University Mental Health Nursing Case Study Report: Mary
VerifiedAdded on 2023/06/09
|11
|2571
|203
Report
AI Summary
This report presents a comprehensive analysis of a mental health nursing case study focusing on a patient named Mary, diagnosed with depression. Part 1 of the report begins with a detailed mental status examination (MSE), assessing Mary's appearance, behavior, attitude, level of consciousness, speech, mood, affect, thought processes, thought content, suicidality, insight, judgment, attention span, memory, and intellectual functioning. A clinical formulation is then provided, summarizing biological, psychological, and social factors contributing to Mary's condition, followed by a prioritized nursing care plan addressing disturbed thought processes and impaired social interaction. The nursing interventions include determining the patient's cognitive function, providing ample time for responses, reducing responsibilities, identifying negative thoughts, and structuring family life. Interventions for impaired social interaction involve activities with minimal concentration, one-to-one activities, and group activities. Part 2 focuses on the therapeutic relationship, emphasizing its components and importance in predicting treatment response. The report also discusses cultural safety in providing care, highlighting the need for cultural competency and sensitivity to Mary's religious beliefs. Finally, the report explores recovery-oriented nursing care, aligning the interventions with the principles of self-direction, respect, person-centered care, empowerment, holistic approach, strength-based, hope, peer support, and non-linear recovery.

Running head: MENTAL HEALTH- NURSING
MENTAL HEALTH- NURSING
Name of the Student:
Name of the University:
Author Note:
MENTAL HEALTH- NURSING
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1MENTAL HEALTH- NURSING
Part 1
The Mental Status Examination
1. Appearance
The patient, Mary appears very clean and tidy. She is seen to wear fashionablet-shirts paired
with jeans. She hasshort and dark hair. However Mary does not wear any makeup. However
often she is also seen sitting wearing her dressing gown.
2. Behaviour
The behaviour of the patient apparently seems normal. However sometimes she has moments
of despair and is tearful on some occasions.
3. Attitude
The patient often feels worthless and hopeless and she thinks that she will not be able to
manage herself and carry on to the next day.
4. Level of Consciousness
The consciousness of the level of the patient is normal.
5. Orientation
6. Speech and Language
Her speech and language does not have any problem however she refuses to talk to others at
times.
7. Mood
Part 1
The Mental Status Examination
1. Appearance
The patient, Mary appears very clean and tidy. She is seen to wear fashionablet-shirts paired
with jeans. She hasshort and dark hair. However Mary does not wear any makeup. However
often she is also seen sitting wearing her dressing gown.
2. Behaviour
The behaviour of the patient apparently seems normal. However sometimes she has moments
of despair and is tearful on some occasions.
3. Attitude
The patient often feels worthless and hopeless and she thinks that she will not be able to
manage herself and carry on to the next day.
4. Level of Consciousness
The consciousness of the level of the patient is normal.
5. Orientation
6. Speech and Language
Her speech and language does not have any problem however she refuses to talk to others at
times.
7. Mood
2MENTAL HEALTH- NURSING
She suffers from mood swings. At times she is apparently normal, and at times she appears
depressed and tearful. She lacks sleep and suffers from insomnia.
8. Affect
As a result of her mood, Mary often lacks the motivation to carry out simple activities like
eating or dressing.
9. Thought Process/Form
She feels worthless and hopeless. She also suffers from thoughts like she will not be able to
survive anymore and will not be able to make it to the next day.
10. Thought Content
Her thought content of the patient is that she will not be able to manage herself anmore and
will not be able to survive.
11. Suicidality and Homicidality
Mary does not have any suicidal thoughts.
12. Insight and Judgment
Mary likes to spend time in the church and admits that she gets pleasure from her visits to the
church.
13. Attention Span
The attention span of the patient is also reduced as she lacks concentration while doing
simple activities even like eating and dressing.
14. Memory
The memory of the patient is normal as she remembers things from her past.
She suffers from mood swings. At times she is apparently normal, and at times she appears
depressed and tearful. She lacks sleep and suffers from insomnia.
8. Affect
As a result of her mood, Mary often lacks the motivation to carry out simple activities like
eating or dressing.
9. Thought Process/Form
She feels worthless and hopeless. She also suffers from thoughts like she will not be able to
survive anymore and will not be able to make it to the next day.
10. Thought Content
Her thought content of the patient is that she will not be able to manage herself anmore and
will not be able to survive.
11. Suicidality and Homicidality
Mary does not have any suicidal thoughts.
12. Insight and Judgment
Mary likes to spend time in the church and admits that she gets pleasure from her visits to the
church.
13. Attention Span
The attention span of the patient is also reduced as she lacks concentration while doing
simple activities even like eating and dressing.
14. Memory
The memory of the patient is normal as she remembers things from her past.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3MENTAL HEALTH- NURSING
15. Intellectual Functioning
The intellectual functioning of the patient is apparently optimal. She understands that if she is
admitted to the hospital again, she would be trouble her family members. She is now adamant
that she needs to stay at home to take care of her children and her husband.
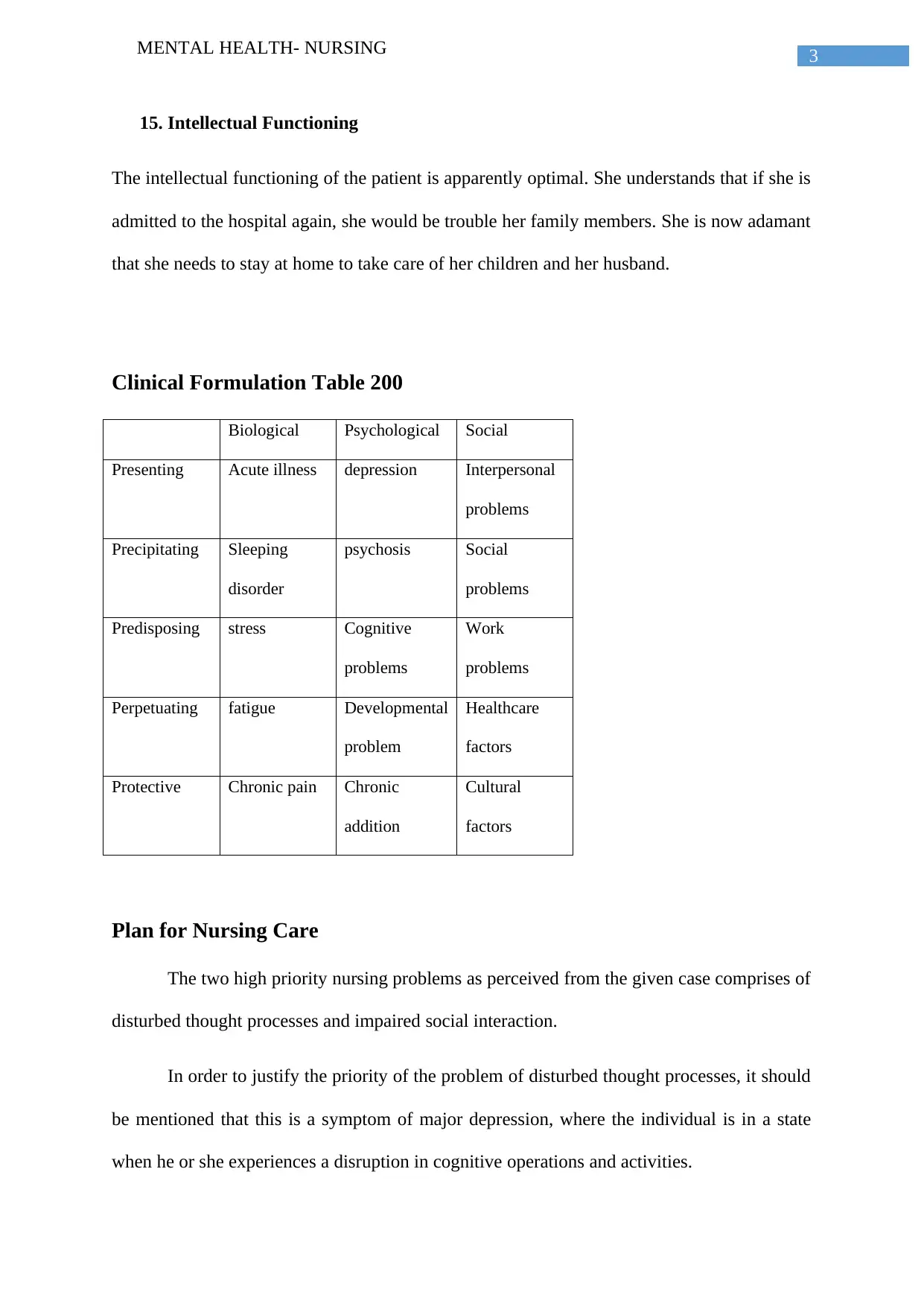
Clinical Formulation Table 200
Biological Psychological Social
Presenting Acute illness depression Interpersonal
problems
Precipitating Sleeping
disorder
psychosis Social
problems
Predisposing stress Cognitive
problems
Work
problems
Perpetuating fatigue Developmental
problem
Healthcare
factors
Protective Chronic pain Chronic
addition
Cultural
factors
Plan for Nursing Care
The two high priority nursing problems as perceived from the given case comprises of
disturbed thought processes and impaired social interaction.
In order to justify the priority of the problem of disturbed thought processes, it should
be mentioned that this is a symptom of major depression, where the individual is in a state
when he or she experiences a disruption in cognitive operations and activities.
15. Intellectual Functioning
The intellectual functioning of the patient is apparently optimal. She understands that if she is
admitted to the hospital again, she would be trouble her family members. She is now adamant
that she needs to stay at home to take care of her children and her husband.
Clinical Formulation Table 200
Biological Psychological Social
Presenting Acute illness depression Interpersonal
problems
Precipitating Sleeping
disorder
psychosis Social
problems
Predisposing stress Cognitive
problems
Work
problems
Perpetuating fatigue Developmental
problem
Healthcare
factors
Protective Chronic pain Chronic
addition
Cultural
factors
Plan for Nursing Care
The two high priority nursing problems as perceived from the given case comprises of
disturbed thought processes and impaired social interaction.
In order to justify the priority of the problem of disturbed thought processes, it should
be mentioned that this is a symptom of major depression, where the individual is in a state
when he or she experiences a disruption in cognitive operations and activities.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4MENTAL HEALTH- NURSING
Similarly in case of impaired social interaction, this is another symptom of major depression
where the patient suffers from inadequate ability if perform quality social exchange.
The nursing interventions that are needed to be carried out in order to address the
problem of disturbed thought processes involves determination of the patient’s level of
cognition function that was present earlier. This can be done by collection of information
from the patient, the family of the patient or the past medical records. This allows to establish
a baseline data which helps the evaluation of the progress of the client. The interventions
should allow the patient ample time to think about the made responses and to frame them
appropriately (Van Bogaert, Kowalski, Weeks & Clarke, 2013). Hurry in such cases might
increase anxiety in the patient. Through the interventions, the patient should be helped out to
postpose the making of major life decisions. This should be done since making of major life
decisions requires normal psychophysiological functioning. The interventions must ensure
that the patient’s responsibilities are reduced. This helps to decrease the feelings of guilt,
anxiety as well as pressure. The client must also be helped out to identify and address the
persisting negative thoughts. This needs to be ensured so that the patient does not feel
hopeless due to the negative thoughts. Such intervening might help to make the patient
happier and healthier. The interventions should also ensure that the client is able to set
structure in the family life in order to set schedules and predictable routines during severe
depressions (Zarea, Nikbakht‐Nasrabadi, Abbaszadeh & Mohammadpour, 2013).
In terms of interventions for the impaired social interventions, it should be ensured
that activities are provided which require minimal concentration. This should be followed as
most of the time the patients of depression lack memory and concentration. In cases, where
the patient is in most depressed state, the interventions need to ensure that the patient is
involved in one to one activity. These activities might help in relieving tension as well as
elevating the mood. Interventions might also involve group activities that helps in socializing
Similarly in case of impaired social interaction, this is another symptom of major depression
where the patient suffers from inadequate ability if perform quality social exchange.
The nursing interventions that are needed to be carried out in order to address the
problem of disturbed thought processes involves determination of the patient’s level of
cognition function that was present earlier. This can be done by collection of information
from the patient, the family of the patient or the past medical records. This allows to establish
a baseline data which helps the evaluation of the progress of the client. The interventions
should allow the patient ample time to think about the made responses and to frame them
appropriately (Van Bogaert, Kowalski, Weeks & Clarke, 2013). Hurry in such cases might
increase anxiety in the patient. Through the interventions, the patient should be helped out to
postpose the making of major life decisions. This should be done since making of major life
decisions requires normal psychophysiological functioning. The interventions must ensure
that the patient’s responsibilities are reduced. This helps to decrease the feelings of guilt,
anxiety as well as pressure. The client must also be helped out to identify and address the
persisting negative thoughts. This needs to be ensured so that the patient does not feel
hopeless due to the negative thoughts. Such intervening might help to make the patient
happier and healthier. The interventions should also ensure that the client is able to set
structure in the family life in order to set schedules and predictable routines during severe
depressions (Zarea, Nikbakht‐Nasrabadi, Abbaszadeh & Mohammadpour, 2013).
In terms of interventions for the impaired social interventions, it should be ensured
that activities are provided which require minimal concentration. This should be followed as
most of the time the patients of depression lack memory and concentration. In cases, where
the patient is in most depressed state, the interventions need to ensure that the patient is
involved in one to one activity. These activities might help in relieving tension as well as
elevating the mood. Interventions might also involve group activities that helps in socializing
5MENTAL HEALTH- NURSING
as it helps to reduce the feelings of isolation. In some cases the patient might also be referred
to self-help groups in the community in order to help the client gain support from the
experiences (Roldán‐Merino et al., 2013).
Clinical handover
The clinical handover follows the ISBAR method that comprises of:
Identification: The patient is Mary, who is 41 years old. She lives with her husband and three
children.
Situation: Mary has been diagnosed with major depression.
Observations: The patient suffers from despair and fatigue. She suffers from sleeping
disorder.
Background: Mary often talks of feeling worthless and hopeless and has made comments in
the past that she can’t see how she will manage to get through another day.
Agreed plan: Evidence based interventions needs to be carried in respect of the nursing
problems of disturbed thought processes and impaired social interaction.
Read back: The mental health care nurses need to be responsible for the patient and must
establish a therapeutic relationship with the patient.
as it helps to reduce the feelings of isolation. In some cases the patient might also be referred
to self-help groups in the community in order to help the client gain support from the
experiences (Roldán‐Merino et al., 2013).
Clinical handover
The clinical handover follows the ISBAR method that comprises of:
Identification: The patient is Mary, who is 41 years old. She lives with her husband and three
children.
Situation: Mary has been diagnosed with major depression.
Observations: The patient suffers from despair and fatigue. She suffers from sleeping
disorder.
Background: Mary often talks of feeling worthless and hopeless and has made comments in
the past that she can’t see how she will manage to get through another day.
Agreed plan: Evidence based interventions needs to be carried in respect of the nursing
problems of disturbed thought processes and impaired social interaction.
Read back: The mental health care nurses need to be responsible for the patient and must
establish a therapeutic relationship with the patient.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6MENTAL HEALTH- NURSING
Part 2
The Therapeutic Relationship
Establishment of therapeutic relationship is a phenomenon that is multifaceted in
nature, which mainly focuses on the alliance between the therapist and the patient.
Therapeutic relationship should comprise of the following components that is development of
therapeutic goals along with consensus on the necessary therapeutic tasks. It also includes the
establishment of a positive affective bond between the patient and therapist. A study by
Rüsch et al., (2014), showed that a quality therapeutic relationship played a significant role in
determining the therapeutic outcome of the patient suffering from depression. Development
of such a high quality therapeutic relationship between Mary and her care giver, early in the
treatment process will help in better predicting the treatment response. The care giver might
be able to assess the symptoms which will show a reduction along with improved congenital
functioning during the treatment period. The care giver should continue to maintain the
relationship even during the follow-up period as the patient is suffering from major
depression.
In relation to the interventions mentioned in the part discussing about the nursing care
for the patients, the therapeutic interventions might include individual therapy that involves
supportive and psychodynamic therapy. Group therapy is also involved which addresses the
gender and the specific problems. It also identifies size, frequency and the safety issues.
Behavioural therapy is also part of the therapeutic intervention that might be carried out by
the patient (Wiger & Mooney, 2014). The patient can also be made to follow art therapy
which will help Mary to express her context using different media.
Part 2
The Therapeutic Relationship
Establishment of therapeutic relationship is a phenomenon that is multifaceted in
nature, which mainly focuses on the alliance between the therapist and the patient.
Therapeutic relationship should comprise of the following components that is development of
therapeutic goals along with consensus on the necessary therapeutic tasks. It also includes the
establishment of a positive affective bond between the patient and therapist. A study by
Rüsch et al., (2014), showed that a quality therapeutic relationship played a significant role in
determining the therapeutic outcome of the patient suffering from depression. Development
of such a high quality therapeutic relationship between Mary and her care giver, early in the
treatment process will help in better predicting the treatment response. The care giver might
be able to assess the symptoms which will show a reduction along with improved congenital
functioning during the treatment period. The care giver should continue to maintain the
relationship even during the follow-up period as the patient is suffering from major
depression.
In relation to the interventions mentioned in the part discussing about the nursing care
for the patients, the therapeutic interventions might include individual therapy that involves
supportive and psychodynamic therapy. Group therapy is also involved which addresses the
gender and the specific problems. It also identifies size, frequency and the safety issues.
Behavioural therapy is also part of the therapeutic intervention that might be carried out by
the patient (Wiger & Mooney, 2014). The patient can also be made to follow art therapy
which will help Mary to express her context using different media.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7MENTAL HEALTH- NURSING
Cultural Safety
In order to maintain cultural safety while providing care to the patients of depression,
cultural competency is required to be maintained by the health professionals and care givers.
The health care providers must be able to provide their service irrespective of the differences
and comply with adeptness such as language, ethnicity, race, or culture. While working with
Mary it should be ensured that health care provider is able to establish a sense of safety and
security along with self awareness while providing care (Kang et al., 2016).
Working with the patient Mary it was perceived that she was a true Christian and she
liked attending services at the church where she found solace. Therefore while working with
her the care giver must keep this in mind and through maintenance of culturally competent
mental health care, services should be provided. In order to do so, the caregiver needs to be
well aware of the community structure and the community practices to which Mary belongs
since the interventions involve making her involve in group activity intervention that involves
the community. The delivery of the nursing care should also ensure that it is based on the
cultural values of the patient along with her believes and behaviour. This will also affect the
interventions like the supportive and the psychodynamic therapy in order to reduce social
isolation of the patient (Chinman et al., 2014).
Recovery-oriented Nursing Care
The health recovery model takes a view of the person’s life through a holistic
approach. The mental health recovery model compromises of the following:
Self-directed
Individualized and person-centered
Empowerment
Holistic
Nonlinear
Strengths-based
Peer support
Cultural Safety
In order to maintain cultural safety while providing care to the patients of depression,
cultural competency is required to be maintained by the health professionals and care givers.
The health care providers must be able to provide their service irrespective of the differences
and comply with adeptness such as language, ethnicity, race, or culture. While working with
Mary it should be ensured that health care provider is able to establish a sense of safety and
security along with self awareness while providing care (Kang et al., 2016).
Working with the patient Mary it was perceived that she was a true Christian and she
liked attending services at the church where she found solace. Therefore while working with
her the care giver must keep this in mind and through maintenance of culturally competent
mental health care, services should be provided. In order to do so, the caregiver needs to be
well aware of the community structure and the community practices to which Mary belongs
since the interventions involve making her involve in group activity intervention that involves
the community. The delivery of the nursing care should also ensure that it is based on the
cultural values of the patient along with her believes and behaviour. This will also affect the
interventions like the supportive and the psychodynamic therapy in order to reduce social
isolation of the patient (Chinman et al., 2014).
Recovery-oriented Nursing Care
The health recovery model takes a view of the person’s life through a holistic
approach. The mental health recovery model compromises of the following:
Self-directed
Individualized and person-centered
Empowerment
Holistic
Nonlinear
Strengths-based
Peer support
8MENTAL HEALTH- NURSING
Respect
Responsibility
Hope
The interventions mentioned in the first part of the paper deals with mainly two
nursing problems of disturbed thought processes and impaired social interaction. The
suggested interventions that might be implemented to address these problems involve the
components of the health recovery model in the following way: the interventions are self
directed as data is collected directly from the patient. The interventions ensure that patient is
given ample time to think about their responses which involves the component of respect. It
also ensures person centred care. The patients should be helped out to make major life
decisions which helps to empower the patient. The interventions help to reduce the anxiety
and the guilt of the patient. This involves a holistic approach of recovery. The client must
also be helped out to identify and address the persisting negative thoughts. This shows that
the element of strength is applied. The interventions also help to make the patient happier and
healthier by reducing negative thoughts. This involves the element of hope in the recovery
process. Interventions in terms of reducing social impairment involve the one to one activities
that again help to empower the patient and provide responsibility and respect through which
recovery can occur. Interventions might also involve group activities that help in socializing
as it helps to reduce the feelings of isolation. This involves the element of peer support this
helping inn recovery. In some cases the patient might also be referred to self-help groups in
the community in order to help the client gain support from the experiences. This involves the
non- linear and strength based elements promoting the recovery (Lloyd-Evans et al., 2014).
Respect
Responsibility
Hope
The interventions mentioned in the first part of the paper deals with mainly two
nursing problems of disturbed thought processes and impaired social interaction. The
suggested interventions that might be implemented to address these problems involve the
components of the health recovery model in the following way: the interventions are self
directed as data is collected directly from the patient. The interventions ensure that patient is
given ample time to think about their responses which involves the component of respect. It
also ensures person centred care. The patients should be helped out to make major life
decisions which helps to empower the patient. The interventions help to reduce the anxiety
and the guilt of the patient. This involves a holistic approach of recovery. The client must
also be helped out to identify and address the persisting negative thoughts. This shows that
the element of strength is applied. The interventions also help to make the patient happier and
healthier by reducing negative thoughts. This involves the element of hope in the recovery
process. Interventions in terms of reducing social impairment involve the one to one activities
that again help to empower the patient and provide responsibility and respect through which
recovery can occur. Interventions might also involve group activities that help in socializing
as it helps to reduce the feelings of isolation. This involves the element of peer support this
helping inn recovery. In some cases the patient might also be referred to self-help groups in
the community in order to help the client gain support from the experiences. This involves the
non- linear and strength based elements promoting the recovery (Lloyd-Evans et al., 2014).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9MENTAL HEALTH- NURSING
References
Chinman, M., George, P., Dougherty, R. H., Daniels, A. S., Ghose, S. S., Swift, A., &
Delphin-Rittmon, M. E. (2014). Peer support services for individuals with serious
mental illnesses: assessing the evidence. Psychiatric Services, 65(4), 429-441.
https://doi.org/10.1176/appi.ps.201300244
Kang, E. K., Jeong, H. S., Moon, E. R., Lee, J. Y., & Lee, K. J. (2016). Cognitive and
language function in aphasic patients assessed with the Korean version of mini-mental
status examination. Annals of rehabilitation medicine, 40(1), 152-161. Retrieved
from: https://synapse.koreamed.org/
Lloyd-Evans, B., Mayo-Wilson, E., Harrison, B., Istead, H., Brown, E., Pilling, S., ... &
Kendall, T. (2014). A systematic review and meta-analysis of randomised controlled
trials of peer support for people with severe mental illness. BMC psychiatry, 14(1),
39. https://doi.org/10.1186/1471-244X-14-39
Roldán‐Merino, J., García, I. C., Ramos‐Pichardo, J. D., Foix‐Sanjuan, A., Quilez‐Jover, J.,
& Montserrat‐Martinez, M. (2013). Impact of personalized in‐home nursing care
plans on dependence in ADLs/IADLs and on family burden among adults diagnosed
with schizophrenia: a randomized controlled study. Perspectives in psychiatric
care, 49(3), 171-178. https://doi.org/10.1111/j.1744-6163.2012.00347.x
Rotella, F., & Mannucci, E. (2013). Depression as a risk factor for diabetes: a meta-analysis
of longitudinal studies. The Journal of clinical psychiatry. Retrieved from:
http://psycnet.apa.org/record/2013-13698-004
Rüsch, N., Müller, M., Lay, B., Corrigan, P. W., Zahn, R., Schönenberger, T., ... & Rössler,
W. (2014). Emotional reactions to involuntary psychiatric hospitalization and stigma-
related stress among people with mental illness. European Archives of Psychiatry and
References
Chinman, M., George, P., Dougherty, R. H., Daniels, A. S., Ghose, S. S., Swift, A., &
Delphin-Rittmon, M. E. (2014). Peer support services for individuals with serious
mental illnesses: assessing the evidence. Psychiatric Services, 65(4), 429-441.
https://doi.org/10.1176/appi.ps.201300244
Kang, E. K., Jeong, H. S., Moon, E. R., Lee, J. Y., & Lee, K. J. (2016). Cognitive and
language function in aphasic patients assessed with the Korean version of mini-mental
status examination. Annals of rehabilitation medicine, 40(1), 152-161. Retrieved
from: https://synapse.koreamed.org/
Lloyd-Evans, B., Mayo-Wilson, E., Harrison, B., Istead, H., Brown, E., Pilling, S., ... &
Kendall, T. (2014). A systematic review and meta-analysis of randomised controlled
trials of peer support for people with severe mental illness. BMC psychiatry, 14(1),
39. https://doi.org/10.1186/1471-244X-14-39
Roldán‐Merino, J., García, I. C., Ramos‐Pichardo, J. D., Foix‐Sanjuan, A., Quilez‐Jover, J.,
& Montserrat‐Martinez, M. (2013). Impact of personalized in‐home nursing care
plans on dependence in ADLs/IADLs and on family burden among adults diagnosed
with schizophrenia: a randomized controlled study. Perspectives in psychiatric
care, 49(3), 171-178. https://doi.org/10.1111/j.1744-6163.2012.00347.x
Rotella, F., & Mannucci, E. (2013). Depression as a risk factor for diabetes: a meta-analysis
of longitudinal studies. The Journal of clinical psychiatry. Retrieved from:
http://psycnet.apa.org/record/2013-13698-004
Rüsch, N., Müller, M., Lay, B., Corrigan, P. W., Zahn, R., Schönenberger, T., ... & Rössler,
W. (2014). Emotional reactions to involuntary psychiatric hospitalization and stigma-
related stress among people with mental illness. European Archives of Psychiatry and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10MENTAL HEALTH- NURSING
Clinical Neuroscience, 264(1), 35-43. Retrieved from:
https://link.springer.com/article/10.1007/s00406-013-0412-5
Van Bogaert, P., Kowalski, C., Weeks, S. M., & Clarke, S. P. (2013). The relationship
between nurse practice environment, nurse work characteristics, burnout and job
outcome and quality of nursing care: a cross-sectional survey. International journal of
nursing studies, 50(12), 1667-1677. https://doi.org/10.1016/j.ijnurstu.2013.05.010
Wiger, D. E., & Mooney, N. B. (2014). Mental Status Exam. The Encyclopedia of Clinical
Psychology, 1-5. https://doi.org/10.1002/9781118625392.wbecp104
Zarea, K., NIKBAKHT‐NASRABADI, A., Abbaszadeh, A., & Mohammadpour, A. (2013).
Psychiatric nursing as ‘different’care: experience of Iranian mental health nurses in
inpatient psychiatric wards. Journal of psychiatric and mental health nursing, 20(2),
124-133. https://doi.org/10.1111/j.1365-2850.2012.01891.x
Clinical Neuroscience, 264(1), 35-43. Retrieved from:
https://link.springer.com/article/10.1007/s00406-013-0412-5
Van Bogaert, P., Kowalski, C., Weeks, S. M., & Clarke, S. P. (2013). The relationship
between nurse practice environment, nurse work characteristics, burnout and job
outcome and quality of nursing care: a cross-sectional survey. International journal of
nursing studies, 50(12), 1667-1677. https://doi.org/10.1016/j.ijnurstu.2013.05.010
Wiger, D. E., & Mooney, N. B. (2014). Mental Status Exam. The Encyclopedia of Clinical
Psychology, 1-5. https://doi.org/10.1002/9781118625392.wbecp104
Zarea, K., NIKBAKHT‐NASRABADI, A., Abbaszadeh, A., & Mohammadpour, A. (2013).
Psychiatric nursing as ‘different’care: experience of Iranian mental health nurses in
inpatient psychiatric wards. Journal of psychiatric and mental health nursing, 20(2),
124-133. https://doi.org/10.1111/j.1365-2850.2012.01891.x
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





