Risk Factors for Microvascular Invasion in HCC: A Clinical Study
VerifiedAdded on 2022/08/21
|19
|12221
|8
Report
AI Summary
This report presents a retrospective clinical study investigating the risk factors associated with microvascular invasion (MVI) in 210 non-metastasis single-lesion HCC patients who underwent hepatic resection. The study collected data on various clinical, preoperative, and postoperative factors, including tumor characteristics, biomarkers, and histological data. Patients were divided into MVI (+) and MVI (-) groups, and statistical analysis was performed to identify significant predictors of MVI. Univariate analysis revealed significant associations between MVI and tumor differentiation, tumor size, AFP levels, and tumor margin. Multivariate logistic regression analysis identified poorly differentiated tumors and tumor size ≥3.5 cm as independent risk factors for MVI. The findings suggest that assessing tumor differentiation and size may aid in predicting MVI risk in HCC patients, potentially guiding treatment strategies and improving patient outcomes. The study highlights the importance of MVI as a key factor in HCC recurrence and survival, emphasizing the need for accurate preoperative MVI assessment.
Abstract
Background: The most frequent cause of cancer-related deaths worldwide is hepatocellular
carcinoma (HCC).The clinical detection and management of HCC have been enhanced, but the long-
term levels of survival are still unsatisfactory. One of the main factors related to patient recovery and
postoperative tumor recurrence was the microvascular invasion (MVI). It is necessary to identify a
risk factor for MVI which will help us predict MVI before the HCC patients are treated.
Method: Retrospective clinical data, including general clinical details, preoperative tumor marker,
inflammatory response factor, other biomarker association with HCC and liver function, tumor
characteristic in imaging modality, and postoperative histological data, are obtained from 210 non-
metastasis single lesion HCC patients who underwent hepatic resection surgery as the only curative
treatment All data divided into two groups: MVI (+) and MVI-). Multivariate research on statistically
important factors is conducted using logistic regression.
Result: The positive MVI score (61/210 patients) exceeded 29%. Significant variation between the
tumors (P=0.001) in size= 3.5 cm (P= 0.001), the alpha-fetoproteine (AFP) amount < 100 μg / L
(P=0.007) and the tumor margin (P<0,0001) was reported in the univariate study. The study of
multivariate logistic regression reveals that the MVI risk factor was separate only for the poorly
differentiated tumor cell (OR=1,470, 95% CI: 1,040-2,077, P=0,029) and tumour cell= 2,50 cm
(OR=2,205, 95% CI: 1,123-4,333, P=0,022).
Conclusion: Poorly differentiated tumor and tumor size ≥3.5 cm are separate risk factors for MVI,
which may help us assess the likelihood of MVI in HCC non-metastasis single lesion patients.
Keywords: hepatocellular carcinoma, microvascular invasion, non-metastasis, single lesion.
1 Introduction
1.1 Overview
Hepatocellular carcinoma (HCC) is the fifth most prevalent malignancy in the world and the sixth
most frequent cause of cancer-related death worldwide. Over the past year, there has been an average
loss of 700,000 globally (1). Liver cirrhosis is the hallmark of HCC in nearly 80% of cases (2). Many
factors are linked with HCC, such as hepatitis B virus (HBV) and hepatitis C virus (HCV) infection
and non-alcoholic fatty liver disease (3, 4). Clinical detection and management of HCC have
increased in the past decade, but long-term survival levels remain unsatisfactory (5). The previous
study showed that the HCC prediction depends on multiple factors such as patient age (6), tumor size,
tumor quantity, tumor vascular tumor invasion (7, 8), serum alfa-fetoprotein (AFP), and extrahepatic
metastasis involvement (10).
Tumor vascular invasion was known as a macrovascular invasion. It could only be seen through
microscopic inspection, primarily through tiny vessels such as a portal vein, core venous arteries of
noncancerous liver tissue, and venous arteries in the tumor capsule with large-sized and medium-sized
vessels (11,12). The invasion was only observed in the microscopic analysis. Invasion of
microvascular tumors was stated to be the most significant risk factor in postoperative early tuber
recurrence (13-16) and is recognized as a consequence of adverse results following HCC surgical
care. Lim et al. (17) stated that the HCC requirements in Milan after surgical resection are more
prominent tumor recurrence and general survival indicators than those for Milan. A small tumor with
no more than 5 cm or three or fewer will be considered for those following the Milan criterion, with
the tumor maximum measuring no more than 3 cm with no signs of macrovascular or extrahepatic
invasion (7). Lim et al. (17) reported that the average patient survival levels without MVI did not vary
greatly, and the Milan patient requirements were not met under Milan requirements. The average
survival rate declines for MVI but dramatically. An exact preoperative MVI estimation is, therefore,
necessary to prepare for care to avoid recurrence and to optimize patient outcomes.
This research was intended to investigate the association between preoperative clinicopathological
results of patients with a histological outcome in hepatic resection of HCC non-metastasis single
lesion and to seek to identify the risk factor for MVI.
Background: The most frequent cause of cancer-related deaths worldwide is hepatocellular
carcinoma (HCC).The clinical detection and management of HCC have been enhanced, but the long-
term levels of survival are still unsatisfactory. One of the main factors related to patient recovery and
postoperative tumor recurrence was the microvascular invasion (MVI). It is necessary to identify a
risk factor for MVI which will help us predict MVI before the HCC patients are treated.
Method: Retrospective clinical data, including general clinical details, preoperative tumor marker,
inflammatory response factor, other biomarker association with HCC and liver function, tumor
characteristic in imaging modality, and postoperative histological data, are obtained from 210 non-
metastasis single lesion HCC patients who underwent hepatic resection surgery as the only curative
treatment All data divided into two groups: MVI (+) and MVI-). Multivariate research on statistically
important factors is conducted using logistic regression.
Result: The positive MVI score (61/210 patients) exceeded 29%. Significant variation between the
tumors (P=0.001) in size= 3.5 cm (P= 0.001), the alpha-fetoproteine (AFP) amount < 100 μg / L
(P=0.007) and the tumor margin (P<0,0001) was reported in the univariate study. The study of
multivariate logistic regression reveals that the MVI risk factor was separate only for the poorly
differentiated tumor cell (OR=1,470, 95% CI: 1,040-2,077, P=0,029) and tumour cell= 2,50 cm
(OR=2,205, 95% CI: 1,123-4,333, P=0,022).
Conclusion: Poorly differentiated tumor and tumor size ≥3.5 cm are separate risk factors for MVI,
which may help us assess the likelihood of MVI in HCC non-metastasis single lesion patients.
Keywords: hepatocellular carcinoma, microvascular invasion, non-metastasis, single lesion.
1 Introduction
1.1 Overview
Hepatocellular carcinoma (HCC) is the fifth most prevalent malignancy in the world and the sixth
most frequent cause of cancer-related death worldwide. Over the past year, there has been an average
loss of 700,000 globally (1). Liver cirrhosis is the hallmark of HCC in nearly 80% of cases (2). Many
factors are linked with HCC, such as hepatitis B virus (HBV) and hepatitis C virus (HCV) infection
and non-alcoholic fatty liver disease (3, 4). Clinical detection and management of HCC have
increased in the past decade, but long-term survival levels remain unsatisfactory (5). The previous
study showed that the HCC prediction depends on multiple factors such as patient age (6), tumor size,
tumor quantity, tumor vascular tumor invasion (7, 8), serum alfa-fetoprotein (AFP), and extrahepatic
metastasis involvement (10).
Tumor vascular invasion was known as a macrovascular invasion. It could only be seen through
microscopic inspection, primarily through tiny vessels such as a portal vein, core venous arteries of
noncancerous liver tissue, and venous arteries in the tumor capsule with large-sized and medium-sized
vessels (11,12). The invasion was only observed in the microscopic analysis. Invasion of
microvascular tumors was stated to be the most significant risk factor in postoperative early tuber
recurrence (13-16) and is recognized as a consequence of adverse results following HCC surgical
care. Lim et al. (17) stated that the HCC requirements in Milan after surgical resection are more
prominent tumor recurrence and general survival indicators than those for Milan. A small tumor with
no more than 5 cm or three or fewer will be considered for those following the Milan criterion, with
the tumor maximum measuring no more than 3 cm with no signs of macrovascular or extrahepatic
invasion (7). Lim et al. (17) reported that the average patient survival levels without MVI did not vary
greatly, and the Milan patient requirements were not met under Milan requirements. The average
survival rate declines for MVI but dramatically. An exact preoperative MVI estimation is, therefore,
necessary to prepare for care to avoid recurrence and to optimize patient outcomes.
This research was intended to investigate the association between preoperative clinicopathological
results of patients with a histological outcome in hepatic resection of HCC non-metastasis single
lesion and to seek to identify the risk factor for MVI.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1.2 Epidemiology of hepatocellular carcinoma
HCC is the main malignant neoplasm originating from hepatocytes, responsible for around 80
percent of all liver cancers, and is the most severe main malignant neoplasm in the liver(18). This
cancer, with over seventy thousand deaths worldwide, is the world's fünfth most prevalent cancer-
related illness and the third most severe cause of cancer-related death (1). In Southeast Asia, China,
and tropical Africa (> 10-20 cases/100,000), the highest occurrence of HCC was reported (18, 19). In
Australia, North America and Europe, the lowest occurrence (1-3 cases/100,000) is reported. HCC has
been reported in the United States and other Western countries throughout the past 35 years.
However, recent statistics show that at least in the United States, the outbreak might have peaked and
is now the ninth leading cause of cancer-related deaths in the United States (20). The incidence of
HCC is further enhanced in obese and non-alcoholic steatohepatitis patients. Obesity and its
associated consequences are becoming a significant cause of HCC in Western countries.
Epidemiological data clearly shows that HCC is primarily linked to environmental causes. The
geographic spread of HCC is directly connected to the occurrence of hepatitis B virus (HBV)
infection. In Taiwan, the management of chronic hepatitis B and C under the auspices of the National
Viral Hepatitis Program has culminated in a decrease in prevalence and mortality related to HCC.
HCC is more prevalent in males than females, with a ratio of 2:1 in its worldwide distribution
and 4:1 in the Asia-Pacific region (18, 21). While sex hormones that play a minor role in the
production of HCC, the highest prevalence in humans are likely to be correlated with higher levels of
risk factors, such as HBV infection, cirrhosis, smoking, and alcohol consumption. The age
distribution of HCC ranges from region to region. In general, the frequency of HCC decreases with
age, but the prevalence of HCC at a young age is found in high incidence areas. This may be linked to
various ages of infection and the natural history of hepatitis B and C(22).
1.3 Risk Factor of hepatocellular carcinoma
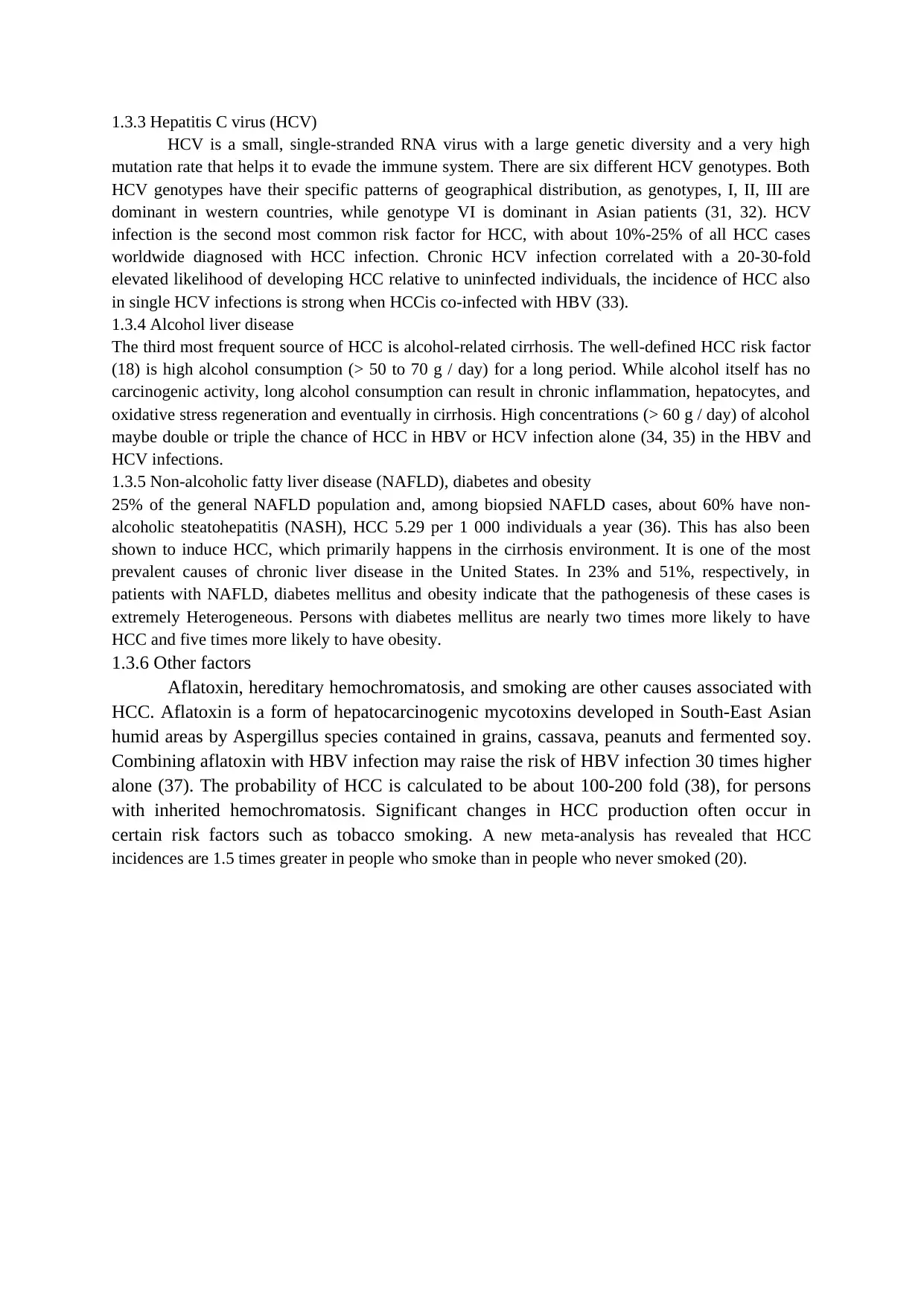
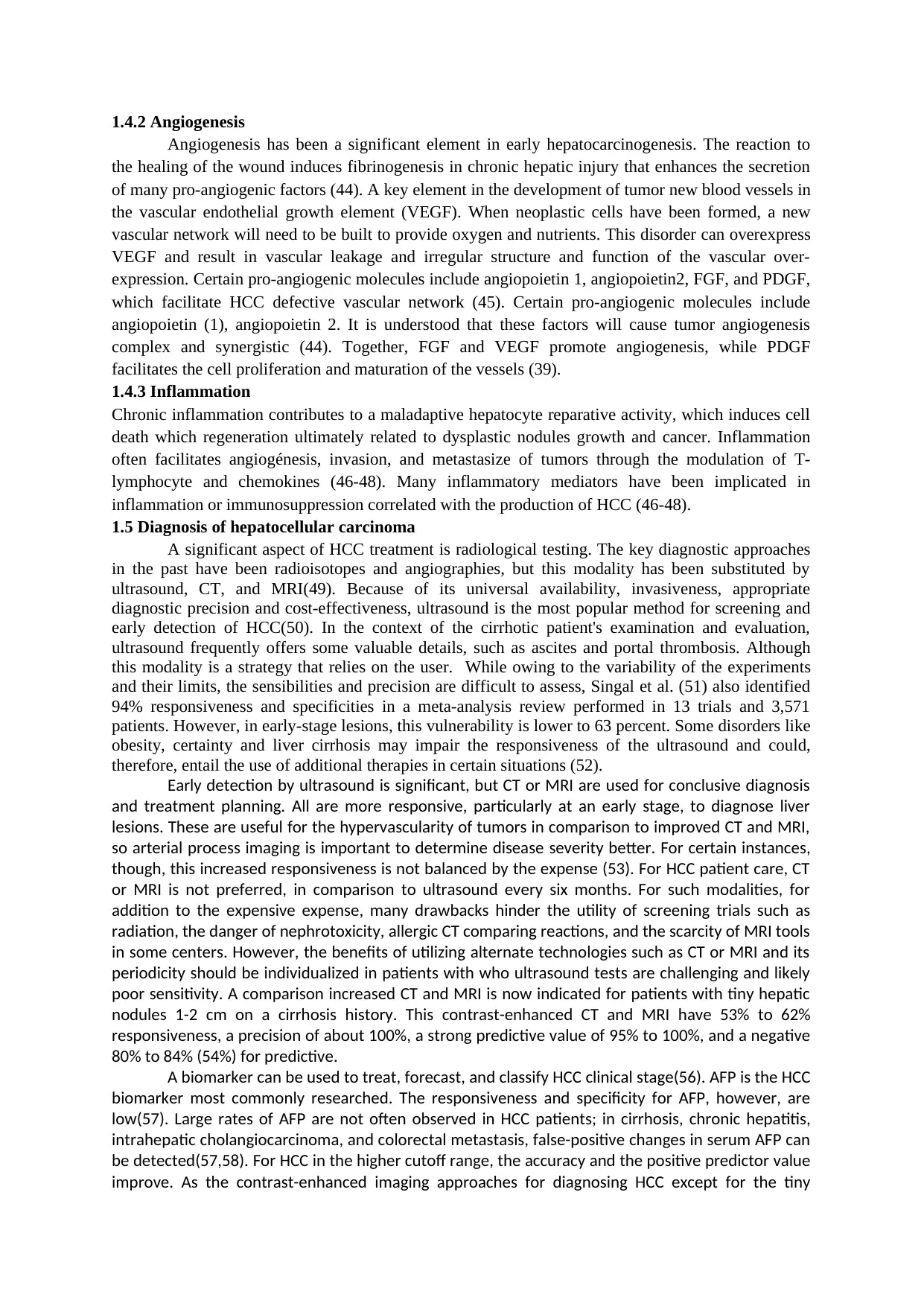
HCC is a chronic disease with several etiological risk factors (Figure 1). About 70% to 90% of HCC
patients have a history of severe liver disease and cirrhosis of the liver, with main risk factors being
hepatitis B virus (HBV), hepatitis C virus (HCV), alcoholic liver disease and non-alcoholic fatty liver
disease (NAFLD) (22, 23). Many risk factors include asthma, hypertension, aflatoxin-contaminated
food, hereditary hemochromatosis, and smoking (21).
1.3.1 Cirrhosis
The link between cirrhosis and primary liver malignancies has been known for a long time. It is
present in about 80 to 90 percent of HCC and plays an important role in HCC growth. Patients with
cirrhosis have raised the chance of HCC more than 30 times (24). One of the most possible causes is
that cirrhosis has a close correlation with several other risk factors contributing to HCC growth, such
as HBV and HCV infection in most of the Asia-Pacific area and alcoholic liver disease in Western
countries (18).
1.3.2 Hepatitis B virus (HBV)
Chronic HBV infection is well known to be linked with HCC. About 50 to 80 percent of HCC
cases worldwide are associated with HBV infection (25). Many meta-analysis reports have found that
the incidence of HCC is 15-20 times higher in HBV infected individuals relative to the uninfected
community, with a mortality rate of about 30 to 50 percent in all instances of persistent HBV infection
(26, 27). In infectious regions such as Southeast Asia, China's transmission of viruses is mainly
through vertical and perinatal penetration relative to developing countries where transmission happens
by sexual and parenteral interaction with contaminated blood, as in the case of intravenous substance
violence. Human HBV is generally divided into ten genotypes (A-J) dependent on its genetic code
(28). Different research has shown that HBV genotypes and mutations are correlated with disease
development and long-term effects of HBV infection. For all genotypes, genotypes C, D and F were
correlated with a greater chance for cirrhosis and HCC (29, 30).
HCC is the main malignant neoplasm originating from hepatocytes, responsible for around 80
percent of all liver cancers, and is the most severe main malignant neoplasm in the liver(18). This
cancer, with over seventy thousand deaths worldwide, is the world's fünfth most prevalent cancer-
related illness and the third most severe cause of cancer-related death (1). In Southeast Asia, China,
and tropical Africa (> 10-20 cases/100,000), the highest occurrence of HCC was reported (18, 19). In
Australia, North America and Europe, the lowest occurrence (1-3 cases/100,000) is reported. HCC has
been reported in the United States and other Western countries throughout the past 35 years.
However, recent statistics show that at least in the United States, the outbreak might have peaked and
is now the ninth leading cause of cancer-related deaths in the United States (20). The incidence of
HCC is further enhanced in obese and non-alcoholic steatohepatitis patients. Obesity and its
associated consequences are becoming a significant cause of HCC in Western countries.
Epidemiological data clearly shows that HCC is primarily linked to environmental causes. The
geographic spread of HCC is directly connected to the occurrence of hepatitis B virus (HBV)
infection. In Taiwan, the management of chronic hepatitis B and C under the auspices of the National
Viral Hepatitis Program has culminated in a decrease in prevalence and mortality related to HCC.
HCC is more prevalent in males than females, with a ratio of 2:1 in its worldwide distribution
and 4:1 in the Asia-Pacific region (18, 21). While sex hormones that play a minor role in the
production of HCC, the highest prevalence in humans are likely to be correlated with higher levels of
risk factors, such as HBV infection, cirrhosis, smoking, and alcohol consumption. The age
distribution of HCC ranges from region to region. In general, the frequency of HCC decreases with
age, but the prevalence of HCC at a young age is found in high incidence areas. This may be linked to
various ages of infection and the natural history of hepatitis B and C(22).
1.3 Risk Factor of hepatocellular carcinoma
HCC is a chronic disease with several etiological risk factors (Figure 1). About 70% to 90% of HCC
patients have a history of severe liver disease and cirrhosis of the liver, with main risk factors being
hepatitis B virus (HBV), hepatitis C virus (HCV), alcoholic liver disease and non-alcoholic fatty liver
disease (NAFLD) (22, 23). Many risk factors include asthma, hypertension, aflatoxin-contaminated
food, hereditary hemochromatosis, and smoking (21).
1.3.1 Cirrhosis
The link between cirrhosis and primary liver malignancies has been known for a long time. It is
present in about 80 to 90 percent of HCC and plays an important role in HCC growth. Patients with
cirrhosis have raised the chance of HCC more than 30 times (24). One of the most possible causes is
that cirrhosis has a close correlation with several other risk factors contributing to HCC growth, such
as HBV and HCV infection in most of the Asia-Pacific area and alcoholic liver disease in Western
countries (18).
1.3.2 Hepatitis B virus (HBV)
Chronic HBV infection is well known to be linked with HCC. About 50 to 80 percent of HCC
cases worldwide are associated with HBV infection (25). Many meta-analysis reports have found that
the incidence of HCC is 15-20 times higher in HBV infected individuals relative to the uninfected
community, with a mortality rate of about 30 to 50 percent in all instances of persistent HBV infection
(26, 27). In infectious regions such as Southeast Asia, China's transmission of viruses is mainly
through vertical and perinatal penetration relative to developing countries where transmission happens
by sexual and parenteral interaction with contaminated blood, as in the case of intravenous substance
violence. Human HBV is generally divided into ten genotypes (A-J) dependent on its genetic code
(28). Different research has shown that HBV genotypes and mutations are correlated with disease
development and long-term effects of HBV infection. For all genotypes, genotypes C, D and F were
correlated with a greater chance for cirrhosis and HCC (29, 30).
1.3.3 Hepatitis C virus (HCV)
HCV is a small, single-stranded RNA virus with a large genetic diversity and a very high
mutation rate that helps it to evade the immune system. There are six different HCV genotypes. Both
HCV genotypes have their specific patterns of geographical distribution, as genotypes, I, II, III are
dominant in western countries, while genotype VI is dominant in Asian patients (31, 32). HCV
infection is the second most common risk factor for HCC, with about 10%-25% of all HCC cases
worldwide diagnosed with HCC infection. Chronic HCV infection correlated with a 20-30-fold
elevated likelihood of developing HCC relative to uninfected individuals, the incidence of HCC also
in single HCV infections is strong when HCCis co-infected with HBV (33).
1.3.4 Alcohol liver disease
The third most frequent source of HCC is alcohol-related cirrhosis. The well-defined HCC risk factor
(18) is high alcohol consumption (> 50 to 70 g / day) for a long period. While alcohol itself has no
carcinogenic activity, long alcohol consumption can result in chronic inflammation, hepatocytes, and
oxidative stress regeneration and eventually in cirrhosis. High concentrations (> 60 g / day) of alcohol
maybe double or triple the chance of HCC in HBV or HCV infection alone (34, 35) in the HBV and
HCV infections.
1.3.5 Non-alcoholic fatty liver disease (NAFLD), diabetes and obesity
25% of the general NAFLD population and, among biopsied NAFLD cases, about 60% have non-
alcoholic steatohepatitis (NASH), HCC 5.29 per 1 000 individuals a year (36). This has also been
shown to induce HCC, which primarily happens in the cirrhosis environment. It is one of the most
prevalent causes of chronic liver disease in the United States. In 23% and 51%, respectively, in
patients with NAFLD, diabetes mellitus and obesity indicate that the pathogenesis of these cases is
extremely Heterogeneous. Persons with diabetes mellitus are nearly two times more likely to have
HCC and five times more likely to have obesity.
1.3.6 Other factors
Aflatoxin, hereditary hemochromatosis, and smoking are other causes associated with
HCC. Aflatoxin is a form of hepatocarcinogenic mycotoxins developed in South-East Asian
humid areas by Aspergillus species contained in grains, cassava, peanuts and fermented soy.
Combining aflatoxin with HBV infection may raise the risk of HBV infection 30 times higher
alone (37). The probability of HCC is calculated to be about 100-200 fold (38), for persons
with inherited hemochromatosis. Significant changes in HCC production often occur in
certain risk factors such as tobacco smoking. A new meta-analysis has revealed that HCC
incidences are 1.5 times greater in people who smoke than in people who never smoked (20).
HCV is a small, single-stranded RNA virus with a large genetic diversity and a very high
mutation rate that helps it to evade the immune system. There are six different HCV genotypes. Both
HCV genotypes have their specific patterns of geographical distribution, as genotypes, I, II, III are
dominant in western countries, while genotype VI is dominant in Asian patients (31, 32). HCV
infection is the second most common risk factor for HCC, with about 10%-25% of all HCC cases
worldwide diagnosed with HCC infection. Chronic HCV infection correlated with a 20-30-fold
elevated likelihood of developing HCC relative to uninfected individuals, the incidence of HCC also
in single HCV infections is strong when HCCis co-infected with HBV (33).
1.3.4 Alcohol liver disease
The third most frequent source of HCC is alcohol-related cirrhosis. The well-defined HCC risk factor
(18) is high alcohol consumption (> 50 to 70 g / day) for a long period. While alcohol itself has no
carcinogenic activity, long alcohol consumption can result in chronic inflammation, hepatocytes, and
oxidative stress regeneration and eventually in cirrhosis. High concentrations (> 60 g / day) of alcohol
maybe double or triple the chance of HCC in HBV or HCV infection alone (34, 35) in the HBV and
HCV infections.
1.3.5 Non-alcoholic fatty liver disease (NAFLD), diabetes and obesity
25% of the general NAFLD population and, among biopsied NAFLD cases, about 60% have non-
alcoholic steatohepatitis (NASH), HCC 5.29 per 1 000 individuals a year (36). This has also been
shown to induce HCC, which primarily happens in the cirrhosis environment. It is one of the most
prevalent causes of chronic liver disease in the United States. In 23% and 51%, respectively, in
patients with NAFLD, diabetes mellitus and obesity indicate that the pathogenesis of these cases is
extremely Heterogeneous. Persons with diabetes mellitus are nearly two times more likely to have
HCC and five times more likely to have obesity.
1.3.6 Other factors
Aflatoxin, hereditary hemochromatosis, and smoking are other causes associated with
HCC. Aflatoxin is a form of hepatocarcinogenic mycotoxins developed in South-East Asian
humid areas by Aspergillus species contained in grains, cassava, peanuts and fermented soy.
Combining aflatoxin with HBV infection may raise the risk of HBV infection 30 times higher
alone (37). The probability of HCC is calculated to be about 100-200 fold (38), for persons
with inherited hemochromatosis. Significant changes in HCC production often occur in
certain risk factors such as tobacco smoking. A new meta-analysis has revealed that HCC
incidences are 1.5 times greater in people who smoke than in people who never smoked (20).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEPATOCELLULAR
CARCINOMA
Genetic Disease
Aflatoxins
HBV
Obesity
Tobacco
Alcohol
Metabolic Syndrome
Obesity
Diabetes
STEATOSIS
NASH
CIRRHOSIS
HCV, HBV
Alcohol
Wilson Disease
NAF
LD
Figure 1. The risk factor of hepatocellular carcinoma
1.4 Pathogenesis of hepatocellular carcinoma
1.4.1 Tumor microenvironment
Hepatocytes experience malignant transformation via tumor killing and apoptosis protection
processes in the pathogenesis of HCC and the development and neovascularization of tumors(21).
Related hepatic injury by oxygen output, cellular DNA disruption, tension at endoplasmic reticular
(ER), and weakened hepatocyte necrosis (39), persistent insults such as HCV, HBV, and alcohol
intake. HCV is an RNA virus with one strand and not inserted into the host genome. However, it can
cause an inflammatory immune reaction that will promote the neoplastic transformation of weakened
hepatocytes. This reaction will be regulated by factors like the tumor necrosis factor (TNF-α) and by
IFNs (40). Contrary to HCV, HBV is a partly double-stranded, circular DNA virus that can be
incorporated into host genomes and promotes infectious, hepatocytic and direct oncogenic
transformation hepatocarcinogenesis(41). The reaction from chronic liver injury includes activation of
macrophages and hepatic stellate cells that generate extracellular matrix components and growth
factors that promote endothelial cell migration, neo-angiogenesis and fibrosis(42). If the fibrosis
emerges from the extracellular matrix (ECM) deposition, it can contribute to the inadequate
distribution of oxygen, which induces cell hypoxia. It may improve the development of tumor growth
factors that stimulate tumor production, and tuber macrophages (TAMs) that suppress anti-tumor
immunity(39, 43), as the hypoxia-inducible-1α (HIF-1α) pro-angiogenic element, a tumor-associated
fibroblast (TAFs).
CARCINOMA
Genetic Disease
Aflatoxins
HBV
Obesity
Tobacco
Alcohol
Metabolic Syndrome
Obesity
Diabetes
STEATOSIS
NASH
CIRRHOSIS
HCV, HBV
Alcohol
Wilson Disease
NAF
LD
Figure 1. The risk factor of hepatocellular carcinoma
1.4 Pathogenesis of hepatocellular carcinoma
1.4.1 Tumor microenvironment
Hepatocytes experience malignant transformation via tumor killing and apoptosis protection
processes in the pathogenesis of HCC and the development and neovascularization of tumors(21).
Related hepatic injury by oxygen output, cellular DNA disruption, tension at endoplasmic reticular
(ER), and weakened hepatocyte necrosis (39), persistent insults such as HCV, HBV, and alcohol
intake. HCV is an RNA virus with one strand and not inserted into the host genome. However, it can
cause an inflammatory immune reaction that will promote the neoplastic transformation of weakened
hepatocytes. This reaction will be regulated by factors like the tumor necrosis factor (TNF-α) and by
IFNs (40). Contrary to HCV, HBV is a partly double-stranded, circular DNA virus that can be
incorporated into host genomes and promotes infectious, hepatocytic and direct oncogenic
transformation hepatocarcinogenesis(41). The reaction from chronic liver injury includes activation of
macrophages and hepatic stellate cells that generate extracellular matrix components and growth
factors that promote endothelial cell migration, neo-angiogenesis and fibrosis(42). If the fibrosis
emerges from the extracellular matrix (ECM) deposition, it can contribute to the inadequate
distribution of oxygen, which induces cell hypoxia. It may improve the development of tumor growth
factors that stimulate tumor production, and tuber macrophages (TAMs) that suppress anti-tumor
immunity(39, 43), as the hypoxia-inducible-1α (HIF-1α) pro-angiogenic element, a tumor-associated
fibroblast (TAFs).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1.4.2 Angiogenesis
Angiogenesis has been a significant element in early hepatocarcinogenesis. The reaction to
the healing of the wound induces fibrinogenesis in chronic hepatic injury that enhances the secretion
of many pro-angiogenic factors (44). A key element in the development of tumor new blood vessels in
the vascular endothelial growth element (VEGF). When neoplastic cells have been formed, a new
vascular network will need to be built to provide oxygen and nutrients. This disorder can overexpress
VEGF and result in vascular leakage and irregular structure and function of the vascular over-
expression. Certain pro-angiogenic molecules include angiopoietin 1, angiopoietin2, FGF, and PDGF,
which facilitate HCC defective vascular network (45). Certain pro-angiogenic molecules include
angiopoietin (1), angiopoietin 2. It is understood that these factors will cause tumor angiogenesis
complex and synergistic (44). Together, FGF and VEGF promote angiogenesis, while PDGF
facilitates the cell proliferation and maturation of the vessels (39).
1.4.3 Inflammation
Chronic inflammation contributes to a maladaptive hepatocyte reparative activity, which induces cell
death which regeneration ultimately related to dysplastic nodules growth and cancer. Inflammation
often facilitates angiogénesis, invasion, and metastasize of tumors through the modulation of T-
lymphocyte and chemokines (46-48). Many inflammatory mediators have been implicated in
inflammation or immunosuppression correlated with the production of HCC (46-48).
1.5 Diagnosis of hepatocellular carcinoma
A significant aspect of HCC treatment is radiological testing. The key diagnostic approaches
in the past have been radioisotopes and angiographies, but this modality has been substituted by
ultrasound, CT, and MRI(49). Because of its universal availability, invasiveness, appropriate
diagnostic precision and cost-effectiveness, ultrasound is the most popular method for screening and
early detection of HCC(50). In the context of the cirrhotic patient's examination and evaluation,
ultrasound frequently offers some valuable details, such as ascites and portal thrombosis. Although
this modality is a strategy that relies on the user. While owing to the variability of the experiments
and their limits, the sensibilities and precision are difficult to assess, Singal et al. (51) also identified
94% responsiveness and specificities in a meta-analysis review performed in 13 trials and 3,571
patients. However, in early-stage lesions, this vulnerability is lower to 63 percent. Some disorders like
obesity, certainty and liver cirrhosis may impair the responsiveness of the ultrasound and could,
therefore, entail the use of additional therapies in certain situations (52).
Early detection by ultrasound is significant, but CT or MRI are used for conclusive diagnosis
and treatment planning. All are more responsive, particularly at an early stage, to diagnose liver
lesions. These are useful for the hypervascularity of tumors in comparison to improved CT and MRI,
so arterial process imaging is important to determine disease severity better. For certain instances,
though, this increased responsiveness is not balanced by the expense (53). For HCC patient care, CT
or MRI is not preferred, in comparison to ultrasound every six months. For such modalities, for
addition to the expensive expense, many drawbacks hinder the utility of screening trials such as
radiation, the danger of nephrotoxicity, allergic CT comparing reactions, and the scarcity of MRI tools
in some centers. However, the benefits of utilizing alternate technologies such as CT or MRI and its
periodicity should be individualized in patients with who ultrasound tests are challenging and likely
poor sensitivity. A comparison increased CT and MRI is now indicated for patients with tiny hepatic
nodules 1-2 cm on a cirrhosis history. This contrast-enhanced CT and MRI have 53% to 62%
responsiveness, a precision of about 100%, a strong predictive value of 95% to 100%, and a negative
80% to 84% (54%) for predictive.
A biomarker can be used to treat, forecast, and classify HCC clinical stage(56). AFP is the HCC
biomarker most commonly researched. The responsiveness and specificity for AFP, however, are
low(57). Large rates of AFP are not often observed in HCC patients; in cirrhosis, chronic hepatitis,
intrahepatic cholangiocarcinoma, and colorectal metastasis, false-positive changes in serum AFP can
be detected(57,58). For HCC in the higher cutoff range, the accuracy and the positive predictor value
improve. As the contrast-enhanced imaging approaches for diagnosing HCC except for the tiny
Angiogenesis has been a significant element in early hepatocarcinogenesis. The reaction to
the healing of the wound induces fibrinogenesis in chronic hepatic injury that enhances the secretion
of many pro-angiogenic factors (44). A key element in the development of tumor new blood vessels in
the vascular endothelial growth element (VEGF). When neoplastic cells have been formed, a new
vascular network will need to be built to provide oxygen and nutrients. This disorder can overexpress
VEGF and result in vascular leakage and irregular structure and function of the vascular over-
expression. Certain pro-angiogenic molecules include angiopoietin 1, angiopoietin2, FGF, and PDGF,
which facilitate HCC defective vascular network (45). Certain pro-angiogenic molecules include
angiopoietin (1), angiopoietin 2. It is understood that these factors will cause tumor angiogenesis
complex and synergistic (44). Together, FGF and VEGF promote angiogenesis, while PDGF
facilitates the cell proliferation and maturation of the vessels (39).
1.4.3 Inflammation
Chronic inflammation contributes to a maladaptive hepatocyte reparative activity, which induces cell
death which regeneration ultimately related to dysplastic nodules growth and cancer. Inflammation
often facilitates angiogénesis, invasion, and metastasize of tumors through the modulation of T-
lymphocyte and chemokines (46-48). Many inflammatory mediators have been implicated in
inflammation or immunosuppression correlated with the production of HCC (46-48).
1.5 Diagnosis of hepatocellular carcinoma
A significant aspect of HCC treatment is radiological testing. The key diagnostic approaches
in the past have been radioisotopes and angiographies, but this modality has been substituted by
ultrasound, CT, and MRI(49). Because of its universal availability, invasiveness, appropriate
diagnostic precision and cost-effectiveness, ultrasound is the most popular method for screening and
early detection of HCC(50). In the context of the cirrhotic patient's examination and evaluation,
ultrasound frequently offers some valuable details, such as ascites and portal thrombosis. Although
this modality is a strategy that relies on the user. While owing to the variability of the experiments
and their limits, the sensibilities and precision are difficult to assess, Singal et al. (51) also identified
94% responsiveness and specificities in a meta-analysis review performed in 13 trials and 3,571
patients. However, in early-stage lesions, this vulnerability is lower to 63 percent. Some disorders like
obesity, certainty and liver cirrhosis may impair the responsiveness of the ultrasound and could,
therefore, entail the use of additional therapies in certain situations (52).
Early detection by ultrasound is significant, but CT or MRI are used for conclusive diagnosis
and treatment planning. All are more responsive, particularly at an early stage, to diagnose liver
lesions. These are useful for the hypervascularity of tumors in comparison to improved CT and MRI,
so arterial process imaging is important to determine disease severity better. For certain instances,
though, this increased responsiveness is not balanced by the expense (53). For HCC patient care, CT
or MRI is not preferred, in comparison to ultrasound every six months. For such modalities, for
addition to the expensive expense, many drawbacks hinder the utility of screening trials such as
radiation, the danger of nephrotoxicity, allergic CT comparing reactions, and the scarcity of MRI tools
in some centers. However, the benefits of utilizing alternate technologies such as CT or MRI and its
periodicity should be individualized in patients with who ultrasound tests are challenging and likely
poor sensitivity. A comparison increased CT and MRI is now indicated for patients with tiny hepatic
nodules 1-2 cm on a cirrhosis history. This contrast-enhanced CT and MRI have 53% to 62%
responsiveness, a precision of about 100%, a strong predictive value of 95% to 100%, and a negative
80% to 84% (54%) for predictive.
A biomarker can be used to treat, forecast, and classify HCC clinical stage(56). AFP is the HCC
biomarker most commonly researched. The responsiveness and specificity for AFP, however, are
low(57). Large rates of AFP are not often observed in HCC patients; in cirrhosis, chronic hepatitis,
intrahepatic cholangiocarcinoma, and colorectal metastasis, false-positive changes in serum AFP can
be detected(57,58). For HCC in the higher cutoff range, the accuracy and the positive predictor value
improve. As the contrast-enhanced imaging approaches for diagnosing HCC except for the tiny
tumor are increased, AFP is still mainly used as a supplementary examination in the patient's hepatic
masses. In the treatment of HCC, only AFP no longer plays a key part but remains valuable in the
surveillance of treated patients following normalization of AFP serum levels for recurrence. Other
biomarkers, des gamma-carboxy prothrombin (DCP), and GPA ratio (L3 fraction) to overall AFP have
also been related to the advanced HCC as well as portal vein invasion, but are currently not
approved as a screening tool because none have been sufficiently tested as monitoring test (59). In
the analysis of the biomarker function in HCC diagnosis, Tunissiolli et al. (60) explain about other
potential biomarkers for HCC diagnostics. Important molecular biomarkers such as GPC3(Glypican-
3), IGF(Insulin-like growth factor), PDGF(Growing Factor), PDGF(Rapamycin Mammalian Target),
Osteopontin, VGF and microRNAs are likely candidates to be clinically tested in the future. Such
important molecular Biomarkers include GPC3 (Glypican-3), GP73 (Golgi Protein 73).
If HCC has been established, an appropriate care strategy will be created for this condition.
The patient's longevity is also directly linked to cirrhosis. Stadium construction requires a degree of
the disease and duration of the function. In terms of the care choice in the HCC case, liver function
evaluation is utterly important. Liver resection is viewed as an alternative for HCC care, the
possibility of liver failure and death following surgery needs to be weighed.
1.6 Staging of hepatocellular carcinoma
1.6.1 Okuda staging
Okuda et al. proposed this staging method in 1984(61). This method is the first to excel in integrating
both tumors and liver function, arising from a retrospective study of 600 HCC patients in Japan and
its roots. Okuda divides HCC into three stages, which are not advanced, modest and highly evolved.
Along with the role of the liver in albumin, bilirubin, and the involvement of ascites, tumor volumes
are known to be less than 50% by level. This device has been in operation globally for more than two
decades since the advancement of diagnostic methods, the tiny tumor which is less than 50 percent
tumor volume may be identified easier, a modern, more precise staging method from the Okuda is no
longer effective and has been developed[62].
1.6.2 Cancer of the Liver Italian Program score (CLIP)
CLIP is an Italian group's basic device architecture to solve Okuda's staging framework constraints.
Combined with the Child-Pugh score, the morphology of the tumor, AFP frequency less than or
greater than four hundred μg / L and Portal Venal Thrombosis. The approach splits the individual into
six groups. Only this scoring system was designed with the appropriate process, but some drawbacks
were also identified. Much of the research patients provided regional care such as PEI and TACE,
with surgical resection in just 2.8 percent of the test subject, so this rating method is not appropriate
for estimating the survival of the patients who receive surgical resection treatment (63-65).
1.6.3 GRETCH system
GRETCH in 1999, along with BCLC from Barcelona, was suggested by Grouped'Etude from France.
Karnofsky Index blends Karnofsky Index < 80% and Serum Bilirubin < 50 μmol / L or Karnofsky
Index < 80%, Serum alkaline Phosphatase (ALP), Serum AFP, and portal restriction presence or
absence of ultrasound inputs. Patients with a varying1-year mortality rate (79%, 34%, and 7%) are
categorized into three categories with small death risk, a moderate death risk, and a strong death risk
(66).
1.6.4 Barcelona clinic liver cancer (BCLC)
First introduced by the American Association for the Treatment of Liver Disease, the American
Society Gastroenterology Society, the European Liver Science Group and the EU Organisation for
Analysis and Treatments for Cancer(67) in 1999, it was revised in 2003 and 2008 until now endorsed
as the basic method of HCC management. Within this categorization, the tumor-type liver activity,
Child pugh-score, physical condition, and signs linked to cancer are classified into five groups (0, A,
B, C and D). For each level, this distinction often provides a clinical guideline focused upon existing
care options such as surgical resection, liver transplantation and stages0 and A ablation. For stage B
masses. In the treatment of HCC, only AFP no longer plays a key part but remains valuable in the
surveillance of treated patients following normalization of AFP serum levels for recurrence. Other
biomarkers, des gamma-carboxy prothrombin (DCP), and GPA ratio (L3 fraction) to overall AFP have
also been related to the advanced HCC as well as portal vein invasion, but are currently not
approved as a screening tool because none have been sufficiently tested as monitoring test (59). In
the analysis of the biomarker function in HCC diagnosis, Tunissiolli et al. (60) explain about other
potential biomarkers for HCC diagnostics. Important molecular biomarkers such as GPC3(Glypican-
3), IGF(Insulin-like growth factor), PDGF(Growing Factor), PDGF(Rapamycin Mammalian Target),
Osteopontin, VGF and microRNAs are likely candidates to be clinically tested in the future. Such
important molecular Biomarkers include GPC3 (Glypican-3), GP73 (Golgi Protein 73).
If HCC has been established, an appropriate care strategy will be created for this condition.
The patient's longevity is also directly linked to cirrhosis. Stadium construction requires a degree of
the disease and duration of the function. In terms of the care choice in the HCC case, liver function
evaluation is utterly important. Liver resection is viewed as an alternative for HCC care, the
possibility of liver failure and death following surgery needs to be weighed.
1.6 Staging of hepatocellular carcinoma
1.6.1 Okuda staging
Okuda et al. proposed this staging method in 1984(61). This method is the first to excel in integrating
both tumors and liver function, arising from a retrospective study of 600 HCC patients in Japan and
its roots. Okuda divides HCC into three stages, which are not advanced, modest and highly evolved.
Along with the role of the liver in albumin, bilirubin, and the involvement of ascites, tumor volumes
are known to be less than 50% by level. This device has been in operation globally for more than two
decades since the advancement of diagnostic methods, the tiny tumor which is less than 50 percent
tumor volume may be identified easier, a modern, more precise staging method from the Okuda is no
longer effective and has been developed[62].
1.6.2 Cancer of the Liver Italian Program score (CLIP)
CLIP is an Italian group's basic device architecture to solve Okuda's staging framework constraints.
Combined with the Child-Pugh score, the morphology of the tumor, AFP frequency less than or
greater than four hundred μg / L and Portal Venal Thrombosis. The approach splits the individual into
six groups. Only this scoring system was designed with the appropriate process, but some drawbacks
were also identified. Much of the research patients provided regional care such as PEI and TACE,
with surgical resection in just 2.8 percent of the test subject, so this rating method is not appropriate
for estimating the survival of the patients who receive surgical resection treatment (63-65).
1.6.3 GRETCH system
GRETCH in 1999, along with BCLC from Barcelona, was suggested by Grouped'Etude from France.
Karnofsky Index blends Karnofsky Index < 80% and Serum Bilirubin < 50 μmol / L or Karnofsky
Index < 80%, Serum alkaline Phosphatase (ALP), Serum AFP, and portal restriction presence or
absence of ultrasound inputs. Patients with a varying1-year mortality rate (79%, 34%, and 7%) are
categorized into three categories with small death risk, a moderate death risk, and a strong death risk
(66).
1.6.4 Barcelona clinic liver cancer (BCLC)
First introduced by the American Association for the Treatment of Liver Disease, the American
Society Gastroenterology Society, the European Liver Science Group and the EU Organisation for
Analysis and Treatments for Cancer(67) in 1999, it was revised in 2003 and 2008 until now endorsed
as the basic method of HCC management. Within this categorization, the tumor-type liver activity,
Child pugh-score, physical condition, and signs linked to cancer are classified into five groups (0, A,
B, C and D). For each level, this distinction often provides a clinical guideline focused upon existing
care options such as surgical resection, liver transplantation and stages0 and A ablation. For stage B
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
patients, TACE is advised, and enabling care for stage C patients is suggested, including sorafenib
and multikinase inhibitor. There are still certain drawbacks to even the BCLC staging. First, it is quite
difficult to use physical standing. Secondly, in actual realistic circumstances, the treatment guideline
for any BCLC level, particularly in patients, might not be sufficient for combination care. Third, stage
B in BCLC phases is heterogeneous and results in the expected variability of this category from
patients with various tumor extensions.
In 2012, Bolondi et al. (68) proposed sub-classing Stage B to address the question of variability in this
community, splitting Stage B into B1-B4 along with different first-line care choices. The new HCC
cohort patients in Taiwan and South Korea (69, 70) have confirmed this subclassification.
1.6.5 Chinese University Prognostic Index (CUPI)
The Hong Kong group introduced CUPI in 2002 and is a cluster of 926 HCC patients seen in one
Hong Kong hospital(71). The finding is obtained from the TNM staging system in combination with
five other prognostic variables, such as complete serum bilirubin, ascites, serum ALP, serum AFP,
and asymptomatic illness. The overall score classified patients into three categories, low risk, medium
risk, and high risk. As a consequence of patients suffering from certain HBV infections in Hong Kong
(79 percent of all patients with cohort disease), this program may not be appropriate for western
communities with a higher incidence of HCV and drug history (72).
1.6.6 TNM classification
The classifications of the TNMs were first reported in 1997 by the American Joint Committee on
Cancer (AJCC) and the International Union for Cancer Control (UICC). This is based on the
prolongation of the main tumor (T), the presence of the lymph node (N) and extrahepatic metastases
(M). By contrast analysis, BCLC was superior to the TNM classification method by stratification and
forecasting, and for stage III population subgroups, the precision of stratification was lost (73).
1.6.7 Japan Integrated Staging Score (JIS score)
Kudo et al. (74)in 2003 indicated the JIS ranking. It consists of 722 patients undergoing HCC care in
two Japanese hospitals. Patients that were graded for categories A, B, and C of Child-Pugh for
corresponding grades 0, 1 and 2. The Liver Cancer Group (LCSGJ) TNM stadium from the stadium I,
II, III, IV shall rate respectively0, 1, 2, 3. Patients are categorized into six categories (0 to 5) by the
average of such ratings. In 2004, this JIS ranking had been checked in a Japanese multicentre, but, in
Western countries, before now (75).
1.7 Invasion and metastasis of hepatocellular carcinoma
HCC is a disease that is very neovascular and is a popular disorder of the HCC vascular invasion.
Macrovascular invasion indicates that the tumor may invade broad vascularization and be established
by picture examination and histology and this form of invasion holds a very weak pronouncement
during homeopathy or transplantation. The appearance of a vascular invasion can be a macrovascular
invasión or microvascular invasion. The Portal Vein Tumor Thrombus (PVTT) is more common than
hepatic venous tumor thrombus of any form of macrovascular invasion, which is attributable to
irregular vein drainage that develops from the hepatic veins into the portal venous during
hepatocarcinogenesis. In BCLC stadiums, macrovascular invasion patient evaluation and care are
focused on PVTT cases, who are found in advanced phase tumors along with metastasizing tumors
that are very poor in median survival (2-4 months) in contrast to PVTT cases (10-24 months). PVTT
and hepatic vein tumor thrombus may be the best predictor for tumor recurrence after hepatic or liver
transplantation treatment in patients without any extrahepatic metastasis, as vascular infiltrating
correlates with systemic tumor dissemination. Liver Cancer Trial Community of Japan has developed
the classification of PVTT in 4 groups by thrombus scope: Vp1 is identified by PVTT presence in the
distal branches, but not in the second branches of the portal vein, Vp3 is described by PVTT presence
in the other branches of the portal vein. Unlike a macrovascular invasion, microvascular invasion
(MVI), since this vascular invasion invades the tiny vascular liver, can only be established by
and multikinase inhibitor. There are still certain drawbacks to even the BCLC staging. First, it is quite
difficult to use physical standing. Secondly, in actual realistic circumstances, the treatment guideline
for any BCLC level, particularly in patients, might not be sufficient for combination care. Third, stage
B in BCLC phases is heterogeneous and results in the expected variability of this category from
patients with various tumor extensions.
In 2012, Bolondi et al. (68) proposed sub-classing Stage B to address the question of variability in this
community, splitting Stage B into B1-B4 along with different first-line care choices. The new HCC
cohort patients in Taiwan and South Korea (69, 70) have confirmed this subclassification.
1.6.5 Chinese University Prognostic Index (CUPI)
The Hong Kong group introduced CUPI in 2002 and is a cluster of 926 HCC patients seen in one
Hong Kong hospital(71). The finding is obtained from the TNM staging system in combination with
five other prognostic variables, such as complete serum bilirubin, ascites, serum ALP, serum AFP,
and asymptomatic illness. The overall score classified patients into three categories, low risk, medium
risk, and high risk. As a consequence of patients suffering from certain HBV infections in Hong Kong
(79 percent of all patients with cohort disease), this program may not be appropriate for western
communities with a higher incidence of HCV and drug history (72).
1.6.6 TNM classification
The classifications of the TNMs were first reported in 1997 by the American Joint Committee on
Cancer (AJCC) and the International Union for Cancer Control (UICC). This is based on the
prolongation of the main tumor (T), the presence of the lymph node (N) and extrahepatic metastases
(M). By contrast analysis, BCLC was superior to the TNM classification method by stratification and
forecasting, and for stage III population subgroups, the precision of stratification was lost (73).
1.6.7 Japan Integrated Staging Score (JIS score)
Kudo et al. (74)in 2003 indicated the JIS ranking. It consists of 722 patients undergoing HCC care in
two Japanese hospitals. Patients that were graded for categories A, B, and C of Child-Pugh for
corresponding grades 0, 1 and 2. The Liver Cancer Group (LCSGJ) TNM stadium from the stadium I,
II, III, IV shall rate respectively0, 1, 2, 3. Patients are categorized into six categories (0 to 5) by the
average of such ratings. In 2004, this JIS ranking had been checked in a Japanese multicentre, but, in
Western countries, before now (75).
1.7 Invasion and metastasis of hepatocellular carcinoma
HCC is a disease that is very neovascular and is a popular disorder of the HCC vascular invasion.
Macrovascular invasion indicates that the tumor may invade broad vascularization and be established
by picture examination and histology and this form of invasion holds a very weak pronouncement
during homeopathy or transplantation. The appearance of a vascular invasion can be a macrovascular
invasión or microvascular invasion. The Portal Vein Tumor Thrombus (PVTT) is more common than
hepatic venous tumor thrombus of any form of macrovascular invasion, which is attributable to
irregular vein drainage that develops from the hepatic veins into the portal venous during
hepatocarcinogenesis. In BCLC stadiums, macrovascular invasion patient evaluation and care are
focused on PVTT cases, who are found in advanced phase tumors along with metastasizing tumors
that are very poor in median survival (2-4 months) in contrast to PVTT cases (10-24 months). PVTT
and hepatic vein tumor thrombus may be the best predictor for tumor recurrence after hepatic or liver
transplantation treatment in patients without any extrahepatic metastasis, as vascular infiltrating
correlates with systemic tumor dissemination. Liver Cancer Trial Community of Japan has developed
the classification of PVTT in 4 groups by thrombus scope: Vp1 is identified by PVTT presence in the
distal branches, but not in the second branches of the portal vein, Vp3 is described by PVTT presence
in the other branches of the portal vein. Unlike a macrovascular invasion, microvascular invasion
(MVI), since this vascular invasion invades the tiny vascular liver, can only be established by
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

histology examination underneath a microscope and is related to the violent action of the tumor. MVI
is also generally recognized as a significant indicator of HCC in curative treatment such as hepatic
resection and liver transplants. This MVI is an initial indication of tumor cell proliferation through the
peritumoral channels and is considered the main pathway for the spread of the intrahepatic tumor.
Research suggests that MVI may be of benefit during surgery when making surgical decisions. For
instance, Mazzaferro et al. (77) revealed in 2009 that there was no substantial variation in the usage of
Milan parameters and MVI negative patients for the five-year survivor's rate following liver
transplantation. Zhao et al. (78) and fan et al. (79) have observed that the incidence of disease-free
survival of MVI anatomical HCC relative to non-anatomical hepatectomy was higher in 2017. An
additional retrospective multi-center analysis in 2019 revealed the long disease-free overall survival
and survival of HCC with successful resection of MVI with large operative limits (80). The
probability of prediction of MVI, therefore, found it to be critical for patients with HCC to make
clinical decisions. Huang et al. (81) analysis showed that MVI occurrence increased by tumor growth,
such as broad tumor sizes, numerous nodules, low tumor variance and advanced BCLC levels in
HCC. Although MVI is a significant indicator of patient survival after procedures, this research has
demonstrated that MvI does not necessarily influence the overall prognosis of patients, it may impact
some patients at certain tumor stages. MVI was not correlated with OS or RFS11, 25, 26 in patients
with BCLC stage 0 (single tumor: 2 cm). Anatomical resection was most probably in the very early
stages of HCC to eliminate the part of the tumor-bearable portal and the tumor nodule eliminated the
risk for MVI. The independent risk factors for OS in patients with BCLC Stage 0 are the age and low
albumin. No tumor factor may serve as the key risk factor in long-term survival. But the univariate
and multivariate study of patients at BCLC stage A indicated that both OS and RFS are correlated
with MVI. MVI is a significant biologic tumor character impacting the recurrence of the tumor and its
ultimate survival. It has prompted us to suggest treating patients with and one MVI and to take
account of patients ' MVI circumstances of the composition of adjuvant therapeutic approaches. MVI
has been separately related to RFS, but not to OS in BCLCstage B patients. While MVI raises the risk
of tumor recurrence in such patients, other factors such as AFP and β-GT may weaken their long-term
contribution to survival.
1.8 Inflammation response factor in hepatocellular carcinoma and its correlation with vascular
invasion
From the history of HCC pathogenesis of the micro-environmental tumor pathway that gradually
transforms the hepatocyte to the malignant tumour, the angiogenesis of the tumor-induced by VEGF
and PDGF, the function of the inflammatory response in apoptosis and cell regeneration and, by
regulators of T lymphocytes and chemokines, tumor angiogenesis, invasion and metastases(46-48). It
has shown a significant function in the production and progression of HCC in the inflammatory
response(82, 83). The chronic inflammatory reaction is the main cause of HCC in patients diagnosed
with HBV and HCV. With inflammation in the production and advancement of HCC, the HCC patient
results from a systemic inflammatory response factor may be expected. Inflammatory response and
metastases of cancer cells, neutrophils and lymphocytes became the main white blood cells. There is
also proof of substantial bio-markers with low forecasting in other cancers, like the HCC, the
neutrophil to lymphocyte (NLR) and the platelet/lymphocyte ratio (PLR It allows for the estimation of
vascular tumor invasion with systemic inflammatory response, but the connection of these variables is
not much researched. In 2017 Yu et al. (84) have noticed that preoperative NLR can be a reliable
biomarker for HCC MVI prediction. Several research has revealed that PLR in MVI patients is higher
than in non-MVI patients. However, fewer studies suggest that the estimate in MVI has a cut-off
value for PLR. In 2018, Rungsakulkij et al. (85) noticed that more than 102 PLRs were an effective
MVI indicator. Nonetheless, Ma et al. (86) found no connection between systemic inflammatory
reactions responses with vascular invasion in HCC in the meta-analysis.
is also generally recognized as a significant indicator of HCC in curative treatment such as hepatic
resection and liver transplants. This MVI is an initial indication of tumor cell proliferation through the
peritumoral channels and is considered the main pathway for the spread of the intrahepatic tumor.
Research suggests that MVI may be of benefit during surgery when making surgical decisions. For
instance, Mazzaferro et al. (77) revealed in 2009 that there was no substantial variation in the usage of
Milan parameters and MVI negative patients for the five-year survivor's rate following liver
transplantation. Zhao et al. (78) and fan et al. (79) have observed that the incidence of disease-free
survival of MVI anatomical HCC relative to non-anatomical hepatectomy was higher in 2017. An
additional retrospective multi-center analysis in 2019 revealed the long disease-free overall survival
and survival of HCC with successful resection of MVI with large operative limits (80). The
probability of prediction of MVI, therefore, found it to be critical for patients with HCC to make
clinical decisions. Huang et al. (81) analysis showed that MVI occurrence increased by tumor growth,
such as broad tumor sizes, numerous nodules, low tumor variance and advanced BCLC levels in
HCC. Although MVI is a significant indicator of patient survival after procedures, this research has
demonstrated that MvI does not necessarily influence the overall prognosis of patients, it may impact
some patients at certain tumor stages. MVI was not correlated with OS or RFS11, 25, 26 in patients
with BCLC stage 0 (single tumor: 2 cm). Anatomical resection was most probably in the very early
stages of HCC to eliminate the part of the tumor-bearable portal and the tumor nodule eliminated the
risk for MVI. The independent risk factors for OS in patients with BCLC Stage 0 are the age and low
albumin. No tumor factor may serve as the key risk factor in long-term survival. But the univariate
and multivariate study of patients at BCLC stage A indicated that both OS and RFS are correlated
with MVI. MVI is a significant biologic tumor character impacting the recurrence of the tumor and its
ultimate survival. It has prompted us to suggest treating patients with and one MVI and to take
account of patients ' MVI circumstances of the composition of adjuvant therapeutic approaches. MVI
has been separately related to RFS, but not to OS in BCLCstage B patients. While MVI raises the risk
of tumor recurrence in such patients, other factors such as AFP and β-GT may weaken their long-term
contribution to survival.
1.8 Inflammation response factor in hepatocellular carcinoma and its correlation with vascular
invasion
From the history of HCC pathogenesis of the micro-environmental tumor pathway that gradually
transforms the hepatocyte to the malignant tumour, the angiogenesis of the tumor-induced by VEGF
and PDGF, the function of the inflammatory response in apoptosis and cell regeneration and, by
regulators of T lymphocytes and chemokines, tumor angiogenesis, invasion and metastases(46-48). It
has shown a significant function in the production and progression of HCC in the inflammatory
response(82, 83). The chronic inflammatory reaction is the main cause of HCC in patients diagnosed
with HBV and HCV. With inflammation in the production and advancement of HCC, the HCC patient
results from a systemic inflammatory response factor may be expected. Inflammatory response and
metastases of cancer cells, neutrophils and lymphocytes became the main white blood cells. There is
also proof of substantial bio-markers with low forecasting in other cancers, like the HCC, the
neutrophil to lymphocyte (NLR) and the platelet/lymphocyte ratio (PLR It allows for the estimation of
vascular tumor invasion with systemic inflammatory response, but the connection of these variables is
not much researched. In 2017 Yu et al. (84) have noticed that preoperative NLR can be a reliable
biomarker for HCC MVI prediction. Several research has revealed that PLR in MVI patients is higher
than in non-MVI patients. However, fewer studies suggest that the estimate in MVI has a cut-off
value for PLR. In 2018, Rungsakulkij et al. (85) noticed that more than 102 PLRs were an effective
MVI indicator. Nonetheless, Ma et al. (86) found no connection between systemic inflammatory
reactions responses with vascular invasion in HCC in the meta-analysis.
1.9Biomarker in hepatocellular carcinoma and its correlation with vascular invasion
For the early identification of HCC, AFP is the most widely employed biomarker. In certain
HCC and other gastrointestinal tumors, this 70-KDa glycoprotein tumor marker was elevated. This
rise is attributed to tumor growth or hepatocyte regeneration. Thus, the amount of AFP in persistent
hepatitis is often raised. This indicated that AFP was unsatisfactorily reactive and precise when HCC
was measured in the early stages; a cut-off value of 20 μg / L could only provide 41-64% sensitivity
and 80-94% (87). ). It was discovered that AFP produces three glycoforms (AFP-L1, AFP-L2 and
AFP-L3) in the production and analysis of AFP. This AFP-L3 is great at detecting HCC early and can
reach 96.2 percent responsiveness and 92 percent accuracy (88), with a cut-off of 15 percent. AFP rise
or healthy tumor AFP-L3 can be used to differentiate between the change in AFP and AFP. Several
experiments have shown that AFP is a stand-alone risk factor for MVI in the identification of MVI,
but the precise cutoff value for predicting MVI is different. In a retrospective review of the patients
that have been affected by liver resection, Fan & al. (79) proposed MvI > 100 μg / Lpredictors (P=
0.004) and Zhao et al. (89) proposed the AFP > 400 μg / L predicting the AFP (P=0.016). There are,
however, minimal MVI detection data concerning AFP-L3.
In addition to a vitamin, K absence protein and antagonist-II (PIVKA-II) mediated protein,
also known as des-μ-carbsyprothrombin (DCP), are another essential biomarker that can be used in
early detection of HCC. An irregular prothrombin protein is detected at higher serum concentrations
in HCC patients than in chronic hepatitis and cirrhosis patients. In contrast to AFP alone, the
diagnostic accuracy of PIVKA-II is higher. The use of AFP and PIVKA-II would also improve the
early detection of responsiveness and specificity for HCC by 47,5%-94% and 53,3%-98,5%. This is
stronger compared to the usage of PIVKA-II or AFP alone. PIVKA-II is an indie risk factor of MVI in
lone HCC, as demonstrated by Hirokawa et al. (90). In the other Yamashita research, (91) PIVKA-II
oscillating to 40 mAU / mL can predict MVI in HCC with less than 3 cm diameters, combined with a
tumor diameter of 2 cm and AFP oscillating to 200 μg / L.
Other biomarkers, such as HSP 70, HSP 90, alpha-enolase(Eno-1), Annexin A2, glutathione synthetic
and beta-actin, have been established to assess MVI in HCC before surgical procedure. Only HSP 70
and Eno-1 have the main biomarker for predicting MVI in HCC, but further studies for these specific
agents are still required (92).
1.10 Imaging modality in the vascular invasion of HCC
In the hepatocellular detection of MVI, certain imaging modalities, including computed tomography
enhanced by contrast (CT), magnetic resonance imaging (MRI), ultrasonography enhanced by
contrast (CEUS) and Positron Computing Tomography (PET), play a role.
1.10.1 Contrast-enhanced CT
Contrast-enhanced CT is a valuable extremely responsive imaging modality that allows hypervascular
HCC detection to be limited to 3 mm (93, 1994). During contrast injection, the Multiphase CT liver
scan contained a late arterial stage shortly after contrast injection (approximately 20 seconds after
contrast injection), the portal vein period (50 seconds after contrast injection) and the delayed process
(2 to 5 minutes after contrast injection). It is best to deliver contrasting content using a mechanical
injector and a saline flush to obtain a nominal injection speed of 3 mL/sec with a minimum of 370 mg
/ mL of contrast. Characteristically, during the arterial process, HCC has changed regardless of the
irregular hepatic blood flow. At this time, the contrast of the underlying liver parenchyma would be
reduced as the accessible veins which are not yet filtered are the most frequent source of the
Parenchymal blood supply. Throughout the portal venous process, the liver parenchyma in the
peripheral region becomes comparatively hyperattenuating and owing to its absence of portal venous
For the early identification of HCC, AFP is the most widely employed biomarker. In certain
HCC and other gastrointestinal tumors, this 70-KDa glycoprotein tumor marker was elevated. This
rise is attributed to tumor growth or hepatocyte regeneration. Thus, the amount of AFP in persistent
hepatitis is often raised. This indicated that AFP was unsatisfactorily reactive and precise when HCC
was measured in the early stages; a cut-off value of 20 μg / L could only provide 41-64% sensitivity
and 80-94% (87). ). It was discovered that AFP produces three glycoforms (AFP-L1, AFP-L2 and
AFP-L3) in the production and analysis of AFP. This AFP-L3 is great at detecting HCC early and can
reach 96.2 percent responsiveness and 92 percent accuracy (88), with a cut-off of 15 percent. AFP rise
or healthy tumor AFP-L3 can be used to differentiate between the change in AFP and AFP. Several
experiments have shown that AFP is a stand-alone risk factor for MVI in the identification of MVI,
but the precise cutoff value for predicting MVI is different. In a retrospective review of the patients
that have been affected by liver resection, Fan & al. (79) proposed MvI > 100 μg / Lpredictors (P=
0.004) and Zhao et al. (89) proposed the AFP > 400 μg / L predicting the AFP (P=0.016). There are,
however, minimal MVI detection data concerning AFP-L3.
In addition to a vitamin, K absence protein and antagonist-II (PIVKA-II) mediated protein,
also known as des-μ-carbsyprothrombin (DCP), are another essential biomarker that can be used in
early detection of HCC. An irregular prothrombin protein is detected at higher serum concentrations
in HCC patients than in chronic hepatitis and cirrhosis patients. In contrast to AFP alone, the
diagnostic accuracy of PIVKA-II is higher. The use of AFP and PIVKA-II would also improve the
early detection of responsiveness and specificity for HCC by 47,5%-94% and 53,3%-98,5%. This is
stronger compared to the usage of PIVKA-II or AFP alone. PIVKA-II is an indie risk factor of MVI in
lone HCC, as demonstrated by Hirokawa et al. (90). In the other Yamashita research, (91) PIVKA-II
oscillating to 40 mAU / mL can predict MVI in HCC with less than 3 cm diameters, combined with a
tumor diameter of 2 cm and AFP oscillating to 200 μg / L.
Other biomarkers, such as HSP 70, HSP 90, alpha-enolase(Eno-1), Annexin A2, glutathione synthetic
and beta-actin, have been established to assess MVI in HCC before surgical procedure. Only HSP 70
and Eno-1 have the main biomarker for predicting MVI in HCC, but further studies for these specific
agents are still required (92).
1.10 Imaging modality in the vascular invasion of HCC
In the hepatocellular detection of MVI, certain imaging modalities, including computed tomography
enhanced by contrast (CT), magnetic resonance imaging (MRI), ultrasonography enhanced by
contrast (CEUS) and Positron Computing Tomography (PET), play a role.
1.10.1 Contrast-enhanced CT
Contrast-enhanced CT is a valuable extremely responsive imaging modality that allows hypervascular
HCC detection to be limited to 3 mm (93, 1994). During contrast injection, the Multiphase CT liver
scan contained a late arterial stage shortly after contrast injection (approximately 20 seconds after
contrast injection), the portal vein period (50 seconds after contrast injection) and the delayed process
(2 to 5 minutes after contrast injection). It is best to deliver contrasting content using a mechanical
injector and a saline flush to obtain a nominal injection speed of 3 mL/sec with a minimum of 370 mg
/ mL of contrast. Characteristically, during the arterial process, HCC has changed regardless of the
irregular hepatic blood flow. At this time, the contrast of the underlying liver parenchyma would be
reduced as the accessible veins which are not yet filtered are the most frequent source of the
Parenchymal blood supply. Throughout the portal venous process, the liver parenchyma in the
peripheral region becomes comparatively hyperattenuating and owing to its absence of portal venous
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
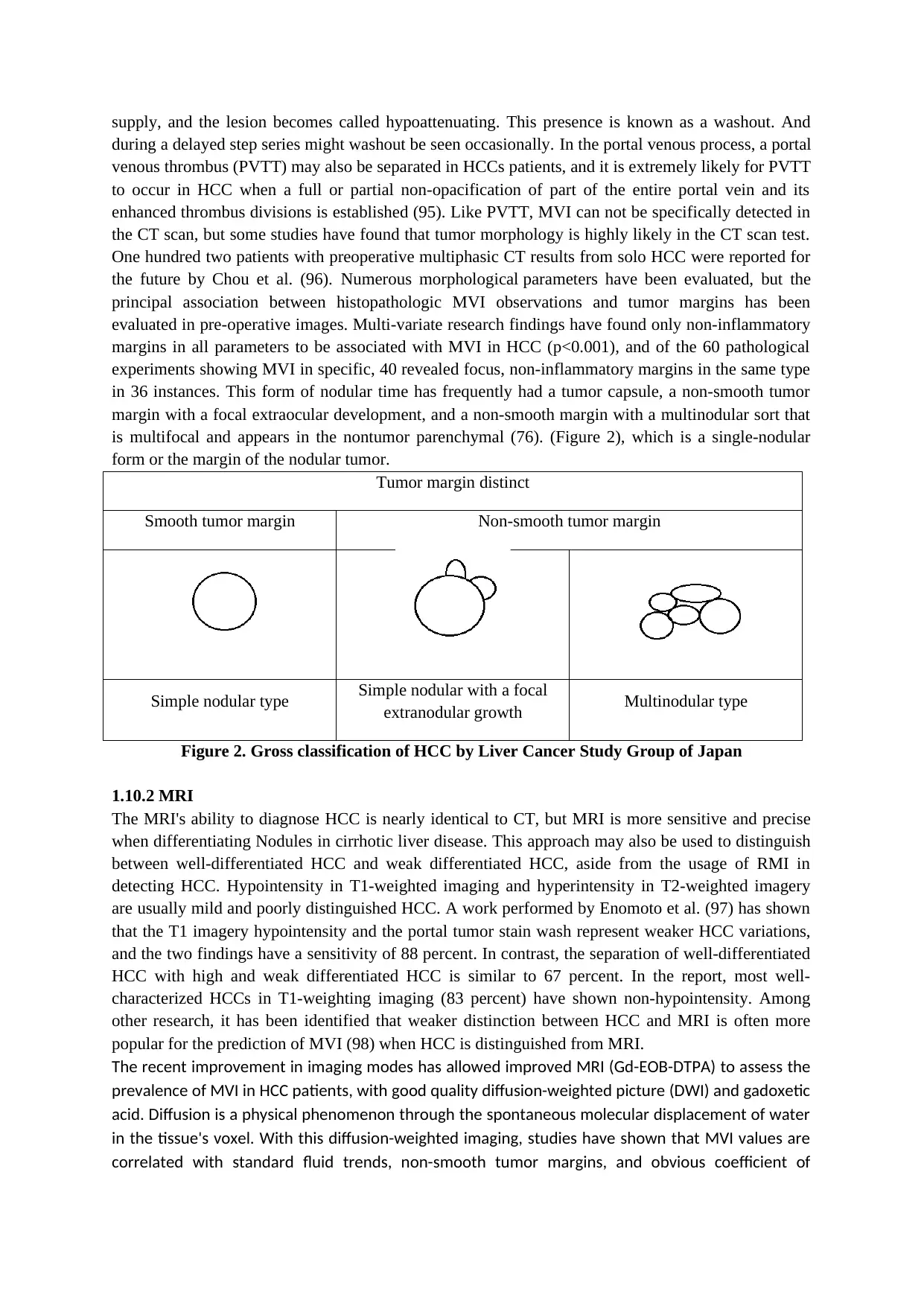
supply, and the lesion becomes called hypoattenuating. This presence is known as a washout. And
during a delayed step series might washout be seen occasionally. In the portal venous process, a portal
venous thrombus (PVTT) may also be separated in HCCs patients, and it is extremely likely for PVTT
to occur in HCC when a full or partial non-opacification of part of the entire portal vein and its
enhanced thrombus divisions is established (95). Like PVTT, MVI can not be specifically detected in
the CT scan, but some studies have found that tumor morphology is highly likely in the CT scan test.
One hundred two patients with preoperative multiphasic CT results from solo HCC were reported for
the future by Chou et al. (96). Numerous morphological parameters have been evaluated, but the
principal association between histopathologic MVI observations and tumor margins has been
evaluated in pre-operative images. Multi-variate research findings have found only non-inflammatory
margins in all parameters to be associated with MVI in HCC (p<0.001), and of the 60 pathological
experiments showing MVI in specific, 40 revealed focus, non-inflammatory margins in the same type
in 36 instances. This form of nodular time has frequently had a tumor capsule, a non-smooth tumor
margin with a focal extraocular development, and a non-smooth margin with a multinodular sort that
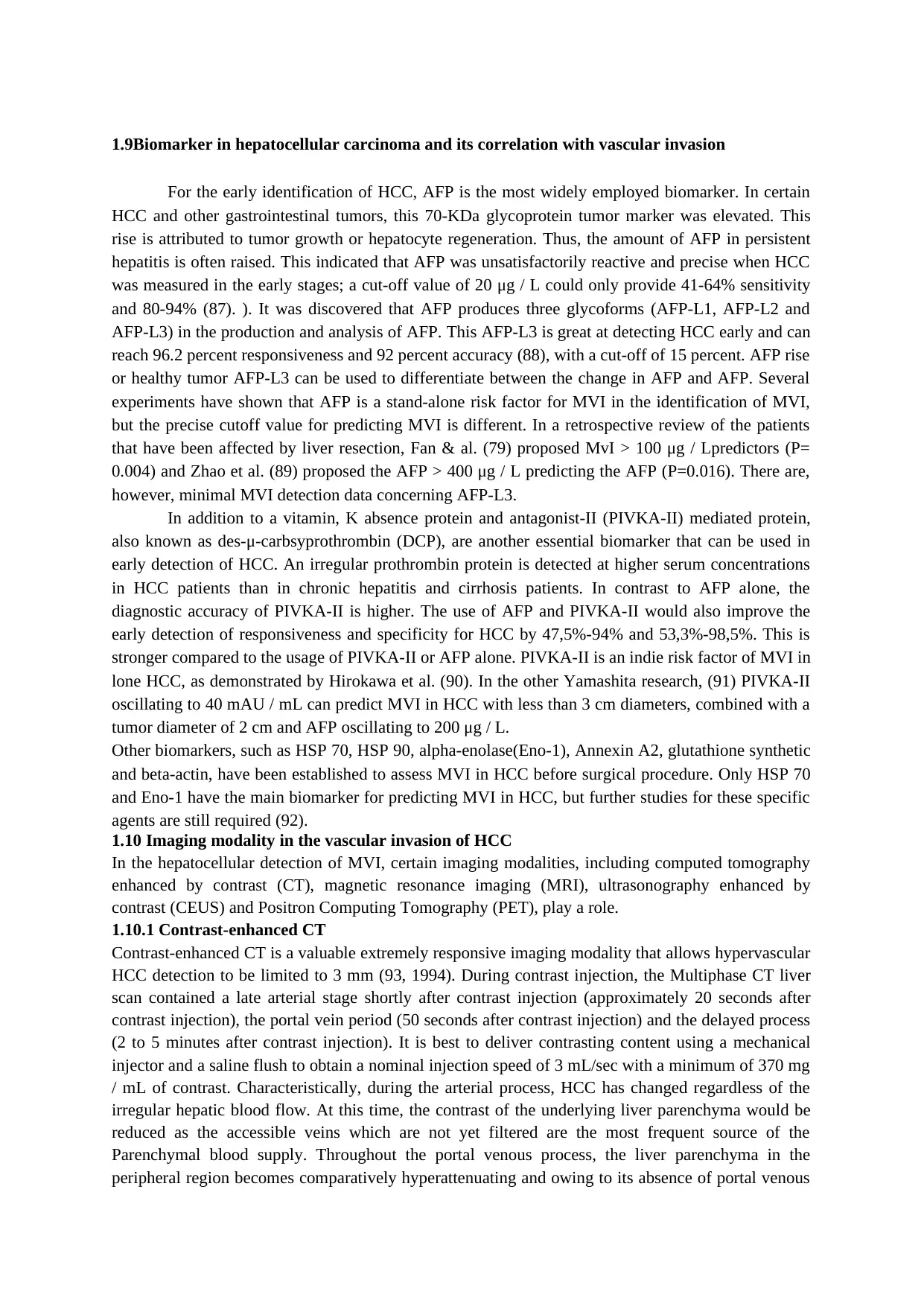
is multifocal and appears in the nontumor parenchymal (76). (Figure 2), which is a single-nodular
form or the margin of the nodular tumor.
Tumor margin distinct
Smooth tumor margin Non-smooth tumor margin
Simple nodular type Simple nodular with a focal
extranodular growth Multinodular type
Figure 2. Gross classification of HCC by Liver Cancer Study Group of Japan
1.10.2 MRI
The MRI's ability to diagnose HCC is nearly identical to CT, but MRI is more sensitive and precise
when differentiating Nodules in cirrhotic liver disease. This approach may also be used to distinguish
between well-differentiated HCC and weak differentiated HCC, aside from the usage of RMI in
detecting HCC. Hypointensity in T1-weighted imaging and hyperintensity in T2-weighted imagery
are usually mild and poorly distinguished HCC. A work performed by Enomoto et al. (97) has shown
that the T1 imagery hypointensity and the portal tumor stain wash represent weaker HCC variations,
and the two findings have a sensitivity of 88 percent. In contrast, the separation of well-differentiated
HCC with high and weak differentiated HCC is similar to 67 percent. In the report, most well-
characterized HCCs in T1-weighting imaging (83 percent) have shown non-hypointensity. Among
other research, it has been identified that weaker distinction between HCC and MRI is often more
popular for the prediction of MVI (98) when HCC is distinguished from MRI.
The recent improvement in imaging modes has allowed improved MRI (Gd-EOB-DTPA) to assess the
prevalence of MVI in HCC patients, with good quality diffusion-weighted picture (DWI) and gadoxetic
acid. Diffusion is a physical phenomenon through the spontaneous molecular displacement of water
in the tissue's voxel. With this diffusion-weighted imaging, studies have shown that MVI values are
correlated with standard fluid trends, non-smooth tumor margins, and obvious coefficient of
during a delayed step series might washout be seen occasionally. In the portal venous process, a portal
venous thrombus (PVTT) may also be separated in HCCs patients, and it is extremely likely for PVTT
to occur in HCC when a full or partial non-opacification of part of the entire portal vein and its
enhanced thrombus divisions is established (95). Like PVTT, MVI can not be specifically detected in
the CT scan, but some studies have found that tumor morphology is highly likely in the CT scan test.
One hundred two patients with preoperative multiphasic CT results from solo HCC were reported for
the future by Chou et al. (96). Numerous morphological parameters have been evaluated, but the
principal association between histopathologic MVI observations and tumor margins has been
evaluated in pre-operative images. Multi-variate research findings have found only non-inflammatory
margins in all parameters to be associated with MVI in HCC (p<0.001), and of the 60 pathological
experiments showing MVI in specific, 40 revealed focus, non-inflammatory margins in the same type
in 36 instances. This form of nodular time has frequently had a tumor capsule, a non-smooth tumor
margin with a focal extraocular development, and a non-smooth margin with a multinodular sort that
is multifocal and appears in the nontumor parenchymal (76). (Figure 2), which is a single-nodular
form or the margin of the nodular tumor.
Tumor margin distinct
Smooth tumor margin Non-smooth tumor margin
Simple nodular type Simple nodular with a focal
extranodular growth Multinodular type
Figure 2. Gross classification of HCC by Liver Cancer Study Group of Japan
1.10.2 MRI
The MRI's ability to diagnose HCC is nearly identical to CT, but MRI is more sensitive and precise
when differentiating Nodules in cirrhotic liver disease. This approach may also be used to distinguish
between well-differentiated HCC and weak differentiated HCC, aside from the usage of RMI in
detecting HCC. Hypointensity in T1-weighted imaging and hyperintensity in T2-weighted imagery
are usually mild and poorly distinguished HCC. A work performed by Enomoto et al. (97) has shown
that the T1 imagery hypointensity and the portal tumor stain wash represent weaker HCC variations,
and the two findings have a sensitivity of 88 percent. In contrast, the separation of well-differentiated
HCC with high and weak differentiated HCC is similar to 67 percent. In the report, most well-
characterized HCCs in T1-weighting imaging (83 percent) have shown non-hypointensity. Among
other research, it has been identified that weaker distinction between HCC and MRI is often more
popular for the prediction of MVI (98) when HCC is distinguished from MRI.
The recent improvement in imaging modes has allowed improved MRI (Gd-EOB-DTPA) to assess the
prevalence of MVI in HCC patients, with good quality diffusion-weighted picture (DWI) and gadoxetic
acid. Diffusion is a physical phenomenon through the spontaneous molecular displacement of water
in the tissue's voxel. With this diffusion-weighted imaging, studies have shown that MVI values are
correlated with standard fluid trends, non-smooth tumor margins, and obvious coefficient of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

diffusion (ADC). In DWI, these ADC values provide details on the stability of the cell membrane,
tissue cellularity and microcapillary infusion. Research by Xu et al. (100) at DWI in limited HCC found
that the effective MVI indicator, with sensibilities and specificities of 66,7 and 78,6 each, can be
lower ADC values (< 1,227 or 10-00 mm2/s) for b-value DWI of 0,500 s / mm2.
Gd-EOB-DTPA is a fairly recent, stable, and well-tolerated liver contrast agent for the acquisition of
dynamic and hepatobiliary process pictures, as a hepatospecific contrasts medium in MRI. The
appearance of a low and hypointense region around the tumor was characterized as a peritumoral-
decreased uptake (PDUA) and is observed at the hepato-biliary stage of enhanced Gd-EOB-DTPA
MRI. PDUA indicates that hepatocytic acid is compromised due to a reduction of portal flow which
may result in hemodynamic modifications due to disruption of the portal branches by tumor
thrombin. In the hepatobiliary process, there are three proposed PDUAs: wedge form, irregular belts
and circular PDUA. Since PDUA is correlated with portal flow failure, previous reports indicate that
HCC vascular invasion may include PDUA (101, 102). However, the clinical impact on the occurrence
of tumor recurrence after tumor resections remains uncertain if PDUA in the hepatobiliary process
of the Gd-EOB-DTPA enhanced MRI.
1.10.3 CEUS
Contrast-enhanced ultrasound (CEUS) was a unique imaging technique that been recognized for
almost 20 years; it allows non-invasive evaluation of liver perfusion through a vascular phase in real-
time. This technique was based on a combination of Doppler examinations and the injection of
microbubble-based contrast agents (103). With Doppler examination only we could assess large
vessels, with the help of microbubble-based contrast agent that can invade both large and small
vessels, it lead us enable to assess both the macrocirculation and microcirculation accurately, making
this modality has the value of sensitivity and specificity in the detection and examine characteristic of
focal liver lesions approaching those CT and MRI (104). The procedure is performed by injecting
intravenously microbubble based contrast agents (USCAs) that can pass through the pulmonary filler
and will remain in intravascular space work as blood vessels markers. After the injection, these
USCAs will be eliminated in 5 to 20 minutes, it will be exhaled via the lungs and some will be filtered
by the kidney and metabolized by the liver (105). This technique is generally safe and well-tolerated.
The contrast agent is not nephrotoxic so it can be used in patients with renal failure, not like enhanced
CT or MRI examination, in which the contrast agents are not appropriate for severely impaired renal
function patients (106).
HCC was defined by the multi-step cycle of hepatocarcinogenesis, which was primarily
supported by the dysfunctional hepatic artery structure in its genetic, neuronal, histological and
hemodynamic variations. In comparison to regenerative nodules with a healthy blood flow with usual
hep and the usually hypervascular dysplastic nodules, these two nodules appear isoechoic to
neighboring liver parenchymal all the time with CEUS (107). In contrast, HCC nodules in CEUS will
show it's typical hyper enhanced in arterial phase and washout in the portal venous and delayed
phases, just like in contrast-enhanced CT and MRI. Even with CEUS, it can provide non-invasively
examination that can show the real-time natures of contrast imaging, whereas enhanced CT and MRI
may fail to show enhance (108).
Besides the use of CEUS in the diagnosis of HCC, it also useful in the examination of
vascular invasion of HCC (109). Detection of the malignant portal or hepatic vein thrombosis is
important in the management decision of HCC. With the ability to show the blood vessels' condition
with injection USCAs, it also makes us be able to found thrombosis inside the vascular, not only for
malignant portal or hepatic vein thrombosis also for benign thrombosis condition. From Tanaka H et
al. (110), they found that CEUS with the use of sonazoid contrast was able to predict poorly
tissue cellularity and microcapillary infusion. Research by Xu et al. (100) at DWI in limited HCC found
that the effective MVI indicator, with sensibilities and specificities of 66,7 and 78,6 each, can be
lower ADC values (< 1,227 or 10-00 mm2/s) for b-value DWI of 0,500 s / mm2.
Gd-EOB-DTPA is a fairly recent, stable, and well-tolerated liver contrast agent for the acquisition of
dynamic and hepatobiliary process pictures, as a hepatospecific contrasts medium in MRI. The
appearance of a low and hypointense region around the tumor was characterized as a peritumoral-
decreased uptake (PDUA) and is observed at the hepato-biliary stage of enhanced Gd-EOB-DTPA
MRI. PDUA indicates that hepatocytic acid is compromised due to a reduction of portal flow which
may result in hemodynamic modifications due to disruption of the portal branches by tumor
thrombin. In the hepatobiliary process, there are three proposed PDUAs: wedge form, irregular belts
and circular PDUA. Since PDUA is correlated with portal flow failure, previous reports indicate that
HCC vascular invasion may include PDUA (101, 102). However, the clinical impact on the occurrence
of tumor recurrence after tumor resections remains uncertain if PDUA in the hepatobiliary process
of the Gd-EOB-DTPA enhanced MRI.
1.10.3 CEUS
Contrast-enhanced ultrasound (CEUS) was a unique imaging technique that been recognized for
almost 20 years; it allows non-invasive evaluation of liver perfusion through a vascular phase in real-
time. This technique was based on a combination of Doppler examinations and the injection of
microbubble-based contrast agents (103). With Doppler examination only we could assess large
vessels, with the help of microbubble-based contrast agent that can invade both large and small
vessels, it lead us enable to assess both the macrocirculation and microcirculation accurately, making
this modality has the value of sensitivity and specificity in the detection and examine characteristic of
focal liver lesions approaching those CT and MRI (104). The procedure is performed by injecting
intravenously microbubble based contrast agents (USCAs) that can pass through the pulmonary filler
and will remain in intravascular space work as blood vessels markers. After the injection, these
USCAs will be eliminated in 5 to 20 minutes, it will be exhaled via the lungs and some will be filtered
by the kidney and metabolized by the liver (105). This technique is generally safe and well-tolerated.
The contrast agent is not nephrotoxic so it can be used in patients with renal failure, not like enhanced
CT or MRI examination, in which the contrast agents are not appropriate for severely impaired renal
function patients (106).
HCC was defined by the multi-step cycle of hepatocarcinogenesis, which was primarily
supported by the dysfunctional hepatic artery structure in its genetic, neuronal, histological and
hemodynamic variations. In comparison to regenerative nodules with a healthy blood flow with usual
hep and the usually hypervascular dysplastic nodules, these two nodules appear isoechoic to
neighboring liver parenchymal all the time with CEUS (107). In contrast, HCC nodules in CEUS will
show it's typical hyper enhanced in arterial phase and washout in the portal venous and delayed
phases, just like in contrast-enhanced CT and MRI. Even with CEUS, it can provide non-invasively
examination that can show the real-time natures of contrast imaging, whereas enhanced CT and MRI
may fail to show enhance (108).
Besides the use of CEUS in the diagnosis of HCC, it also useful in the examination of
vascular invasion of HCC (109). Detection of the malignant portal or hepatic vein thrombosis is
important in the management decision of HCC. With the ability to show the blood vessels' condition
with injection USCAs, it also makes us be able to found thrombosis inside the vascular, not only for
malignant portal or hepatic vein thrombosis also for benign thrombosis condition. From Tanaka H et
al. (110), they found that CEUS with the use of sonazoid contrast was able to predict poorly
differentiation and MVI on HCC with sensitivity 100% and 40%, and specificity 91% and 92%
respectively. However, on the other study using CEUS for predicting MVI is not very useful, because
the location of MVI can be apart from the adjacent peritumoral tissues or more than 1 cm peritumoral
distance, made another modality to become the preferred choice in the prediction of MVI (111).
1.10.4 18F-FDG PET/CT
Positron emission tomography-computed tomography (PET/CT) is very important in oncology. These
two combinations of modality are highly sensitive in the diagnosis of malignancies. The most
commonly used marker in PET/CT is 18F-fludeoxyglucose (18F-FDG). This is an analog of glucose
used in the process of glucose metabolism inside the cell (112). It has been a few years that PET/CT
used as a diagnostic tool for various cancer and its tumor metastases. According to the current
European Association for the Study of the Liver Clinical Practice Guidelines, the use of 18F-FDG
PET/CT in the diagnosis of HCC is limited because of the variability 18F-FDG uptake in HCC, made
the sensitivity of this modality in detecting HCC is less than 40%, which is less than enhanced CT and
MRI examination, became the reasons why 18F-FDG PET/CT is not routinely used in HCC workup
(113). However, when the tumor is poorly differentiated HCC, the uptake of 18F-FDG is significantly
increased, even Wu et al. (114) showed a sensitivity of 18F-FDG PET/CT is 83.3% in poorly
differentiated HCC compare to 35% in well-differentiated and moderately differentiated HCC. With
the condition that poorly differentiated HCC is more to has a worse prognosis and possibility of tumor
metastasis, it made this modality is useful in detecting distant metastasis (115). Also in the study of
Kornberg et al. (116), they found that preoperative 18F-FDG uptake in PET/CT not only could predict
the poorly differentiated HCC but also could be the predictor of MVI, with high positive predictive
value and negative predictive value (87.5% and 88.5% respectively). It also supported by a study from
Ahn et al. (117) in the prediction of MVI in 51 patients with HCC before liver transplant, and they
reported tumor to normal liver standardized uptake value ratio (RSUVmax) more than 1.2 also
significantly associated with MVI (with P<0.001) with its high specificity of 86.6% and sensitivity of
64.3%. In the other multicenter retrospective cohort study in South Korea by Hyun SH et al. (118)
that studied about the ability of 18F-FDG PET/CT in predicting MVI before surgical treatment found
that TLR could be the predictor of MVI (with AUC=0.704), followed by tumor size (AUC=0.685)
and AFP (AUC=0.670).
1.11 Treatment of HCC and the effect of vascular invasion
1.11.1 Surgery
Partial resection, pathology, and liver transplantation are used in HCC surgery. The option for HCC
surgical intervention is to decide whether the tumor is restricted to the liver, size, and position of the
tumor, and to assess the underlying hepatic disorder from the existence of portal hypertension and
general symptoms of patients. Tumor resection is regarded as the first-line therapy, without vascular
invasion confirmation, in discrete tumors and without maintaining the role of liver according to the
BCLC staging scheme. Resection is useful for a variety of reasons, takes little time to pass, allows for
pathological tumor tests, and does not preclude potential liver transplantation (could be used for liver
transplantation bridging treatment) (119). Total resection should be achieved as a resection confined
to at least a distance of 1 cm of tumor-free, where the portal device is extracted along with the tumor
owing to its mechanical complications where larger liver parenchymal loss; This procedure is more
complicated. Latest work by Fan et al. (79) indicates that anatomical resection in solitary little HCC
(always 5 cm) with MVI is greater than non-anatomic resection, with a cumulative survival rate of
five years (85% vs. 55%, P=0.024) and five years disease-free survival rate (37% vs. 21%, P=0.025).
respectively. However, on the other study using CEUS for predicting MVI is not very useful, because
the location of MVI can be apart from the adjacent peritumoral tissues or more than 1 cm peritumoral
distance, made another modality to become the preferred choice in the prediction of MVI (111).
1.10.4 18F-FDG PET/CT
Positron emission tomography-computed tomography (PET/CT) is very important in oncology. These
two combinations of modality are highly sensitive in the diagnosis of malignancies. The most
commonly used marker in PET/CT is 18F-fludeoxyglucose (18F-FDG). This is an analog of glucose
used in the process of glucose metabolism inside the cell (112). It has been a few years that PET/CT
used as a diagnostic tool for various cancer and its tumor metastases. According to the current
European Association for the Study of the Liver Clinical Practice Guidelines, the use of 18F-FDG
PET/CT in the diagnosis of HCC is limited because of the variability 18F-FDG uptake in HCC, made
the sensitivity of this modality in detecting HCC is less than 40%, which is less than enhanced CT and
MRI examination, became the reasons why 18F-FDG PET/CT is not routinely used in HCC workup
(113). However, when the tumor is poorly differentiated HCC, the uptake of 18F-FDG is significantly
increased, even Wu et al. (114) showed a sensitivity of 18F-FDG PET/CT is 83.3% in poorly
differentiated HCC compare to 35% in well-differentiated and moderately differentiated HCC. With
the condition that poorly differentiated HCC is more to has a worse prognosis and possibility of tumor
metastasis, it made this modality is useful in detecting distant metastasis (115). Also in the study of
Kornberg et al. (116), they found that preoperative 18F-FDG uptake in PET/CT not only could predict
the poorly differentiated HCC but also could be the predictor of MVI, with high positive predictive
value and negative predictive value (87.5% and 88.5% respectively). It also supported by a study from
Ahn et al. (117) in the prediction of MVI in 51 patients with HCC before liver transplant, and they
reported tumor to normal liver standardized uptake value ratio (RSUVmax) more than 1.2 also
significantly associated with MVI (with P<0.001) with its high specificity of 86.6% and sensitivity of
64.3%. In the other multicenter retrospective cohort study in South Korea by Hyun SH et al. (118)
that studied about the ability of 18F-FDG PET/CT in predicting MVI before surgical treatment found
that TLR could be the predictor of MVI (with AUC=0.704), followed by tumor size (AUC=0.685)
and AFP (AUC=0.670).
1.11 Treatment of HCC and the effect of vascular invasion
1.11.1 Surgery
Partial resection, pathology, and liver transplantation are used in HCC surgery. The option for HCC
surgical intervention is to decide whether the tumor is restricted to the liver, size, and position of the
tumor, and to assess the underlying hepatic disorder from the existence of portal hypertension and
general symptoms of patients. Tumor resection is regarded as the first-line therapy, without vascular
invasion confirmation, in discrete tumors and without maintaining the role of liver according to the
BCLC staging scheme. Resection is useful for a variety of reasons, takes little time to pass, allows for
pathological tumor tests, and does not preclude potential liver transplantation (could be used for liver
transplantation bridging treatment) (119). Total resection should be achieved as a resection confined
to at least a distance of 1 cm of tumor-free, where the portal device is extracted along with the tumor
owing to its mechanical complications where larger liver parenchymal loss; This procedure is more
complicated. Latest work by Fan et al. (79) indicates that anatomical resection in solitary little HCC
(always 5 cm) with MVI is greater than non-anatomic resection, with a cumulative survival rate of
five years (85% vs. 55%, P=0.024) and five years disease-free survival rate (37% vs. 21%, P=0.025).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
