Lower extremity 0 2 2
Upper extremity 0 1 1
Head/scalp 1 0 1
Burn 28
Acute
Lower extremity 0 2 2
Upper extremity 0 1 1
Sequelae
Facial scars 1 2 3
Upper extremity 1 1 2
Neck 12 8 20
Nakarmi et al Annals of Plastic Surgery• Volume 00, Number 00, Month 2018
2 www.annalsplasticsurgery.com © 2018 Wolters Kluwer Health, Inc. All rights res
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
performed by a team consisting of a local and visiting surgeons in order
to optimize focused learning; both local surgeons then participated in
flap in-setting and microanastomosis.Surgeries priorto May 2008
and those done at National Trauma Center were performed with operat-
ing loupes. The remaining flaps were performed with operating micro-
scopes.Postoperatively,patients remained intubated overnightif the
surgery lasted for 12 hours or longer or if there were issues with venti-
lation.Patients were generally transferred to the postoperative ward
(which is a step-down unit with a 4:1 patient-to-nurse ratio) or to the in-
tensive care unit if they were intubated. Flaps were monitored by clini-
cal examination and Dopplerevery 15 minutes for2 hours,every
30 minutes for the next 2 hours, and then every 2 hours for the next
2 days. Flap monitoring was subsequently done every 6 hours until dis-
charge. Feeding was started after 24 hours of flap observation, except
for cases of oral surgery in which feeding via nasogastric tube was per-
formed until oral feeding after the fifth postoperative day. Most of the
oral cancer patients received temporary tracheostomy that was typically
removed by 1 week after a plugging trial. Patients were given 2500 IU
of heparin intravenously twice daily for 5 days and low-dose aspirin for
a month. Discharge criteria included no further need for flap monitor-
ing, resolved flap swelling, tracheostomy and nasogastric tube removed,
adequate oral intake, and independent patient mobility.
RESULTS
Demographics
A total of 108 free flaps in 103 patients were reviewed. Males
outnumbered females (Table 1). The average age was 34.5 years (range,
8–73 years),with patients mostfrequently in the 16- to 30-year age
group (39.8%).
Indications of Free Flap
Indication for free flap was tumor (36%),trauma (27%),burn
(26%), and other (11%) such as congenital hairy nevus, infection, facial
nerve palsy, and flap redo. The most common indications for free flap
are further subdivided by gender and etiology, shown in Table 2.
Flap Characteristics and Timing
Altogether, 10 different types of flaps were performed (Table 3).
The numberof casesincreased from the firstto second year
(2007–2008) in the setting of an influx of oral cancer cases from
peripheral hospitals and remained in the range of 5 to 8 per year
until 2015, when it increased to a maximum of 25 with 6 different
types of flaps because of an overflow of earthquake-injured pa-
tients. The flap types increased further to 7 in 2017 (Fig. 1). Four
patients received more than 1 flap, where 1 patient received 3 flaps
and the others each received 2 flaps.
Flap Outcomes
Mean hospital stay was 15.1 days (range, 5–67 days; S
On average,patients with radial artery forearm flaps (RAFFs) h
shortest hospital stay (mean, 12.5; range, 5–45 days), and t
fibular flaps (FFFs) had the longest stay (mean, 18.6; range,
Most of the patients who had prolonged hospital stay had or
complications, or death in the hospital.
Complications
Complications included flap loss, infection, hematoma,
tality.There were a total of 9 flap losses (4 FFFs,2 RAFFs,2 rectus
abdominis,1 anterolateralthigh [ALT]) due to arterialinflow insuffi-
ciency (n = 3) or venous congestion (n = 6). Salvage proced
plete flap loss included repeat free flap(s) (n = 3) and skin g
without a local muscle flap (n = 3). Partial flap failure occurr
(RAFF, ALT, and latissimus dorsi, 1 each). Salvage procedure
flap failure included secondary closure afterwound care orexcision
(n = 2) and split-thickness skin grafting (n = 1).Infection occurred in
13 cases, requiring drainage (n = 2), removal of retained ga
readmission for intravenous antibiotics (n = 1), and repeat s
of the donor site (n = 1). The remainder were managed con
Two instances of postoperative hematoma were managed s
with evacuation, whereas 1 led to venous congestion and fla
patients died postoperatively in the hospital. Three of these
due to medical complications (1 had pneumonia, whereas 2
pneumonia and metastasis of tumor due to incomplete rese
tients with significantcomorbidities,in addition to metastatic diseas
One death was due to hemorrhage from the operated site in
a possible anastomotic leak orrupture ofa majorvein aftertumor
extension (Table 4).
There were 4 instances of cancer recurrence. In 2 of th
inadequate excision was suspected at the time of surgery b
TABLE 1.Patient Demographics
Sex
Age Group, y Female Male Total
0–15 6 4 10
16–30 19 22 41
31–45 15 10 25
46–60 1 17 18
61–75 2 7 9
Total 43 60 103
TABLE 2.Breakdown of Common Indications
Types Female Male Subtotal Total
Tumor 39
Head and Neck 12 22 34
•Oral cancer 2 15 17
•Ameloblastoma and other
benign tumors of oral cavity
9 6 15
•Marjolin ulcer scalp 1 1 2
Extremities 3 1 4
Trunk 0 1 1
Trauma 29
Acute
Lower extremity 6 19 25
Upper extremity 0 0 0
Chronic
Lower extremity 0 2 2
Upper extremity 0 1 1
Head/scalp 1 0 1
Burn 28
Acute
Lower extremity 0 2 2
Upper extremity 0 1 1
Sequelae
Facial scars 1 2 3
Upper extremity 1 1 2
Neck 12 8 20
Nakarmi et al Annals of Plastic Surgery• Volume 00, Number 00, Month 2018
2 www.annalsplasticsurgery.com © 2018 Wolters Kluwer Health, Inc. All rights res
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
aggressive tumor pathology and/or delayed presentation (1 Marjolin ul-
cer, 1 dermatomyosarcoma). The other 2 cases were both oral cancers.
Three of these patients died within 2 years.
Cases
Case 61: A 27-year-old man presented with a burn ulcer of the
anteriorthird of his foot(Fig.2). Biopsy proved no carcinomatous
changes. An RAFF was performed to cover the defect after excision.
Two years postoperatively, mild pressure changes were noted, but the
patient has otherwise done well with modified footwear.
Case 97: A 72-year-old man presented with well-differentiated
squamous cell carcinoma of the left foot, which was already deformed
by leprosy (Fig. 3). Prior excision and biopsy had been performed, and
pathology confirmed complete excision of the tumor.Reconstruction
was achieved with a contralateral medial plantar artery free flap.
Case 100: A 20-year-old man presented with a right heel defect
from a degloving injury (Fig. 4). Debridement was performed, followed
by reconstruction with a rectus abdominis free flap.
DISCUSSION
Reconstructive microsurgery is a vital yet underutilized skill in de-
veloping countries. In this study, we profile the microsurgical experience
in Nepal and demonstrate that workshops hosted by expatri
tions have helped to build the skill and capacity for free tiss
this developing setting.Overall,our study demonstrates a trend of
creasing total number of cases, increasing cases done by th
independently and greater variety of free flaps performed.As shown
in Figure 1, the number of cases increased in 2008 when the
microsurgery workshops,with 3 cases done outside the workshop
No workshop was held in 2013 and 2014, but the local team
to do several free flaps, almost 1 every 2 months. In 2015, 1
within workshops,and 11 free flaps were outside the workshops
2016,the localteam performed more free flaps outside than d
workshops. In 2017, there were 4 workshops, with only 2 fla
outside workshops. This can be attributed to the fact that a
of cases were done during the workshop, leaving few cases
surgeons to do by themselves. Overall, 56.5% of cases (61/1
done during workshops, and 43.5% (47/108) were outside w
The RAFF was the most common flap, although reliance on t
decreased throughout the study period as surgeons became
cient at other flaps.
Characteristics and outcomes in ourstudy are similarto
those in the limited number of published studies on microsu
from developing countries.The mostcommon indications in our
series were tumor (36%),trauma (27%),and burn (26%),which
FIGURE 1.Yearly distribution of free flaps.
TABLE 3.Types of Free Flaps
Year
No.
Workshops RAFF FFF ALT Rectus LD Scap DCIA Gracilis TFL MPA Total
2007 1 4 4 (4)
2008 3 3 6 4 2 15 (12)
2009 1 4 3 7 (6)
2010 1 5 1 1 7 (3)
2011 1 2 1 2 5 (4)
2012 1 4 2 1 1 8 (3)
2013 0 1 2 1 1 5 (0)
2014 0 5 1 1 7 (0)
2015 3 9 3 8 2 2 1 25 (14)
2016 1 2 1 5 1 1 10 (2)
2017 4 2 2 4 2 3 1 1 15 (13)
Total 16 41 21 24 9 6 1 1 1 3 1 108 (61)
The numbers in the parentheses indicate the number done during a workshop.
DCIA, deep circumflex iliac artery; FFF, free fibular flap; LD, latissimus dorsi; MPA, medial plantar artery; Rectus, rectus abdominis; S
fascia lata.
Annals of Plastic Surgery• Volume 00, Number 00, Month 2018 Free Flaps at phect-NEPAL Hospita
© 2018 Wolters Kluwer Health, Inc. All rights reserved. www.annalsplasticsurgery.com3
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
cer, 1 dermatomyosarcoma). The other 2 cases were both oral cancers.
Three of these patients died within 2 years.
Cases
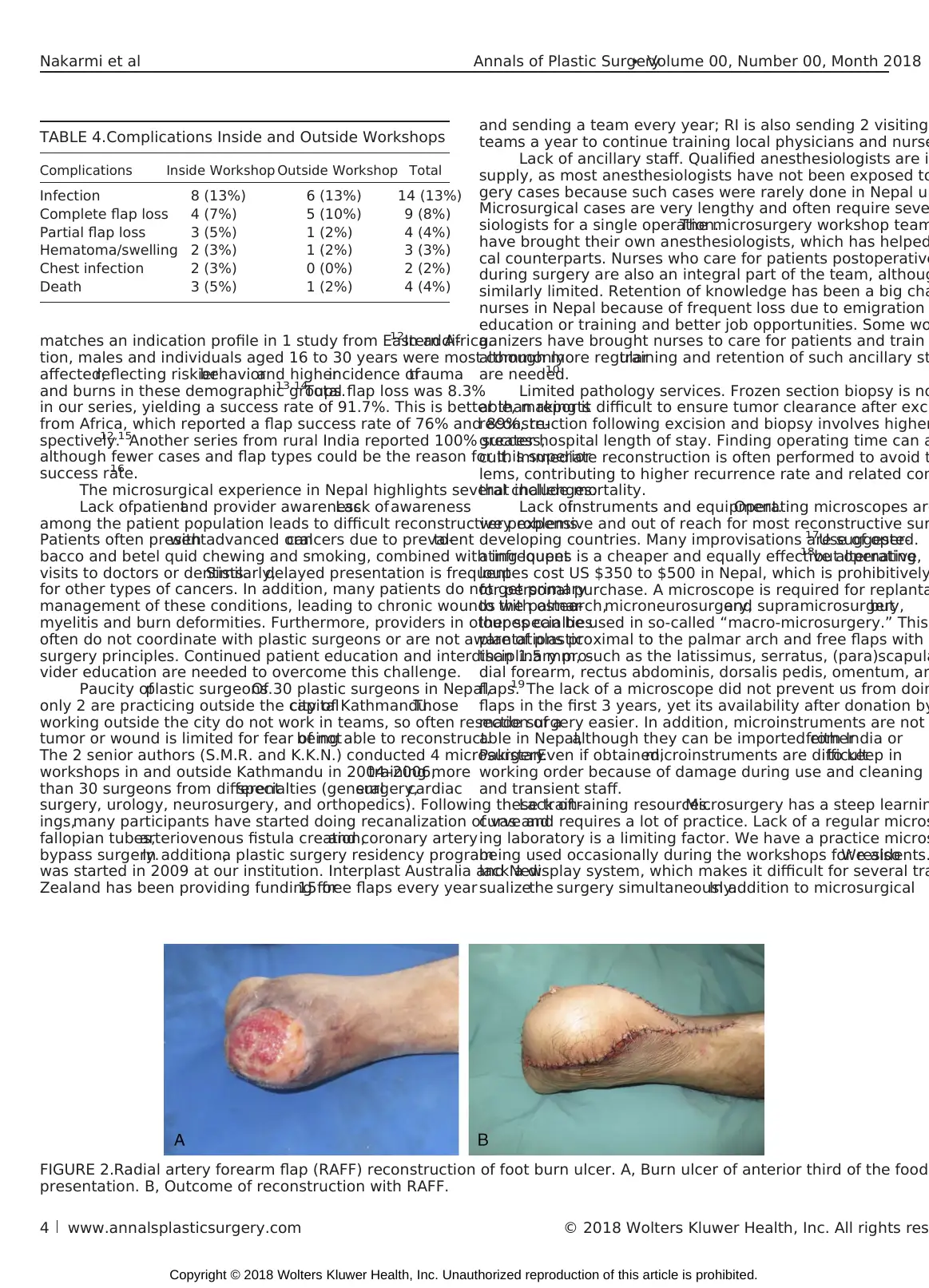
Case 61: A 27-year-old man presented with a burn ulcer of the
anteriorthird of his foot(Fig.2). Biopsy proved no carcinomatous
changes. An RAFF was performed to cover the defect after excision.
Two years postoperatively, mild pressure changes were noted, but the
patient has otherwise done well with modified footwear.
Case 97: A 72-year-old man presented with well-differentiated
squamous cell carcinoma of the left foot, which was already deformed
by leprosy (Fig. 3). Prior excision and biopsy had been performed, and
pathology confirmed complete excision of the tumor.Reconstruction
was achieved with a contralateral medial plantar artery free flap.
Case 100: A 20-year-old man presented with a right heel defect
from a degloving injury (Fig. 4). Debridement was performed, followed
by reconstruction with a rectus abdominis free flap.
DISCUSSION
Reconstructive microsurgery is a vital yet underutilized skill in de-
veloping countries. In this study, we profile the microsurgical experience
in Nepal and demonstrate that workshops hosted by expatri
tions have helped to build the skill and capacity for free tiss
this developing setting.Overall,our study demonstrates a trend of
creasing total number of cases, increasing cases done by th
independently and greater variety of free flaps performed.As shown
in Figure 1, the number of cases increased in 2008 when the
microsurgery workshops,with 3 cases done outside the workshop
No workshop was held in 2013 and 2014, but the local team
to do several free flaps, almost 1 every 2 months. In 2015, 1
within workshops,and 11 free flaps were outside the workshops
2016,the localteam performed more free flaps outside than d
workshops. In 2017, there were 4 workshops, with only 2 fla
outside workshops. This can be attributed to the fact that a
of cases were done during the workshop, leaving few cases
surgeons to do by themselves. Overall, 56.5% of cases (61/1
done during workshops, and 43.5% (47/108) were outside w
The RAFF was the most common flap, although reliance on t
decreased throughout the study period as surgeons became
cient at other flaps.
Characteristics and outcomes in ourstudy are similarto
those in the limited number of published studies on microsu
from developing countries.The mostcommon indications in our
series were tumor (36%),trauma (27%),and burn (26%),which
FIGURE 1.Yearly distribution of free flaps.
TABLE 3.Types of Free Flaps
Year
No.
Workshops RAFF FFF ALT Rectus LD Scap DCIA Gracilis TFL MPA Total
2007 1 4 4 (4)
2008 3 3 6 4 2 15 (12)
2009 1 4 3 7 (6)
2010 1 5 1 1 7 (3)
2011 1 2 1 2 5 (4)
2012 1 4 2 1 1 8 (3)
2013 0 1 2 1 1 5 (0)
2014 0 5 1 1 7 (0)
2015 3 9 3 8 2 2 1 25 (14)
2016 1 2 1 5 1 1 10 (2)
2017 4 2 2 4 2 3 1 1 15 (13)
Total 16 41 21 24 9 6 1 1 1 3 1 108 (61)
The numbers in the parentheses indicate the number done during a workshop.
DCIA, deep circumflex iliac artery; FFF, free fibular flap; LD, latissimus dorsi; MPA, medial plantar artery; Rectus, rectus abdominis; S
fascia lata.
Annals of Plastic Surgery• Volume 00, Number 00, Month 2018 Free Flaps at phect-NEPAL Hospita
© 2018 Wolters Kluwer Health, Inc. All rights reserved. www.annalsplasticsurgery.com3
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
matches an indication profile in 1 study from Eastern Africa.12In addi-
tion, males and individuals aged 16 to 30 years were most commonly
affected,reflecting riskierbehaviorand higherincidence oftrauma
and burns in these demographic groups.13,14
Total flap loss was 8.3%
in our series, yielding a success rate of 91.7%. This is better than reports
from Africa, which reported a flap success rate of 76% and 89%, re-
spectively.12,15
Another series from rural India reported 100% success,
although fewer cases and flap types could be the reason for this superior
success rate.16
The microsurgical experience in Nepal highlights several challenges:
Lack ofpatientand provider awareness.Lack ofawareness
among the patient population leads to difficult reconstructive problems.
Patients often presentwith advanced oralcancers due to prevalentto-
bacco and betel quid chewing and smoking, combined with infrequent
visits to doctors or dentists.Similarly,delayed presentation is frequent
for other types of cancers. In addition, many patients do not get primary
management of these conditions, leading to chronic wounds with osteo-
myelitis and burn deformities. Furthermore, providers in other specialties
often do not coordinate with plastic surgeons or are not aware of plastic
surgery principles. Continued patient education and interdisciplinary pro-
vider education are needed to overcome this challenge.
Paucity ofplastic surgeons.Of 30 plastic surgeons in Nepal,
only 2 are practicing outside the capitalcity of Kathmandu.Those
working outside the city do not work in teams, so often resection of a
tumor or wound is limited for fear of notbeing able to reconstruct.
The 2 senior authors (S.M.R. and K.K.N.) conducted 4 microsurgery
workshops in and outside Kathmandu in 2004–2006,training more
than 30 surgeons from differentspecialties (generalsurgery,cardiac
surgery, urology, neurosurgery, and orthopedics). Following these train-
ings,many participants have started doing recanalization of vas and
fallopian tubes,arteriovenous fistula creation,and coronary artery
bypass surgery.In addition,a plastic surgery residency program
was started in 2009 at our institution. Interplast Australia and New
Zealand has been providing funding for15 free flaps every year
and sending a team every year; RI is also sending 2 visiting
teams a year to continue training local physicians and nurse
Lack of ancillary staff. Qualified anesthesiologists are i
supply, as most anesthesiologists have not been exposed to
gery cases because such cases were rarely done in Nepal un
Microsurgical cases are very lengthy and often require seve
siologists for a single operation.The microsurgery workshop team
have brought their own anesthesiologists, which has helped
cal counterparts. Nurses who care for patients postoperative
during surgery are also an integral part of the team, althoug
similarly limited. Retention of knowledge has been a big cha
nurses in Nepal because of frequent loss due to emigration
education or training and better job opportunities. Some wo
ganizers have brought nurses to care for patients and train
although more regulartraining and retention of such ancillary st
are needed.10
Limited pathology services. Frozen section biopsy is no
able, making it difficult to ensure tumor clearance after exci
reconstruction following excision and biopsy involves higher
greater hospital length of stay. Finding operating time can a
cult. Immediate reconstruction is often performed to avoid t
lems, contributing to higher recurrence rate and related com
that include mortality.
Lack ofinstruments and equipment.Operating microscopes are
very expensive and out of reach for most reconstructive sur
developing countries. Many improvisations are suggested.17Use of oper-
ating loupes is a cheaper and equally effective alternative,18but operating
loupes cost US $350 to $500 in Nepal, which is prohibitively
for personal purchase. A microscope is required for replanta
to the palmararch,microneurosurgery,and supramicrosurgery,but
loupes can be used in so-called “macro-microsurgery.” This
plantations proximal to the palmar arch and free flaps with
than 1.5 mm, such as the latissimus, serratus, (para)scapula
dial forearm, rectus abdominis, dorsalis pedis, omentum, an
flaps.19 The lack of a microscope did not prevent us from doin
flaps in the first 3 years, yet its availability after donation by
made surgery easier. In addition, microinstruments are not
able in Nepal,although they can be imported eitherfrom India or
Pakistan.Even if obtained,microinstruments are difficultto keep in
working order because of damage during use and cleaning b
and transient staff.
Lack oftraining resources.Microsurgery has a steep learnin
curve and requires a lot of practice. Lack of a regular micros
ing laboratory is a limiting factor. We have a practice micros
being used occasionally during the workshops for residents.We also
lack a display system, which makes it difficult for several tra
sualizethe surgery simultaneously.In addition to microsurgical
TABLE 4.Complications Inside and Outside Workshops
Complications Inside Workshop Outside Workshop Total
Infection 8 (13%) 6 (13%) 14 (13%)
Complete flap loss 4 (7%) 5 (10%) 9 (8%)
Partial flap loss 3 (5%) 1 (2%) 4 (4%)
Hematoma/swelling 2 (3%) 1 (2%) 3 (3%)
Chest infection 2 (3%) 0 (0%) 2 (2%)
Death 3 (5%) 1 (2%) 4 (4%)
FIGURE 2.Radial artery forearm flap (RAFF) reconstruction of foot burn ulcer. A, Burn ulcer of anterior third of the food
presentation. B, Outcome of reconstruction with RAFF.
Nakarmi et al Annals of Plastic Surgery• Volume 00, Number 00, Month 2018
4 www.annalsplasticsurgery.com © 2018 Wolters Kluwer Health, Inc. All rights res
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
tion, males and individuals aged 16 to 30 years were most commonly
affected,reflecting riskierbehaviorand higherincidence oftrauma
and burns in these demographic groups.13,14
Total flap loss was 8.3%
in our series, yielding a success rate of 91.7%. This is better than reports
from Africa, which reported a flap success rate of 76% and 89%, re-
spectively.12,15
Another series from rural India reported 100% success,
although fewer cases and flap types could be the reason for this superior
success rate.16
The microsurgical experience in Nepal highlights several challenges:
Lack ofpatientand provider awareness.Lack ofawareness
among the patient population leads to difficult reconstructive problems.
Patients often presentwith advanced oralcancers due to prevalentto-
bacco and betel quid chewing and smoking, combined with infrequent
visits to doctors or dentists.Similarly,delayed presentation is frequent
for other types of cancers. In addition, many patients do not get primary
management of these conditions, leading to chronic wounds with osteo-
myelitis and burn deformities. Furthermore, providers in other specialties
often do not coordinate with plastic surgeons or are not aware of plastic
surgery principles. Continued patient education and interdisciplinary pro-
vider education are needed to overcome this challenge.
Paucity ofplastic surgeons.Of 30 plastic surgeons in Nepal,
only 2 are practicing outside the capitalcity of Kathmandu.Those
working outside the city do not work in teams, so often resection of a
tumor or wound is limited for fear of notbeing able to reconstruct.
The 2 senior authors (S.M.R. and K.K.N.) conducted 4 microsurgery
workshops in and outside Kathmandu in 2004–2006,training more
than 30 surgeons from differentspecialties (generalsurgery,cardiac
surgery, urology, neurosurgery, and orthopedics). Following these train-
ings,many participants have started doing recanalization of vas and
fallopian tubes,arteriovenous fistula creation,and coronary artery
bypass surgery.In addition,a plastic surgery residency program
was started in 2009 at our institution. Interplast Australia and New
Zealand has been providing funding for15 free flaps every year
and sending a team every year; RI is also sending 2 visiting
teams a year to continue training local physicians and nurse
Lack of ancillary staff. Qualified anesthesiologists are i
supply, as most anesthesiologists have not been exposed to
gery cases because such cases were rarely done in Nepal un
Microsurgical cases are very lengthy and often require seve
siologists for a single operation.The microsurgery workshop team
have brought their own anesthesiologists, which has helped
cal counterparts. Nurses who care for patients postoperative
during surgery are also an integral part of the team, althoug
similarly limited. Retention of knowledge has been a big cha
nurses in Nepal because of frequent loss due to emigration
education or training and better job opportunities. Some wo
ganizers have brought nurses to care for patients and train
although more regulartraining and retention of such ancillary st
are needed.10
Limited pathology services. Frozen section biopsy is no
able, making it difficult to ensure tumor clearance after exci
reconstruction following excision and biopsy involves higher
greater hospital length of stay. Finding operating time can a
cult. Immediate reconstruction is often performed to avoid t
lems, contributing to higher recurrence rate and related com
that include mortality.
Lack ofinstruments and equipment.Operating microscopes are
very expensive and out of reach for most reconstructive sur
developing countries. Many improvisations are suggested.17Use of oper-
ating loupes is a cheaper and equally effective alternative,18but operating
loupes cost US $350 to $500 in Nepal, which is prohibitively
for personal purchase. A microscope is required for replanta
to the palmararch,microneurosurgery,and supramicrosurgery,but
loupes can be used in so-called “macro-microsurgery.” This
plantations proximal to the palmar arch and free flaps with
than 1.5 mm, such as the latissimus, serratus, (para)scapula
dial forearm, rectus abdominis, dorsalis pedis, omentum, an
flaps.19 The lack of a microscope did not prevent us from doin
flaps in the first 3 years, yet its availability after donation by
made surgery easier. In addition, microinstruments are not
able in Nepal,although they can be imported eitherfrom India or
Pakistan.Even if obtained,microinstruments are difficultto keep in
working order because of damage during use and cleaning b
and transient staff.
Lack oftraining resources.Microsurgery has a steep learnin
curve and requires a lot of practice. Lack of a regular micros
ing laboratory is a limiting factor. We have a practice micros
being used occasionally during the workshops for residents.We also
lack a display system, which makes it difficult for several tra
sualizethe surgery simultaneously.In addition to microsurgical
TABLE 4.Complications Inside and Outside Workshops
Complications Inside Workshop Outside Workshop Total
Infection 8 (13%) 6 (13%) 14 (13%)
Complete flap loss 4 (7%) 5 (10%) 9 (8%)
Partial flap loss 3 (5%) 1 (2%) 4 (4%)
Hematoma/swelling 2 (3%) 1 (2%) 3 (3%)
Chest infection 2 (3%) 0 (0%) 2 (2%)
Death 3 (5%) 1 (2%) 4 (4%)
FIGURE 2.Radial artery forearm flap (RAFF) reconstruction of foot burn ulcer. A, Burn ulcer of anterior third of the food
presentation. B, Outcome of reconstruction with RAFF.
Nakarmi et al Annals of Plastic Surgery• Volume 00, Number 00, Month 2018
4 www.annalsplasticsurgery.com © 2018 Wolters Kluwer Health, Inc. All rights res
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.

anastomoses, flap harvesting skills also need to be learned and perfected
because of the importance of handling the flap and pedicle. Fresh per-
fused human cadavers can give almost real life experience,20,21
yet ca-
davers are not easily available in developing countries.22
Prohibitive cost. Microsurgery is costly because of long opera-
tive time, high utilization of medicines and supplies, and involvement
of many surgeons, anesthesiologists, nurses, and other support staff in
the operating room and afterward. Although the government of Nepal
has made many health-related services free of cost,microsurgery is
not covered by government funding. Cases in our series were made pos-
sible largely because of the financial support of foundations (IAN,
RI) and other third parties. Costs are likely to be even higher in pri-
vate hospitals,discouraging such institutions from offering these
surgeries. Developing a robust microsurgery practice in Nepal will
require a more sustainable funding scheme.
CONCLUSION
Free flap transfer allows reconstruction of the most challenging
tissue defects that result from tumor resection, trauma, burns, and other
circumstances that frequently occur in developing countries. Microsur-
gery is thus a critical skill for surgeons in these settings, but there are
several challenges that prevent its widespread adoption. In Nepal, train-
ing and support of local health personnel have increased local capability
to perform microsurgical reconstruction and are an important step in
creating a sustainable model.
ACKNOWLEDGMENTS
The authors thank Damien Grinsell, FRACS, country director for
Nepal,Interplast Australia and New Zealand,ReSurge International,
and British Foundation for InternationalReconstructive Surgery
and Training.
REFERENCES
1. Shrime MG, Bickler SW, Alkire BC, et al. Global burden of surgical dise
an estimation from the provider perspective. Lancet Global Health. 20
S8–S9.
2. Alkire B, Raykar NP, Shrime MG, et al. Global access to surgical care:
ling study. Lancet Global Health. 2015;3:e316–e323.
3. Corlew DS. Estimation of impact of surgical disease through economic
of cleft lip and palate care. World J Surg. 2010;34:391–396.
4. Semer NB, Sullivan SR, Meara JG. Plastic surgery and global health: h
surgery impacts the global burden of surgical disease. J Plast Reconst
Surg. 2010;63:1244–1248.
5. Figus A, Fioramonti P, Morselli P, et al. Interplast Italy: a 20-year plast
constructive surgery humanitarian experience in developing countriePlast
Reconstr Surg. 2009;124:1340–1348.
6. d'Agostino S,Del Rossi C, Del Curto S, et al. Surgery ofcongenital
malformations in developing countries: experience in 13 humanitaria
during 9 years. Pediatr Med Chir. 2001;23:117–121.
7. Magee WP,VanderBurg R, HatcherKW. Cleft lip and palate as a cost-
effective health care treatment in the developing world. World J Surg.
420–427.
8. AbenavoliFM. Operation Smile humanitarian missions.PlastReconstr Surg.
2005;115:356–357.
9. Persing J. The changing role of volunteer organizations and host coun
tions: a personal perspective. Ann Plast Surg. 2012;68:5–6.
10. Silinzieds A,Simmons L,Edward KL,et al. Nurse education in developing
countries—Australian plastics and microsurgicalnurses in Nepal.PlastSurg
Nurs. 2012;32:148–155.
11. Corlew DS.Perspectives on plastic surgery and global health.Ann Plast Surg.
2009;62:473–477.
12. Citron I, Galiwango G, Hodges A. Challenges in global microsurgery: a
review of outcomes at an East African hospital.J Plast Reconstr Aesthet Surg.
2016;69:189–195.
13. Gupta S, Mahmood U, Gurung S, et al. Burns in Nepal: a population ba
assessment. Burns. 2015;41:1126–1132.
FIGURE 3.Medial plantar artery free flap reconstruction of cancer excision of foot. A, Ulcerating squamous cell carcinom
prior to excision. B, Reconstruction with contralateral medial plantar artery free flap.
FIGURE 4.Rectus abdominis free flap reconstruction of degloving injury of foot. A, Primary defect following debridemen
B, Inset of rectus abdominis free muscle flap. C, Final reconstruction with skin graft over muscle flap.
Annals of Plastic Surgery• Volume 00, Number 00, Month 2018 Free Flaps at phect-NEPAL Hospita
© 2018 Wolters Kluwer Health, Inc. All rights reserved. www.annalsplasticsurgery.com5
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
because of the importance of handling the flap and pedicle. Fresh per-
fused human cadavers can give almost real life experience,20,21
yet ca-
davers are not easily available in developing countries.22
Prohibitive cost. Microsurgery is costly because of long opera-
tive time, high utilization of medicines and supplies, and involvement
of many surgeons, anesthesiologists, nurses, and other support staff in
the operating room and afterward. Although the government of Nepal
has made many health-related services free of cost,microsurgery is
not covered by government funding. Cases in our series were made pos-
sible largely because of the financial support of foundations (IAN,
RI) and other third parties. Costs are likely to be even higher in pri-
vate hospitals,discouraging such institutions from offering these
surgeries. Developing a robust microsurgery practice in Nepal will
require a more sustainable funding scheme.
CONCLUSION
Free flap transfer allows reconstruction of the most challenging
tissue defects that result from tumor resection, trauma, burns, and other
circumstances that frequently occur in developing countries. Microsur-
gery is thus a critical skill for surgeons in these settings, but there are
several challenges that prevent its widespread adoption. In Nepal, train-
ing and support of local health personnel have increased local capability
to perform microsurgical reconstruction and are an important step in
creating a sustainable model.
ACKNOWLEDGMENTS
The authors thank Damien Grinsell, FRACS, country director for
Nepal,Interplast Australia and New Zealand,ReSurge International,
and British Foundation for InternationalReconstructive Surgery
and Training.
REFERENCES
1. Shrime MG, Bickler SW, Alkire BC, et al. Global burden of surgical dise
an estimation from the provider perspective. Lancet Global Health. 20
S8–S9.
2. Alkire B, Raykar NP, Shrime MG, et al. Global access to surgical care:
ling study. Lancet Global Health. 2015;3:e316–e323.
3. Corlew DS. Estimation of impact of surgical disease through economic
of cleft lip and palate care. World J Surg. 2010;34:391–396.
4. Semer NB, Sullivan SR, Meara JG. Plastic surgery and global health: h
surgery impacts the global burden of surgical disease. J Plast Reconst
Surg. 2010;63:1244–1248.
5. Figus A, Fioramonti P, Morselli P, et al. Interplast Italy: a 20-year plast
constructive surgery humanitarian experience in developing countriePlast
Reconstr Surg. 2009;124:1340–1348.
6. d'Agostino S,Del Rossi C, Del Curto S, et al. Surgery ofcongenital
malformations in developing countries: experience in 13 humanitaria
during 9 years. Pediatr Med Chir. 2001;23:117–121.
7. Magee WP,VanderBurg R, HatcherKW. Cleft lip and palate as a cost-
effective health care treatment in the developing world. World J Surg.
420–427.
8. AbenavoliFM. Operation Smile humanitarian missions.PlastReconstr Surg.
2005;115:356–357.
9. Persing J. The changing role of volunteer organizations and host coun
tions: a personal perspective. Ann Plast Surg. 2012;68:5–6.
10. Silinzieds A,Simmons L,Edward KL,et al. Nurse education in developing
countries—Australian plastics and microsurgicalnurses in Nepal.PlastSurg
Nurs. 2012;32:148–155.
11. Corlew DS.Perspectives on plastic surgery and global health.Ann Plast Surg.
2009;62:473–477.
12. Citron I, Galiwango G, Hodges A. Challenges in global microsurgery: a
review of outcomes at an East African hospital.J Plast Reconstr Aesthet Surg.
2016;69:189–195.
13. Gupta S, Mahmood U, Gurung S, et al. Burns in Nepal: a population ba
assessment. Burns. 2015;41:1126–1132.
FIGURE 3.Medial plantar artery free flap reconstruction of cancer excision of foot. A, Ulcerating squamous cell carcinom
prior to excision. B, Reconstruction with contralateral medial plantar artery free flap.
FIGURE 4.Rectus abdominis free flap reconstruction of degloving injury of foot. A, Primary defect following debridemen
B, Inset of rectus abdominis free muscle flap. C, Final reconstruction with skin graft over muscle flap.
Annals of Plastic Surgery• Volume 00, Number 00, Month 2018 Free Flaps at phect-NEPAL Hospita
© 2018 Wolters Kluwer Health, Inc. All rights reserved. www.annalsplasticsurgery.com5
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

14. Gupta S,Gupta SK,Devkota S,et al. Fall injuries in Nepal:a countrywide
population-based survey. Ann Glob Health. 2015;81:487–494.
15. Nangole WF, Khainga S, Aswani J, et al. Free flaps in a resource constrained
environment: a five-year experience-outcomes and lessons learned. Plast Surg
Int. 2015;2015:194174.
16. Trivedi NP, Trivedi P, Trivedi H, et al. Microvascular free flap reconstruction for
head and neck cancer in a resource-constrained environment in rural India. Indian
J Plast Surg. 2013;46:82–86.
17. Peltola TJ,MäntyjärviM, Teräsvirta M,et al. Build your own multipur-
pose,economically priced portable stereo microscope.Trop Doct.2000;30:
28–29.
18. PannucciCJ, Basta MN,Kovach SJ,etal.Loupes-only microsurgery is a safe
alternative to the operating microscope: an analysis of 1,649 consecu
breast reconstructions. J Reconstr Microsurg. 2015;31:636–642.
19. Pieptu D, Luchian S.Loupes-only microsurgery. Microsurgery. 2003;23
20. Carey JN,MinnetiM, Leland HA,et al. Perfused fresh cadavers:method for
application to surgical simulation. Am J Surg. 2015;210:179–187.
21. Carey JN,RommerE, SheckterC, et al. Simulation ofplastic surgery and
microvascular procedures using perfused fresh human cadavers. J Pla
Aesthet Surg. 2014;67:e42–e48.
22. Anyanwu GE,Udemezue OO,ObikiliEN. Dark age of sourcing cadavers in
developing countries: a Nigerian survey. Clin Anat. 2011;24:831–836.
Nakarmi et al Annals of Plastic Surgery• Volume 00, Number 00, Month 2018
6 www.annalsplasticsurgery.com © 2018 Wolters Kluwer Health, Inc. All rights res
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.View publication statsView publication stats
population-based survey. Ann Glob Health. 2015;81:487–494.
15. Nangole WF, Khainga S, Aswani J, et al. Free flaps in a resource constrained
environment: a five-year experience-outcomes and lessons learned. Plast Surg
Int. 2015;2015:194174.
16. Trivedi NP, Trivedi P, Trivedi H, et al. Microvascular free flap reconstruction for
head and neck cancer in a resource-constrained environment in rural India. Indian
J Plast Surg. 2013;46:82–86.
17. Peltola TJ,MäntyjärviM, Teräsvirta M,et al. Build your own multipur-
pose,economically priced portable stereo microscope.Trop Doct.2000;30:
28–29.
18. PannucciCJ, Basta MN,Kovach SJ,etal.Loupes-only microsurgery is a safe
alternative to the operating microscope: an analysis of 1,649 consecu
breast reconstructions. J Reconstr Microsurg. 2015;31:636–642.
19. Pieptu D, Luchian S.Loupes-only microsurgery. Microsurgery. 2003;23
20. Carey JN,MinnetiM, Leland HA,et al. Perfused fresh cadavers:method for
application to surgical simulation. Am J Surg. 2015;210:179–187.
21. Carey JN,RommerE, SheckterC, et al. Simulation ofplastic surgery and
microvascular procedures using perfused fresh human cadavers. J Pla
Aesthet Surg. 2014;67:e42–e48.
22. Anyanwu GE,Udemezue OO,ObikiliEN. Dark age of sourcing cadavers in
developing countries: a Nigerian survey. Clin Anat. 2011;24:831–836.
Nakarmi et al Annals of Plastic Surgery• Volume 00, Number 00, Month 2018
6 www.annalsplasticsurgery.com © 2018 Wolters Kluwer Health, Inc. All rights res
Copyright © 2018 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.View publication statsView publication stats
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.