Research Report: Antibiotic Therapy Effects on Neonatal NEC
VerifiedAdded on 2023/01/19
|26
|5845
|86
Report
AI Summary
This report investigates the effects of antibiotic therapy on necrotizing enterocolitis (NEC), a severe inflammatory condition affecting the intestines of neonates, particularly preterm and low birth weight infants. The study explores the significance of NEC, its high mortality rates, and the role of antibiotics in treatment. It reviews existing literature, including studies on the microbiome's role in NEC development, the impact of antibiotic exposure on infant health, and the risks associated with antibiotic resistance. The report synthesizes evidence from various databases, analyzing the benefits and limitations of antibiotic therapy, and the importance of considering antibiotic composition and potential side effects. The report highlights the need for careful antibiotic selection and provides recommendations to improve neonatal care. The report also includes a PICO question, evidence search strategy and individual evidence summary to further support the research.

Running head: EFFECTS OF ANTIBIOTIC THERAPY ON NEC 1
The Effects of Antibiotic Therapy on Necrotizing Enterocolitis
Name
Institution
The Effects of Antibiotic Therapy on Necrotizing Enterocolitis
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 2
Problem
AlFaleh and Anabrees (2014) describe necrotizing enterocolitis (henceforth NEC) as an
inflammatory ailment that affects the human intestines and is associated with sepsis. The
researchers explain that in most cases, NEC is complicated by issues such as perforation, and
peritonitis and may result to death. As a consequence, Astrug, and Claud (2018) term NEC as
one of the commonest and devastating conditions among neonates. Similarly, the researchers
demystify that to date, no viable remedies of eradicating NEC have been established. Such
attributes make the study of the effects of antibiotics on NEC a priority for research. Babatunde
et al. (2015) explain that the high degrees of involvement depicted by NEC makes the condition
one of the most acquired in surgical and clinical settings among neonatal and the main cause of
mortality among infants across the globe. The researchers demystify that the rate of morbidity
and mortality resulting from NEC is inversely proportional to the gestational weight and age of
the infant at birth even though it is exacerbated among newborns that require surgery and those
presenting birth weights ranging between 500g and 1500g. Similarly, Albert et al. (2018) reveal
that the condition manifests in about 5% of the hospitalizations related to neonatal care and
among 5% to 10% of newborns who present low birth weights.
Significance of the Study
NEC is characterized by an inflammatory disorder of the gastrointestinal region with a
greater presence among preterm and low birth weight infants. According to (ref), the condition
manifests as an exaggerated and severe ailment in environments that are characterized with
intestinal immaturity; an aspect that increases the susceptibility to the invasion of pathogenic
bacteria. The pathology of NEC extends in severe incidences to present a clinicopathological
syndrome with variable systemic symptoms. (ref 6) explain that NEC has a progressive intensity
resulting from the coagulation of the GIT. Such complications play a n essential role in revealing
the efficacy of the current study.
Problem
AlFaleh and Anabrees (2014) describe necrotizing enterocolitis (henceforth NEC) as an
inflammatory ailment that affects the human intestines and is associated with sepsis. The
researchers explain that in most cases, NEC is complicated by issues such as perforation, and
peritonitis and may result to death. As a consequence, Astrug, and Claud (2018) term NEC as
one of the commonest and devastating conditions among neonates. Similarly, the researchers
demystify that to date, no viable remedies of eradicating NEC have been established. Such
attributes make the study of the effects of antibiotics on NEC a priority for research. Babatunde
et al. (2015) explain that the high degrees of involvement depicted by NEC makes the condition
one of the most acquired in surgical and clinical settings among neonatal and the main cause of
mortality among infants across the globe. The researchers demystify that the rate of morbidity
and mortality resulting from NEC is inversely proportional to the gestational weight and age of
the infant at birth even though it is exacerbated among newborns that require surgery and those
presenting birth weights ranging between 500g and 1500g. Similarly, Albert et al. (2018) reveal
that the condition manifests in about 5% of the hospitalizations related to neonatal care and
among 5% to 10% of newborns who present low birth weights.
Significance of the Study
NEC is characterized by an inflammatory disorder of the gastrointestinal region with a
greater presence among preterm and low birth weight infants. According to (ref), the condition
manifests as an exaggerated and severe ailment in environments that are characterized with
intestinal immaturity; an aspect that increases the susceptibility to the invasion of pathogenic
bacteria. The pathology of NEC extends in severe incidences to present a clinicopathological
syndrome with variable systemic symptoms. (ref 6) explain that NEC has a progressive intensity
resulting from the coagulation of the GIT. Such complications play a n essential role in revealing
the efficacy of the current study.
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 3
The levels of mortality attributed to neonatal sepsis have undergone a significant decline
since the introduction of antibiotics. Despite such developments, Esmaeilizand et al. (2017)
explain that infections still remain the most significant causes of mortality and morbidity among
newborns. Hackam et al. (2018) consider late-onset sepsis as the major cause of death among
preterm infants within the first two weeks of life. The nature of NEC as a multifactorial and
complex condition reveals the significance of the present study. The study seeks to undertake a
critical analysis of prematurity, intestinal colonization and use of formula feeding as the three
causative factors for NEC. However, Gordon et al. (2012) consider prematurity as the most
important factor when studying the pathogenesis of NEC. Currently, physicians consider
antibiotics as the most effective medications in the neonatal unit.
As a consequence AlFaleh and Anabrees (2014) states that most of the infants who
present extremely low birth weights (< 1kg) are exposed to antibiotics in their first postnatal
days. However, the researchers explain that there are tendencies that physicians and caregivers
may overuse antibiotics among neonates despite the presence of a wider range of guidelines and
policy frameworks that explain the appropriate application of antibiotics. According to Reed et
al. (2018), the ineffective use of antibiotics in the neonatal phase of life exposes the child to the
vulnerabilities associated with the disturbance of the microbial colonizing the neonate; a
situation which may result to colonization with the MDR bacteria. Similarly, the scholars reveal
that exposure to antibiotics in the neonatal phase of life is closely related to detrimental
outcomes, allergic conditions, obesity and inflammatory bowel ailments in the adult stages of
life. Therefore, the current study plays an effective role in undertaking a critical appraisal and
synthesis of evidence from previous researches to synthesize evidence from previous scholarly
works revealing a wider range of antibiotic exposures among neonates and the risk of developing
NEC.
PICO Question
In neonates with necrotizing enterocolitis, does antibiotic therapy compared to usual care
lead to clinically significant outcomes?
The levels of mortality attributed to neonatal sepsis have undergone a significant decline
since the introduction of antibiotics. Despite such developments, Esmaeilizand et al. (2017)
explain that infections still remain the most significant causes of mortality and morbidity among
newborns. Hackam et al. (2018) consider late-onset sepsis as the major cause of death among
preterm infants within the first two weeks of life. The nature of NEC as a multifactorial and
complex condition reveals the significance of the present study. The study seeks to undertake a
critical analysis of prematurity, intestinal colonization and use of formula feeding as the three
causative factors for NEC. However, Gordon et al. (2012) consider prematurity as the most
important factor when studying the pathogenesis of NEC. Currently, physicians consider
antibiotics as the most effective medications in the neonatal unit.
As a consequence AlFaleh and Anabrees (2014) states that most of the infants who
present extremely low birth weights (< 1kg) are exposed to antibiotics in their first postnatal
days. However, the researchers explain that there are tendencies that physicians and caregivers
may overuse antibiotics among neonates despite the presence of a wider range of guidelines and
policy frameworks that explain the appropriate application of antibiotics. According to Reed et
al. (2018), the ineffective use of antibiotics in the neonatal phase of life exposes the child to the
vulnerabilities associated with the disturbance of the microbial colonizing the neonate; a
situation which may result to colonization with the MDR bacteria. Similarly, the scholars reveal
that exposure to antibiotics in the neonatal phase of life is closely related to detrimental
outcomes, allergic conditions, obesity and inflammatory bowel ailments in the adult stages of
life. Therefore, the current study plays an effective role in undertaking a critical appraisal and
synthesis of evidence from previous researches to synthesize evidence from previous scholarly
works revealing a wider range of antibiotic exposures among neonates and the risk of developing
NEC.
PICO Question
In neonates with necrotizing enterocolitis, does antibiotic therapy compared to usual care
lead to clinically significant outcomes?
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 4
Evidence
Search Strategy
The search strategy adopted for the current study was initiated in consultation with a
librarian, a local epidemiologist, a neonatologist and a pediatric pharmacologist. The study
adopted scholarly evidences from databases such as Embase, CINAHL, Cochrane Library,
Excerpta Medica Database, MEDLINE and EBCOhost using the terms adopted in the PICO
question. The authors of the scholarly materials obtained were not contacted to avail
supplementary information regarding their publications. Further, no search was undertaken in the
grey literature.
The search strategy in Embase, CINAHL, Cochrane Library, Excerpta Medica Database,
MEDLINE and EBCOhost databases was as follows: ‘newborns infants’ and ‘antibacterial
agents’ with any of the following outcomes ‘necrotizing, enterocolitis’ or ‘mortality’. The first
search was undertaken by the use of a free text in Embase, CINAHL, Cochrane Library,
Excerpta Medica Database, MEDLINE and EBCOhost through combination of the key words
‘neonatal, low birth weight’ ‘infant, post mature’, ‘premature, infant’ or ‘newborn, infant’ with
the terms ‘antibacterial agents’ or ‘antibiotics’ with ‘necrotizing enterocolitis’. However, the
Embase database adopts certain specific keywords such as ‘newborn’ and ‘antibiotic agent’ the
keywords were combined with the term ‘necrotizing enterocolitis’. Finally, a critical review of
the citations and references lists adopted in the studies and other previous reviews were
incorporated to foster the identification of other eligible studies. The citations were then
combined with the exclusion of duplicates and triplicates.
A Summary of Evidences
The role of microbiome in the development of NEC
All the studies adopted described antibiotics as the most commonly prescribed medical
remedies for necrotizing anterocolitis even though they impose great negative effects on the side
Evidence
Search Strategy
The search strategy adopted for the current study was initiated in consultation with a
librarian, a local epidemiologist, a neonatologist and a pediatric pharmacologist. The study
adopted scholarly evidences from databases such as Embase, CINAHL, Cochrane Library,
Excerpta Medica Database, MEDLINE and EBCOhost using the terms adopted in the PICO
question. The authors of the scholarly materials obtained were not contacted to avail
supplementary information regarding their publications. Further, no search was undertaken in the
grey literature.
The search strategy in Embase, CINAHL, Cochrane Library, Excerpta Medica Database,
MEDLINE and EBCOhost databases was as follows: ‘newborns infants’ and ‘antibacterial
agents’ with any of the following outcomes ‘necrotizing, enterocolitis’ or ‘mortality’. The first
search was undertaken by the use of a free text in Embase, CINAHL, Cochrane Library,
Excerpta Medica Database, MEDLINE and EBCOhost through combination of the key words
‘neonatal, low birth weight’ ‘infant, post mature’, ‘premature, infant’ or ‘newborn, infant’ with
the terms ‘antibacterial agents’ or ‘antibiotics’ with ‘necrotizing enterocolitis’. However, the
Embase database adopts certain specific keywords such as ‘newborn’ and ‘antibiotic agent’ the
keywords were combined with the term ‘necrotizing enterocolitis’. Finally, a critical review of
the citations and references lists adopted in the studies and other previous reviews were
incorporated to foster the identification of other eligible studies. The citations were then
combined with the exclusion of duplicates and triplicates.
A Summary of Evidences
The role of microbiome in the development of NEC
All the studies adopted described antibiotics as the most commonly prescribed medical
remedies for necrotizing anterocolitis even though they impose great negative effects on the side
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 5
of the affected infants. Similarly, AlFaleh ,and Anabrees (2014); Astrug, and Claud (2018);
Autmizguine et al. (2015); Babatunde et al. (2015); Esmaeilizand et al. (2017); and Gordon et al.
(2012) revealed that NEC is one of the most devastating conditions that affects about 15% of
neonatal infants. The researchers explain that even though the pathogenesis of NEC remains
unexplained, there are tendencies that the existing defects in the processes that lead to the
development and commensalism of the host microbiome as the most significant contributors. On
the other hand, the studies conducted by Samuels et al. (2016); Staude et al. (2018); Stey et al.
(2016); Bellodas and Kadrofske (2019); and Ting et al. (2016) revealed that the advancement of
NEC is presented by uncontrolled inflammations in the intestinal region that are highly capable
of causing sepsis, tissue necrosis and perforation. Further, Isani et al. (2019) explain that NEC is
associated with increased mortality rates of up to 30% despite the fact that it may depict
substantial long and short term morbidities. McEwen et al. (2018); Seale et al. (2018), Fan et al.
(2018); AlFaleh and Anabrees (2014); Ting et al. (2018); and Albert et al. (2018) identify
prematurity as the greatest risk factor for necrotizing enterocolitis.
The Murine models adopted by Pammi, and Haque (2015) and Hackam et al. (2018)
identify bacterial colonization of the intestines as the most essential factor in fostering the
development of NEC among infants. However, most of the researches incorporated for this study
do not identify a specific bacterial species as the causative agent for NEC. Gordon et al. (2012)
explain that longitudinal analyses of fecal microbiomes obtained from infants based on the
studies conducted by Autmizguine et al. (2015) and Ting et al. (2018) have played an essential
role in shedding light on the existing variations in the colonization patterns and composition of
microbiomes with the ability to develop NEC and those that lack such potentials. For instance,
the study conducted by Esmaeilizand et al. (2017) revealed that the presence of bacterial agents
such as Proteobacteria and Actinobacteria is in great abundance in the fecal matter of infants.
The scholars explain that Proteobacteria and Actinobacteria later develop NEC. On the other
hand, the experimental study conducted by Isani et al. (2019) revealed that the concentration of
bacterial agents such as Bacteriodetes and Bifidobacteria is minimal in the fecal matter of
infants. Similarly, the researchers reveal that fecal dysbiosis is associated with an increase in the
population of microbes of the phyla Firmicutes and Proteobacteria and proceed the advabcemeb
of NEC among neonates.
of the affected infants. Similarly, AlFaleh ,and Anabrees (2014); Astrug, and Claud (2018);
Autmizguine et al. (2015); Babatunde et al. (2015); Esmaeilizand et al. (2017); and Gordon et al.
(2012) revealed that NEC is one of the most devastating conditions that affects about 15% of
neonatal infants. The researchers explain that even though the pathogenesis of NEC remains
unexplained, there are tendencies that the existing defects in the processes that lead to the
development and commensalism of the host microbiome as the most significant contributors. On
the other hand, the studies conducted by Samuels et al. (2016); Staude et al. (2018); Stey et al.
(2016); Bellodas and Kadrofske (2019); and Ting et al. (2016) revealed that the advancement of
NEC is presented by uncontrolled inflammations in the intestinal region that are highly capable
of causing sepsis, tissue necrosis and perforation. Further, Isani et al. (2019) explain that NEC is
associated with increased mortality rates of up to 30% despite the fact that it may depict
substantial long and short term morbidities. McEwen et al. (2018); Seale et al. (2018), Fan et al.
(2018); AlFaleh and Anabrees (2014); Ting et al. (2018); and Albert et al. (2018) identify
prematurity as the greatest risk factor for necrotizing enterocolitis.
The Murine models adopted by Pammi, and Haque (2015) and Hackam et al. (2018)
identify bacterial colonization of the intestines as the most essential factor in fostering the
development of NEC among infants. However, most of the researches incorporated for this study
do not identify a specific bacterial species as the causative agent for NEC. Gordon et al. (2012)
explain that longitudinal analyses of fecal microbiomes obtained from infants based on the
studies conducted by Autmizguine et al. (2015) and Ting et al. (2018) have played an essential
role in shedding light on the existing variations in the colonization patterns and composition of
microbiomes with the ability to develop NEC and those that lack such potentials. For instance,
the study conducted by Esmaeilizand et al. (2017) revealed that the presence of bacterial agents
such as Proteobacteria and Actinobacteria is in great abundance in the fecal matter of infants.
The scholars explain that Proteobacteria and Actinobacteria later develop NEC. On the other
hand, the experimental study conducted by Isani et al. (2019) revealed that the concentration of
bacterial agents such as Bacteriodetes and Bifidobacteria is minimal in the fecal matter of
infants. Similarly, the researchers reveal that fecal dysbiosis is associated with an increase in the
population of microbes of the phyla Firmicutes and Proteobacteria and proceed the advabcemeb
of NEC among neonates.
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 6
The effects of antibiotic therapy
The studies by Gordon et al. (2012); Babatunde et al. (2015); and Reed et al. (2018)
emphasized on the efficacy of prenatal and postnatal exposure to antibiotics as a critical
contributor to the dysbiosis that leads to the presence of NEC. Ting et al. (2018) explain that
prophylactic administration of antibiotics can be applied as a significant procedure in fostering
the prevention of NEC among infants. The scholars explain that the administration of
prophylactic enteral antigiotics such as kenamycin, gentanicin and vancomycin is of critical
essence in fostering great reductions in the rates and symptomatic effects of NEC and a
significant reduction in the number of death related to NEC. However, the aforementioned
studies present several limitations. For instance, the inability of the researchers in these studies to
give a clear account of the diets and feeding schedules adopted by the infants under
consideration, limited adjustments for confounding, and failure to report the possible harmful
effects of the antibiotics adopted reveal their limitations. On the other hand, Gordon et al. (2012)
explain that over the years, NIC units have undergone great changes in terms of upgrade. Such
changes include the adoption of standardized feeding protocols, adoption of donor milk from
humans in the absence of breast milk and the introduction of enteral feeds at an early stage of
life.
On the other hand, Seale et al. (2018) explain that there are tendencies that prolonged
exposure of infants to antibiotics plays a role in increasing the child’s levels of resistance against
the drug. For instance, the scholars demystify that adoption of enteral kenamycin treatments
revealed a positive relationship with the increase in the population of bacteria that are resistant to
antibiotics. Comparatively, the study by Isani et al. (2019) revealed that the use of enteral
vancomycin therapy did not depict a positive relationship with the levels of antibiotic resistance
even though it showed a positive relationship in the levels of microbiota depicting predominant
Gram negative yeast and bacteria. Ideally, predominant Gram negative yeast and bacteria impose
great harmful effects on the side of a premature host.
Over the years, premature neonates have been exposed to broad spectrum antibiotics as a
universal remedy in their first days of life. However, Ting et al. (2016) explain that there are
The effects of antibiotic therapy
The studies by Gordon et al. (2012); Babatunde et al. (2015); and Reed et al. (2018)
emphasized on the efficacy of prenatal and postnatal exposure to antibiotics as a critical
contributor to the dysbiosis that leads to the presence of NEC. Ting et al. (2018) explain that
prophylactic administration of antibiotics can be applied as a significant procedure in fostering
the prevention of NEC among infants. The scholars explain that the administration of
prophylactic enteral antigiotics such as kenamycin, gentanicin and vancomycin is of critical
essence in fostering great reductions in the rates and symptomatic effects of NEC and a
significant reduction in the number of death related to NEC. However, the aforementioned
studies present several limitations. For instance, the inability of the researchers in these studies to
give a clear account of the diets and feeding schedules adopted by the infants under
consideration, limited adjustments for confounding, and failure to report the possible harmful
effects of the antibiotics adopted reveal their limitations. On the other hand, Gordon et al. (2012)
explain that over the years, NIC units have undergone great changes in terms of upgrade. Such
changes include the adoption of standardized feeding protocols, adoption of donor milk from
humans in the absence of breast milk and the introduction of enteral feeds at an early stage of
life.
On the other hand, Seale et al. (2018) explain that there are tendencies that prolonged
exposure of infants to antibiotics plays a role in increasing the child’s levels of resistance against
the drug. For instance, the scholars demystify that adoption of enteral kenamycin treatments
revealed a positive relationship with the increase in the population of bacteria that are resistant to
antibiotics. Comparatively, the study by Isani et al. (2019) revealed that the use of enteral
vancomycin therapy did not depict a positive relationship with the levels of antibiotic resistance
even though it showed a positive relationship in the levels of microbiota depicting predominant
Gram negative yeast and bacteria. Ideally, predominant Gram negative yeast and bacteria impose
great harmful effects on the side of a premature host.
Over the years, premature neonates have been exposed to broad spectrum antibiotics as a
universal remedy in their first days of life. However, Ting et al. (2016) explain that there are
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 7
tendencies that the neonatal may be exposed to a prolonged course of antibiotic treatments for
culture-negative and/or culture-positive sepsis. The study conducted by Yajamanyam et al.
(2014) revealed that prolonged exposure of antenatal and post natal antibiotics increases the risk
of developing NEC. For instance, Seale et al. (2018) demystify that the administration of
antibiotics suppresses intestinal flora that in turn lead to increased risk of acquiring NEC.
Recommendations
There is need for physicians to undertake a critical analysis of the composition of
antibiotics before administration to infants. As aforementioned, the use of enteral vancomycin
therapy does not depict a positive relationship with the levels of antibiotic resistance even though
it showed a positive relationship in the levels of microbiota depicting predominant Gram
negative yeast and bacteria. However, predominant Gram negative yeast and bacteria impose
great harmful effects on the side of a premature host. Therefore, there is need for provision of
additional information whenever enteral antibiotics are recommended for underdeveloped
neonates with low weight.
While the exposure of infants and their mothers to perinatal and antenatal antibiotics
could lead to negative effects such as the suppression of intestinal flora that play a role in
increasing the risk of NEC, there is need for physicians to prescribe alternative antibiotics such
as ampicilin and gentamycin based on their effectiveness in reducing the effects of NEC.
Translation
The study recommends that physicians should opt for the administration of ampicilin and
gentamycin while seeking for relevant additional information whenever enteral antibiotics are
recommended for underdeveloped neonates with low weight. These recommendations are
feasible and appropriate to the modern day medical practices as they are evidence based.
However, the study preempts that the existing organizational cultures in healthcare institutions
will act as barriers to effective implementation of these recommendations. To foresee the
implementation of the recommendations identified institutional trainings targeting caregivers
tendencies that the neonatal may be exposed to a prolonged course of antibiotic treatments for
culture-negative and/or culture-positive sepsis. The study conducted by Yajamanyam et al.
(2014) revealed that prolonged exposure of antenatal and post natal antibiotics increases the risk
of developing NEC. For instance, Seale et al. (2018) demystify that the administration of
antibiotics suppresses intestinal flora that in turn lead to increased risk of acquiring NEC.
Recommendations
There is need for physicians to undertake a critical analysis of the composition of
antibiotics before administration to infants. As aforementioned, the use of enteral vancomycin
therapy does not depict a positive relationship with the levels of antibiotic resistance even though
it showed a positive relationship in the levels of microbiota depicting predominant Gram
negative yeast and bacteria. However, predominant Gram negative yeast and bacteria impose
great harmful effects on the side of a premature host. Therefore, there is need for provision of
additional information whenever enteral antibiotics are recommended for underdeveloped
neonates with low weight.
While the exposure of infants and their mothers to perinatal and antenatal antibiotics
could lead to negative effects such as the suppression of intestinal flora that play a role in
increasing the risk of NEC, there is need for physicians to prescribe alternative antibiotics such
as ampicilin and gentamycin based on their effectiveness in reducing the effects of NEC.
Translation
The study recommends that physicians should opt for the administration of ampicilin and
gentamycin while seeking for relevant additional information whenever enteral antibiotics are
recommended for underdeveloped neonates with low weight. These recommendations are
feasible and appropriate to the modern day medical practices as they are evidence based.
However, the study preempts that the existing organizational cultures in healthcare institutions
will act as barriers to effective implementation of these recommendations. To foresee the
implementation of the recommendations identified institutional trainings targeting caregivers
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 8
working in neonatal care units on the effects of antibiotic therapy on necrotizing enterocolitis
will be organized. Educational materials on this topic and instructors are the major resources
needed to foresee the implementation of the action plan. On the other hand, surveys and
scorecards will be adopted to evaluate the effectiveness of the proposed changes in clinical
settings. The findings of the proposed changes will be disseminated through publications in
healthcare journals and periodicals.
Measurable goal
To train at least 6 nurses from 15 healthcare institutions in Texas on the effects of antibiotic
therapy on necrotizing enterocolitis by the end of August 2019.
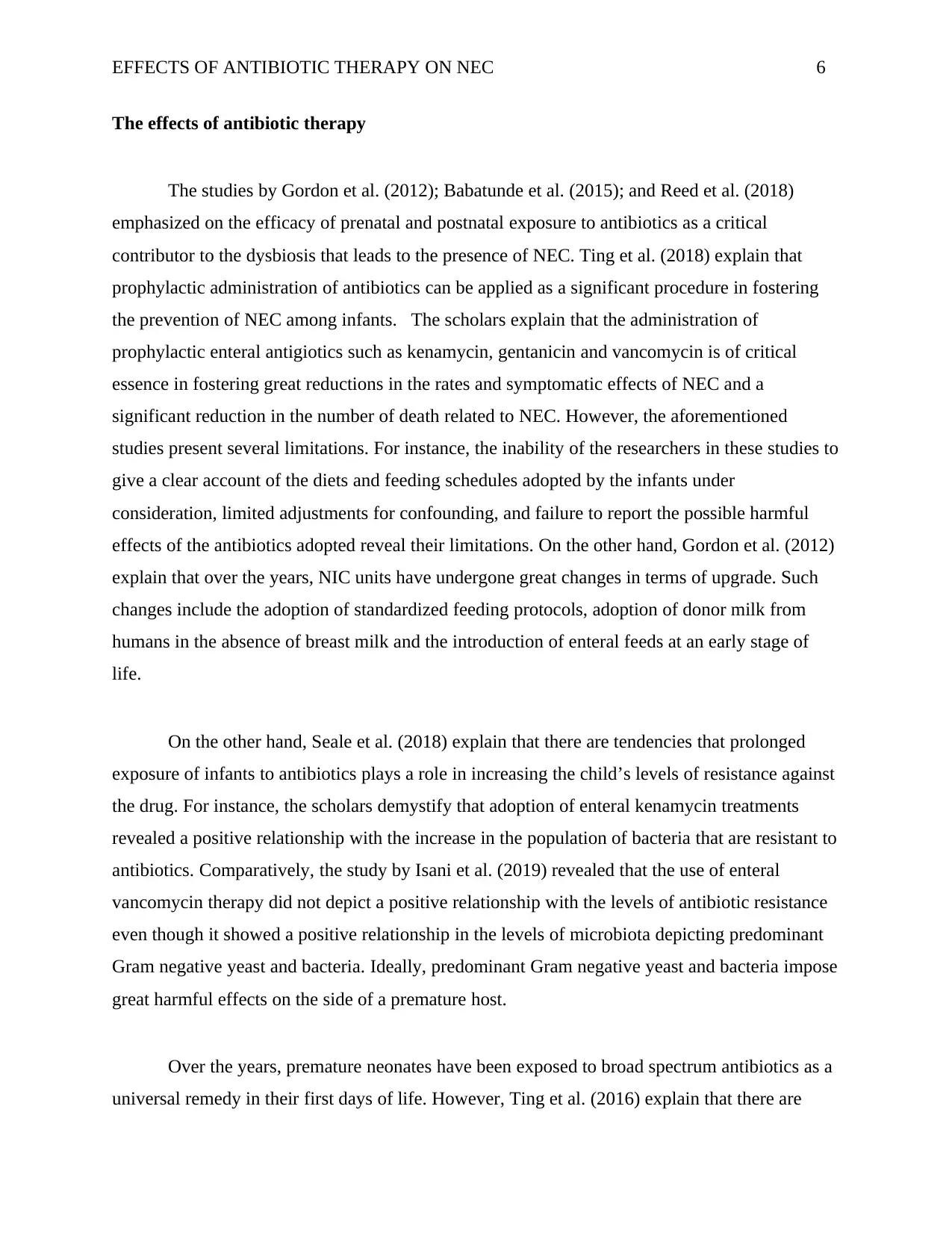
Timeline
Period Activity
April 2019 Prepare study materials on NEC
May 2019 Seek permission from 15 healthcare
institutions in Texas to engage caregivers in
the educational sessions
June- Mid -August 2019 Educate caregivers on the effects of antibiotic
therapy on necrotizing enterocolitis.
Mid-August 2019 –Early September 2019 Administer the survey
Early –Mid September 2019 Publish results
working in neonatal care units on the effects of antibiotic therapy on necrotizing enterocolitis
will be organized. Educational materials on this topic and instructors are the major resources
needed to foresee the implementation of the action plan. On the other hand, surveys and
scorecards will be adopted to evaluate the effectiveness of the proposed changes in clinical
settings. The findings of the proposed changes will be disseminated through publications in
healthcare journals and periodicals.
Measurable goal
To train at least 6 nurses from 15 healthcare institutions in Texas on the effects of antibiotic
therapy on necrotizing enterocolitis by the end of August 2019.
Timeline
Period Activity
April 2019 Prepare study materials on NEC
May 2019 Seek permission from 15 healthcare
institutions in Texas to engage caregivers in
the educational sessions
June- Mid -August 2019 Educate caregivers on the effects of antibiotic
therapy on necrotizing enterocolitis.
Mid-August 2019 –Early September 2019 Administer the survey
Early –Mid September 2019 Publish results

EFFECTS OF ANTIBIOTIC THERAPY ON NEC 9
Conclusion
The study proceeded with the aim of finding answers to the PICO question: In neonates
with necrotizing enterocolitis, does antibiotic therapy compared to usual care lead to clinically
significant outcomes? The study plays an effective role in undertaking a critical appraisal and
synthesis of evidence from previous researches to synthesize evidence from previous scholarly
works revealing a wider range of antibiotic exposures among neonates and the risk of developing
NEC. The study recommends that physicians should opt for the administration of ampicilin and
gentamycin while seeking for relevant additional information whenever enteral antibiotics are
adopted for underdeveloped neonates with low weight.
Conclusion
The study proceeded with the aim of finding answers to the PICO question: In neonates
with necrotizing enterocolitis, does antibiotic therapy compared to usual care lead to clinically
significant outcomes? The study plays an effective role in undertaking a critical appraisal and
synthesis of evidence from previous researches to synthesize evidence from previous scholarly
works revealing a wider range of antibiotic exposures among neonates and the risk of developing
NEC. The study recommends that physicians should opt for the administration of ampicilin and
gentamycin while seeking for relevant additional information whenever enteral antibiotics are
adopted for underdeveloped neonates with low weight.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

EFFECTS OF ANTIBIOTIC THERAPY ON NEC 10
References
Albert, J., Kaur, I., Bajwa, G., Touch, S., Souder, E., Long, S., & Bhandari, V. (2018,
November). 175. Implementation of Clinical Practice Guidelines for Care of Neonates
With Necrotizing Enterocolitis Reduces Broad Spectrum Antibiotic Use in the Neonatal
Intensive Care Unit. In Open Forum Infectious Diseases, (Vol. 5, No. suppl_1, pp. S78-
S78). US: Oxford University Press.
Astrug, L., & Claud, E. (2018). Neonatal Necrotizing Enterocolitis. Gastroenterology and
Nutrition: Neonatology Questions and Controversies, 87.
AlFaleh, K., & Anabrees, J. (2014). Probiotics for prevention of necrotizing enterocolitis in
preterm infants. Evidence
‐Based Child Health: A Cochrane Review Journal, 9(3), 584-
671. https://doi.org/10.1002/ebch.1976
Autmizguine, J., Hornik, C. P., Benjamin, D. K., Laughon, M. M., Clark, R. H., Cotten, C. M., ...
& Smith, P. B. (2015). Anaerobic antimicrobial therapy after necrotizing enterocolitis in
VLBW infants. Pediatrics, 135(1), e117-e125. doi: 10.1542/peds.2014-2141
Babatunde, K. A., Irene, A.,Dongo, A. &Sylvester, A. (2015). Advanced necrotizing
enterocolitis with tension pneumoperitoneum in a full-term Nigerian neonate: A case
report. Indian Journal of Basic and Applied Medical Research, 4(3), 86-89. Retrieved
from https://ijbamr.com/pdf/June%202015%2086-89.pdf.pdf
Bellodas S., J., & Kadrofske, M. (2019). Necrotizing enterocolitis. Neurogastroenterology &
Motility, 31(3), e13569.
References
Albert, J., Kaur, I., Bajwa, G., Touch, S., Souder, E., Long, S., & Bhandari, V. (2018,
November). 175. Implementation of Clinical Practice Guidelines for Care of Neonates
With Necrotizing Enterocolitis Reduces Broad Spectrum Antibiotic Use in the Neonatal
Intensive Care Unit. In Open Forum Infectious Diseases, (Vol. 5, No. suppl_1, pp. S78-
S78). US: Oxford University Press.
Astrug, L., & Claud, E. (2018). Neonatal Necrotizing Enterocolitis. Gastroenterology and
Nutrition: Neonatology Questions and Controversies, 87.
AlFaleh, K., & Anabrees, J. (2014). Probiotics for prevention of necrotizing enterocolitis in
preterm infants. Evidence
‐Based Child Health: A Cochrane Review Journal, 9(3), 584-
671. https://doi.org/10.1002/ebch.1976
Autmizguine, J., Hornik, C. P., Benjamin, D. K., Laughon, M. M., Clark, R. H., Cotten, C. M., ...
& Smith, P. B. (2015). Anaerobic antimicrobial therapy after necrotizing enterocolitis in
VLBW infants. Pediatrics, 135(1), e117-e125. doi: 10.1542/peds.2014-2141
Babatunde, K. A., Irene, A.,Dongo, A. &Sylvester, A. (2015). Advanced necrotizing
enterocolitis with tension pneumoperitoneum in a full-term Nigerian neonate: A case
report. Indian Journal of Basic and Applied Medical Research, 4(3), 86-89. Retrieved
from https://ijbamr.com/pdf/June%202015%2086-89.pdf.pdf
Bellodas S., J., & Kadrofske, M. (2019). Necrotizing enterocolitis. Neurogastroenterology &
Motility, 31(3), e13569.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 11
Esmaeilizand, R., Shah, P. S., Seshia, M., Yee, W., Yoon, E. W., & Dow, K. (2017). Antibiotic
exposure and development of necrotizing enterocolitis in very preterm
neonates. Paediatrics& child health, 23(4), e56-e61. https://doi.org/10.1093/pch/pxx169
Fan, X., Zhang, L., Tang, J., Chen, C., Chen, J., Qu, Y., & Mu, D. (2018). The initial
prophylactic antibiotic usage and subsequent necrotizing enterocolitis in high-risk
premature infants: a systematic review and meta-analysis. Pediatric surgery
international, 34(1), 35-45.
Gordon, P., Christensen, R., Weitkamp, J. H., & Maheshwari, A. (2012). Mapping the new world
of necrotizing enterocolitis (NEC): review and opinion. The e-journal of neonatology
research, 2(4), 145. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3666872/pdf/nihms435179.pdf
Hackam, D. J., Sodhi, C. P., & Good, M. (2018). New insights into necrotizing enterocolitis:
from laboratory observation to personalized prevention and treatment. Journal of
pediatric surgery.
Isani, M. A., Delaplain, P. T., Grishin, A., & Ford, H. R. (2018). Evolving understanding of
neonatal necrotizing enterocolitis. Current opinion in pediatrics, 30(3), 417-423.
McEwen, S. A., Angulo, F. J., Collignon, P. J., & Conly, J. M. (2018). Unintended consequences
associated with national-level restrictions on antimicrobial use in food-producing
animals. The Lancet Planetary Health, 2(7), e279-e282.
Pammi, M., & Haque, K. N. (2015). Pentoxifylline for treatment of sepsis and necrotizing
enterocolitis in neonates. Cochrane Database of Systematic Reviews, (3).
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004205.pub3
Esmaeilizand, R., Shah, P. S., Seshia, M., Yee, W., Yoon, E. W., & Dow, K. (2017). Antibiotic
exposure and development of necrotizing enterocolitis in very preterm
neonates. Paediatrics& child health, 23(4), e56-e61. https://doi.org/10.1093/pch/pxx169
Fan, X., Zhang, L., Tang, J., Chen, C., Chen, J., Qu, Y., & Mu, D. (2018). The initial
prophylactic antibiotic usage and subsequent necrotizing enterocolitis in high-risk
premature infants: a systematic review and meta-analysis. Pediatric surgery
international, 34(1), 35-45.
Gordon, P., Christensen, R., Weitkamp, J. H., & Maheshwari, A. (2012). Mapping the new world
of necrotizing enterocolitis (NEC): review and opinion. The e-journal of neonatology
research, 2(4), 145. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3666872/pdf/nihms435179.pdf
Hackam, D. J., Sodhi, C. P., & Good, M. (2018). New insights into necrotizing enterocolitis:
from laboratory observation to personalized prevention and treatment. Journal of
pediatric surgery.
Isani, M. A., Delaplain, P. T., Grishin, A., & Ford, H. R. (2018). Evolving understanding of
neonatal necrotizing enterocolitis. Current opinion in pediatrics, 30(3), 417-423.
McEwen, S. A., Angulo, F. J., Collignon, P. J., & Conly, J. M. (2018). Unintended consequences
associated with national-level restrictions on antimicrobial use in food-producing
animals. The Lancet Planetary Health, 2(7), e279-e282.
Pammi, M., & Haque, K. N. (2015). Pentoxifylline for treatment of sepsis and necrotizing
enterocolitis in neonates. Cochrane Database of Systematic Reviews, (3).
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004205.pub3
EFFECTS OF ANTIBIOTIC THERAPY ON NEC 12
Reed, B. D., Schibler, K. R., Deshmukh, H., Ambalavanan, N., & Morrow, A. L. (2018). The
impact of maternal antibiotics on neonatal disease. The Journal of pediatrics, 197, 97-
103.
Samuels, N., van de Graaf, R., Been, J. V., De Jonge, R. C., Hanff, L. M., Wijnen, R. M., ... &
Vermeulen, M. J. (2016). Necrotising enterocolitis and mortality in preterm infants after
introduction of probiotics: a quasi-experimental study. Scientific reports, 6, 31643.
https://doi.org/10.1038/srep31643
Seale, J. V., Hutchinson, R. A., Fleming, P. F., Sinha, A., Kempley, S. T., Husain, S. M., &
Millar, M. R. (2018). Does antibiotic choice for the treatment of suspected late-onset
sepsis in premature infants determine the risk of developing necrotising enterocolitis? A
systematic review. Early human development, 123, 6-10.
Staude, B., Oehmke, F., Lauer, T., Behnke, J., Göpel, W., Schloter, M., ... & Ehrhardt, H. (2018).
The Microbiome and Preterm Birth: A Change in Paradigm with Profound Implications
for Pathophysiologic Concepts and Novel Therapeutic Strategies. BioMed research
international, 2018.
Stey, A., Barnert, E. S., Tseng, C. H., Keeler, E., Needleman, J., Leng, M., ... & Shew, S. B.
(2015). Outcomes and costs of surgical treatments of necrotizing
enterocolitis. Pediatrics, 135(5), e1190-e1197. doi: 10.1542/peds.2014-1058
Ting, J. Y., Synnes, A., Roberts, A., Deshpandey, A., Dow, K., Yoon, E. W., ... & Shah, P. S.
(2016). Association between antibiotic use and neonatal mortality and morbidities in very
low-birth-weight infants without culture-proven sepsis or necrotizing enterocolitis. JAMA
pediatrics, 170(12), 1181-1187. doi:10.1001/jamapediatrics.2016.2132
Ting, J. Y., Synnes, A., Roberts, A., Deshpandey, A. C., Dow, K., Yang, J., ... & Canadian
Neonatal Network. (2018). Association of antibiotic utilization and neurodevelopmental
Reed, B. D., Schibler, K. R., Deshmukh, H., Ambalavanan, N., & Morrow, A. L. (2018). The
impact of maternal antibiotics on neonatal disease. The Journal of pediatrics, 197, 97-
103.
Samuels, N., van de Graaf, R., Been, J. V., De Jonge, R. C., Hanff, L. M., Wijnen, R. M., ... &
Vermeulen, M. J. (2016). Necrotising enterocolitis and mortality in preterm infants after
introduction of probiotics: a quasi-experimental study. Scientific reports, 6, 31643.
https://doi.org/10.1038/srep31643
Seale, J. V., Hutchinson, R. A., Fleming, P. F., Sinha, A., Kempley, S. T., Husain, S. M., &
Millar, M. R. (2018). Does antibiotic choice for the treatment of suspected late-onset
sepsis in premature infants determine the risk of developing necrotising enterocolitis? A
systematic review. Early human development, 123, 6-10.
Staude, B., Oehmke, F., Lauer, T., Behnke, J., Göpel, W., Schloter, M., ... & Ehrhardt, H. (2018).
The Microbiome and Preterm Birth: A Change in Paradigm with Profound Implications
for Pathophysiologic Concepts and Novel Therapeutic Strategies. BioMed research
international, 2018.
Stey, A., Barnert, E. S., Tseng, C. H., Keeler, E., Needleman, J., Leng, M., ... & Shew, S. B.
(2015). Outcomes and costs of surgical treatments of necrotizing
enterocolitis. Pediatrics, 135(5), e1190-e1197. doi: 10.1542/peds.2014-1058
Ting, J. Y., Synnes, A., Roberts, A., Deshpandey, A., Dow, K., Yoon, E. W., ... & Shah, P. S.
(2016). Association between antibiotic use and neonatal mortality and morbidities in very
low-birth-weight infants without culture-proven sepsis or necrotizing enterocolitis. JAMA
pediatrics, 170(12), 1181-1187. doi:10.1001/jamapediatrics.2016.2132
Ting, J. Y., Synnes, A., Roberts, A., Deshpandey, A. C., Dow, K., Yang, J., ... & Canadian
Neonatal Network. (2018). Association of antibiotic utilization and neurodevelopmental
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 26
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
