In-depth Case Study: Myocardial Infarction - Diagnosis and Treatment
VerifiedAdded on 2023/06/12
|7
|1931
|147
Case Study
AI Summary
This case study presents a 56-year-old male, Mr. Crawford, with a history of hypertension and obesity, who presented with symptoms indicative of an acute myocardial infarction (MI). The case details his clinical presentation, including prolonged chest pain, shortness of breath, and elevated blood pressure. Diagnostic tests, such as ECG and cardiac enzyme analysis, confirmed an ST-elevation myocardial infarction (STEMI). The pathophysiology explains the underlying mechanisms, including atherosclerotic plaque rupture and thrombus formation. The management involved immediate interventions like heparin, reteplase, morphine, and aspirin, followed by continuous monitoring and thrombolytic therapy. The study further elaborates on the biochemical and morphological changes associated with myocardial ischemia, emphasizing the importance of early antithrombotic and anticoagulant treatment. The discussion covers the role of cardiac biomarkers, electrolyte imbalances, and potential complications such as cardiogenic shock and pulmonary congestion. The case concludes with relevant references, providing a comprehensive overview of the diagnosis, management, and pathophysiology of myocardial infarction. Desklib provides access to similar case studies and study resources for students.

RUNNING HEAD: MYOCARDIAL INFARCTION 1
A CASE STUDY OF MYOCARDIAL INFARCTION
Students Name
Course Title
Institutional affiliation
A CASE STUDY OF MYOCARDIAL INFARCTION
Students Name
Course Title
Institutional affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MYOCARDIAL INFARCTION 2
Student Case Study
Student Name:
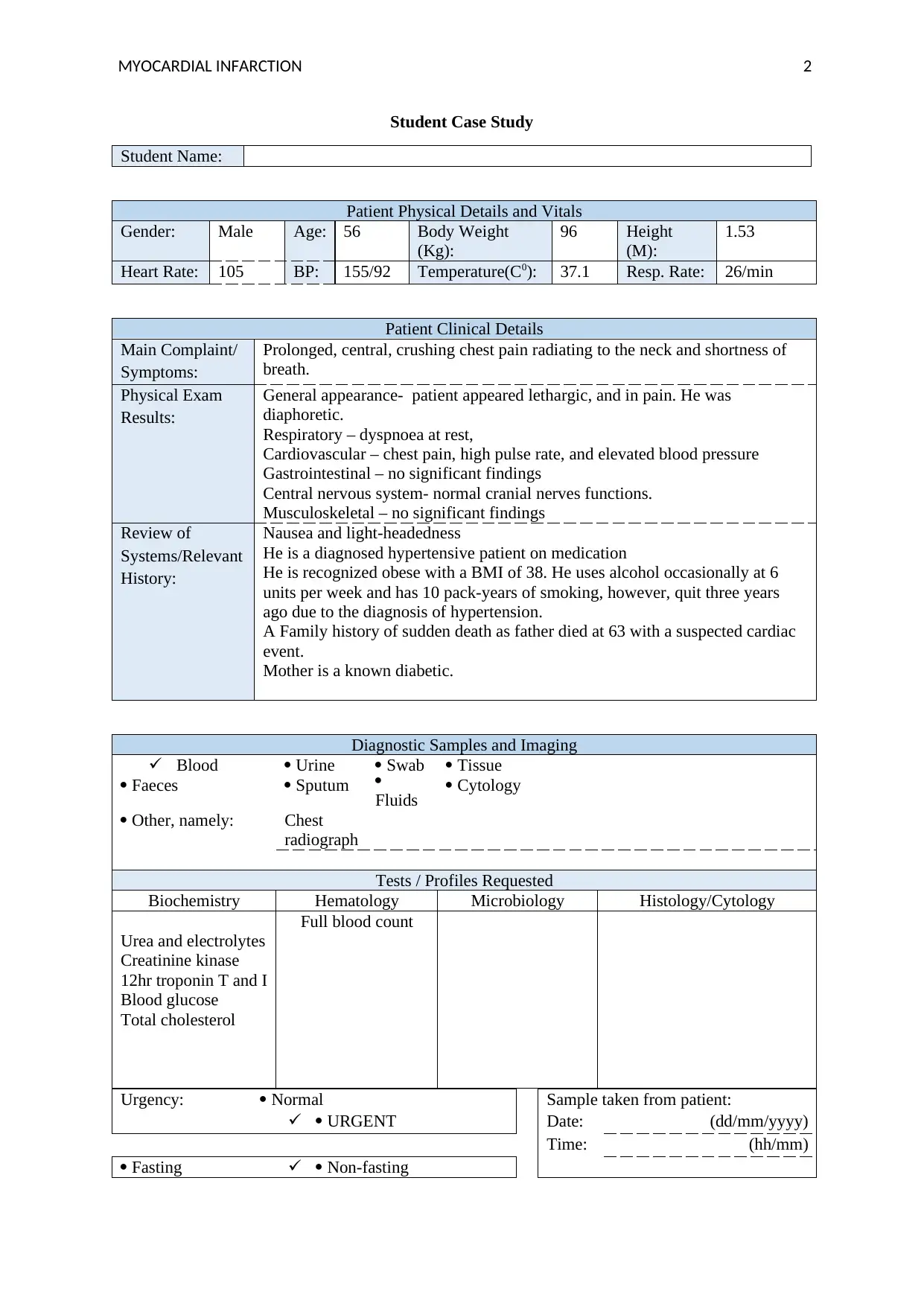
Patient Physical Details and Vitals
Gender: Male Age: 56 Body Weight
(Kg):
96 Height
(M):
1.53
Heart Rate: 105 BP: 155/92 Temperature(C0): 37.1 Resp. Rate: 26/min
Patient Clinical Details
Main Complaint/
Symptoms:
Prolonged, central, crushing chest pain radiating to the neck and shortness of
breath.
Physical Exam
Results:
General appearance- patient appeared lethargic, and in pain. He was
diaphoretic.
Respiratory – dyspnoea at rest,
Cardiovascular – chest pain, high pulse rate, and elevated blood pressure
Gastrointestinal – no significant findings
Central nervous system- normal cranial nerves functions.
Musculoskeletal – no significant findings
Review of
Systems/Relevant
History:
Nausea and light-headedness
He is a diagnosed hypertensive patient on medication
He is recognized obese with a BMI of 38. He uses alcohol occasionally at 6
units per week and has 10 pack-years of smoking, however, quit three years
ago due to the diagnosis of hypertension.
A Family history of sudden death as father died at 63 with a suspected cardiac
event.
Mother is a known diabetic.
Diagnostic Samples and Imaging
Blood
Faeces
Urine
Sputum
Swab
Fluids
Tissue
Cytology
Other, namely: Chest
radiograph
Tests / Profiles Requested
Biochemistry Hematology Microbiology Histology/Cytology
Urea and electrolytes
Creatinine kinase
12hr troponin T and I
Blood glucose
Total cholesterol
Full blood count
Urgency: Normal Sample taken from patient:
URGENT Date: (dd/mm/yyyy)
Time: (hh/mm)
Fasting Non-fasting
Student Case Study
Student Name:
Patient Physical Details and Vitals
Gender: Male Age: 56 Body Weight
(Kg):
96 Height
(M):
1.53
Heart Rate: 105 BP: 155/92 Temperature(C0): 37.1 Resp. Rate: 26/min
Patient Clinical Details
Main Complaint/
Symptoms:
Prolonged, central, crushing chest pain radiating to the neck and shortness of
breath.
Physical Exam
Results:
General appearance- patient appeared lethargic, and in pain. He was
diaphoretic.
Respiratory – dyspnoea at rest,
Cardiovascular – chest pain, high pulse rate, and elevated blood pressure
Gastrointestinal – no significant findings
Central nervous system- normal cranial nerves functions.
Musculoskeletal – no significant findings
Review of
Systems/Relevant
History:
Nausea and light-headedness
He is a diagnosed hypertensive patient on medication
He is recognized obese with a BMI of 38. He uses alcohol occasionally at 6
units per week and has 10 pack-years of smoking, however, quit three years
ago due to the diagnosis of hypertension.
A Family history of sudden death as father died at 63 with a suspected cardiac
event.
Mother is a known diabetic.
Diagnostic Samples and Imaging
Blood
Faeces
Urine
Sputum
Swab
Fluids
Tissue
Cytology
Other, namely: Chest
radiograph
Tests / Profiles Requested
Biochemistry Hematology Microbiology Histology/Cytology
Urea and electrolytes
Creatinine kinase
12hr troponin T and I
Blood glucose
Total cholesterol
Full blood count
Urgency: Normal Sample taken from patient:
URGENT Date: (dd/mm/yyyy)
Time: (hh/mm)
Fasting Non-fasting
MYOCARDIAL INFARCTION 3
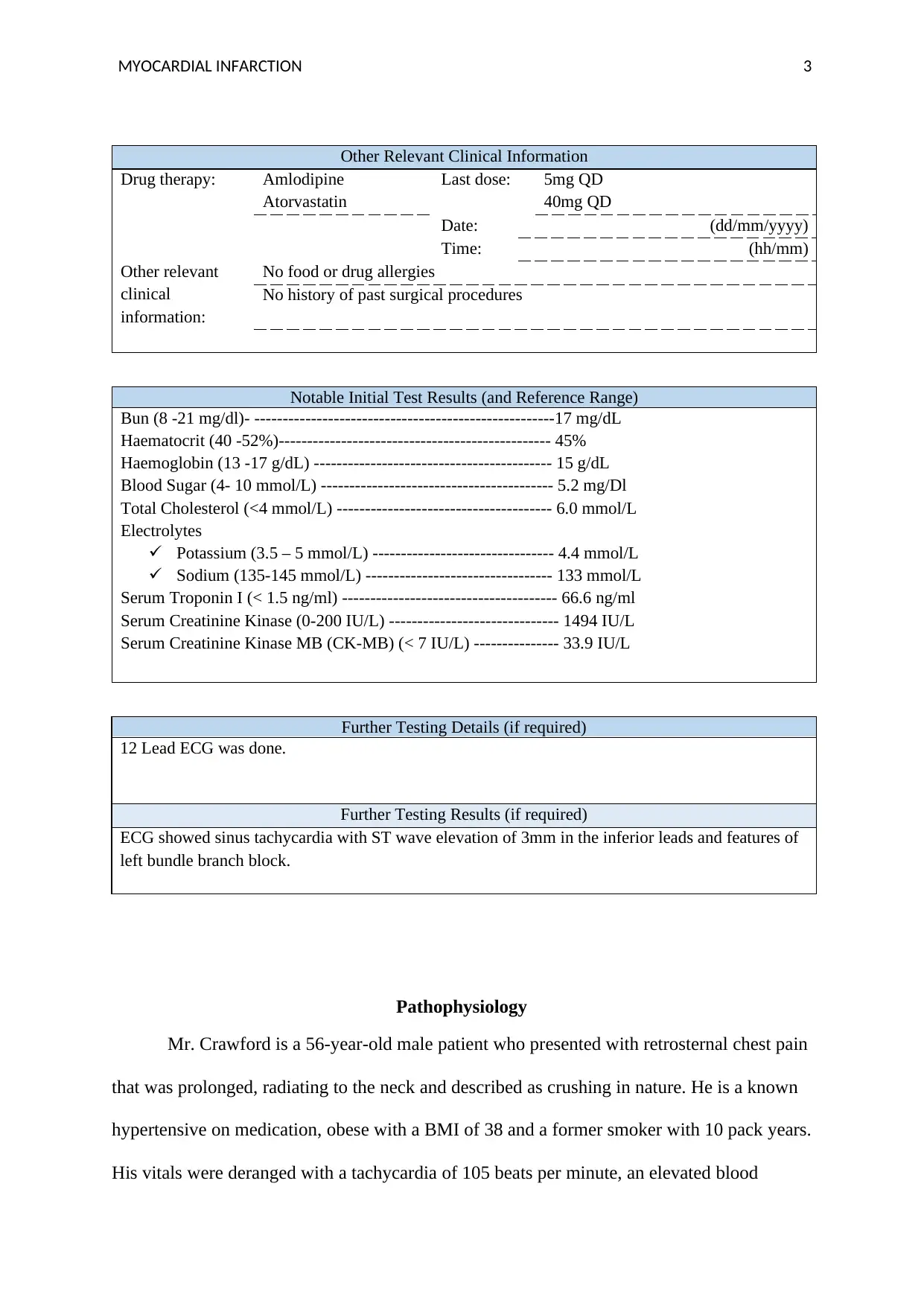
Other Relevant Clinical Information
Drug therapy: Amlodipine
Atorvastatin
Last dose: 5mg QD
40mg QD
Date: (dd/mm/yyyy)
Time: (hh/mm)
Other relevant
clinical
information:
No food or drug allergies
No history of past surgical procedures
Notable Initial Test Results (and Reference Range)
Bun (8 -21 mg/dl)- -----------------------------------------------------17 mg/dL
Haematocrit (40 -52%)------------------------------------------------ 45%
Haemoglobin (13 -17 g/dL) ------------------------------------------ 15 g/dL
Blood Sugar (4- 10 mmol/L) ----------------------------------------- 5.2 mg/Dl
Total Cholesterol (<4 mmol/L) -------------------------------------- 6.0 mmol/L
Electrolytes
Potassium (3.5 – 5 mmol/L) -------------------------------- 4.4 mmol/L
Sodium (135-145 mmol/L) --------------------------------- 133 mmol/L
Serum Troponin I (< 1.5 ng/ml) -------------------------------------- 66.6 ng/ml
Serum Creatinine Kinase (0-200 IU/L) ------------------------------ 1494 IU/L
Serum Creatinine Kinase MB (CK-MB) (< 7 IU/L) --------------- 33.9 IU/L
Further Testing Details (if required)
12 Lead ECG was done.
Further Testing Results (if required)
ECG showed sinus tachycardia with ST wave elevation of 3mm in the inferior leads and features of
left bundle branch block.
Pathophysiology
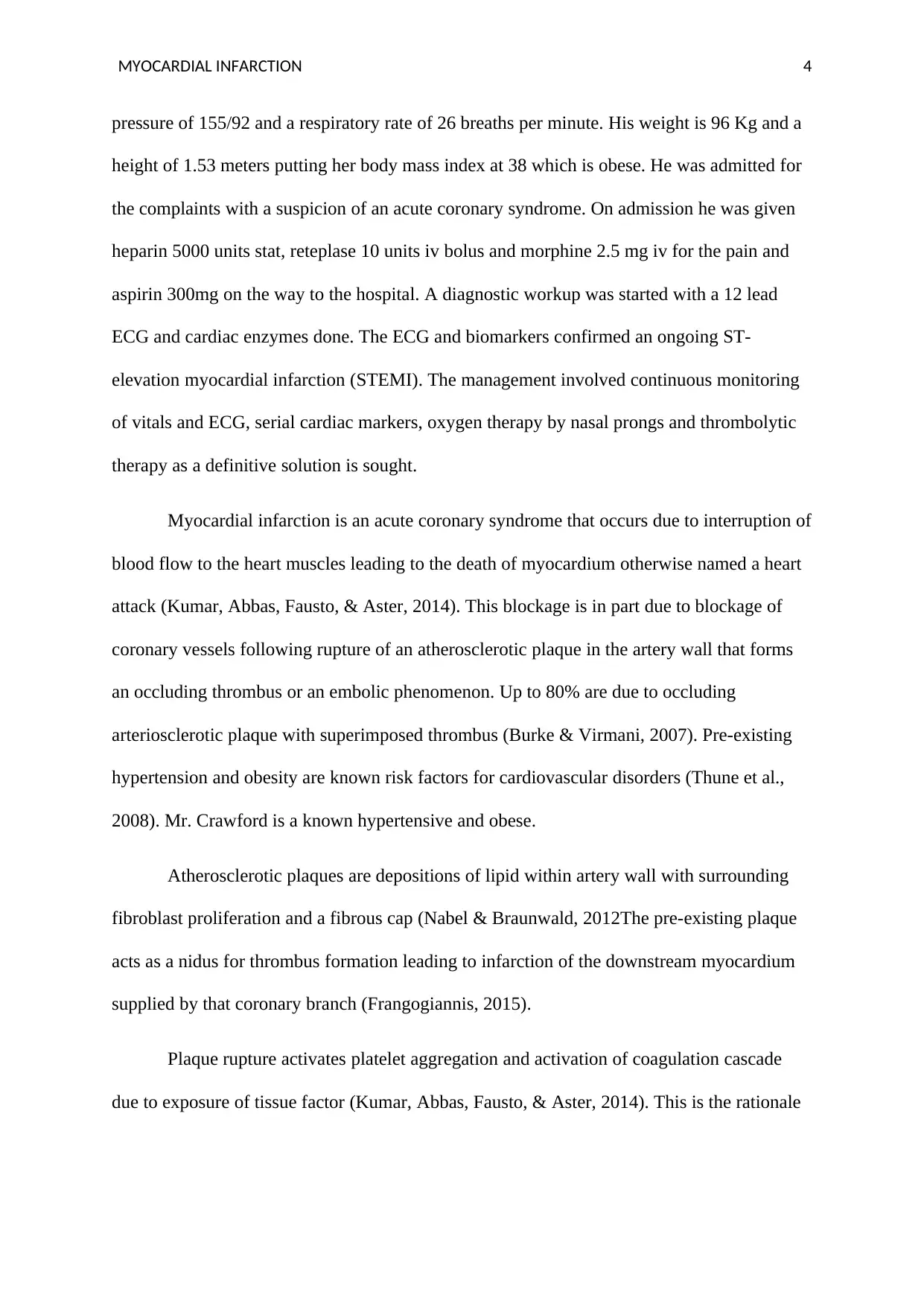
Mr. Crawford is a 56-year-old male patient who presented with retrosternal chest pain
that was prolonged, radiating to the neck and described as crushing in nature. He is a known
hypertensive on medication, obese with a BMI of 38 and a former smoker with 10 pack years.
His vitals were deranged with a tachycardia of 105 beats per minute, an elevated blood
Other Relevant Clinical Information
Drug therapy: Amlodipine
Atorvastatin
Last dose: 5mg QD
40mg QD
Date: (dd/mm/yyyy)
Time: (hh/mm)
Other relevant
clinical
information:
No food or drug allergies
No history of past surgical procedures
Notable Initial Test Results (and Reference Range)
Bun (8 -21 mg/dl)- -----------------------------------------------------17 mg/dL
Haematocrit (40 -52%)------------------------------------------------ 45%
Haemoglobin (13 -17 g/dL) ------------------------------------------ 15 g/dL
Blood Sugar (4- 10 mmol/L) ----------------------------------------- 5.2 mg/Dl
Total Cholesterol (<4 mmol/L) -------------------------------------- 6.0 mmol/L
Electrolytes
Potassium (3.5 – 5 mmol/L) -------------------------------- 4.4 mmol/L
Sodium (135-145 mmol/L) --------------------------------- 133 mmol/L
Serum Troponin I (< 1.5 ng/ml) -------------------------------------- 66.6 ng/ml
Serum Creatinine Kinase (0-200 IU/L) ------------------------------ 1494 IU/L
Serum Creatinine Kinase MB (CK-MB) (< 7 IU/L) --------------- 33.9 IU/L
Further Testing Details (if required)
12 Lead ECG was done.
Further Testing Results (if required)
ECG showed sinus tachycardia with ST wave elevation of 3mm in the inferior leads and features of
left bundle branch block.
Pathophysiology
Mr. Crawford is a 56-year-old male patient who presented with retrosternal chest pain
that was prolonged, radiating to the neck and described as crushing in nature. He is a known
hypertensive on medication, obese with a BMI of 38 and a former smoker with 10 pack years.
His vitals were deranged with a tachycardia of 105 beats per minute, an elevated blood
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MYOCARDIAL INFARCTION 4
pressure of 155/92 and a respiratory rate of 26 breaths per minute. His weight is 96 Kg and a
height of 1.53 meters putting her body mass index at 38 which is obese. He was admitted for
the complaints with a suspicion of an acute coronary syndrome. On admission he was given
heparin 5000 units stat, reteplase 10 units iv bolus and morphine 2.5 mg iv for the pain and
aspirin 300mg on the way to the hospital. A diagnostic workup was started with a 12 lead
ECG and cardiac enzymes done. The ECG and biomarkers confirmed an ongoing ST-
elevation myocardial infarction (STEMI). The management involved continuous monitoring
of vitals and ECG, serial cardiac markers, oxygen therapy by nasal prongs and thrombolytic
therapy as a definitive solution is sought.
Myocardial infarction is an acute coronary syndrome that occurs due to interruption of
blood flow to the heart muscles leading to the death of myocardium otherwise named a heart
attack (Kumar, Abbas, Fausto, & Aster, 2014). This blockage is in part due to blockage of
coronary vessels following rupture of an atherosclerotic plaque in the artery wall that forms
an occluding thrombus or an embolic phenomenon. Up to 80% are due to occluding
arteriosclerotic plaque with superimposed thrombus (Burke & Virmani, 2007). Pre-existing
hypertension and obesity are known risk factors for cardiovascular disorders (Thune et al.,
2008). Mr. Crawford is a known hypertensive and obese.
Atherosclerotic plaques are depositions of lipid within artery wall with surrounding
fibroblast proliferation and a fibrous cap (Nabel & Braunwald, 2012The pre-existing plaque
acts as a nidus for thrombus formation leading to infarction of the downstream myocardium
supplied by that coronary branch (Frangogiannis, 2015).
Plaque rupture activates platelet aggregation and activation of coagulation cascade
due to exposure of tissue factor (Kumar, Abbas, Fausto, & Aster, 2014). This is the rationale
pressure of 155/92 and a respiratory rate of 26 breaths per minute. His weight is 96 Kg and a
height of 1.53 meters putting her body mass index at 38 which is obese. He was admitted for
the complaints with a suspicion of an acute coronary syndrome. On admission he was given
heparin 5000 units stat, reteplase 10 units iv bolus and morphine 2.5 mg iv for the pain and
aspirin 300mg on the way to the hospital. A diagnostic workup was started with a 12 lead
ECG and cardiac enzymes done. The ECG and biomarkers confirmed an ongoing ST-
elevation myocardial infarction (STEMI). The management involved continuous monitoring
of vitals and ECG, serial cardiac markers, oxygen therapy by nasal prongs and thrombolytic
therapy as a definitive solution is sought.
Myocardial infarction is an acute coronary syndrome that occurs due to interruption of
blood flow to the heart muscles leading to the death of myocardium otherwise named a heart
attack (Kumar, Abbas, Fausto, & Aster, 2014). This blockage is in part due to blockage of
coronary vessels following rupture of an atherosclerotic plaque in the artery wall that forms
an occluding thrombus or an embolic phenomenon. Up to 80% are due to occluding
arteriosclerotic plaque with superimposed thrombus (Burke & Virmani, 2007). Pre-existing
hypertension and obesity are known risk factors for cardiovascular disorders (Thune et al.,
2008). Mr. Crawford is a known hypertensive and obese.
Atherosclerotic plaques are depositions of lipid within artery wall with surrounding
fibroblast proliferation and a fibrous cap (Nabel & Braunwald, 2012The pre-existing plaque
acts as a nidus for thrombus formation leading to infarction of the downstream myocardium
supplied by that coronary branch (Frangogiannis, 2015).
Plaque rupture activates platelet aggregation and activation of coagulation cascade
due to exposure of tissue factor (Kumar, Abbas, Fausto, & Aster, 2014). This is the rationale
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MYOCARDIAL INFARCTION 5
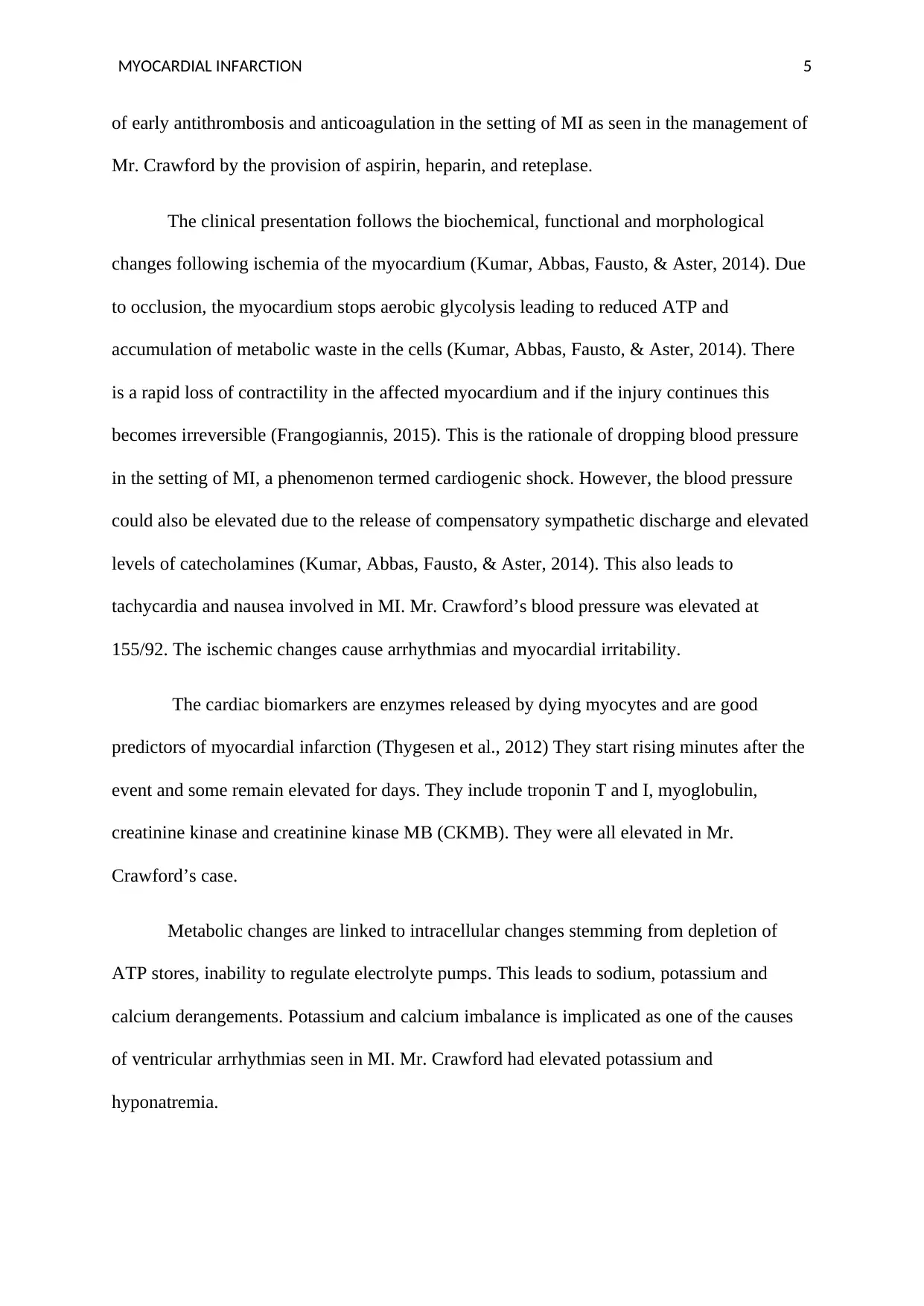
of early antithrombosis and anticoagulation in the setting of MI as seen in the management of
Mr. Crawford by the provision of aspirin, heparin, and reteplase.
The clinical presentation follows the biochemical, functional and morphological
changes following ischemia of the myocardium (Kumar, Abbas, Fausto, & Aster, 2014). Due
to occlusion, the myocardium stops aerobic glycolysis leading to reduced ATP and
accumulation of metabolic waste in the cells (Kumar, Abbas, Fausto, & Aster, 2014). There
is a rapid loss of contractility in the affected myocardium and if the injury continues this
becomes irreversible (Frangogiannis, 2015). This is the rationale of dropping blood pressure
in the setting of MI, a phenomenon termed cardiogenic shock. However, the blood pressure
could also be elevated due to the release of compensatory sympathetic discharge and elevated
levels of catecholamines (Kumar, Abbas, Fausto, & Aster, 2014). This also leads to
tachycardia and nausea involved in MI. Mr. Crawford’s blood pressure was elevated at
155/92. The ischemic changes cause arrhythmias and myocardial irritability.
The cardiac biomarkers are enzymes released by dying myocytes and are good
predictors of myocardial infarction (Thygesen et al., 2012) They start rising minutes after the
event and some remain elevated for days. They include troponin T and I, myoglobulin,
creatinine kinase and creatinine kinase MB (CKMB). They were all elevated in Mr.
Crawford’s case.
Metabolic changes are linked to intracellular changes stemming from depletion of
ATP stores, inability to regulate electrolyte pumps. This leads to sodium, potassium and
calcium derangements. Potassium and calcium imbalance is implicated as one of the causes
of ventricular arrhythmias seen in MI. Mr. Crawford had elevated potassium and
hyponatremia.
of early antithrombosis and anticoagulation in the setting of MI as seen in the management of
Mr. Crawford by the provision of aspirin, heparin, and reteplase.
The clinical presentation follows the biochemical, functional and morphological
changes following ischemia of the myocardium (Kumar, Abbas, Fausto, & Aster, 2014). Due
to occlusion, the myocardium stops aerobic glycolysis leading to reduced ATP and
accumulation of metabolic waste in the cells (Kumar, Abbas, Fausto, & Aster, 2014). There
is a rapid loss of contractility in the affected myocardium and if the injury continues this
becomes irreversible (Frangogiannis, 2015). This is the rationale of dropping blood pressure
in the setting of MI, a phenomenon termed cardiogenic shock. However, the blood pressure
could also be elevated due to the release of compensatory sympathetic discharge and elevated
levels of catecholamines (Kumar, Abbas, Fausto, & Aster, 2014). This also leads to
tachycardia and nausea involved in MI. Mr. Crawford’s blood pressure was elevated at
155/92. The ischemic changes cause arrhythmias and myocardial irritability.
The cardiac biomarkers are enzymes released by dying myocytes and are good
predictors of myocardial infarction (Thygesen et al., 2012) They start rising minutes after the
event and some remain elevated for days. They include troponin T and I, myoglobulin,
creatinine kinase and creatinine kinase MB (CKMB). They were all elevated in Mr.
Crawford’s case.
Metabolic changes are linked to intracellular changes stemming from depletion of
ATP stores, inability to regulate electrolyte pumps. This leads to sodium, potassium and
calcium derangements. Potassium and calcium imbalance is implicated as one of the causes
of ventricular arrhythmias seen in MI. Mr. Crawford had elevated potassium and
hyponatremia.
MYOCARDIAL INFARCTION 6
The etiology of chest pain in myocardium ischemia is poorly understood but has been
hypothesized to be due to the release of chemical mediators triggered by ischemic changes
within the myocardium cells (Leach & Fisher, 2013). Circulatory derangements are however
due to ventricular dysfunction caused by loss of myocardium (Walker & Colledge, 2013).
Infarction of myocardium heals by scar formation leading to permanent loss of contractility
in that area. If the dysfunction is systolic, cardiac output drops leading to a fall in blood
pressure and coronary perfusion (Walker & Colledge, 2013). This has the disadvantage of
potentiating the ischemia. A diastolic dysfunction will lead to increased left ventricular
diastolic pressure that causes back pressure to the lungs that manifest as pulmonary
congestion (Walker & Colledge, 2013). This leads to hypoxemia and difficulty breathing,
impaired oxygen transport and further ischemia. A chest radiograph was requested for Mr.
Crawford to access pulmonary congestion and also the cardiac profile.
The etiology of chest pain in myocardium ischemia is poorly understood but has been
hypothesized to be due to the release of chemical mediators triggered by ischemic changes
within the myocardium cells (Leach & Fisher, 2013). Circulatory derangements are however
due to ventricular dysfunction caused by loss of myocardium (Walker & Colledge, 2013).
Infarction of myocardium heals by scar formation leading to permanent loss of contractility
in that area. If the dysfunction is systolic, cardiac output drops leading to a fall in blood
pressure and coronary perfusion (Walker & Colledge, 2013). This has the disadvantage of
potentiating the ischemia. A diastolic dysfunction will lead to increased left ventricular
diastolic pressure that causes back pressure to the lungs that manifest as pulmonary
congestion (Walker & Colledge, 2013). This leads to hypoxemia and difficulty breathing,
impaired oxygen transport and further ischemia. A chest radiograph was requested for Mr.
Crawford to access pulmonary congestion and also the cardiac profile.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MYOCARDIAL INFARCTION 7
References
Burke, A. P., & Virmani, R. (2007). Pathophysiology of Acute Myocardial Infarction.
Medical Clinics of North America, 91(4), 553-572.
doi:https://doi.org/10.1016/j.mcna.2007.03.005
Frangogiannis, N. G. (2015). Pathophysiology of Myocardial Infarction. Compr Physiol,
5(4), 1841-1875.
Kumar, V., Abbas, A. K., Fausto, N., & Aster, J. C. (2014). Robbins and Cotran pathologic
basis of disease, professional edition. London: Elsevier health sciences.
Leach, A., & Fisher, M. (2013). Myocardial ischaemia and cardiac pain – a mysterious
relationship. British Journal of Pain, 7(1), 23–30.
http://doi.org/10.1177/2049463712474648
Nabel, E. G., & Braunwald, E. (2012). A tale of coronary artery disease and myocardial
infarction. New England Journal of Medicine, 366(1), 54-63.
Thune, J. J., Signorovitch, J., Kober, L., Velazquez, E. J., McMurray, J. J., Califf, R. M., ... &
Pfeffer, M. A. (2008). Effect of antecedent hypertension and follow-up blood pressure
on outcomes after high-risk myocardial infarction. Hypertension, 51(1), 48-54.
Thygesen, K., Alpert, J. S., Jaffe, A. S., Simoons, M. L., Chaitman, B. R., White, H. D., ... &
White, H. D. (2012). Third universal definition of myocardial infarction. European
heart journal, 33(20), 2551-2567.
Walker, B. R., & Colledge, N. R. (2013). Davidson's Principles and Practice of Medicine E-
Book. Elsevier Health Sciences.
References
Burke, A. P., & Virmani, R. (2007). Pathophysiology of Acute Myocardial Infarction.
Medical Clinics of North America, 91(4), 553-572.
doi:https://doi.org/10.1016/j.mcna.2007.03.005
Frangogiannis, N. G. (2015). Pathophysiology of Myocardial Infarction. Compr Physiol,
5(4), 1841-1875.
Kumar, V., Abbas, A. K., Fausto, N., & Aster, J. C. (2014). Robbins and Cotran pathologic
basis of disease, professional edition. London: Elsevier health sciences.
Leach, A., & Fisher, M. (2013). Myocardial ischaemia and cardiac pain – a mysterious
relationship. British Journal of Pain, 7(1), 23–30.
http://doi.org/10.1177/2049463712474648
Nabel, E. G., & Braunwald, E. (2012). A tale of coronary artery disease and myocardial
infarction. New England Journal of Medicine, 366(1), 54-63.
Thune, J. J., Signorovitch, J., Kober, L., Velazquez, E. J., McMurray, J. J., Califf, R. M., ... &
Pfeffer, M. A. (2008). Effect of antecedent hypertension and follow-up blood pressure
on outcomes after high-risk myocardial infarction. Hypertension, 51(1), 48-54.
Thygesen, K., Alpert, J. S., Jaffe, A. S., Simoons, M. L., Chaitman, B. R., White, H. D., ... &
White, H. D. (2012). Third universal definition of myocardial infarction. European
heart journal, 33(20), 2551-2567.
Walker, B. R., & Colledge, N. R. (2013). Davidson's Principles and Practice of Medicine E-
Book. Elsevier Health Sciences.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




