SARAH Network Motor-Functional Evaluation Scale for Cerebral Palsy
VerifiedAdded on 2023/06/26
|36
|14369
|222
Practical Assignment
AI Summary
This document presents the SARAH Network of Rehabilitation Hospitals' motor-functional evaluation scale designed for children and adolescents with cerebral palsy. It includes a detailed assessment form covering various aspects of motor function, such as neurological state, motor acquisitions (head balance, rolling, creeping), locomotion (gait, wheelchair, walker, canes/crutches), gross motor skills (climbing stairs, kicking a ball, running, jumping), upper limb function (reaching, prehension, manual function), and activities of daily living (feeding, dressing, hygiene). The form provides a structured approach to evaluating patients, including sections for patient profile, neurological state, orthosis/prosthesis use, special conditions, and handedness. It outlines how to compute scores and interpret them based on age groups, offering a comprehensive tool for assessing and tracking motor-functional development in individuals with cerebral palsy. Desklib provides access to this and other solved assignments.
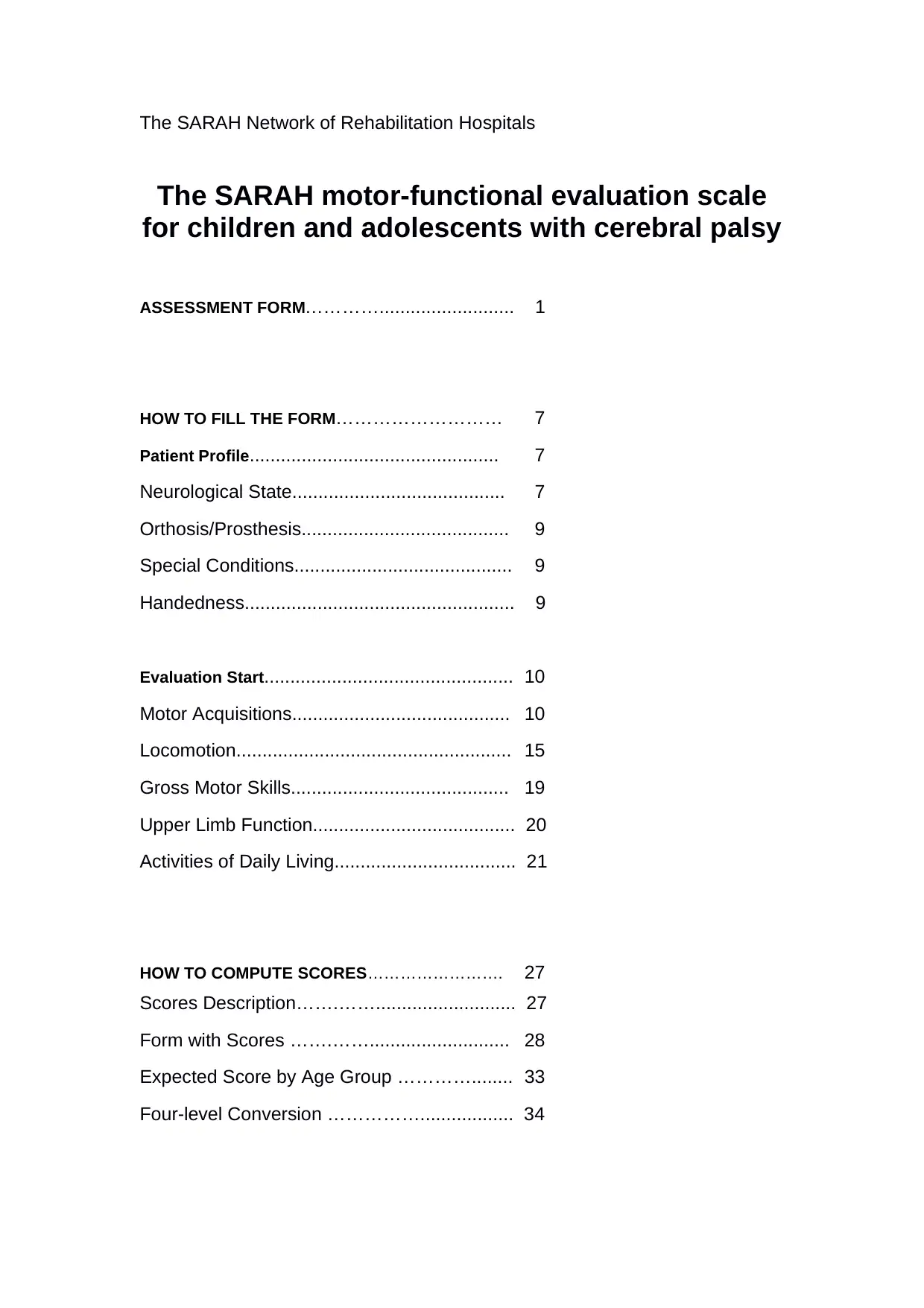
The SARAH Network of Rehabilitation Hospitals
The SARAH motor-functional evaluation scale
for children and adolescents with cerebral palsy
ASSESSMENT FORM………….......................... 1
HOW TO FILL THE FORM……………………… 7
Patient Profile................................................ 7
Neurological State......................................... 7
Orthosis/Prosthesis........................................ 9
Special Conditions.......................................... 9
Handedness.................................................... 9
Evaluation Start................................................ 10
Motor Acquisitions.......................................... 10
Locomotion..................................................... 15
Gross Motor Skills.......................................... 19
Upper Limb Function....................................... 20
Activities of Daily Living................................... 21
HOW TO COMPUTE SCORES……………………. 27
Scores Description…….……........................... 27
Form with Scores …….……........................... 28
Expected Score by Age Group …………........ 33
Four-level Conversion …………….................. 34
The SARAH motor-functional evaluation scale
for children and adolescents with cerebral palsy
ASSESSMENT FORM………….......................... 1
HOW TO FILL THE FORM……………………… 7
Patient Profile................................................ 7
Neurological State......................................... 7
Orthosis/Prosthesis........................................ 9
Special Conditions.......................................... 9
Handedness.................................................... 9
Evaluation Start................................................ 10
Motor Acquisitions.......................................... 10
Locomotion..................................................... 15
Gross Motor Skills.......................................... 19
Upper Limb Function....................................... 20
Activities of Daily Living................................... 21
HOW TO COMPUTE SCORES……………………. 27
Scores Description…….……........................... 27
Form with Scores …….……........................... 28
Expected Score by Age Group …………........ 33
Four-level Conversion …………….................. 34
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
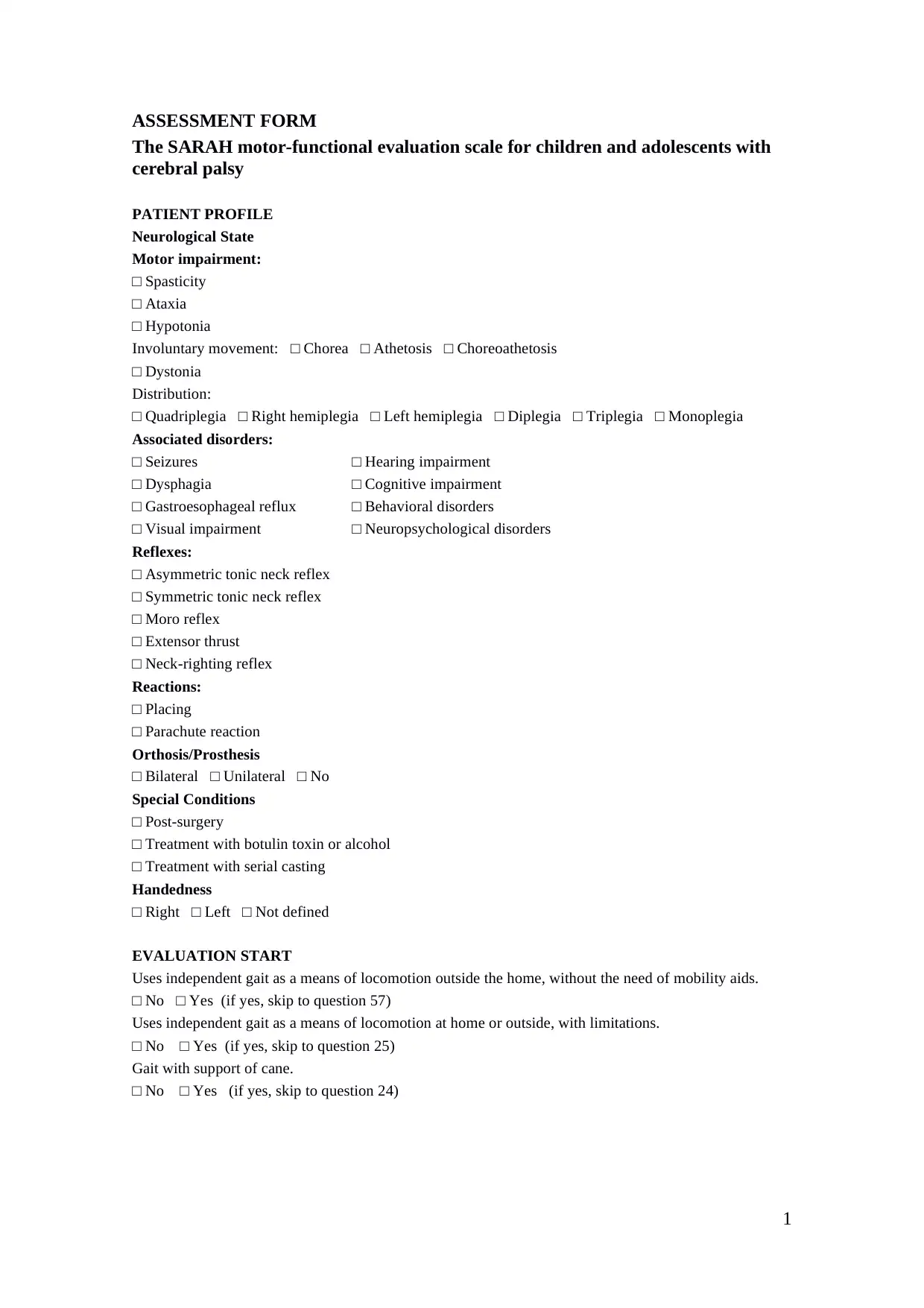
ASSESSMENT FORM
The SARAH motor-functional evaluation scale for children and adolescents with
cerebral palsy
PATIENT PROFILE
Neurological State
Motor impairment:
□ Spasticity
□ Ataxia
□ Hypotonia
Involuntary movement: □ Chorea □ Athetosis □ Choreoathetosis
□ Dystonia
Distribution:
□ Quadriplegia □ Right hemiplegia □ Left hemiplegia □ Diplegia □ Triplegia □ Monoplegia
Associated disorders:
□ Seizures □ Hearing impairment
□ Dysphagia □ Cognitive impairment
□ Gastroesophageal reflux □ Behavioral disorders
□ Visual impairment □ Neuropsychological disorders
Reflexes:
□ Asymmetric tonic neck reflex
□ Symmetric tonic neck reflex
□ Moro reflex
□ Extensor thrust
□ Neck-righting reflex
Reactions:
□ Placing
□ Parachute reaction
Orthosis/Prosthesis
□ Bilateral □ Unilateral □ No
Special Conditions
□ Post-surgery
□ Treatment with botulin toxin or alcohol
□ Treatment with serial casting
Handedness
□ Right □ Left □ Not defined
EVALUATION START
Uses independent gait as a means of locomotion outside the home, without the need of mobility aids.
□ No □ Yes (if yes, skip to question 57)
Uses independent gait as a means of locomotion at home or outside, with limitations.
□ No □ Yes (if yes, skip to question 25)
Gait with support of cane.
□ No □ Yes (if yes, skip to question 24)
ASSESSMENT FORM
The SARAH motor-functional evaluation scale for children and adolescents with
cerebral palsy
PATIENT PROFILE
Neurological State
Motor impairment:
□ Spasticity
□ Ataxia
□ Hypotonia
Involuntary movement: □ Chorea □ Athetosis □ Choreoathetosis
□ Dystonia
Distribution:
□ Quadriplegia □ Right hemiplegia □ Left hemiplegia □ Diplegia □ Triplegia □ Monoplegia
Associated disorders:
□ Seizures □ Hearing impairment
□ Dysphagia □ Cognitive impairment
□ Gastroesophageal reflux □ Behavioral disorders
□ Visual impairment □ Neuropsychological disorders
Reflexes:
□ Asymmetric tonic neck reflex
□ Symmetric tonic neck reflex
□ Moro reflex
□ Extensor thrust
□ Neck-righting reflex
Reactions:
□ Placing
□ Parachute reaction
Orthosis/Prosthesis
□ Bilateral □ Unilateral □ No
Special Conditions
□ Post-surgery
□ Treatment with botulin toxin or alcohol
□ Treatment with serial casting
Handedness
□ Right □ Left □ Not defined
EVALUATION START
Uses independent gait as a means of locomotion outside the home, without the need of mobility aids.
□ No □ Yes (if yes, skip to question 57)
Uses independent gait as a means of locomotion at home or outside, with limitations.
□ No □ Yes (if yes, skip to question 25)
Gait with support of cane.
□ No □ Yes (if yes, skip to question 24)
2
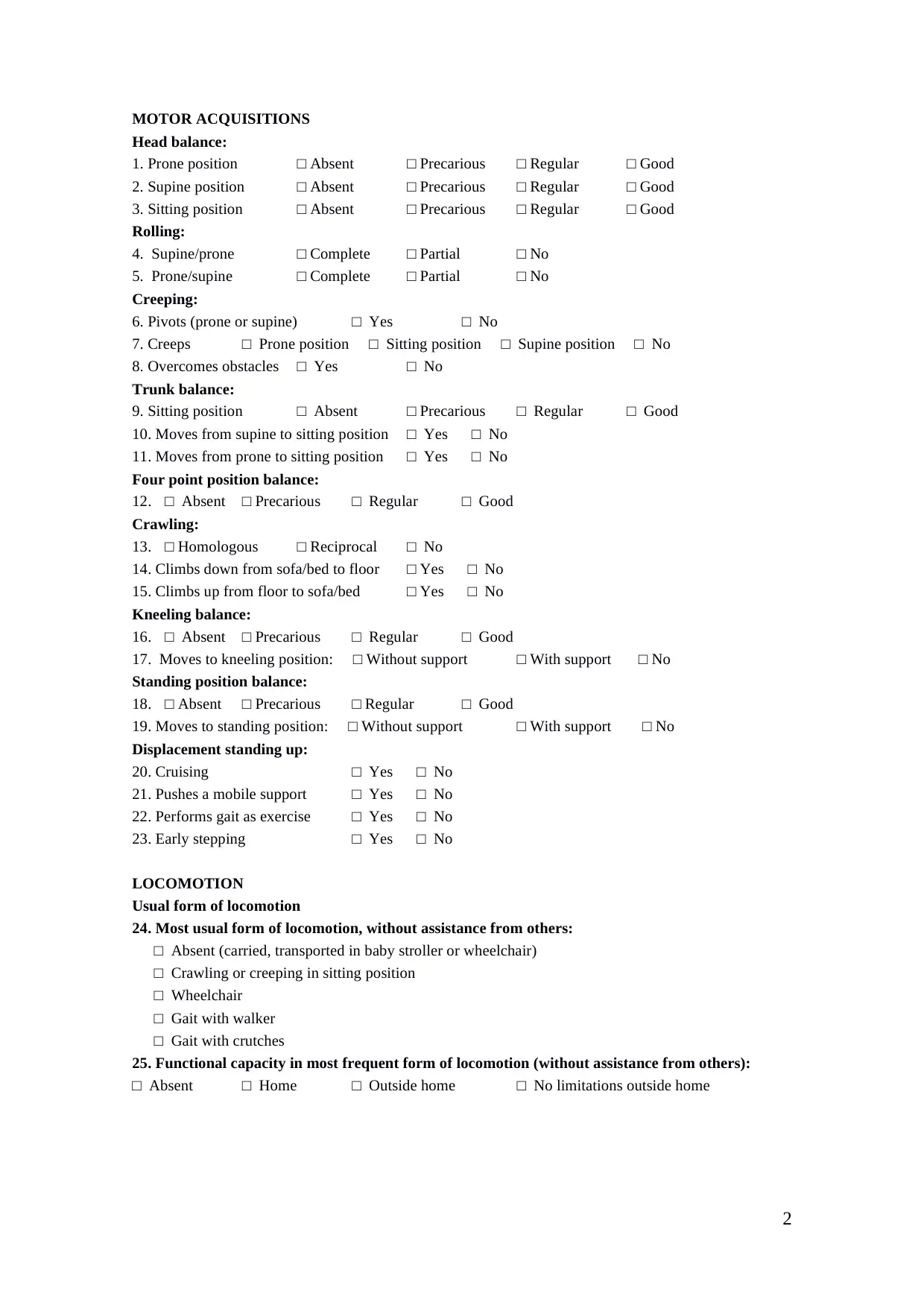
MOTOR ACQUISITIONS
Head balance:
1. Prone position □ Absent □ Precarious □ Regular □ Good
2. Supine position □ Absent □ Precarious □ Regular □ Good
3. Sitting position □ Absent □ Precarious □ Regular □ Good
Rolling:
4. Supine/prone □ Complete □ Partial □ No
5. Prone/supine □ Complete □ Partial □ No
Creeping:
6. Pivots (prone or supine) □ Yes □ No
7. Creeps □ Prone position □ Sitting position □ Supine position □ No
8. Overcomes obstacles □ Yes □ No
Trunk balance:
9. Sitting position □ Absent □ Precarious □ Regular □ Good
10. Moves from supine to sitting position □ Yes □ No
11. Moves from prone to sitting position □ Yes □ No
Four point position balance:
12. □ Absent □ Precarious □ Regular □ Good
Crawling:
13. □ Homologous □ Reciprocal □ No
14. Climbs down from sofa/bed to floor □ Yes □ No
15. Climbs up from floor to sofa/bed □ Yes □ No
Kneeling balance:
16. □ Absent □ Precarious □ Regular □ Good
17. Moves to kneeling position: □ Without support □ With support □ No
Standing position balance:
18. □ Absent □ Precarious □ Regular □ Good
19. Moves to standing position: □ Without support □ With support □ No
Displacement standing up:
20. Cruising □ Yes □ No
21. Pushes a mobile support □ Yes □ No
22. Performs gait as exercise □ Yes □ No
23. Early stepping □ Yes □ No
LOCOMOTION
Usual form of locomotion
24. Most usual form of locomotion, without assistance from others:
□ Absent (carried, transported in baby stroller or wheelchair)
□ Crawling or creeping in sitting position
□ Wheelchair
□ Gait with walker
□ Gait with crutches
25. Functional capacity in most frequent form of locomotion (without assistance from others):
□ Absent □ Home □ Outside home □ No limitations outside home
MOTOR ACQUISITIONS
Head balance:
1. Prone position □ Absent □ Precarious □ Regular □ Good
2. Supine position □ Absent □ Precarious □ Regular □ Good
3. Sitting position □ Absent □ Precarious □ Regular □ Good
Rolling:
4. Supine/prone □ Complete □ Partial □ No
5. Prone/supine □ Complete □ Partial □ No
Creeping:
6. Pivots (prone or supine) □ Yes □ No
7. Creeps □ Prone position □ Sitting position □ Supine position □ No
8. Overcomes obstacles □ Yes □ No
Trunk balance:
9. Sitting position □ Absent □ Precarious □ Regular □ Good
10. Moves from supine to sitting position □ Yes □ No
11. Moves from prone to sitting position □ Yes □ No
Four point position balance:
12. □ Absent □ Precarious □ Regular □ Good
Crawling:
13. □ Homologous □ Reciprocal □ No
14. Climbs down from sofa/bed to floor □ Yes □ No
15. Climbs up from floor to sofa/bed □ Yes □ No
Kneeling balance:
16. □ Absent □ Precarious □ Regular □ Good
17. Moves to kneeling position: □ Without support □ With support □ No
Standing position balance:
18. □ Absent □ Precarious □ Regular □ Good
19. Moves to standing position: □ Without support □ With support □ No
Displacement standing up:
20. Cruising □ Yes □ No
21. Pushes a mobile support □ Yes □ No
22. Performs gait as exercise □ Yes □ No
23. Early stepping □ Yes □ No
LOCOMOTION
Usual form of locomotion
24. Most usual form of locomotion, without assistance from others:
□ Absent (carried, transported in baby stroller or wheelchair)
□ Crawling or creeping in sitting position
□ Wheelchair
□ Gait with walker
□ Gait with crutches
25. Functional capacity in most frequent form of locomotion (without assistance from others):
□ Absent □ Home □ Outside home □ No limitations outside home
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
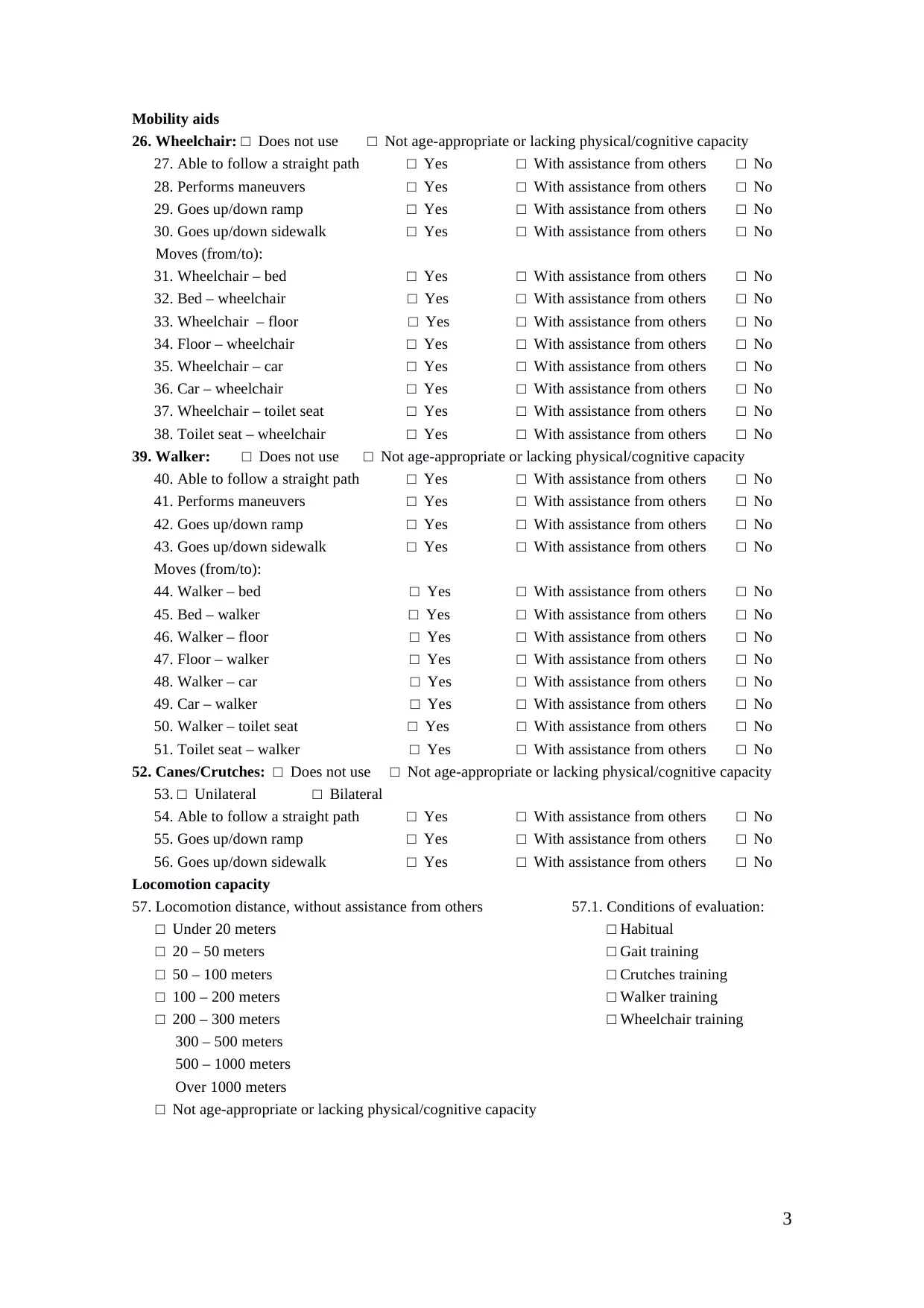
Mobility aids
26. Wheelchair: □ Does not use □ Not age-appropriate or lacking physical/cognitive capacity
27. Able to follow a straight path □ Yes □ With assistance from others □ No
28. Performs maneuvers □ Yes □ With assistance from others □ No
29. Goes up/down ramp □ Yes □ With assistance from others □ No
30. Goes up/down sidewalk □ Yes □ With assistance from others □ No
Moves (from/to):
31. Wheelchair – bed □ Yes □ With assistance from others □ No
32. Bed – wheelchair □ Yes □ With assistance from others □ No
33. Wheelchair – floor □ Yes □ With assistance from others □ No
34. Floor – wheelchair □ Yes □ With assistance from others □ No
35. Wheelchair – car □ Yes □ With assistance from others □ No
36. Car – wheelchair □ Yes □ With assistance from others □ No
37. Wheelchair – toilet seat □ Yes □ With assistance from others □ No
38. Toilet seat – wheelchair □ Yes □ With assistance from others □ No
39. Walker: □ Does not use □ Not age-appropriate or lacking physical/cognitive capacity
40. Able to follow a straight path □ Yes □ With assistance from others □ No
41. Performs maneuvers □ Yes □ With assistance from others □ No
42. Goes up/down ramp □ Yes □ With assistance from others □ No
43. Goes up/down sidewalk □ Yes □ With assistance from others □ No
Moves (from/to):
44. Walker – bed □ Yes □ With assistance from others □ No
45. Bed – walker □ Yes □ With assistance from others □ No
46. Walker – floor □ Yes □ With assistance from others □ No
47. Floor – walker □ Yes □ With assistance from others □ No
48. Walker – car □ Yes □ With assistance from others □ No
49. Car – walker □ Yes □ With assistance from others □ No
50. Walker – toilet seat □ Yes □ With assistance from others □ No
51. Toilet seat – walker □ Yes □ With assistance from others □ No
52. Canes/Crutches: □ Does not use □ Not age-appropriate or lacking physical/cognitive capacity
53. □ Unilateral □ Bilateral
54. Able to follow a straight path □ Yes □ With assistance from others □ No
55. Goes up/down ramp □ Yes □ With assistance from others □ No
56. Goes up/down sidewalk □ Yes □ With assistance from others □ No
Locomotion capacity
57. Locomotion distance, without assistance from others 57.1. Conditions of evaluation:
□ Under 20 meters □ Habitual
□ 20 – 50 meters □ Gait training
□ 50 – 100 meters □ Crutches training
□ 100 – 200 meters □ Walker training
□ 200 – 300 meters □ Wheelchair training
300 – 500 meters
500 – 1000 meters
Over 1000 meters
□ Not age-appropriate or lacking physical/cognitive capacity
Mobility aids
26. Wheelchair: □ Does not use □ Not age-appropriate or lacking physical/cognitive capacity
27. Able to follow a straight path □ Yes □ With assistance from others □ No
28. Performs maneuvers □ Yes □ With assistance from others □ No
29. Goes up/down ramp □ Yes □ With assistance from others □ No
30. Goes up/down sidewalk □ Yes □ With assistance from others □ No
Moves (from/to):
31. Wheelchair – bed □ Yes □ With assistance from others □ No
32. Bed – wheelchair □ Yes □ With assistance from others □ No
33. Wheelchair – floor □ Yes □ With assistance from others □ No
34. Floor – wheelchair □ Yes □ With assistance from others □ No
35. Wheelchair – car □ Yes □ With assistance from others □ No
36. Car – wheelchair □ Yes □ With assistance from others □ No
37. Wheelchair – toilet seat □ Yes □ With assistance from others □ No
38. Toilet seat – wheelchair □ Yes □ With assistance from others □ No
39. Walker: □ Does not use □ Not age-appropriate or lacking physical/cognitive capacity
40. Able to follow a straight path □ Yes □ With assistance from others □ No
41. Performs maneuvers □ Yes □ With assistance from others □ No
42. Goes up/down ramp □ Yes □ With assistance from others □ No
43. Goes up/down sidewalk □ Yes □ With assistance from others □ No
Moves (from/to):
44. Walker – bed □ Yes □ With assistance from others □ No
45. Bed – walker □ Yes □ With assistance from others □ No
46. Walker – floor □ Yes □ With assistance from others □ No
47. Floor – walker □ Yes □ With assistance from others □ No
48. Walker – car □ Yes □ With assistance from others □ No
49. Car – walker □ Yes □ With assistance from others □ No
50. Walker – toilet seat □ Yes □ With assistance from others □ No
51. Toilet seat – walker □ Yes □ With assistance from others □ No
52. Canes/Crutches: □ Does not use □ Not age-appropriate or lacking physical/cognitive capacity
53. □ Unilateral □ Bilateral
54. Able to follow a straight path □ Yes □ With assistance from others □ No
55. Goes up/down ramp □ Yes □ With assistance from others □ No
56. Goes up/down sidewalk □ Yes □ With assistance from others □ No
Locomotion capacity
57. Locomotion distance, without assistance from others 57.1. Conditions of evaluation:
□ Under 20 meters □ Habitual
□ 20 – 50 meters □ Gait training
□ 50 – 100 meters □ Crutches training
□ 100 – 200 meters □ Walker training
□ 200 – 300 meters □ Wheelchair training
300 – 500 meters
500 – 1000 meters
Over 1000 meters
□ Not age-appropriate or lacking physical/cognitive capacity
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
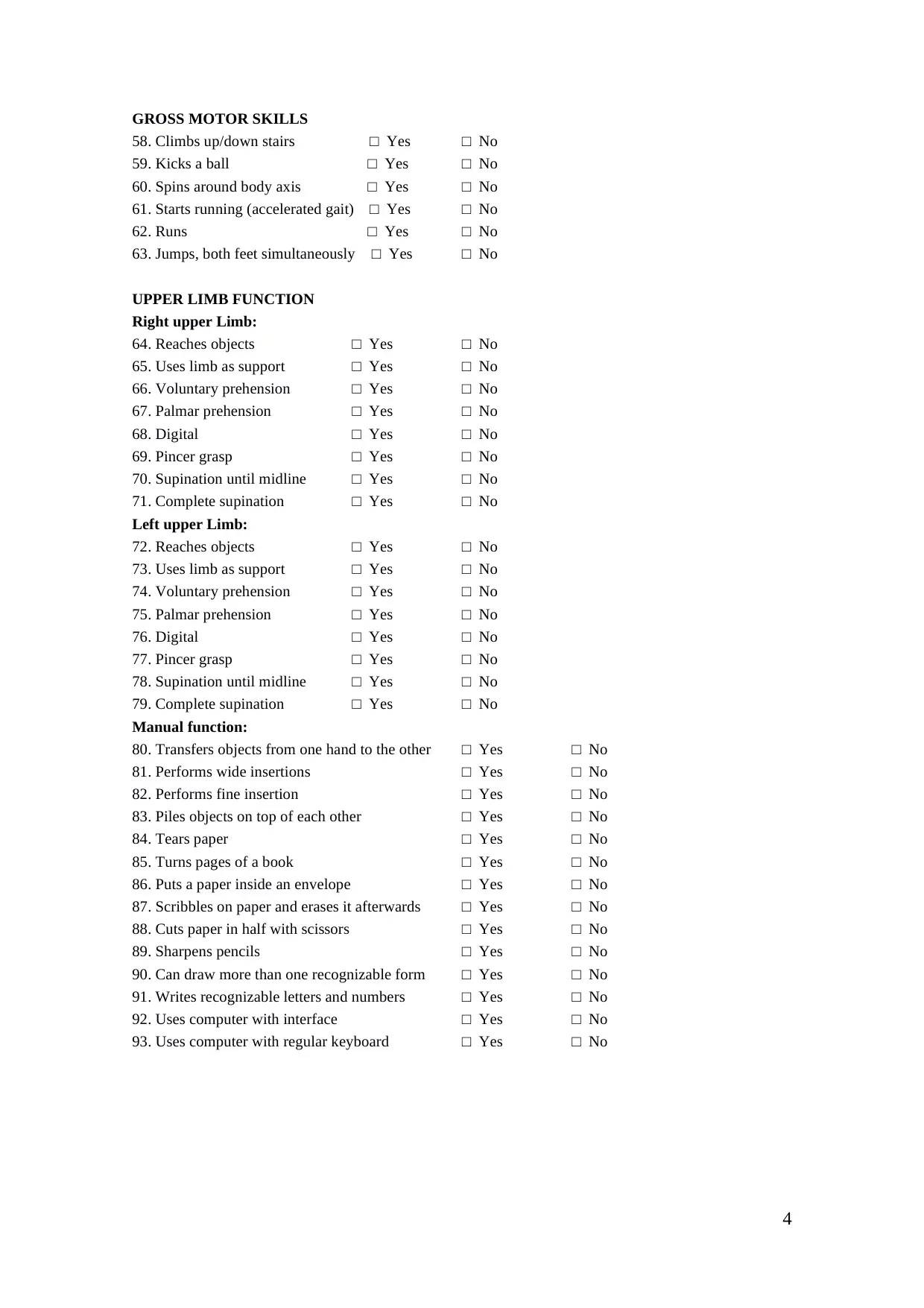
GROSS MOTOR SKILLS
58. Climbs up/down stairs □ Yes □ No
59. Kicks a ball □ Yes □ No
60. Spins around body axis □ Yes □ No
61. Starts running (accelerated gait) □ Yes □ No
62. Runs □ Yes □ No
63. Jumps, both feet simultaneously □ Yes □ No
UPPER LIMB FUNCTION
Right upper Limb:
64. Reaches objects □ Yes □ No
65. Uses limb as support □ Yes □ No
66. Voluntary prehension □ Yes □ No
67. Palmar prehension □ Yes □ No
68. Digital □ Yes □ No
69. Pincer grasp □ Yes □ No
70. Supination until midline □ Yes □ No
71. Complete supination □ Yes □ No
Left upper Limb:
72. Reaches objects □ Yes □ No
73. Uses limb as support □ Yes □ No
74. Voluntary prehension □ Yes □ No
75. Palmar prehension □ Yes □ No
76. Digital □ Yes □ No
77. Pincer grasp □ Yes □ No
78. Supination until midline □ Yes □ No
79. Complete supination □ Yes □ No
Manual function:
80. Transfers objects from one hand to the other □ Yes □ No
81. Performs wide insertions □ Yes □ No
82. Performs fine insertion □ Yes □ No
83. Piles objects on top of each other □ Yes □ No
84. Tears paper □ Yes □ No
85. Turns pages of a book □ Yes □ No
86. Puts a paper inside an envelope □ Yes □ No
87. Scribbles on paper and erases it afterwards □ Yes □ No
88. Cuts paper in half with scissors □ Yes □ No
89. Sharpens pencils □ Yes □ No
90. Can draw more than one recognizable form □ Yes □ No
91. Writes recognizable letters and numbers □ Yes □ No
92. Uses computer with interface □ Yes □ No
93. Uses computer with regular keyboard □ Yes □ No
GROSS MOTOR SKILLS
58. Climbs up/down stairs □ Yes □ No
59. Kicks a ball □ Yes □ No
60. Spins around body axis □ Yes □ No
61. Starts running (accelerated gait) □ Yes □ No
62. Runs □ Yes □ No
63. Jumps, both feet simultaneously □ Yes □ No
UPPER LIMB FUNCTION
Right upper Limb:
64. Reaches objects □ Yes □ No
65. Uses limb as support □ Yes □ No
66. Voluntary prehension □ Yes □ No
67. Palmar prehension □ Yes □ No
68. Digital □ Yes □ No
69. Pincer grasp □ Yes □ No
70. Supination until midline □ Yes □ No
71. Complete supination □ Yes □ No
Left upper Limb:
72. Reaches objects □ Yes □ No
73. Uses limb as support □ Yes □ No
74. Voluntary prehension □ Yes □ No
75. Palmar prehension □ Yes □ No
76. Digital □ Yes □ No
77. Pincer grasp □ Yes □ No
78. Supination until midline □ Yes □ No
79. Complete supination □ Yes □ No
Manual function:
80. Transfers objects from one hand to the other □ Yes □ No
81. Performs wide insertions □ Yes □ No
82. Performs fine insertion □ Yes □ No
83. Piles objects on top of each other □ Yes □ No
84. Tears paper □ Yes □ No
85. Turns pages of a book □ Yes □ No
86. Puts a paper inside an envelope □ Yes □ No
87. Scribbles on paper and erases it afterwards □ Yes □ No
88. Cuts paper in half with scissors □ Yes □ No
89. Sharpens pencils □ Yes □ No
90. Can draw more than one recognizable form □ Yes □ No
91. Writes recognizable letters and numbers □ Yes □ No
92. Uses computer with interface □ Yes □ No
93. Uses computer with regular keyboard □ Yes □ No
5
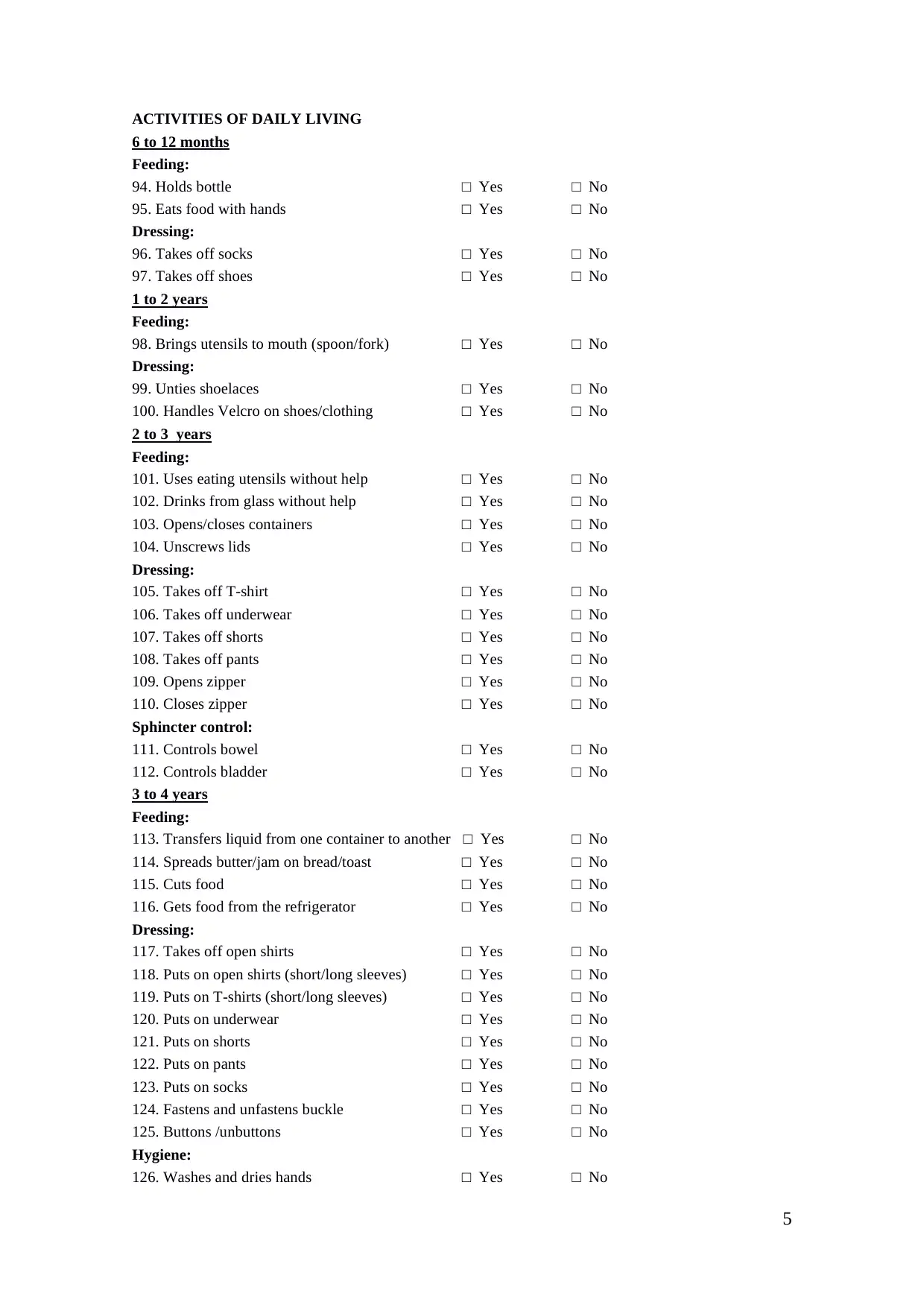
ACTIVITIES OF DAILY LIVING
6 to 12 months
Feeding:
94. Holds bottle □ Yes □ No
95. Eats food with hands □ Yes □ No
Dressing:
96. Takes off socks □ Yes □ No
97. Takes off shoes □ Yes □ No
1 to 2 years
Feeding:
98. Brings utensils to mouth (spoon/fork) □ Yes □ No
Dressing:
99. Unties shoelaces □ Yes □ No
100. Handles Velcro on shoes/clothing □ Yes □ No
2 to 3 years
Feeding:
101. Uses eating utensils without help □ Yes □ No
102. Drinks from glass without help □ Yes □ No
103. Opens/closes containers □ Yes □ No
104. Unscrews lids □ Yes □ No
Dressing:
105. Takes off T-shirt □ Yes □ No
106. Takes off underwear □ Yes □ No
107. Takes off shorts □ Yes □ No
108. Takes off pants □ Yes □ No
109. Opens zipper □ Yes □ No
110. Closes zipper □ Yes □ No
Sphincter control:
111. Controls bowel □ Yes □ No
112. Controls bladder □ Yes □ No
3 to 4 years
Feeding:
113. Transfers liquid from one container to another □ Yes □ No
114. Spreads butter/jam on bread/toast □ Yes □ No
115. Cuts food □ Yes □ No
116. Gets food from the refrigerator □ Yes □ No
Dressing:
117. Takes off open shirts □ Yes □ No
118. Puts on open shirts (short/long sleeves) □ Yes □ No
119. Puts on T-shirts (short/long sleeves) □ Yes □ No
120. Puts on underwear □ Yes □ No
121. Puts on shorts □ Yes □ No
122. Puts on pants □ Yes □ No
123. Puts on socks □ Yes □ No
124. Fastens and unfastens buckle □ Yes □ No
125. Buttons /unbuttons □ Yes □ No
Hygiene:
126. Washes and dries hands □ Yes □ No
ACTIVITIES OF DAILY LIVING
6 to 12 months
Feeding:
94. Holds bottle □ Yes □ No
95. Eats food with hands □ Yes □ No
Dressing:
96. Takes off socks □ Yes □ No
97. Takes off shoes □ Yes □ No
1 to 2 years
Feeding:
98. Brings utensils to mouth (spoon/fork) □ Yes □ No
Dressing:
99. Unties shoelaces □ Yes □ No
100. Handles Velcro on shoes/clothing □ Yes □ No
2 to 3 years
Feeding:
101. Uses eating utensils without help □ Yes □ No
102. Drinks from glass without help □ Yes □ No
103. Opens/closes containers □ Yes □ No
104. Unscrews lids □ Yes □ No
Dressing:
105. Takes off T-shirt □ Yes □ No
106. Takes off underwear □ Yes □ No
107. Takes off shorts □ Yes □ No
108. Takes off pants □ Yes □ No
109. Opens zipper □ Yes □ No
110. Closes zipper □ Yes □ No
Sphincter control:
111. Controls bowel □ Yes □ No
112. Controls bladder □ Yes □ No
3 to 4 years
Feeding:
113. Transfers liquid from one container to another □ Yes □ No
114. Spreads butter/jam on bread/toast □ Yes □ No
115. Cuts food □ Yes □ No
116. Gets food from the refrigerator □ Yes □ No
Dressing:
117. Takes off open shirts □ Yes □ No
118. Puts on open shirts (short/long sleeves) □ Yes □ No
119. Puts on T-shirts (short/long sleeves) □ Yes □ No
120. Puts on underwear □ Yes □ No
121. Puts on shorts □ Yes □ No
122. Puts on pants □ Yes □ No
123. Puts on socks □ Yes □ No
124. Fastens and unfastens buckle □ Yes □ No
125. Buttons /unbuttons □ Yes □ No
Hygiene:
126. Washes and dries hands □ Yes □ No
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
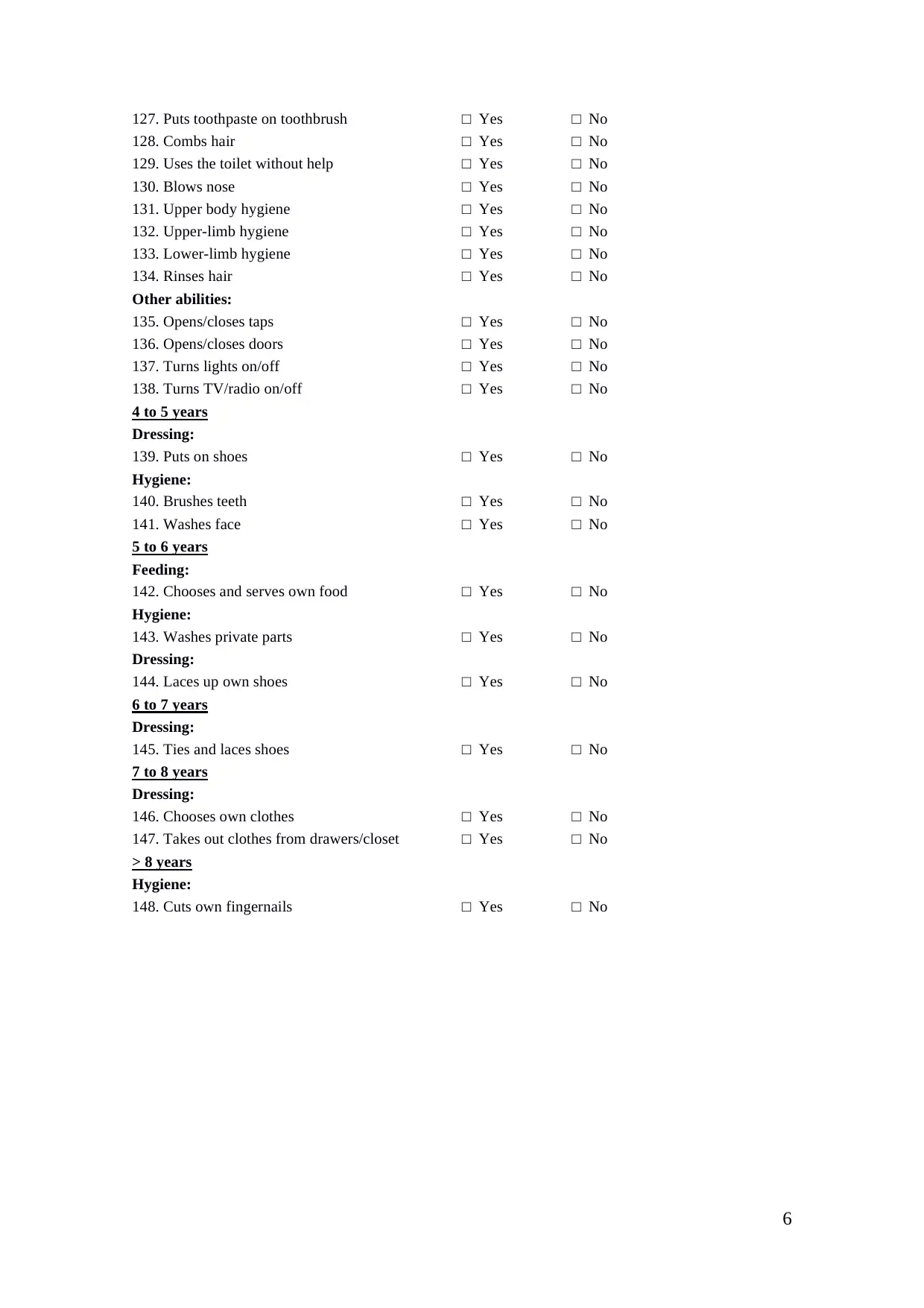
6
127. Puts toothpaste on toothbrush □ Yes □ No
128. Combs hair □ Yes □ No
129. Uses the toilet without help □ Yes □ No
130. Blows nose □ Yes □ No
131. Upper body hygiene □ Yes □ No
132. Upper-limb hygiene □ Yes □ No
133. Lower-limb hygiene □ Yes □ No
134. Rinses hair □ Yes □ No
Other abilities:
135. Opens/closes taps □ Yes □ No
136. Opens/closes doors □ Yes □ No
137. Turns lights on/off □ Yes □ No
138. Turns TV/radio on/off □ Yes □ No
4 to 5 years
Dressing:
139. Puts on shoes □ Yes □ No
Hygiene:
140. Brushes teeth □ Yes □ No
141. Washes face □ Yes □ No
5 to 6 years
Feeding:
142. Chooses and serves own food □ Yes □ No
Hygiene:
143. Washes private parts □ Yes □ No
Dressing:
144. Laces up own shoes □ Yes □ No
6 to 7 years
Dressing:
145. Ties and laces shoes □ Yes □ No
7 to 8 years
Dressing:
146. Chooses own clothes □ Yes □ No
147. Takes out clothes from drawers/closet □ Yes □ No
> 8 years
Hygiene:
148. Cuts own fingernails □ Yes □ No
127. Puts toothpaste on toothbrush □ Yes □ No
128. Combs hair □ Yes □ No
129. Uses the toilet without help □ Yes □ No
130. Blows nose □ Yes □ No
131. Upper body hygiene □ Yes □ No
132. Upper-limb hygiene □ Yes □ No
133. Lower-limb hygiene □ Yes □ No
134. Rinses hair □ Yes □ No
Other abilities:
135. Opens/closes taps □ Yes □ No
136. Opens/closes doors □ Yes □ No
137. Turns lights on/off □ Yes □ No
138. Turns TV/radio on/off □ Yes □ No
4 to 5 years
Dressing:
139. Puts on shoes □ Yes □ No
Hygiene:
140. Brushes teeth □ Yes □ No
141. Washes face □ Yes □ No
5 to 6 years
Feeding:
142. Chooses and serves own food □ Yes □ No
Hygiene:
143. Washes private parts □ Yes □ No
Dressing:
144. Laces up own shoes □ Yes □ No
6 to 7 years
Dressing:
145. Ties and laces shoes □ Yes □ No
7 to 8 years
Dressing:
146. Chooses own clothes □ Yes □ No
147. Takes out clothes from drawers/closet □ Yes □ No
> 8 years
Hygiene:
148. Cuts own fingernails □ Yes □ No
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
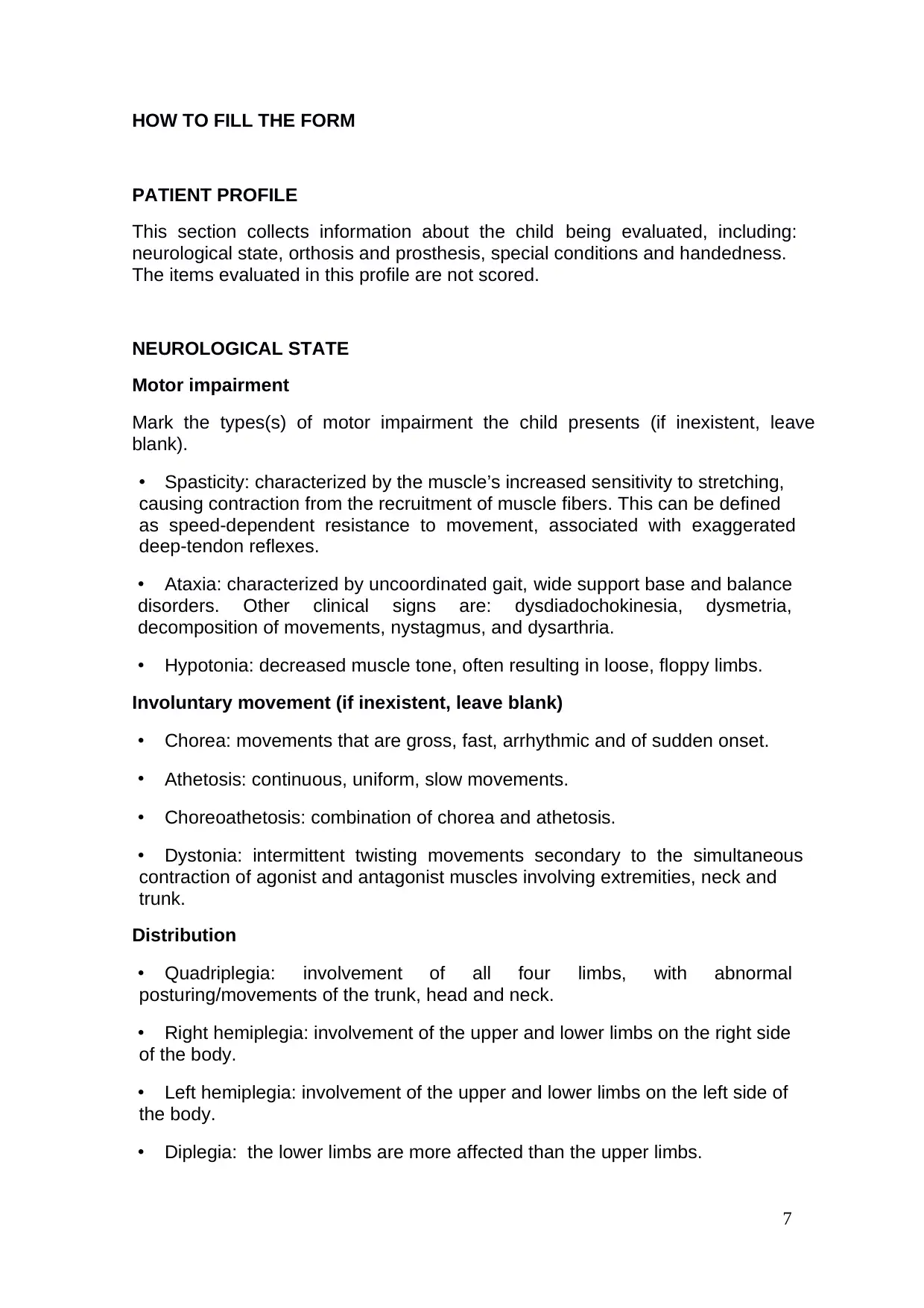
HOW TO FILL THE FORM
PATIENT PROFILE
This section collects information about the child being evaluated, including:
neurological state, orthosis and prosthesis, special conditions and handedness.
The items evaluated in this profile are not scored.
NEUROLOGICAL STATE
Motor impairment
Mark the types(s) of motor impairment the child presents (if inexistent, leave
blank).
• Spasticity: characterized by the muscle’s increased sensitivity to stretching,
causing contraction from the recruitment of muscle fibers. This can be defined
as speed-dependent resistance to movement, associated with exaggerated
deep-tendon reflexes.
• Ataxia: characterized by uncoordinated gait, wide support base and balance
disorders. Other clinical signs are: dysdiadochokinesia, dysmetria,
decomposition of movements, nystagmus, and dysarthria.
• Hypotonia: decreased muscle tone, often resulting in loose, floppy limbs.
Involuntary movement (if inexistent, leave blank)
• Chorea: movements that are gross, fast, arrhythmic and of sudden onset.
• Athetosis: continuous, uniform, slow movements.
• Choreoathetosis: combination of chorea and athetosis.
• Dystonia: intermittent twisting movements secondary to the simultaneous
contraction of agonist and antagonist muscles involving extremities, neck and
trunk.
Distribution
• Quadriplegia: involvement of all four limbs, with abnormal
posturing/movements of the trunk, head and neck.
• Right hemiplegia: involvement of the upper and lower limbs on the right side
of the body.
• Left hemiplegia: involvement of the upper and lower limbs on the left side of
the body.
• Diplegia: the lower limbs are more affected than the upper limbs.
HOW TO FILL THE FORM
PATIENT PROFILE
This section collects information about the child being evaluated, including:
neurological state, orthosis and prosthesis, special conditions and handedness.
The items evaluated in this profile are not scored.
NEUROLOGICAL STATE
Motor impairment
Mark the types(s) of motor impairment the child presents (if inexistent, leave
blank).
• Spasticity: characterized by the muscle’s increased sensitivity to stretching,
causing contraction from the recruitment of muscle fibers. This can be defined
as speed-dependent resistance to movement, associated with exaggerated
deep-tendon reflexes.
• Ataxia: characterized by uncoordinated gait, wide support base and balance
disorders. Other clinical signs are: dysdiadochokinesia, dysmetria,
decomposition of movements, nystagmus, and dysarthria.
• Hypotonia: decreased muscle tone, often resulting in loose, floppy limbs.
Involuntary movement (if inexistent, leave blank)
• Chorea: movements that are gross, fast, arrhythmic and of sudden onset.
• Athetosis: continuous, uniform, slow movements.
• Choreoathetosis: combination of chorea and athetosis.
• Dystonia: intermittent twisting movements secondary to the simultaneous
contraction of agonist and antagonist muscles involving extremities, neck and
trunk.
Distribution
• Quadriplegia: involvement of all four limbs, with abnormal
posturing/movements of the trunk, head and neck.
• Right hemiplegia: involvement of the upper and lower limbs on the right side
of the body.
• Left hemiplegia: involvement of the upper and lower limbs on the left side of
the body.
• Diplegia: the lower limbs are more affected than the upper limbs.
8
• Triplegia: predominant involvement of 3 limbs, normally the lower limbs and
one of the upper limbs.
• Monoplegia: involvement of only one limb.
Associated disorders (if inexistent, leave blank)
• Seizures
• Dysphagia
• Gastroesophageal reflux
• Visual impairment
• Hearing deficits
• Cognitive impairment
• Behavioral disorders
• Neuropsychological disorders.
Reflexes
Should be tested in children up to 2 years of age; or in cases of tetraplegia
and/or involuntary movements up to 7 years of age (if inexistent, leave blank)
• Asymmetric tonic neck reflex: flexion of the upper and lower limbs on the
skull side and extension on the facing side in supine position. In some children
with cerebral palsy, only one of the upper limbs may manifest an obvious reflex,
together with a milder postural change in one of the lower limb.
• Symmetric tonic neck reflex: the child is placed in the crawling position.
When the head in flexed ventrally, flexion of the forelimbs and extension of the
lower limbs results; extension of the head and neck causes extension of the
upper limbs and flexion of the lower limbs.
• Moro reflex: is a sudden abduction and extension of the upper limbs with
spreading of the fingers followed by an embrace.
• Extensor thrust: the child is lifted by the axilla and suspended and then
lowered so that the feet touch the floor. A positive response consists in
extension of the lower limbs progressing upward into the trunk.
• Neck-righting reflex: positive if the shoulder girdle and trunk turn
simultaneously when the head is turned.
• Triplegia: predominant involvement of 3 limbs, normally the lower limbs and
one of the upper limbs.
• Monoplegia: involvement of only one limb.
Associated disorders (if inexistent, leave blank)
• Seizures
• Dysphagia
• Gastroesophageal reflux
• Visual impairment
• Hearing deficits
• Cognitive impairment
• Behavioral disorders
• Neuropsychological disorders.
Reflexes
Should be tested in children up to 2 years of age; or in cases of tetraplegia
and/or involuntary movements up to 7 years of age (if inexistent, leave blank)
• Asymmetric tonic neck reflex: flexion of the upper and lower limbs on the
skull side and extension on the facing side in supine position. In some children
with cerebral palsy, only one of the upper limbs may manifest an obvious reflex,
together with a milder postural change in one of the lower limb.
• Symmetric tonic neck reflex: the child is placed in the crawling position.
When the head in flexed ventrally, flexion of the forelimbs and extension of the
lower limbs results; extension of the head and neck causes extension of the
upper limbs and flexion of the lower limbs.
• Moro reflex: is a sudden abduction and extension of the upper limbs with
spreading of the fingers followed by an embrace.
• Extensor thrust: the child is lifted by the axilla and suspended and then
lowered so that the feet touch the floor. A positive response consists in
extension of the lower limbs progressing upward into the trunk.
• Neck-righting reflex: positive if the shoulder girdle and trunk turn
simultaneously when the head is turned.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
Reactions (if inexistent leave blank)
• Placing: Should be tested in children between 3 months and 2 years of age.
Hold the child by the chest and axilla, bring the dorsal surface of the feet
upward against the edge of a table. Automatic foot placement on the tabletop
surface occurs either symmetrically or asymmetrically.
• Parachute reaction: Should be tested in children between 7 months and 2
years of age. Place the child in a prone position. Lift horizontally from the table
and then quickly lower to tabletop or similar surface. This movement should
yield an automatic protective extension of the upper limbs and hands. If the
child has severe impairment of an upper limb, the protective placement of the
upper limbs may be unilateral.
ORTHOSIS/PROSTHESIS
• Yes: wears orthosis/prosthesis. Specify if it is unilateral or bilateral and the
reason for its use.
• No: does not wear orthosis/prosthesis.
SPECIAL CONDITIONS
• Post-surgery: fill out this item in cases up to 1 year post-surgery.
• Treatment with botulin toxin or alcohol: fill out this item in cases up to 6
months post-procedure.
• Treatment with serial casting: fill out this item in cases up to 6 months post-
procedure.
HANDEDNESS
• Mark the manual dominance (right or left). This information can be obtained
from the family and should be confirmed by observing the child’s performance
during the evaluation. In case the manual dominance is not defined, mark “not
defined”.
Reactions (if inexistent leave blank)
• Placing: Should be tested in children between 3 months and 2 years of age.
Hold the child by the chest and axilla, bring the dorsal surface of the feet
upward against the edge of a table. Automatic foot placement on the tabletop
surface occurs either symmetrically or asymmetrically.
• Parachute reaction: Should be tested in children between 7 months and 2
years of age. Place the child in a prone position. Lift horizontally from the table
and then quickly lower to tabletop or similar surface. This movement should
yield an automatic protective extension of the upper limbs and hands. If the
child has severe impairment of an upper limb, the protective placement of the
upper limbs may be unilateral.
ORTHOSIS/PROSTHESIS
• Yes: wears orthosis/prosthesis. Specify if it is unilateral or bilateral and the
reason for its use.
• No: does not wear orthosis/prosthesis.
SPECIAL CONDITIONS
• Post-surgery: fill out this item in cases up to 1 year post-surgery.
• Treatment with botulin toxin or alcohol: fill out this item in cases up to 6
months post-procedure.
• Treatment with serial casting: fill out this item in cases up to 6 months post-
procedure.
HANDEDNESS
• Mark the manual dominance (right or left). This information can be obtained
from the family and should be confirmed by observing the child’s performance
during the evaluation. In case the manual dominance is not defined, mark “not
defined”.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
EVALUATION START
I. Uses independent gait as a means of locomotion outside the home.
Yes: walks without assistance (no reliance on hand-held mobility devices
or a caregiver). The minimal distance that the child should be able to
walk is 300 meters. If marking this item “yes”, skip to item 57. Full credit
will be given for items 1-56).
No: incapable of unassisted gait outside. Proceed to the next item (II).
II. Uses independent gait as a means of locomotion at home or outside, with
limitations.
Yes: walks without assistance (no reliance on hand-held mobility devices
or a caregiver) at home or outside. The maximum distance that the child
is able to walk is 100 meters. If marking “yes”, skip to item 25. Full credit
will be given for items 1-24).
No: incapable of unassisted gait at home or outside. Proceed to the next
item (III).
III. Gait with support of cane
Yes: walks with cane but without caregiver’s assistance (at home or
outside). If marking “yes”, skip to item 24. Full credit will be given for
items 1-23).
No: unable to walk with canes or without caregiver’s assistance. Proceed
to item 1.
MOTOR ACQUISITIONS
Head balance:
1. Prone position
Absent: the child does not lift head.
Precarious: cervical extension up to 45° with head oscillations, then head
drops back down.
Regular: cervical extension > or equal 45° and maintains this position for
at least 10 seconds. Has difficulties rotating head or there are head
oscillations during movement.
Good: extends head 90°,maintains this position and is capable of cervical
rotation without oscillations.
EVALUATION START
I. Uses independent gait as a means of locomotion outside the home.
Yes: walks without assistance (no reliance on hand-held mobility devices
or a caregiver). The minimal distance that the child should be able to
walk is 300 meters. If marking this item “yes”, skip to item 57. Full credit
will be given for items 1-56).
No: incapable of unassisted gait outside. Proceed to the next item (II).
II. Uses independent gait as a means of locomotion at home or outside, with
limitations.
Yes: walks without assistance (no reliance on hand-held mobility devices
or a caregiver) at home or outside. The maximum distance that the child
is able to walk is 100 meters. If marking “yes”, skip to item 25. Full credit
will be given for items 1-24).
No: incapable of unassisted gait at home or outside. Proceed to the next
item (III).
III. Gait with support of cane
Yes: walks with cane but without caregiver’s assistance (at home or
outside). If marking “yes”, skip to item 24. Full credit will be given for
items 1-23).
No: unable to walk with canes or without caregiver’s assistance. Proceed
to item 1.
MOTOR ACQUISITIONS
Head balance:
1. Prone position
Absent: the child does not lift head.
Precarious: cervical extension up to 45° with head oscillations, then head
drops back down.
Regular: cervical extension > or equal 45° and maintains this position for
at least 10 seconds. Has difficulties rotating head or there are head
oscillations during movement.
Good: extends head 90°,maintains this position and is capable of cervical
rotation without oscillations.
11
2. Supine position
Absent: hyperextension of head when pulled by the arms to sitting
position.
Precarious: when first being pulled into the sitting position, there are
attempts at maintaining head and trunk alignment, but then head
oscillates and drops back down during the second half of movement arc.
Regular: head drops back down only during the final part of the
maneuver, or partial flexion of the head sustained during entire
movement arc.
Good: flexes head at beginning of maneuver (chin-tuck) and maintains it
aligned with the trunk or in maximal flexion entire movement arc
3. Sitting position
Absent: does not extend the head.
Precarious: does not maintain head and trunk alignment, but tries to
extend head. Head oscillations are observed.
Regular: head and trunk alignment maintained for at least 10 seconds,
but unable to rotate head or does so with head oscillations.
Good: head and trunk alignment maintained, head rotation without
oscillations.
Rolling:
4. Supine/prone
Complete: rolls from supine to prone.
Partial: rolls from supine to lateral decubitus. Mark this item if the child
rolling from supine to prone is "accidental" (this is caused by an
imbalance and not by a controlled action).
No: does not roll from supine to lateral decubitus or to prone, despite
intention to do so.
5. Prone/supine
Complete: voluntarily rolls from prone to supine.
Partial: rolls from prone to lateral decubitus. Full score if the rolling from
prone is “accidental”.
No: does not roll from prone to lateral decubitus or to supine, despite
intention to do so.
2. Supine position
Absent: hyperextension of head when pulled by the arms to sitting
position.
Precarious: when first being pulled into the sitting position, there are
attempts at maintaining head and trunk alignment, but then head
oscillates and drops back down during the second half of movement arc.
Regular: head drops back down only during the final part of the
maneuver, or partial flexion of the head sustained during entire
movement arc.
Good: flexes head at beginning of maneuver (chin-tuck) and maintains it
aligned with the trunk or in maximal flexion entire movement arc
3. Sitting position
Absent: does not extend the head.
Precarious: does not maintain head and trunk alignment, but tries to
extend head. Head oscillations are observed.
Regular: head and trunk alignment maintained for at least 10 seconds,
but unable to rotate head or does so with head oscillations.
Good: head and trunk alignment maintained, head rotation without
oscillations.
Rolling:
4. Supine/prone
Complete: rolls from supine to prone.
Partial: rolls from supine to lateral decubitus. Mark this item if the child
rolling from supine to prone is "accidental" (this is caused by an
imbalance and not by a controlled action).
No: does not roll from supine to lateral decubitus or to prone, despite
intention to do so.
5. Prone/supine
Complete: voluntarily rolls from prone to supine.
Partial: rolls from prone to lateral decubitus. Full score if the rolling from
prone is “accidental”.
No: does not roll from prone to lateral decubitus or to supine, despite
intention to do so.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 36
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.