Impact of Breastfeeding Education on Neonatal Mortality in Rural India
VerifiedAdded on 2022/10/18
|17
|5464
|12
Report
AI Summary
This report details a randomized controlled trial investigating the impact of breastfeeding education, incorporating motivational interviews, on neonatal mortality rates in rural India. The study addresses the significant public health issue of suboptimal breastfeeding practices and their contribution to infant deaths, particularly in the first week of life. The research explores the current levels of knowledge and awareness among pregnant and lactating women regarding breastfeeding, aiming to improve their understanding and confidence through educational programs and motivational interviews. The study employs a pre- and post-intervention design, with participants randomized into intervention and control groups. The intervention group receives education and motivational interviews, while the control group receives standard care. The methodology includes the assessment of breastfeeding practices based on WHO criteria and the evaluation of outcomes such as the rate, frequency, and duration of breastfeeding, as well as neonatal mortality rates. Ethical considerations are addressed through informed consent, anonymity, and confidentiality. The report includes a detailed action plan, methodology, and variables, providing a comprehensive overview of the study's design and objectives, with the goal of promoting exclusive breastfeeding and reducing neonatal mortality in rural India.
Health Advancement and Promotion
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Title: Breastfeeding education with motivational interview and its impact on neonatal
mortality in rural India – A randomised controlled trial.
Background and rationale:
In rural India, sun-optimal breastfeeding is accounting for 1.4 million child death and 43.5
million Disability Adjusted Life Years (DALYs). Moreover, 77 % deaths and 85 % DALYs
occur due to non-exclusive breastfeeding. Approximately 50 % of these deaths occur in the
first week of life (Veeranki et al., 2017). Hypothermia and hypoglycaemia are the main
contributing factors for neonatal deaths attributable to non-exclusive breastfeeding.
Immediate breastfeeding followed by exclusive breastfeeding improve the health and survival
of the infants. In most of the developing countries including rural India, most of the late
neonatal deaths occur due to infectious diseases such as sepsis, acute respiratory tract
infection, meningitis, omphalitis and diarrhoea. Infants with adequate breastfeeding have
fewer rates of stomach problem, breathing problem, less ear infections, improved speech and
vision and overall physical and mental development. It is evident that colostrum feeding and
breastfeeding particularly breastfeeding protect against neonatal deaths (Mehta, Panneer,
Ghosh-Jerath, and Racine, 2017).
Breastfeeding should be analysed on the differential basis because it has been observed that
breastfeeding overstated in the urban mothers in comparison to the rural mothers. If
breastfeeding analysis performed for urban and rural mothers together, there are chances of
misreading analysis. Long duration impact of breastfeeding on overall growth and
development depends on the locality which means whether these mothers residing in urban or
rural India (Behera and Pillai, 2016). Mothers in the urban India are more educated in
comparison to the mothers in the rural India. Hence, urban mothers are more health conscious
about their children in comparison to the rural mothers. Education should be considered as
the important factor in the analysis of the impact of breastfeeding on the long-term health
outcomes. Since, health of children in rural India is not up to optimal level even though these
are adequately breastfed. It is mainly due to inadequate attention given by these mothers
towards health of these children (Oakley et al., 2017; Trojanowska, Brodowicz-Król, and
Trojanowska, 2017). Another factor which should be considered in the analysis of
breastfeeding is the duration of breastfeeding. There are chances that children with
heterogenous breastfeeding duration incorporated in the analysis of breastfeeding would
result in the variable conclusion and it would be difficult to make exact conclusion. Source of
2
mortality in rural India – A randomised controlled trial.
Background and rationale:
In rural India, sun-optimal breastfeeding is accounting for 1.4 million child death and 43.5
million Disability Adjusted Life Years (DALYs). Moreover, 77 % deaths and 85 % DALYs
occur due to non-exclusive breastfeeding. Approximately 50 % of these deaths occur in the
first week of life (Veeranki et al., 2017). Hypothermia and hypoglycaemia are the main
contributing factors for neonatal deaths attributable to non-exclusive breastfeeding.
Immediate breastfeeding followed by exclusive breastfeeding improve the health and survival
of the infants. In most of the developing countries including rural India, most of the late
neonatal deaths occur due to infectious diseases such as sepsis, acute respiratory tract
infection, meningitis, omphalitis and diarrhoea. Infants with adequate breastfeeding have
fewer rates of stomach problem, breathing problem, less ear infections, improved speech and
vision and overall physical and mental development. It is evident that colostrum feeding and
breastfeeding particularly breastfeeding protect against neonatal deaths (Mehta, Panneer,
Ghosh-Jerath, and Racine, 2017).
Breastfeeding should be analysed on the differential basis because it has been observed that
breastfeeding overstated in the urban mothers in comparison to the rural mothers. If
breastfeeding analysis performed for urban and rural mothers together, there are chances of
misreading analysis. Long duration impact of breastfeeding on overall growth and
development depends on the locality which means whether these mothers residing in urban or
rural India (Behera and Pillai, 2016). Mothers in the urban India are more educated in
comparison to the mothers in the rural India. Hence, urban mothers are more health conscious
about their children in comparison to the rural mothers. Education should be considered as
the important factor in the analysis of the impact of breastfeeding on the long-term health
outcomes. Since, health of children in rural India is not up to optimal level even though these
are adequately breastfed. It is mainly due to inadequate attention given by these mothers
towards health of these children (Oakley et al., 2017; Trojanowska, Brodowicz-Król, and
Trojanowska, 2017). Another factor which should be considered in the analysis of
breastfeeding is the duration of breastfeeding. There are chances that children with
heterogenous breastfeeding duration incorporated in the analysis of breastfeeding would
result in the variable conclusion and it would be difficult to make exact conclusion. Source of
2
data is also an important factor in the analysis of breastfeeding. It is evident that there is no
homogeneity in the data obtained from the mothers and social workers. Mothers with reduced
confidence are prone to inadequate breastfeeding which give inaccurate data. Inadequate
knowledge about accurate breastfeeding method is also responsible for inadequate
breastfeeding (Hvatum and Glavin, 2017).
Accurate outcome of breastfeeding programme can be achieved in the population where
inadequate breastfeeding is the major issue. Mothers of the rural India are also associated
with the inadequate breastfeeding; hence, this study is designed to implement in the mothers
of rural India. Breastfeeding health promotion should incorporate factors such as
improvement in the basic knowledge about breastfeeding, improvement in positive attitude of
different stakeholders for promotion of breastfeeding programme and provision of support
comprising of lactating groups and support to the working mothers with insufficient
maternity leave (Dinour and Szaro, 2017).
Pregnant women’s perceived importance for breastfeeding, intention for breastfeeding and
self-efficiency and self-confidence are being considered as the significant motivational
factors for maintaining breastfeeding. In the previous studies, it has been established that
proper counselling and support are necessary for initiation and maintenance of breastfeeding
practice (Leruth, Goodman, Bragg, and Gray, 2017). Moreover, education about the
importance of human milk and breastfeeding during early antenatal period would be helpful
in initiating and maintaining breastfeeding. In addition to the education, motivational
interview is an important aspect for initiating and maintaining breastfeeding. Motivational
interview is a unique approach comprised of instruction and advice which help to discover
and resolve uncertainty and to alter behavioural changes about breastfeeding. Motivational
interview improves self-motivation through identifying own problems, taking change actions
and believing change is possible. Meta-analysis and several controlled studies established that
motivational interview programme can significantly improve breastfeeding in lactating
mothers (Wilhelm, Aguirre, Koehler, and Rodehorst, 2015). Mellin, Poplawski, Gole, and
Mass., (2011) demonstrated that educational programme and educational protocol proved
beneficial in improving exclusive breastfeeding, knowledge, comfort level and attitudes of
lactating women towards breastfeeding. Patel and Patel, (2016) demonstrated that dedicated
lactation specialists can significantly improve the exclusive breastfeeding rates in lactating
mothers.
3
homogeneity in the data obtained from the mothers and social workers. Mothers with reduced
confidence are prone to inadequate breastfeeding which give inaccurate data. Inadequate
knowledge about accurate breastfeeding method is also responsible for inadequate
breastfeeding (Hvatum and Glavin, 2017).
Accurate outcome of breastfeeding programme can be achieved in the population where
inadequate breastfeeding is the major issue. Mothers of the rural India are also associated
with the inadequate breastfeeding; hence, this study is designed to implement in the mothers
of rural India. Breastfeeding health promotion should incorporate factors such as
improvement in the basic knowledge about breastfeeding, improvement in positive attitude of
different stakeholders for promotion of breastfeeding programme and provision of support
comprising of lactating groups and support to the working mothers with insufficient
maternity leave (Dinour and Szaro, 2017).
Pregnant women’s perceived importance for breastfeeding, intention for breastfeeding and
self-efficiency and self-confidence are being considered as the significant motivational
factors for maintaining breastfeeding. In the previous studies, it has been established that
proper counselling and support are necessary for initiation and maintenance of breastfeeding
practice (Leruth, Goodman, Bragg, and Gray, 2017). Moreover, education about the
importance of human milk and breastfeeding during early antenatal period would be helpful
in initiating and maintaining breastfeeding. In addition to the education, motivational
interview is an important aspect for initiating and maintaining breastfeeding. Motivational
interview is a unique approach comprised of instruction and advice which help to discover
and resolve uncertainty and to alter behavioural changes about breastfeeding. Motivational
interview improves self-motivation through identifying own problems, taking change actions
and believing change is possible. Meta-analysis and several controlled studies established that
motivational interview programme can significantly improve breastfeeding in lactating
mothers (Wilhelm, Aguirre, Koehler, and Rodehorst, 2015). Mellin, Poplawski, Gole, and
Mass., (2011) demonstrated that educational programme and educational protocol proved
beneficial in improving exclusive breastfeeding, knowledge, comfort level and attitudes of
lactating women towards breastfeeding. Patel and Patel, (2016) demonstrated that dedicated
lactation specialists can significantly improve the exclusive breastfeeding rates in lactating
mothers.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Breastfeeding not only improve the child’s health but also improve mother’s health and
mother-infant bonding. Hence, World Health Organisation (WHO) recommended exclusive
breastfeeding from birth to six months in addition to the age-appropriate breastfeeding and
complementary breastfeeding for more than two years. Most of the women are unable to
follow WHO recommendation mainly due to lack of knowledge of importance of
breastfeeding. Antenatal education is essential for improving breastfeeding. Systematic
review demonstrated that breastfeeding education is more beneficial as compared to the peer
counselling and lactation consultation. However, peer counselling and lactation consultation
can be implemented as complementary breastfeeding health promotion techniques. However,
there is no good evidence available from randomised controlled trials for demonstrating
superiority of breastfeeding educational programme over peer counselling and lactation
consultant. Hence, this study is undertaken to improve the understanding the effect of
breastfeeding education on frequency and duration of breastfeeding.
Research questions:
1. What is level of knowledge and awareness of pregnant and lactating women about
importance and process of breastfeeding in rural India ?
2. What is effect of improvement in the knowledge and awareness of pregnant and
lactating women on health outcome and mortality rate of neonates ?
Goals:
Short-term goals established for this research study comprise of augmentation of knowledge
about ideal breastfeeding practice and improved confidence about breastfeeding. Long-term
goals established for this comprise of improvement in rate, frequency and duration of
breastfeeding and reduction in the neonates mortality rate.
Aims and objectives:
Aim :
Aim of this breastfeeding health promotion programme was to promote exclusive
breastfeeding in pregnant women in rural India.
Objectives of breastfeeding promotion:
1. To provide education and training about breastfeeding to the pregnant women.
4
mother-infant bonding. Hence, World Health Organisation (WHO) recommended exclusive
breastfeeding from birth to six months in addition to the age-appropriate breastfeeding and
complementary breastfeeding for more than two years. Most of the women are unable to
follow WHO recommendation mainly due to lack of knowledge of importance of
breastfeeding. Antenatal education is essential for improving breastfeeding. Systematic
review demonstrated that breastfeeding education is more beneficial as compared to the peer
counselling and lactation consultation. However, peer counselling and lactation consultation
can be implemented as complementary breastfeeding health promotion techniques. However,
there is no good evidence available from randomised controlled trials for demonstrating
superiority of breastfeeding educational programme over peer counselling and lactation
consultant. Hence, this study is undertaken to improve the understanding the effect of
breastfeeding education on frequency and duration of breastfeeding.
Research questions:
1. What is level of knowledge and awareness of pregnant and lactating women about
importance and process of breastfeeding in rural India ?
2. What is effect of improvement in the knowledge and awareness of pregnant and
lactating women on health outcome and mortality rate of neonates ?
Goals:
Short-term goals established for this research study comprise of augmentation of knowledge
about ideal breastfeeding practice and improved confidence about breastfeeding. Long-term
goals established for this comprise of improvement in rate, frequency and duration of
breastfeeding and reduction in the neonates mortality rate.
Aims and objectives:
Aim :
Aim of this breastfeeding health promotion programme was to promote exclusive
breastfeeding in pregnant women in rural India.
Objectives of breastfeeding promotion:
1. To provide education and training about breastfeeding to the pregnant women.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2. To conduct motivational interview in pregnant women to improve exclusive
breastfeeding.
3. To assess and compare improvement in exclusive breastfeeding among control and
intervention group.
4. To assess conversion of predominant breastfeeding to exclusive breastfeeding.
Action plan:
Ethical consideration:
Ethical consideration is a vital component of the research study. Ethical consideration ensures
integrity, reliability and validity of the research. Research protocol for the conduction of the
study was prepared by the principal investigator and approved by the institutional human
ethics committee. Approval from the ethical committee ensures following policies and codes
of Institutional Review Board (IRB) at every step of the research study (Nicholson, 2015).
Information about the study was provided to the participants through verbal explanation and
through broacher. Written informed consent was taken from each participant. Ethical
standards were maintained through preserving anonymity and confidentiality of the
participants. Provision was made for the participants to withdraw from the study at time
point.
Plan:
It has been established that training and education to the women in the antenatal period is
more beneficial in improving outcome of breastfeeding programme. Hence, in this
programme women in the rural India incorporated in health promotion programme.
Breastfeeding was assessed in recruited participants based on the criteria of World Health
Organisation. Infant and Young Child Feeding (IYCF) practices comprised of different
categories of breastfeeding such as early initiation breastfeeding (children were put on breast
within one hour of birth), exclusive breastfeeding up to 6 months (children up to 6 months
were on breastfeeding only), predominant breastfeeding (children up to 5 months were on
breastfeeding along with other sources of nutrition like juice) and bottle feeding (children
with breastfeeding and nutrition using bottle with nipple up to 23 months of age) (Chaturvedi,
Nakkeeran, Doshi, Patel, and Bhagwat, 2014). In this study, exclusive breastfeeding
programme was considered.
5
breastfeeding.
3. To assess and compare improvement in exclusive breastfeeding among control and
intervention group.
4. To assess conversion of predominant breastfeeding to exclusive breastfeeding.
Action plan:
Ethical consideration:
Ethical consideration is a vital component of the research study. Ethical consideration ensures
integrity, reliability and validity of the research. Research protocol for the conduction of the
study was prepared by the principal investigator and approved by the institutional human
ethics committee. Approval from the ethical committee ensures following policies and codes
of Institutional Review Board (IRB) at every step of the research study (Nicholson, 2015).
Information about the study was provided to the participants through verbal explanation and
through broacher. Written informed consent was taken from each participant. Ethical
standards were maintained through preserving anonymity and confidentiality of the
participants. Provision was made for the participants to withdraw from the study at time
point.
Plan:
It has been established that training and education to the women in the antenatal period is
more beneficial in improving outcome of breastfeeding programme. Hence, in this
programme women in the rural India incorporated in health promotion programme.
Breastfeeding was assessed in recruited participants based on the criteria of World Health
Organisation. Infant and Young Child Feeding (IYCF) practices comprised of different
categories of breastfeeding such as early initiation breastfeeding (children were put on breast
within one hour of birth), exclusive breastfeeding up to 6 months (children up to 6 months
were on breastfeeding only), predominant breastfeeding (children up to 5 months were on
breastfeeding along with other sources of nutrition like juice) and bottle feeding (children
with breastfeeding and nutrition using bottle with nipple up to 23 months of age) (Chaturvedi,
Nakkeeran, Doshi, Patel, and Bhagwat, 2014). In this study, exclusive breastfeeding
programme was considered.
5
In addition to the education and training, other techniques such as prenatal care, lactation
consultant, peer support and counselling and social media and marketing were considered.
For prenatal care, pregnant women were selected from the Gynaecology department of PHC,
lactation consultants were recruited instantly after child birth, breastfeeding promotion was
demonstrated to the peers of the pregnant women and breastfeeding promotion was
advertised in the PHC and circulated through social media.
Methodology:
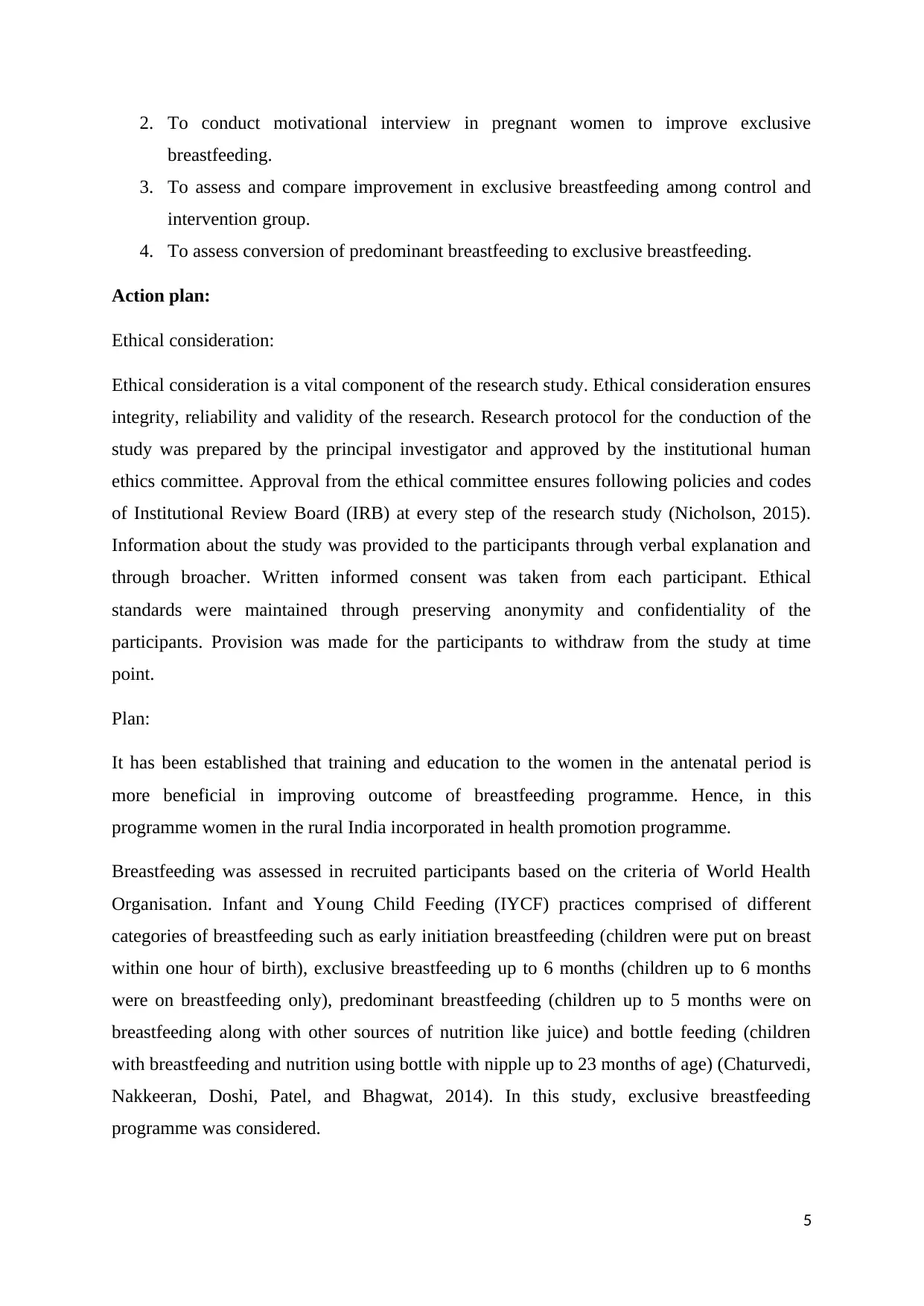
In the current study, randomised controlled research design was implemented with the pre
and post intervention design. Randomised controlled trial is beneficial in the evaluation of
effect of intervention on the outcome on the specific population with similar characteristics.
Participants are usually grouped in different groups based on the similar characteristics. In
randomised controlled trial, both the groups are usually subjected to similar type of
intervention to measure the similar outcome of interest. It is beneficial in the measuring
difference in the outcome of two groups after providing intervention. Randomised controlled
trials are the prospective studies with high scientific validity which provides best scientific
validity for the study. Randomised controlled trial is considered as the Gold standard study
designs which eliminate the chances of selection of bias. Randomised controlled trials
neutralises factors except dependent and independent variables; hence, it is useful in
measuring outcome in terms of cause and effect (Cook et al., 2015).
Sample and its size:
In this study, 550 mothers were assessed for participation in the study. Out of 550
participants, 500 participants were selected for the participation in the study based on the
inclusion and inclusion criteria. Written consent forms were taken from the selected
participants. Non-probability convenience sampling method was employed as a sampling
method. Non-probability convenience sampling method can be considered as the appropriate
method for the study because participants for the participation can be easily contacted and
easily reached (Chandler and Shapiro, 2016). 95 % of the recruited population were
considered with 95 % confidence level and 5 % confidence interval.
Inclusion criteria:
1. Women in their first pregnancy,
2. Being in 32nd gestational week,
6
consultant, peer support and counselling and social media and marketing were considered.
For prenatal care, pregnant women were selected from the Gynaecology department of PHC,
lactation consultants were recruited instantly after child birth, breastfeeding promotion was
demonstrated to the peers of the pregnant women and breastfeeding promotion was
advertised in the PHC and circulated through social media.
Methodology:
In the current study, randomised controlled research design was implemented with the pre
and post intervention design. Randomised controlled trial is beneficial in the evaluation of
effect of intervention on the outcome on the specific population with similar characteristics.
Participants are usually grouped in different groups based on the similar characteristics. In
randomised controlled trial, both the groups are usually subjected to similar type of
intervention to measure the similar outcome of interest. It is beneficial in the measuring
difference in the outcome of two groups after providing intervention. Randomised controlled
trials are the prospective studies with high scientific validity which provides best scientific
validity for the study. Randomised controlled trial is considered as the Gold standard study
designs which eliminate the chances of selection of bias. Randomised controlled trials
neutralises factors except dependent and independent variables; hence, it is useful in
measuring outcome in terms of cause and effect (Cook et al., 2015).
Sample and its size:
In this study, 550 mothers were assessed for participation in the study. Out of 550
participants, 500 participants were selected for the participation in the study based on the
inclusion and inclusion criteria. Written consent forms were taken from the selected
participants. Non-probability convenience sampling method was employed as a sampling
method. Non-probability convenience sampling method can be considered as the appropriate
method for the study because participants for the participation can be easily contacted and
easily reached (Chandler and Shapiro, 2016). 95 % of the recruited population were
considered with 95 % confidence level and 5 % confidence interval.
Inclusion criteria:
1. Women in their first pregnancy,
2. Being in 32nd gestational week,
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3. Being married,
4. Not working,
5. Without physical disabilities,
6. Not diagnosed chronic diseases and psychological disorders,
7. Not associated with risky pregnancy,
And
8. Not undergoing a planned cesarean section.
Education and Training methodology:
1. Pre-evaluation of knowledge about breastfeeding was conducted among participated
women through pre-defined questionnaires.
2. Planned education and training was provided for the recruited women keeping in
mind gaps in the knowledge. Training was provided through standardised module.
3. Theoretical information was provided and breastfeeding was provided through
different medias.
4. Training and education curriculum comprised of case-studies, participatory learning
methods, group discussions and direct teaching-learning through experts in the field.
5. Weekly monitoring of learning and reflection on previous schedule learning were
conducted.
6. Post-evaluation was conducted through assessment of parameters such as
improvement in the rate and frequency of breastfeeding and reduction in the neonates
mortality rates.
Randomisation:
Baseline characteristics of the participants were collected prior to the randomisation.
Randomisation was performed using grouped tabulated method with Microsoft excel.
Randomisation facilitate distribution of participants with identical baseline characteristics to
both interventional and control group. Baseline characteristics were decided based on the
knowledge of participants on breastfeeding. 250 participants each were distributed in
intervention and control group.
7
4. Not working,
5. Without physical disabilities,
6. Not diagnosed chronic diseases and psychological disorders,
7. Not associated with risky pregnancy,
And
8. Not undergoing a planned cesarean section.
Education and Training methodology:
1. Pre-evaluation of knowledge about breastfeeding was conducted among participated
women through pre-defined questionnaires.
2. Planned education and training was provided for the recruited women keeping in
mind gaps in the knowledge. Training was provided through standardised module.
3. Theoretical information was provided and breastfeeding was provided through
different medias.
4. Training and education curriculum comprised of case-studies, participatory learning
methods, group discussions and direct teaching-learning through experts in the field.
5. Weekly monitoring of learning and reflection on previous schedule learning were
conducted.
6. Post-evaluation was conducted through assessment of parameters such as
improvement in the rate and frequency of breastfeeding and reduction in the neonates
mortality rates.
Randomisation:
Baseline characteristics of the participants were collected prior to the randomisation.
Randomisation was performed using grouped tabulated method with Microsoft excel.
Randomisation facilitate distribution of participants with identical baseline characteristics to
both interventional and control group. Baseline characteristics were decided based on the
knowledge of participants on breastfeeding. 250 participants each were distributed in
intervention and control group.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
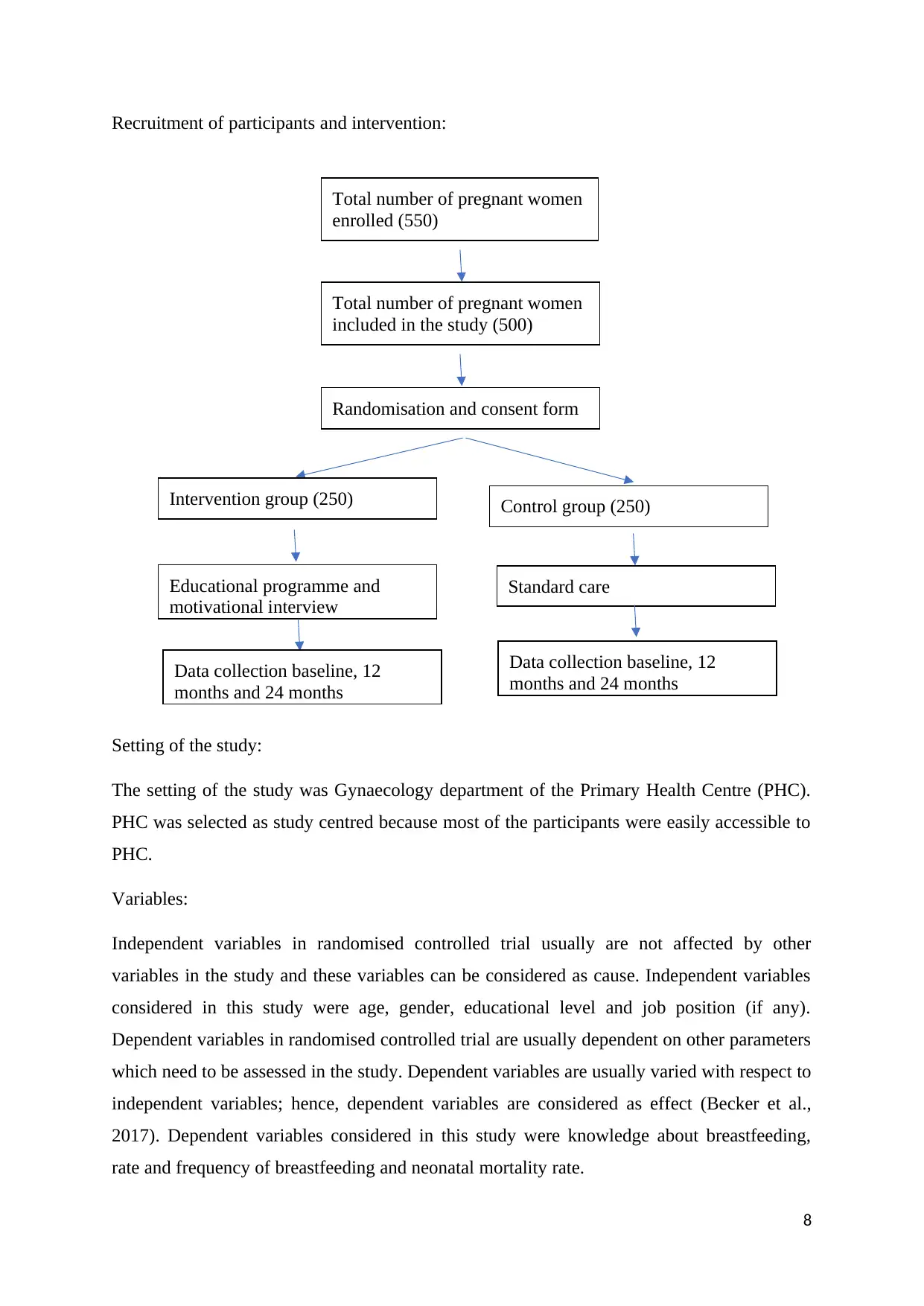
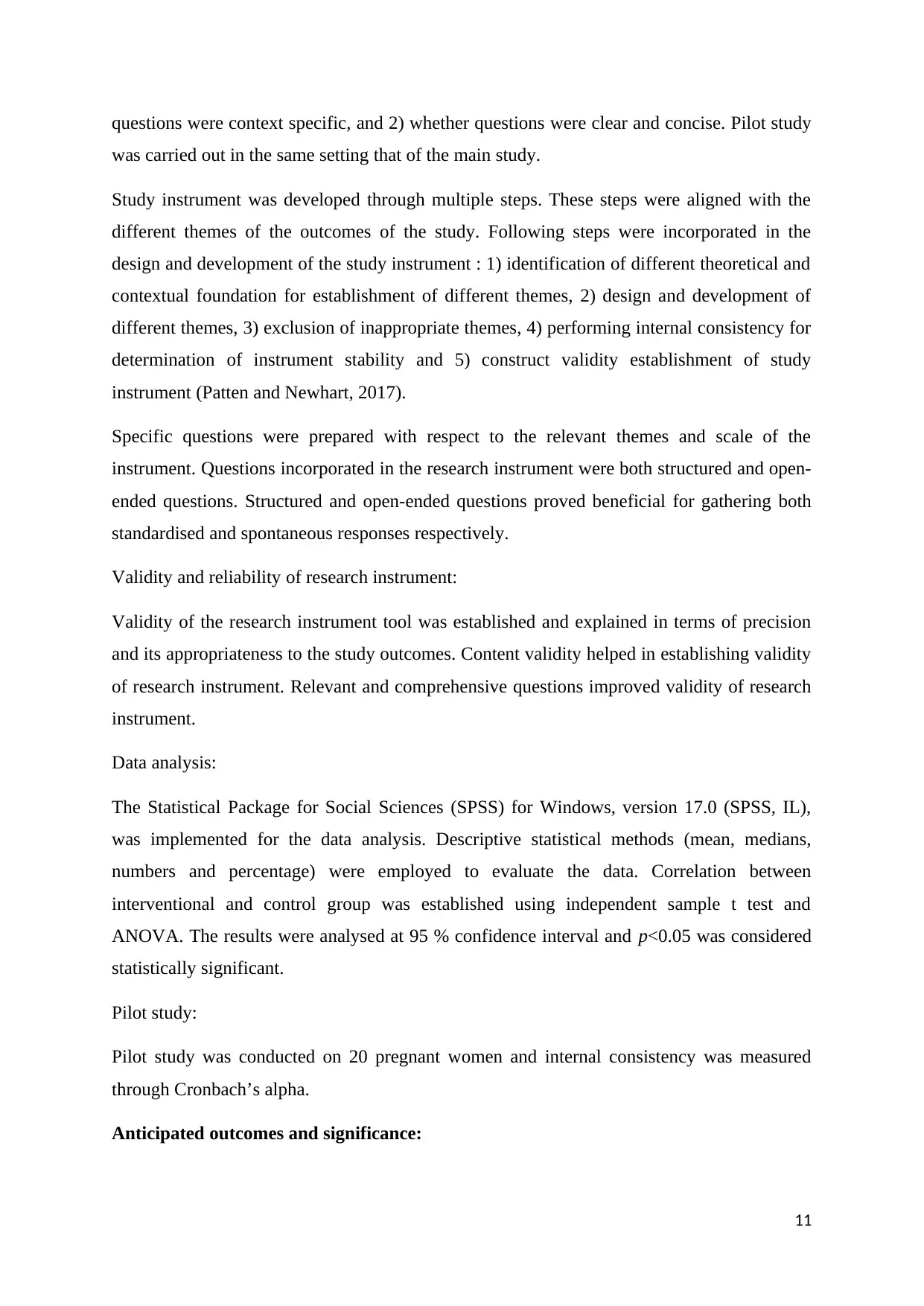
Recruitment of participants and intervention:
Setting of the study:
The setting of the study was Gynaecology department of the Primary Health Centre (PHC).
PHC was selected as study centred because most of the participants were easily accessible to
PHC.
Variables:
Independent variables in randomised controlled trial usually are not affected by other
variables in the study and these variables can be considered as cause. Independent variables
considered in this study were age, gender, educational level and job position (if any).
Dependent variables in randomised controlled trial are usually dependent on other parameters
which need to be assessed in the study. Dependent variables are usually varied with respect to
independent variables; hence, dependent variables are considered as effect (Becker et al.,
2017). Dependent variables considered in this study were knowledge about breastfeeding,
rate and frequency of breastfeeding and neonatal mortality rate.
8
Total number of pregnant women
enrolled (550)
Total number of pregnant women
included in the study (500)
Randomisation and consent form
Intervention group (250) Control group (250)
Educational programme and
motivational interview
Standard care
Data collection baseline, 12
months and 24 months
Data collection baseline, 12
months and 24 months
Setting of the study:
The setting of the study was Gynaecology department of the Primary Health Centre (PHC).
PHC was selected as study centred because most of the participants were easily accessible to
PHC.
Variables:
Independent variables in randomised controlled trial usually are not affected by other
variables in the study and these variables can be considered as cause. Independent variables
considered in this study were age, gender, educational level and job position (if any).
Dependent variables in randomised controlled trial are usually dependent on other parameters
which need to be assessed in the study. Dependent variables are usually varied with respect to
independent variables; hence, dependent variables are considered as effect (Becker et al.,
2017). Dependent variables considered in this study were knowledge about breastfeeding,
rate and frequency of breastfeeding and neonatal mortality rate.
8
Total number of pregnant women
enrolled (550)
Total number of pregnant women
included in the study (500)
Randomisation and consent form
Intervention group (250) Control group (250)
Educational programme and
motivational interview
Standard care
Data collection baseline, 12
months and 24 months
Data collection baseline, 12
months and 24 months
Data collection:
Data was collected by using different tools such as Antenatal Breastfeeding Self-efficacy
Scale (BSES)-Short Form, the Postnatal BSES-Short Form, the Infant Breastfeeding
Assessment Tool (IBFAT), the Antenatal Pregnant Women Information Form, the Postnatal
Maternal Information Form, and the BMP Rating Scale. These scales and tools were adopted
form the literature and senior researcher modified it according to the needs and requirements
of the study centre and participants of this study. Antenatal BSES-Short Form is the version
of the Postpartum BSES which comprises of 14 questions (Abuidhail, Mrayan, and Jaradat,
2019). Validity and reliability of Antenatal BSES-Short Form is found to be Cronbach’s
alpha of 0.87. Postnatal BSES-Short Form comprised of 14 questions and its validity and
reliability was found to be Cronbach’s alpha 0.86. Postnatal BSES-Short Form is useful in
evaluating extent feeling of mothers adequacy in breastfeeding. IBFAT scale which
comprises of six questions used for identifying limitations of breastfeeding self-efficiency
during breastfeeding of infants (Altuntas et al., 2014).
Antenatal pregnant women information form was prepared by the experienced researchers
though relevant literature. It consists of 7 questions which consists of socio-economic aspects
of the pregnant women. Postnatal maternal information from was prepared by the
experienced researcher through relevant literature. It consists of 10 questions comprised of
experience of obstetrical, breastfeeding and neonates characteristics. Breastfeeding
improvement programme (BIP) scale was created by the experienced researchers through
relevant literature. BIP scale mainly comprised of information related to 1) intention of
women regarding breastfeeding, 2) perceived importance of women about breastfeeding and
3) self-confidence and self-efficiency of women about breastfeeding. Data related to intention
of women was collected in terms of Yes or No. Data related to perceived importance and
self-confidence and self-efficacy was rated between 0 to 5 scale. Visual analog scale was
used for the collection of data (Cangöl and Şahin, 2017).
Data collection procedure:
The pregnant who attended Gynaecology department of PHC were assigned to intervention
and control groups based on the randomisation. Data was collected through different forms
such as Antenatal Pregnant Women Information Form, Antenatal BSES-Short Form, and the
BMP Rating Scale to both groups. Initially, data was collected for the participants in the
experimental group (Abuidhail, Mrayan, and Jaradat, 2019; Cangöl and Şahin, 2017).
9
Data was collected by using different tools such as Antenatal Breastfeeding Self-efficacy
Scale (BSES)-Short Form, the Postnatal BSES-Short Form, the Infant Breastfeeding
Assessment Tool (IBFAT), the Antenatal Pregnant Women Information Form, the Postnatal
Maternal Information Form, and the BMP Rating Scale. These scales and tools were adopted
form the literature and senior researcher modified it according to the needs and requirements
of the study centre and participants of this study. Antenatal BSES-Short Form is the version
of the Postpartum BSES which comprises of 14 questions (Abuidhail, Mrayan, and Jaradat,
2019). Validity and reliability of Antenatal BSES-Short Form is found to be Cronbach’s
alpha of 0.87. Postnatal BSES-Short Form comprised of 14 questions and its validity and
reliability was found to be Cronbach’s alpha 0.86. Postnatal BSES-Short Form is useful in
evaluating extent feeling of mothers adequacy in breastfeeding. IBFAT scale which
comprises of six questions used for identifying limitations of breastfeeding self-efficiency
during breastfeeding of infants (Altuntas et al., 2014).
Antenatal pregnant women information form was prepared by the experienced researchers
though relevant literature. It consists of 7 questions which consists of socio-economic aspects
of the pregnant women. Postnatal maternal information from was prepared by the
experienced researcher through relevant literature. It consists of 10 questions comprised of
experience of obstetrical, breastfeeding and neonates characteristics. Breastfeeding
improvement programme (BIP) scale was created by the experienced researchers through
relevant literature. BIP scale mainly comprised of information related to 1) intention of
women regarding breastfeeding, 2) perceived importance of women about breastfeeding and
3) self-confidence and self-efficiency of women about breastfeeding. Data related to intention
of women was collected in terms of Yes or No. Data related to perceived importance and
self-confidence and self-efficacy was rated between 0 to 5 scale. Visual analog scale was
used for the collection of data (Cangöl and Şahin, 2017).
Data collection procedure:
The pregnant who attended Gynaecology department of PHC were assigned to intervention
and control groups based on the randomisation. Data was collected through different forms
such as Antenatal Pregnant Women Information Form, Antenatal BSES-Short Form, and the
BMP Rating Scale to both groups. Initially, data was collected for the participants in the
experimental group (Abuidhail, Mrayan, and Jaradat, 2019; Cangöl and Şahin, 2017).
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Observational and clinical data was collected for the duration of 24 months. Data was
collected at baseline, at 12 months and at 24 months. Data at 12 and 24 months was collected
after implementation of education and training programme and motivational interview. Data
was mainly collected under two categories such as 1) assessment of knowledge and attitude
of pregnant and lactating women about breastfeeding before and after implementation of
intervention and 2) assessment of health improvement of neonates before and after
implementation of intervention.
1) Assessment of knowledge and attitude of pregnant and lactating women about
breastfeeding before and after implementation of intervention: Questionnaires were
circulated to participants of both control and intervention group. Nurses were assigned
to circulate questionnaires and collect the responses. Participants were asked to
complete the questionnaire in the PHC premises and fixed duration of 1 hr was given
for the completion of questionnaires. Questionnaires were provided to the participants
at the time of their visit to the PHC. Nurses who know the participants were not
allowed to collect the data due to chances of biasness in the data collection. Nurses
ensured that all the participants understand the questions and respond to it in an
effective manner.
2) Assessment of health improvement of neonates before and after implementation of
intervention: Data was collected in terms of evidence of different disease in the
children, outcome of disease in neonates and incidence of death in neonates.
Potential bias during data collection was addressed by incorporating below steps : 1)
validated questionnaire were incorporated which were based on the peer-reviewed literature,
2) categorisation of questions were based on the thematic categorisation; hence, dropout rate
of participants was less, and 3) questions incorporated in the study were aligned with
objective of the study.
Study instrument:
Study instrument was developed for collection of data. Study instrument was pre-tested for
reliability and validity of data collection. Prior to implementation in main study, study
instrument was pre-tested in pilot study comprising of a smaller number of participants.
Research instrument was approved by the experienced researcher after qualification in the
pilot study. Pre-testing of research instrument was carried out 1) for assessment of whether
10
collected at baseline, at 12 months and at 24 months. Data at 12 and 24 months was collected
after implementation of education and training programme and motivational interview. Data
was mainly collected under two categories such as 1) assessment of knowledge and attitude
of pregnant and lactating women about breastfeeding before and after implementation of
intervention and 2) assessment of health improvement of neonates before and after
implementation of intervention.
1) Assessment of knowledge and attitude of pregnant and lactating women about
breastfeeding before and after implementation of intervention: Questionnaires were
circulated to participants of both control and intervention group. Nurses were assigned
to circulate questionnaires and collect the responses. Participants were asked to
complete the questionnaire in the PHC premises and fixed duration of 1 hr was given
for the completion of questionnaires. Questionnaires were provided to the participants
at the time of their visit to the PHC. Nurses who know the participants were not
allowed to collect the data due to chances of biasness in the data collection. Nurses
ensured that all the participants understand the questions and respond to it in an
effective manner.
2) Assessment of health improvement of neonates before and after implementation of
intervention: Data was collected in terms of evidence of different disease in the
children, outcome of disease in neonates and incidence of death in neonates.
Potential bias during data collection was addressed by incorporating below steps : 1)
validated questionnaire were incorporated which were based on the peer-reviewed literature,
2) categorisation of questions were based on the thematic categorisation; hence, dropout rate
of participants was less, and 3) questions incorporated in the study were aligned with
objective of the study.
Study instrument:
Study instrument was developed for collection of data. Study instrument was pre-tested for
reliability and validity of data collection. Prior to implementation in main study, study
instrument was pre-tested in pilot study comprising of a smaller number of participants.
Research instrument was approved by the experienced researcher after qualification in the
pilot study. Pre-testing of research instrument was carried out 1) for assessment of whether
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
questions were context specific, and 2) whether questions were clear and concise. Pilot study
was carried out in the same setting that of the main study.
Study instrument was developed through multiple steps. These steps were aligned with the
different themes of the outcomes of the study. Following steps were incorporated in the
design and development of the study instrument : 1) identification of different theoretical and
contextual foundation for establishment of different themes, 2) design and development of
different themes, 3) exclusion of inappropriate themes, 4) performing internal consistency for
determination of instrument stability and 5) construct validity establishment of study
instrument (Patten and Newhart, 2017).
Specific questions were prepared with respect to the relevant themes and scale of the
instrument. Questions incorporated in the research instrument were both structured and open-
ended questions. Structured and open-ended questions proved beneficial for gathering both
standardised and spontaneous responses respectively.
Validity and reliability of research instrument:
Validity of the research instrument tool was established and explained in terms of precision
and its appropriateness to the study outcomes. Content validity helped in establishing validity
of research instrument. Relevant and comprehensive questions improved validity of research
instrument.
Data analysis:
The Statistical Package for Social Sciences (SPSS) for Windows, version 17.0 (SPSS, IL),
was implemented for the data analysis. Descriptive statistical methods (mean, medians,
numbers and percentage) were employed to evaluate the data. Correlation between
interventional and control group was established using independent sample t test and
ANOVA. The results were analysed at 95 % confidence interval and p˂0.05 was considered
statistically significant.
Pilot study:
Pilot study was conducted on 20 pregnant women and internal consistency was measured
through Cronbach’s alpha.
Anticipated outcomes and significance:
11
was carried out in the same setting that of the main study.
Study instrument was developed through multiple steps. These steps were aligned with the
different themes of the outcomes of the study. Following steps were incorporated in the
design and development of the study instrument : 1) identification of different theoretical and
contextual foundation for establishment of different themes, 2) design and development of
different themes, 3) exclusion of inappropriate themes, 4) performing internal consistency for
determination of instrument stability and 5) construct validity establishment of study
instrument (Patten and Newhart, 2017).
Specific questions were prepared with respect to the relevant themes and scale of the
instrument. Questions incorporated in the research instrument were both structured and open-
ended questions. Structured and open-ended questions proved beneficial for gathering both
standardised and spontaneous responses respectively.
Validity and reliability of research instrument:
Validity of the research instrument tool was established and explained in terms of precision
and its appropriateness to the study outcomes. Content validity helped in establishing validity
of research instrument. Relevant and comprehensive questions improved validity of research
instrument.
Data analysis:
The Statistical Package for Social Sciences (SPSS) for Windows, version 17.0 (SPSS, IL),
was implemented for the data analysis. Descriptive statistical methods (mean, medians,
numbers and percentage) were employed to evaluate the data. Correlation between
interventional and control group was established using independent sample t test and
ANOVA. The results were analysed at 95 % confidence interval and p˂0.05 was considered
statistically significant.
Pilot study:
Pilot study was conducted on 20 pregnant women and internal consistency was measured
through Cronbach’s alpha.
Anticipated outcomes and significance:
11
Sociodemographic characteristics of all the participants would be collected during the data
collection. Information about concern and issues of pregnant women about breastfeeding
would be collected. This information would be beneficial in addressing the specific issues
related to each woman. Moreover, information about the difference between the
interventional and control group would be gathered. Difference between the interventional
group and control group would confirm the effectiveness of intervention. Information about
the perceived importance and self-confidence and self-efficacy would be gathered.
Participants in the interventional group would be more intended to breastfed as compared to
control group; however, participants of the experimental interventional group would be more
anxious during breastfeeding. Anxiety in participants in interventional group participants
during breastfeeding might be due to first time breastfeeding and pressure of undergoing
training and education. Self-confidence and self-efficacy of participants of the experimental
group would be more in comparison to the control group participants because detailed
knowledge obtained regarding skills of breastfeeding. Difference in the number of
participants who breastfed in the first half-hour in control and interventional group wold be
assessed. This assessment would be helpful in understanding effectiveness of knowledge and
training provided to the participants of the interventional group. Difference in the rate and
frequency of breastfeeding among control and interventional group participants would be
evaluated. Based on the experience of researchers, it has been estimated that rate and
frequency of breastfeeding would be more in interventional group in comparison to the
control group participants. Rate of administration of supplementary food would be more in
control group in comparison to the interventional group. Additional supplementation of
supplementary food is not required in the interventional group because nutritional
requirements of neonates in interventional group can be effectively fulfilled through
breastfeeding alone. Average number of women and percentage of women from each group
can be calculated from this study. This information would be useful in assessing the
generalisation of the outcome of the study. Collected information about the exclusive
breastfeeding would be helpful in assessing the health status of neonates and its correlation
with breastfeeding. Weight loss in neonates in interventional group would be less in
comparison to the neonates in the control group. Moreover, mortality rate of neonates would
be less in interventional group as compared to the neonates in the control group. Information
related to the weight loss and mortality rate would be helpful in establishing relationship
between the exclusive breastfeeding and health of neonates.
12
collection. Information about concern and issues of pregnant women about breastfeeding
would be collected. This information would be beneficial in addressing the specific issues
related to each woman. Moreover, information about the difference between the
interventional and control group would be gathered. Difference between the interventional
group and control group would confirm the effectiveness of intervention. Information about
the perceived importance and self-confidence and self-efficacy would be gathered.
Participants in the interventional group would be more intended to breastfed as compared to
control group; however, participants of the experimental interventional group would be more
anxious during breastfeeding. Anxiety in participants in interventional group participants
during breastfeeding might be due to first time breastfeeding and pressure of undergoing
training and education. Self-confidence and self-efficacy of participants of the experimental
group would be more in comparison to the control group participants because detailed
knowledge obtained regarding skills of breastfeeding. Difference in the number of
participants who breastfed in the first half-hour in control and interventional group wold be
assessed. This assessment would be helpful in understanding effectiveness of knowledge and
training provided to the participants of the interventional group. Difference in the rate and
frequency of breastfeeding among control and interventional group participants would be
evaluated. Based on the experience of researchers, it has been estimated that rate and
frequency of breastfeeding would be more in interventional group in comparison to the
control group participants. Rate of administration of supplementary food would be more in
control group in comparison to the interventional group. Additional supplementation of
supplementary food is not required in the interventional group because nutritional
requirements of neonates in interventional group can be effectively fulfilled through
breastfeeding alone. Average number of women and percentage of women from each group
can be calculated from this study. This information would be useful in assessing the
generalisation of the outcome of the study. Collected information about the exclusive
breastfeeding would be helpful in assessing the health status of neonates and its correlation
with breastfeeding. Weight loss in neonates in interventional group would be less in
comparison to the neonates in the control group. Moreover, mortality rate of neonates would
be less in interventional group as compared to the neonates in the control group. Information
related to the weight loss and mortality rate would be helpful in establishing relationship
between the exclusive breastfeeding and health of neonates.
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


