NRSG353 Assignment: Detailed Analysis of Liver Cirrhosis Case
VerifiedAdded on 2023/04/24
|12
|2912
|140
Report
AI Summary
This report provides a detailed analysis of a liver cirrhosis case study, focusing on a 48-year-old male patient. The report outlines the disease, causes, incidence, and risk factors of liver cirrhosis, discussing its impact on the patient and his family. It examines three common signs and symptoms, explaining their underlying pathophysiology. The report further delves into the pharmacodynamics and pharmacokinetics of beta-blockers, a common class of drugs relevant to the patient's condition. Finally, it develops a prioritized nursing care plan for the patient upon admission, detailing goals, interventions, and rationales for the first eight hours. The report utilizes citations to support all information presented.

Running head: DETAIL ANALYSIS ON LIVER CIRHOSSIS
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Name of the Student:
Name of the University:
Author note:
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Name of the Student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Q1) Outline the disease, causes, incidence and risk factors. Discuss the impact of the selected
disease on the patient and their family
Liver cirrhosis results due to liver damage, when scar tissue replaces the healthy cells
in the body. In this condition, the liver is incapable to carry out any vital activities such as
production and metabolism of proteins, filtering of toxins and drugs and production of blood
coagulation factors (Healthdirect.gov.au, 2019).
There are many causes responsible for liver cirrhosis resulting in liver fail or damage.
The common causes of liver cirrhosis includes consumption of excess alcohol, long-term
infection from hepatitis C and hepatitis B, accumulation of additional fat or fatty liver,
autoimmune diseases associated with liver such as autoimmune hepatitis, congenital liver
diseases like haemochromatosis and alcohol-associated liver disease, which include non-
alcoholic steatohepatitis (NASH) and non-alcoholic fatty liver disease (NAFLD)
(Betterhealth.vic.gov.au, 2019).
The death rate directly linked to the alcohol consumption has decreased over years as
compared to the mortality rate in 1990s. The Australian Bureau of Statistics (ABS) compared
the mortality rate and recorded 5.1 demises per 100,000 Australians in the year 2017. In
2017, 1,336 death were recorded due to alcohol consumption with higher incidence in males
as compared to females (Abs.gov.au, 2019). Alcohol-related liver disease is considered as the
most significant sponsor in mortality gap of Australia including both females and males with
an approximate age of 35-54 years. In United Nations, approximately 88,000 people die due
to alcohol-associated disease. Hence, alcohol is marked as the fourth chief preventable reason
of demise in United Nations (Mokdad et al., 2014).
The various risk factors associated with liver leading to the condition of liver cirrhosis
includes the following (Tsochatzis, Bosch & Burroughs, 2014):
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Q1) Outline the disease, causes, incidence and risk factors. Discuss the impact of the selected
disease on the patient and their family
Liver cirrhosis results due to liver damage, when scar tissue replaces the healthy cells
in the body. In this condition, the liver is incapable to carry out any vital activities such as
production and metabolism of proteins, filtering of toxins and drugs and production of blood
coagulation factors (Healthdirect.gov.au, 2019).
There are many causes responsible for liver cirrhosis resulting in liver fail or damage.
The common causes of liver cirrhosis includes consumption of excess alcohol, long-term
infection from hepatitis C and hepatitis B, accumulation of additional fat or fatty liver,
autoimmune diseases associated with liver such as autoimmune hepatitis, congenital liver
diseases like haemochromatosis and alcohol-associated liver disease, which include non-
alcoholic steatohepatitis (NASH) and non-alcoholic fatty liver disease (NAFLD)
(Betterhealth.vic.gov.au, 2019).
The death rate directly linked to the alcohol consumption has decreased over years as
compared to the mortality rate in 1990s. The Australian Bureau of Statistics (ABS) compared
the mortality rate and recorded 5.1 demises per 100,000 Australians in the year 2017. In
2017, 1,336 death were recorded due to alcohol consumption with higher incidence in males
as compared to females (Abs.gov.au, 2019). Alcohol-related liver disease is considered as the
most significant sponsor in mortality gap of Australia including both females and males with
an approximate age of 35-54 years. In United Nations, approximately 88,000 people die due
to alcohol-associated disease. Hence, alcohol is marked as the fourth chief preventable reason
of demise in United Nations (Mokdad et al., 2014).
The various risk factors associated with liver leading to the condition of liver cirrhosis
includes the following (Tsochatzis, Bosch & Burroughs, 2014):
2
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Chronic hepatitis B
Chronic hepatitis C
Excess intake of alcohol and cigarette smoking
Autoimmune liver sickness such as biliary cirrhosis, autoimmune hepatitis and
sclerosing cholangitis.
Rare inherited alcohol-associated liver disease, Wilson disease and hemochromatosis.
Overweight and obesity
Sustained exposure to poisonous chemicals
In the case study, the patient used to smoke and consume alcohol every day. He had a
previous history of drug abuse. He was also diagnosed with Hepatitis C approximately 10
years ago. These risk factors were responsible for the bad condition of James, which
eventually lead to advancement of his liver impairment. With the increasing complexity of
hepatocytes progression in the patient, the severity level of liver damage was increasing,
which ultimately lead to symptomatic liver cirrhosis.
The deteriorating health condition of the patient was effecting his and family’s quality of
life, which included emotional, physical, social and financial conditions (Potosek et al.,
2014). The factors such as muscle cramps, weight loss and reduced appetite had decreased
the physical ability of the patient to involve with his kids activity, hence reducing his quality
time with his family. As the patient was a truck driver, he was not financially sound and
could possibly lose his work due to his bad health, which would have a negative impact on
the care taking of his family, increasing the possibility of emotional conflict and financial
strain.
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Chronic hepatitis B
Chronic hepatitis C
Excess intake of alcohol and cigarette smoking
Autoimmune liver sickness such as biliary cirrhosis, autoimmune hepatitis and
sclerosing cholangitis.
Rare inherited alcohol-associated liver disease, Wilson disease and hemochromatosis.
Overweight and obesity
Sustained exposure to poisonous chemicals
In the case study, the patient used to smoke and consume alcohol every day. He had a
previous history of drug abuse. He was also diagnosed with Hepatitis C approximately 10
years ago. These risk factors were responsible for the bad condition of James, which
eventually lead to advancement of his liver impairment. With the increasing complexity of
hepatocytes progression in the patient, the severity level of liver damage was increasing,
which ultimately lead to symptomatic liver cirrhosis.
The deteriorating health condition of the patient was effecting his and family’s quality of
life, which included emotional, physical, social and financial conditions (Potosek et al.,
2014). The factors such as muscle cramps, weight loss and reduced appetite had decreased
the physical ability of the patient to involve with his kids activity, hence reducing his quality
time with his family. As the patient was a truck driver, he was not financially sound and
could possibly lose his work due to his bad health, which would have a negative impact on
the care taking of his family, increasing the possibility of emotional conflict and financial
strain.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
DETAIL ANALYSIS ON LIVER CIRRHOSIS
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
DETAIL ANALYSIS ON LIVER CIRRHOSIS
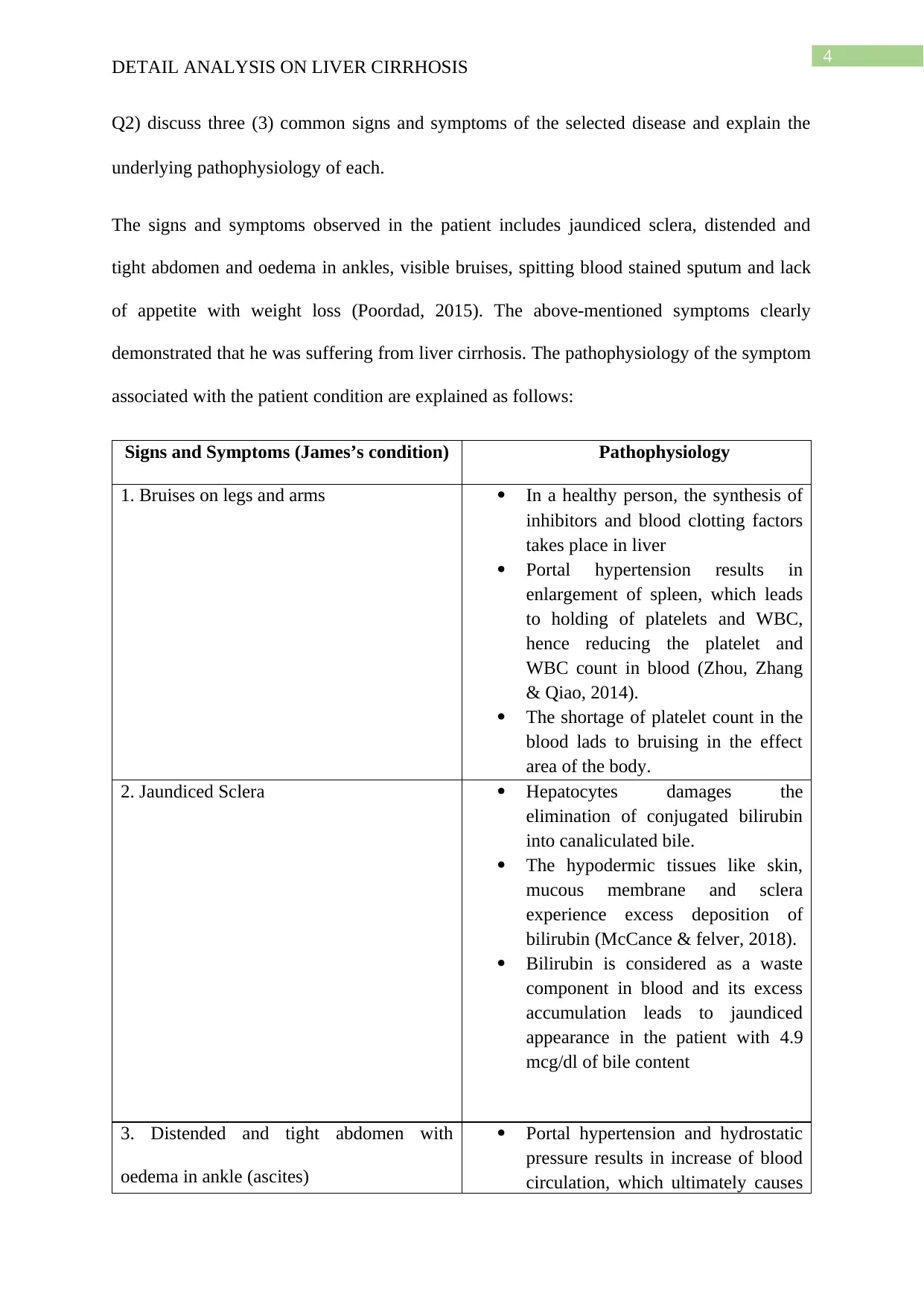
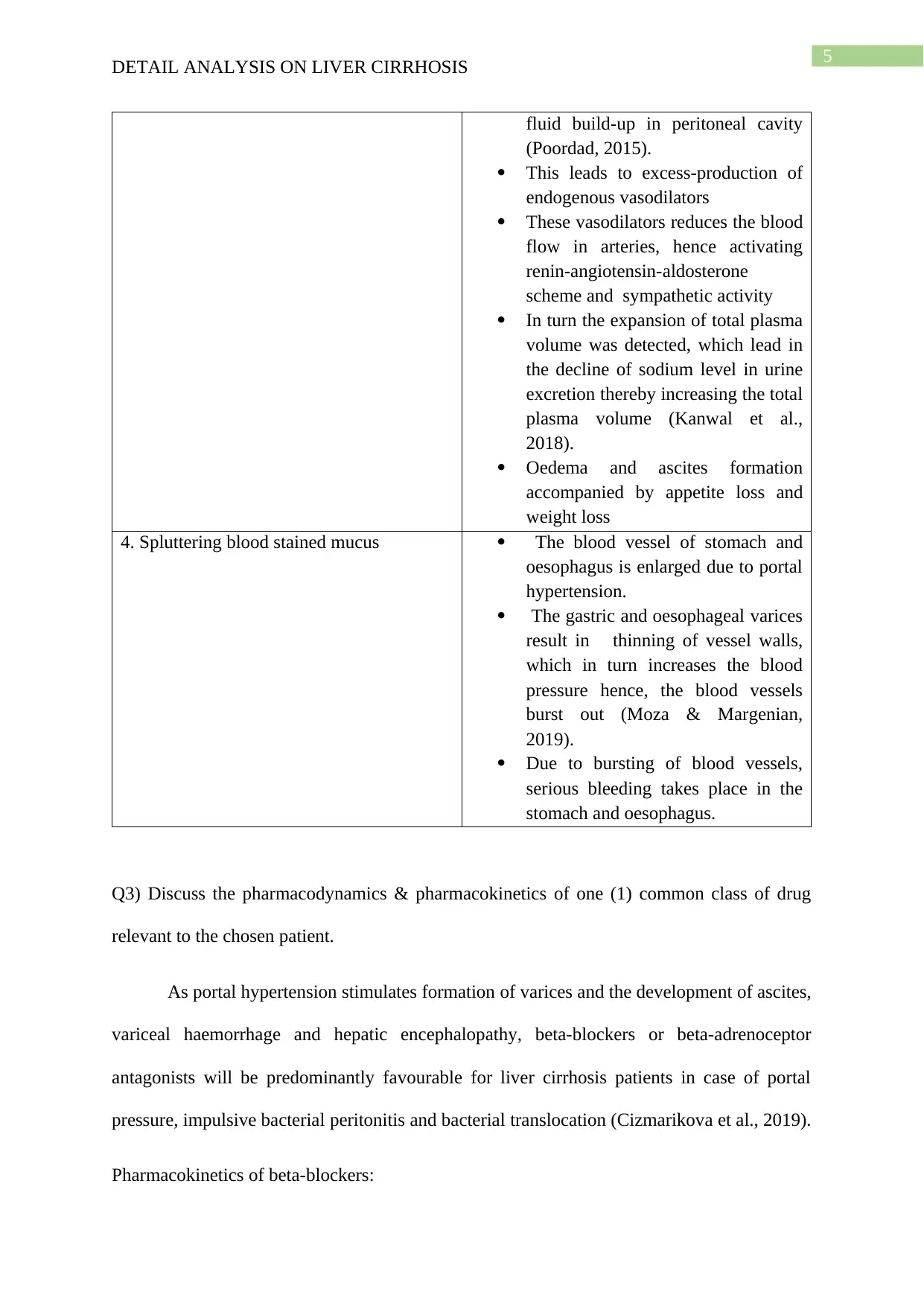
Q2) discuss three (3) common signs and symptoms of the selected disease and explain the
underlying pathophysiology of each.
The signs and symptoms observed in the patient includes jaundiced sclera, distended and
tight abdomen and oedema in ankles, visible bruises, spitting blood stained sputum and lack
of appetite with weight loss (Poordad, 2015). The above-mentioned symptoms clearly
demonstrated that he was suffering from liver cirrhosis. The pathophysiology of the symptom
associated with the patient condition are explained as follows:
Signs and Symptoms (James’s condition) Pathophysiology
1. Bruises on legs and arms In a healthy person, the synthesis of
inhibitors and blood clotting factors
takes place in liver
Portal hypertension results in
enlargement of spleen, which leads
to holding of platelets and WBC,
hence reducing the platelet and
WBC count in blood (Zhou, Zhang
& Qiao, 2014).
The shortage of platelet count in the
blood lads to bruising in the effect
area of the body.
2. Jaundiced Sclera Hepatocytes damages the
elimination of conjugated bilirubin
into canaliculated bile.
The hypodermic tissues like skin,
mucous membrane and sclera
experience excess deposition of
bilirubin (McCance & felver, 2018).
Bilirubin is considered as a waste
component in blood and its excess
accumulation leads to jaundiced
appearance in the patient with 4.9
mcg/dl of bile content
3. Distended and tight abdomen with
oedema in ankle (ascites)
Portal hypertension and hydrostatic
pressure results in increase of blood
circulation, which ultimately causes
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Q2) discuss three (3) common signs and symptoms of the selected disease and explain the
underlying pathophysiology of each.
The signs and symptoms observed in the patient includes jaundiced sclera, distended and
tight abdomen and oedema in ankles, visible bruises, spitting blood stained sputum and lack
of appetite with weight loss (Poordad, 2015). The above-mentioned symptoms clearly
demonstrated that he was suffering from liver cirrhosis. The pathophysiology of the symptom
associated with the patient condition are explained as follows:
Signs and Symptoms (James’s condition) Pathophysiology
1. Bruises on legs and arms In a healthy person, the synthesis of
inhibitors and blood clotting factors
takes place in liver
Portal hypertension results in
enlargement of spleen, which leads
to holding of platelets and WBC,
hence reducing the platelet and
WBC count in blood (Zhou, Zhang
& Qiao, 2014).
The shortage of platelet count in the
blood lads to bruising in the effect
area of the body.
2. Jaundiced Sclera Hepatocytes damages the
elimination of conjugated bilirubin
into canaliculated bile.
The hypodermic tissues like skin,
mucous membrane and sclera
experience excess deposition of
bilirubin (McCance & felver, 2018).
Bilirubin is considered as a waste
component in blood and its excess
accumulation leads to jaundiced
appearance in the patient with 4.9
mcg/dl of bile content
3. Distended and tight abdomen with
oedema in ankle (ascites)
Portal hypertension and hydrostatic
pressure results in increase of blood
circulation, which ultimately causes
5
DETAIL ANALYSIS ON LIVER CIRRHOSIS
fluid build-up in peritoneal cavity
(Poordad, 2015).
This leads to excess-production of
endogenous vasodilators
These vasodilators reduces the blood
flow in arteries, hence activating
renin-angiotensin-aldosterone
scheme and sympathetic activity
In turn the expansion of total plasma
volume was detected, which lead in
the decline of sodium level in urine
excretion thereby increasing the total
plasma volume (Kanwal et al.,
2018).
Oedema and ascites formation
accompanied by appetite loss and
weight loss
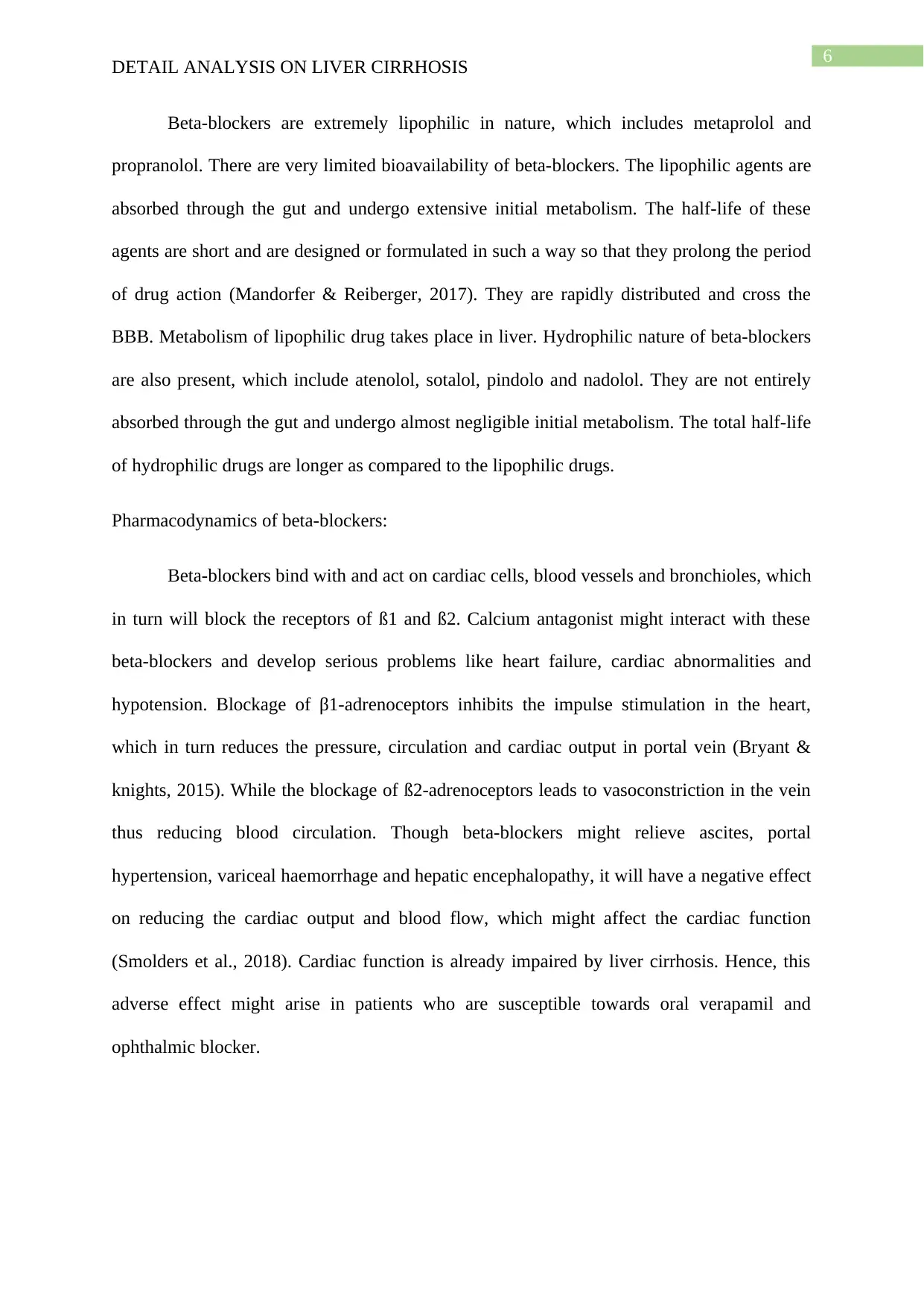
4. Spluttering blood stained mucus The blood vessel of stomach and
oesophagus is enlarged due to portal
hypertension.
The gastric and oesophageal varices
result in thinning of vessel walls,
which in turn increases the blood
pressure hence, the blood vessels
burst out (Moza & Margenian,
2019).
Due to bursting of blood vessels,
serious bleeding takes place in the
stomach and oesophagus.
Q3) Discuss the pharmacodynamics & pharmacokinetics of one (1) common class of drug
relevant to the chosen patient.
As portal hypertension stimulates formation of varices and the development of ascites,
variceal haemorrhage and hepatic encephalopathy, beta-blockers or beta-adrenoceptor
antagonists will be predominantly favourable for liver cirrhosis patients in case of portal
pressure, impulsive bacterial peritonitis and bacterial translocation (Cizmarikova et al., 2019).
Pharmacokinetics of beta-blockers:
DETAIL ANALYSIS ON LIVER CIRRHOSIS
fluid build-up in peritoneal cavity
(Poordad, 2015).
This leads to excess-production of
endogenous vasodilators
These vasodilators reduces the blood
flow in arteries, hence activating
renin-angiotensin-aldosterone
scheme and sympathetic activity
In turn the expansion of total plasma
volume was detected, which lead in
the decline of sodium level in urine
excretion thereby increasing the total
plasma volume (Kanwal et al.,
2018).
Oedema and ascites formation
accompanied by appetite loss and
weight loss
4. Spluttering blood stained mucus The blood vessel of stomach and
oesophagus is enlarged due to portal
hypertension.
The gastric and oesophageal varices
result in thinning of vessel walls,
which in turn increases the blood
pressure hence, the blood vessels
burst out (Moza & Margenian,
2019).
Due to bursting of blood vessels,
serious bleeding takes place in the
stomach and oesophagus.
Q3) Discuss the pharmacodynamics & pharmacokinetics of one (1) common class of drug
relevant to the chosen patient.
As portal hypertension stimulates formation of varices and the development of ascites,
variceal haemorrhage and hepatic encephalopathy, beta-blockers or beta-adrenoceptor
antagonists will be predominantly favourable for liver cirrhosis patients in case of portal
pressure, impulsive bacterial peritonitis and bacterial translocation (Cizmarikova et al., 2019).
Pharmacokinetics of beta-blockers:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Beta-blockers are extremely lipophilic in nature, which includes metaprolol and
propranolol. There are very limited bioavailability of beta-blockers. The lipophilic agents are
absorbed through the gut and undergo extensive initial metabolism. The half-life of these
agents are short and are designed or formulated in such a way so that they prolong the period
of drug action (Mandorfer & Reiberger, 2017). They are rapidly distributed and cross the
BBB. Metabolism of lipophilic drug takes place in liver. Hydrophilic nature of beta-blockers
are also present, which include atenolol, sotalol, pindolo and nadolol. They are not entirely
absorbed through the gut and undergo almost negligible initial metabolism. The total half-life
of hydrophilic drugs are longer as compared to the lipophilic drugs.
Pharmacodynamics of beta-blockers:
Beta-blockers bind with and act on cardiac cells, blood vessels and bronchioles, which
in turn will block the receptors of ß1 and ß2. Calcium antagonist might interact with these
beta-blockers and develop serious problems like heart failure, cardiac abnormalities and
hypotension. Blockage of β1-adrenoceptors inhibits the impulse stimulation in the heart,
which in turn reduces the pressure, circulation and cardiac output in portal vein (Bryant &
knights, 2015). While the blockage of ß2-adrenoceptors leads to vasoconstriction in the vein
thus reducing blood circulation. Though beta-blockers might relieve ascites, portal
hypertension, variceal haemorrhage and hepatic encephalopathy, it will have a negative effect
on reducing the cardiac output and blood flow, which might affect the cardiac function
(Smolders et al., 2018). Cardiac function is already impaired by liver cirrhosis. Hence, this
adverse effect might arise in patients who are susceptible towards oral verapamil and
ophthalmic blocker.
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Beta-blockers are extremely lipophilic in nature, which includes metaprolol and
propranolol. There are very limited bioavailability of beta-blockers. The lipophilic agents are
absorbed through the gut and undergo extensive initial metabolism. The half-life of these
agents are short and are designed or formulated in such a way so that they prolong the period
of drug action (Mandorfer & Reiberger, 2017). They are rapidly distributed and cross the
BBB. Metabolism of lipophilic drug takes place in liver. Hydrophilic nature of beta-blockers
are also present, which include atenolol, sotalol, pindolo and nadolol. They are not entirely
absorbed through the gut and undergo almost negligible initial metabolism. The total half-life
of hydrophilic drugs are longer as compared to the lipophilic drugs.
Pharmacodynamics of beta-blockers:
Beta-blockers bind with and act on cardiac cells, blood vessels and bronchioles, which
in turn will block the receptors of ß1 and ß2. Calcium antagonist might interact with these
beta-blockers and develop serious problems like heart failure, cardiac abnormalities and
hypotension. Blockage of β1-adrenoceptors inhibits the impulse stimulation in the heart,
which in turn reduces the pressure, circulation and cardiac output in portal vein (Bryant &
knights, 2015). While the blockage of ß2-adrenoceptors leads to vasoconstriction in the vein
thus reducing blood circulation. Though beta-blockers might relieve ascites, portal
hypertension, variceal haemorrhage and hepatic encephalopathy, it will have a negative effect
on reducing the cardiac output and blood flow, which might affect the cardiac function
(Smolders et al., 2018). Cardiac function is already impaired by liver cirrhosis. Hence, this
adverse effect might arise in patients who are susceptible towards oral verapamil and
ophthalmic blocker.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Q4) In order of priority, develop a nursing care plan for your chosen patient who has just
arrived on the ward from ED. Nursing care plan goals, interventions and rationales must
relate to the first 8 hours post ward admission
The patient was diagnosed in the emergency department (ED) and in such situations,
the nursing care strategy initiates using Airway, Breathing, and Circulation (ABC) sequence
(Liou, 2014). The patient had a clear airway with normal respiratory rate and 95% of 6L
SpO2 received through Hudson Mask that is satisfactory in his stage or condition. The
nursing care plan for the patient would include the risk assessment for severe haemorrhage.
The aim of this care plan would be to reduce hypovolemic shock to further prevent any
complication of renal failure, hepatic decomposition and bacterial infection related to internal
bleeding (Mueller et al., 2014). As the patient was suffering from blood loss, the urgency of
his clinical presentation will decide the treatment approaches. The patient’s immune system
was weak as he was suffering from tachycardia, tachypnea and leukopenia; detail analysis
was required to monitor his health symptoms and thus creating a nursing care plan to
eliminate the symptoms of patient. The approved medication should be given to the patient,
which include antibiotics, beta-blockers and frusemide. Nursing care plan involves
monitoring of patient renal output and weight in order to prevent the side effects of
electrolytic imbalance and dehydration. In case the patient lack response to diuretic therapy,
he will be provided with an external catheter (Halcomb & Ashley, 2019).
The patient was spitting blood stained sputum since few weeks, which was due to
portal hypertension in case of patient suffering from liver cirrhosis. This can further result in
haemorrhagic shock, which is indicated from the pulse rate, haemoglobin count and systolic
blood pressure of the patient (Qi, Han & Fan, 2014). From the patient history, it was clear
that he was suffering from variceal haemorrhage as his haemoglobin, WBC, albumin and
platelets count was low below the required values. Nursing care plan includes the
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Q4) In order of priority, develop a nursing care plan for your chosen patient who has just
arrived on the ward from ED. Nursing care plan goals, interventions and rationales must
relate to the first 8 hours post ward admission
The patient was diagnosed in the emergency department (ED) and in such situations,
the nursing care strategy initiates using Airway, Breathing, and Circulation (ABC) sequence
(Liou, 2014). The patient had a clear airway with normal respiratory rate and 95% of 6L
SpO2 received through Hudson Mask that is satisfactory in his stage or condition. The
nursing care plan for the patient would include the risk assessment for severe haemorrhage.
The aim of this care plan would be to reduce hypovolemic shock to further prevent any
complication of renal failure, hepatic decomposition and bacterial infection related to internal
bleeding (Mueller et al., 2014). As the patient was suffering from blood loss, the urgency of
his clinical presentation will decide the treatment approaches. The patient’s immune system
was weak as he was suffering from tachycardia, tachypnea and leukopenia; detail analysis
was required to monitor his health symptoms and thus creating a nursing care plan to
eliminate the symptoms of patient. The approved medication should be given to the patient,
which include antibiotics, beta-blockers and frusemide. Nursing care plan involves
monitoring of patient renal output and weight in order to prevent the side effects of
electrolytic imbalance and dehydration. In case the patient lack response to diuretic therapy,
he will be provided with an external catheter (Halcomb & Ashley, 2019).
The patient was spitting blood stained sputum since few weeks, which was due to
portal hypertension in case of patient suffering from liver cirrhosis. This can further result in
haemorrhagic shock, which is indicated from the pulse rate, haemoglobin count and systolic
blood pressure of the patient (Qi, Han & Fan, 2014). From the patient history, it was clear
that he was suffering from variceal haemorrhage as his haemoglobin, WBC, albumin and
platelets count was low below the required values. Nursing care plan includes the
8
DETAIL ANALYSIS ON LIVER CIRRHOSIS
investigation techniques, which is conducted for the patient like magnetic resonance imaging,
ultrasonography and computerised tomography for detecting the occurrence focal
abnormalities in case of hepatocellular carcinoma and ascites (Huber et al., 2015). It will also
show the quantity of portal blood flow. In few circumstances of hematemesis, an external
endotracheal tube is required to assess the consciousness level of a patient and further
prevention of pulmonary aspiration and hypoxia. If the patient requires any surgical
approach, then the nurse should explain the entire procedure to the patient highlighting the
possible risk. Before the commencement of the surgical procedure, the patient must sign an
informed consent. The requirements should be ensured by the nurse before surgery, which
includes monitoring instructed fasting condition, proper medication and correct
documentation (Porter, 2018). The haemoglobin level, conscious level, renal output, and
monitoring of vital signs are few important criteria, which should be assessed before the
surgery.
The nurse should provide support to the patient by educating the patient, providing
correct information to the patient, supporting the patient, listening to the patient carefully, and
evaluating the patient’s health symptoms (Moses, 2018). In this case study, the patient
required a detail knowledge on his visible sign and symptoms, diagnosis, knowledge about
fluid retention and hypertension, knowledge on medication and the level of progression of the
disease.
DETAIL ANALYSIS ON LIVER CIRRHOSIS
investigation techniques, which is conducted for the patient like magnetic resonance imaging,
ultrasonography and computerised tomography for detecting the occurrence focal
abnormalities in case of hepatocellular carcinoma and ascites (Huber et al., 2015). It will also
show the quantity of portal blood flow. In few circumstances of hematemesis, an external
endotracheal tube is required to assess the consciousness level of a patient and further
prevention of pulmonary aspiration and hypoxia. If the patient requires any surgical
approach, then the nurse should explain the entire procedure to the patient highlighting the
possible risk. Before the commencement of the surgical procedure, the patient must sign an
informed consent. The requirements should be ensured by the nurse before surgery, which
includes monitoring instructed fasting condition, proper medication and correct
documentation (Porter, 2018). The haemoglobin level, conscious level, renal output, and
monitoring of vital signs are few important criteria, which should be assessed before the
surgery.
The nurse should provide support to the patient by educating the patient, providing
correct information to the patient, supporting the patient, listening to the patient carefully, and
evaluating the patient’s health symptoms (Moses, 2018). In this case study, the patient
required a detail knowledge on his visible sign and symptoms, diagnosis, knowledge about
fluid retention and hypertension, knowledge on medication and the level of progression of the
disease.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
DETAIL ANALYSIS ON LIVER CIRRHOSIS
References
Abs.gov.au. (2019). 3303.0 - Causes of Death, Australia, 2017. Retrieved from
http://www.abs.gov.au/ausstats/abs@.nsf/latestProducts/3303.0Media
%20Release62017
Betterhealth.vic.gov.au. (2019). Cirrhosis of the liver. Retrieved from
https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/cirrhosis-of-
the-liver
Bryant, B., & Knights, K. (2015). Pharmacology for health professionals (Fourth ed.).
Chatswood, Australia: Elsevier Australia.
Čižmáriková, R., Habala, L., Valentová, J., & Markuliak, M. (2019). Survey of
Pharmacological Activity and Pharmacokinetics of Selected β-Adrenergic Blockers in
Regard to Their Stereochemistry. Applied Sciences, 9(4), 625
Halcomb, E., & Ashley, C. (2019). Are Australian general practice nurses underutilised?: An
examination of current roles and task satisfaction. Collegian.
Healthdirect.gov.au. (2019). Cirrhosis of the liver. Retrieved from
https://www.healthdirect.gov.au/cirrhosis-of-the-liver
Huber, A., Ebner, L., Heverhagen, J. T., & Christe, A. (2015). State-of-the-art imaging of
liver fibrosis and cirrhosis: A comprehensive review of current applications and future
perspectives. European journal of radiology open, 2, 90-100.
Kanwal, F., Tapper, E. B., Ho, C., Asrani, S. K., Ovchinsky, N., Poterucha, J., ... & Volk, M.
(2018). Development of Quality Measures in Cirrhosis by the Practice Metrics
Committee of the American Association for the Study of Liver Diseases. Hepatology.
Liou, I. W. (2014). Management of end-stage liver disease. Medical Clinics, 98(1), 119-152.
DETAIL ANALYSIS ON LIVER CIRRHOSIS
References
Abs.gov.au. (2019). 3303.0 - Causes of Death, Australia, 2017. Retrieved from
http://www.abs.gov.au/ausstats/abs@.nsf/latestProducts/3303.0Media
%20Release62017
Betterhealth.vic.gov.au. (2019). Cirrhosis of the liver. Retrieved from
https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/cirrhosis-of-
the-liver
Bryant, B., & Knights, K. (2015). Pharmacology for health professionals (Fourth ed.).
Chatswood, Australia: Elsevier Australia.
Čižmáriková, R., Habala, L., Valentová, J., & Markuliak, M. (2019). Survey of
Pharmacological Activity and Pharmacokinetics of Selected β-Adrenergic Blockers in
Regard to Their Stereochemistry. Applied Sciences, 9(4), 625
Halcomb, E., & Ashley, C. (2019). Are Australian general practice nurses underutilised?: An
examination of current roles and task satisfaction. Collegian.
Healthdirect.gov.au. (2019). Cirrhosis of the liver. Retrieved from
https://www.healthdirect.gov.au/cirrhosis-of-the-liver
Huber, A., Ebner, L., Heverhagen, J. T., & Christe, A. (2015). State-of-the-art imaging of
liver fibrosis and cirrhosis: A comprehensive review of current applications and future
perspectives. European journal of radiology open, 2, 90-100.
Kanwal, F., Tapper, E. B., Ho, C., Asrani, S. K., Ovchinsky, N., Poterucha, J., ... & Volk, M.
(2018). Development of Quality Measures in Cirrhosis by the Practice Metrics
Committee of the American Association for the Study of Liver Diseases. Hepatology.
Liou, I. W. (2014). Management of end-stage liver disease. Medical Clinics, 98(1), 119-152.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Mandorfer, M., & Reiberger, T. (2017). Beta blockers and cirrhosis, 2016. Dig Liver Dis., 49,
3–10.
McCance, K., & Felver, L. (2018). Study guide for Pathophysiology : The biologic basis for
disease in adults and children, eighth edition (8th ed.). St Louis: Elsevier - Health
Sciences Division.
Mokdad, A. A., Lopez, A. D., Shahraz, S., Lozano, R., Mokdad, A. H., Stanaway, J., ... &
Naghavi, M. (2014). Liver cirrhosis mortality in 187 countries between 1980 and
2010: a systematic analysis. BMC medicine, 12(1), 145.
Moses, A. (2018). Health coaching: Empowering patients to improve health outcomes in
rural Australia. Australian Nursing and Midwifery Journal, 26(4), 42.
Moza, D., & Margenian, C. (2019). A62 LIVER CLEANSE, A SOLUTION OR
PROBLEM? A CASE REPORT. Journal of the Canadian Association of
Gastroenterology, 2(Supplement_2), 125-126.
Poordad, F. F. (2015). Presentation and complications associated with cirrhosis of the liver.
Current medical research and opinion, 31(5), 925-937.
Porter, K. L. (2018). Recognition of Clinical Deterioration: Does Nursing and Patient
Education Improve Outcomes? (Doctoral dissertation, Grand Canyon University).
Potosek, J., Curry, M., Buss, M., & Chittenden, E. (2014). Integration of palliative care in
end-stage liver disease and liver transplantation. Journal of palliative medicine,
17(11), 1271-1277.
Qi, X., Han, G., & Fan, D. (2014). Management of portal vein thrombosis in liver cirrhosis.
Nature reviews Gastroenterology & hepatology, 11(7), 435.
Smolders, E. J., ter Horst, P. J., Wolters, S., & Burger, D. M. (2018). Cardiovascular Risk
Management and Hepatitis C: Combining Drugs. Clinical pharmacokinetics, 1-28.
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Mandorfer, M., & Reiberger, T. (2017). Beta blockers and cirrhosis, 2016. Dig Liver Dis., 49,
3–10.
McCance, K., & Felver, L. (2018). Study guide for Pathophysiology : The biologic basis for
disease in adults and children, eighth edition (8th ed.). St Louis: Elsevier - Health
Sciences Division.
Mokdad, A. A., Lopez, A. D., Shahraz, S., Lozano, R., Mokdad, A. H., Stanaway, J., ... &
Naghavi, M. (2014). Liver cirrhosis mortality in 187 countries between 1980 and
2010: a systematic analysis. BMC medicine, 12(1), 145.
Moses, A. (2018). Health coaching: Empowering patients to improve health outcomes in
rural Australia. Australian Nursing and Midwifery Journal, 26(4), 42.
Moza, D., & Margenian, C. (2019). A62 LIVER CLEANSE, A SOLUTION OR
PROBLEM? A CASE REPORT. Journal of the Canadian Association of
Gastroenterology, 2(Supplement_2), 125-126.
Poordad, F. F. (2015). Presentation and complications associated with cirrhosis of the liver.
Current medical research and opinion, 31(5), 925-937.
Porter, K. L. (2018). Recognition of Clinical Deterioration: Does Nursing and Patient
Education Improve Outcomes? (Doctoral dissertation, Grand Canyon University).
Potosek, J., Curry, M., Buss, M., & Chittenden, E. (2014). Integration of palliative care in
end-stage liver disease and liver transplantation. Journal of palliative medicine,
17(11), 1271-1277.
Qi, X., Han, G., & Fan, D. (2014). Management of portal vein thrombosis in liver cirrhosis.
Nature reviews Gastroenterology & hepatology, 11(7), 435.
Smolders, E. J., ter Horst, P. J., Wolters, S., & Burger, D. M. (2018). Cardiovascular Risk
Management and Hepatitis C: Combining Drugs. Clinical pharmacokinetics, 1-28.

11
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Tsochatzis, E. A., Bosch, J., & Burroughs, A. K. (2014). Liver cirrhosis. The Lancet,
383(9930), 1749-1761.
Zhou, W. C., Zhang, Q. B., & Qiao, L. (2014). Pathogenesis of liver cirrhosis. World journal
of gastroenterology: WJG, 20(23), 7312.
DETAIL ANALYSIS ON LIVER CIRRHOSIS
Tsochatzis, E. A., Bosch, J., & Burroughs, A. K. (2014). Liver cirrhosis. The Lancet,
383(9930), 1749-1761.
Zhou, W. C., Zhang, Q. B., & Qiao, L. (2014). Pathogenesis of liver cirrhosis. World journal
of gastroenterology: WJG, 20(23), 7312.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





