NICE Dementia Policy Critique: Analysis and Recommendations
VerifiedAdded on 2023/06/04
|17
|5130
|392
Report
AI Summary
This report presents a critical analysis of the NICE Dementia Guidelines, a policy designed to support and care for individuals suffering from dementia. The critique encompasses various aspects of the policy, including involving dementia patients in care decisions, diagnosis procedures, care coordination, interventions for cognition and wellbeing, pharmacological interventions, managing non-cognitive symptoms, and handling risks during hospital admissions. The report identifies areas for improvement, such as better training for caregivers, seamless transfer of patient records, and strategies for managing challenging behaviors. A literature review supports the proposed updates, emphasizing the importance of skilled caregivers, anger management training, and comprehensive record-keeping. The updated policy aims to ensure respectful and effective care for dementia patients and their families, with a focus on patient consent, advanced care planning, and multidisciplinary support.

1
Policy Critique
Introduction: Old age is a time when the organs of human body start to lose its effectiveness.
Along with immunity system, different integral organs become weak. As a result, old people
become more prone to develop illnesses. With old age, the chances of contracting a disease rise.
It is found that a large percentage of people having ailment is over 60 years old. Therefore, it can
be said that old age is a stage where a person becomes vulnerable to catch diseases or disorders.
Some of these diseases are curable while many of them are long term and cannot be entirely
cured. Medications and counselling are used to keep such illnesses under control to help the
patient lead a normal life (van Bussel et al. 2017). One such common long term disease is
Dementia. Dementia is an illness involving memory of a person. A dementia affected person
suffers from short term memory loss and tends to forget significant life incidents (Wang et al.
2016). It impacts of their regular activities in a negative way. It has been found that most of the
dementia patients are over 60 years old. Hence, they need constant support of a care giver in
order to carry out their functions. This report is regarding the policy which has been introduced
by National Institute for Clinical Excellence (NICE) to enable proper support and care for the
patients suffering from Dementia. The policy is having a number of guidelines which are
critically analysed and evaluated in this report.
Overview of the current policy: As the prevalence of Dementia is increasing rapidly in Europe,
there was a need of suitable policy to cope with the situation. It has been found that old people
are mostly affected by dementia, most of the patients aged above 60 years. NICE Dementia
Guidelines had been introduced to allow the dementia affected people to lead a normal healthy
life. The primary and major effect of Dementia is memory loss. Such type of illness may hamper
the regular activities of a person, especially if the patient is an aged person (Dewing & Dijk,
2016). Therefore, care support is required for dementia patients so that they can effortlessly carry
out their regular tasks. Dementia affects brain cells of the person, making a negative impact on
their memory. The forgetfulness makes the patient confused and annoyed. Moreover, if the
patient is over 60 years old, it is likely that the patient will be showing challenging behaviour.
Therefore, it is important for the care staff to follow a number of guidelines while taking care of
Policy Critique
Introduction: Old age is a time when the organs of human body start to lose its effectiveness.
Along with immunity system, different integral organs become weak. As a result, old people
become more prone to develop illnesses. With old age, the chances of contracting a disease rise.
It is found that a large percentage of people having ailment is over 60 years old. Therefore, it can
be said that old age is a stage where a person becomes vulnerable to catch diseases or disorders.
Some of these diseases are curable while many of them are long term and cannot be entirely
cured. Medications and counselling are used to keep such illnesses under control to help the
patient lead a normal life (van Bussel et al. 2017). One such common long term disease is
Dementia. Dementia is an illness involving memory of a person. A dementia affected person
suffers from short term memory loss and tends to forget significant life incidents (Wang et al.
2016). It impacts of their regular activities in a negative way. It has been found that most of the
dementia patients are over 60 years old. Hence, they need constant support of a care giver in
order to carry out their functions. This report is regarding the policy which has been introduced
by National Institute for Clinical Excellence (NICE) to enable proper support and care for the
patients suffering from Dementia. The policy is having a number of guidelines which are
critically analysed and evaluated in this report.
Overview of the current policy: As the prevalence of Dementia is increasing rapidly in Europe,
there was a need of suitable policy to cope with the situation. It has been found that old people
are mostly affected by dementia, most of the patients aged above 60 years. NICE Dementia
Guidelines had been introduced to allow the dementia affected people to lead a normal healthy
life. The primary and major effect of Dementia is memory loss. Such type of illness may hamper
the regular activities of a person, especially if the patient is an aged person (Dewing & Dijk,
2016). Therefore, care support is required for dementia patients so that they can effortlessly carry
out their regular tasks. Dementia affects brain cells of the person, making a negative impact on
their memory. The forgetfulness makes the patient confused and annoyed. Moreover, if the
patient is over 60 years old, it is likely that the patient will be showing challenging behaviour.
Therefore, it is important for the care staff to follow a number of guidelines while taking care of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
an aged person affected with dementia (Mast et al. 2016). The NICE Dementia Guidelines aim to
improve the overall condition of dementia patients. The guidelines are related to-
Involving people living with dementia in decisions about their care
Diagnosis
Care coordination
Interventions to promote cognition, independence and wellbeing
Pharmacological interventions for dementia
Medicines that may cause cognitive impairment
Managing non-cognitive symptoms
Assessing and managing other long-term conditions in people living with dementia
Risks during hospital admission
The policy allows the patient to make decisions regarding the care they are being provided with.
The patients are encouraged to share their opinions and views regarding the healthcare services.
Additional communicative tools such as visual aids and simplified text can be used to enable
effective communication between the patient and the care giver. Structured tools can be used as
well to know the personal history of the dementia patient along with their likes, dislikes and
daily routine (Karlsson et al. 2016). All these things are essential to render proper support to the
patient suffering from dementia. According to the policy, sufficient information should be
provided to the care giver regarding the condition of the patient. During diagnosis, it is
mandatory to provide the care giver and the family members of the patient with the information
regarding the dementia subtype from which the patient is suffering; the contact information of
the healthcare or social care team assigned to handle the case; the affects dementia has on driving
so that the DVLA or Driver and Vehicle Licensing Agency and car insurers can be informed
beforehand; legal rights and responsibilities they possess; right to reasonable adjustments for
those who are working or looking for the same; effectiveness and contact information of the
local support group, national charities, online forums, legal and financial advisors, advocacy
services etc (Pink, O’Brien, Robinson & Longson, 2018). The policy also suggests that the
consent of the patient must be sought before providing the services. Which information is to be
shared and with whom, this is sole decision of the patient, and the decision of the patient has to
be documented (Lopes, 2016). Follow-up process, as per the guidelines, is optional; a patient
an aged person affected with dementia (Mast et al. 2016). The NICE Dementia Guidelines aim to
improve the overall condition of dementia patients. The guidelines are related to-
Involving people living with dementia in decisions about their care
Diagnosis
Care coordination
Interventions to promote cognition, independence and wellbeing
Pharmacological interventions for dementia
Medicines that may cause cognitive impairment
Managing non-cognitive symptoms
Assessing and managing other long-term conditions in people living with dementia
Risks during hospital admission
The policy allows the patient to make decisions regarding the care they are being provided with.
The patients are encouraged to share their opinions and views regarding the healthcare services.
Additional communicative tools such as visual aids and simplified text can be used to enable
effective communication between the patient and the care giver. Structured tools can be used as
well to know the personal history of the dementia patient along with their likes, dislikes and
daily routine (Karlsson et al. 2016). All these things are essential to render proper support to the
patient suffering from dementia. According to the policy, sufficient information should be
provided to the care giver regarding the condition of the patient. During diagnosis, it is
mandatory to provide the care giver and the family members of the patient with the information
regarding the dementia subtype from which the patient is suffering; the contact information of
the healthcare or social care team assigned to handle the case; the affects dementia has on driving
so that the DVLA or Driver and Vehicle Licensing Agency and car insurers can be informed
beforehand; legal rights and responsibilities they possess; right to reasonable adjustments for
those who are working or looking for the same; effectiveness and contact information of the
local support group, national charities, online forums, legal and financial advisors, advocacy
services etc (Pink, O’Brien, Robinson & Longson, 2018). The policy also suggests that the
consent of the patient must be sought before providing the services. Which information is to be
shared and with whom, this is sole decision of the patient, and the decision of the patient has to
be documented (Lopes, 2016). Follow-up process, as per the guidelines, is optional; a patient
3
may or may not opt for it. Dementia affected people and their care givers must be aware about
the people or agencies with whom they can contact regarding changes in requirements
(Vandrevala et al. 2017). The policy instructs to ask the dementia affected people to participate
in different surveys and researches related studies. In advanced care planning, a dementia
affected person is to share their wishes, beliefs, preferences, values regarding future care
(Goodarzi et al. 2016). They can take decisions regarding refusal to treatment and place of death.
However, changes can be made to these decisions during care review. To identify a dementia
patient, initial assessment must be done through gathering background information and history
(Lee, Weston & Hillier, 2018). On suspecting dementia, physical examination should take place.
Cognitive testing is beneficial in this context. Although a normal score in cognitive instrument is
not adequate to rule out the chances of dementia. On further suspicion the person should be
referred to specialist dementia diagnostic service. Upon confirmation of dementia, the family of
the patient and the care giver should get access to hospital or primary-care-based
multidisciplinary dementia service or the memory service (McCormick, 2015). The dementia
affected person should be helped with an experienced health or social care professional, who will
render needful care coordination. The major task of the health or social care professional would
be developing a proper care plan for the patient (Fleming, Goodenough, Low, Chenoweth &
Brodaty, 2016). The professional would also review the plan, take decisions related to execution
of the same, record the post execution progress and provide a copy of the plan to the care giver
and family of the patient. According to the policy, it is the responsibility of the care providers to
enable seamless transfer of relevant information to other care settings where the patient would be
transferred. Relevant information regarding the health of the patient should be recorded and the
support plan should be updated accordingly (Müller, Lautenschläger, Meyer & Stephan, 2017).
The policy covers the wellbeing of the dementia affected people along with those who are not
having any care giver, people who do not have access to transport or have difficulty in using the
same, people with physical or psychological impairment or learning disabilities, people who are
less likely to opt for health and social care services, people having other responsibilities
regarding job, children etc. The policy allows a range of activities developed as per the person’s
preferences which aim to promote wellness. People with mild or moderate dementia are directed
to opt for group cognitive stimulation therapy or group reminiscence therapy or occupational
therapy (Groot et al. 2016). As per the guidelines there are multiple services which must not be
may or may not opt for it. Dementia affected people and their care givers must be aware about
the people or agencies with whom they can contact regarding changes in requirements
(Vandrevala et al. 2017). The policy instructs to ask the dementia affected people to participate
in different surveys and researches related studies. In advanced care planning, a dementia
affected person is to share their wishes, beliefs, preferences, values regarding future care
(Goodarzi et al. 2016). They can take decisions regarding refusal to treatment and place of death.
However, changes can be made to these decisions during care review. To identify a dementia
patient, initial assessment must be done through gathering background information and history
(Lee, Weston & Hillier, 2018). On suspecting dementia, physical examination should take place.
Cognitive testing is beneficial in this context. Although a normal score in cognitive instrument is
not adequate to rule out the chances of dementia. On further suspicion the person should be
referred to specialist dementia diagnostic service. Upon confirmation of dementia, the family of
the patient and the care giver should get access to hospital or primary-care-based
multidisciplinary dementia service or the memory service (McCormick, 2015). The dementia
affected person should be helped with an experienced health or social care professional, who will
render needful care coordination. The major task of the health or social care professional would
be developing a proper care plan for the patient (Fleming, Goodenough, Low, Chenoweth &
Brodaty, 2016). The professional would also review the plan, take decisions related to execution
of the same, record the post execution progress and provide a copy of the plan to the care giver
and family of the patient. According to the policy, it is the responsibility of the care providers to
enable seamless transfer of relevant information to other care settings where the patient would be
transferred. Relevant information regarding the health of the patient should be recorded and the
support plan should be updated accordingly (Müller, Lautenschläger, Meyer & Stephan, 2017).
The policy covers the wellbeing of the dementia affected people along with those who are not
having any care giver, people who do not have access to transport or have difficulty in using the
same, people with physical or psychological impairment or learning disabilities, people who are
less likely to opt for health and social care services, people having other responsibilities
regarding job, children etc. The policy allows a range of activities developed as per the person’s
preferences which aim to promote wellness. People with mild or moderate dementia are directed
to opt for group cognitive stimulation therapy or group reminiscence therapy or occupational
therapy (Groot et al. 2016). As per the guidelines there are multiple services which must not be
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

4
offered to the dementia patients such as acupuncture, ginseng, herbal formulations, and vitamin
E supplements. There are also some significant guidelines in the policy related to the
medications used for Alzheimer’s disease.
Consultation - of improving policy: The NICE Dementia Guidelines is undoubtedly a
significant policy for the betterment of the dementia affected people. But it is necessary to bring
about certain new and updated implementations which would increase the effectiveness of the
same. In the meantime, improvement of a policy does not take place overnight. It requires a lot
of research and study to recognize various aspects of a policy. Further analysis brings out certain
loopholes which are replaced or updated in accordance to the requirement. It takes simultaneous
research and review to identify problems within a system or a policy. Before implementing
changes to a policy it is essential to discuss with significant people of the organisation. There is
always a starting point of a change and in this case it started from identification of the issue. The
issue is found in the context of elderly people suffering from dementia. At first both the positive
and negative factors are to be identified and analysed critically in order to gain information
having higher level of accuracy. In this context, information was gathered through effective
communication with dementia affected people aged more than years. To identify the problem,
the care givers and families of the elderly people suffering from dementia were interviewed
thoroughly. After a number of interviews and effective chat session with dementia patients, the
problem which was vogue earlier came out clearer. The issues were less trained care givers,
difficulty in transferring medical records to different care settings, extreme challenging
behaviour shown by patients, frequent clashes between families and staff members etc. These
problems were discussed with the staff member of dementia care centres and health and social
care professionals. After long brainstorming sessions a number of changes were made to the
existing policy to make it more feasible. The updated policy required the care providers to go
through extensive training, mandatory anger management classes, and updated system to enable
seamless record keeping and record transferring. New ideas were formulated and tested before
final implementation of updated policy. Valuable feedbacks were gained afterwards.
offered to the dementia patients such as acupuncture, ginseng, herbal formulations, and vitamin
E supplements. There are also some significant guidelines in the policy related to the
medications used for Alzheimer’s disease.
Consultation - of improving policy: The NICE Dementia Guidelines is undoubtedly a
significant policy for the betterment of the dementia affected people. But it is necessary to bring
about certain new and updated implementations which would increase the effectiveness of the
same. In the meantime, improvement of a policy does not take place overnight. It requires a lot
of research and study to recognize various aspects of a policy. Further analysis brings out certain
loopholes which are replaced or updated in accordance to the requirement. It takes simultaneous
research and review to identify problems within a system or a policy. Before implementing
changes to a policy it is essential to discuss with significant people of the organisation. There is
always a starting point of a change and in this case it started from identification of the issue. The
issue is found in the context of elderly people suffering from dementia. At first both the positive
and negative factors are to be identified and analysed critically in order to gain information
having higher level of accuracy. In this context, information was gathered through effective
communication with dementia affected people aged more than years. To identify the problem,
the care givers and families of the elderly people suffering from dementia were interviewed
thoroughly. After a number of interviews and effective chat session with dementia patients, the
problem which was vogue earlier came out clearer. The issues were less trained care givers,
difficulty in transferring medical records to different care settings, extreme challenging
behaviour shown by patients, frequent clashes between families and staff members etc. These
problems were discussed with the staff member of dementia care centres and health and social
care professionals. After long brainstorming sessions a number of changes were made to the
existing policy to make it more feasible. The updated policy required the care providers to go
through extensive training, mandatory anger management classes, and updated system to enable
seamless record keeping and record transferring. New ideas were formulated and tested before
final implementation of updated policy. Valuable feedbacks were gained afterwards.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Literature review: Comprehensive review of the new policies was made with the help of a
number of relevant literature databases such as PubMed, CINHAL. The empirical evidence
provided by these databases help in increasing effectiveness of the new policies. As far as this
policy is concerned, the care providers should be careful about their actions as healthcare sector
is a sensitive sector and long term illnesses like dementia require proper care. The most common
issue with dementia patients is challenging behaviour. As the disease involves brain cells the
patient experiences mood swings which sometimes come out as challenging behaviour. This
affects care giver the most. As the policy suggests consent of patient before rendering service, a
patient with challenging behaviour is difficult to handle. Therefore, the updated policy suggests
that if the patient is found to be incapable of taking own decisions then the health or social care
professional taking care of them can decide the services they will be going through. Dementia
patients are mostly having poor decision making skill; therefore the care givers should be able to
take certain decision which may impact the health of the patient (Chen, Huang, Yeh, Huang &
Chen, 2015). The care givers should be well-equipped with skills which are needful to take care
of a dementia affected person. Lack of adequate knowledge and skills in the care giver can result
in deterioration of health of the patient (Barbosa, Sousa, Nolan & Figueiredo, 2015). Therefore,
relevant skills are compulsory for dementia care givers. Also, to avoid conflicts between
patient’s family and staff members, the updated policy introduces mandatory anger management
classes for the care givers and staff members. In the updated policy, the care providers are
strictly instructed to keep proper record of the patient’s condition and share the same with
another care setting if the patient is moved there. Seamless transferring of data would allow
better quality of care for the patients (Macdonald & Mears, 2018). The new updated policy also
highlights that there must be no ill treatment towards the patient or the family. Any staff unable
to follow the same would be suspended from the organisation. It is believed that this can make
the bond between the patient and family with the care providers better and more trustworthy. The
updated policy also focuses on organising training programmes for the newly recruited staff
members to boost their effectiveness.
Implementation of updated policy: After formulating new guidelines and adding some new
relevant ones, these are to be implemented in the updated version of the policy. The new policy
Literature review: Comprehensive review of the new policies was made with the help of a
number of relevant literature databases such as PubMed, CINHAL. The empirical evidence
provided by these databases help in increasing effectiveness of the new policies. As far as this
policy is concerned, the care providers should be careful about their actions as healthcare sector
is a sensitive sector and long term illnesses like dementia require proper care. The most common
issue with dementia patients is challenging behaviour. As the disease involves brain cells the
patient experiences mood swings which sometimes come out as challenging behaviour. This
affects care giver the most. As the policy suggests consent of patient before rendering service, a
patient with challenging behaviour is difficult to handle. Therefore, the updated policy suggests
that if the patient is found to be incapable of taking own decisions then the health or social care
professional taking care of them can decide the services they will be going through. Dementia
patients are mostly having poor decision making skill; therefore the care givers should be able to
take certain decision which may impact the health of the patient (Chen, Huang, Yeh, Huang &
Chen, 2015). The care givers should be well-equipped with skills which are needful to take care
of a dementia affected person. Lack of adequate knowledge and skills in the care giver can result
in deterioration of health of the patient (Barbosa, Sousa, Nolan & Figueiredo, 2015). Therefore,
relevant skills are compulsory for dementia care givers. Also, to avoid conflicts between
patient’s family and staff members, the updated policy introduces mandatory anger management
classes for the care givers and staff members. In the updated policy, the care providers are
strictly instructed to keep proper record of the patient’s condition and share the same with
another care setting if the patient is moved there. Seamless transferring of data would allow
better quality of care for the patients (Macdonald & Mears, 2018). The new updated policy also
highlights that there must be no ill treatment towards the patient or the family. Any staff unable
to follow the same would be suspended from the organisation. It is believed that this can make
the bond between the patient and family with the care providers better and more trustworthy. The
updated policy also focuses on organising training programmes for the newly recruited staff
members to boost their effectiveness.
Implementation of updated policy: After formulating new guidelines and adding some new
relevant ones, these are to be implemented in the updated version of the policy. The new policy

6
is aimed to meet the objectives of the organisation and providing desired outcome to the patients.
To execute the new updated policy an action plan containing required steps needs to be followed.
Action Plan: (Refer to the other document)
Evaluation: The prime objective of the updated policy is to strengthen the dementia care policy
by adding some relevant guidelines which would improve the health condition of the dementia
affected people. From diagnosis to care provision, all these aspects are covered efficiently in the
new version of policy. Effective communication is the key to build rapport with the patient
which would help the care giver to render needful health and social care services to the patient
(Zimmerman, Sloane & Reed, 2014).
Conclusion: Dementia is a much talked about illness. There are a large number of elderly people
suffering from different forms of dementia across Europe. The updated policy aims to reduce the
number of dementia affected people with its well-defined guidelines and critically analysed
methods. The new updated policy suggests that care givers should be well-trained and more
sensible while taking care of a dementia affected person. Challenging behaviour should be
managed with efficacy and effective communication should be initiated between the care givers
and patients so that a deeper understanding can be obtained regarding their condition (Dam, de
Vugt, Klinkenberg, Verhey & van Boxtel, 2016). This would allow the patients to lead a normal
life and reduce the number of affected people across the globe.
References
Barbosa, A., Sousa, L., Nolan, M., & Figueiredo, D. (2015). Effects of person-centered care
approaches to dementia care on staff: a systematic review. American Journal of Alzheimer's
Disease & Other Dementias®, 30(8), 713-722.
is aimed to meet the objectives of the organisation and providing desired outcome to the patients.
To execute the new updated policy an action plan containing required steps needs to be followed.
Action Plan: (Refer to the other document)
Evaluation: The prime objective of the updated policy is to strengthen the dementia care policy
by adding some relevant guidelines which would improve the health condition of the dementia
affected people. From diagnosis to care provision, all these aspects are covered efficiently in the
new version of policy. Effective communication is the key to build rapport with the patient
which would help the care giver to render needful health and social care services to the patient
(Zimmerman, Sloane & Reed, 2014).
Conclusion: Dementia is a much talked about illness. There are a large number of elderly people
suffering from different forms of dementia across Europe. The updated policy aims to reduce the
number of dementia affected people with its well-defined guidelines and critically analysed
methods. The new updated policy suggests that care givers should be well-trained and more
sensible while taking care of a dementia affected person. Challenging behaviour should be
managed with efficacy and effective communication should be initiated between the care givers
and patients so that a deeper understanding can be obtained regarding their condition (Dam, de
Vugt, Klinkenberg, Verhey & van Boxtel, 2016). This would allow the patients to lead a normal
life and reduce the number of affected people across the globe.
References
Barbosa, A., Sousa, L., Nolan, M., & Figueiredo, D. (2015). Effects of person-centered care
approaches to dementia care on staff: a systematic review. American Journal of Alzheimer's
Disease & Other Dementias®, 30(8), 713-722.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
Chen, H. M., Huang, M. F., Yeh, Y. C., Huang, W. H., & Chen, C. S. (2015). Effectiveness of
coping strategies intervention on caregiver burden among caregivers of elderly patients with
dementia. Psychogeriatrics, 15(1), 20-25.
Dam, A. E., de Vugt, M. E., Klinkenberg, I. P., Verhey, F. R., & van Boxtel, M. P. (2016). A
systematic review of social support interventions for caregivers of people with dementia: are
they doing what they promise?. Maturitas, 85, 117-130.
Dewing, J., & Dijk, S. (2016). What is the current state of care for older people with dementia in
general hospitals? A literature review. Dementia, 15(1), 106-124.
Fleming, R., Goodenough, B., Low, L. F., Chenoweth, L., & Brodaty, H. (2016). The
relationship between the quality of the built environment and the quality of life of people with
dementia in residential care. Dementia, 15(4), 663-680.
Goodarzi, Z., Mele, B., Guo, S., Hanson, H., Jette, N., Patten, S., ... & Holroyd-Leduc, J. (2016).
Guidelines for dementia or Parkinson’s disease with depression or anxiety: a systematic
review. BMC neurology, 16(1), 244.
Groot, C., Hooghiemstra, A. M., Raijmakers, P. G. H. M., Van Berckel, B. N. M., Scheltens, P.,
Scherder, E. J. A., ... & Ossenkoppele, R. (2016). The effect of physical activity on cognitive
function in patients with dementia: a meta-analysis of randomized control trials. Ageing research
reviews, 25, 13-23.
Karlsson, S., Bleijlevens, M., Roe, B., Saks, K., Martin, M. S., Stephan, A., ... &
RightTimeCarePlace Consortium. (2015). Dementia care in European countries, from the
perspective of people with dementia and their caregivers. Journal of advanced nursing, 71(6),
1405-1416.
Lee, L., Weston, W., & Hillier, L. (2018). Education to improve dementia care: Impact of a
structured clinical reasoning approach. Family medicine, 50(3), 195-203.
Lopes, M. A. (2016). PREVALENCE OF DEPRESSION IN ELDERLY INPATIENTS WITH
COGNITIVE AND FUNCTIONAL IMPAIRMENT AND DEMENTIA. Alzheimer's &
Dementia: The Journal of the Alzheimer's Association, 12(7), P496.
Chen, H. M., Huang, M. F., Yeh, Y. C., Huang, W. H., & Chen, C. S. (2015). Effectiveness of
coping strategies intervention on caregiver burden among caregivers of elderly patients with
dementia. Psychogeriatrics, 15(1), 20-25.
Dam, A. E., de Vugt, M. E., Klinkenberg, I. P., Verhey, F. R., & van Boxtel, M. P. (2016). A
systematic review of social support interventions for caregivers of people with dementia: are
they doing what they promise?. Maturitas, 85, 117-130.
Dewing, J., & Dijk, S. (2016). What is the current state of care for older people with dementia in
general hospitals? A literature review. Dementia, 15(1), 106-124.
Fleming, R., Goodenough, B., Low, L. F., Chenoweth, L., & Brodaty, H. (2016). The
relationship between the quality of the built environment and the quality of life of people with
dementia in residential care. Dementia, 15(4), 663-680.
Goodarzi, Z., Mele, B., Guo, S., Hanson, H., Jette, N., Patten, S., ... & Holroyd-Leduc, J. (2016).
Guidelines for dementia or Parkinson’s disease with depression or anxiety: a systematic
review. BMC neurology, 16(1), 244.
Groot, C., Hooghiemstra, A. M., Raijmakers, P. G. H. M., Van Berckel, B. N. M., Scheltens, P.,
Scherder, E. J. A., ... & Ossenkoppele, R. (2016). The effect of physical activity on cognitive
function in patients with dementia: a meta-analysis of randomized control trials. Ageing research
reviews, 25, 13-23.
Karlsson, S., Bleijlevens, M., Roe, B., Saks, K., Martin, M. S., Stephan, A., ... &
RightTimeCarePlace Consortium. (2015). Dementia care in European countries, from the
perspective of people with dementia and their caregivers. Journal of advanced nursing, 71(6),
1405-1416.
Lee, L., Weston, W., & Hillier, L. (2018). Education to improve dementia care: Impact of a
structured clinical reasoning approach. Family medicine, 50(3), 195-203.
Lopes, M. A. (2016). PREVALENCE OF DEPRESSION IN ELDERLY INPATIENTS WITH
COGNITIVE AND FUNCTIONAL IMPAIRMENT AND DEMENTIA. Alzheimer's &
Dementia: The Journal of the Alzheimer's Association, 12(7), P496.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Macdonald, G., & Mears, J. (Eds.). (2018). Dementia as Social Experience: Valuing Life and
Care. Routledge.
Mast, G., Fernandes, K., Tadrous, M., Martins, D., Herrmann, N., & Gomes, T. (2016).
Persistence of antipsychotic treatment in elderly dementia patients: a retrospective, population-
based cohort study. Drugs-real world outcomes, 3(2), 175-182.
McCormick, S. (2015). Choosing make believe: pretence or re-orientatation in the care of
individuals living with dementia?.
Müller, C., Lautenschläger, S., Meyer, G., & Stephan, A. (2017). Interventions to support people
with dementia and their caregivers during the transition from home care to nursing home care: A
systematic review. International journal of nursing studies, 71, 139-152.
Pink, J., O’Brien, J., Robinson, L., & Longson, D. (2018). Dementia: assessment, management
and support: summary of updated NICE guidance. bmj, 361, k2438.
van Bussel, E. F., Richard, E., Arts, D. L., Nooyens, A. C., Coloma, P. M., de Waal, M. W., ... &
Smeets, H. (2017). Dementia incidence trend over 1992-2014 in the Netherlands: Analysis of
primary care data. PLoS medicine, 14(3), e1002235.
Vandrevala, T., Samsi, K., Rose, C., Adenrele, C., Barnes, C., & Manthorpe, J. (2017). Perceived
needs for support among care home staff providing end of life care for people with dementia: A
qualitative study. International journal of geriatric psychiatry, 32(2), 155-163.
Wang, C., Gao, S., Hendrie, H. C., Kesterson, J., Campbell, N. L., Shekhar, A., & Callahan, C.
M. (2016). Antidepressant use in the elderly is associated with an increased risk of
dementia. Alzheimer disease and associated disorders, 30(2), 99.
Zimmerman, S., Sloane, P. D., & Reed, D. (2014). Dementia prevalence and care in assisted
living. Health Affairs, 33(4), 658-666.
Macdonald, G., & Mears, J. (Eds.). (2018). Dementia as Social Experience: Valuing Life and
Care. Routledge.
Mast, G., Fernandes, K., Tadrous, M., Martins, D., Herrmann, N., & Gomes, T. (2016).
Persistence of antipsychotic treatment in elderly dementia patients: a retrospective, population-
based cohort study. Drugs-real world outcomes, 3(2), 175-182.
McCormick, S. (2015). Choosing make believe: pretence or re-orientatation in the care of
individuals living with dementia?.
Müller, C., Lautenschläger, S., Meyer, G., & Stephan, A. (2017). Interventions to support people
with dementia and their caregivers during the transition from home care to nursing home care: A
systematic review. International journal of nursing studies, 71, 139-152.
Pink, J., O’Brien, J., Robinson, L., & Longson, D. (2018). Dementia: assessment, management
and support: summary of updated NICE guidance. bmj, 361, k2438.
van Bussel, E. F., Richard, E., Arts, D. L., Nooyens, A. C., Coloma, P. M., de Waal, M. W., ... &
Smeets, H. (2017). Dementia incidence trend over 1992-2014 in the Netherlands: Analysis of
primary care data. PLoS medicine, 14(3), e1002235.
Vandrevala, T., Samsi, K., Rose, C., Adenrele, C., Barnes, C., & Manthorpe, J. (2017). Perceived
needs for support among care home staff providing end of life care for people with dementia: A
qualitative study. International journal of geriatric psychiatry, 32(2), 155-163.
Wang, C., Gao, S., Hendrie, H. C., Kesterson, J., Campbell, N. L., Shekhar, A., & Callahan, C.
M. (2016). Antidepressant use in the elderly is associated with an increased risk of
dementia. Alzheimer disease and associated disorders, 30(2), 99.
Zimmerman, S., Sloane, P. D., & Reed, D. (2014). Dementia prevalence and care in assisted
living. Health Affairs, 33(4), 658-666.
9
Appendix - A
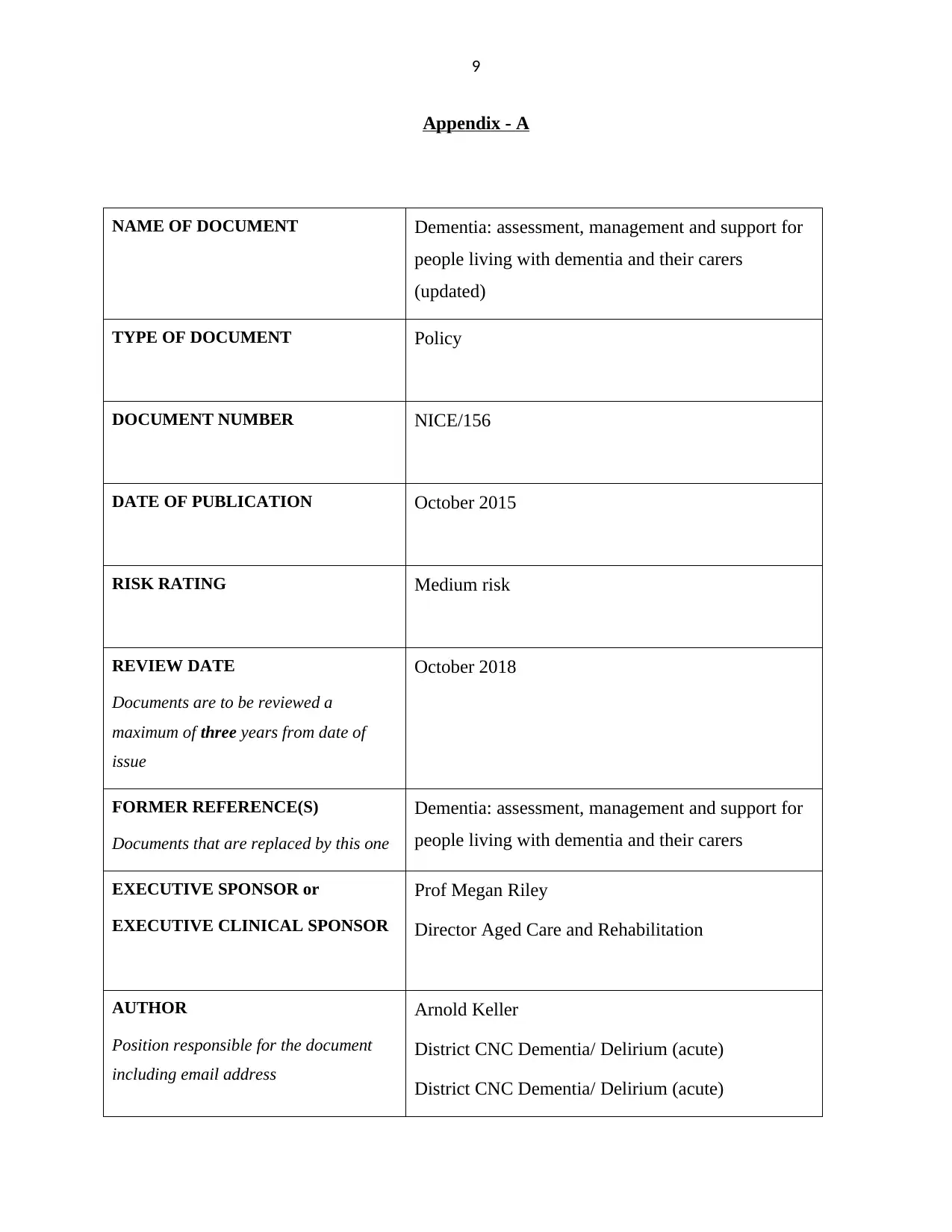
NAME OF DOCUMENT Dementia: assessment, management and support for
people living with dementia and their carers
(updated)
TYPE OF DOCUMENT Policy
DOCUMENT NUMBER NICE/156
DATE OF PUBLICATION October 2015
RISK RATING Medium risk
REVIEW DATE
Documents are to be reviewed a
maximum of three years from date of
issue
October 2018
FORMER REFERENCE(S)
Documents that are replaced by this one
Dementia: assessment, management and support for
people living with dementia and their carers
EXECUTIVE SPONSOR or
EXECUTIVE CLINICAL SPONSOR
Prof Megan Riley
Director Aged Care and Rehabilitation
AUTHOR
Position responsible for the document
including email address
Arnold Keller
District CNC Dementia/ Delirium (acute)
District CNC Dementia/ Delirium (acute)
Appendix - A
NAME OF DOCUMENT Dementia: assessment, management and support for
people living with dementia and their carers
(updated)
TYPE OF DOCUMENT Policy
DOCUMENT NUMBER NICE/156
DATE OF PUBLICATION October 2015
RISK RATING Medium risk
REVIEW DATE
Documents are to be reviewed a
maximum of three years from date of
issue
October 2018
FORMER REFERENCE(S)
Documents that are replaced by this one
Dementia: assessment, management and support for
people living with dementia and their carers
EXECUTIVE SPONSOR or
EXECUTIVE CLINICAL SPONSOR
Prof Megan Riley
Director Aged Care and Rehabilitation
AUTHOR
Position responsible for the document
including email address
Arnold Keller
District CNC Dementia/ Delirium (acute)
District CNC Dementia/ Delirium (acute)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
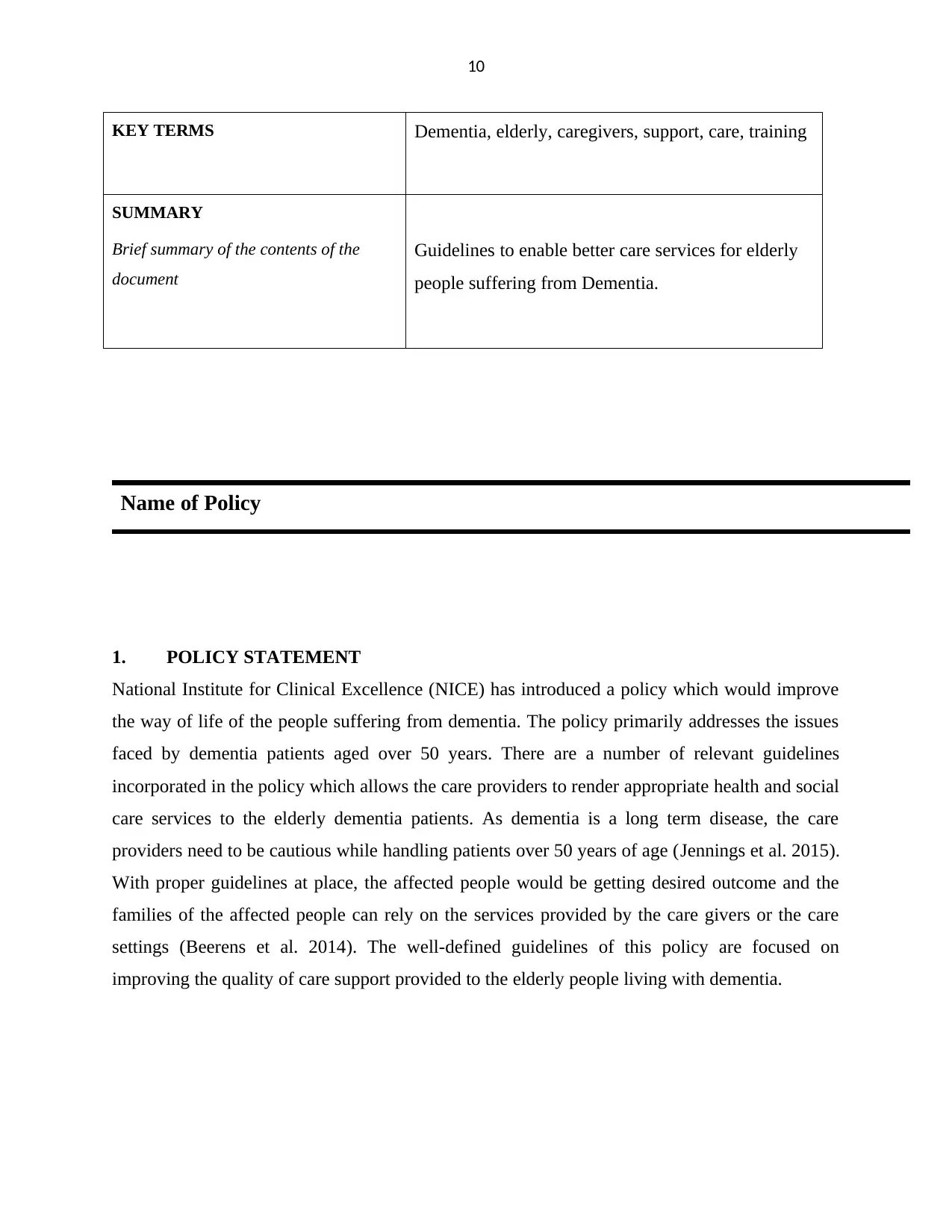
KEY TERMS Dementia, elderly, caregivers, support, care, training
SUMMARY
Brief summary of the contents of the
document
Guidelines to enable better care services for elderly
people suffering from Dementia.
Name of Policy
1. POLICY STATEMENT
National Institute for Clinical Excellence (NICE) has introduced a policy which would improve
the way of life of the people suffering from dementia. The policy primarily addresses the issues
faced by dementia patients aged over 50 years. There are a number of relevant guidelines
incorporated in the policy which allows the care providers to render appropriate health and social
care services to the elderly dementia patients. As dementia is a long term disease, the care
providers need to be cautious while handling patients over 50 years of age (Jennings et al. 2015).
With proper guidelines at place, the affected people would be getting desired outcome and the
families of the affected people can rely on the services provided by the care givers or the care
settings (Beerens et al. 2014). The well-defined guidelines of this policy are focused on
improving the quality of care support provided to the elderly people living with dementia.
KEY TERMS Dementia, elderly, caregivers, support, care, training
SUMMARY
Brief summary of the contents of the
document
Guidelines to enable better care services for elderly
people suffering from Dementia.
Name of Policy
1. POLICY STATEMENT
National Institute for Clinical Excellence (NICE) has introduced a policy which would improve
the way of life of the people suffering from dementia. The policy primarily addresses the issues
faced by dementia patients aged over 50 years. There are a number of relevant guidelines
incorporated in the policy which allows the care providers to render appropriate health and social
care services to the elderly dementia patients. As dementia is a long term disease, the care
providers need to be cautious while handling patients over 50 years of age (Jennings et al. 2015).
With proper guidelines at place, the affected people would be getting desired outcome and the
families of the affected people can rely on the services provided by the care givers or the care
settings (Beerens et al. 2014). The well-defined guidelines of this policy are focused on
improving the quality of care support provided to the elderly people living with dementia.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
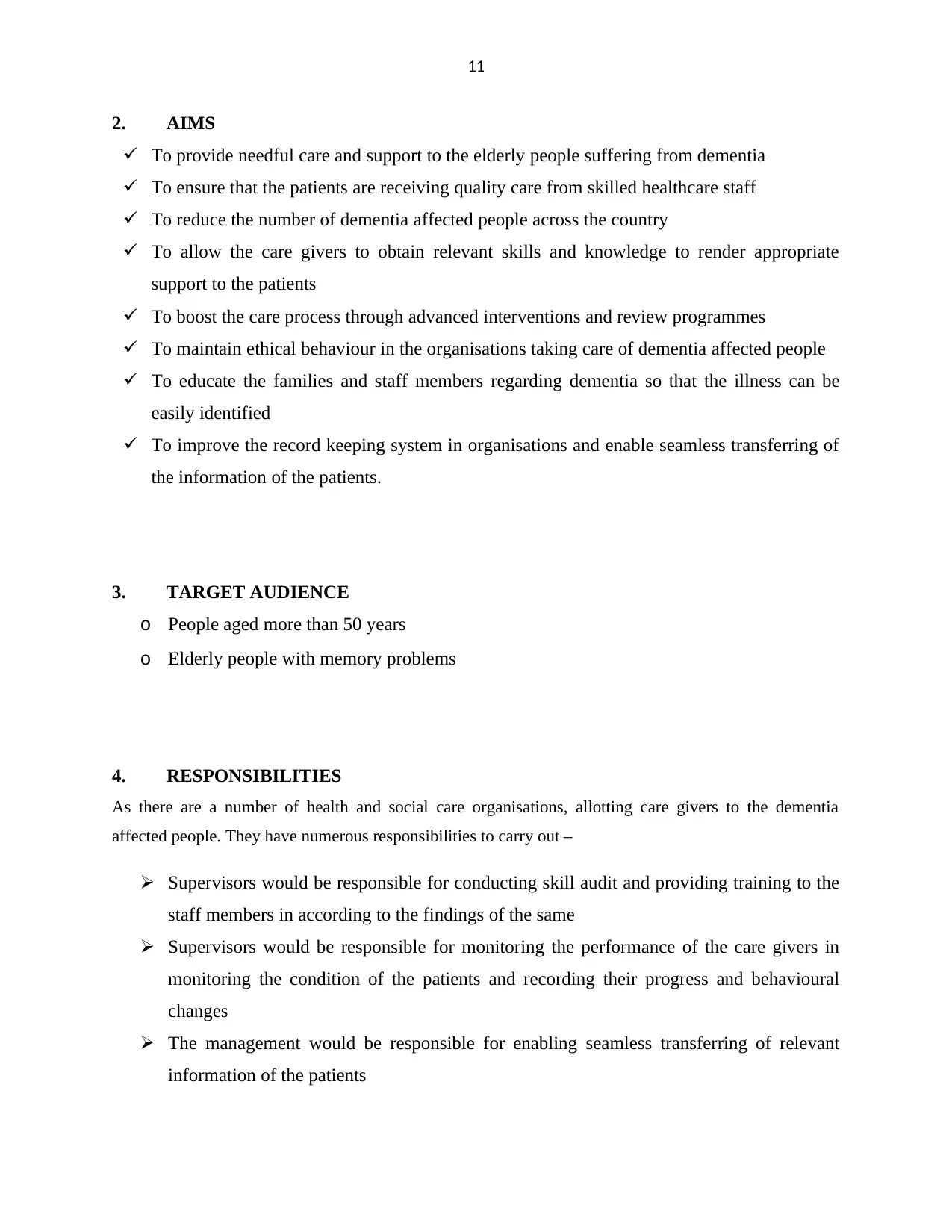
2. AIMS
To provide needful care and support to the elderly people suffering from dementia
To ensure that the patients are receiving quality care from skilled healthcare staff
To reduce the number of dementia affected people across the country
To allow the care givers to obtain relevant skills and knowledge to render appropriate
support to the patients
To boost the care process through advanced interventions and review programmes
To maintain ethical behaviour in the organisations taking care of dementia affected people
To educate the families and staff members regarding dementia so that the illness can be
easily identified
To improve the record keeping system in organisations and enable seamless transferring of
the information of the patients.
3. TARGET AUDIENCE
o People aged more than 50 years
o Elderly people with memory problems
4. RESPONSIBILITIES
As there are a number of health and social care organisations, allotting care givers to the dementia
affected people. They have numerous responsibilities to carry out –
Supervisors would be responsible for conducting skill audit and providing training to the
staff members in according to the findings of the same
Supervisors would be responsible for monitoring the performance of the care givers in
monitoring the condition of the patients and recording their progress and behavioural
changes
The management would be responsible for enabling seamless transferring of relevant
information of the patients
2. AIMS
To provide needful care and support to the elderly people suffering from dementia
To ensure that the patients are receiving quality care from skilled healthcare staff
To reduce the number of dementia affected people across the country
To allow the care givers to obtain relevant skills and knowledge to render appropriate
support to the patients
To boost the care process through advanced interventions and review programmes
To maintain ethical behaviour in the organisations taking care of dementia affected people
To educate the families and staff members regarding dementia so that the illness can be
easily identified
To improve the record keeping system in organisations and enable seamless transferring of
the information of the patients.
3. TARGET AUDIENCE
o People aged more than 50 years
o Elderly people with memory problems
4. RESPONSIBILITIES
As there are a number of health and social care organisations, allotting care givers to the dementia
affected people. They have numerous responsibilities to carry out –
Supervisors would be responsible for conducting skill audit and providing training to the
staff members in according to the findings of the same
Supervisors would be responsible for monitoring the performance of the care givers in
monitoring the condition of the patients and recording their progress and behavioural
changes
The management would be responsible for enabling seamless transferring of relevant
information of the patients
12
Staff members would be responsible for controlling their anger and irritation and behave
properly with the families of the patients
Care givers would be responsible for building a good rapport with the patient so that
deeper understanding can be obtained regarding their issues through effective
communication
Care givers would be responsible for gaining more skills and knowledge which can help
them providing required services to the patients
Care givers would be responsible for familiarising themselves with advanced procedures
to identify a dementia patient.
5. DEFINITIONS
Dementia is caused by impairment of brain cells which results in short term memory loss in the affected
person (Mol, Moser & Pols, 2015).
6. DOCUMENTATION
Cognitive testing is helpful for identification of a dementia affected person (Brooker & Latham, 2015).
7. REFERENCES
Beerens, H. C., Sutcliffe, C., Renom-Guiteras, A., Soto, M. E., Suhonen, R., Zabalegui, A., ... &
RightTimePlaceCare Consortium. (2014). Quality of life and quality of care for people with
dementia receiving long term institutional care or professional home care: the European
RightTimePlaceCare study. Journal of the American Medical Directors Association, 15(1), 54-
61.
Brooker, D., & Latham, I. (2015). Person-centred dementia care: Making services better with
the VIPS framework. Jessica Kingsley Publishers.
Staff members would be responsible for controlling their anger and irritation and behave
properly with the families of the patients
Care givers would be responsible for building a good rapport with the patient so that
deeper understanding can be obtained regarding their issues through effective
communication
Care givers would be responsible for gaining more skills and knowledge which can help
them providing required services to the patients
Care givers would be responsible for familiarising themselves with advanced procedures
to identify a dementia patient.
5. DEFINITIONS
Dementia is caused by impairment of brain cells which results in short term memory loss in the affected
person (Mol, Moser & Pols, 2015).
6. DOCUMENTATION
Cognitive testing is helpful for identification of a dementia affected person (Brooker & Latham, 2015).
7. REFERENCES
Beerens, H. C., Sutcliffe, C., Renom-Guiteras, A., Soto, M. E., Suhonen, R., Zabalegui, A., ... &
RightTimePlaceCare Consortium. (2014). Quality of life and quality of care for people with
dementia receiving long term institutional care or professional home care: the European
RightTimePlaceCare study. Journal of the American Medical Directors Association, 15(1), 54-
61.
Brooker, D., & Latham, I. (2015). Person-centred dementia care: Making services better with
the VIPS framework. Jessica Kingsley Publishers.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



