Health Workforce Analysis: Mongolia and Australia - Environmental Scan
VerifiedAdded on 2021/06/15
|17
|3670
|21
Report
AI Summary
This report provides a detailed analysis of the health workforce in Mongolia and Australia, examining various factors that influence healthcare delivery, including population, labor force, and health facilities. It begins with an environmental scan of both countries, utilizing data from WHO fact sheets and academic articles to highlight the current state of their healthcare systems. The report then delves into the profile data of the health workforce, categorizing professionals and analyzing their density per population. Key critical issues are addressed, focusing on challenges such as workforce distribution, funding, and the impact of aging populations and chronic illnesses. Furthermore, the report proposes strategies based on the WHO 2016 report "Working for health and growth: investing in the health workforce", offering recommendations to implement an effective workforce plan, addressing issues like the distribution of human resources, management in health systems, and the overall governance. Tables are included to present data on healthcare workers' density in both countries, providing a comprehensive overview of the health workforce landscape.

Running head: HEALTH WORKFORCE 1
Health workforce
(Author’s name)
(Institutional Affiliation)
Health workforce
(Author’s name)
(Institutional Affiliation)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Health Workforce 2
Executive summary
The health workforce of a country simply means the ability of a country to attain
health goals and the set objectives on knowledge, motivation, skills, and deployment of
employees for organization and healthcare provider services. There are various factors
that determine a type of a health workforce in a country which includes a population of
the country, labor force available, health facilities, registered professionals, and civil
services payroll registered. This report gives an environmental scan of the intrinsic and
extrinsic factors surrounding the health care system of Mongolia and Australia, the
current state of affairs in the health sector while still giving a clear description using data
from WHO fact sheets and other academic articles from both countries, the critical issues
that need to be addressed in the country paying keen attention to their human resources
for health development plan for the year 2011 to 2025. It also clearly depicts strategies
that should be undertaken by the country health sector based on the ten recommendations
developed in the WHO 2016 report “Working for health and growth: investing in the
health workforce” as a framework which can be undertaken to implement an effective
workforce plan.
Executive summary
The health workforce of a country simply means the ability of a country to attain
health goals and the set objectives on knowledge, motivation, skills, and deployment of
employees for organization and healthcare provider services. There are various factors
that determine a type of a health workforce in a country which includes a population of
the country, labor force available, health facilities, registered professionals, and civil
services payroll registered. This report gives an environmental scan of the intrinsic and
extrinsic factors surrounding the health care system of Mongolia and Australia, the
current state of affairs in the health sector while still giving a clear description using data
from WHO fact sheets and other academic articles from both countries, the critical issues
that need to be addressed in the country paying keen attention to their human resources
for health development plan for the year 2011 to 2025. It also clearly depicts strategies
that should be undertaken by the country health sector based on the ten recommendations
developed in the WHO 2016 report “Working for health and growth: investing in the
health workforce” as a framework which can be undertaken to implement an effective
workforce plan.
Health Workforce 3
Contents
Executive summary.........................................................................................................................2
1.0 Introduction................................................................................................................................4
2.0 Environmental Scan...................................................................................................................4
3.0 Profile Data for health work force.............................................................................................6
4.0 Critical issues to be addressed.................................................................................................10
5.0 Strategies relevant to implement workforce plan....................................................................13
6.0 Conclusion...............................................................................................................................14
7.0 References................................................................................................................................16
Table of tables
Table 1.1: Density of health care workers in Australia per 1000 population
Table 1.2: Country health description as per World Health Organization
Table 1.3 Skilled health personnel per 10000 population and all nurses and Midwives in
Mongolia
Table 1.3 Skilled health personnel per 10000 population and all nurses and Midwives in
Australia
Contents
Executive summary.........................................................................................................................2
1.0 Introduction................................................................................................................................4
2.0 Environmental Scan...................................................................................................................4
3.0 Profile Data for health work force.............................................................................................6
4.0 Critical issues to be addressed.................................................................................................10
5.0 Strategies relevant to implement workforce plan....................................................................13
6.0 Conclusion...............................................................................................................................14
7.0 References................................................................................................................................16
Table of tables
Table 1.1: Density of health care workers in Australia per 1000 population
Table 1.2: Country health description as per World Health Organization
Table 1.3 Skilled health personnel per 10000 population and all nurses and Midwives in
Mongolia
Table 1.3 Skilled health personnel per 10000 population and all nurses and Midwives in
Australia
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Health Workforce 4
1.0 Introduction
According to World Health Organization (WHO), health workforce of a country includes
the ability of the country to meet health goals and objectives majorly on knowledge, motivation,
skills, and deployment of individuals for organization and deliverance of health
services("HEALTH WORKFORCE", 2018). There are various factors that determine a type of a
health workforce in a country which includes a population of the country, labor force available,
health facilities, registered professionals, and civil services payroll registered (Deloitte Access
Economics, 2016). This study seeks to analyze and address the health workforce of Mongolia
and Australia ("Australian Health", 2016).
In this study Mongolia is selected as it is among middle level income as state by WHO
situated in the same region as Australia , that is, Western Pacific Region, thus it may health
workforce issues related with Australia’s. Mongolia is a sparsely populated landlocked country
situated in Central Asia with a population density of 1.8 per kilometer. The population is
estimated to be 2 81188 though the figure has been increasing by 1.8 % annually ("Human
Resources for Health-Mongolia", 2014). Despite an increase in population, the human resources
for health have not shown a significant increase. There is low government funding for health and
the health workforce is poorly distributed ("Australian Health", 2016). On the other hand, the
population in Australia has been rapidly growing day by day. According to the health
department, the aging population has created a burden due to an increase in health disabilities.
People aged over 65 years are expected to increase by about 4 million by 2051 ("Australian
Health", 2016). Therefore various areas of the health workforce of the countries are included in
the study which includes an environmental scan of the country, profile of health workforce
1.0 Introduction
According to World Health Organization (WHO), health workforce of a country includes
the ability of the country to meet health goals and objectives majorly on knowledge, motivation,
skills, and deployment of individuals for organization and deliverance of health
services("HEALTH WORKFORCE", 2018). There are various factors that determine a type of a
health workforce in a country which includes a population of the country, labor force available,
health facilities, registered professionals, and civil services payroll registered (Deloitte Access
Economics, 2016). This study seeks to analyze and address the health workforce of Mongolia
and Australia ("Australian Health", 2016).
In this study Mongolia is selected as it is among middle level income as state by WHO
situated in the same region as Australia , that is, Western Pacific Region, thus it may health
workforce issues related with Australia’s. Mongolia is a sparsely populated landlocked country
situated in Central Asia with a population density of 1.8 per kilometer. The population is
estimated to be 2 81188 though the figure has been increasing by 1.8 % annually ("Human
Resources for Health-Mongolia", 2014). Despite an increase in population, the human resources
for health have not shown a significant increase. There is low government funding for health and
the health workforce is poorly distributed ("Australian Health", 2016). On the other hand, the
population in Australia has been rapidly growing day by day. According to the health
department, the aging population has created a burden due to an increase in health disabilities.
People aged over 65 years are expected to increase by about 4 million by 2051 ("Australian
Health", 2016). Therefore various areas of the health workforce of the countries are included in
the study which includes an environmental scan of the country, profile of health workforce
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Workforce 5
available, critical issues that need to be addressed and strategies relevant to implement the
workforce plan.
2.0 Environmental Scan
` According to WHO-Mongolia Country Cooperation Strategy 2010-2015, the health care
systems are divided into three major levels which include national levels, province levels, and
the soum level. The Mongolian health system is based on a former Soviet model which put
greater emphasis on the hospitals for curative care rather than on preventive and promotes care.
According to WHO statistics, there are about 68 hospital beds per 10000 individuals in Mongolia
("Human Resources for Health-Mongolia", 2014). A number of specialized hospitals and
institutions like National Center for Communicable Diseases have been developed to cater for a
large burden of communicable diseases. However, the challenges have remained in regulations
of the quality and the cost of services. The major funding for health services in the country is
from government incurring a total expenditure or around 76% of the total state budget where
about 21% is covered by health insurance and the rest 3% for individual self-care service
("Health Service Delivery Profile Mongolia", 2012).
In 2008, the statistical data and facts showed that there were about 35254 workers in the
health sector of Mongolia. The number had increased up to 41124 in 2011. Although it may be
considered as an increase in the health workforce, the current staffing levels are considered
insufficient with a great shortage of doctors and nurses ("Human Resources for Health-
Mongolia", 2014). Women play a major role in the health workforce of Mongolia. About 82% of
all workers in the health workforce of Mongolia are women. There are about 79% women
medical doctors, 98% women nurses and 80% medical imaging operators. Regarding the
available, critical issues that need to be addressed and strategies relevant to implement the
workforce plan.
2.0 Environmental Scan
` According to WHO-Mongolia Country Cooperation Strategy 2010-2015, the health care
systems are divided into three major levels which include national levels, province levels, and
the soum level. The Mongolian health system is based on a former Soviet model which put
greater emphasis on the hospitals for curative care rather than on preventive and promotes care.
According to WHO statistics, there are about 68 hospital beds per 10000 individuals in Mongolia
("Human Resources for Health-Mongolia", 2014). A number of specialized hospitals and
institutions like National Center for Communicable Diseases have been developed to cater for a
large burden of communicable diseases. However, the challenges have remained in regulations
of the quality and the cost of services. The major funding for health services in the country is
from government incurring a total expenditure or around 76% of the total state budget where
about 21% is covered by health insurance and the rest 3% for individual self-care service
("Health Service Delivery Profile Mongolia", 2012).
In 2008, the statistical data and facts showed that there were about 35254 workers in the
health sector of Mongolia. The number had increased up to 41124 in 2011. Although it may be
considered as an increase in the health workforce, the current staffing levels are considered
insufficient with a great shortage of doctors and nurses ("Human Resources for Health-
Mongolia", 2014). Women play a major role in the health workforce of Mongolia. About 82% of
all workers in the health workforce of Mongolia are women. There are about 79% women
medical doctors, 98% women nurses and 80% medical imaging operators. Regarding the
Health Workforce 6
distribution of workers, there are about 6 doctors per 10000 population and there is great
shortage especially in soum and sub soum hospitals.
According to Productivity Commission of Australia in 2015, there has been an increase in
demand for health and community services. At the same time growth and establishments of
funding has decreased ("Workforce Overview - Australian Institute of Health and Welfare",
2018). Therefore the government of Australia has been actively transitioning in such a way that
individuals have been given responsibility to take care of their health in terms of financial
contributions. These changes have brought impacts to service health providers and also the mode
of delivery ("Australian Health", 2016). Due to this reason, the government and health
organizations have developed vocational education and training (VET) systems in order to
support national workforce and skills development. New national structures and processes are
being considered at the same time there have been experienced changes to territories and state
funding ("Rural Health Workforce Australia", 2018). Therefore the VET sector has been
embracing these changes in order to develop community health services and strong health
workforce that will cater for future demand. The government and all other stakeholders are
working forward to ensure VET policy and funding are implemented in order to support effective
workforce planning ("Australian Health Workforce", 2015).
Unlike in Mongolia, Australia major health challenges have been attributed to the
increase in aging population and chronic illness ("Rural Health Workforce Australia", 2018).
The number of individuals aged over 65 with chronic illness is expected to increase up to 4.1
million by the year 2051. Over one million of these people are considered to need high care in
residential facilities and about 370, 000 are estimated to need low-level health care ("Australian
distribution of workers, there are about 6 doctors per 10000 population and there is great
shortage especially in soum and sub soum hospitals.
According to Productivity Commission of Australia in 2015, there has been an increase in
demand for health and community services. At the same time growth and establishments of
funding has decreased ("Workforce Overview - Australian Institute of Health and Welfare",
2018). Therefore the government of Australia has been actively transitioning in such a way that
individuals have been given responsibility to take care of their health in terms of financial
contributions. These changes have brought impacts to service health providers and also the mode
of delivery ("Australian Health", 2016). Due to this reason, the government and health
organizations have developed vocational education and training (VET) systems in order to
support national workforce and skills development. New national structures and processes are
being considered at the same time there have been experienced changes to territories and state
funding ("Rural Health Workforce Australia", 2018). Therefore the VET sector has been
embracing these changes in order to develop community health services and strong health
workforce that will cater for future demand. The government and all other stakeholders are
working forward to ensure VET policy and funding are implemented in order to support effective
workforce planning ("Australian Health Workforce", 2015).
Unlike in Mongolia, Australia major health challenges have been attributed to the
increase in aging population and chronic illness ("Rural Health Workforce Australia", 2018).
The number of individuals aged over 65 with chronic illness is expected to increase up to 4.1
million by the year 2051. Over one million of these people are considered to need high care in
residential facilities and about 370, 000 are estimated to need low-level health care ("Australian
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Health Workforce 7
Health", 2016). Other than that, the aging health workforce and associated projected retirements
have become most of the critical factor facing the government and community. Early childhood
education and care sector have also increased demand due to increase in population. According
to Australian Government Department of Education Employment and Workforce Relation in
2012, there has been an increase of about 20% of child care services in Australia of which the
number is expected to increase by 2.2 million by 2031 ("Rural Health Workforce Australia",
2018).
3.0 Profile Data for health workforce
According to WHO, the aggregated data of the health workforce is classified according to
9 major groups: Physicians include all general medical practitioners and medical practitioner
specialists, Midwifery and nursing personnel which include all nursing personnel, midwifery
personnel, and both nursing and midwifery associates (WHO ,2015). Traditional birth attendants
are included as community health workers. Public and environmental workers include
environmental and public health officers, hygienists, environmental and public health
technicians, district health officers, sanitarians, food sanitation, public health inspectors and
safety inspectors. Community and health workers include community health officers, family
health workers, traditional birth attendants, community health education workers and
complementary medical practitioners("High-Level commission on Health Employment and
Economic Growth", 2018). Other health workers include all other groups of health providers
such as dieticians, medical assistants, occupation therapist, nutritionists, medical imaging,
optometrist, therapeutic equipment’s technicians, opticians, personal care workers, medical
trainees, physiotherapist and speech pathologist ("Australian Health", 2016). Health management
and support workers include all other categories of health systems workers such as
Health", 2016). Other than that, the aging health workforce and associated projected retirements
have become most of the critical factor facing the government and community. Early childhood
education and care sector have also increased demand due to increase in population. According
to Australian Government Department of Education Employment and Workforce Relation in
2012, there has been an increase of about 20% of child care services in Australia of which the
number is expected to increase by 2.2 million by 2031 ("Rural Health Workforce Australia",
2018).
3.0 Profile Data for health workforce
According to WHO, the aggregated data of the health workforce is classified according to
9 major groups: Physicians include all general medical practitioners and medical practitioner
specialists, Midwifery and nursing personnel which include all nursing personnel, midwifery
personnel, and both nursing and midwifery associates (WHO ,2015). Traditional birth attendants
are included as community health workers. Public and environmental workers include
environmental and public health officers, hygienists, environmental and public health
technicians, district health officers, sanitarians, food sanitation, public health inspectors and
safety inspectors. Community and health workers include community health officers, family
health workers, traditional birth attendants, community health education workers and
complementary medical practitioners("High-Level commission on Health Employment and
Economic Growth", 2018). Other health workers include all other groups of health providers
such as dieticians, medical assistants, occupation therapist, nutritionists, medical imaging,
optometrist, therapeutic equipment’s technicians, opticians, personal care workers, medical
trainees, physiotherapist and speech pathologist ("Australian Health", 2016). Health management
and support workers include all other categories of health systems workers such as
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Workforce 8
administrative managers, health economists, health policy layers, health statisticians, medical
health records specialists, ambulance drivers, health information technicians, maintenance staff
and general management staff("WHO", 2018).
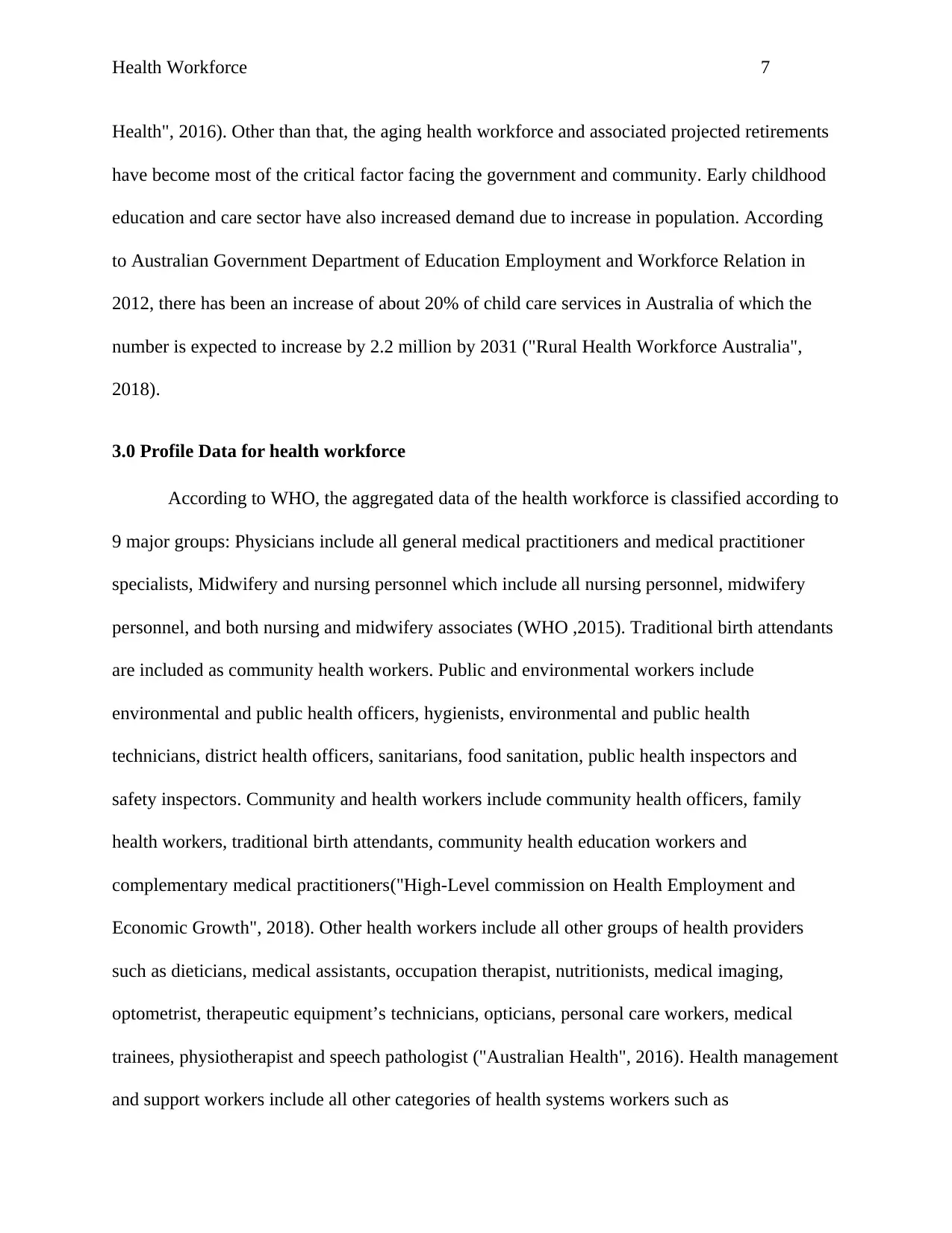
The following table represents the density of health care workers in Australia and
Mongolia per 1000 population from the years 1996, 2001, 2006, 2009, 2010, 2012 and 2015 by
WHO("WHO", 2018).
Table 1.1: Density of health care workers in Australia per 1000 population
Year
Physici
ans
density
Nursing
and
midwifer
y
personnel
density
dentistr
y
personn
el
density
Pharmaceu
tical
personnel
density
Laborator
y health
workers
density
Environm
ental and
health
workers
density
Community
and
traditional
health
workers
density
Other
health
workers
density
Health
management
and support
density
2015 3.496 12.379 0.578 0.847 0.861
2012 3.246 10.14 0.557 0.76 N/A 0.178 N/A 0.78
2010 0.866 N/A 0.088 N/A 0.919
2009 2.885 9.246 0.666 1.11 NA N/A 4.446
2006 2.672 10.78 1.438 0.744 0.508 0.049 10.326 0.095
2001 2.479 9.728 1.103 0.723 0.431 0.197 1.986 25.29
1996 2.53 010.33 1.273 0.672 0.356 0.039 6.668
Nurses and physician play a major role in the healthcare of Mongolia. However,
despite the low levels of all health workforces in the country, their ratio per 10,000 populations is
administrative managers, health economists, health policy layers, health statisticians, medical
health records specialists, ambulance drivers, health information technicians, maintenance staff
and general management staff("WHO", 2018).
The following table represents the density of health care workers in Australia and
Mongolia per 1000 population from the years 1996, 2001, 2006, 2009, 2010, 2012 and 2015 by
WHO("WHO", 2018).
Table 1.1: Density of health care workers in Australia per 1000 population
Year
Physici
ans
density
Nursing
and
midwifer
y
personnel
density
dentistr
y
personn
el
density
Pharmaceu
tical
personnel
density
Laborator
y health
workers
density
Environm
ental and
health
workers
density
Community
and
traditional
health
workers
density
Other
health
workers
density
Health
management
and support
density
2015 3.496 12.379 0.578 0.847 0.861
2012 3.246 10.14 0.557 0.76 N/A 0.178 N/A 0.78
2010 0.866 N/A 0.088 N/A 0.919
2009 2.885 9.246 0.666 1.11 NA N/A 4.446
2006 2.672 10.78 1.438 0.744 0.508 0.049 10.326 0.095
2001 2.479 9.728 1.103 0.723 0.431 0.197 1.986 25.29
1996 2.53 010.33 1.273 0.672 0.356 0.039 6.668
Nurses and physician play a major role in the healthcare of Mongolia. However,
despite the low levels of all health workforces in the country, their ratio per 10,000 populations is
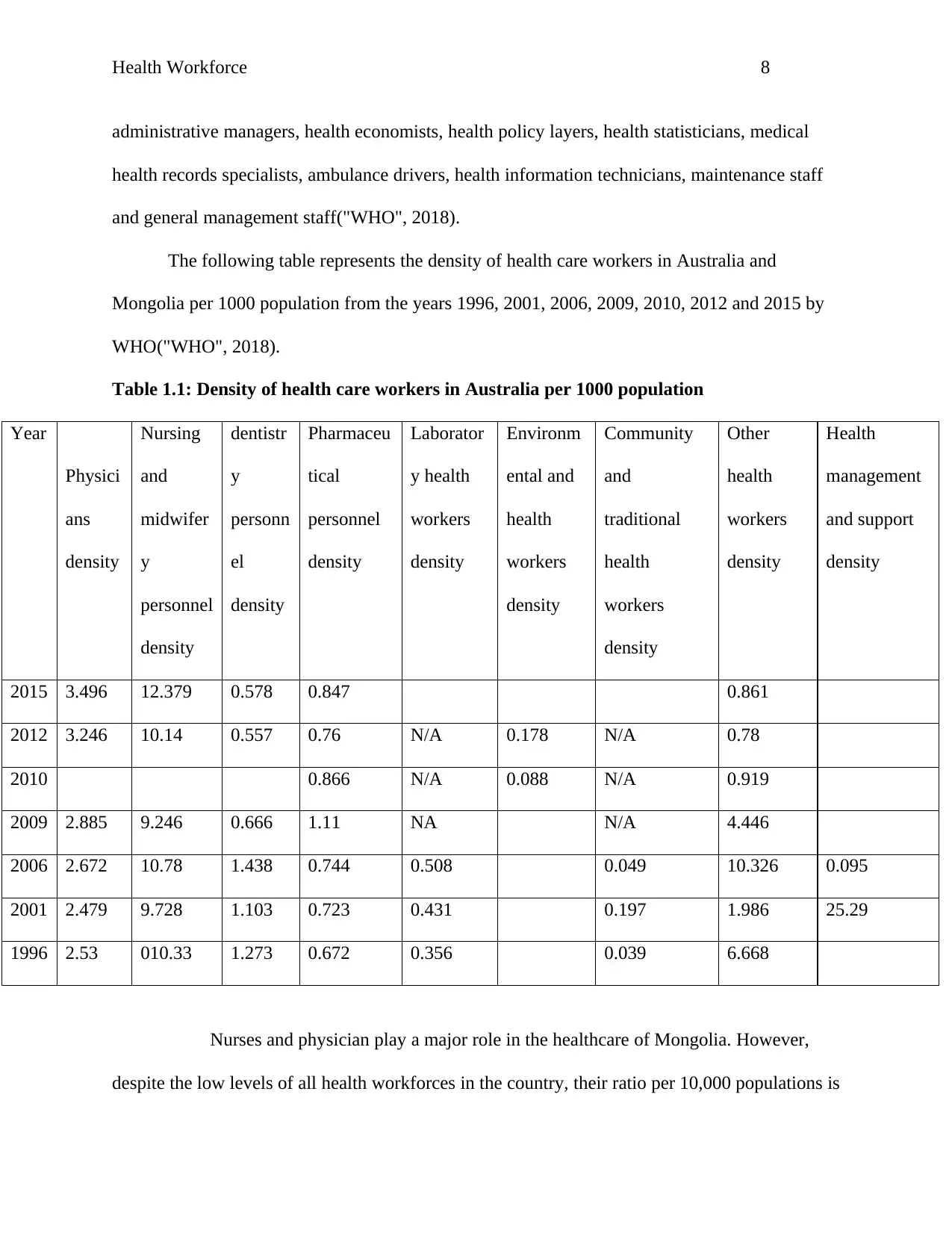
Health Workforce 9
highly poor("WHO", 2018). This could have been the reason for high mortality rates for infants
and mothers.
Table 1.2: Density of health care workers in Mongolia per 1000 population
Year
Physici
ans
density
Nursing
and
midwifer
y
personnel
density
dentistr
y
personn
el
density
Pharmaceu
tical
personnel
density
Laborator
y health
workers
density
Environm
ental and
health
workers
density
Community
and
traditional
health
workers
density
Other
health
workers
density
Health
management
and support
density
2015 0.508 0.294
2012 1.333 0.28
2010 0.196 0.434
2009 0.198 0.408 0.123 0.045
2008 0.195 0.444 1 0.035 0.023 0.448
2002 0.138 0.447 2.95
There has been an improvement from both countries where the number of workers in
both Mongolia and Austria has been increasing from year to year. The ratio of doctors to nurses
in Australia is generally high as compared to Mongolia ("Australian Health", 2016). The number
of all health workers per 10000 populations in Australia is high as compared to in Mongolia.
However, both countries experience a deficit in such a way neither of them can be termed as
having a good health workforce ("Rural Health Workforce Australia", 2018). The tables below
represent a total number of skilled health personnel in Mongolia and Australia per 10000
highly poor("WHO", 2018). This could have been the reason for high mortality rates for infants
and mothers.
Table 1.2: Density of health care workers in Mongolia per 1000 population
Year
Physici
ans
density
Nursing
and
midwifer
y
personnel
density
dentistr
y
personn
el
density
Pharmaceu
tical
personnel
density
Laborator
y health
workers
density
Environm
ental and
health
workers
density
Community
and
traditional
health
workers
density
Other
health
workers
density
Health
management
and support
density
2015 0.508 0.294
2012 1.333 0.28
2010 0.196 0.434
2009 0.198 0.408 0.123 0.045
2008 0.195 0.444 1 0.035 0.023 0.448
2002 0.138 0.447 2.95
There has been an improvement from both countries where the number of workers in
both Mongolia and Austria has been increasing from year to year. The ratio of doctors to nurses
in Australia is generally high as compared to Mongolia ("Australian Health", 2016). The number
of all health workers per 10000 populations in Australia is high as compared to in Mongolia.
However, both countries experience a deficit in such a way neither of them can be termed as
having a good health workforce ("Rural Health Workforce Australia", 2018). The tables below
represent a total number of skilled health personnel in Mongolia and Australia per 10000
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Health Workforce 10
population and the total number of all nurses and midwives in both countries in the years 2013,
2014 and 2015.
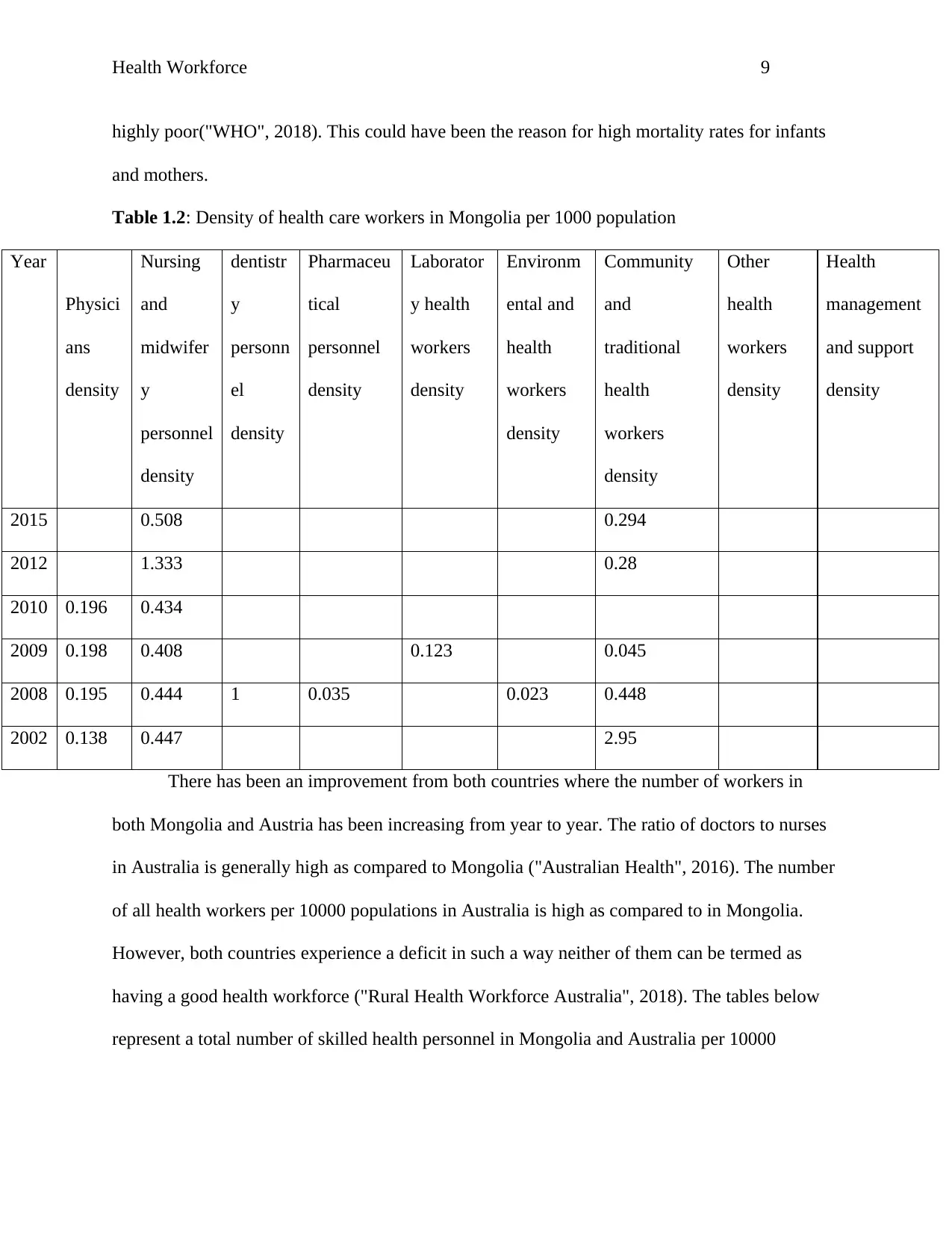
Table 1.3 Skilled health personnel per 10000 population and all nurses and
Midwives in Mongolia
Years Skilled health personnel per
10000 population
All nurses and midwives
2014 72.62 11836
2013 65.6 10964
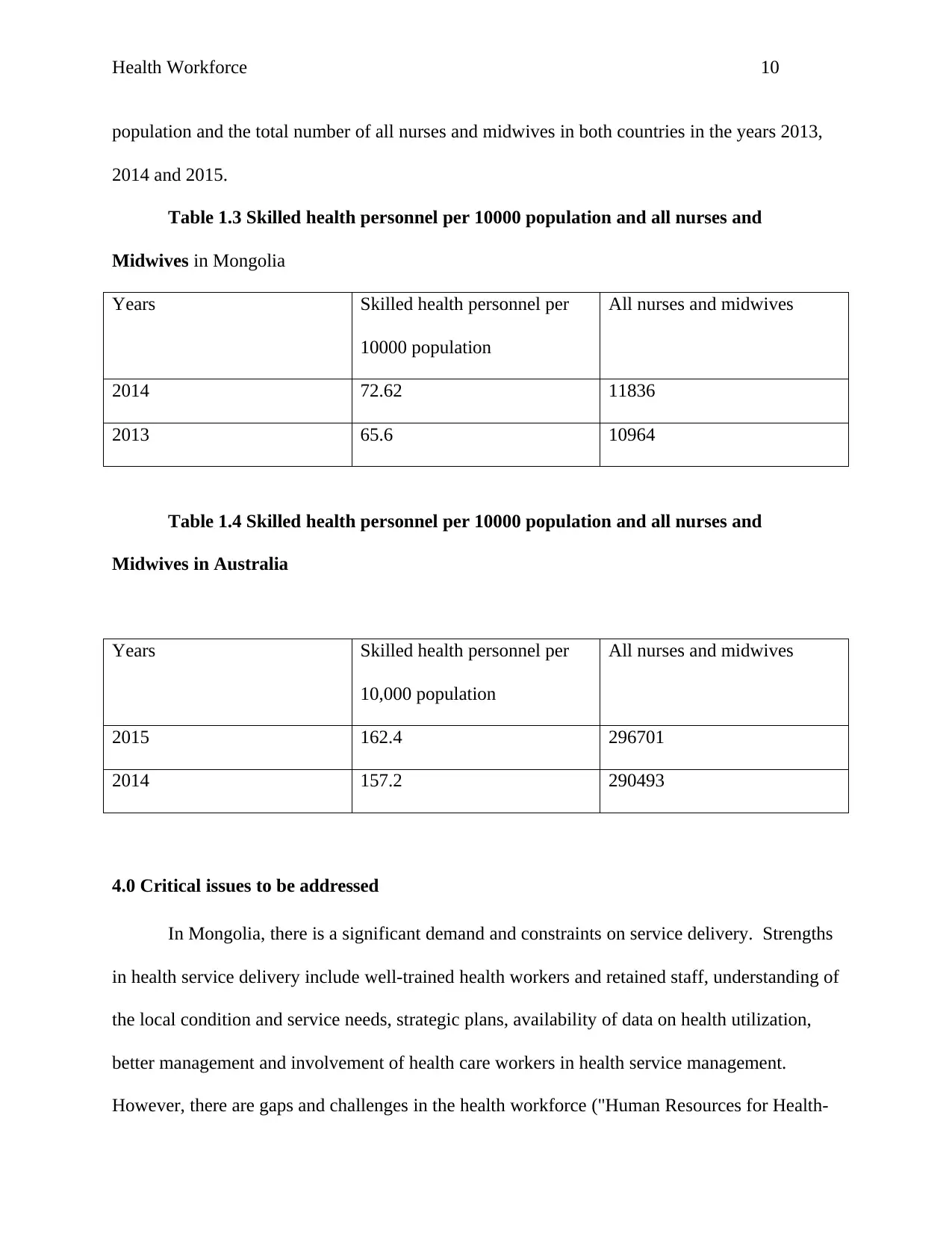
Table 1.4 Skilled health personnel per 10000 population and all nurses and
Midwives in Australia
Years Skilled health personnel per
10,000 population
All nurses and midwives
2015 162.4 296701
2014 157.2 290493
4.0 Critical issues to be addressed
In Mongolia, there is a significant demand and constraints on service delivery. Strengths
in health service delivery include well-trained health workers and retained staff, understanding of
the local condition and service needs, strategic plans, availability of data on health utilization,
better management and involvement of health care workers in health service management.
However, there are gaps and challenges in the health workforce ("Human Resources for Health-
population and the total number of all nurses and midwives in both countries in the years 2013,
2014 and 2015.
Table 1.3 Skilled health personnel per 10000 population and all nurses and
Midwives in Mongolia
Years Skilled health personnel per
10000 population
All nurses and midwives
2014 72.62 11836
2013 65.6 10964
Table 1.4 Skilled health personnel per 10000 population and all nurses and
Midwives in Australia
Years Skilled health personnel per
10,000 population
All nurses and midwives
2015 162.4 296701
2014 157.2 290493
4.0 Critical issues to be addressed
In Mongolia, there is a significant demand and constraints on service delivery. Strengths
in health service delivery include well-trained health workers and retained staff, understanding of
the local condition and service needs, strategic plans, availability of data on health utilization,
better management and involvement of health care workers in health service management.
However, there are gaps and challenges in the health workforce ("Human Resources for Health-
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Workforce 11
Mongolia", 2014). The health workforce capacity is poorly distributed of which the
responsibilities and roles including family group practices are not well defined. In addition, the
health service efficiency is poor due to various reasons which include poor referral systems and
gate-keeping, inappropriate use of both outpatient and inpatient care, poor distribution of
hospitals and beds, poor mismatching of health needs and supplies, insufficient coordination
between levels of care and responsibilities and outdated guidelines and protocols ("Health
Service Delivery Profile Mongolia", 2012).
Mongolia has a burden of both communicable and non-communicable diseases. In 2011,
around 43000 cases of different communicable illnesses were registered. The incidences of
mumps, viral hepatitis, scarlet fever, tick-borne diseases and syphilis increased by 0.1 to 20
percent of the cases per 10000 populations as compared to the previous years ("Health Service
Delivery Profile Mongolia", 2012). Currently, Mongolia is experiencing both demographic and
epidemiological transition where there is a decline in mortality and morbidity of communicable
diseases and an increase in chronic noncommunicable conditions. This is well demonstrated
throughout the country where circulatory diseases and cancer contributed over 75% of the total
mortality ("Human Resources for Health-Mongolia", 2014).
The national health workforce strategic framework(NHWSF) in Australia is a policy and
planning guideline for health workforce intended to take place in the next ten years ("Australian
Health Workforce", 2015). The framework was developed in order to cater for the current
emerging human resources for health (HRM) challenges (Aged and Community Services
Australia,2016). It covers all related frameworks covering Aboriginal and Torres Strait Islander
health workforce and also the overall health workforce in both regional and remote areas
("Australian Health", 2016). Several principles are covered in the framework which includes
Mongolia", 2014). The health workforce capacity is poorly distributed of which the
responsibilities and roles including family group practices are not well defined. In addition, the
health service efficiency is poor due to various reasons which include poor referral systems and
gate-keeping, inappropriate use of both outpatient and inpatient care, poor distribution of
hospitals and beds, poor mismatching of health needs and supplies, insufficient coordination
between levels of care and responsibilities and outdated guidelines and protocols ("Health
Service Delivery Profile Mongolia", 2012).
Mongolia has a burden of both communicable and non-communicable diseases. In 2011,
around 43000 cases of different communicable illnesses were registered. The incidences of
mumps, viral hepatitis, scarlet fever, tick-borne diseases and syphilis increased by 0.1 to 20
percent of the cases per 10000 populations as compared to the previous years ("Health Service
Delivery Profile Mongolia", 2012). Currently, Mongolia is experiencing both demographic and
epidemiological transition where there is a decline in mortality and morbidity of communicable
diseases and an increase in chronic noncommunicable conditions. This is well demonstrated
throughout the country where circulatory diseases and cancer contributed over 75% of the total
mortality ("Human Resources for Health-Mongolia", 2014).
The national health workforce strategic framework(NHWSF) in Australia is a policy and
planning guideline for health workforce intended to take place in the next ten years ("Australian
Health Workforce", 2015). The framework was developed in order to cater for the current
emerging human resources for health (HRM) challenges (Aged and Community Services
Australia,2016). It covers all related frameworks covering Aboriginal and Torres Strait Islander
health workforce and also the overall health workforce in both regional and remote areas
("Australian Health", 2016). Several principles are covered in the framework which includes
Health Workforce 12
distribution of all health workforces in an equitable manner to all Australians that recognize the
specific requirements and needs of the people (Community Services and Health Industry Skills
Council,2015).
5.0 Strategies relevant to implement a workforce plan
The health workforce in Mongolia faces by various challenges including the inequality
distribution of human resources for health(HRM), poor management in health systems, lack of
enough structural resources, inadequate health workforce, poor health workers pay, poor quality
control, lack of enough trained health personnel and overall systems of governance in both
public and private sectors(AHPRA,2018) . To manage these challenges, certain strategies by
WHO 2016 report “Working for health and growth: investing in the health workforce” are
recommended ("Australian Health", 2016). These include jobs creation, education of health
workers, gender and women rights, proper use of technology in health systems, proper approach
in crises and humanitarians settings, reforms in health services and delivery, increase in health
financing, encouragement and involvement in partnership and cooperation, international
cooperation and proper data, information and accountability (Shamian, 2016).
The Ministry of Health of Mongolia and the governance at the local level should
embrace job creation through stimulation of decent health sectors jobs majorly in youths and
women with the right skills and standard numbers in both rural and urban areas ("Department of
Health | Health workforce", 2018). This can be done by creating labor market policies in health
sectors which can boost sustainable health workforce thus preventing workers to have second
jobs in private sectors but creating a gap for new jobs ("Human Resources for Health-Mongolia",
2014). Due to the fact that health sector is growing in Mongolia employing women and
distribution of all health workforces in an equitable manner to all Australians that recognize the
specific requirements and needs of the people (Community Services and Health Industry Skills
Council,2015).
5.0 Strategies relevant to implement a workforce plan
The health workforce in Mongolia faces by various challenges including the inequality
distribution of human resources for health(HRM), poor management in health systems, lack of
enough structural resources, inadequate health workforce, poor health workers pay, poor quality
control, lack of enough trained health personnel and overall systems of governance in both
public and private sectors(AHPRA,2018) . To manage these challenges, certain strategies by
WHO 2016 report “Working for health and growth: investing in the health workforce” are
recommended ("Australian Health", 2016). These include jobs creation, education of health
workers, gender and women rights, proper use of technology in health systems, proper approach
in crises and humanitarians settings, reforms in health services and delivery, increase in health
financing, encouragement and involvement in partnership and cooperation, international
cooperation and proper data, information and accountability (Shamian, 2016).
The Ministry of Health of Mongolia and the governance at the local level should
embrace job creation through stimulation of decent health sectors jobs majorly in youths and
women with the right skills and standard numbers in both rural and urban areas ("Department of
Health | Health workforce", 2018). This can be done by creating labor market policies in health
sectors which can boost sustainable health workforce thus preventing workers to have second
jobs in private sectors but creating a gap for new jobs ("Human Resources for Health-Mongolia",
2014). Due to the fact that health sector is growing in Mongolia employing women and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




