Critical Analysis of Pediatric Epilepsy MRI Protocol in Neuroradiology
VerifiedAdded on 2023/06/03
|10
|2752
|193
Report
AI Summary
This report provides a critical analysis of a specific Magnetic Resonance Imaging (MRI) protocol used in pediatric neuroradiology for diagnosing epilepsy in children aged zero to nine years. It identifies the clinical significance and justification of the MRI protocol, emphasizing its role in pinpointing epileptogenic zones and underlying causes such as cortical malformations or temporal sclerosis. The methodology section details the specific sequences, scanning ranges, and slice sizes used, particularly highlighting the advantages of 3T Magnetom for its high resolution and efficiency. The discussion section compares MRI with other imaging techniques, addresses safety measures for pediatric patients and operators, and critically appraises the benefits and limitations of the MRI protocol. The analysis covers brain parts like intracranial arteries, brain stem, and parenchyma, explaining how MRI aids in detecting abnormalities. The report concludes by affirming MRI as an efficient and safe method for diagnosing epilepsy, while also acknowledging its limitations such as cost and time consumption.
MAGNETIC RESONANCE IMAGING PROTOCOL FOR EPILEPSY.
Introduction.
Magnetic resonance pediatric protocol for epilepsy is a combination of procedures specifically
designed for diagnosis of seizures in children of the age zero months to nine years. The range
and mode of scanning in this protocol differ depending on the part of brain being scanned.
(Donald, 2001).
Protocol identification.
In diagnosis of epilepsy, a specific magnetic resonance sequences are used to identify and map
the epileptogenic zones of the brain’s functional areas responsible for speech and movement.
This helps in establishing the disorders causing seizures such as cortical malformation or
underdevelopment and sclerosis of mesial temporal. This protocol considers the body size and
brain development of the child.
Clinical significance and justification of MRI protocol for epilepsy.
Magnetic resonance imaging as a diagnostic tool has great significance in clinical environment.
This include but not limited to production of cross-sectional images of body internal organs with
clear details which are important in providing required information for diagnosis. In addition, it
yields the highest diagnostic details within the shortest time possible. These properties of MRI
protocol are significant for diagnosing epilepsy because it is required to point out the underlying
symptoms which will be the causes of epilepsy in future that cannot be viewed from the known
causes during imaging process. This include such parts of brain as venous infarction form
thrombosis which are the new causes of seizures can only be scanned by MRI. The correct
details from scanning helps in setting up the proper medication approaches.
Methodology.
Epilepsy is a disorder related to neurological malfunctioning in the brain where there is failure in
the proper electrical functioning (Erasmo & Faan, 2018).
Epilepsy can be caused by a range of factors which has major effects on the brain. These include
extreme fever, stroke, brain tumor, oxygen deficiency, severe and chronic brain injury and
malformation of brain during pregnancy among other causes (Ramli, Rahmat, Lim, & Tan,
2015).
Introduction.
Magnetic resonance pediatric protocol for epilepsy is a combination of procedures specifically
designed for diagnosis of seizures in children of the age zero months to nine years. The range
and mode of scanning in this protocol differ depending on the part of brain being scanned.
(Donald, 2001).
Protocol identification.
In diagnosis of epilepsy, a specific magnetic resonance sequences are used to identify and map
the epileptogenic zones of the brain’s functional areas responsible for speech and movement.
This helps in establishing the disorders causing seizures such as cortical malformation or
underdevelopment and sclerosis of mesial temporal. This protocol considers the body size and
brain development of the child.
Clinical significance and justification of MRI protocol for epilepsy.
Magnetic resonance imaging as a diagnostic tool has great significance in clinical environment.
This include but not limited to production of cross-sectional images of body internal organs with
clear details which are important in providing required information for diagnosis. In addition, it
yields the highest diagnostic details within the shortest time possible. These properties of MRI
protocol are significant for diagnosing epilepsy because it is required to point out the underlying
symptoms which will be the causes of epilepsy in future that cannot be viewed from the known
causes during imaging process. This include such parts of brain as venous infarction form
thrombosis which are the new causes of seizures can only be scanned by MRI. The correct
details from scanning helps in setting up the proper medication approaches.
Methodology.
Epilepsy is a disorder related to neurological malfunctioning in the brain where there is failure in
the proper electrical functioning (Erasmo & Faan, 2018).
Epilepsy can be caused by a range of factors which has major effects on the brain. These include
extreme fever, stroke, brain tumor, oxygen deficiency, severe and chronic brain injury and
malformation of brain during pregnancy among other causes (Ramli, Rahmat, Lim, & Tan,
2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
To manage the epilepsy, a proper diagnosis should be carried out to identify the cause. Among
the methods used include blood test to check if there is any infectious disease, brain electrical
activity test using electroencephalogram and brain scan and imaging test using magnetic
resonance and imaging scan to check for any abnormalities in the brain such as brain tumors
(Erasmo & Faan, 2018).
Magnetic resonance pediatric protocol for epilepsy consists of specific sequence for diagnostic
purposes in children of nine years and below.
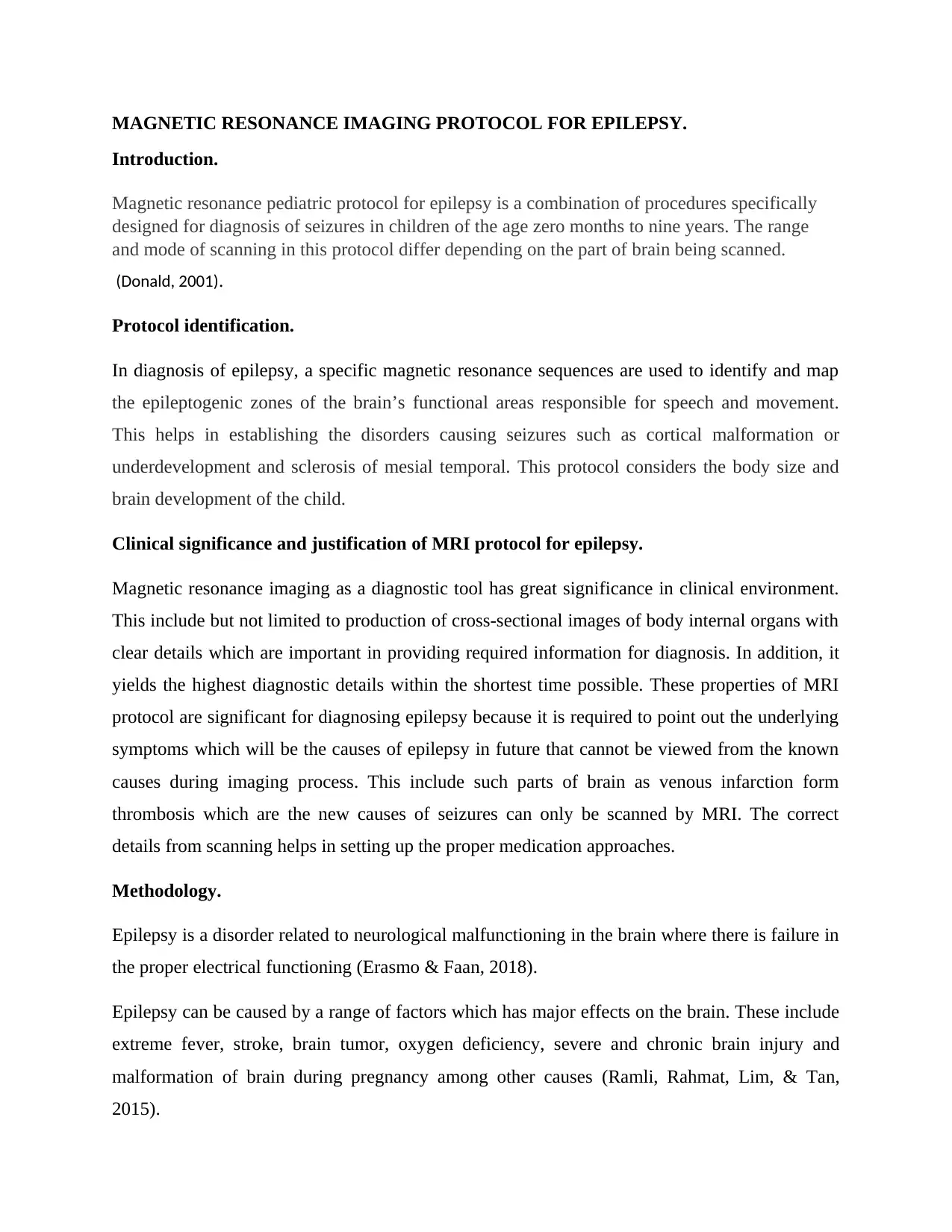
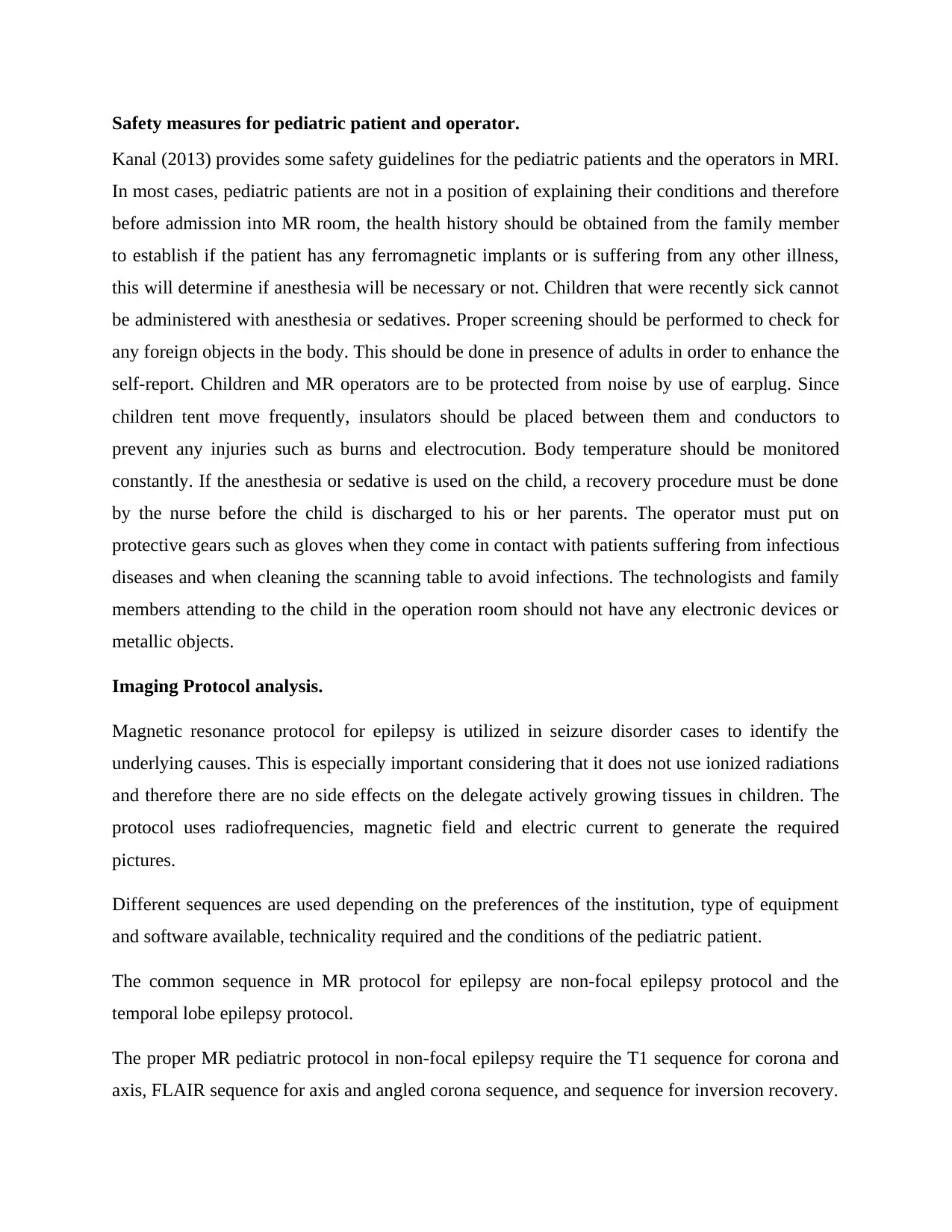
Scanning ranges, mode, slice and gap size differ depending on the body part being scanned.
Some of the specifications are as shown in figure 1 below (OHSU, 2014).
Figure 1. Magnetic resonance protocol for epilepsy in children of between zero months to
nine years in 3T.
the methods used include blood test to check if there is any infectious disease, brain electrical
activity test using electroencephalogram and brain scan and imaging test using magnetic
resonance and imaging scan to check for any abnormalities in the brain such as brain tumors
(Erasmo & Faan, 2018).
Magnetic resonance pediatric protocol for epilepsy consists of specific sequence for diagnostic
purposes in children of nine years and below.
Scanning ranges, mode, slice and gap size differ depending on the body part being scanned.
Some of the specifications are as shown in figure 1 below (OHSU, 2014).
Figure 1. Magnetic resonance protocol for epilepsy in children of between zero months to
nine years in 3T.

In children between the age of zero months and two years, the slice size used is three millimeters
while the gap size is one millimeter. In children of the age between two to nine years, the slice
used is four millimeters while the gap size is one millimeter.
Selection criteria.
The preferred method for epilepsy diagnosis in children is MRI protocol because they give
highly precise and specific details of internal body organs. This is important in ensuring proper
diagnosis (Trattnig, Pinker, Ba-Ssalamah, & Nobauer-Huhmann, 2016).
In the MRI technology, 3 Tesla Magnetom is the best for carrying out diagnosis of epilepsy. This
is because it has the highest and strongest magnetic field which goes up to 3T. This is stronger
compared to the 1.5 Tesla scanner which had a relatively low magnetic field strength. The
magnetic field strength is measured in Tesla(T). 3T Magnetom provides the highly detailed
anatomic information of the central nervous system with very clear images due to its high
resolution. This clarity makes diagnosis very easy. In addition to the strong magnetic field and
clear images, 3T Magnetom is highly efficient. it performs scanning quicker without a lot of
noise as compared to other MRI scanners. The quality services and patient’s safety are among
the criteria used in choosing the best protocol for diagnosing any illness (Lee, et al., 2017).
Protocol justification.
3T MR pediatric protocol for epilepsy has specific sequences which only work best on the
persons below ten years of age. This is due to their immature and small size anatomical parts.
This protocol is also advantageous as it gives three-dimensional pictures of the whole or part of
brain. Below are examples of photos from 3T MR pediatric protocol scanning process.
while the gap size is one millimeter. In children of the age between two to nine years, the slice
used is four millimeters while the gap size is one millimeter.
Selection criteria.
The preferred method for epilepsy diagnosis in children is MRI protocol because they give
highly precise and specific details of internal body organs. This is important in ensuring proper
diagnosis (Trattnig, Pinker, Ba-Ssalamah, & Nobauer-Huhmann, 2016).
In the MRI technology, 3 Tesla Magnetom is the best for carrying out diagnosis of epilepsy. This
is because it has the highest and strongest magnetic field which goes up to 3T. This is stronger
compared to the 1.5 Tesla scanner which had a relatively low magnetic field strength. The
magnetic field strength is measured in Tesla(T). 3T Magnetom provides the highly detailed
anatomic information of the central nervous system with very clear images due to its high
resolution. This clarity makes diagnosis very easy. In addition to the strong magnetic field and
clear images, 3T Magnetom is highly efficient. it performs scanning quicker without a lot of
noise as compared to other MRI scanners. The quality services and patient’s safety are among
the criteria used in choosing the best protocol for diagnosing any illness (Lee, et al., 2017).
Protocol justification.
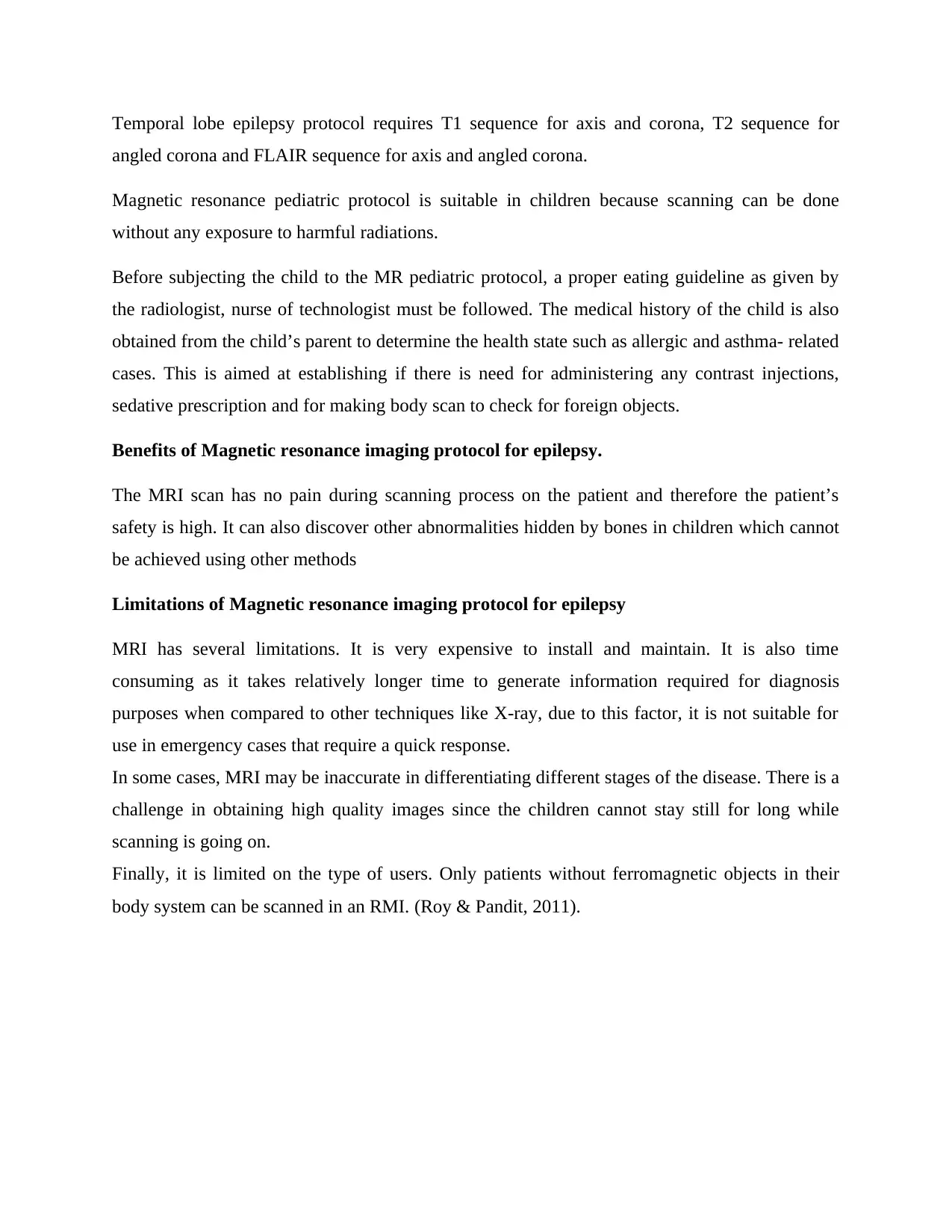
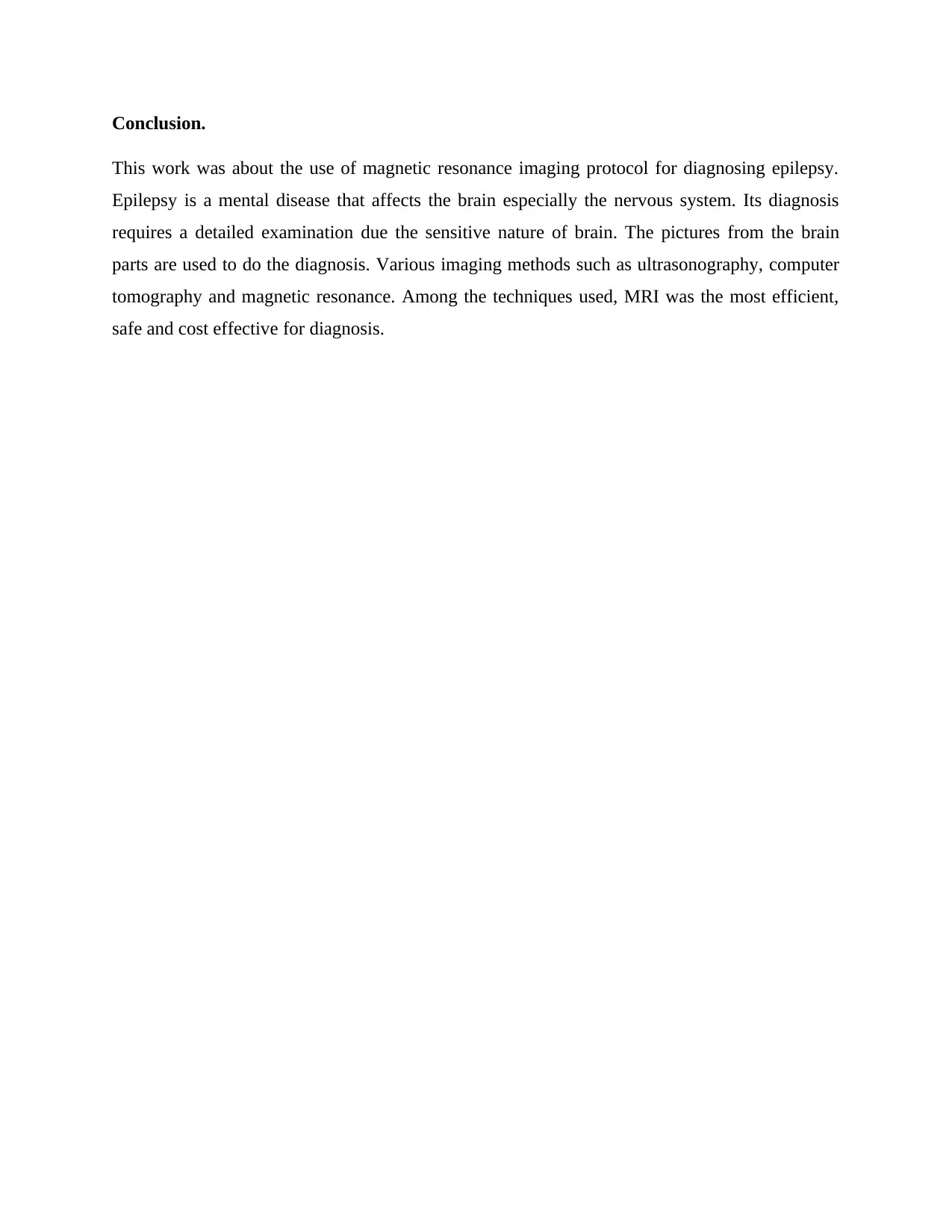
3T MR pediatric protocol for epilepsy has specific sequences which only work best on the
persons below ten years of age. This is due to their immature and small size anatomical parts.
This protocol is also advantageous as it gives three-dimensional pictures of the whole or part of
brain. Below are examples of photos from 3T MR pediatric protocol scanning process.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
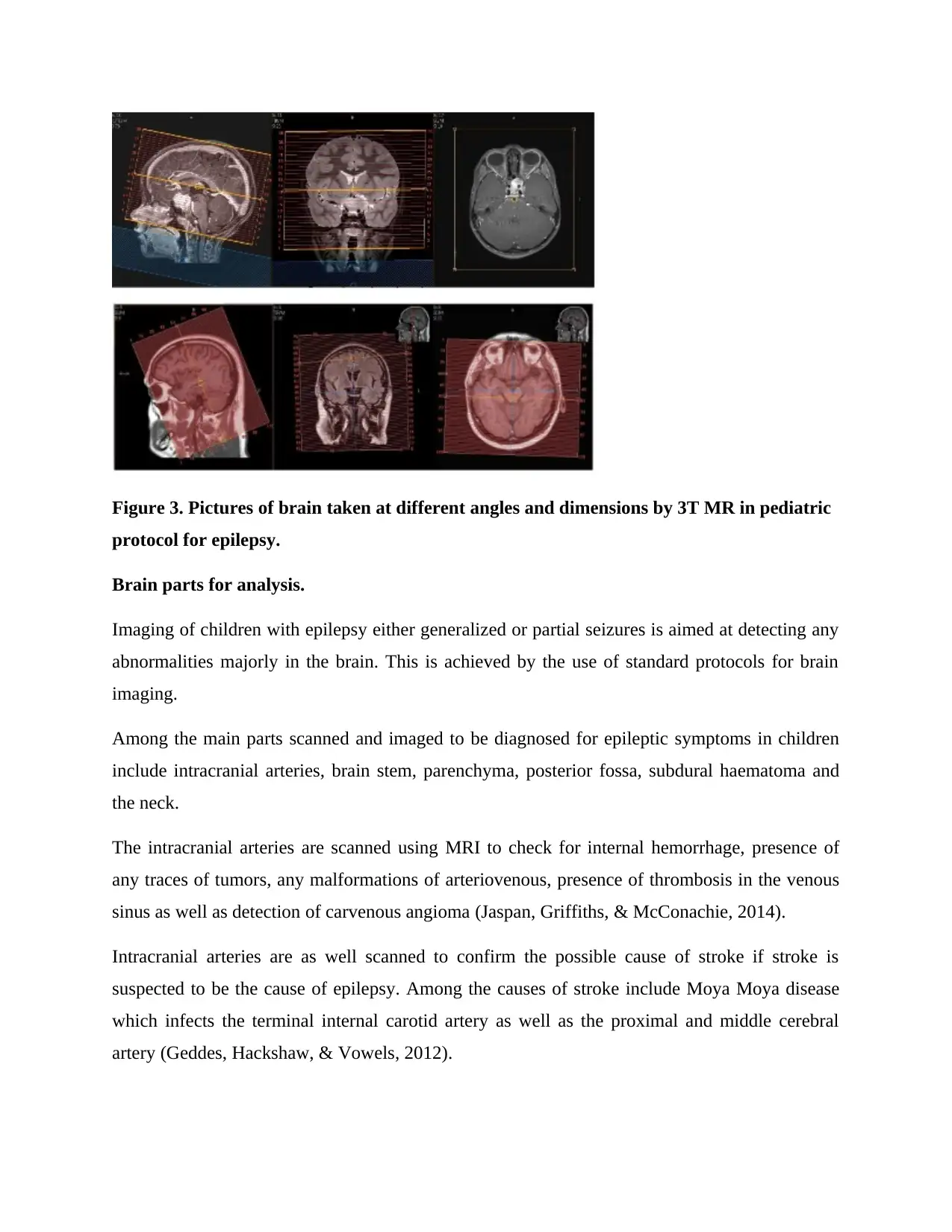
Figure 3. Pictures of brain taken at different angles and dimensions by 3T MR in pediatric
protocol for epilepsy.
Brain parts for analysis.
Imaging of children with epilepsy either generalized or partial seizures is aimed at detecting any
abnormalities majorly in the brain. This is achieved by the use of standard protocols for brain
imaging.
Among the main parts scanned and imaged to be diagnosed for epileptic symptoms in children
include intracranial arteries, brain stem, parenchyma, posterior fossa, subdural haematoma and
the neck.
The intracranial arteries are scanned using MRI to check for internal hemorrhage, presence of
any traces of tumors, any malformations of arteriovenous, presence of thrombosis in the venous
sinus as well as detection of carvenous angioma (Jaspan, Griffiths, & McConachie, 2014).
Intracranial arteries are as well scanned to confirm the possible cause of stroke if stroke is
suspected to be the cause of epilepsy. Among the causes of stroke include Moya Moya disease
which infects the terminal internal carotid artery as well as the proximal and middle cerebral
artery (Geddes, Hackshaw, & Vowels, 2012).
protocol for epilepsy.
Brain parts for analysis.
Imaging of children with epilepsy either generalized or partial seizures is aimed at detecting any
abnormalities majorly in the brain. This is achieved by the use of standard protocols for brain
imaging.
Among the main parts scanned and imaged to be diagnosed for epileptic symptoms in children
include intracranial arteries, brain stem, parenchyma, posterior fossa, subdural haematoma and
the neck.
The intracranial arteries are scanned using MRI to check for internal hemorrhage, presence of
any traces of tumors, any malformations of arteriovenous, presence of thrombosis in the venous
sinus as well as detection of carvenous angioma (Jaspan, Griffiths, & McConachie, 2014).
Intracranial arteries are as well scanned to confirm the possible cause of stroke if stroke is
suspected to be the cause of epilepsy. Among the causes of stroke include Moya Moya disease
which infects the terminal internal carotid artery as well as the proximal and middle cerebral
artery (Geddes, Hackshaw, & Vowels, 2012).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Brain stem is another item for analysis. Thee cervical cord in the brain stem is examined to check
for any hypoxic-ischaemic injury and trauma which results from the mechanical shaking of the
child which leads to shearing effect (Geddes, Vowels, & Hackshaw, 2012).
Parenchyma and subdural haematoma in the posterior fossa and calvarium are analyzed for any
injury to the head which is non-accidental such as continuous abnormality in the neurological
functioning.
Finally, the neck in children with posterior circulation is also examined to check for any arterial
dissection. There is a tendency of fat accumulation in this area which will interfere with proper
blood circulation to the brain leading to oxygen shortage (Ganesan, Prengler, & McShane, 2013).
Instrumental requirements.
The analysis of the above brain parts is done by RMI since it is highly sensitive and efficient
compared to other methods such as CT angiography (Haugen & Boyesen, 2011).
The instrumental requirement to achieve high quality data in the infants and children with small
body organs, the RMI device has a large size of matrix which ranges to above 257 by 257 and a
wider field of view of about 200 micrometers. The size of slice in terms of thickness is also
reduced to about 4 millimeters to improve transparency. Finally, the RMI used has a highly
sensitive heads coil for receiving radio waves in an efficient and quicker way.
Discussion
This section covers a comparison between different imaging techniques used for diagnosis
purposes in treatment of epilepsy. It as well describes the important features that must be met by
the equipment to be used in imaging. In addition, the state of patient who can be diagnosed with
the assistance of a given technique are also covered.
for any hypoxic-ischaemic injury and trauma which results from the mechanical shaking of the
child which leads to shearing effect (Geddes, Vowels, & Hackshaw, 2012).
Parenchyma and subdural haematoma in the posterior fossa and calvarium are analyzed for any
injury to the head which is non-accidental such as continuous abnormality in the neurological
functioning.
Finally, the neck in children with posterior circulation is also examined to check for any arterial
dissection. There is a tendency of fat accumulation in this area which will interfere with proper
blood circulation to the brain leading to oxygen shortage (Ganesan, Prengler, & McShane, 2013).
Instrumental requirements.
The analysis of the above brain parts is done by RMI since it is highly sensitive and efficient
compared to other methods such as CT angiography (Haugen & Boyesen, 2011).
The instrumental requirement to achieve high quality data in the infants and children with small
body organs, the RMI device has a large size of matrix which ranges to above 257 by 257 and a
wider field of view of about 200 micrometers. The size of slice in terms of thickness is also
reduced to about 4 millimeters to improve transparency. Finally, the RMI used has a highly
sensitive heads coil for receiving radio waves in an efficient and quicker way.
Discussion
This section covers a comparison between different imaging techniques used for diagnosis
purposes in treatment of epilepsy. It as well describes the important features that must be met by
the equipment to be used in imaging. In addition, the state of patient who can be diagnosed with
the assistance of a given technique are also covered.
Safety measures for pediatric patient and operator.
Kanal (2013) provides some safety guidelines for the pediatric patients and the operators in MRI.
In most cases, pediatric patients are not in a position of explaining their conditions and therefore
before admission into MR room, the health history should be obtained from the family member
to establish if the patient has any ferromagnetic implants or is suffering from any other illness,
this will determine if anesthesia will be necessary or not. Children that were recently sick cannot
be administered with anesthesia or sedatives. Proper screening should be performed to check for
any foreign objects in the body. This should be done in presence of adults in order to enhance the
self-report. Children and MR operators are to be protected from noise by use of earplug. Since
children tent move frequently, insulators should be placed between them and conductors to
prevent any injuries such as burns and electrocution. Body temperature should be monitored
constantly. If the anesthesia or sedative is used on the child, a recovery procedure must be done
by the nurse before the child is discharged to his or her parents. The operator must put on
protective gears such as gloves when they come in contact with patients suffering from infectious
diseases and when cleaning the scanning table to avoid infections. The technologists and family
members attending to the child in the operation room should not have any electronic devices or
metallic objects.
Imaging Protocol analysis.
Magnetic resonance protocol for epilepsy is utilized in seizure disorder cases to identify the
underlying causes. This is especially important considering that it does not use ionized radiations
and therefore there are no side effects on the delegate actively growing tissues in children. The
protocol uses radiofrequencies, magnetic field and electric current to generate the required
pictures.
Different sequences are used depending on the preferences of the institution, type of equipment
and software available, technicality required and the conditions of the pediatric patient.
The common sequence in MR protocol for epilepsy are non-focal epilepsy protocol and the
temporal lobe epilepsy protocol.
The proper MR pediatric protocol in non-focal epilepsy require the T1 sequence for corona and
axis, FLAIR sequence for axis and angled corona sequence, and sequence for inversion recovery.
Kanal (2013) provides some safety guidelines for the pediatric patients and the operators in MRI.
In most cases, pediatric patients are not in a position of explaining their conditions and therefore
before admission into MR room, the health history should be obtained from the family member
to establish if the patient has any ferromagnetic implants or is suffering from any other illness,
this will determine if anesthesia will be necessary or not. Children that were recently sick cannot
be administered with anesthesia or sedatives. Proper screening should be performed to check for
any foreign objects in the body. This should be done in presence of adults in order to enhance the
self-report. Children and MR operators are to be protected from noise by use of earplug. Since
children tent move frequently, insulators should be placed between them and conductors to
prevent any injuries such as burns and electrocution. Body temperature should be monitored
constantly. If the anesthesia or sedative is used on the child, a recovery procedure must be done
by the nurse before the child is discharged to his or her parents. The operator must put on
protective gears such as gloves when they come in contact with patients suffering from infectious
diseases and when cleaning the scanning table to avoid infections. The technologists and family
members attending to the child in the operation room should not have any electronic devices or
metallic objects.
Imaging Protocol analysis.
Magnetic resonance protocol for epilepsy is utilized in seizure disorder cases to identify the
underlying causes. This is especially important considering that it does not use ionized radiations
and therefore there are no side effects on the delegate actively growing tissues in children. The
protocol uses radiofrequencies, magnetic field and electric current to generate the required
pictures.
Different sequences are used depending on the preferences of the institution, type of equipment
and software available, technicality required and the conditions of the pediatric patient.
The common sequence in MR protocol for epilepsy are non-focal epilepsy protocol and the
temporal lobe epilepsy protocol.
The proper MR pediatric protocol in non-focal epilepsy require the T1 sequence for corona and
axis, FLAIR sequence for axis and angled corona sequence, and sequence for inversion recovery.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Temporal lobe epilepsy protocol requires T1 sequence for axis and corona, T2 sequence for
angled corona and FLAIR sequence for axis and angled corona.
Magnetic resonance pediatric protocol is suitable in children because scanning can be done
without any exposure to harmful radiations.
Before subjecting the child to the MR pediatric protocol, a proper eating guideline as given by
the radiologist, nurse of technologist must be followed. The medical history of the child is also
obtained from the child’s parent to determine the health state such as allergic and asthma- related
cases. This is aimed at establishing if there is need for administering any contrast injections,
sedative prescription and for making body scan to check for foreign objects.
Benefits of Magnetic resonance imaging protocol for epilepsy.
The MRI scan has no pain during scanning process on the patient and therefore the patient’s
safety is high. It can also discover other abnormalities hidden by bones in children which cannot
be achieved using other methods
Limitations of Magnetic resonance imaging protocol for epilepsy
MRI has several limitations. It is very expensive to install and maintain. It is also time
consuming as it takes relatively longer time to generate information required for diagnosis
purposes when compared to other techniques like X-ray, due to this factor, it is not suitable for
use in emergency cases that require a quick response.
In some cases, MRI may be inaccurate in differentiating different stages of the disease. There is a
challenge in obtaining high quality images since the children cannot stay still for long while
scanning is going on.
Finally, it is limited on the type of users. Only patients without ferromagnetic objects in their
body system can be scanned in an RMI. (Roy & Pandit, 2011).
angled corona and FLAIR sequence for axis and angled corona.
Magnetic resonance pediatric protocol is suitable in children because scanning can be done
without any exposure to harmful radiations.
Before subjecting the child to the MR pediatric protocol, a proper eating guideline as given by
the radiologist, nurse of technologist must be followed. The medical history of the child is also
obtained from the child’s parent to determine the health state such as allergic and asthma- related
cases. This is aimed at establishing if there is need for administering any contrast injections,
sedative prescription and for making body scan to check for foreign objects.
Benefits of Magnetic resonance imaging protocol for epilepsy.
The MRI scan has no pain during scanning process on the patient and therefore the patient’s
safety is high. It can also discover other abnormalities hidden by bones in children which cannot
be achieved using other methods
Limitations of Magnetic resonance imaging protocol for epilepsy
MRI has several limitations. It is very expensive to install and maintain. It is also time
consuming as it takes relatively longer time to generate information required for diagnosis
purposes when compared to other techniques like X-ray, due to this factor, it is not suitable for
use in emergency cases that require a quick response.
In some cases, MRI may be inaccurate in differentiating different stages of the disease. There is a
challenge in obtaining high quality images since the children cannot stay still for long while
scanning is going on.
Finally, it is limited on the type of users. Only patients without ferromagnetic objects in their
body system can be scanned in an RMI. (Roy & Pandit, 2011).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Conclusion.
This work was about the use of magnetic resonance imaging protocol for diagnosing epilepsy.
Epilepsy is a mental disease that affects the brain especially the nervous system. Its diagnosis
requires a detailed examination due the sensitive nature of brain. The pictures from the brain
parts are used to do the diagnosis. Various imaging methods such as ultrasonography, computer
tomography and magnetic resonance. Among the techniques used, MRI was the most efficient,
safe and cost effective for diagnosis.
This work was about the use of magnetic resonance imaging protocol for diagnosing epilepsy.
Epilepsy is a mental disease that affects the brain especially the nervous system. Its diagnosis
requires a detailed examination due the sensitive nature of brain. The pictures from the brain
parts are used to do the diagnosis. Various imaging methods such as ultrasonography, computer
tomography and magnetic resonance. Among the techniques used, MRI was the most efficient,
safe and cost effective for diagnosis.
References
Donald, W. (2001, may monday). Infection Control Today. MRI: Use, Safety, and Patient Care, pp. 1-5.
Erasmo, A., & Faan, M. (2018). Neuroimaging in Epilepsy. Neurology, 2.
Ganesan, V., Prengler, M., & McShane, M. (2013). Investigation of risk factors in children with arterial
ischaemic stroke. Ann Neurol, 167–173.
Geddes, J., Hackshaw, A., & Vowels, G. (2012). Neuropathology of inflicted head injury in children.
Patterns of brain damage, 1290–1298.
Geddes, J., Vowels, G., & Hackshaw, A. (2012). Neuropathology of inflicted brain injury in children.
Microscopic brain injury in infants, 1299–1306.
Haugen, I., & Boyesen, P. (2011). Imaging modalities in hand osteoarthritis. status and perspectives of
conventional radiology, magnetic resonance imaging, and ultrasonography, 248.
Jaspan, T., Griffiths, P., & McConachie, N. (2014). Neuroimaging for non-accidental head injury in
childhood. a proposed protocol, 44–53.
Lee, V., Hecht, E., Taouli, B., Chen, Q., Prince, K., & Oesingmann, N. (2017). Body and cardiovascular MR
imaging at 3.0 T. Radiology, 692–705.
McQueen, F., Lassere, M., & Duer-Jensen, A. (2012). Testing an OMERACT MRI scoring system for
peripheral psoriatic arthritis in cross-sectional and longitudinal settings. J Rheumatol, 1811–15.
pol, J. (2013). The comparison of efficacy of different imaging techniques in assessment of wrist joints
and metacarpophalangeal joints in patients with psoriatic arthritis. Polish journal of Radiology,
78.
Ramli, N., Rahmat, K., Lim, K., & Tan, C. (2015). Neuroimaging inrefractory epilepsy. Current practice and
evolving trends, 1791-800.
Roy, T., & Pandit, A. (2011). Neuroimaging in epilepsy. Ann Indian Acad Neurol.
Satu, K., Hanna, H., Tarja, L., Liisa, M., & Eija, G. (2016). CHILDREN WITH EPILEPSY. Chicago: Jay .
Tim, N. (2018, January Tuesday). Medical News Today. Are X-rays really safe?, p. 3.
Trattnig, S., Pinker, K., Ba-Ssalamah, A., & Nobauer-Huhmann, I.-M. (2016). The optimal use of contrast
agents at high field MRI. Eur. Radiol 16, 1280–1287.
Wassenberg, S., Fischer, V., & Herborn, G. (2013). A method to score radiographic change in psoriatic
arthritis. Z Rheumatol publishers.
Wittoek, R., Lans, L., & Lambrecht, V. (2011). Reliability and construct validity of ultrasonography of soft
tissue and destructive changes in erosive osteoarthritis of the interphalangeal finger joints. a
comparison with MRI, 278-83.
OHSU (2014). MR pediatric epilepsy/ seizure brain WO protocol. Diagnostic radiology,1.
kanal, K. (2013). MR guideline on safety. MR technologist version.
Donald, W. (2001, may monday). Infection Control Today. MRI: Use, Safety, and Patient Care, pp. 1-5.
Erasmo, A., & Faan, M. (2018). Neuroimaging in Epilepsy. Neurology, 2.
Ganesan, V., Prengler, M., & McShane, M. (2013). Investigation of risk factors in children with arterial
ischaemic stroke. Ann Neurol, 167–173.
Geddes, J., Hackshaw, A., & Vowels, G. (2012). Neuropathology of inflicted head injury in children.
Patterns of brain damage, 1290–1298.
Geddes, J., Vowels, G., & Hackshaw, A. (2012). Neuropathology of inflicted brain injury in children.
Microscopic brain injury in infants, 1299–1306.
Haugen, I., & Boyesen, P. (2011). Imaging modalities in hand osteoarthritis. status and perspectives of
conventional radiology, magnetic resonance imaging, and ultrasonography, 248.
Jaspan, T., Griffiths, P., & McConachie, N. (2014). Neuroimaging for non-accidental head injury in
childhood. a proposed protocol, 44–53.
Lee, V., Hecht, E., Taouli, B., Chen, Q., Prince, K., & Oesingmann, N. (2017). Body and cardiovascular MR
imaging at 3.0 T. Radiology, 692–705.
McQueen, F., Lassere, M., & Duer-Jensen, A. (2012). Testing an OMERACT MRI scoring system for
peripheral psoriatic arthritis in cross-sectional and longitudinal settings. J Rheumatol, 1811–15.
pol, J. (2013). The comparison of efficacy of different imaging techniques in assessment of wrist joints
and metacarpophalangeal joints in patients with psoriatic arthritis. Polish journal of Radiology,
78.
Ramli, N., Rahmat, K., Lim, K., & Tan, C. (2015). Neuroimaging inrefractory epilepsy. Current practice and
evolving trends, 1791-800.
Roy, T., & Pandit, A. (2011). Neuroimaging in epilepsy. Ann Indian Acad Neurol.
Satu, K., Hanna, H., Tarja, L., Liisa, M., & Eija, G. (2016). CHILDREN WITH EPILEPSY. Chicago: Jay .
Tim, N. (2018, January Tuesday). Medical News Today. Are X-rays really safe?, p. 3.
Trattnig, S., Pinker, K., Ba-Ssalamah, A., & Nobauer-Huhmann, I.-M. (2016). The optimal use of contrast
agents at high field MRI. Eur. Radiol 16, 1280–1287.
Wassenberg, S., Fischer, V., & Herborn, G. (2013). A method to score radiographic change in psoriatic
arthritis. Z Rheumatol publishers.
Wittoek, R., Lans, L., & Lambrecht, V. (2011). Reliability and construct validity of ultrasonography of soft
tissue and destructive changes in erosive osteoarthritis of the interphalangeal finger joints. a
comparison with MRI, 278-83.
OHSU (2014). MR pediatric epilepsy/ seizure brain WO protocol. Diagnostic radiology,1.
kanal, K. (2013). MR guideline on safety. MR technologist version.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.