Netherlands Euthanasia: Nursing Staff Attitudes, Decision Making
VerifiedAdded on 2023/06/14
|14
|6935
|353
Report
AI Summary
This report presents a nation-wide survey conducted in the Netherlands to explore the attitudes and involvement of nursing staff (registered nurses and certified nursing assistants) regarding euthanasia. The study, utilizing a pre-existing research panel, investigates nursing staff's views on decision-making processes, their actual involvement in the performance of euthanasia, and the relationship between their background characteristics and their attitudes and involvement. Key findings reveal that the majority of nursing staff desire involvement in decision-making processes related to euthanasia, but not all are aware of the legal limitations regarding their role in administering lethal drugs. The study emphasizes the need for informing nursing staff about relevant legislation and professional guidelines to ensure ethical and legally sound practices. The research employs descriptive statistics and multivariate logistic regression analyses to analyze the survey data collected from 587 respondents, providing valuable insights into the perspectives and experiences of nursing staff in the context of legalized euthanasia in the Netherlands.
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
Postprint
Version
1.0
Journal website http://linkinghub.elsevier.com/retrieve/pii/S0738-3991(15)30121-X
Pubmed link http://www.ncbi.nlm.nih.gov/pubmed/26613667
DOI 10.1016/j.pec.2015.11.008
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
Nursing staff and euthanasia in the Netherlands. A
nation-wide survey on attitudes and involvement in
decision making and the performance of
euthanasia
ANNEKE L. FRANCKEA, B, C, , , GWENDA ALBERSD, JOHAN BILSENE, ANKE J.E. DE VEERA, ,
BREGJE D. ONWUTEAKA-PHILIPSENB, C
a NIVEL—Netherlands Institute of Health Services Research, Utrecht, The Netherlands
b Department of Public and Occupational Health, EMGO Institute for Health and Care
Research, VU Medical Center, Amsterdam, The Netherlands
c Expertise Center for Palliative Care Amsterdam, VU Medical Center, Amsterdam, The
Netherlands
d Federation Palliative Care Flanders, Vilvoorde, Belgium
e Mental Health and Wellbeing Research Group, Department of Public Health, Vrije
Universiteit Brussel, Belgium
ABSTRACT
Objectives: To give insight into Dutch nursing staff’s attitudes and involvement
regarding euthanasia.
Methods: The sample was recruited from a nation-wide existent research panel
of registered nurses and certified nursing assistants. Descriptive analyses and
multivariate logistic regression analyses were performed.
Results: 587 respondents (response of 65%) completed the questionnaire. The
majority (83%) state that physicians have to discuss the decision about
euthanasia with the nurses involved. Besides, 69% state that a physician should
discuss a euthanasia request with nurses who have regular contact with a patient.
Nursing staff who have religious or other beliefs that they consider important for
their attitude towards end-of-life decisions, and staff working in a hospital or
home care, are most likely to have this opinion. Being present during the
euthanasia is quite unusual: only a small group (7%) report that this has ever
been the case in their entire working life. Seven% (incorrectly) think they are
allowed to administer the lethal drugs.
Conclusion: The majority want to be involved in decision-making processes
about euthanasia. Not all are aware that they are not legally allowed to
administer the lethal drugs.
Practice implications: Nursing staff should be informed of relevant existing
legislation and professional guidelines.
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
Postprint
Version
1.0
Journal website http://linkinghub.elsevier.com/retrieve/pii/S0738-3991(15)30121-X
Pubmed link http://www.ncbi.nlm.nih.gov/pubmed/26613667
DOI 10.1016/j.pec.2015.11.008
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
Nursing staff and euthanasia in the Netherlands. A
nation-wide survey on attitudes and involvement in
decision making and the performance of
euthanasia
ANNEKE L. FRANCKEA, B, C, , , GWENDA ALBERSD, JOHAN BILSENE, ANKE J.E. DE VEERA, ,
BREGJE D. ONWUTEAKA-PHILIPSENB, C
a NIVEL—Netherlands Institute of Health Services Research, Utrecht, The Netherlands
b Department of Public and Occupational Health, EMGO Institute for Health and Care
Research, VU Medical Center, Amsterdam, The Netherlands
c Expertise Center for Palliative Care Amsterdam, VU Medical Center, Amsterdam, The
Netherlands
d Federation Palliative Care Flanders, Vilvoorde, Belgium
e Mental Health and Wellbeing Research Group, Department of Public Health, Vrije
Universiteit Brussel, Belgium
ABSTRACT
Objectives: To give insight into Dutch nursing staff’s attitudes and involvement
regarding euthanasia.
Methods: The sample was recruited from a nation-wide existent research panel
of registered nurses and certified nursing assistants. Descriptive analyses and
multivariate logistic regression analyses were performed.
Results: 587 respondents (response of 65%) completed the questionnaire. The
majority (83%) state that physicians have to discuss the decision about
euthanasia with the nurses involved. Besides, 69% state that a physician should
discuss a euthanasia request with nurses who have regular contact with a patient.
Nursing staff who have religious or other beliefs that they consider important for
their attitude towards end-of-life decisions, and staff working in a hospital or
home care, are most likely to have this opinion. Being present during the
euthanasia is quite unusual: only a small group (7%) report that this has ever
been the case in their entire working life. Seven% (incorrectly) think they are
allowed to administer the lethal drugs.
Conclusion: The majority want to be involved in decision-making processes
about euthanasia. Not all are aware that they are not legally allowed to
administer the lethal drugs.
Practice implications: Nursing staff should be informed of relevant existing
legislation and professional guidelines.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
1. INTRODUCTION
As of 2002, euthanasia in the Netherlands has been regulated by the Termination of
Life on Request and Assisted Suicide Act, often called the ‘euthanasia act’ [1]. In the
‘80s’ and ‘90s’ of the previous century, euthanasia practices were still a crime
according to the Dutch Penal code. However, due to the development of
jurisprudence, Dutch courts tolerated if a physician had performed the euthanasia in
an unbearably suffering patient with a voluntary euthanasia request, and after
consultation with an independent physician [2]. In the euthanasia act – and
accordingly in this paper – euthanasia is defined as the administering of lethal drugs
by a physician with the explicit intention to end a patient’s life at the patient’s
explicit request. Comparable euthanasia acts exist in Belgium and Luxembourg.
The legal conditions and actual practice of euthanasia in the aforementioned
countries have been the subject of much international debate [3]. Yet there are no
indications that after euthanasia has been made legal, the number of euthanasia cases
increased. In 2010, of all deaths in the Netherlands, 2.8% were the result of
euthanasia. This rate is comparable with those in 2001 and 1995 [4]. Euthanasia is
only possible in The Netherlands under very strict conditions. Only physicians are
legally allowed to give lethal drugs to terminate the life of a patient, and only when
criteria of due care are met [1]. In addition, only physicians have the legal authority
to make the decision to perform euthanasia and they are also the only persons who
are allowed to administer the lethal drugs. Nursing staff, or other non-doctors who
administer lethal drugs, risk prosecution and disciplinary measures.
Nonetheless, nursing staff often have frequent and close contacts with patients at the
end of life. They may therefore be confronted with patients with a euthanasia request
and could be one of the first people with whom the patient discusses the euthanasia
request [5]. Only the Belgian euthanasia act, however, pays attention to the nursing
role in the decision-making process, stating that the physician has to discuss the
euthanasia request with the nursing team involved in the care for the patient.
Although the role of nursing staff is not described in the Dutch euthanasia act, this
role is clarified and demarcated in the professional guidelines of the Dutch national
nurses’ and physicians’ associations [6] and [7]. These guidelines also recommend
that if nursing staff (registered nurses or certified nursing assistants) are involved in
the daily care of a patient with a euthanasia request, they should also be involved in
decision-making. In addition, the guidelines clearly state that nursing staff are not
allowed to administer the lethal drugs. Nursing staff are advised that if they are
present during the administration of euthanasia, they should only perform tasks
whereby at least one other act must follow to end the life of the patient [7]. This
means, for example, that a registered nurse or a certified nursing assistant may
prepare the lethal drugs when a physician asks them to do so, but they should never
turn on the drip valve or perform other actions directly resulting in the death of the
patient.
Six relevant international literature reviews shed some light on nursing staff’s
attitudes and involvement regarding euthanasia [5], [8], [9], [10], [11] and [12].
Some of the international reviews focused on attitudes regarding euthanasia, and on
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
1. INTRODUCTION
As of 2002, euthanasia in the Netherlands has been regulated by the Termination of
Life on Request and Assisted Suicide Act, often called the ‘euthanasia act’ [1]. In the
‘80s’ and ‘90s’ of the previous century, euthanasia practices were still a crime
according to the Dutch Penal code. However, due to the development of
jurisprudence, Dutch courts tolerated if a physician had performed the euthanasia in
an unbearably suffering patient with a voluntary euthanasia request, and after
consultation with an independent physician [2]. In the euthanasia act – and
accordingly in this paper – euthanasia is defined as the administering of lethal drugs
by a physician with the explicit intention to end a patient’s life at the patient’s
explicit request. Comparable euthanasia acts exist in Belgium and Luxembourg.
The legal conditions and actual practice of euthanasia in the aforementioned
countries have been the subject of much international debate [3]. Yet there are no
indications that after euthanasia has been made legal, the number of euthanasia cases
increased. In 2010, of all deaths in the Netherlands, 2.8% were the result of
euthanasia. This rate is comparable with those in 2001 and 1995 [4]. Euthanasia is
only possible in The Netherlands under very strict conditions. Only physicians are
legally allowed to give lethal drugs to terminate the life of a patient, and only when
criteria of due care are met [1]. In addition, only physicians have the legal authority
to make the decision to perform euthanasia and they are also the only persons who
are allowed to administer the lethal drugs. Nursing staff, or other non-doctors who
administer lethal drugs, risk prosecution and disciplinary measures.
Nonetheless, nursing staff often have frequent and close contacts with patients at the
end of life. They may therefore be confronted with patients with a euthanasia request
and could be one of the first people with whom the patient discusses the euthanasia
request [5]. Only the Belgian euthanasia act, however, pays attention to the nursing
role in the decision-making process, stating that the physician has to discuss the
euthanasia request with the nursing team involved in the care for the patient.
Although the role of nursing staff is not described in the Dutch euthanasia act, this
role is clarified and demarcated in the professional guidelines of the Dutch national
nurses’ and physicians’ associations [6] and [7]. These guidelines also recommend
that if nursing staff (registered nurses or certified nursing assistants) are involved in
the daily care of a patient with a euthanasia request, they should also be involved in
decision-making. In addition, the guidelines clearly state that nursing staff are not
allowed to administer the lethal drugs. Nursing staff are advised that if they are
present during the administration of euthanasia, they should only perform tasks
whereby at least one other act must follow to end the life of the patient [7]. This
means, for example, that a registered nurse or a certified nursing assistant may
prepare the lethal drugs when a physician asks them to do so, but they should never
turn on the drip valve or perform other actions directly resulting in the death of the
patient.
Six relevant international literature reviews shed some light on nursing staff’s
attitudes and involvement regarding euthanasia [5], [8], [9], [10], [11] and [12].
Some of the international reviews focused on attitudes regarding euthanasia, and on
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
factors affecting these attitudes. For instance, the Gielen et al. review [10] found a
relationship between staff’s religious beliefs or world view and negative attitudes
regarding euthanasia. The review of Verpoort et al. [11] also pointed to an influence
of religion, besides other influential background characteristics: nursing staff with a
strong religious faith, older nurses and those with many contacts with terminally ill
patients appeared to be more likely to oppose euthanasia. The most recent review, the
one by Vézina-Im et al. [12], however, found no significant relationship between
having religious beliefs and attitudes regarding euthanasia in more than half of the
studies included in their review, which contradicts the earlier reviews of Gielen et al.
[10] and Verpoort et al. [11].
Hence the relationship between nurses’ characteristics and attitudes is addressed, but
the relationship between nurses’ characteristics and actual euthanasia practices is
absent in existent reviews. Nevertheless, the international review of De Beer et al. [5]
revealed that nursing staff are often involved in decision making, but also on some
occasions in the actual administration of the lethal drugs. Furthermore, the review of
De Beer et al. included a Dutch study of Muller et al. published in 1997 [13], in
which general practitioners and nursing-home physicians indicated that nursing staff
administered the lethal drug(s) to the patients in 4% and 3% of the euthanasia cases
respectively; the corresponding figure for medical specialists in hospitals was 21%.
The aforementioned six literature reviews included just a small number of research
publications of Dutch origin, despite the fact that euthanasia policy and practices in
the Netherlands have received much international attention. After going through all
the reference lists in the reviews, we could identify only six underlying Dutch studies
addressing nursing staff’s attitudes or practices in relation to euthanasia [13], [14],
[15], [16], [17] and [18]. However, data collection in all these studies was performed
before or around the year 2002 (the year when the Dutch euthanasia act came into
force). Hence these studies do not give a topical picture anymore. Therefore this
paper addresses the following research questions:
1. What views and attitudes do Dutch nursing staff have regarding involvement
in decision making about euthanasia and regarding involvement in the actual
performance of euthanasia?
2. To what extent and in what way are Dutch nursing staff actually involved in
decision making about euthanasia and the performance of euthanasia?
3. What is the relationship between the background characteristics of nursing
staff on the one hand and attitudes and involvement in the performance of euthanasia
on the other hand?
2. METHODS
2.1. Sample
The study sample was recruited from a pre-existing national research sample of
nursing staff in the Netherlands, hereinafter referred to as the Nursing Staff Panel
[19] and [20]. This panel consists of a permanent group of registered nurses (RNs)
and certified nursing assistants (CNAs) who are prepared to fill in questionnaires on
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
factors affecting these attitudes. For instance, the Gielen et al. review [10] found a
relationship between staff’s religious beliefs or world view and negative attitudes
regarding euthanasia. The review of Verpoort et al. [11] also pointed to an influence
of religion, besides other influential background characteristics: nursing staff with a
strong religious faith, older nurses and those with many contacts with terminally ill
patients appeared to be more likely to oppose euthanasia. The most recent review, the
one by Vézina-Im et al. [12], however, found no significant relationship between
having religious beliefs and attitudes regarding euthanasia in more than half of the
studies included in their review, which contradicts the earlier reviews of Gielen et al.
[10] and Verpoort et al. [11].
Hence the relationship between nurses’ characteristics and attitudes is addressed, but
the relationship between nurses’ characteristics and actual euthanasia practices is
absent in existent reviews. Nevertheless, the international review of De Beer et al. [5]
revealed that nursing staff are often involved in decision making, but also on some
occasions in the actual administration of the lethal drugs. Furthermore, the review of
De Beer et al. included a Dutch study of Muller et al. published in 1997 [13], in
which general practitioners and nursing-home physicians indicated that nursing staff
administered the lethal drug(s) to the patients in 4% and 3% of the euthanasia cases
respectively; the corresponding figure for medical specialists in hospitals was 21%.
The aforementioned six literature reviews included just a small number of research
publications of Dutch origin, despite the fact that euthanasia policy and practices in
the Netherlands have received much international attention. After going through all
the reference lists in the reviews, we could identify only six underlying Dutch studies
addressing nursing staff’s attitudes or practices in relation to euthanasia [13], [14],
[15], [16], [17] and [18]. However, data collection in all these studies was performed
before or around the year 2002 (the year when the Dutch euthanasia act came into
force). Hence these studies do not give a topical picture anymore. Therefore this
paper addresses the following research questions:
1. What views and attitudes do Dutch nursing staff have regarding involvement
in decision making about euthanasia and regarding involvement in the actual
performance of euthanasia?
2. To what extent and in what way are Dutch nursing staff actually involved in
decision making about euthanasia and the performance of euthanasia?
3. What is the relationship between the background characteristics of nursing
staff on the one hand and attitudes and involvement in the performance of euthanasia
on the other hand?
2. METHODS
2.1. Sample
The study sample was recruited from a pre-existing national research sample of
nursing staff in the Netherlands, hereinafter referred to as the Nursing Staff Panel
[19] and [20]. This panel consists of a permanent group of registered nurses (RNs)
and certified nursing assistants (CNAs) who are prepared to fill in questionnaires on
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
current topics in nursing care. The age and gender distribution of the members of the
Nursing Staff Panel corresponds to the age and gender distribution of the total Dutch
nursing staff population. Participation is voluntary and anonymous.
RNs and CNAs are both nursing staff members. Compared to CNAs in most other
countries, Dutch CNAs go through a rather lengthy vocational education programme
lasting three years. Dutch RNs comprise nursing staff educated to associate degree
level (3–3.5 years of basic nursing education) or bachelor’s degree (4 years of basic
nursing education).
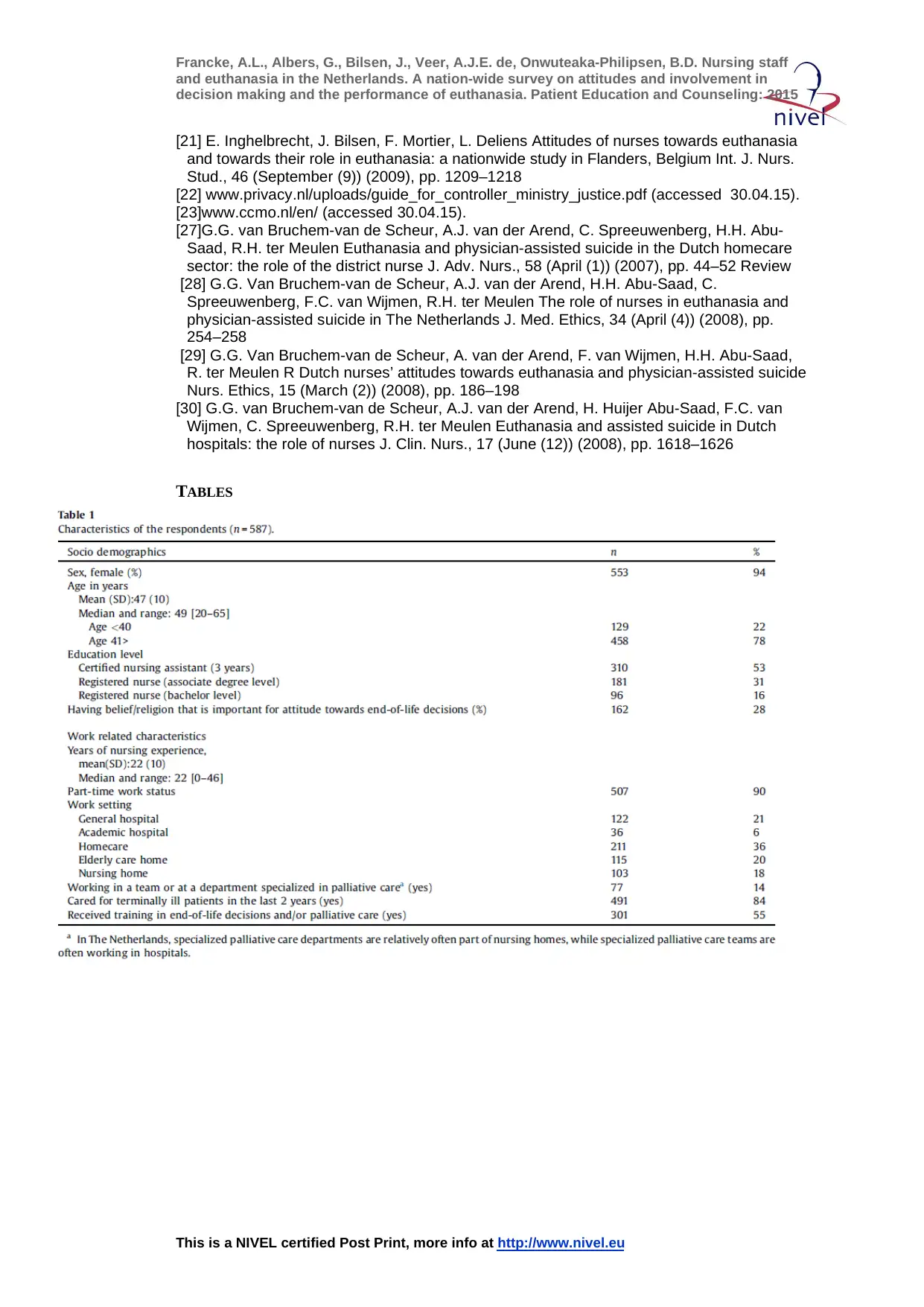
2.2. Data collection
In 2011, all 903 participants in the Nursing Staff Panel who worked in general or
academic hospitals, home care, nursing homes or elderly care homes were sent a
survey questionnaire by post. If no response was received within two weeks, a
reminder was posted, and – if needed – two weeks later again. Besides some
background characteristics (see Table 1), the questionnaire addressed attitudes
regarding euthanasia. The statements about attitudes (see Table 2) were all derived
from an existing survey questionnaire developed, tested and used in research in
Flanders, the Dutch-language part of Belgium [21]. This existent questionnaire was
based on literature study, consultation of experts, focus group discussions and pilot-
testing [21]. The participants were asked to what extent they agreed with each
statement about attitudes, by choosing between five response categories (1 = strongly
disagree; 2 = disagree; 3 = neutral; 4 = agree; 5 = strongly agree).
[TABLE 1][TABLE 2]
Another part of the questionnaire contained self-developed items regarding actual
involvement in decision making and the performance of euthanasia (see Table 3).
The content validity of these self-developed items was based on study of relevant
literature (among which the professional guidelines on euthanasia [6] and [7]), and
by discussing them within a group of experts (a lawyer, an ethicist, a nurse/nursing
scientist and a health scientist).
[TABLE 3. ]
2.3. ANALYSIS
Descriptive statistics were used to describe the background characteristics of
respondents and to answer the research questions numbers 1 and 2. Prior to these
descriptive analyses, the five response categories for the statements about attitudes
were condensed into three categories (1 = agree or strongly agree; 2 = neutral;
3 = disagree or strongly disagree).
In order to answer research question number 3, a backward multiple logistic
regression (with removal at p < 0.05) was performed and odds ratios and 95%
confidence intervals were calculated. Three core items from the survey questionnaire
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
current topics in nursing care. The age and gender distribution of the members of the
Nursing Staff Panel corresponds to the age and gender distribution of the total Dutch
nursing staff population. Participation is voluntary and anonymous.
RNs and CNAs are both nursing staff members. Compared to CNAs in most other
countries, Dutch CNAs go through a rather lengthy vocational education programme
lasting three years. Dutch RNs comprise nursing staff educated to associate degree
level (3–3.5 years of basic nursing education) or bachelor’s degree (4 years of basic
nursing education).
2.2. Data collection
In 2011, all 903 participants in the Nursing Staff Panel who worked in general or
academic hospitals, home care, nursing homes or elderly care homes were sent a
survey questionnaire by post. If no response was received within two weeks, a
reminder was posted, and – if needed – two weeks later again. Besides some
background characteristics (see Table 1), the questionnaire addressed attitudes
regarding euthanasia. The statements about attitudes (see Table 2) were all derived
from an existing survey questionnaire developed, tested and used in research in
Flanders, the Dutch-language part of Belgium [21]. This existent questionnaire was
based on literature study, consultation of experts, focus group discussions and pilot-
testing [21]. The participants were asked to what extent they agreed with each
statement about attitudes, by choosing between five response categories (1 = strongly
disagree; 2 = disagree; 3 = neutral; 4 = agree; 5 = strongly agree).
[TABLE 1][TABLE 2]
Another part of the questionnaire contained self-developed items regarding actual
involvement in decision making and the performance of euthanasia (see Table 3).
The content validity of these self-developed items was based on study of relevant
literature (among which the professional guidelines on euthanasia [6] and [7]), and
by discussing them within a group of experts (a lawyer, an ethicist, a nurse/nursing
scientist and a health scientist).
[TABLE 3. ]
2.3. ANALYSIS
Descriptive statistics were used to describe the background characteristics of
respondents and to answer the research questions numbers 1 and 2. Prior to these
descriptive analyses, the five response categories for the statements about attitudes
were condensed into three categories (1 = agree or strongly agree; 2 = neutral;
3 = disagree or strongly disagree).
In order to answer research question number 3, a backward multiple logistic
regression (with removal at p < 0.05) was performed and odds ratios and 95%
confidence intervals were calculated. Three core items from the survey questionnaire
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
were used as dependent variables in these analyses; representing different important
aspects of attitudes and experiences of nursing staff, namely attitudes regarding
communication with doctors, professional boundaries, and actual involvement in
euthanasia decision-making (see Table 4). No dependant variable regarding actual
involvement in administration of euthanatics was chosen, since the number of
nursing staff involved in this was too small. We used two response categories for
each dependent variable, namely ‘agree or strongly agree’ or ‘yes’ versus the other
categories ‘neutral’, ‘disagree or strongly disagree’ or ‘no’.
[TABLE 4]
Background characteristics (see the top row in Table 4) were entered in the analysis
as independent variables. Then separate logistic regression models were fitted for
each dependent variable. All analyses were performed using SPSS 16.0.
2.4. Ethical aspects
All respondents received an information letter together with the survey questionnaire
explaining the aim of the study. The responses were stored and analysed
anonymously, in accordance with the Dutch act on the protection of personal data
[22]. Formal ethical approval of this study was not required under the applicable
Dutch legislation [23], since all respondents were competent individuals and this
survey study did not involve any interventions or treatments.
3. RESULTS
3.1. Response rate and characteristics
A total of 587 of the 903 participants who were sent the questionnaire completed the
questionnaire (response of 65%). Table 1 provides the participants’ background
characteristics.
3.2. Views and attitudes regarding involvement in decision making
The majority see a role for themselves in decision making about euthanasia: 69%
agree with the statement that the physician should discuss a request for euthanasia
with nurses who have regular contact with a patient (see Table 2). An even larger
group (83%) agree with the statement that physicians have to discuss the decision to
administer drugs in lethal doses with the nurses involved. Moreover, almost half
(46%) state that a patient is more likely to address a request for euthanasia to a nurse
than to a physician.
3.3. Views and attitudes regarding involvement in the performance of
euthanasia
Not all respondents are convinced that their colleagues are familiar with the relevant
legal rules: less than half (43%) agree with the statement that most nurses know
which actions they are allowed to perform in the case of euthanasia. However, also
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
were used as dependent variables in these analyses; representing different important
aspects of attitudes and experiences of nursing staff, namely attitudes regarding
communication with doctors, professional boundaries, and actual involvement in
euthanasia decision-making (see Table 4). No dependant variable regarding actual
involvement in administration of euthanatics was chosen, since the number of
nursing staff involved in this was too small. We used two response categories for
each dependent variable, namely ‘agree or strongly agree’ or ‘yes’ versus the other
categories ‘neutral’, ‘disagree or strongly disagree’ or ‘no’.
[TABLE 4]
Background characteristics (see the top row in Table 4) were entered in the analysis
as independent variables. Then separate logistic regression models were fitted for
each dependent variable. All analyses were performed using SPSS 16.0.
2.4. Ethical aspects
All respondents received an information letter together with the survey questionnaire
explaining the aim of the study. The responses were stored and analysed
anonymously, in accordance with the Dutch act on the protection of personal data
[22]. Formal ethical approval of this study was not required under the applicable
Dutch legislation [23], since all respondents were competent individuals and this
survey study did not involve any interventions or treatments.
3. RESULTS
3.1. Response rate and characteristics
A total of 587 of the 903 participants who were sent the questionnaire completed the
questionnaire (response of 65%). Table 1 provides the participants’ background
characteristics.
3.2. Views and attitudes regarding involvement in decision making
The majority see a role for themselves in decision making about euthanasia: 69%
agree with the statement that the physician should discuss a request for euthanasia
with nurses who have regular contact with a patient (see Table 2). An even larger
group (83%) agree with the statement that physicians have to discuss the decision to
administer drugs in lethal doses with the nurses involved. Moreover, almost half
(46%) state that a patient is more likely to address a request for euthanasia to a nurse
than to a physician.
3.3. Views and attitudes regarding involvement in the performance of
euthanasia
Not all respondents are convinced that their colleagues are familiar with the relevant
legal rules: less than half (43%) agree with the statement that most nurses know
which actions they are allowed to perform in the case of euthanasia. However, also
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
the respondents themselves do not all know that they are not legally allowed to
administer the lethal drugs: 75% give the correct response to the relevant statement
about whether administering drugs in case of euthanasia is a task that nurses are
allowed to perform, while 7% think they are allowed to administer the lethal drugs,
and another 18% give a ‘neutral’ answer, which might indicate that they are not quite
sure about the proper response. Regarding the willingness to administer euthanatics,
the answers vary: 33% agree with the statement that (s)he would in no case be
prepared to administer the drugs in lethal doses, while the other respondents give a
neutral answer (26%) or disagree with the statement (41%).
In addition, 18% agree with the statement that (s)he would be in no case prepared to
participate in the termination of a patient’s life, and 67% state that in the case of
euthanasia the nurse’s task is restricted to the care of the patient and his or her next
of kin.
3.4. Involvement in decision making
Twenty-four percent say that a physician has on at least one occasion involved them
in the decision making about a request for euthanasia, while a smaller group (12%)
say that they have experienced a situation where a patient with whom they had
regular contacts made a euthanasia request but the physician did not discuss this with
them. Respondents were also asked whether they had ever been the first person with
whom a patient discussed a request for euthanasia: about a third (38%) say that this
has indeed occurred. Also about a third (35%) say that they have informed a
physician about a patient’s request for euthanasia on at least one occasion. Only 3%
report that they have ever refused to participate in decision making regarding
euthanasia (see Table 3).
3.5. Involvement in the performance of euthanasia
Respondents were also asked whether they have ever (in their entire working life)
been present during the performance of euthanasia to assist the physician. A small
group (7%) indicate that this has indeed been the case. A small group (10%) also say
that they have been present to support the patient or relatives (see Table 3). In
addition, respondents were asked about involvement in the preparations for
euthanasia. Very few (3% or less) say that they have ever brought the lethal drugs
from the pharmacy, connected the infusion line, dissolved the drugs and/or prepared
the syringe. Finally, few respondents indicate that they have ever turned on the drip
valve (2%) or administered the lethal drugs (1%).
3.6. Relations with background characteristics
Table 4 shows that nursing staff who have religious or other beliefs that they
consider important for their attitude towards end-of-life decisions, and those who
work in an academic or general hospital or in home care are most likely to agree that
the physician has to discuss a patient’s euthanasia request with the nursing staff
involved in the care for the patient. In addition, those working in academic hospitals
are most likely to think that a nurse is allowed to administer the lethal drugs.
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
the respondents themselves do not all know that they are not legally allowed to
administer the lethal drugs: 75% give the correct response to the relevant statement
about whether administering drugs in case of euthanasia is a task that nurses are
allowed to perform, while 7% think they are allowed to administer the lethal drugs,
and another 18% give a ‘neutral’ answer, which might indicate that they are not quite
sure about the proper response. Regarding the willingness to administer euthanatics,
the answers vary: 33% agree with the statement that (s)he would in no case be
prepared to administer the drugs in lethal doses, while the other respondents give a
neutral answer (26%) or disagree with the statement (41%).
In addition, 18% agree with the statement that (s)he would be in no case prepared to
participate in the termination of a patient’s life, and 67% state that in the case of
euthanasia the nurse’s task is restricted to the care of the patient and his or her next
of kin.
3.4. Involvement in decision making
Twenty-four percent say that a physician has on at least one occasion involved them
in the decision making about a request for euthanasia, while a smaller group (12%)
say that they have experienced a situation where a patient with whom they had
regular contacts made a euthanasia request but the physician did not discuss this with
them. Respondents were also asked whether they had ever been the first person with
whom a patient discussed a request for euthanasia: about a third (38%) say that this
has indeed occurred. Also about a third (35%) say that they have informed a
physician about a patient’s request for euthanasia on at least one occasion. Only 3%
report that they have ever refused to participate in decision making regarding
euthanasia (see Table 3).
3.5. Involvement in the performance of euthanasia
Respondents were also asked whether they have ever (in their entire working life)
been present during the performance of euthanasia to assist the physician. A small
group (7%) indicate that this has indeed been the case. A small group (10%) also say
that they have been present to support the patient or relatives (see Table 3). In
addition, respondents were asked about involvement in the preparations for
euthanasia. Very few (3% or less) say that they have ever brought the lethal drugs
from the pharmacy, connected the infusion line, dissolved the drugs and/or prepared
the syringe. Finally, few respondents indicate that they have ever turned on the drip
valve (2%) or administered the lethal drugs (1%).
3.6. Relations with background characteristics
Table 4 shows that nursing staff who have religious or other beliefs that they
consider important for their attitude towards end-of-life decisions, and those who
work in an academic or general hospital or in home care are most likely to agree that
the physician has to discuss a patient’s euthanasia request with the nursing staff
involved in the care for the patient. In addition, those working in academic hospitals
are most likely to think that a nurse is allowed to administer the lethal drugs.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
Moreover, being a registered nurse, working in an academic or general hospital or in
a nursing home, having cared for terminally ill patients in the previous two years,
and working in a specialised palliative care team/department is associated with
having been actually involved in decisions concerning euthanasia (see Table 4).
4. DISCUSSION AND CONCLUSION
4.1. Discussion
The majority of the respondents consider it important to be involved in decision
making regarding euthanasia. Almost seven out of ten state that a physician should
discuss a request for euthanasia with nurses who have regular contact with a patient,
and even a larger group state that physicians have to discuss the decision to
administer drugs in lethal doses with the nurses involved. Almost none report that
they have ever refused to participate in decision making regarding euthanasia. The
results also show that a substantial proportion of nursing staff were actually involved
by a physician and/or by a patient in the decision-making process about euthanasia.
Nursing staff are rather often the first persons with whom a patient discusses a
request for euthanasia.
However, nursing staff’s views regarding the legal boundaries are sometimes
incorrect: 7% incorrectly think they are allowed to administer the lethal drugs. A
smaller group (1–2 %) have ever been actually involved in the actual administration
of euthanatics. Even though this concerns a small group, the latter finding is
remarkable since the Dutch euthanasia act is clear that only doctors may administer
euthanatics, under strict conditions of due care.
That nursing staff administer euthanatics in some cases is not new. In the
introduction section we already mentioned the international literature review of De
Beer et al. [5], indicating that nursing staff are on some occasions involved in the
actual administration of the lethal drugs, and also previous Dutch studies
[13] and [16] pointed into this direction. The Muller et al. study [13] published in
1997 showed that Dutch nursing staff administered the euthanatics in 3–21% of the
euthanasia cases, depending on the setting, while the research by Van Bruchem-Van
de Scheur published in 2004 [16], later also published in 2007 and 2008 [27], [28],
[29] and [30] established that nurses in the Netherlands administered the lethal drugs
in about 12% of the euthanasia cases (12.2%).
Our study was performed years after these previous Dutch studies, and about a
decade after this law came into force. Whether nurses are involved less frequently in
the administration of the lethal drugs now cannot be said with full certainty, since the
earlier studies used different research samples. Nonetheless, the percentages that we
found for the involvement of nurses in administering the medication are very low.
That might be partially due to the professional guidelines that have been published in
the last decade and which describe professional and legal boundaries [6] and [7].
However, we must take account of the fact that our results do not show whether the
reported involvement in administering lethal drugs was before of after the
introduction of these guidelines. Given the extended working experience of a
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
Moreover, being a registered nurse, working in an academic or general hospital or in
a nursing home, having cared for terminally ill patients in the previous two years,
and working in a specialised palliative care team/department is associated with
having been actually involved in decisions concerning euthanasia (see Table 4).
4. DISCUSSION AND CONCLUSION
4.1. Discussion
The majority of the respondents consider it important to be involved in decision
making regarding euthanasia. Almost seven out of ten state that a physician should
discuss a request for euthanasia with nurses who have regular contact with a patient,
and even a larger group state that physicians have to discuss the decision to
administer drugs in lethal doses with the nurses involved. Almost none report that
they have ever refused to participate in decision making regarding euthanasia. The
results also show that a substantial proportion of nursing staff were actually involved
by a physician and/or by a patient in the decision-making process about euthanasia.
Nursing staff are rather often the first persons with whom a patient discusses a
request for euthanasia.
However, nursing staff’s views regarding the legal boundaries are sometimes
incorrect: 7% incorrectly think they are allowed to administer the lethal drugs. A
smaller group (1–2 %) have ever been actually involved in the actual administration
of euthanatics. Even though this concerns a small group, the latter finding is
remarkable since the Dutch euthanasia act is clear that only doctors may administer
euthanatics, under strict conditions of due care.
That nursing staff administer euthanatics in some cases is not new. In the
introduction section we already mentioned the international literature review of De
Beer et al. [5], indicating that nursing staff are on some occasions involved in the
actual administration of the lethal drugs, and also previous Dutch studies
[13] and [16] pointed into this direction. The Muller et al. study [13] published in
1997 showed that Dutch nursing staff administered the euthanatics in 3–21% of the
euthanasia cases, depending on the setting, while the research by Van Bruchem-Van
de Scheur published in 2004 [16], later also published in 2007 and 2008 [27], [28],
[29] and [30] established that nurses in the Netherlands administered the lethal drugs
in about 12% of the euthanasia cases (12.2%).
Our study was performed years after these previous Dutch studies, and about a
decade after this law came into force. Whether nurses are involved less frequently in
the administration of the lethal drugs now cannot be said with full certainty, since the
earlier studies used different research samples. Nonetheless, the percentages that we
found for the involvement of nurses in administering the medication are very low.
That might be partially due to the professional guidelines that have been published in
the last decade and which describe professional and legal boundaries [6] and [7].
However, we must take account of the fact that our results do not show whether the
reported involvement in administering lethal drugs was before of after the
introduction of these guidelines. Given the extended working experience of a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
proportion of the respondents (see Table 1), the involvement may have been in some
occasions longer ago, even before euthanasia has been regulated by the euthanasia
act.
This paper also addresses the relationship between background characteristics and
relevant attitudes. In the introduction section we already referred to the recent
international literature review by Vézina-Im et al. [12] showing that religious beliefs
were not significantly related to attitudes regarding euthanasia in more than half of
the studies they included in their review, while in contrast studies included in the
international reviews of Gielen et al. [10] and Verpoort et al. [11] pointed fairly
unanimously to such an association. We also did find that nursing staff having
religious or other beliefs that they considered important for their attitudes towards
end-of-life decisions, were more likely to agree with the statement that a physician
should discuss euthanasia requests with them. In addition, nursing staff working in
academic hospitals were more often in agreement with the statement that
administering lethal drugs in the case of euthanasia is a task that nurses are allowed
to perform. This finding is probably connected to the fact that nurses working in
academic settings are very used to giving all kinds of medication by means of
infusions.
The study has methodological strengths as the use of a nation-wide research sample
of nursing staff and the relatively high response rate of 65%. Nevertheless we must
keep in mind that particularly in research on a sensitive topic such as euthanasia,
non-response can lead to bias. For example, it could be that nursing staff who have
administered euthanatics, which is a criminal offense, are more represented in the
non-response group.
Our quantitative approach also involves limitations, because we do not always know
how nursing staff interpreted some terms used. For instance, the finding that 18%
agree with the statement that (s)he would be in no case prepared to participate in the
termination of a patient’s life can be interpreted in different ways, since we cannot be
sure what respondents would regard as falling under ‘participation’: Another
limitation is that the survey results do not provide clear insights into the personal
reasons and moral considerations behind certain answers. To better interpret the
survey results, and to spread more light on the reasons why and circumstances in
which some nursing staff members are prepared to participate in euthanasia
practices, we recommend additional qualitative interviews. It is possible that the
reasons why nursing staff occasionally administer lethal drugs to patients with a
euthanasia request, not only concern a lack of knowledge about the legal limits.
Another possible reason may be that nurses find it difficult to refuse requests from
doctors to administer the lethal drugs.
4.2. Conclusion
The majority of Dutch nursing staff find that a physician should discuss a request for
euthanasia with nurses who have regular contact with the patient. Nursing staff who
have religious or other beliefs that they consider important for their attitudes towards
end-of-life decisions, or who are working in a hospital or home care setting are most
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
proportion of the respondents (see Table 1), the involvement may have been in some
occasions longer ago, even before euthanasia has been regulated by the euthanasia
act.
This paper also addresses the relationship between background characteristics and
relevant attitudes. In the introduction section we already referred to the recent
international literature review by Vézina-Im et al. [12] showing that religious beliefs
were not significantly related to attitudes regarding euthanasia in more than half of
the studies they included in their review, while in contrast studies included in the
international reviews of Gielen et al. [10] and Verpoort et al. [11] pointed fairly
unanimously to such an association. We also did find that nursing staff having
religious or other beliefs that they considered important for their attitudes towards
end-of-life decisions, were more likely to agree with the statement that a physician
should discuss euthanasia requests with them. In addition, nursing staff working in
academic hospitals were more often in agreement with the statement that
administering lethal drugs in the case of euthanasia is a task that nurses are allowed
to perform. This finding is probably connected to the fact that nurses working in
academic settings are very used to giving all kinds of medication by means of
infusions.
The study has methodological strengths as the use of a nation-wide research sample
of nursing staff and the relatively high response rate of 65%. Nevertheless we must
keep in mind that particularly in research on a sensitive topic such as euthanasia,
non-response can lead to bias. For example, it could be that nursing staff who have
administered euthanatics, which is a criminal offense, are more represented in the
non-response group.
Our quantitative approach also involves limitations, because we do not always know
how nursing staff interpreted some terms used. For instance, the finding that 18%
agree with the statement that (s)he would be in no case prepared to participate in the
termination of a patient’s life can be interpreted in different ways, since we cannot be
sure what respondents would regard as falling under ‘participation’: Another
limitation is that the survey results do not provide clear insights into the personal
reasons and moral considerations behind certain answers. To better interpret the
survey results, and to spread more light on the reasons why and circumstances in
which some nursing staff members are prepared to participate in euthanasia
practices, we recommend additional qualitative interviews. It is possible that the
reasons why nursing staff occasionally administer lethal drugs to patients with a
euthanasia request, not only concern a lack of knowledge about the legal limits.
Another possible reason may be that nurses find it difficult to refuse requests from
doctors to administer the lethal drugs.
4.2. Conclusion
The majority of Dutch nursing staff find that a physician should discuss a request for
euthanasia with nurses who have regular contact with the patient. Nursing staff who
have religious or other beliefs that they consider important for their attitudes towards
end-of-life decisions, or who are working in a hospital or home care setting are most
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
likely to have this opinion. In practice, nursing staff are often actually involved in
decision making. In contrast, being involved in the actual performance of euthanasia
is quite unusual, although not all nursing staff members are aware that they are not
legally allowed to administer the lethal drugs.
4.3. Practice implications
Nursing staff can make a significant contribution to the decision-making process, by
functioning as a communication partner of the patient and the doctor. Involvement in
euthanasia decision-making can be important to support patient and family.
However, nursing staff must also be aware that they are not allowed to administer the
lethal medication. All nursing staff must be acquainted with relevant existing
legislation and professional guidelines on euthanasia decision making and practices.
We recommend to address these issues in vocational training and continuing
education for RNs and CNAs, so that nursing staff take account of their professional
roles and boundaries in the care for people with a euthanasia request.
CONFLICTS OF INTEREST
None.
CONTRIBUTIONS OF THE AUTHOR
All authors have made substantial contributions to this paper.
- ALF contributed to: (1) the conception and design of the study, (2) analysis
and interpretation of data, (3) drafting the article; (4) final approval of the paper.
- GA contributed to: (1) the conception and design of the study, (2) analysis
and interpretation of data, (2) co-drafting the article, (3) final approval of the paper.
- JB contributed to: (1) the conception and design of the study, (2) revising the
manuscript critically, (3) final approval of the paper.
- AJEdeV contributed to (1) the conception and design of the study, (2)
acquisition of data, (3) analysis and interpretation of data, (3) revising the manuscript
critically, (4) final approval of the paper.
- BO-P contributed to (1) the conception and design of the study, (2) revising
the manuscript critically, (3) final approval of the paper.
REMOVAL OF PERSONAL IDENTIFIERS
I confirm all personal identifiers have been removed or disguised so the persons
described are not identifiable and cannot be identified through the details of the
story.
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
likely to have this opinion. In practice, nursing staff are often actually involved in
decision making. In contrast, being involved in the actual performance of euthanasia
is quite unusual, although not all nursing staff members are aware that they are not
legally allowed to administer the lethal drugs.
4.3. Practice implications
Nursing staff can make a significant contribution to the decision-making process, by
functioning as a communication partner of the patient and the doctor. Involvement in
euthanasia decision-making can be important to support patient and family.
However, nursing staff must also be aware that they are not allowed to administer the
lethal medication. All nursing staff must be acquainted with relevant existing
legislation and professional guidelines on euthanasia decision making and practices.
We recommend to address these issues in vocational training and continuing
education for RNs and CNAs, so that nursing staff take account of their professional
roles and boundaries in the care for people with a euthanasia request.
CONFLICTS OF INTEREST
None.
CONTRIBUTIONS OF THE AUTHOR
All authors have made substantial contributions to this paper.
- ALF contributed to: (1) the conception and design of the study, (2) analysis
and interpretation of data, (3) drafting the article; (4) final approval of the paper.
- GA contributed to: (1) the conception and design of the study, (2) analysis
and interpretation of data, (2) co-drafting the article, (3) final approval of the paper.
- JB contributed to: (1) the conception and design of the study, (2) revising the
manuscript critically, (3) final approval of the paper.
- AJEdeV contributed to (1) the conception and design of the study, (2)
acquisition of data, (3) analysis and interpretation of data, (3) revising the manuscript
critically, (4) final approval of the paper.
- BO-P contributed to (1) the conception and design of the study, (2) revising
the manuscript critically, (3) final approval of the paper.
REMOVAL OF PERSONAL IDENTIFIERS
I confirm all personal identifiers have been removed or disguised so the persons
described are not identifiable and cannot be identified through the details of the
story.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
FUNDING
This paper was written within the framework of a study funded by the Dutch
Ministry of Health who had no other involvement in the study than being the source
of funding.
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
FUNDING
This paper was written within the framework of a study funded by the Dutch
Ministry of Health who had no other involvement in the study than being the source
of funding.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
REFERENCES
[1] http://wetten.overheid.nl/BWBR0012410/geldigheidsdatum_23-10-2015 [Termination of
Life on Request and Assisted Suicide Act].
[2] S. Gevers Euthanasia law and practice in The Netherlands Br. Med. Bull., 52 (2) (1996),
pp. 326–333
[3] M.J. Shariff Assisted death and the slippery slope-finding clarity amid advocacy,
convergence, and complexity Curr. Oncol., 19 (June (3)) (2012), pp. 143–154
[4] B.D. Onwuteaka-Philipsen, A. Brinkman-Stoppelenburg, C. Penning, G.J. de Jong-Krul,
J.J. van Delden, A. van der Heide Trends in end-of-life practices before and after the
enactment of the euthanasia law in the Netherlands from 1990 to 2010: a repeated cross-
sectional survey Lancet, 380 (September (9845)) (2012), pp. 908–915
[5] T. De Beer, C. Gastmans, B. Dierckx de Casterlé Involvement of nurses in euthanasia: a
review of the literature J. Med. Ethics., 30 (October (5)) (2004), pp. 494–498
[6] AVVV, NU’91, KNMG, Handreiking voor samenwerking artsen, verpleegkundigen en
verzorgenden bij euthanasie. [Guide for collaboration between doctors, nurses and nursing
assistants regarding euthanasia] Utrecht: 2006.
[7] C. Vossen, Hoe handel je zorgvuldig bij euthanasie. Handreiking voor een goede
samenwerking tussen arts, verpleegkundige en verzorgende. [How you can act carefully
regarding euthanasia. Guide to good collaboration between doctor, nurse and nurse
assistant]. (V and VN). Van der Weij BV, Hilversum, 2007.
[8] M. Berghs, B. Dierckx De Casterle, C. Gastmans The complexity of nurses’ attitudes
toward euthanasia: a review of the literature J. Med. Ethics, 31 (8) (2005), pp. 441–446
[9] N. De Bal, C. Gastmans, B. Dierckx De Casterlé Nurses’ involvement in the care of
patients requesting euthanasia: a review of the literature Int. J. Nur. Stud., 45 (4) (2008),
pp. 626–644
[10]J. Gielen, S. van den Branden, B. Broeckaert Religion and nurses’ attitudes to
euthanasia and physician assisted suicide Nurs. Ethics, 16 (May (3)) (2009), pp. 303–318
[11] C. Verpoort, C. Gastmans, N. De Bal, B. Dierckx de Casterlé Nurses’ attitudes to
euthanasia: a review of the literature Nurs. Ethics, 11 (4) (2004), pp. 349–365 Review
[12] L.A. Vézina-Im, M. Lavoie, P. Krol, M. Olivier-D'Avignon Motivations of physicians and
nurses to practice voluntary euthanasia: a systematic review BMC Palliat Care, 13 (April 10
(1)) (2014), p. 20
[13] M.T. Muller, L. Pijnenborg, B.D. Onwuteaka-Philipsen, G. van der Wal, J.T. van Eijk
The role of the nurse in active euthanasia and physician-assisted suicide J. Adv. Nurs., 26
(1997), pp. 424–430
[14] M.L. Rurup, B.D. Onwuteaka-Philipsen, H.R. Pasman, M.W. Ribbe, G. van der Wal
Attitudes of physicians, nurses and relatives towards end-of-life decisions concerning
nursing home patients with dementia Patient Educ. Couns., 61 (2006), pp. 372–380
[15]A.M. The ‘Vanavond om 8 uur..’ Verpleegkundige dilemma's bij euthanasie en andere
beslissingen rond het levenseinde. [Tonight at 8 o'clock.. Nursing dilemmas in euthanasia
and other decisions at the end of life.] Houten: Bohn Stafleu Van Loghum, 1997.
[16] G.G. van Bruchem-van de Scheur, A.J. van der Arend, C., Spreeuwenberg, F. van
Wijmen, R.H. ter Meulen, De rol van verpleegkundigen bij medische beslissingen rond het
levenseinde. Verslag van een landelijk onderzoek naar betrokkenheid en praktijken [The
role of nurses in decision making at the end of life. Report of a national study about
involvement and practices], Utrecht: Uitgeverij De Tijdstroom 2004.
[17] A. van de Scheur, A. van der Arend The role of the nurse in euthanasia: a Dutch study
Nurs. Ethics, 5 (1998), pp. 497–508
[18] Y.M. van der Brug, J. de Lange, H. Philipsen Ervaringen van verpleegkundigen met
euthanasie bij aids-patienten: [Expereinces of nurses with euthanasia in AIDS patients]
Verpleegkunde, 11 (1996), pp. 143–155
[19] G. Albers, A.L. Francke, A.J. de Veer, J. Bilsen, B.D. Onwuteaka-Philipsen Attitudes of
nursing staff towards involvement in medical end-of-life decisions: a national survey study
Patient Educ. Couns., 94 (January (1)) (2014), pp. 4–9
[20] A.J. de Veer, A.L. Francke, E.P. Poortvliet Nurses’ involvement in end-of-life decisions
Cancer Nurs. May-Jun, 31 (May–June (3)) (2008), pp. 222–228
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
REFERENCES
[1] http://wetten.overheid.nl/BWBR0012410/geldigheidsdatum_23-10-2015 [Termination of
Life on Request and Assisted Suicide Act].
[2] S. Gevers Euthanasia law and practice in The Netherlands Br. Med. Bull., 52 (2) (1996),
pp. 326–333
[3] M.J. Shariff Assisted death and the slippery slope-finding clarity amid advocacy,
convergence, and complexity Curr. Oncol., 19 (June (3)) (2012), pp. 143–154
[4] B.D. Onwuteaka-Philipsen, A. Brinkman-Stoppelenburg, C. Penning, G.J. de Jong-Krul,
J.J. van Delden, A. van der Heide Trends in end-of-life practices before and after the
enactment of the euthanasia law in the Netherlands from 1990 to 2010: a repeated cross-
sectional survey Lancet, 380 (September (9845)) (2012), pp. 908–915
[5] T. De Beer, C. Gastmans, B. Dierckx de Casterlé Involvement of nurses in euthanasia: a
review of the literature J. Med. Ethics., 30 (October (5)) (2004), pp. 494–498
[6] AVVV, NU’91, KNMG, Handreiking voor samenwerking artsen, verpleegkundigen en
verzorgenden bij euthanasie. [Guide for collaboration between doctors, nurses and nursing
assistants regarding euthanasia] Utrecht: 2006.
[7] C. Vossen, Hoe handel je zorgvuldig bij euthanasie. Handreiking voor een goede
samenwerking tussen arts, verpleegkundige en verzorgende. [How you can act carefully
regarding euthanasia. Guide to good collaboration between doctor, nurse and nurse
assistant]. (V and VN). Van der Weij BV, Hilversum, 2007.
[8] M. Berghs, B. Dierckx De Casterle, C. Gastmans The complexity of nurses’ attitudes
toward euthanasia: a review of the literature J. Med. Ethics, 31 (8) (2005), pp. 441–446
[9] N. De Bal, C. Gastmans, B. Dierckx De Casterlé Nurses’ involvement in the care of
patients requesting euthanasia: a review of the literature Int. J. Nur. Stud., 45 (4) (2008),
pp. 626–644
[10]J. Gielen, S. van den Branden, B. Broeckaert Religion and nurses’ attitudes to
euthanasia and physician assisted suicide Nurs. Ethics, 16 (May (3)) (2009), pp. 303–318
[11] C. Verpoort, C. Gastmans, N. De Bal, B. Dierckx de Casterlé Nurses’ attitudes to
euthanasia: a review of the literature Nurs. Ethics, 11 (4) (2004), pp. 349–365 Review
[12] L.A. Vézina-Im, M. Lavoie, P. Krol, M. Olivier-D'Avignon Motivations of physicians and
nurses to practice voluntary euthanasia: a systematic review BMC Palliat Care, 13 (April 10
(1)) (2014), p. 20
[13] M.T. Muller, L. Pijnenborg, B.D. Onwuteaka-Philipsen, G. van der Wal, J.T. van Eijk
The role of the nurse in active euthanasia and physician-assisted suicide J. Adv. Nurs., 26
(1997), pp. 424–430
[14] M.L. Rurup, B.D. Onwuteaka-Philipsen, H.R. Pasman, M.W. Ribbe, G. van der Wal
Attitudes of physicians, nurses and relatives towards end-of-life decisions concerning
nursing home patients with dementia Patient Educ. Couns., 61 (2006), pp. 372–380
[15]A.M. The ‘Vanavond om 8 uur..’ Verpleegkundige dilemma's bij euthanasie en andere
beslissingen rond het levenseinde. [Tonight at 8 o'clock.. Nursing dilemmas in euthanasia
and other decisions at the end of life.] Houten: Bohn Stafleu Van Loghum, 1997.
[16] G.G. van Bruchem-van de Scheur, A.J. van der Arend, C., Spreeuwenberg, F. van
Wijmen, R.H. ter Meulen, De rol van verpleegkundigen bij medische beslissingen rond het
levenseinde. Verslag van een landelijk onderzoek naar betrokkenheid en praktijken [The
role of nurses in decision making at the end of life. Report of a national study about
involvement and practices], Utrecht: Uitgeverij De Tijdstroom 2004.
[17] A. van de Scheur, A. van der Arend The role of the nurse in euthanasia: a Dutch study
Nurs. Ethics, 5 (1998), pp. 497–508
[18] Y.M. van der Brug, J. de Lange, H. Philipsen Ervaringen van verpleegkundigen met
euthanasie bij aids-patienten: [Expereinces of nurses with euthanasia in AIDS patients]
Verpleegkunde, 11 (1996), pp. 143–155
[19] G. Albers, A.L. Francke, A.J. de Veer, J. Bilsen, B.D. Onwuteaka-Philipsen Attitudes of
nursing staff towards involvement in medical end-of-life decisions: a national survey study
Patient Educ. Couns., 94 (January (1)) (2014), pp. 4–9
[20] A.J. de Veer, A.L. Francke, E.P. Poortvliet Nurses’ involvement in end-of-life decisions
Cancer Nurs. May-Jun, 31 (May–June (3)) (2008), pp. 222–228
Francke, A.L., Albers, G., Bilsen, J., Veer, A.J.E. de, Onwuteaka-Philipsen, B.D. Nursing staff
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
[21] E. Inghelbrecht, J. Bilsen, F. Mortier, L. Deliens Attitudes of nurses towards euthanasia
and towards their role in euthanasia: a nationwide study in Flanders, Belgium Int. J. Nurs.
Stud., 46 (September (9)) (2009), pp. 1209–1218
[22] www.privacy.nl/uploads/guide_for_controller_ministry_justice.pdf (accessed 30.04.15).
[23]www.ccmo.nl/en/ (accessed 30.04.15).
[27]G.G. van Bruchem-van de Scheur, A.J. van der Arend, C. Spreeuwenberg, H.H. Abu-
Saad, R.H. ter Meulen Euthanasia and physician-assisted suicide in the Dutch homecare
sector: the role of the district nurse J. Adv. Nurs., 58 (April (1)) (2007), pp. 44–52 Review
[28] G.G. Van Bruchem-van de Scheur, A.J. van der Arend, H.H. Abu-Saad, C.
Spreeuwenberg, F.C. van Wijmen, R.H. ter Meulen The role of nurses in euthanasia and
physician-assisted suicide in The Netherlands J. Med. Ethics, 34 (April (4)) (2008), pp.
254–258
[29] G.G. Van Bruchem-van de Scheur, A. van der Arend, F. van Wijmen, H.H. Abu-Saad,
R. ter Meulen R Dutch nurses’ attitudes towards euthanasia and physician-assisted suicide
Nurs. Ethics, 15 (March (2)) (2008), pp. 186–198
[30] G.G. van Bruchem-van de Scheur, A.J. van der Arend, H. Huijer Abu-Saad, F.C. van
Wijmen, C. Spreeuwenberg, R.H. ter Meulen Euthanasia and assisted suicide in Dutch
hospitals: the role of nurses J. Clin. Nurs., 17 (June (12)) (2008), pp. 1618–1626
TABLES
and euthanasia in the Netherlands. A nation-wide survey on attitudes and involvement in
decision making and the performance of euthanasia. Patient Education and Counseling: 2015
This is a NIVEL certified Post Print, more info at http://www.nivel.eu
[21] E. Inghelbrecht, J. Bilsen, F. Mortier, L. Deliens Attitudes of nurses towards euthanasia
and towards their role in euthanasia: a nationwide study in Flanders, Belgium Int. J. Nurs.
Stud., 46 (September (9)) (2009), pp. 1209–1218
[22] www.privacy.nl/uploads/guide_for_controller_ministry_justice.pdf (accessed 30.04.15).
[23]www.ccmo.nl/en/ (accessed 30.04.15).
[27]G.G. van Bruchem-van de Scheur, A.J. van der Arend, C. Spreeuwenberg, H.H. Abu-
Saad, R.H. ter Meulen Euthanasia and physician-assisted suicide in the Dutch homecare
sector: the role of the district nurse J. Adv. Nurs., 58 (April (1)) (2007), pp. 44–52 Review
[28] G.G. Van Bruchem-van de Scheur, A.J. van der Arend, H.H. Abu-Saad, C.
Spreeuwenberg, F.C. van Wijmen, R.H. ter Meulen The role of nurses in euthanasia and
physician-assisted suicide in The Netherlands J. Med. Ethics, 34 (April (4)) (2008), pp.
254–258
[29] G.G. Van Bruchem-van de Scheur, A. van der Arend, F. van Wijmen, H.H. Abu-Saad,
R. ter Meulen R Dutch nurses’ attitudes towards euthanasia and physician-assisted suicide
Nurs. Ethics, 15 (March (2)) (2008), pp. 186–198
[30] G.G. van Bruchem-van de Scheur, A.J. van der Arend, H. Huijer Abu-Saad, F.C. van
Wijmen, C. Spreeuwenberg, R.H. ter Meulen Euthanasia and assisted suicide in Dutch
hospitals: the role of nurses J. Clin. Nurs., 17 (June (12)) (2008), pp. 1618–1626
TABLES
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.