Comparing National Health Workforce Plans: Australia and Japan
VerifiedAdded on 2023/06/10
|17
|3917
|312
Report
AI Summary
This report provides a comparative analysis of the health workforce plans of Australia and Japan, examining their approaches to meet current and future healthcare needs. The report begins with an executive summary and table of contents, followed by an introduction highlighting the importance of health workforce planning. It then presents environmental scans of both Australia and Japan, detailing their healthcare systems, populations, and economic contexts. Data profiles are compared, including workforce statistics on doctors, nurses, and other medical practitioners, and critical issues such as aging workforce, gender imbalances and inadequate domestic practitioners are discussed. The report evaluates each country's plans in relation to WHO health workforce priorities, concluding that Japan's plan is effective due to its ability to produce skilled practitioners. The report suggests that Australia needs to implement WHO recommendations to ensure an accessible and skilled workforce. The report uses WHO reports, government websites and scholarly literature. The report concludes that the Japanese health workforce plan effective because of its ability to produce adequate skilled practitioners that meet the country demand for health care services. Australia will require implementing all WHO recommendations on health workforce to foster adequate, accessible, and highly skilled health workforce that is responsive to meet expected health needs of Australians.
UNIT:
NAME:
DATE:
NAME:
DATE:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Executive Summary
Lack of an appropriate health workforce plan can threaten a health system ability to deliver
health care to it population. Health human resource plan provide strategic framework for the
future by ensuring a health system prepares medical practitioners to meet expected population
health demands (Rees, Crampton, Gauld, & MacDonell, 2018). The following report analyses
Australian and Japanese health workforce plans to find out if they have prioritized WHO health
workforce priorities. The report uses WHO reports, available information from government
websites and scholarly literature. The report found out that the countries haven’t fully
implemented WHO health workforce priorities. The report also found that the Japanese health
workforce is well organized and delivers quality, accessible and affordable health care even
without the need of implementing the WHO health workforce recommendations. The reports
therefore concludes that the Japanese health workforce plan effective because of its ability to
produce adequate skilled practitioners that meet the country demand for health care services.
Australia will require implementing all WHO recommendations on health workforce to foster
adequate, accessible, and highly skilled health workforce that is responsive to meet expected
health needs of Australians.
Lack of an appropriate health workforce plan can threaten a health system ability to deliver
health care to it population. Health human resource plan provide strategic framework for the
future by ensuring a health system prepares medical practitioners to meet expected population
health demands (Rees, Crampton, Gauld, & MacDonell, 2018). The following report analyses
Australian and Japanese health workforce plans to find out if they have prioritized WHO health
workforce priorities. The report uses WHO reports, available information from government
websites and scholarly literature. The report found out that the countries haven’t fully
implemented WHO health workforce priorities. The report also found that the Japanese health
workforce is well organized and delivers quality, accessible and affordable health care even
without the need of implementing the WHO health workforce recommendations. The reports
therefore concludes that the Japanese health workforce plan effective because of its ability to
produce adequate skilled practitioners that meet the country demand for health care services.
Australia will require implementing all WHO recommendations on health workforce to foster
adequate, accessible, and highly skilled health workforce that is responsive to meet expected
health needs of Australians.
Table of Contents
Introduction.................................................................................................................................................4
Environmental Scan.....................................................................................................................................5
Australia..................................................................................................................................................5
Japan.......................................................................................................................................................6
Data Profile..................................................................................................................................................7
Summary Data Profile Table 2015...........................................................................................................7
Current Supply.........................................................................................................................................8
Age and Gender.....................................................................................................................................10
Critical Issues.............................................................................................................................................11
Australia................................................................................................................................................11
Japan.....................................................................................................................................................12
Evaluation of Australia and Japan..............................................................................................................13
Conclusion.................................................................................................................................................15
References.................................................................................................................................................16
Introduction.................................................................................................................................................4
Environmental Scan.....................................................................................................................................5
Australia..................................................................................................................................................5
Japan.......................................................................................................................................................6
Data Profile..................................................................................................................................................7
Summary Data Profile Table 2015...........................................................................................................7
Current Supply.........................................................................................................................................8
Age and Gender.....................................................................................................................................10
Critical Issues.............................................................................................................................................11
Australia................................................................................................................................................11
Japan.....................................................................................................................................................12
Evaluation of Australia and Japan..............................................................................................................13
Conclusion.................................................................................................................................................15
References.................................................................................................................................................16
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

National Health Workforce Plan
Comparison Australia Vs Japan
Introduction
A health workforce plan is an important aspect to meeting a country’s current and future health
care needs. Human resource is an integral part of any health system and requires appropriate
planning from several stakeholders to optimally deliver quality and accessible health care
(Crettenden et al., 2014). World Health Organization (WHO) defines health workforce as all
individual whose work is for protecting and improving health of the communities. They include
practitioners in clinical and non clinical field who administer public and individual health
interventions. An effective national health workforce plan aim to ensuring all citizens in all
locations have access of skilled health practitioner, who is well equipped, supported and
motivated (Craveiro et al., 2018). A national health plan targets to achieve national health goals,
obligations, and commitment of its citizens. According to WHO, a health workforce plan has to
be comprehensive and address health workforce finances, policies of practice, partnership for
optimal health care, leadership in health sector, and health resource management systems. Lack
of an explicit health human resource planning threatens a country’s healthcare systems capacity
to attain its objectives. A national health workforce plan should therefore focus on developing a
healthcare system that is responsive to a population needs and expectations. The following report
compares Australian and Japan national health workforce plan. Japan healthcare is good a
comparison to Australian healthcare because of a developed country similar to Australia and has
the highest outcome in terms of life expectancy in the whole world. This will show the difference
in health workforce planning or planning process that causes the difference. This will involve
environmental scanning, preparation of workforce profiles and discussion of critical issues to
addressed in the countries health workforce plan. The report will also evaluate each country’s
national workforce plans to find out if they are addressing WHO priorities in health workforce.
Environmental Scan
This section analyses the Australian and Singaporean health workforce using national and
international health workforce plans and included polices and plans for health workforce. This
Comparison Australia Vs Japan
Introduction
A health workforce plan is an important aspect to meeting a country’s current and future health
care needs. Human resource is an integral part of any health system and requires appropriate
planning from several stakeholders to optimally deliver quality and accessible health care
(Crettenden et al., 2014). World Health Organization (WHO) defines health workforce as all
individual whose work is for protecting and improving health of the communities. They include
practitioners in clinical and non clinical field who administer public and individual health
interventions. An effective national health workforce plan aim to ensuring all citizens in all
locations have access of skilled health practitioner, who is well equipped, supported and
motivated (Craveiro et al., 2018). A national health plan targets to achieve national health goals,
obligations, and commitment of its citizens. According to WHO, a health workforce plan has to
be comprehensive and address health workforce finances, policies of practice, partnership for
optimal health care, leadership in health sector, and health resource management systems. Lack
of an explicit health human resource planning threatens a country’s healthcare systems capacity
to attain its objectives. A national health workforce plan should therefore focus on developing a
healthcare system that is responsive to a population needs and expectations. The following report
compares Australian and Japan national health workforce plan. Japan healthcare is good a
comparison to Australian healthcare because of a developed country similar to Australia and has
the highest outcome in terms of life expectancy in the whole world. This will show the difference
in health workforce planning or planning process that causes the difference. This will involve
environmental scanning, preparation of workforce profiles and discussion of critical issues to
addressed in the countries health workforce plan. The report will also evaluate each country’s
national workforce plans to find out if they are addressing WHO priorities in health workforce.
Environmental Scan
This section analyses the Australian and Singaporean health workforce using national and
international health workforce plans and included polices and plans for health workforce. This
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
will enable understanding of the factors shaping each country’s health workforce plan and
planning processes.
Australia
Australia has a population of 24.13 million people. The country has a GDP of more than USD
1.205 trillion and USD 49927.82 per capita income. The Australian government bears health care
cost through Medicare Scheme. The Medicare Scheme help low and poor incomer citizens pay
medical bills (McGrail, & Humphreys, 2015). The country has 102802 medical practitioners
distributed in different capacities in the country’s health system. The Australian health workforce
recorded a growth rate of 1.6% from year 2012 to 2015. Medical practitioners work an average
of 42 hours per week with a female to male ratio of 2:5. The country old workforce above 55
years is 1 in every 4 practitioners. Australia also recorded 3210 student commencement of
medical undergraduate studies in 2015.
The Australian health workforce is planned and managed by the government through The
Department of Health. The Department of Health has Health Workforce Australia that is directly
involved in promotion and management of adequate health workforce in Australia. The HWA
uses policies and programme mission is to address challenges in the health workforce of
providing innovative, skilled, and flexible workforce for the Australian health system (Buchan,
Twigg, Dussault, Duffield, & Stone, 2015). The HWA has developed a long term national
workforce projection. This projection is for planning doctors, midwives and nurses workforce to
2015 called HW 2025. This framework is the bases of developing policies that ensure the
countries health workforce continually meet the people’s need.
The Australian health workforce is faced by several challenges that require appropriate planning
to build capacity for the future. The first challenge in the health is inadequate domestic
practitioners. The country relies on internationally recruited practitioners. Secondly, there is an
increasing aging population in the country who consume more health care as compared to a
young population. Another challenge for the Australian health system relating to workforce is
cost. It estimated that health workforce cost account for 70% of the total healthcare cost in the
country. Lastly, the Australian health system has distribution challenge with much rural parts
lacking access to qualified practitioners. Therefore, the Australian health workforce require
planning processes.
Australia
Australia has a population of 24.13 million people. The country has a GDP of more than USD
1.205 trillion and USD 49927.82 per capita income. The Australian government bears health care
cost through Medicare Scheme. The Medicare Scheme help low and poor incomer citizens pay
medical bills (McGrail, & Humphreys, 2015). The country has 102802 medical practitioners
distributed in different capacities in the country’s health system. The Australian health workforce
recorded a growth rate of 1.6% from year 2012 to 2015. Medical practitioners work an average
of 42 hours per week with a female to male ratio of 2:5. The country old workforce above 55
years is 1 in every 4 practitioners. Australia also recorded 3210 student commencement of
medical undergraduate studies in 2015.
The Australian health workforce is planned and managed by the government through The
Department of Health. The Department of Health has Health Workforce Australia that is directly
involved in promotion and management of adequate health workforce in Australia. The HWA
uses policies and programme mission is to address challenges in the health workforce of
providing innovative, skilled, and flexible workforce for the Australian health system (Buchan,
Twigg, Dussault, Duffield, & Stone, 2015). The HWA has developed a long term national
workforce projection. This projection is for planning doctors, midwives and nurses workforce to
2015 called HW 2025. This framework is the bases of developing policies that ensure the
countries health workforce continually meet the people’s need.
The Australian health workforce is faced by several challenges that require appropriate planning
to build capacity for the future. The first challenge in the health is inadequate domestic
practitioners. The country relies on internationally recruited practitioners. Secondly, there is an
increasing aging population in the country who consume more health care as compared to a
young population. Another challenge for the Australian health system relating to workforce is
cost. It estimated that health workforce cost account for 70% of the total healthcare cost in the
country. Lastly, the Australian health system has distribution challenge with much rural parts
lacking access to qualified practitioners. Therefore, the Australian health workforce require
appropriate planning to meet it people’s health care need by addressing the current issues and
preparing for the future challenges.
Japan
Japan has a population of 127.3 million people with 61.9 million being males an 65.4 million
being females. The country has a negative population growth of -0.71%. The Japanese
population has experienced a decline since the year 2005. The country also has the highest
proportion of order people than young people. The Japan economy has a GDP of more than USD
4.072 trillion and more than USD 31935 GDP per Capita. The Japanese healthcare system is
administered using an integrated structure that comprise of national bureaucracy that is the
ministry of Health, Labour and Welfare (MHLW), prefectural public health department and
municipal public health department. The MHLW is the overall body that has responsibility for
the health care and occupations in health. The Japan health workforce recorded 3362855 workers
in 2013 which was an increase by 4.3%. There health workforce has 2.38 doctors per 1000
people which is below the OECD average which requires 3.1. The nurse per 1000 citizens is
11.39 above the average 8.8 recommendation of the OECD. The Japan health workforce is
women dominated making up 75% of the total medical practitioners in the country.
The MHLW is responsible for health workforce planning and policies development. The MHLW
Health Policy Bureau ensures policies are developed and monitored through regular surveys and
advisory. The health workforce training programmes are managed by the Japanese Medical
Administration Division and Reg8inal Health Care Planning Division. The country workforce
demand is expected to increase by 50-100% by the year 2025. The country therefore faces a
challenge of increasing the number of practitioners by more than half of the current number of
practitioners. The challenges in the Japanese health workforce are caused by increasing aged
population that will demand more health care services and increasing lifestyle diseases in the
country (Beck et al., 2018).
Data Profile
Japan and Australia health workforce can be compared by use of graphs and tables to show
similarities and difference. This will compare and contrast the two health workforce performance
and plans.
preparing for the future challenges.
Japan
Japan has a population of 127.3 million people with 61.9 million being males an 65.4 million
being females. The country has a negative population growth of -0.71%. The Japanese
population has experienced a decline since the year 2005. The country also has the highest
proportion of order people than young people. The Japan economy has a GDP of more than USD
4.072 trillion and more than USD 31935 GDP per Capita. The Japanese healthcare system is
administered using an integrated structure that comprise of national bureaucracy that is the
ministry of Health, Labour and Welfare (MHLW), prefectural public health department and
municipal public health department. The MHLW is the overall body that has responsibility for
the health care and occupations in health. The Japan health workforce recorded 3362855 workers
in 2013 which was an increase by 4.3%. There health workforce has 2.38 doctors per 1000
people which is below the OECD average which requires 3.1. The nurse per 1000 citizens is
11.39 above the average 8.8 recommendation of the OECD. The Japan health workforce is
women dominated making up 75% of the total medical practitioners in the country.
The MHLW is responsible for health workforce planning and policies development. The MHLW
Health Policy Bureau ensures policies are developed and monitored through regular surveys and
advisory. The health workforce training programmes are managed by the Japanese Medical
Administration Division and Reg8inal Health Care Planning Division. The country workforce
demand is expected to increase by 50-100% by the year 2025. The country therefore faces a
challenge of increasing the number of practitioners by more than half of the current number of
practitioners. The challenges in the Japanese health workforce are caused by increasing aged
population that will demand more health care services and increasing lifestyle diseases in the
country (Beck et al., 2018).
Data Profile
Japan and Australia health workforce can be compared by use of graphs and tables to show
similarities and difference. This will compare and contrast the two health workforce performance
and plans.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
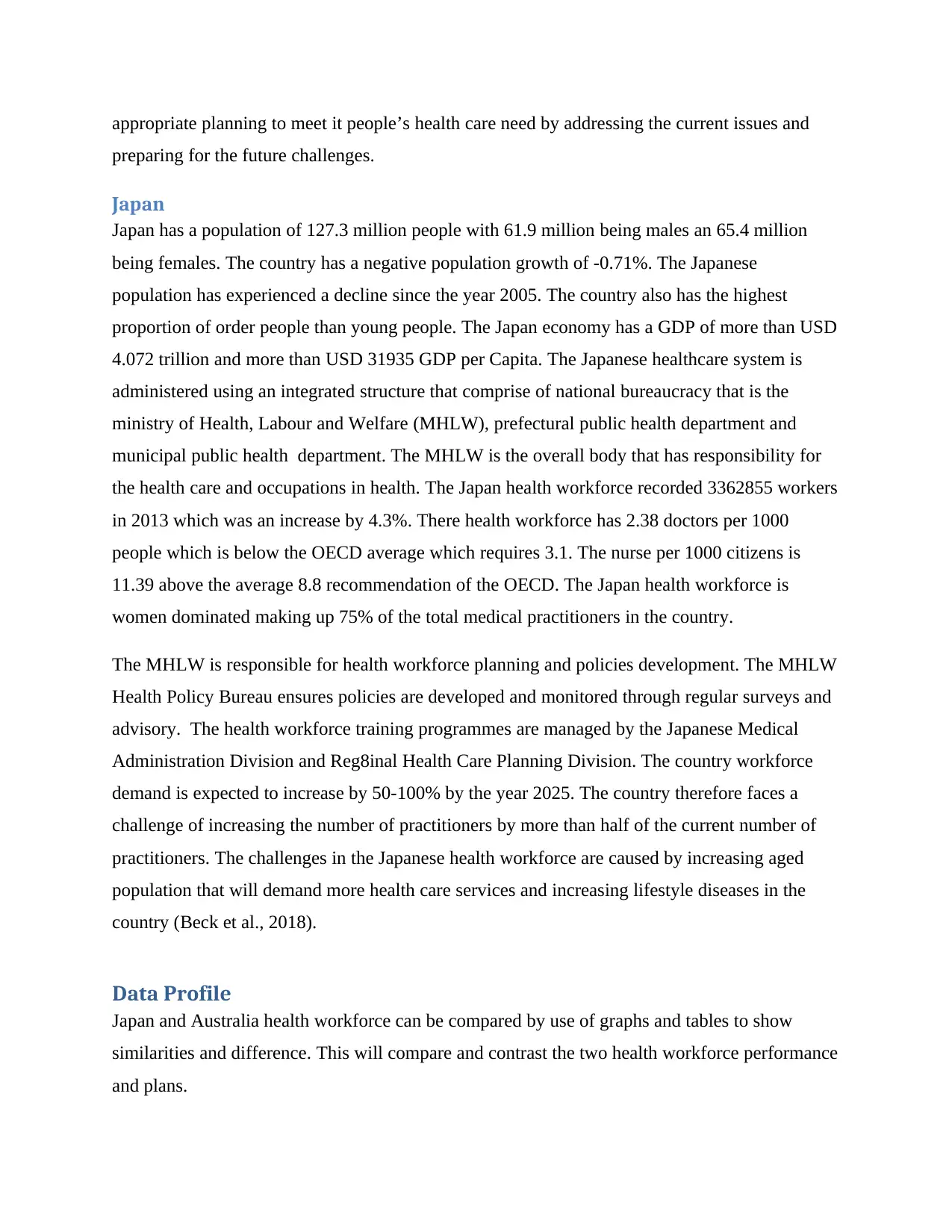
Summary Data Profile Table 2015
Categories Japan Australia
Population 127.3 million 24.13 Million
Doctors 319,480 102,805
Nurses 1,535,161 307,104
Midwives 38,486 28,211
Total Medical
Practitioners
1893127 438120
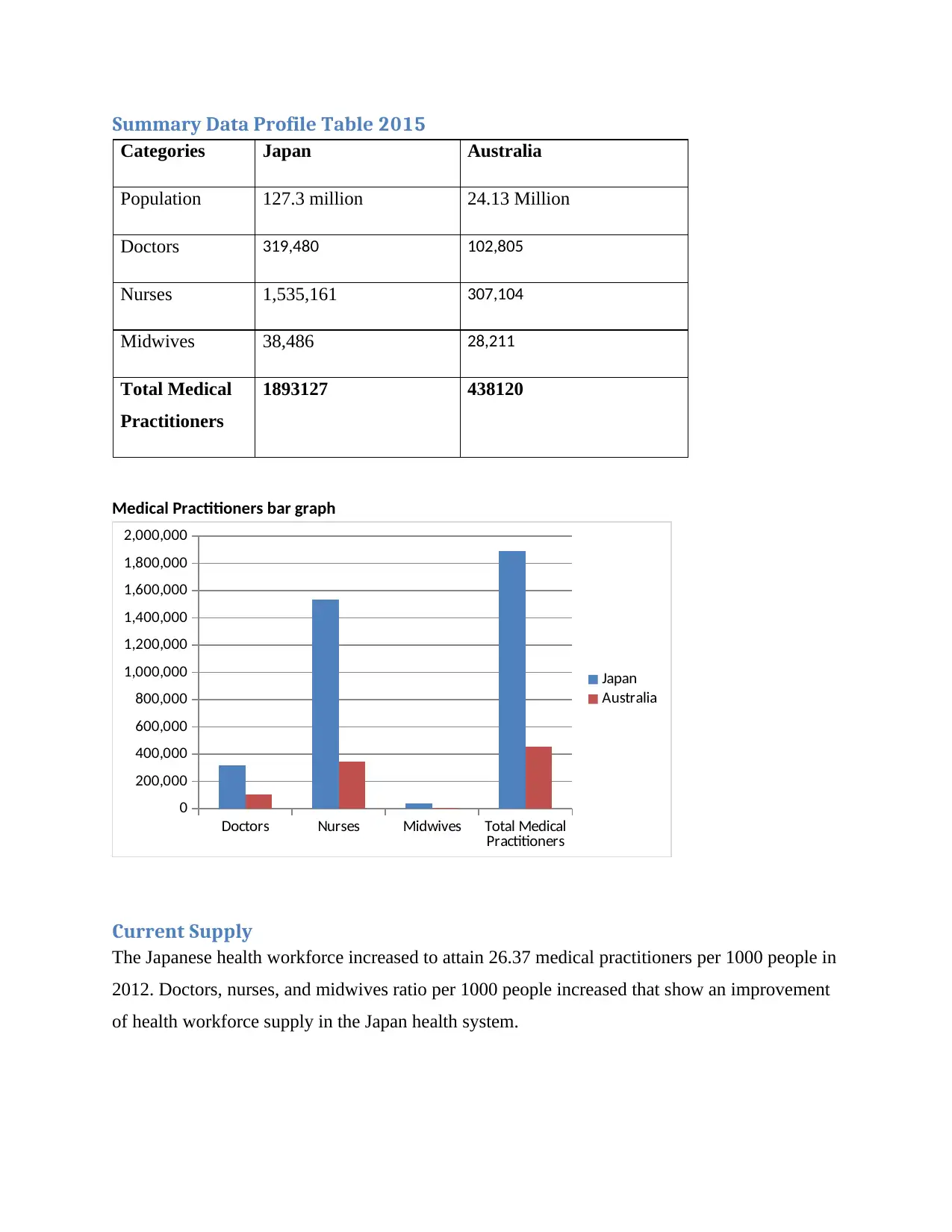
Medical Practitioners bar graph
Doctors Nurses Midwives Total Medical
Practitioners
0
200,000
400,000
600,000
800,000
1,000,000
1,200,000
1,400,000
1,600,000
1,800,000
2,000,000
Japan
Australia
Current Supply
The Japanese health workforce increased to attain 26.37 medical practitioners per 1000 people in
2012. Doctors, nurses, and midwives ratio per 1000 people increased that show an improvement
of health workforce supply in the Japan health system.
Categories Japan Australia
Population 127.3 million 24.13 Million
Doctors 319,480 102,805
Nurses 1,535,161 307,104
Midwives 38,486 28,211
Total Medical
Practitioners
1893127 438120
Medical Practitioners bar graph
Doctors Nurses Midwives Total Medical
Practitioners
0
200,000
400,000
600,000
800,000
1,000,000
1,200,000
1,400,000
1,600,000
1,800,000
2,000,000
Japan
Australia
Current Supply
The Japanese health workforce increased to attain 26.37 medical practitioners per 1000 people in
2012. Doctors, nurses, and midwives ratio per 1000 people increased that show an improvement
of health workforce supply in the Japan health system.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Australia health workforce improved from 2012 to attain 375 medical practitioners per 1000
people in 2015. This represented a 1.8% annual growth of health workforce.
people in 2015. This represented a 1.8% annual growth of health workforce.
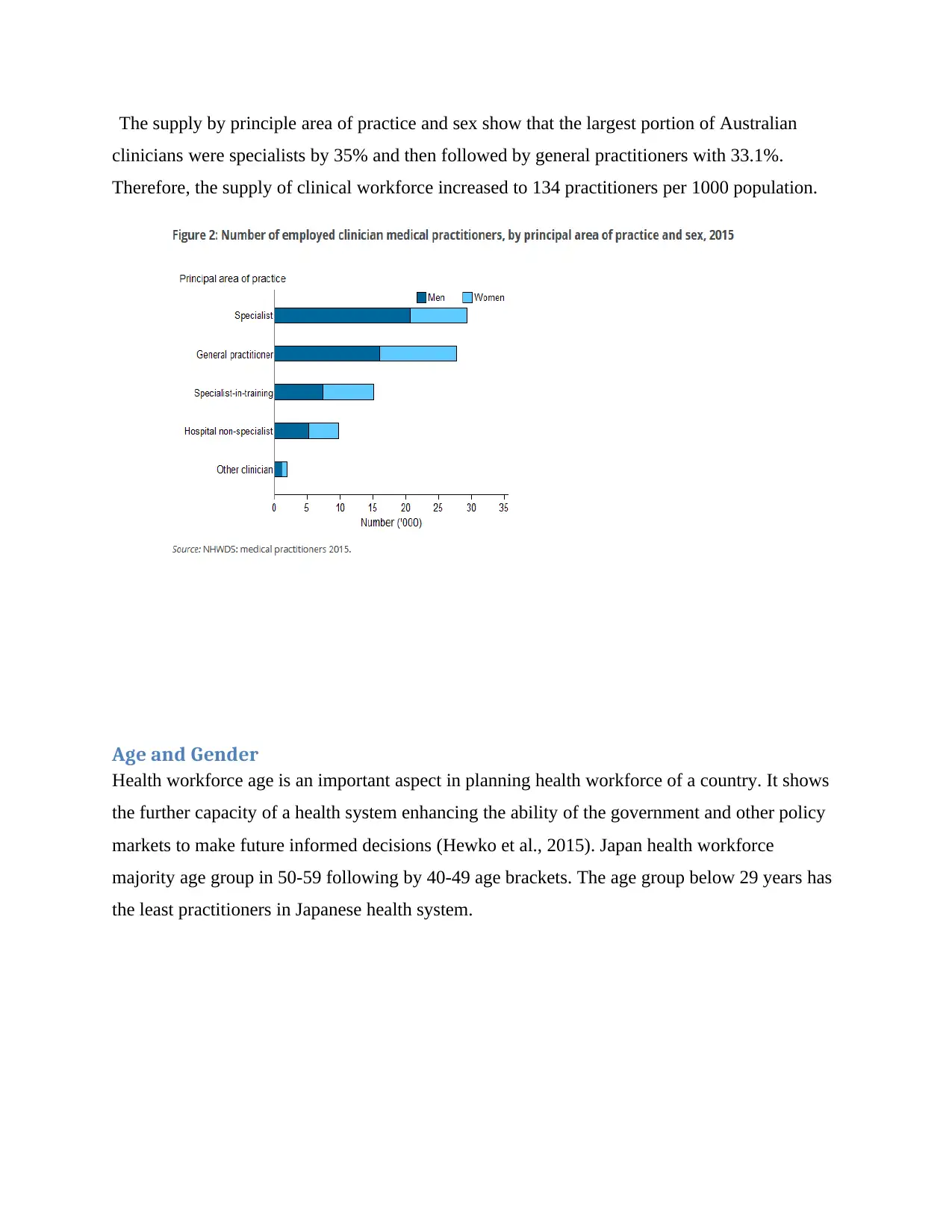
The supply by principle area of practice and sex show that the largest portion of Australian
clinicians were specialists by 35% and then followed by general practitioners with 33.1%.
Therefore, the supply of clinical workforce increased to 134 practitioners per 1000 population.
Age and Gender
Health workforce age is an important aspect in planning health workforce of a country. It shows
the further capacity of a health system enhancing the ability of the government and other policy
markets to make future informed decisions (Hewko et al., 2015). Japan health workforce
majority age group in 50-59 following by 40-49 age brackets. The age group below 29 years has
the least practitioners in Japanese health system.
clinicians were specialists by 35% and then followed by general practitioners with 33.1%.
Therefore, the supply of clinical workforce increased to 134 practitioners per 1000 population.
Age and Gender
Health workforce age is an important aspect in planning health workforce of a country. It shows
the further capacity of a health system enhancing the ability of the government and other policy
markets to make future informed decisions (Hewko et al., 2015). Japan health workforce
majority age group in 50-59 following by 40-49 age brackets. The age group below 29 years has
the least practitioners in Japanese health system.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
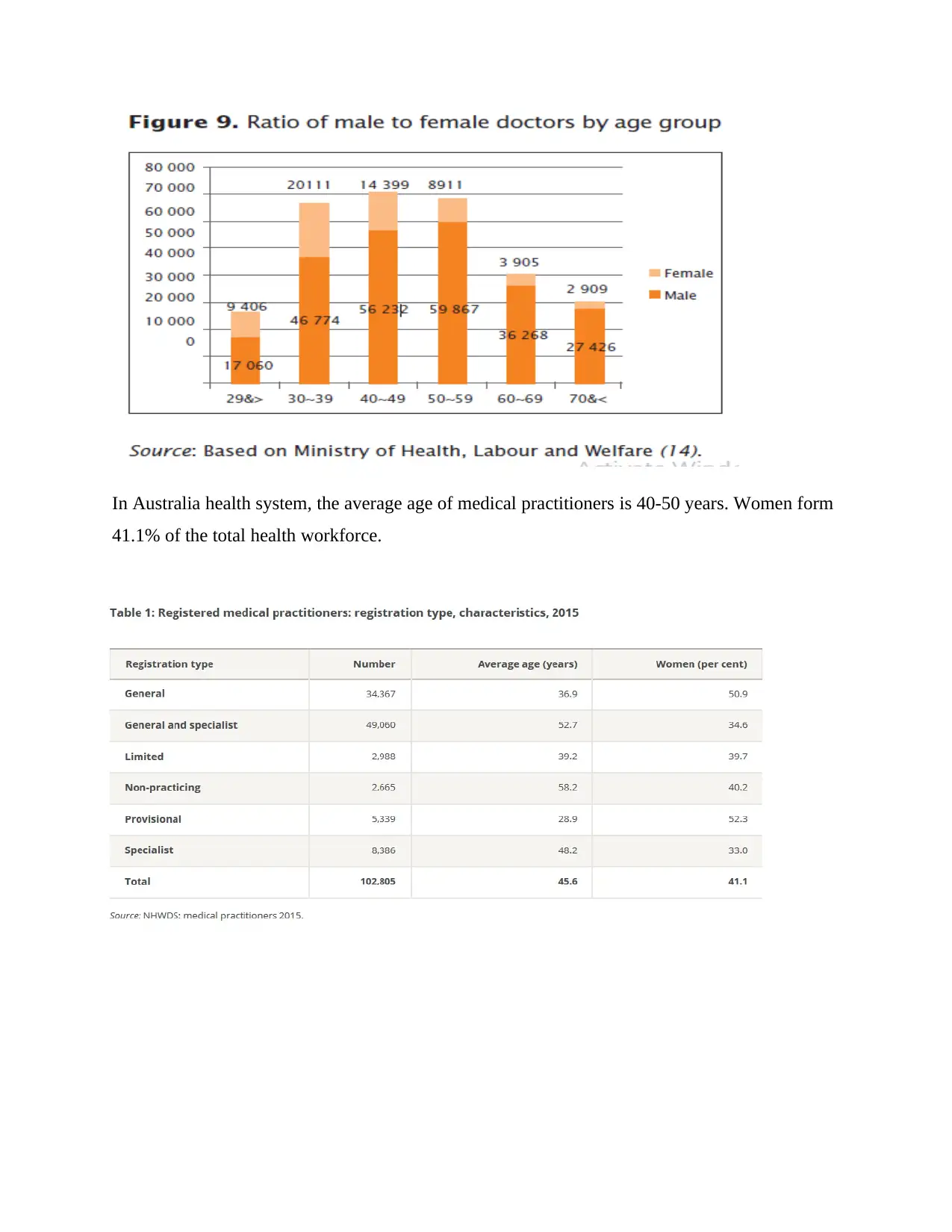
In Australia health system, the average age of medical practitioners is 40-50 years. Women form
41.1% of the total health workforce.
41.1% of the total health workforce.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
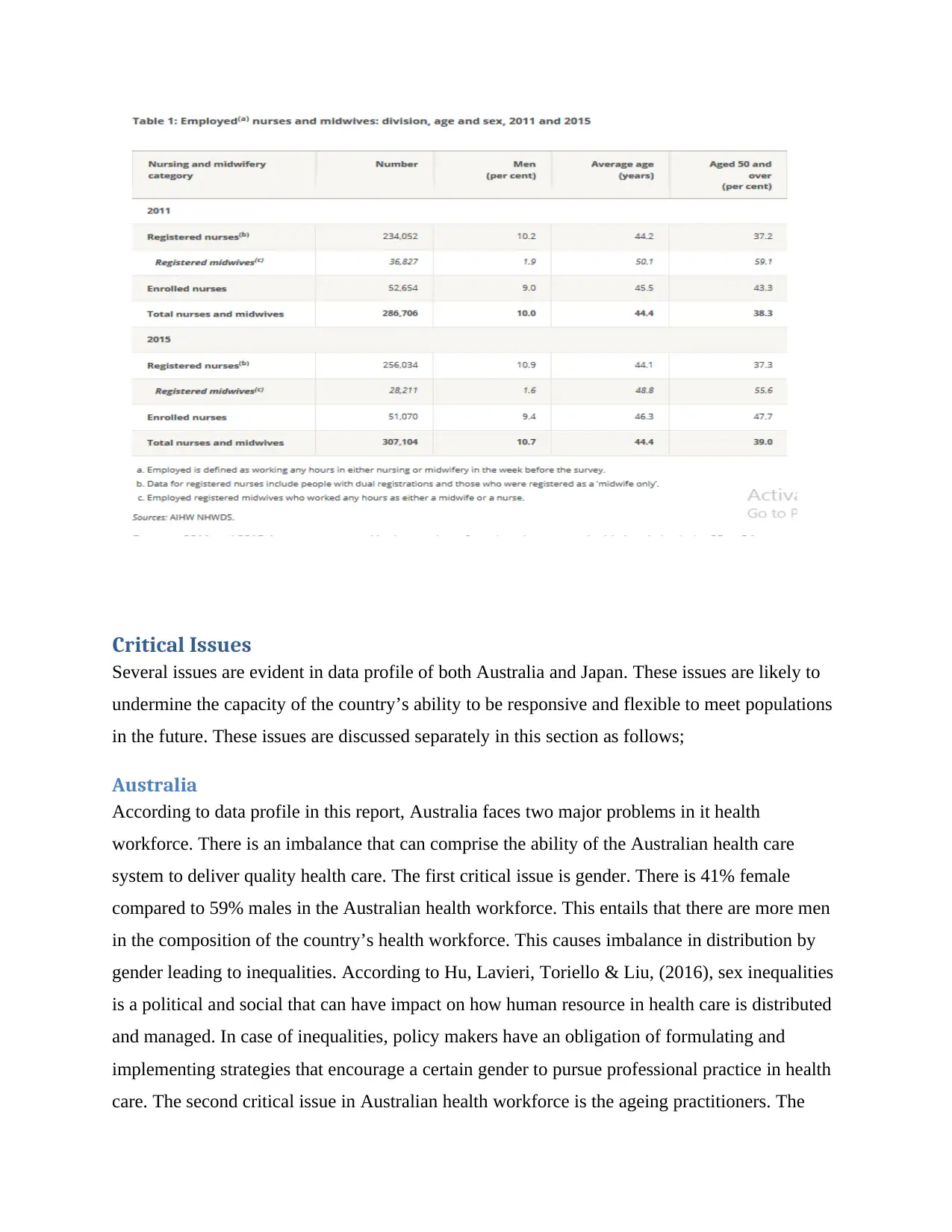
Critical Issues
Several issues are evident in data profile of both Australia and Japan. These issues are likely to
undermine the capacity of the country’s ability to be responsive and flexible to meet populations
in the future. These issues are discussed separately in this section as follows;
Australia
According to data profile in this report, Australia faces two major problems in it health
workforce. There is an imbalance that can comprise the ability of the Australian health care
system to deliver quality health care. The first critical issue is gender. There is 41% female
compared to 59% males in the Australian health workforce. This entails that there are more men
in the composition of the country’s health workforce. This causes imbalance in distribution by
gender leading to inequalities. According to Hu, Lavieri, Toriello & Liu, (2016), sex inequalities
is a political and social that can have impact on how human resource in health care is distributed
and managed. In case of inequalities, policy makers have an obligation of formulating and
implementing strategies that encourage a certain gender to pursue professional practice in health
care. The second critical issue in Australian health workforce is the ageing practitioners. The
Several issues are evident in data profile of both Australia and Japan. These issues are likely to
undermine the capacity of the country’s ability to be responsive and flexible to meet populations
in the future. These issues are discussed separately in this section as follows;
Australia
According to data profile in this report, Australia faces two major problems in it health
workforce. There is an imbalance that can comprise the ability of the Australian health care
system to deliver quality health care. The first critical issue is gender. There is 41% female
compared to 59% males in the Australian health workforce. This entails that there are more men
in the composition of the country’s health workforce. This causes imbalance in distribution by
gender leading to inequalities. According to Hu, Lavieri, Toriello & Liu, (2016), sex inequalities
is a political and social that can have impact on how human resource in health care is distributed
and managed. In case of inequalities, policy makers have an obligation of formulating and
implementing strategies that encourage a certain gender to pursue professional practice in health
care. The second critical issue in Australian health workforce is the ageing practitioners. The
average age of medical practitioners is 45 years old. This entails that by the year 2025 most of
the practitioners in the practice be retiring or preparing to retire from the health system.
Lafortune, (2014) stated that age is an important factor to planning future availability and
capacity of a health system. A young aged health workforce indicate a growing capacity that will
meet the population health care need in the future while an old aged medical practitioners in an
indication of a health system that will not be responsive to future needs of a population.
Therefore, an aging health workforce is threat to a health system ability to deliver accessible
health care to citizens of a country. Australia therefore has to handle aging and gender issues in
the health workforce to avoid the issues undermining the capacity of projected increased demand
for health services in the future.
Japan
The Japanese health workforce is faced with several issues that if not addressed in the health
workforce plan can undermine the ability of the country health system to deliver quality and
accessible health care to its citizens. The first critical issue in the Japan health workforce is the
aging human resource. The majority of medicine practitioners are between 50 to 59 years of age.
This age group of highly qualified workforce will not be available in the future and therefore the
MHLW require appropriate planning to successful develop by training new practitioners. The
Japanese health workforce has a very low health workforce of 29 years and below. This is an
indicator that there are many practitioners who are likely to vacant the health system while at the
same time there is low recruitment level of new practitioners. According to Balasubramanian et
al., (2015) health workforce planners should periodically monitor the age of practitioners to plan
for succession of employees in the health system without leaving a gap at any particular time.
The second critical issue in Japan health workforce is motivation to work in the health care
sector. The Japan has a high level of people who does not contribute to the country’s workforce.
Some practitioners were leaving the health system with an objective to returning in the future.
Lopes, Almeida, & Almada-Lobo, (2015) states that motivation is an important part of a health
workforce plan that enable professional practitioners to have willingness to participate in a health
system. A health workforce plan has to attract, recruit, and retain medical practitioners to
enhance efficiency of human resource performance in the health care (Naccarella, Wraight, &
Gorman, 2016). Therefore, the Japan health workforce plan needs to consider aging practitioners
the practitioners in the practice be retiring or preparing to retire from the health system.
Lafortune, (2014) stated that age is an important factor to planning future availability and
capacity of a health system. A young aged health workforce indicate a growing capacity that will
meet the population health care need in the future while an old aged medical practitioners in an
indication of a health system that will not be responsive to future needs of a population.
Therefore, an aging health workforce is threat to a health system ability to deliver accessible
health care to citizens of a country. Australia therefore has to handle aging and gender issues in
the health workforce to avoid the issues undermining the capacity of projected increased demand
for health services in the future.
Japan
The Japanese health workforce is faced with several issues that if not addressed in the health
workforce plan can undermine the ability of the country health system to deliver quality and
accessible health care to its citizens. The first critical issue in the Japan health workforce is the
aging human resource. The majority of medicine practitioners are between 50 to 59 years of age.
This age group of highly qualified workforce will not be available in the future and therefore the
MHLW require appropriate planning to successful develop by training new practitioners. The
Japanese health workforce has a very low health workforce of 29 years and below. This is an
indicator that there are many practitioners who are likely to vacant the health system while at the
same time there is low recruitment level of new practitioners. According to Balasubramanian et
al., (2015) health workforce planners should periodically monitor the age of practitioners to plan
for succession of employees in the health system without leaving a gap at any particular time.
The second critical issue in Japan health workforce is motivation to work in the health care
sector. The Japan has a high level of people who does not contribute to the country’s workforce.
Some practitioners were leaving the health system with an objective to returning in the future.
Lopes, Almeida, & Almada-Lobo, (2015) states that motivation is an important part of a health
workforce plan that enable professional practitioners to have willingness to participate in a health
system. A health workforce plan has to attract, recruit, and retain medical practitioners to
enhance efficiency of human resource performance in the health care (Naccarella, Wraight, &
Gorman, 2016). Therefore, the Japan health workforce plan needs to consider aging practitioners
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




