University Nursing Care Plan for Mr. Thompson: Assessment 7
VerifiedAdded on 2023/01/05
|24
|4745
|29
Homework Assignment
AI Summary
This document presents a detailed nursing care plan for Mr. Peter Thompson, a 64-year-old patient admitted to the hospital with pneumonia and concerns about fluid buildup. The assignment, likely for a nursing student, outlines multiple nursing diagnoses, including anxiety related to shortness of breath, hypertension, risk of infection due to a pressure ulcer, depression, pain, risk of fluid overload, and activity intolerance. For each diagnosis, the plan includes expected patient outcomes, specific nursing interventions (such as oxygen therapy, medication management, wound care, and emotional support), rationales explaining the importance of each intervention, and evaluation criteria to assess the effectiveness of the care provided. The plan incorporates evidence-based practice, referencing relevant research to support the chosen interventions and expected results. The care plan addresses the patient's complex medical history, which includes diabetes, hypertension, asthma, and the recent loss of his wife, demonstrating a holistic approach to patient care.

Running head: NURSING DIAGNOSIS ASSIGNMENT
NURSING DIAGNOSIS ASSIGNMENT
Name of the student:
Name of the university:
Author note:
NURSING DIAGNOSIS ASSIGNMENT
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING DIAGNOSIS ASSIGNMENT
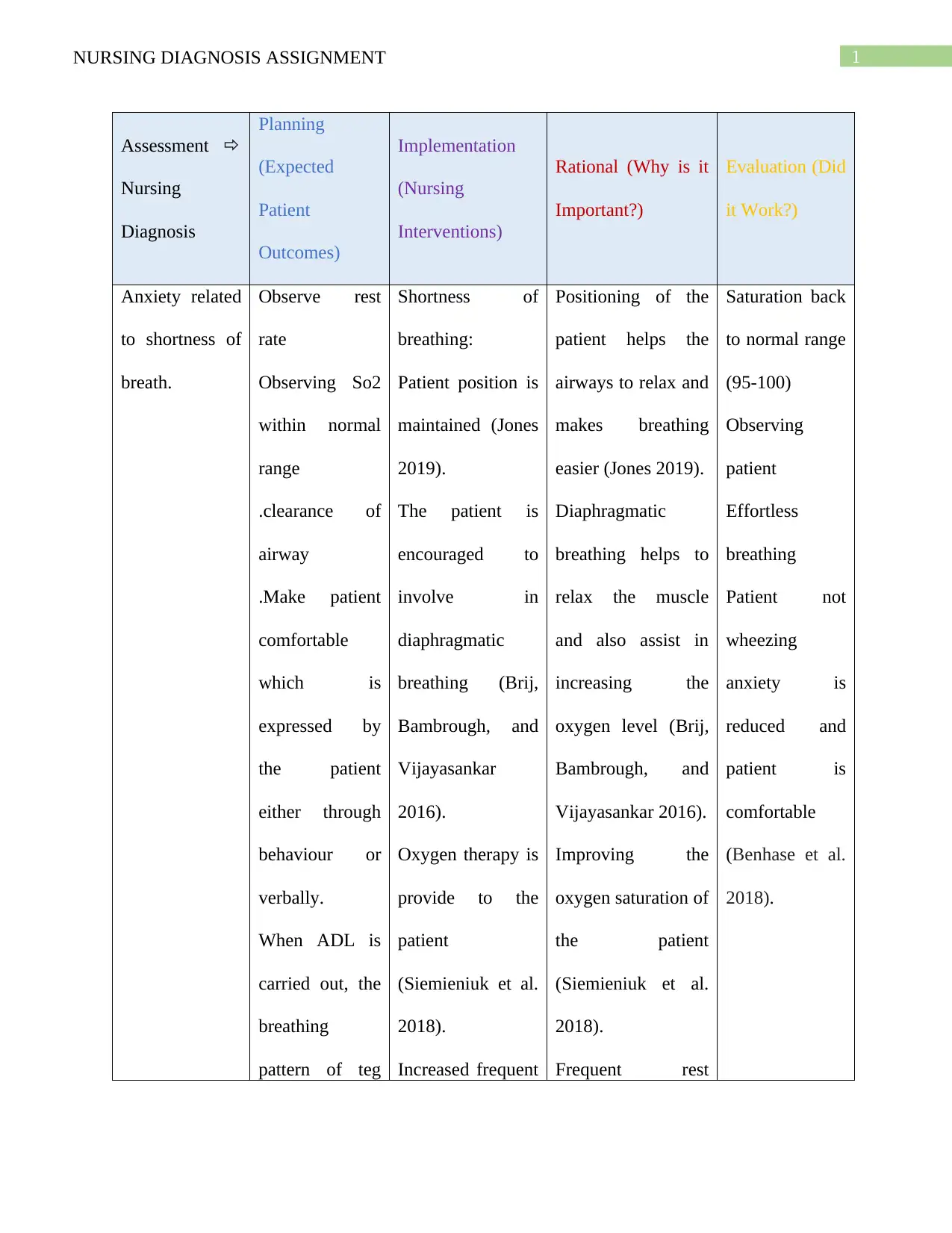
Assessment
Nursing
Diagnosis
Planning
(Expected
Patient
Outcomes)
Implementation
(Nursing
Interventions)
Rational (Why is it
Important?)
Evaluation (Did
it Work?)
Anxiety related
to shortness of
breath.
Observe rest
rate
Observing So2
within normal
range
.clearance of
airway
.Make patient
comfortable
which is
expressed by
the patient
either through
behaviour or
verbally.
When ADL is
carried out, the
breathing
pattern of teg
Shortness of
breathing:
Patient position is
maintained (Jones
2019).
The patient is
encouraged to
involve in
diaphragmatic
breathing (Brij,
Bambrough, and
Vijayasankar
2016).
Oxygen therapy is
provide to the
patient
(Siemieniuk et al.
2018).
Increased frequent
Positioning of the
patient helps the
airways to relax and
makes breathing
easier (Jones 2019).
Diaphragmatic
breathing helps to
relax the muscle
and also assist in
increasing the
oxygen level (Brij,
Bambrough, and
Vijayasankar 2016).
Improving the
oxygen saturation of
the patient
(Siemieniuk et al.
2018).
Frequent rest
Saturation back
to normal range
(95-100)
Observing
patient
Effortless
breathing
Patient not
wheezing
anxiety is
reduced and
patient is
comfortable
(Benhase et al.
2018).
Assessment
Nursing
Diagnosis
Planning
(Expected
Patient
Outcomes)
Implementation
(Nursing
Interventions)
Rational (Why is it
Important?)
Evaluation (Did
it Work?)
Anxiety related
to shortness of
breath.
Observe rest
rate
Observing So2
within normal
range
.clearance of
airway
.Make patient
comfortable
which is
expressed by
the patient
either through
behaviour or
verbally.
When ADL is
carried out, the
breathing
pattern of teg
Shortness of
breathing:
Patient position is
maintained (Jones
2019).
The patient is
encouraged to
involve in
diaphragmatic
breathing (Brij,
Bambrough, and
Vijayasankar
2016).
Oxygen therapy is
provide to the
patient
(Siemieniuk et al.
2018).
Increased frequent
Positioning of the
patient helps the
airways to relax and
makes breathing
easier (Jones 2019).
Diaphragmatic
breathing helps to
relax the muscle
and also assist in
increasing the
oxygen level (Brij,
Bambrough, and
Vijayasankar 2016).
Improving the
oxygen saturation of
the patient
(Siemieniuk et al.
2018).
Frequent rest
Saturation back
to normal range
(95-100)
Observing
patient
Effortless
breathing
Patient not
wheezing
anxiety is
reduced and
patient is
comfortable
(Benhase et al.
2018).
2NURSING DIAGNOSIS ASSIGNMENT
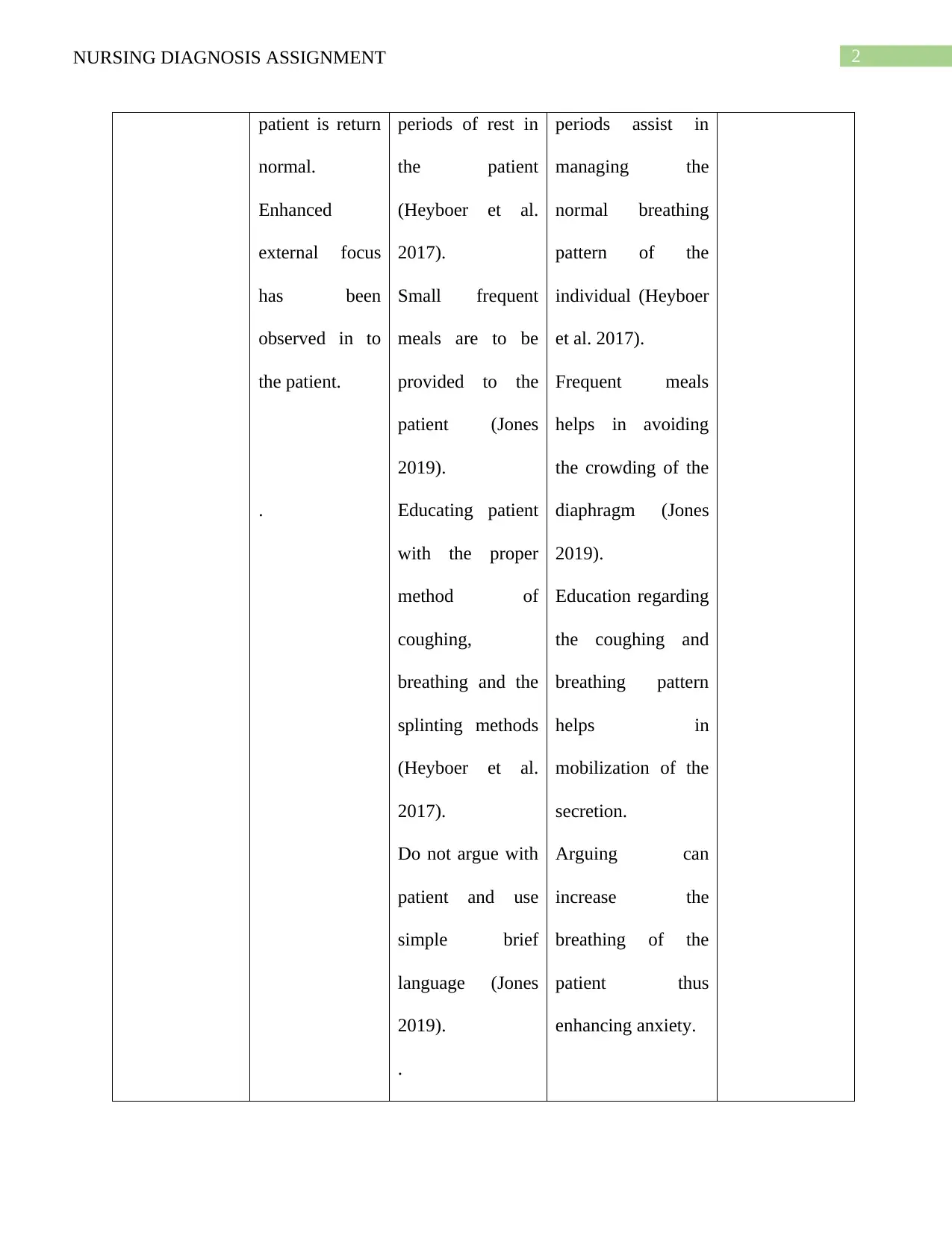
patient is return
normal.
Enhanced
external focus
has been
observed in to
the patient.
.
periods of rest in
the patient
(Heyboer et al.
2017).
Small frequent
meals are to be
provided to the
patient (Jones
2019).
Educating patient
with the proper
method of
coughing,
breathing and the
splinting methods
(Heyboer et al.
2017).
Do not argue with
patient and use
simple brief
language (Jones
2019).
.
periods assist in
managing the
normal breathing
pattern of the
individual (Heyboer
et al. 2017).
Frequent meals
helps in avoiding
the crowding of the
diaphragm (Jones
2019).
Education regarding
the coughing and
breathing pattern
helps in
mobilization of the
secretion.
Arguing can
increase the
breathing of the
patient thus
enhancing anxiety.
patient is return
normal.
Enhanced
external focus
has been
observed in to
the patient.
.
periods of rest in
the patient
(Heyboer et al.
2017).
Small frequent
meals are to be
provided to the
patient (Jones
2019).
Educating patient
with the proper
method of
coughing,
breathing and the
splinting methods
(Heyboer et al.
2017).
Do not argue with
patient and use
simple brief
language (Jones
2019).
.
periods assist in
managing the
normal breathing
pattern of the
individual (Heyboer
et al. 2017).
Frequent meals
helps in avoiding
the crowding of the
diaphragm (Jones
2019).
Education regarding
the coughing and
breathing pattern
helps in
mobilization of the
secretion.
Arguing can
increase the
breathing of the
patient thus
enhancing anxiety.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING DIAGNOSIS ASSIGNMENT
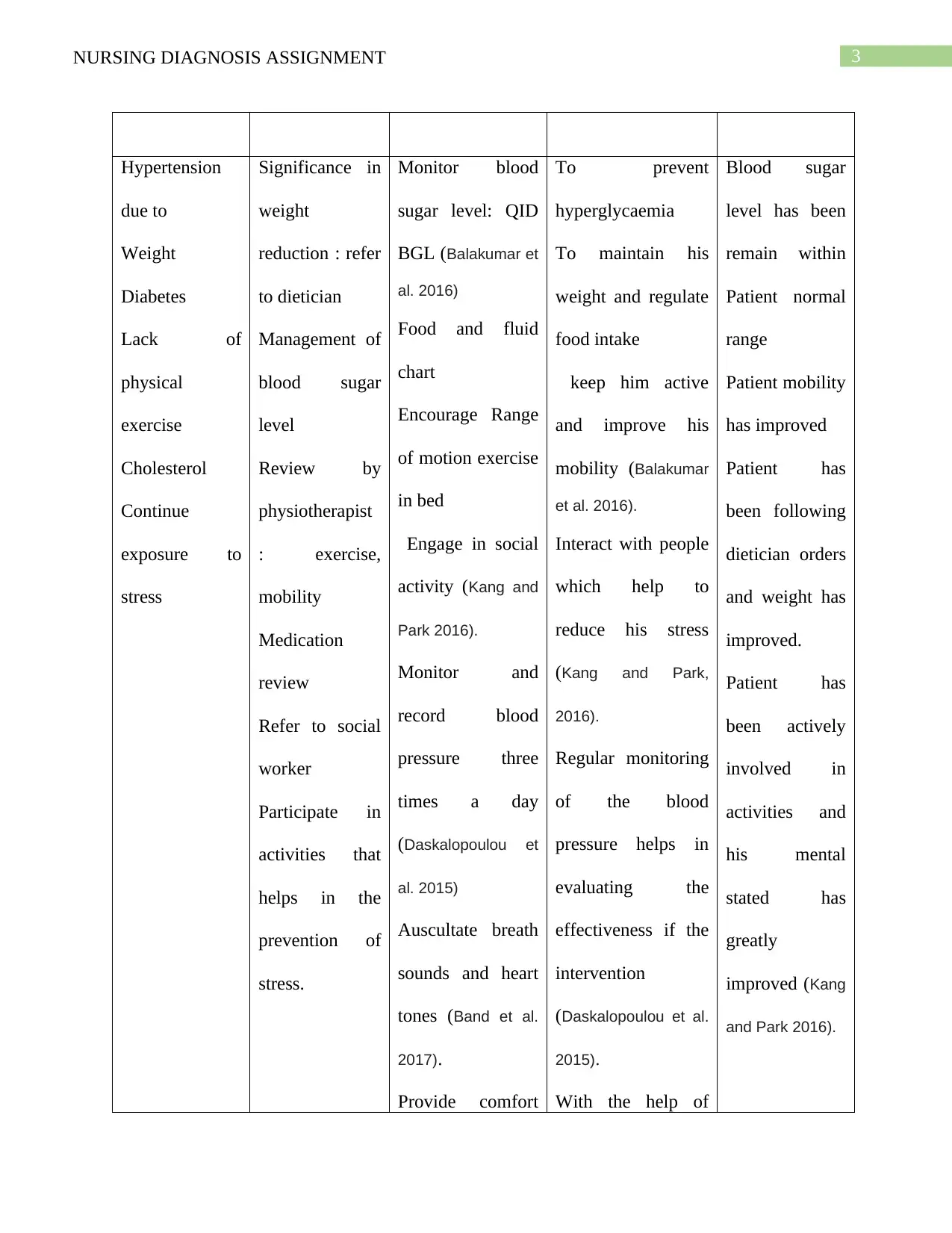
Hypertension
due to
Weight
Diabetes
Lack of
physical
exercise
Cholesterol
Continue
exposure to
stress
Significance in
weight
reduction : refer
to dietician
Management of
blood sugar
level
Review by
physiotherapist
: exercise,
mobility
Medication
review
Refer to social
worker
Participate in
activities that
helps in the
prevention of
stress.
Monitor blood
sugar level: QID
BGL (Balakumar et
al. 2016)
Food and fluid
chart
Encourage Range
of motion exercise
in bed
Engage in social
activity (Kang and
Park 2016).
Monitor and
record blood
pressure three
times a day
(Daskalopoulou et
al. 2015)
Auscultate breath
sounds and heart
tones (Band et al.
2017).
Provide comfort
To prevent
hyperglycaemia
To maintain his
weight and regulate
food intake
keep him active
and improve his
mobility (Balakumar
et al. 2016).
Interact with people
which help to
reduce his stress
(Kang and Park,
2016).
Regular monitoring
of the blood
pressure helps in
evaluating the
effectiveness if the
intervention
(Daskalopoulou et al.
2015).
With the help of
Blood sugar
level has been
remain within
Patient normal
range
Patient mobility
has improved
Patient has
been following
dietician orders
and weight has
improved.
Patient has
been actively
involved in
activities and
his mental
stated has
greatly
improved (Kang
and Park 2016).
Hypertension
due to
Weight
Diabetes
Lack of
physical
exercise
Cholesterol
Continue
exposure to
stress
Significance in
weight
reduction : refer
to dietician
Management of
blood sugar
level
Review by
physiotherapist
: exercise,
mobility
Medication
review
Refer to social
worker
Participate in
activities that
helps in the
prevention of
stress.
Monitor blood
sugar level: QID
BGL (Balakumar et
al. 2016)
Food and fluid
chart
Encourage Range
of motion exercise
in bed
Engage in social
activity (Kang and
Park 2016).
Monitor and
record blood
pressure three
times a day
(Daskalopoulou et
al. 2015)
Auscultate breath
sounds and heart
tones (Band et al.
2017).
Provide comfort
To prevent
hyperglycaemia
To maintain his
weight and regulate
food intake
keep him active
and improve his
mobility (Balakumar
et al. 2016).
Interact with people
which help to
reduce his stress
(Kang and Park,
2016).
Regular monitoring
of the blood
pressure helps in
evaluating the
effectiveness if the
intervention
(Daskalopoulou et al.
2015).
With the help of
Blood sugar
level has been
remain within
Patient normal
range
Patient mobility
has improved
Patient has
been following
dietician orders
and weight has
improved.
Patient has
been actively
involved in
activities and
his mental
stated has
greatly
improved (Kang
and Park 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING DIAGNOSIS ASSIGNMENT
measures to the
patient (Band et al.
2017).
Medication is
provided to the
patient as
prescribed by the
doctor (Conn et al.
2015).
different sounds, the
nurse is able to
identify condition of
the patient (Band et
al. 2017).
Comfort measures
such as neck
massage helps the
patient to relax and
manages the blood
level to normal
(Band et al. 2017).
Medication such as
beta-blockers helps
in lowering the
blood pressure
(Conn et al. 2015). .
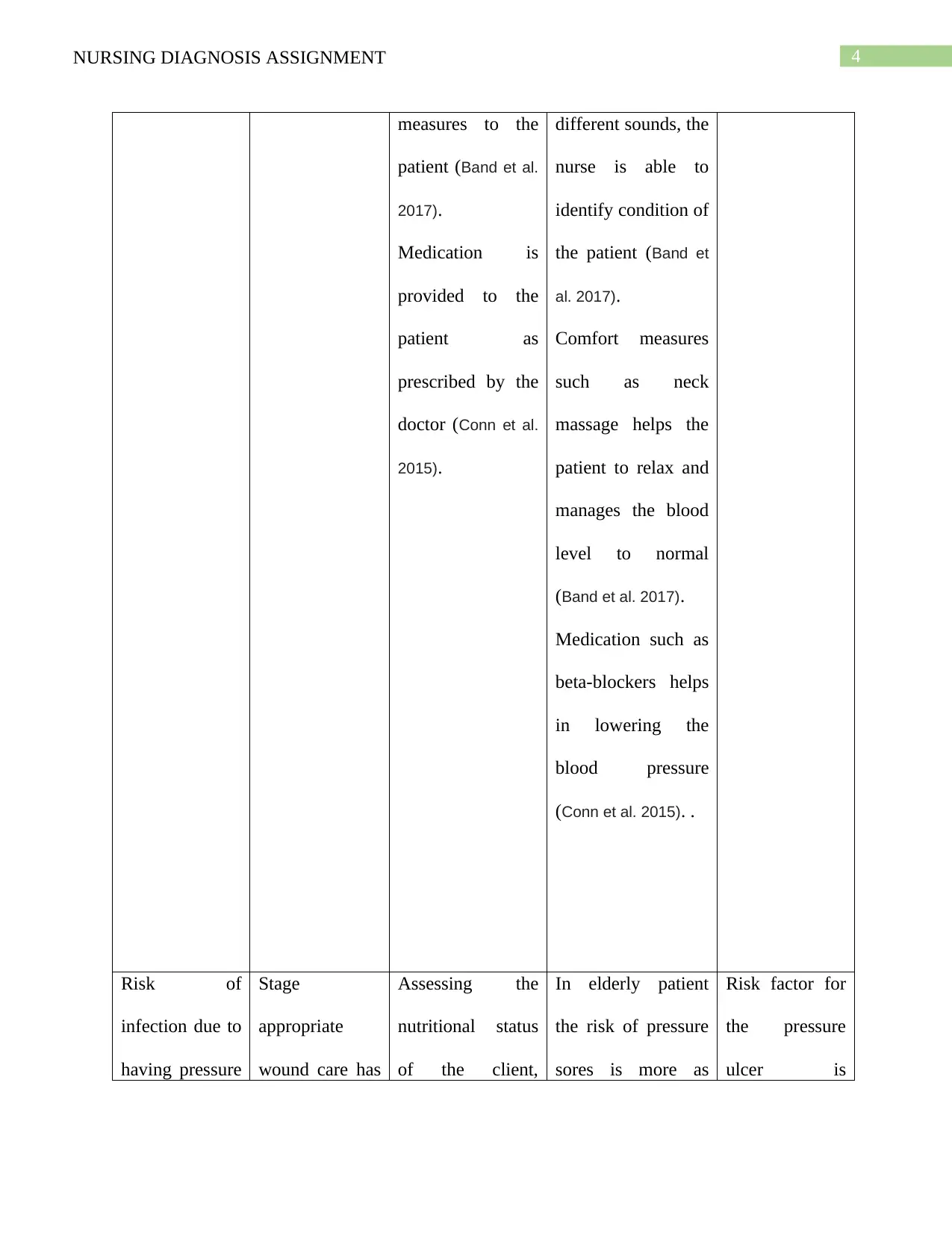
Risk of
infection due to
having pressure
Stage
appropriate
wound care has
Assessing the
nutritional status
of the client,
In elderly patient
the risk of pressure
sores is more as
Risk factor for
the pressure
ulcer is
measures to the
patient (Band et al.
2017).
Medication is
provided to the
patient as
prescribed by the
doctor (Conn et al.
2015).
different sounds, the
nurse is able to
identify condition of
the patient (Band et
al. 2017).
Comfort measures
such as neck
massage helps the
patient to relax and
manages the blood
level to normal
(Band et al. 2017).
Medication such as
beta-blockers helps
in lowering the
blood pressure
(Conn et al. 2015). .
Risk of
infection due to
having pressure
Stage
appropriate
wound care has
Assessing the
nutritional status
of the client,
In elderly patient
the risk of pressure
sores is more as
Risk factor for
the pressure
ulcer is
5NURSING DIAGNOSIS ASSIGNMENT
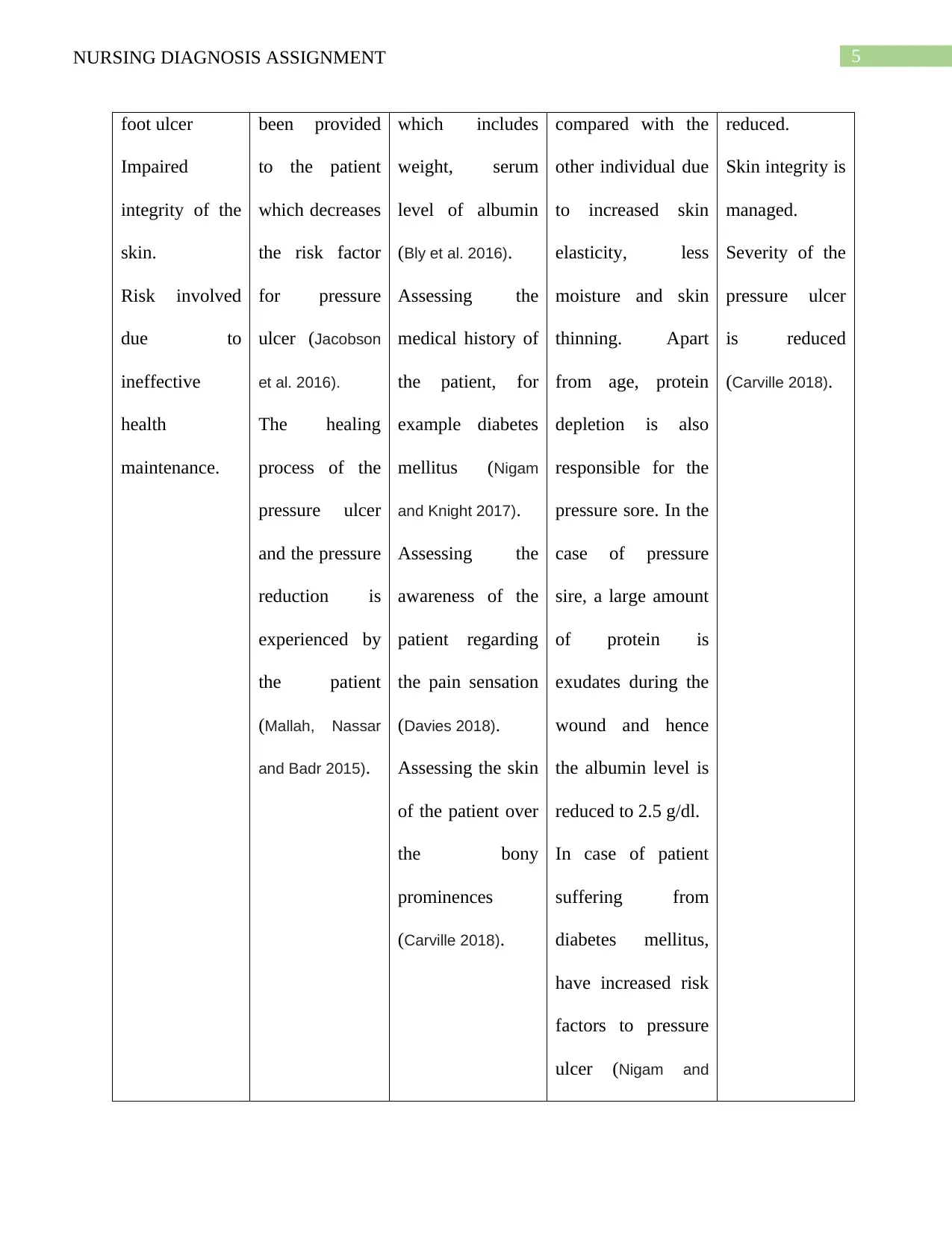
foot ulcer
Impaired
integrity of the
skin.
Risk involved
due to
ineffective
health
maintenance.
been provided
to the patient
which decreases
the risk factor
for pressure
ulcer (Jacobson
et al. 2016).
The healing
process of the
pressure ulcer
and the pressure
reduction is
experienced by
the patient
(Mallah, Nassar
and Badr 2015).
which includes
weight, serum
level of albumin
(Bly et al. 2016).
Assessing the
medical history of
the patient, for
example diabetes
mellitus (Nigam
and Knight 2017).
Assessing the
awareness of the
patient regarding
the pain sensation
(Davies 2018).
Assessing the skin
of the patient over
the bony
prominences
(Carville 2018).
compared with the
other individual due
to increased skin
elasticity, less
moisture and skin
thinning. Apart
from age, protein
depletion is also
responsible for the
pressure sore. In the
case of pressure
sire, a large amount
of protein is
exudates during the
wound and hence
the albumin level is
reduced to 2.5 g/dl.
In case of patient
suffering from
diabetes mellitus,
have increased risk
factors to pressure
ulcer (Nigam and
reduced.
Skin integrity is
managed.
Severity of the
pressure ulcer
is reduced
(Carville 2018).
foot ulcer
Impaired
integrity of the
skin.
Risk involved
due to
ineffective
health
maintenance.
been provided
to the patient
which decreases
the risk factor
for pressure
ulcer (Jacobson
et al. 2016).
The healing
process of the
pressure ulcer
and the pressure
reduction is
experienced by
the patient
(Mallah, Nassar
and Badr 2015).
which includes
weight, serum
level of albumin
(Bly et al. 2016).
Assessing the
medical history of
the patient, for
example diabetes
mellitus (Nigam
and Knight 2017).
Assessing the
awareness of the
patient regarding
the pain sensation
(Davies 2018).
Assessing the skin
of the patient over
the bony
prominences
(Carville 2018).
compared with the
other individual due
to increased skin
elasticity, less
moisture and skin
thinning. Apart
from age, protein
depletion is also
responsible for the
pressure sore. In the
case of pressure
sire, a large amount
of protein is
exudates during the
wound and hence
the albumin level is
reduced to 2.5 g/dl.
In case of patient
suffering from
diabetes mellitus,
have increased risk
factors to pressure
ulcer (Nigam and
reduced.
Skin integrity is
managed.
Severity of the
pressure ulcer
is reduced
(Carville 2018).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING DIAGNOSIS ASSIGNMENT
Knight 2017).
Client awareness
regarding the pain
sensation. Client
with reduced
awareness do not
feel the pain stimuli
and do not shift
position possessing
more pressure in the
ulcer increasing its
severity (Davies
2018).
Bony provinces skin
have the highest
risk of infection due
to tissue ischemia
caused by the
compression of an
ulcer against the
hard surface
(Carville 2018).
Knight 2017).
Client awareness
regarding the pain
sensation. Client
with reduced
awareness do not
feel the pain stimuli
and do not shift
position possessing
more pressure in the
ulcer increasing its
severity (Davies
2018).
Bony provinces skin
have the highest
risk of infection due
to tissue ischemia
caused by the
compression of an
ulcer against the
hard surface
(Carville 2018).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING DIAGNOSIS ASSIGNMENT
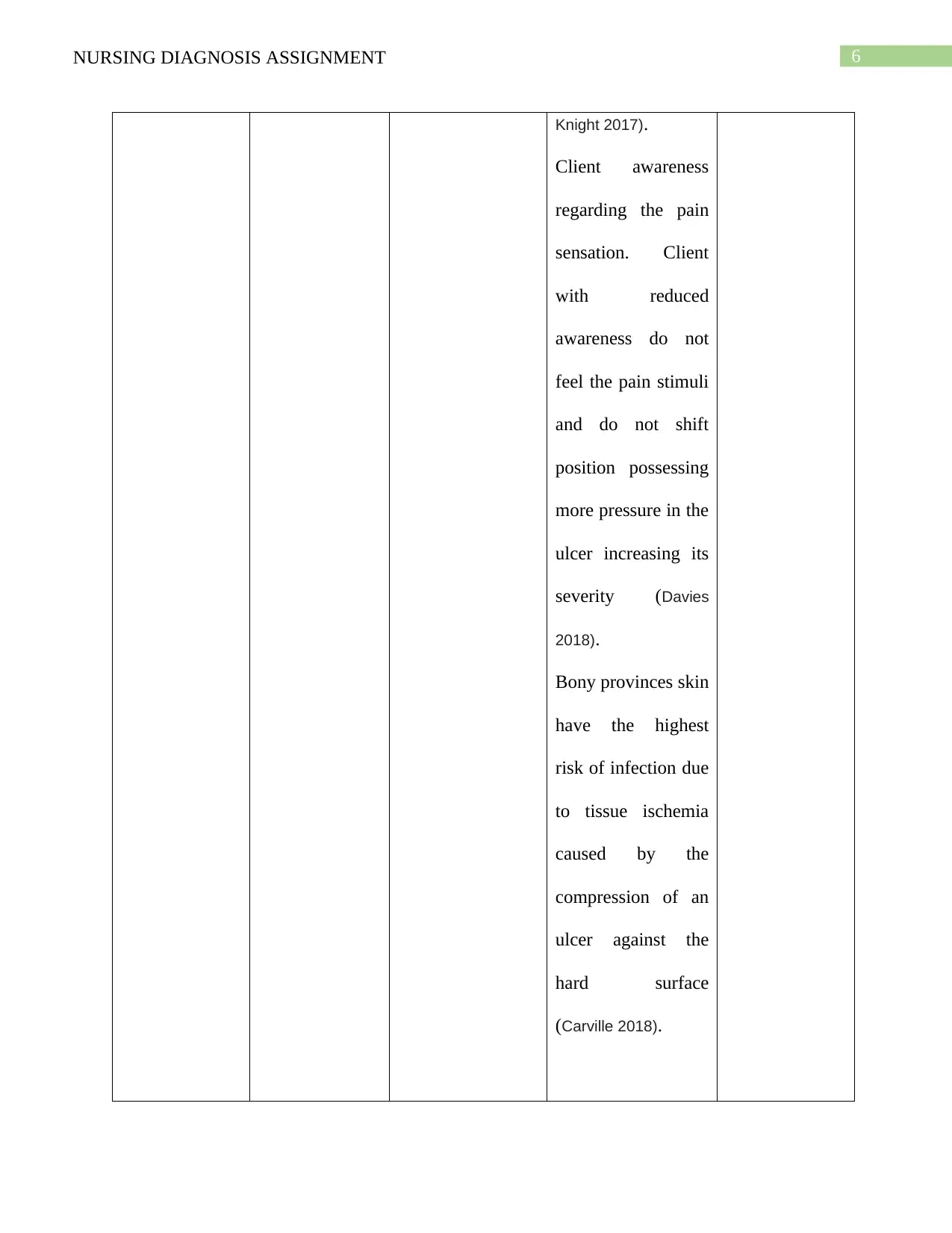
Depression due
to his wife
death and
health issues
Mr Thompson
will state that
he has gained
comfort.
He will take
care of himself
He will start
socializing with
other
individuals in
the hospital
(Gallagher et al.
2016)
The patient is
encouraged to
write a journal
which expresses
his thought and
daily reflection
(Mozley 2017).
Try to minimize
the responsibility
of the patient
(Mozley 2017).
Assist the patient
to identify the
negative thoughts
and develop
strategies to avoid
such thoughts.
Determination of
the previous
cognitive
functioning of the
Writing journal
helps the patient to
overcome from the
distress and grief of
his wife (Mozley
2017).
Minimising the
responsibility of the
patient decreases
the anxiety and
pressure of the
individual.
This intervention
helps the patients to
lead and healthy
and useful life
(Mozley 2017).
It helps the
establishment of the
baseline data that
assist in the
The patient has
gained comfort.
He started
taking care of
his self.
He started
socializing with
others
(Gallagher et al.
2016).
Depression due
to his wife
death and
health issues
Mr Thompson
will state that
he has gained
comfort.
He will take
care of himself
He will start
socializing with
other
individuals in
the hospital
(Gallagher et al.
2016)
The patient is
encouraged to
write a journal
which expresses
his thought and
daily reflection
(Mozley 2017).
Try to minimize
the responsibility
of the patient
(Mozley 2017).
Assist the patient
to identify the
negative thoughts
and develop
strategies to avoid
such thoughts.
Determination of
the previous
cognitive
functioning of the
Writing journal
helps the patient to
overcome from the
distress and grief of
his wife (Mozley
2017).
Minimising the
responsibility of the
patient decreases
the anxiety and
pressure of the
individual.
This intervention
helps the patients to
lead and healthy
and useful life
(Mozley 2017).
It helps the
establishment of the
baseline data that
assist in the
The patient has
gained comfort.
He started
taking care of
his self.
He started
socializing with
others
(Gallagher et al.
2016).
8NURSING DIAGNOSIS ASSIGNMENT
patient.
Assist the patient
to postpone
important decision
of life (Abraha et
al. 2017).
evaluation of the
patient’s progress.
Major important
decision should be
made with optimal
psychophysiological
functioning. Hence
such major decision
should be postponed
during any distress
(Abraha et al. 2017).
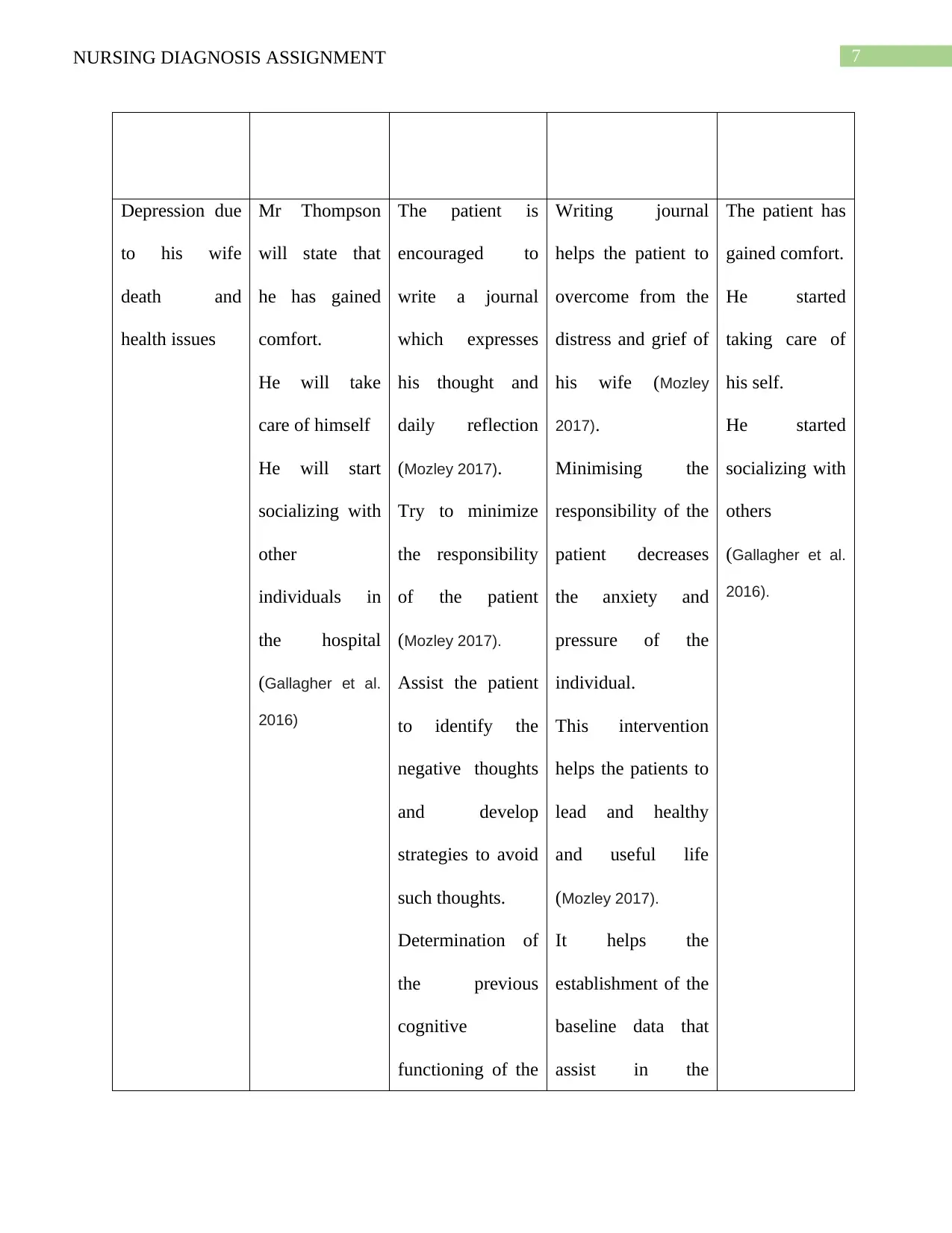
Pain due to
Chest drainage
Short term:
The pain of the
patient has been
decreased from
the before
between 3 to 4
hours as stated
by the patient.
Long term :
After 3 to 4
days of the
Monitor the
breathing sounds
of the patient.
The pain of the
patient is assessed
and rated on the
pain scale.
The pain scale is
used to rate to
evaluate the
location and the
Regular monitoring
of the breathing
sounds of the
patient helps in
determining the
health condition of
the patient.
It helps in
evaluation of the
pain of the patient
(Yeung 2016)
Short term
The patient
stated that pain
has been
reduced.
Long term:
The patient is
able to
participate in
activities which
will help in
patient.
Assist the patient
to postpone
important decision
of life (Abraha et
al. 2017).
evaluation of the
patient’s progress.
Major important
decision should be
made with optimal
psychophysiological
functioning. Hence
such major decision
should be postponed
during any distress
(Abraha et al. 2017).
Pain due to
Chest drainage
Short term:
The pain of the
patient has been
decreased from
the before
between 3 to 4
hours as stated
by the patient.
Long term :
After 3 to 4
days of the
Monitor the
breathing sounds
of the patient.
The pain of the
patient is assessed
and rated on the
pain scale.
The pain scale is
used to rate to
evaluate the
location and the
Regular monitoring
of the breathing
sounds of the
patient helps in
determining the
health condition of
the patient.
It helps in
evaluation of the
pain of the patient
(Yeung 2016)
Short term
The patient
stated that pain
has been
reduced.
Long term:
The patient is
able to
participate in
activities which
will help in
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
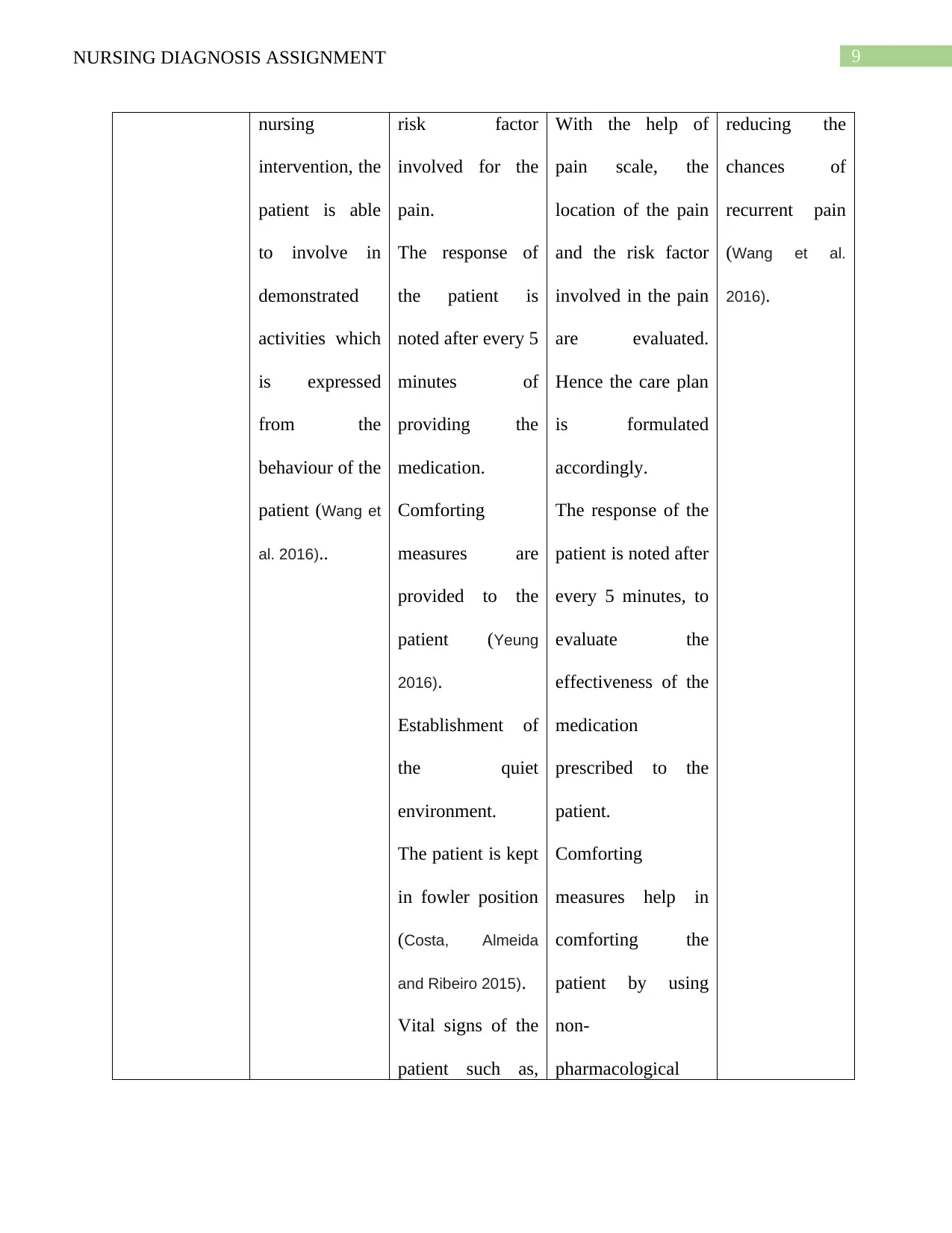
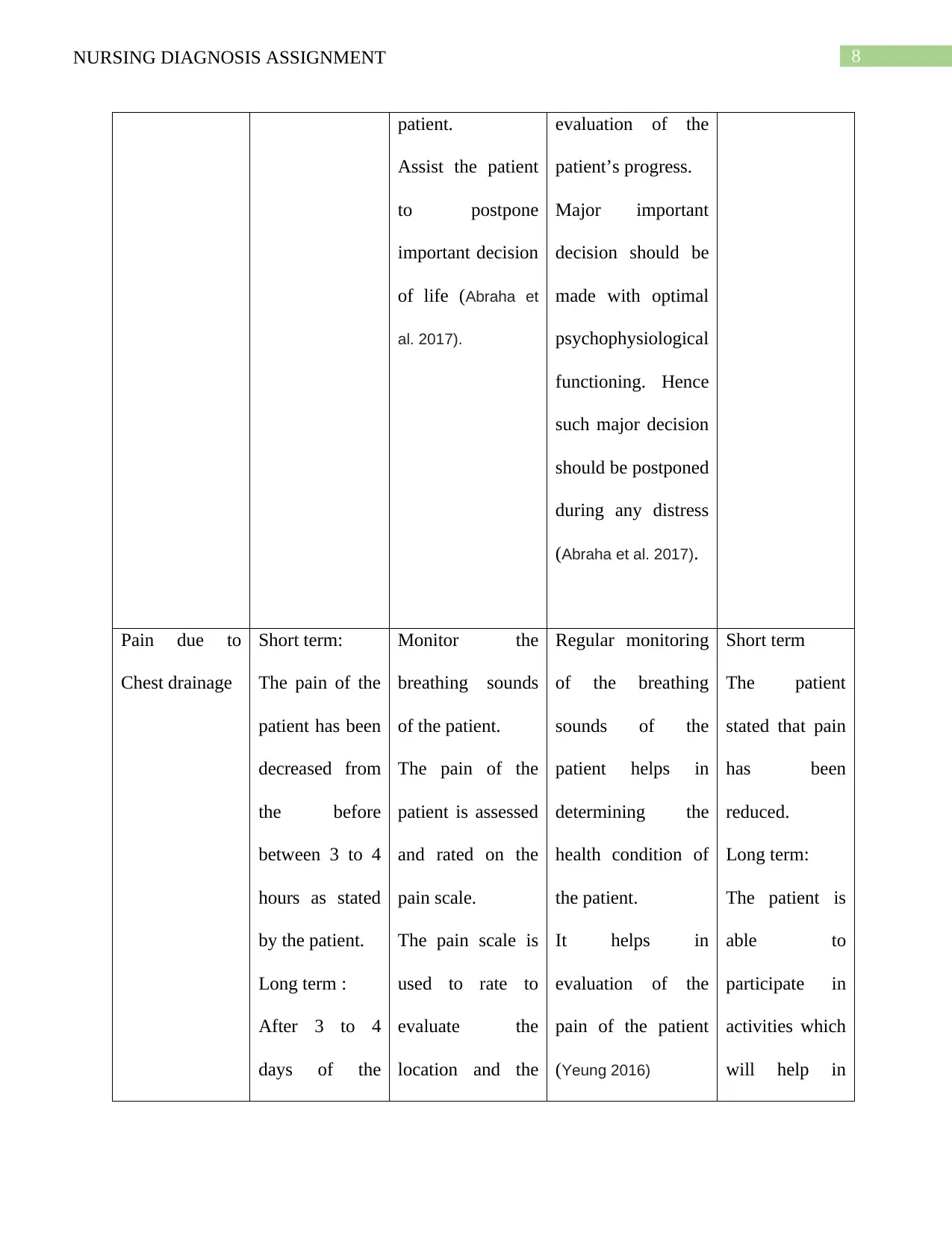
9NURSING DIAGNOSIS ASSIGNMENT
nursing
intervention, the
patient is able
to involve in
demonstrated
activities which
is expressed
from the
behaviour of the
patient (Wang et
al. 2016)..
risk factor
involved for the
pain.
The response of
the patient is
noted after every 5
minutes of
providing the
medication.
Comforting
measures are
provided to the
patient (Yeung
2016).
Establishment of
the quiet
environment.
The patient is kept
in fowler position
(Costa, Almeida
and Ribeiro 2015).
Vital signs of the
patient such as,
With the help of
pain scale, the
location of the pain
and the risk factor
involved in the pain
are evaluated.
Hence the care plan
is formulated
accordingly.
The response of the
patient is noted after
every 5 minutes, to
evaluate the
effectiveness of the
medication
prescribed to the
patient.
Comforting
measures help in
comforting the
patient by using
non-
pharmacological
reducing the
chances of
recurrent pain
(Wang et al.
2016).
nursing
intervention, the
patient is able
to involve in
demonstrated
activities which
is expressed
from the
behaviour of the
patient (Wang et
al. 2016)..
risk factor
involved for the
pain.
The response of
the patient is
noted after every 5
minutes of
providing the
medication.
Comforting
measures are
provided to the
patient (Yeung
2016).
Establishment of
the quiet
environment.
The patient is kept
in fowler position
(Costa, Almeida
and Ribeiro 2015).
Vital signs of the
patient such as,
With the help of
pain scale, the
location of the pain
and the risk factor
involved in the pain
are evaluated.
Hence the care plan
is formulated
accordingly.
The response of the
patient is noted after
every 5 minutes, to
evaluate the
effectiveness of the
medication
prescribed to the
patient.
Comforting
measures help in
comforting the
patient by using
non-
pharmacological
reducing the
chances of
recurrent pain
(Wang et al.
2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING DIAGNOSIS ASSIGNMENT
blood pressure,
pulse rate are
measured.
pain management
strategies.
Quite environment
is provided to the
patient as it helps in
reducing the
demand of energy
on the individual.
Fowler position
helps in chest
expansion which
improves
oxygenation of the
patient (Costa,
Almeida and Ribeiro
2015).
By measuring the
vital signs of the
patient, chances if
further complication
can be measured.
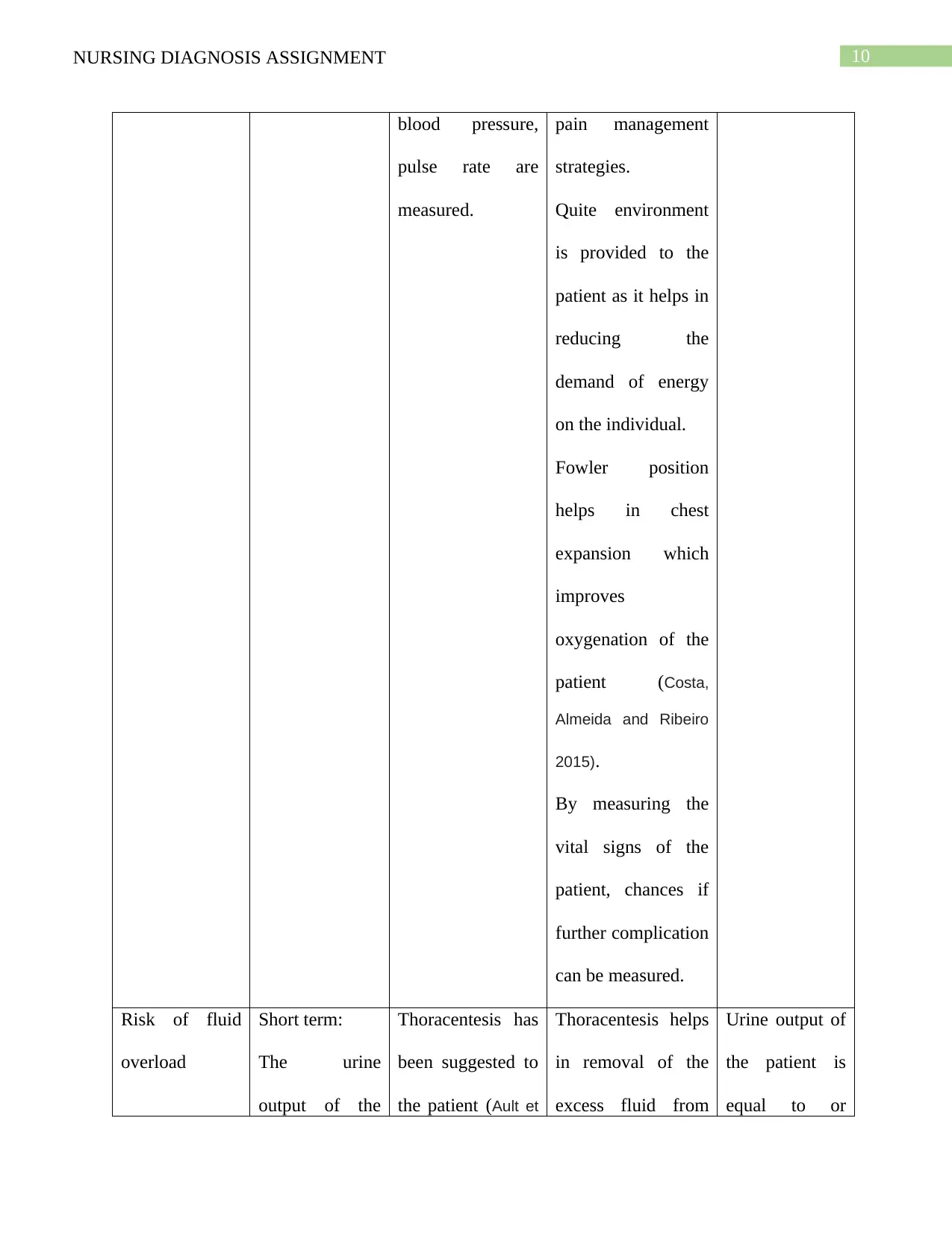
Risk of fluid
overload
Short term:
The urine
output of the
Thoracentesis has
been suggested to
the patient (Ault et
Thoracentesis helps
in removal of the
excess fluid from
Urine output of
the patient is
equal to or
blood pressure,
pulse rate are
measured.
pain management
strategies.
Quite environment
is provided to the
patient as it helps in
reducing the
demand of energy
on the individual.
Fowler position
helps in chest
expansion which
improves
oxygenation of the
patient (Costa,
Almeida and Ribeiro
2015).
By measuring the
vital signs of the
patient, chances if
further complication
can be measured.
Risk of fluid
overload
Short term:
The urine
output of the
Thoracentesis has
been suggested to
the patient (Ault et
Thoracentesis helps
in removal of the
excess fluid from
Urine output of
the patient is
equal to or
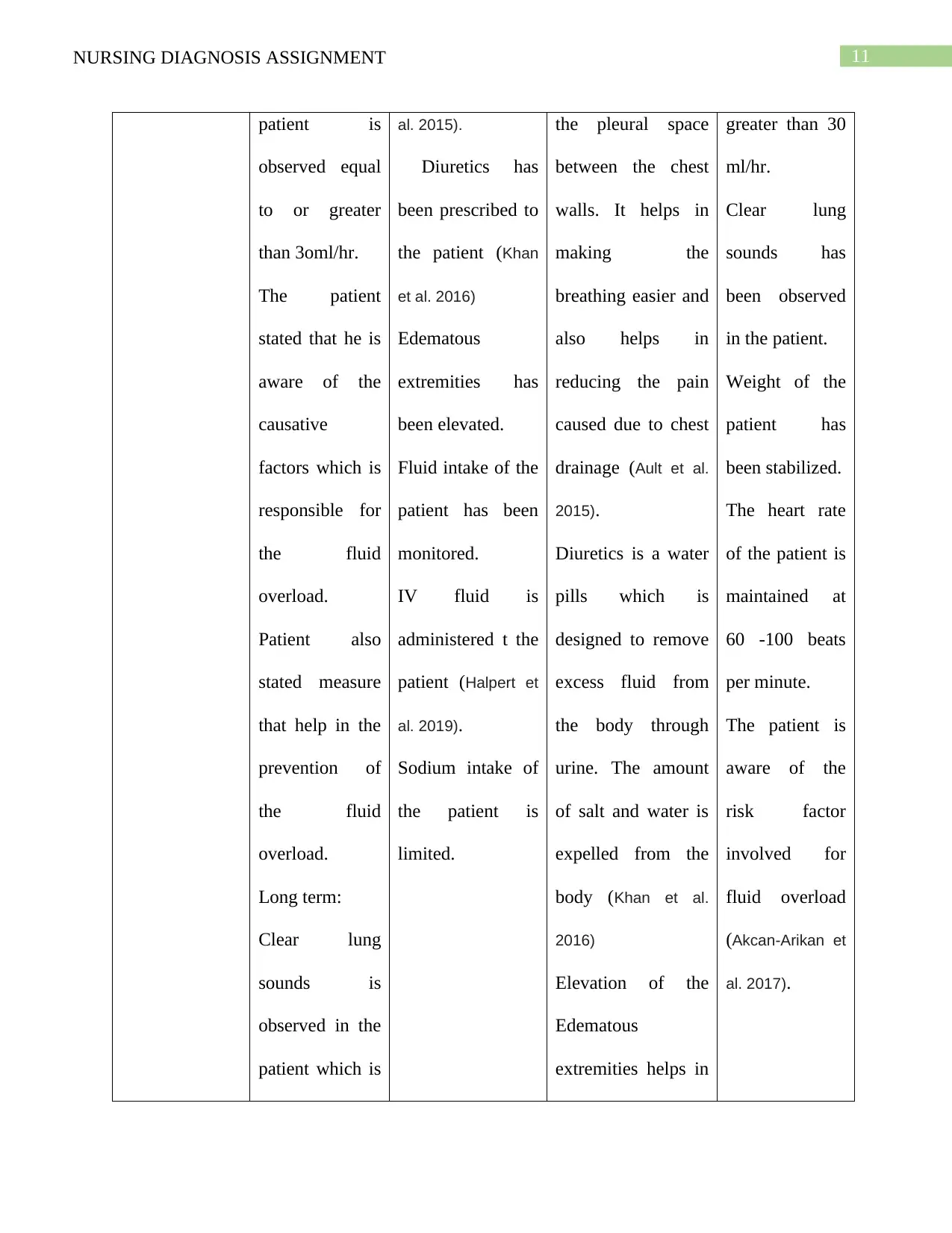
11NURSING DIAGNOSIS ASSIGNMENT
patient is
observed equal
to or greater
than 3oml/hr.
The patient
stated that he is
aware of the
causative
factors which is
responsible for
the fluid
overload.
Patient also
stated measure
that help in the
prevention of
the fluid
overload.
Long term:
Clear lung
sounds is
observed in the
patient which is
al. 2015).
Diuretics has
been prescribed to
the patient (Khan
et al. 2016)
Edematous
extremities has
been elevated.
Fluid intake of the
patient has been
monitored.
IV fluid is
administered t the
patient (Halpert et
al. 2019).
Sodium intake of
the patient is
limited.
the pleural space
between the chest
walls. It helps in
making the
breathing easier and
also helps in
reducing the pain
caused due to chest
drainage (Ault et al.
2015).
Diuretics is a water
pills which is
designed to remove
excess fluid from
the body through
urine. The amount
of salt and water is
expelled from the
body (Khan et al.
2016)
Elevation of the
Edematous
extremities helps in
greater than 30
ml/hr.
Clear lung
sounds has
been observed
in the patient.
Weight of the
patient has
been stabilized.
The heart rate
of the patient is
maintained at
60 -100 beats
per minute.
The patient is
aware of the
risk factor
involved for
fluid overload
(Akcan-Arikan et
al. 2017).
patient is
observed equal
to or greater
than 3oml/hr.
The patient
stated that he is
aware of the
causative
factors which is
responsible for
the fluid
overload.
Patient also
stated measure
that help in the
prevention of
the fluid
overload.
Long term:
Clear lung
sounds is
observed in the
patient which is
al. 2015).
Diuretics has
been prescribed to
the patient (Khan
et al. 2016)
Edematous
extremities has
been elevated.
Fluid intake of the
patient has been
monitored.
IV fluid is
administered t the
patient (Halpert et
al. 2019).
Sodium intake of
the patient is
limited.
the pleural space
between the chest
walls. It helps in
making the
breathing easier and
also helps in
reducing the pain
caused due to chest
drainage (Ault et al.
2015).
Diuretics is a water
pills which is
designed to remove
excess fluid from
the body through
urine. The amount
of salt and water is
expelled from the
body (Khan et al.
2016)
Elevation of the
Edematous
extremities helps in
greater than 30
ml/hr.
Clear lung
sounds has
been observed
in the patient.
Weight of the
patient has
been stabilized.
The heart rate
of the patient is
maintained at
60 -100 beats
per minute.
The patient is
aware of the
risk factor
involved for
fluid overload
(Akcan-Arikan et
al. 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 24
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





