NRSG353 Case Study: Analysis of Congestive Cardiac Failure Patient
VerifiedAdded on 2023/06/15
|10
|2596
|447
Case Study
AI Summary
This case study comprehensively analyzes congestive cardiac failure, addressing its causes such as coronary artery disease, hypertension, dilated cardiomyopathy, thyroid disease, and diabetes, along with associated risk factors like high blood pressure, smoking, and obesity. It details the impact on patients, including depression and financial strain on families. The study identifies five common signs and symptoms—oedema, shortness of breath, nausea/vomiting, increased urination, and chest pain—linking each to its underlying pathophysiology. Furthermore, it describes two common drug classes, ACE inhibitors and angiotensin receptor blockers, explaining their physiological effects on the body. The analysis prioritizes nursing care strategies within the first 24 hours post-admission, emphasizing nursing assessment, diagnosis, planning, interventions, and evaluation, ensuring a holistic approach to patient care and management. Desklib offers a wealth of similar case studies and resources for students.

Running head: CONGESTIVE CARDIAC FAILURE
Congestive Cardiac Failure
Student’s Name
Institutional Affiliation
Congestive Cardiac Failure
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CONGESTIVE CARDIAC FAILURE 2
Congestive Cardiac Failure
Outline the causes, incidence and risk factors of the identified condition and how
it can impact on the patient and family (400 words)
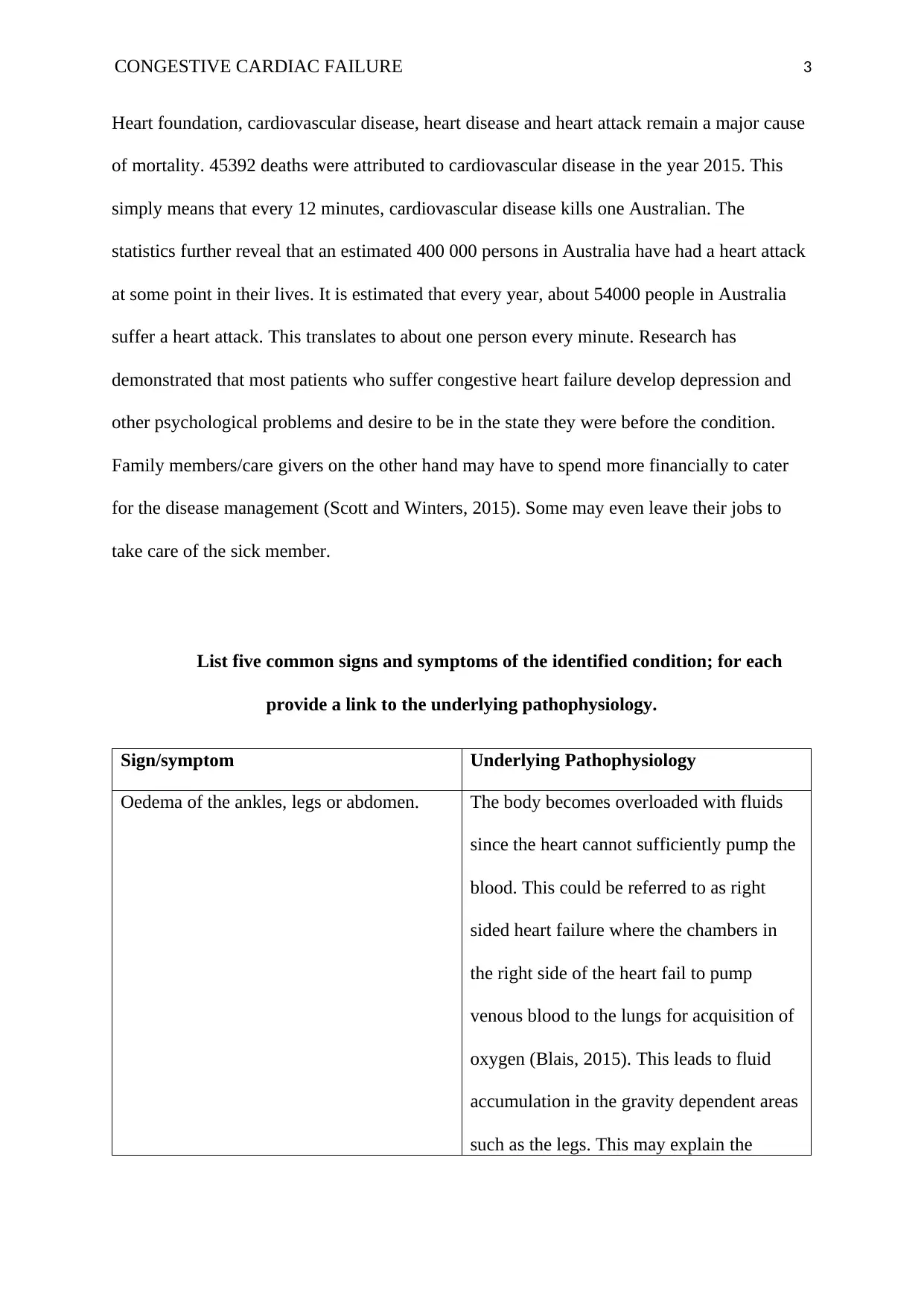
Congestive cardiac failure has several causes. One is coronary artery disease. In this
condition, a fat plaque develops in the coronary artery leading to its constriction. As a result,
blood flow to the heart muscle is significantly reduced. With time, the heart muscle dies
leading to myocardial infarction (Syed, 2014). The second cause of congestive cardiac failure
is high blood pressure (hypertension). In this situation, the heart muscles must do a lot of
work to pump blood due to factors such as constricted arteries or hypernatremia. With time,
the heart muscle may weaken which could cause congestive cardiac failure. The third cause is
dilated cardiomyopathy. This is a condition where the ventricles enlarge, and it is the third
most common cause of heart failure and heart transplants. Fourth, is thyroid disease. This
may be hyperthyroidism which causes rapid heartbeat or heart intolerance or hypothyroidism
which causes bradycardia (slow heart beat). Another cause is diabetes. According to Chin et
al (2014), diabetes causes heart failure indirectly through damaging kidneys and nerves.
Other causes include congenital heart defects, myocarditis, kidney disease, pericarditis,
hemochromatosis and amyloidosis.
There are several factors that increase the risk of congestive cardiac failure. If
unmonitored these factors have a high likelihood of resulting to heart failure. These include
high blood pressure, smoking, overweight and obesity, leading a physically inactive lifestyle,
having a family history of heart disease, having a high serum cholesterol, prediabetes and
diabetes, and having a family history of preeclampsia during pregnancy. As the risk factors
suggest, the lifestyle one leads including dietary habits and physical activity has some
relation with congestive heart failure (Edelmann et al, 2018). According to the Australian
Congestive Cardiac Failure
Outline the causes, incidence and risk factors of the identified condition and how
it can impact on the patient and family (400 words)
Congestive cardiac failure has several causes. One is coronary artery disease. In this
condition, a fat plaque develops in the coronary artery leading to its constriction. As a result,
blood flow to the heart muscle is significantly reduced. With time, the heart muscle dies
leading to myocardial infarction (Syed, 2014). The second cause of congestive cardiac failure
is high blood pressure (hypertension). In this situation, the heart muscles must do a lot of
work to pump blood due to factors such as constricted arteries or hypernatremia. With time,
the heart muscle may weaken which could cause congestive cardiac failure. The third cause is
dilated cardiomyopathy. This is a condition where the ventricles enlarge, and it is the third
most common cause of heart failure and heart transplants. Fourth, is thyroid disease. This
may be hyperthyroidism which causes rapid heartbeat or heart intolerance or hypothyroidism
which causes bradycardia (slow heart beat). Another cause is diabetes. According to Chin et
al (2014), diabetes causes heart failure indirectly through damaging kidneys and nerves.
Other causes include congenital heart defects, myocarditis, kidney disease, pericarditis,
hemochromatosis and amyloidosis.
There are several factors that increase the risk of congestive cardiac failure. If
unmonitored these factors have a high likelihood of resulting to heart failure. These include
high blood pressure, smoking, overweight and obesity, leading a physically inactive lifestyle,
having a family history of heart disease, having a high serum cholesterol, prediabetes and
diabetes, and having a family history of preeclampsia during pregnancy. As the risk factors
suggest, the lifestyle one leads including dietary habits and physical activity has some
relation with congestive heart failure (Edelmann et al, 2018). According to the Australian
CONGESTIVE CARDIAC FAILURE 3
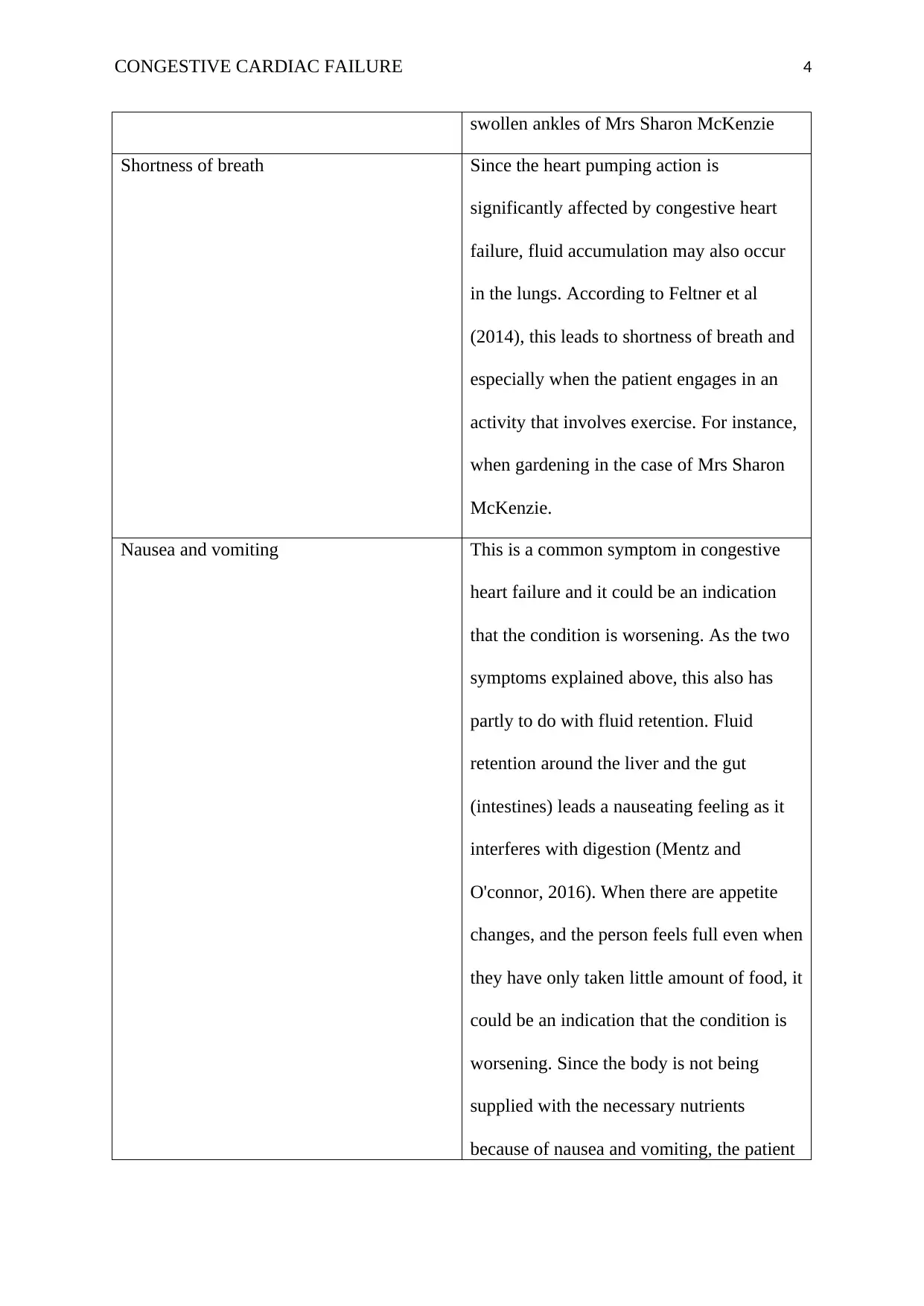
Heart foundation, cardiovascular disease, heart disease and heart attack remain a major cause
of mortality. 45392 deaths were attributed to cardiovascular disease in the year 2015. This
simply means that every 12 minutes, cardiovascular disease kills one Australian. The
statistics further reveal that an estimated 400 000 persons in Australia have had a heart attack
at some point in their lives. It is estimated that every year, about 54000 people in Australia
suffer a heart attack. This translates to about one person every minute. Research has
demonstrated that most patients who suffer congestive heart failure develop depression and
other psychological problems and desire to be in the state they were before the condition.
Family members/care givers on the other hand may have to spend more financially to cater
for the disease management (Scott and Winters, 2015). Some may even leave their jobs to
take care of the sick member.
List five common signs and symptoms of the identified condition; for each
provide a link to the underlying pathophysiology.
Sign/symptom Underlying Pathophysiology
Oedema of the ankles, legs or abdomen. The body becomes overloaded with fluids
since the heart cannot sufficiently pump the
blood. This could be referred to as right
sided heart failure where the chambers in
the right side of the heart fail to pump
venous blood to the lungs for acquisition of
oxygen (Blais, 2015). This leads to fluid
accumulation in the gravity dependent areas
such as the legs. This may explain the
Heart foundation, cardiovascular disease, heart disease and heart attack remain a major cause
of mortality. 45392 deaths were attributed to cardiovascular disease in the year 2015. This
simply means that every 12 minutes, cardiovascular disease kills one Australian. The
statistics further reveal that an estimated 400 000 persons in Australia have had a heart attack
at some point in their lives. It is estimated that every year, about 54000 people in Australia
suffer a heart attack. This translates to about one person every minute. Research has
demonstrated that most patients who suffer congestive heart failure develop depression and
other psychological problems and desire to be in the state they were before the condition.
Family members/care givers on the other hand may have to spend more financially to cater
for the disease management (Scott and Winters, 2015). Some may even leave their jobs to
take care of the sick member.
List five common signs and symptoms of the identified condition; for each
provide a link to the underlying pathophysiology.
Sign/symptom Underlying Pathophysiology
Oedema of the ankles, legs or abdomen. The body becomes overloaded with fluids
since the heart cannot sufficiently pump the
blood. This could be referred to as right
sided heart failure where the chambers in
the right side of the heart fail to pump
venous blood to the lungs for acquisition of
oxygen (Blais, 2015). This leads to fluid
accumulation in the gravity dependent areas
such as the legs. This may explain the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CONGESTIVE CARDIAC FAILURE 4
swollen ankles of Mrs Sharon McKenzie
Shortness of breath Since the heart pumping action is
significantly affected by congestive heart
failure, fluid accumulation may also occur
in the lungs. According to Feltner et al
(2014), this leads to shortness of breath and
especially when the patient engages in an
activity that involves exercise. For instance,
when gardening in the case of Mrs Sharon
McKenzie.
Nausea and vomiting This is a common symptom in congestive
heart failure and it could be an indication
that the condition is worsening. As the two
symptoms explained above, this also has
partly to do with fluid retention. Fluid
retention around the liver and the gut
(intestines) leads a nauseating feeling as it
interferes with digestion (Mentz and
O'connor, 2016). When there are appetite
changes, and the person feels full even when
they have only taken little amount of food, it
could be an indication that the condition is
worsening. Since the body is not being
supplied with the necessary nutrients
because of nausea and vomiting, the patient
swollen ankles of Mrs Sharon McKenzie
Shortness of breath Since the heart pumping action is
significantly affected by congestive heart
failure, fluid accumulation may also occur
in the lungs. According to Feltner et al
(2014), this leads to shortness of breath and
especially when the patient engages in an
activity that involves exercise. For instance,
when gardening in the case of Mrs Sharon
McKenzie.
Nausea and vomiting This is a common symptom in congestive
heart failure and it could be an indication
that the condition is worsening. As the two
symptoms explained above, this also has
partly to do with fluid retention. Fluid
retention around the liver and the gut
(intestines) leads a nauseating feeling as it
interferes with digestion (Mentz and
O'connor, 2016). When there are appetite
changes, and the person feels full even when
they have only taken little amount of food, it
could be an indication that the condition is
worsening. Since the body is not being
supplied with the necessary nutrients
because of nausea and vomiting, the patient
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CONGESTIVE CARDIAC FAILURE 5
becomes dizzy. This could explain the mild
nausea and dizziness of Mrs Sharon
McKenzie.
Nausea and vomiting could also be a side
effect of the drugs.
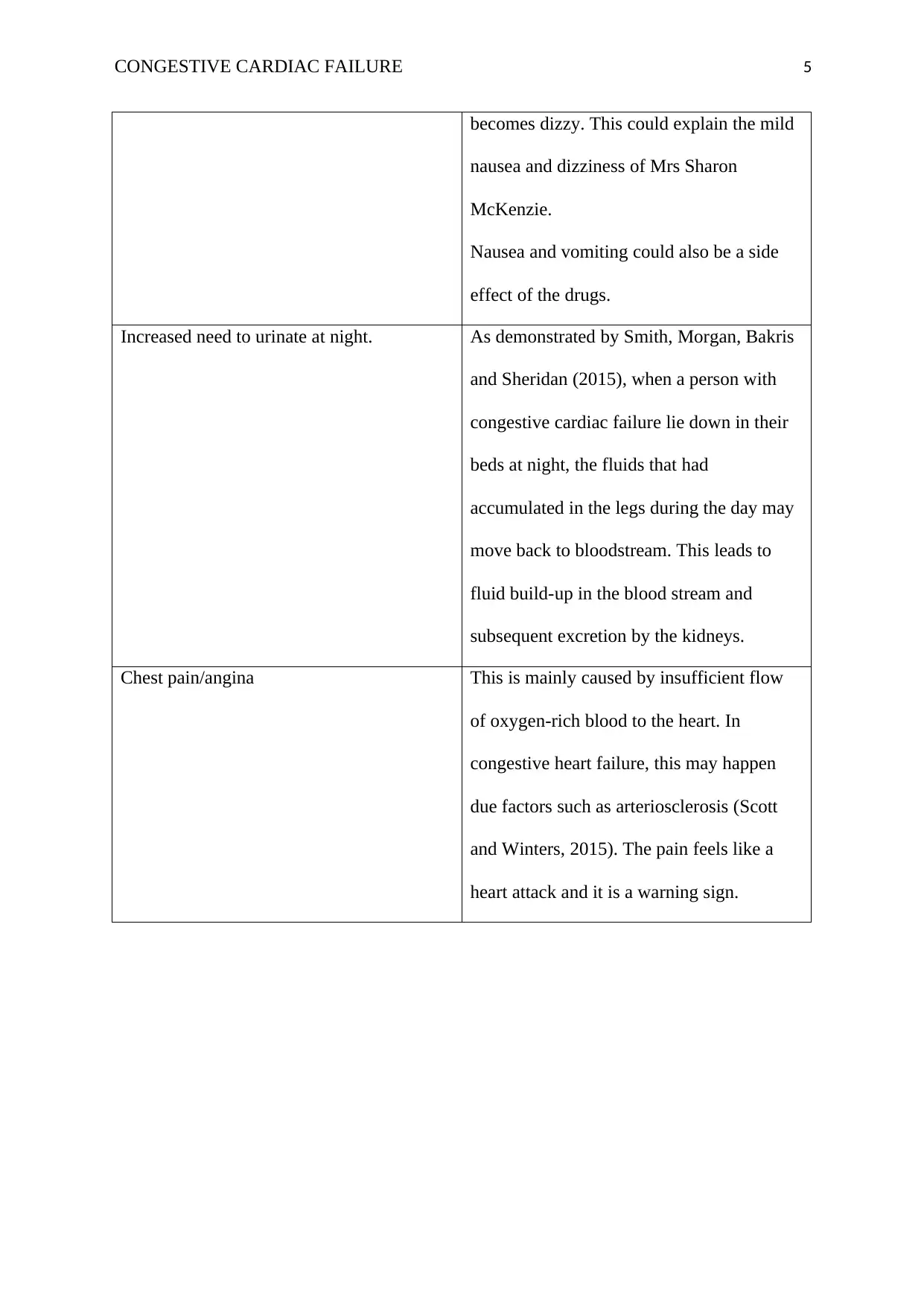
Increased need to urinate at night. As demonstrated by Smith, Morgan, Bakris
and Sheridan (2015), when a person with
congestive cardiac failure lie down in their
beds at night, the fluids that had
accumulated in the legs during the day may
move back to bloodstream. This leads to
fluid build-up in the blood stream and
subsequent excretion by the kidneys.
Chest pain/angina This is mainly caused by insufficient flow
of oxygen-rich blood to the heart. In
congestive heart failure, this may happen
due factors such as arteriosclerosis (Scott
and Winters, 2015). The pain feels like a
heart attack and it is a warning sign.
becomes dizzy. This could explain the mild
nausea and dizziness of Mrs Sharon
McKenzie.
Nausea and vomiting could also be a side
effect of the drugs.
Increased need to urinate at night. As demonstrated by Smith, Morgan, Bakris
and Sheridan (2015), when a person with
congestive cardiac failure lie down in their
beds at night, the fluids that had
accumulated in the legs during the day may
move back to bloodstream. This leads to
fluid build-up in the blood stream and
subsequent excretion by the kidneys.
Chest pain/angina This is mainly caused by insufficient flow
of oxygen-rich blood to the heart. In
congestive heart failure, this may happen
due factors such as arteriosclerosis (Scott
and Winters, 2015). The pain feels like a
heart attack and it is a warning sign.
CONGESTIVE CARDIAC FAILURE 6
Describe two common classes of drugs used for patients with the identified
condition including physiological effect of each class on the body.
The first class to be discussed will be Angiotensin-Converting Enzyme (ACE)
inhibitors. Angiotensin II is a chemical that is produced by the body and it circulates in the
blood primarily. According to Reddy, Melenovsky, Redfield, Nishimura, and Borlaug (2016),
this chemical causes contraction of the muscles surrounding the blood vessels. The result is
constriction of the blood vessels and a subsequent increase in blood pressure (hypertension).
This enzyme is formed through conversion of angiotensin I in the blood by the Angiotensin
Converting Enzyme (ACE). Angiotensin Converting Enzyme inhibitors (ACE inhibitors) are
medications/drugs that significantly slow or inhibit the activity of the ACE enzyme. As a
result, the blood vessels dilate, and blood pressure does not rise significantly. The reduction
in the blood pressure makes the process of pumping the blood smooth and may reduce to the
deterioration rate of a congestive cardiac failure (Poppas and Rounds, 2002). Therefore, this
class of drugs is very important in treatment and management of congestive cardiac failure
since in most cases the blood pressure is usually high. For instance, the blood pressure of Mrs
Sharon McKenzie is high at 170/110 mmHg.
The second class of drugs used in treatment and management of congestive cardiac
failure is angiotensin receptor blockers. As observed above, the chemical angiotensin causes
the muscles of blood vessel to contract leading to their constriction. Subsequently, the blood
pressure rises, and the heart must do more work to pump the blood. This is not desirable in
congestive heart failure as one of the goals to treatment is offer rest to the heart muscles.
Angiotensin receptor blockers are medications that lead to blocking of the binding of
angiotensin II to receptors found on the muscles surrounding the blood vessel walls. This
inhibition renders useless the work of the angiotensin II chemical as they cannot exert their
function without binding to the receptors (Morton, Fontaine, Hudak and Gallo, 2017).
Describe two common classes of drugs used for patients with the identified
condition including physiological effect of each class on the body.
The first class to be discussed will be Angiotensin-Converting Enzyme (ACE)
inhibitors. Angiotensin II is a chemical that is produced by the body and it circulates in the
blood primarily. According to Reddy, Melenovsky, Redfield, Nishimura, and Borlaug (2016),
this chemical causes contraction of the muscles surrounding the blood vessels. The result is
constriction of the blood vessels and a subsequent increase in blood pressure (hypertension).
This enzyme is formed through conversion of angiotensin I in the blood by the Angiotensin
Converting Enzyme (ACE). Angiotensin Converting Enzyme inhibitors (ACE inhibitors) are
medications/drugs that significantly slow or inhibit the activity of the ACE enzyme. As a
result, the blood vessels dilate, and blood pressure does not rise significantly. The reduction
in the blood pressure makes the process of pumping the blood smooth and may reduce to the
deterioration rate of a congestive cardiac failure (Poppas and Rounds, 2002). Therefore, this
class of drugs is very important in treatment and management of congestive cardiac failure
since in most cases the blood pressure is usually high. For instance, the blood pressure of Mrs
Sharon McKenzie is high at 170/110 mmHg.
The second class of drugs used in treatment and management of congestive cardiac
failure is angiotensin receptor blockers. As observed above, the chemical angiotensin causes
the muscles of blood vessel to contract leading to their constriction. Subsequently, the blood
pressure rises, and the heart must do more work to pump the blood. This is not desirable in
congestive heart failure as one of the goals to treatment is offer rest to the heart muscles.
Angiotensin receptor blockers are medications that lead to blocking of the binding of
angiotensin II to receptors found on the muscles surrounding the blood vessel walls. This
inhibition renders useless the work of the angiotensin II chemical as they cannot exert their
function without binding to the receptors (Morton, Fontaine, Hudak and Gallo, 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CONGESTIVE CARDIAC FAILURE 7
Consequently, the blood vessels dilate, and the blood pressure is reduced. The heart muscles
are accorded rest as a result since the heart does not have to do a lot of work to pump the
blood. In this way, these types of medications come in handy to treat and manage congestive
heart failure and prevent further deterioration of the heart muscle.
Identify and explain, in order of priority the nursing care strategies you, as the
registered nurse, should use within the first 24 hours post admission for this patient.
The first step would be nursing assessment. This would include several aspects such
as health history and physical examination. In health history, the assessment would include
the following: an assessment of the signs and symptoms such as oedema, shortness of breath
and dizziness/fatigue; exploring the patient’s level of understanding, the self-management
strategies employed and the willingness to adhere to the strategies. The physical examination
would include an assessment of the following: auscultating the lungs to detect whether there
are wheezes or crackles; assessing the JVD to detect any distension; assessing the liver for
hepatojugular reflux; assess the parts of the body that are dependent for oedema and
perfusion.
The next step would be developing a diagnosis. This would be guided by the
assessment data collected. The diagnosis could be the following for Mrs Sharon McKenzie:
excess fluid volume related to congestive heart failure and activity intolerance related to
decreased cardiac output. After coming up with appropriate diagnosis, the next thing to do
should be coming up with a plan and goals of management. These could focus on the
following: achieving a reduction in fatigue, relieving fluid overload (oedema) symptoms,
promoting physical activity and teaching the patient about the program of self-care.
Consequently, the blood vessels dilate, and the blood pressure is reduced. The heart muscles
are accorded rest as a result since the heart does not have to do a lot of work to pump the
blood. In this way, these types of medications come in handy to treat and manage congestive
heart failure and prevent further deterioration of the heart muscle.
Identify and explain, in order of priority the nursing care strategies you, as the
registered nurse, should use within the first 24 hours post admission for this patient.
The first step would be nursing assessment. This would include several aspects such
as health history and physical examination. In health history, the assessment would include
the following: an assessment of the signs and symptoms such as oedema, shortness of breath
and dizziness/fatigue; exploring the patient’s level of understanding, the self-management
strategies employed and the willingness to adhere to the strategies. The physical examination
would include an assessment of the following: auscultating the lungs to detect whether there
are wheezes or crackles; assessing the JVD to detect any distension; assessing the liver for
hepatojugular reflux; assess the parts of the body that are dependent for oedema and
perfusion.
The next step would be developing a diagnosis. This would be guided by the
assessment data collected. The diagnosis could be the following for Mrs Sharon McKenzie:
excess fluid volume related to congestive heart failure and activity intolerance related to
decreased cardiac output. After coming up with appropriate diagnosis, the next thing to do
should be coming up with a plan and goals of management. These could focus on the
following: achieving a reduction in fatigue, relieving fluid overload (oedema) symptoms,
promoting physical activity and teaching the patient about the program of self-care.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CONGESTIVE CARDIAC FAILURE 8
The next step would be developing nursing interventions. Examples of such
interventions are explained next. One is promoting the tolerance of activity. This could be
achieved through a mild to moderate physical exercise for a total of 30 minutes each day. The
nurse and the physician could collaborate to come up with a schedule that promotes pacing
and prioritization of activities. The second nursing intervention could be managing the fluid
volume. The fluid status of the patient should be monitored closely and ensure a plan that
leads to normal fluid status. For instance, the patient should be on sodium restricted diet and
taking their medication as prescribed. These are some of the interventions that could lead to
efficient treatment of the patient. After identifying the nursing strategies, the following step
would be developing nursing priorities. These could include the following: improvement of
the myocardial contractility; reducing the volume of fluid overload and prevention of
complications, provision of information about disease, the therapeutic needs and prevention
of recurrences.
The next step would be evaluation. The evaluation would be based on the patient’s
expected outcomes. The following could be evaluated: tolerance for increased activity,
achievement and maintenance of fluid balance and adherence to the self-care regimen. As
part of the care process, it is also important that documentation be done. The documentation
should include the following: findings of the assessment; balance of the fluid intake and
output; the degree to which fluid retention is taking place; results from laboratory tests and
other diagnosis; patient’s response to treatment, education offered, and other interventions
offered and achievement or progress towards desired outcomes.
The next step would be developing nursing interventions. Examples of such
interventions are explained next. One is promoting the tolerance of activity. This could be
achieved through a mild to moderate physical exercise for a total of 30 minutes each day. The
nurse and the physician could collaborate to come up with a schedule that promotes pacing
and prioritization of activities. The second nursing intervention could be managing the fluid
volume. The fluid status of the patient should be monitored closely and ensure a plan that
leads to normal fluid status. For instance, the patient should be on sodium restricted diet and
taking their medication as prescribed. These are some of the interventions that could lead to
efficient treatment of the patient. After identifying the nursing strategies, the following step
would be developing nursing priorities. These could include the following: improvement of
the myocardial contractility; reducing the volume of fluid overload and prevention of
complications, provision of information about disease, the therapeutic needs and prevention
of recurrences.
The next step would be evaluation. The evaluation would be based on the patient’s
expected outcomes. The following could be evaluated: tolerance for increased activity,
achievement and maintenance of fluid balance and adherence to the self-care regimen. As
part of the care process, it is also important that documentation be done. The documentation
should include the following: findings of the assessment; balance of the fluid intake and
output; the degree to which fluid retention is taking place; results from laboratory tests and
other diagnosis; patient’s response to treatment, education offered, and other interventions
offered and achievement or progress towards desired outcomes.
CONGESTIVE CARDIAC FAILURE 9
References
Blais, K. (2015). Professional nursing practice: Concepts and perspectives. Pearson.
Chin, M. P., Wrolstad, D., Bakris, G. L., Chertow, G. M., de Zeeuw, D., Goldsberry, A., ... &
Meyer, C. J. (2014). Risk factors for heart failure in patients with type 2 diabetes
mellitus and stage 4 chronic kidney disease treated with bardoxolone methyl. Journal
of cardiac failure, 20(12), 953-958.
Edelmann, F., Knosalla, C., Mörike, K., Muth, C., Prien, P., Störk, S., ... & Group, H. F. D.
(2018). Chronic Heart Failure. Deutsches Ärzteblatt International, 115(8), 124.
Feltner, C., Jones, C. D., Cené, C. W., Zheng, Z. J., Sueta, C. A., Coker-Schwimmer, E. J., ...
& Jonas, D. E. (2014). Transitional care interventions to prevent readmissions for
persons with heart failure: a systematic review and meta-analysis. Annals of internal
medicine, 160(11), 774-784.
Mentz, R. J., & O'connor, C. M. (2016). Pathophysiology and clinical evaluation of acute
heart failure. Nature Reviews Cardiology, 13(1), 28.
Morrissey, R. P., Czer, L., & Shah, P. K. (2011). Chronic heart failure. American Journal of
Cardiovascular Drugs, 11(3), 153-171.
Morton, P. G., Fontaine, D., Hudak, C. M., & Gallo, B. M. (2017). Critical care nursing: a
holistic approach (p. 1056). Lippincott Williams & Wilkins.
Poppas, A., & Rounds, S. (2002). Congestive heart failure. American journal of respiratory
and critical care medicine, 165(1), 4-8.
Reddy, Y. N., Melenovsky, V., Redfield, M. M., Nishimura, R. A., & Borlaug, B. A. (2016).
High-output heart failure: a 15-year experience. Journal of the American College of
Cardiology, 68(5), 473-482.
References
Blais, K. (2015). Professional nursing practice: Concepts and perspectives. Pearson.
Chin, M. P., Wrolstad, D., Bakris, G. L., Chertow, G. M., de Zeeuw, D., Goldsberry, A., ... &
Meyer, C. J. (2014). Risk factors for heart failure in patients with type 2 diabetes
mellitus and stage 4 chronic kidney disease treated with bardoxolone methyl. Journal
of cardiac failure, 20(12), 953-958.
Edelmann, F., Knosalla, C., Mörike, K., Muth, C., Prien, P., Störk, S., ... & Group, H. F. D.
(2018). Chronic Heart Failure. Deutsches Ärzteblatt International, 115(8), 124.
Feltner, C., Jones, C. D., Cené, C. W., Zheng, Z. J., Sueta, C. A., Coker-Schwimmer, E. J., ...
& Jonas, D. E. (2014). Transitional care interventions to prevent readmissions for
persons with heart failure: a systematic review and meta-analysis. Annals of internal
medicine, 160(11), 774-784.
Mentz, R. J., & O'connor, C. M. (2016). Pathophysiology and clinical evaluation of acute
heart failure. Nature Reviews Cardiology, 13(1), 28.
Morrissey, R. P., Czer, L., & Shah, P. K. (2011). Chronic heart failure. American Journal of
Cardiovascular Drugs, 11(3), 153-171.
Morton, P. G., Fontaine, D., Hudak, C. M., & Gallo, B. M. (2017). Critical care nursing: a
holistic approach (p. 1056). Lippincott Williams & Wilkins.
Poppas, A., & Rounds, S. (2002). Congestive heart failure. American journal of respiratory
and critical care medicine, 165(1), 4-8.
Reddy, Y. N., Melenovsky, V., Redfield, M. M., Nishimura, R. A., & Borlaug, B. A. (2016).
High-output heart failure: a 15-year experience. Journal of the American College of
Cardiology, 68(5), 473-482.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CONGESTIVE CARDIAC FAILURE
10
Scott, M. C., & Winters, M. E. (2015). Congestive heart failure. Emergency Medicine
Clinics, 33(3), 553-562.
Shah, K., Parekh, N., Clopton, P., Anand, I., Christenson, R., Daniels, L., ... & Neath, S. X.
(2018). Improved survival in patients with diastolic heart failure discharged on beta-
blocker and ace inhibitors. Journal of the American College of Cardiology, 61(10
Supplement), E634.
Smith, T. W., Morgan, J. P., Bakris, G. L., & Sheridan, A. M. (2015). Differences between
angiotensin converting enzyme inhibitors and receptor blockers. UpToDate.
http://www. uptodate. com/contents/differences-between-angiotensinconverting-
enzyme-inhibitors-and-receptor-blockers. Accessed December, 29.
Syed, S. (2014). Congestive Cardiac Failure.
10
Scott, M. C., & Winters, M. E. (2015). Congestive heart failure. Emergency Medicine
Clinics, 33(3), 553-562.
Shah, K., Parekh, N., Clopton, P., Anand, I., Christenson, R., Daniels, L., ... & Neath, S. X.
(2018). Improved survival in patients with diastolic heart failure discharged on beta-
blocker and ace inhibitors. Journal of the American College of Cardiology, 61(10
Supplement), E634.
Smith, T. W., Morgan, J. P., Bakris, G. L., & Sheridan, A. M. (2015). Differences between
angiotensin converting enzyme inhibitors and receptor blockers. UpToDate.
http://www. uptodate. com/contents/differences-between-angiotensinconverting-
enzyme-inhibitors-and-receptor-blockers. Accessed December, 29.
Syed, S. (2014). Congestive Cardiac Failure.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





