NUR250 S1 2018: Comprehensive Patient Assessment & Care Plan Report
VerifiedAdded on 2023/06/14
|12
|4158
|81
Report
AI Summary
This report presents a comprehensive patient assessment and care plan developed for NUR250 Medical Surgical Nursing 1. It includes a primary and focused patient assessment using the ABCD technique, arterial blood gas assessment, and palpation. The care plan addresses nursing problems such as the risk of infection spread, self-care deficit, imbalanced fluid volume, hyperthermia, and hypertension, providing detailed nursing interventions, rationales, and indicators for plan effectiveness. The report also discusses medication management, focusing on oseltamivir and paracetamol, explaining their mechanisms of action and therapeutic effects. This document provides valuable insights into nursing care strategies and assessment techniques in a medical-surgical setting.
NUR250 Assessment 1 S1 2018
Assignment template
It is recommended you do not delete the heading and the information below.
Please note: As indicated in Assessment 1 information, a cover sheet, title and contents
pages are not required
Before you begin take a minute to fill in your details in the footer to ensure your document is
identifiable. To access the footer, double click on the grey writing “Last name….” at the bottom of the
page above. Once you have done that, double click here to come back to this page.
Information about the required line spacing and font size and type is in the Assessment 1 information
document in the Assessment 1 folder on NUR250 Learnline. Take a minute to check that this document
meets those requirements.
To avoid or minimise problems with formatting, it is recommended you
• Use the headings provided
• Don’t copy from another document onto this template
• Don’t delete the section breaks on the document
Submission of your assignment means you have read and understood the
• University policies and procedures related to academic integrity
• Assessment 1 presentation guidelines
Start to write your assignment here. Word count is calculated from this point.
Task 1: Patient assessment
First and foremost, the registered nurse will have to begin with primary assessment of the
patient with the ABCD technique. It is the most common assessment technique and this helps in
determination of the dangers that the patient in under as well. The tool begins with airway
assessment. For patients with any respiratory disorders, the airway assessment will explore the
details of the gas exchange and respiratory rate of the patient. The nurse will assess the secretion,
respiratory noises, coughing and airway condition of the patient. The breathing assessment will
assess the bilateral air movement, breathing sounds and respiratory rate and rhythm will be
Assignment template
It is recommended you do not delete the heading and the information below.
Please note: As indicated in Assessment 1 information, a cover sheet, title and contents
pages are not required
Before you begin take a minute to fill in your details in the footer to ensure your document is
identifiable. To access the footer, double click on the grey writing “Last name….” at the bottom of the
page above. Once you have done that, double click here to come back to this page.
Information about the required line spacing and font size and type is in the Assessment 1 information
document in the Assessment 1 folder on NUR250 Learnline. Take a minute to check that this document
meets those requirements.
To avoid or minimise problems with formatting, it is recommended you
• Use the headings provided
• Don’t copy from another document onto this template
• Don’t delete the section breaks on the document
Submission of your assignment means you have read and understood the
• University policies and procedures related to academic integrity
• Assessment 1 presentation guidelines
Start to write your assignment here. Word count is calculated from this point.
Task 1: Patient assessment
First and foremost, the registered nurse will have to begin with primary assessment of the
patient with the ABCD technique. It is the most common assessment technique and this helps in
determination of the dangers that the patient in under as well. The tool begins with airway
assessment. For patients with any respiratory disorders, the airway assessment will explore the
details of the gas exchange and respiratory rate of the patient. The nurse will assess the secretion,
respiratory noises, coughing and airway condition of the patient. The breathing assessment will
assess the bilateral air movement, breathing sounds and respiratory rate and rhythm will be
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
assessed, the circulation assessment will check pulse, temperature, skin colour, and capillary
refill time. Disability assessment will check activity tolerance and consciousness of the patient
using tools like Alert Voice Pain Unconscious score or Gross Motor Function Classification
System (Olgers, Dijkstra, Drost-de Klerck & Ter Maaten, 2014).
In the second step the patient will require focused or targeted assessment like the arterial
blood gases assessment. Arterial blood gas test assesses the functional capability of the lungs of
the patient and the level of gaseous exchange in the patient’s body. This assessment mainly
checks the PaO2 levels or the ability of the lungs to move oxygen into blood, PaCO2 levels or the
ability of the lungs to remove CO2 from the blood, lactate accumulation levels, and the acid/base
status of the arterial blood. As Jim, the patient in case study, had been suffering from influenza
infection; this assessment will reveal critical information regarding the lung capacity and burden
(Dugas et al., 2012).
The third assessment that will be given to the patient will be another focussed
assessment, and it will be focussed checking the palpation of the patient. This assessment will
include the bilateral symmetry of chest expansion, skin condition of the patient, capillary refill,
fremitus or tactile assessment, and checking for Subcutaneous emphysema. For any respiratory
disorder or any infection that causes respiratory distress, there is a significant impact on the lung
capacity. Along with that, the excessive mucous production and fluid volume back up, when
combined, can have a significant impact on the chest cavity of the patient. This assessment will
assess the load of the lungs and respiratory muscles or any chances for excess fluid volume that
can lead to bilateral asymmetry of the chest wall and will also provide critical information
regarding the infection spread (Ortiz, Rudd, Clark, Jacob & West, 2013).
Task 2: Care planning
Nursing Care Plan: Jim
Note: Dot points recommended in care plan. Click and type in each cell, click enter in a cell to make it
longer. Do not remove text from the template.
refill time. Disability assessment will check activity tolerance and consciousness of the patient
using tools like Alert Voice Pain Unconscious score or Gross Motor Function Classification
System (Olgers, Dijkstra, Drost-de Klerck & Ter Maaten, 2014).
In the second step the patient will require focused or targeted assessment like the arterial
blood gases assessment. Arterial blood gas test assesses the functional capability of the lungs of
the patient and the level of gaseous exchange in the patient’s body. This assessment mainly
checks the PaO2 levels or the ability of the lungs to move oxygen into blood, PaCO2 levels or the
ability of the lungs to remove CO2 from the blood, lactate accumulation levels, and the acid/base
status of the arterial blood. As Jim, the patient in case study, had been suffering from influenza
infection; this assessment will reveal critical information regarding the lung capacity and burden
(Dugas et al., 2012).
The third assessment that will be given to the patient will be another focussed
assessment, and it will be focussed checking the palpation of the patient. This assessment will
include the bilateral symmetry of chest expansion, skin condition of the patient, capillary refill,
fremitus or tactile assessment, and checking for Subcutaneous emphysema. For any respiratory
disorder or any infection that causes respiratory distress, there is a significant impact on the lung
capacity. Along with that, the excessive mucous production and fluid volume back up, when
combined, can have a significant impact on the chest cavity of the patient. This assessment will
assess the load of the lungs and respiratory muscles or any chances for excess fluid volume that
can lead to bilateral asymmetry of the chest wall and will also provide critical information
regarding the infection spread (Ortiz, Rudd, Clark, Jacob & West, 2013).
Task 2: Care planning
Nursing Care Plan: Jim
Note: Dot points recommended in care plan. Click and type in each cell, click enter in a cell to make it
longer. Do not remove text from the template.
A reminder that all rationales must be referenced
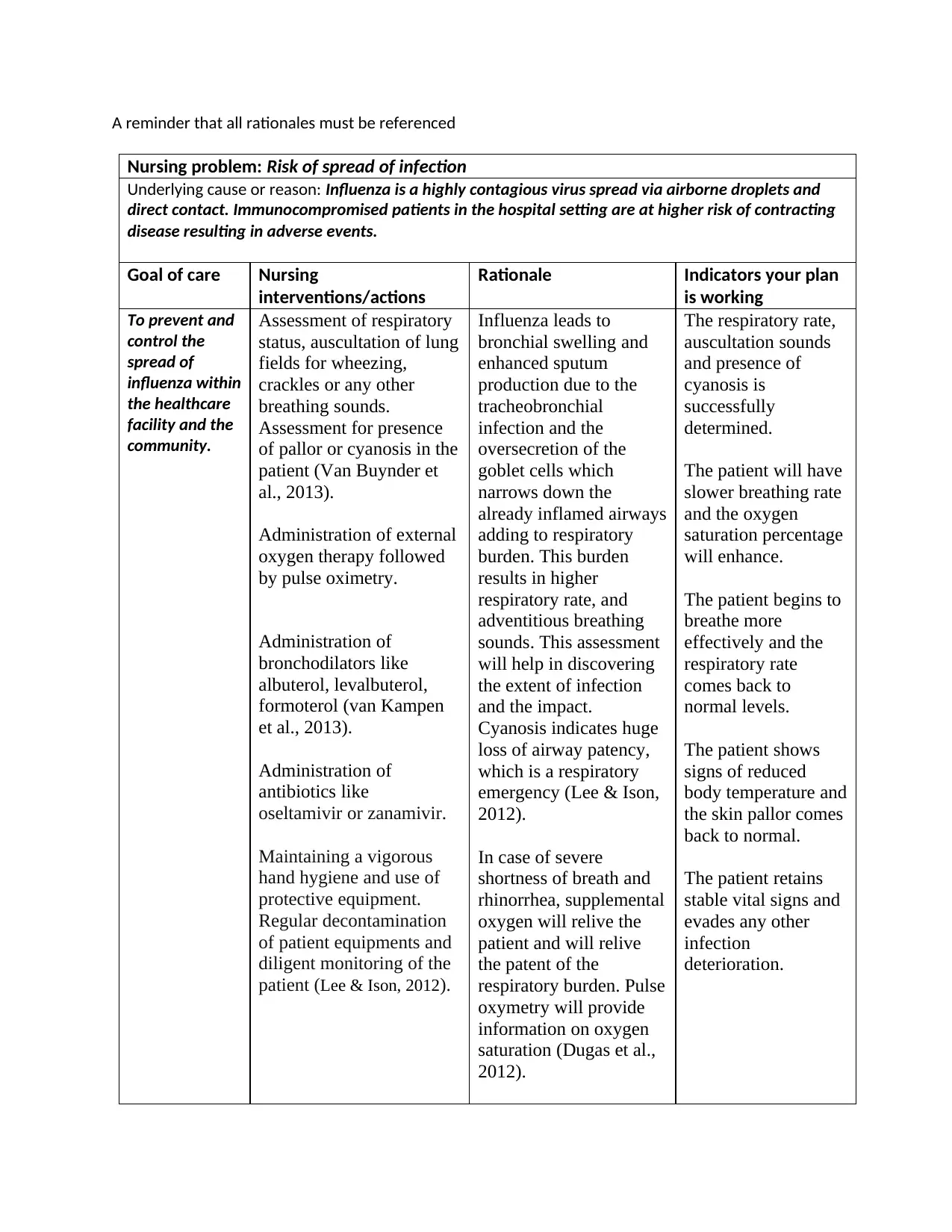
Nursing problem: Risk of spread of infection
Underlying cause or reason: Influenza is a highly contagious virus spread via airborne droplets and
direct contact. Immunocompromised patients in the hospital setting are at higher risk of contracting
disease resulting in adverse events.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
To prevent and
control the
spread of
influenza within
the healthcare
facility and the
community.
Assessment of respiratory
status, auscultation of lung
fields for wheezing,
crackles or any other
breathing sounds.
Assessment for presence
of pallor or cyanosis in the
patient (Van Buynder et
al., 2013).
Administration of external
oxygen therapy followed
by pulse oximetry.
Administration of
bronchodilators like
albuterol, levalbuterol,
formoterol (van Kampen
et al., 2013).
Administration of
antibiotics like
oseltamivir or zanamivir.
Maintaining a vigorous
hand hygiene and use of
protective equipment.
Regular decontamination
of patient equipments and
diligent monitoring of the
patient (Lee & Ison, 2012).
Influenza leads to
bronchial swelling and
enhanced sputum
production due to the
tracheobronchial
infection and the
oversecretion of the
goblet cells which
narrows down the
already inflamed airways
adding to respiratory
burden. This burden
results in higher
respiratory rate, and
adventitious breathing
sounds. This assessment
will help in discovering
the extent of infection
and the impact.
Cyanosis indicates huge
loss of airway patency,
which is a respiratory
emergency (Lee & Ison,
2012).
In case of severe
shortness of breath and
rhinorrhea, supplemental
oxygen will relive the
patient and will relive
the patent of the
respiratory burden. Pulse
oxymetry will provide
information on oxygen
saturation (Dugas et al.,
2012).
The respiratory rate,
auscultation sounds
and presence of
cyanosis is
successfully
determined.
The patient will have
slower breathing rate
and the oxygen
saturation percentage
will enhance.
The patient begins to
breathe more
effectively and the
respiratory rate
comes back to
normal levels.
The patient shows
signs of reduced
body temperature and
the skin pallor comes
back to normal.
The patient retains
stable vital signs and
evades any other
infection
deterioration.
Nursing problem: Risk of spread of infection
Underlying cause or reason: Influenza is a highly contagious virus spread via airborne droplets and
direct contact. Immunocompromised patients in the hospital setting are at higher risk of contracting
disease resulting in adverse events.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
To prevent and
control the
spread of
influenza within
the healthcare
facility and the
community.
Assessment of respiratory
status, auscultation of lung
fields for wheezing,
crackles or any other
breathing sounds.
Assessment for presence
of pallor or cyanosis in the
patient (Van Buynder et
al., 2013).
Administration of external
oxygen therapy followed
by pulse oximetry.
Administration of
bronchodilators like
albuterol, levalbuterol,
formoterol (van Kampen
et al., 2013).
Administration of
antibiotics like
oseltamivir or zanamivir.
Maintaining a vigorous
hand hygiene and use of
protective equipment.
Regular decontamination
of patient equipments and
diligent monitoring of the
patient (Lee & Ison, 2012).
Influenza leads to
bronchial swelling and
enhanced sputum
production due to the
tracheobronchial
infection and the
oversecretion of the
goblet cells which
narrows down the
already inflamed airways
adding to respiratory
burden. This burden
results in higher
respiratory rate, and
adventitious breathing
sounds. This assessment
will help in discovering
the extent of infection
and the impact.
Cyanosis indicates huge
loss of airway patency,
which is a respiratory
emergency (Lee & Ison,
2012).
In case of severe
shortness of breath and
rhinorrhea, supplemental
oxygen will relive the
patient and will relive
the patent of the
respiratory burden. Pulse
oxymetry will provide
information on oxygen
saturation (Dugas et al.,
2012).
The respiratory rate,
auscultation sounds
and presence of
cyanosis is
successfully
determined.
The patient will have
slower breathing rate
and the oxygen
saturation percentage
will enhance.
The patient begins to
breathe more
effectively and the
respiratory rate
comes back to
normal levels.
The patient shows
signs of reduced
body temperature and
the skin pallor comes
back to normal.
The patient retains
stable vital signs and
evades any other
infection
deterioration.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The bronchodilators will
expand the constricted
bronchial muscle and
will help in reviving the
breathing process (Noah
& Noah, 2013).
These antiviral
medications will act on
controlling the spread of
the infection and will
help in reducing
vulnerability to further
deterioration (Van
Buynder et al., 2013).
Targeted infection
control and diligent
monitoring will help in
reducing the infection
and will evade the
chances of secondary
infections (van Kampen
et al., 2013).
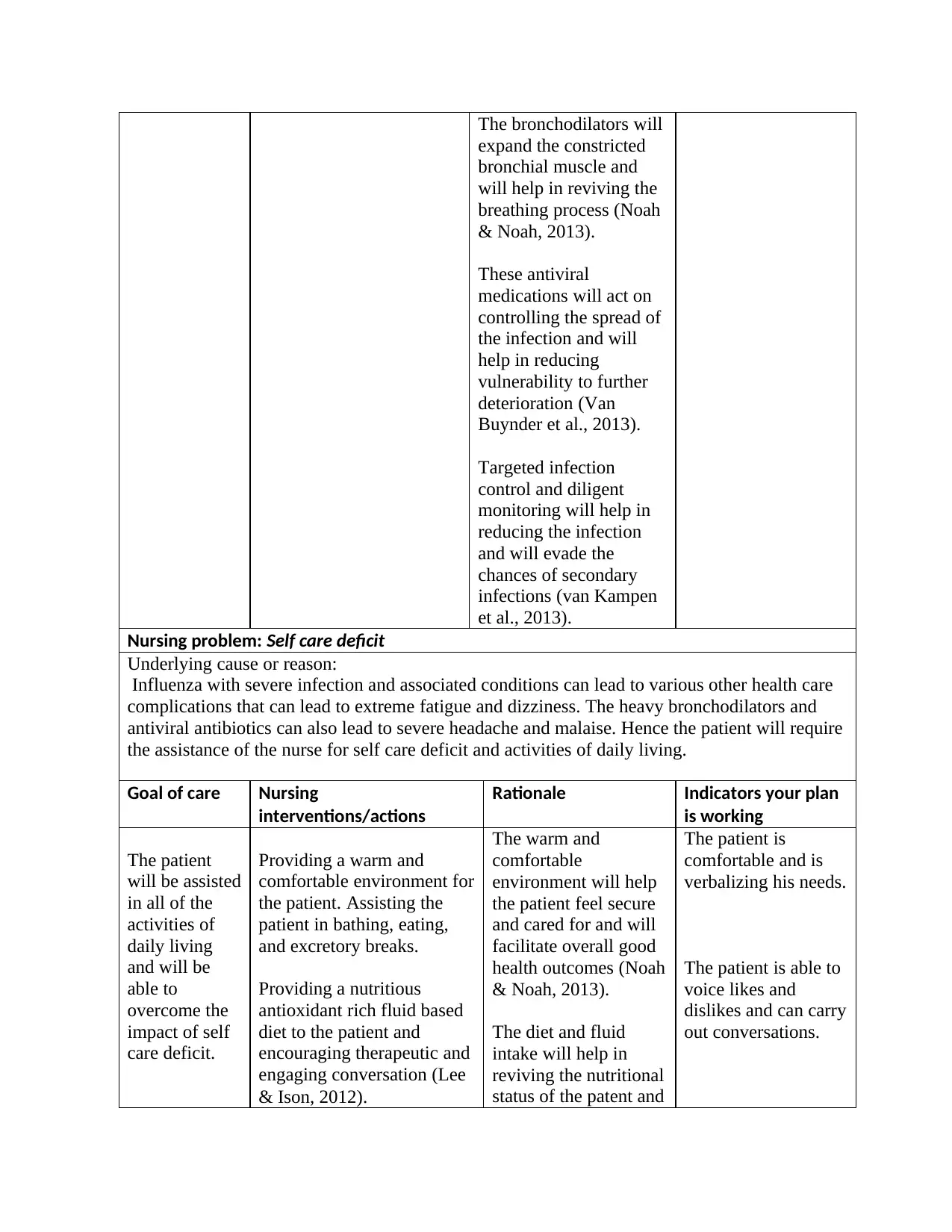
Nursing problem: Self care deficit
Underlying cause or reason:
Influenza with severe infection and associated conditions can lead to various other health care
complications that can lead to extreme fatigue and dizziness. The heavy bronchodilators and
antiviral antibiotics can also lead to severe headache and malaise. Hence the patient will require
the assistance of the nurse for self care deficit and activities of daily living.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The patient
will be assisted
in all of the
activities of
daily living
and will be
able to
overcome the
impact of self
care deficit.
Providing a warm and
comfortable environment for
the patient. Assisting the
patient in bathing, eating,
and excretory breaks.
Providing a nutritious
antioxidant rich fluid based
diet to the patient and
encouraging therapeutic and
engaging conversation (Lee
& Ison, 2012).
The warm and
comfortable
environment will help
the patient feel secure
and cared for and will
facilitate overall good
health outcomes (Noah
& Noah, 2013).
The diet and fluid
intake will help in
reviving the nutritional
status of the patent and
The patient is
comfortable and is
verbalizing his needs.
The patient is able to
voice likes and
dislikes and can carry
out conversations.
expand the constricted
bronchial muscle and
will help in reviving the
breathing process (Noah
& Noah, 2013).
These antiviral
medications will act on
controlling the spread of
the infection and will
help in reducing
vulnerability to further
deterioration (Van
Buynder et al., 2013).
Targeted infection
control and diligent
monitoring will help in
reducing the infection
and will evade the
chances of secondary
infections (van Kampen
et al., 2013).
Nursing problem: Self care deficit
Underlying cause or reason:
Influenza with severe infection and associated conditions can lead to various other health care
complications that can lead to extreme fatigue and dizziness. The heavy bronchodilators and
antiviral antibiotics can also lead to severe headache and malaise. Hence the patient will require
the assistance of the nurse for self care deficit and activities of daily living.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The patient
will be assisted
in all of the
activities of
daily living
and will be
able to
overcome the
impact of self
care deficit.
Providing a warm and
comfortable environment for
the patient. Assisting the
patient in bathing, eating,
and excretory breaks.
Providing a nutritious
antioxidant rich fluid based
diet to the patient and
encouraging therapeutic and
engaging conversation (Lee
& Ison, 2012).
The warm and
comfortable
environment will help
the patient feel secure
and cared for and will
facilitate overall good
health outcomes (Noah
& Noah, 2013).
The diet and fluid
intake will help in
reviving the nutritional
status of the patent and
The patient is
comfortable and is
verbalizing his needs.
The patient is able to
voice likes and
dislikes and can carry
out conversations.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
will help in reducing
the fatigue
(Babizhayev & Deyev,
2012).
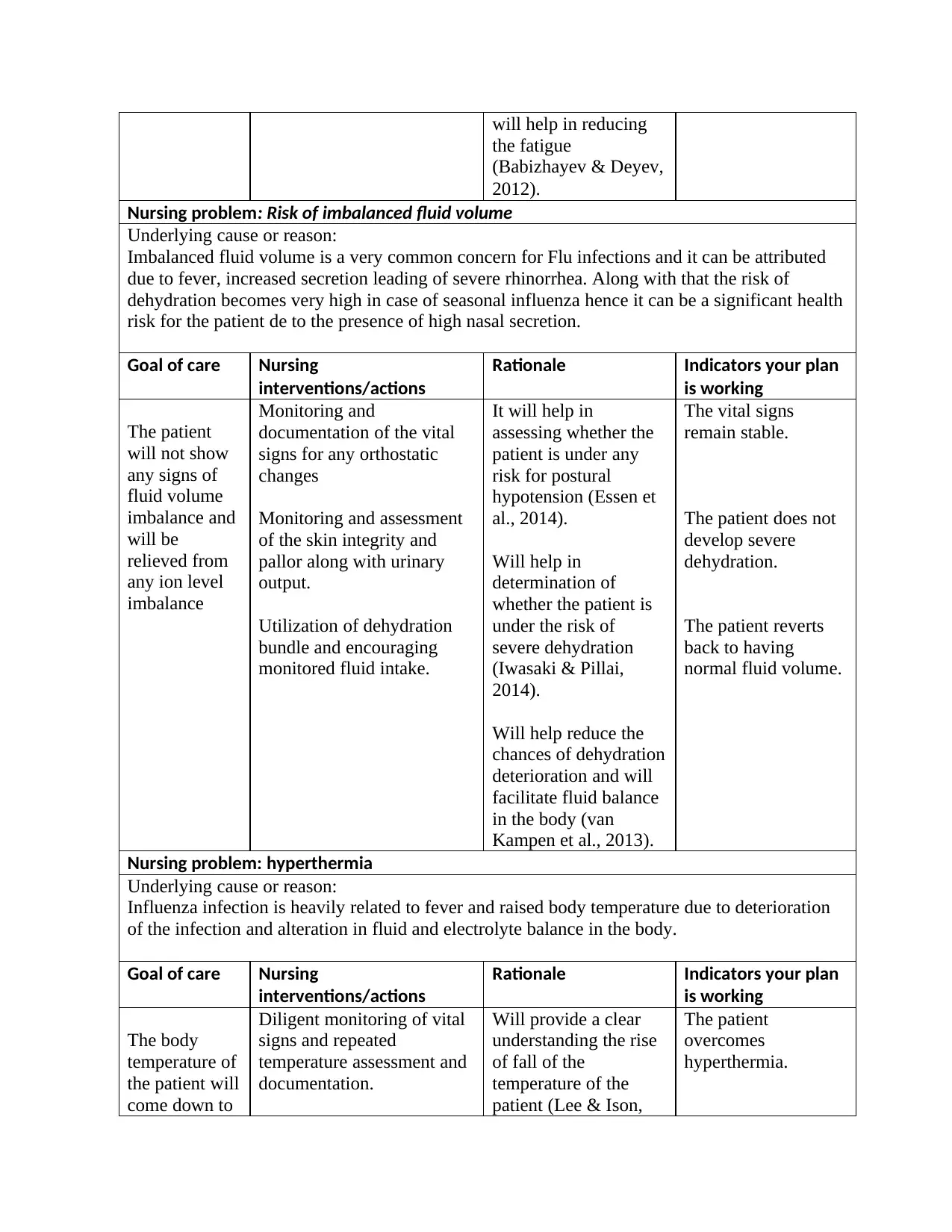
Nursing problem: Risk of imbalanced fluid volume
Underlying cause or reason:
Imbalanced fluid volume is a very common concern for Flu infections and it can be attributed
due to fever, increased secretion leading of severe rhinorrhea. Along with that the risk of
dehydration becomes very high in case of seasonal influenza hence it can be a significant health
risk for the patient de to the presence of high nasal secretion.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The patient
will not show
any signs of
fluid volume
imbalance and
will be
relieved from
any ion level
imbalance
Monitoring and
documentation of the vital
signs for any orthostatic
changes
Monitoring and assessment
of the skin integrity and
pallor along with urinary
output.
Utilization of dehydration
bundle and encouraging
monitored fluid intake.
It will help in
assessing whether the
patient is under any
risk for postural
hypotension (Essen et
al., 2014).
Will help in
determination of
whether the patient is
under the risk of
severe dehydration
(Iwasaki & Pillai,
2014).
Will help reduce the
chances of dehydration
deterioration and will
facilitate fluid balance
in the body (van
Kampen et al., 2013).
The vital signs
remain stable.
The patient does not
develop severe
dehydration.
The patient reverts
back to having
normal fluid volume.
Nursing problem: hyperthermia
Underlying cause or reason:
Influenza infection is heavily related to fever and raised body temperature due to deterioration
of the infection and alteration in fluid and electrolyte balance in the body.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The body
temperature of
the patient will
come down to
Diligent monitoring of vital
signs and repeated
temperature assessment and
documentation.
Will provide a clear
understanding the rise
of fall of the
temperature of the
patient (Lee & Ison,
The patient
overcomes
hyperthermia.
the fatigue
(Babizhayev & Deyev,
2012).
Nursing problem: Risk of imbalanced fluid volume
Underlying cause or reason:
Imbalanced fluid volume is a very common concern for Flu infections and it can be attributed
due to fever, increased secretion leading of severe rhinorrhea. Along with that the risk of
dehydration becomes very high in case of seasonal influenza hence it can be a significant health
risk for the patient de to the presence of high nasal secretion.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The patient
will not show
any signs of
fluid volume
imbalance and
will be
relieved from
any ion level
imbalance
Monitoring and
documentation of the vital
signs for any orthostatic
changes
Monitoring and assessment
of the skin integrity and
pallor along with urinary
output.
Utilization of dehydration
bundle and encouraging
monitored fluid intake.
It will help in
assessing whether the
patient is under any
risk for postural
hypotension (Essen et
al., 2014).
Will help in
determination of
whether the patient is
under the risk of
severe dehydration
(Iwasaki & Pillai,
2014).
Will help reduce the
chances of dehydration
deterioration and will
facilitate fluid balance
in the body (van
Kampen et al., 2013).
The vital signs
remain stable.
The patient does not
develop severe
dehydration.
The patient reverts
back to having
normal fluid volume.
Nursing problem: hyperthermia
Underlying cause or reason:
Influenza infection is heavily related to fever and raised body temperature due to deterioration
of the infection and alteration in fluid and electrolyte balance in the body.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The body
temperature of
the patient will
come down to
Diligent monitoring of vital
signs and repeated
temperature assessment and
documentation.
Will provide a clear
understanding the rise
of fall of the
temperature of the
patient (Lee & Ison,
The patient
overcomes
hyperthermia.
normal levels Administration of
antipyretic medication and
giving sponge baths to the
patient.
Using cooling blankets if
required by the patient.
2012).
It will help in reducing
the temperature of the
patient (Noah & Noah,
2013).
Will help in physically
reducing the
temperature and
provide utmost
comfort to the patient
(Lee & Ison, 2012).
The body
temperature of the
patient is visibly
reduced.
The patient gradually
regains normal body
temperature and the
patient is
comfortable.
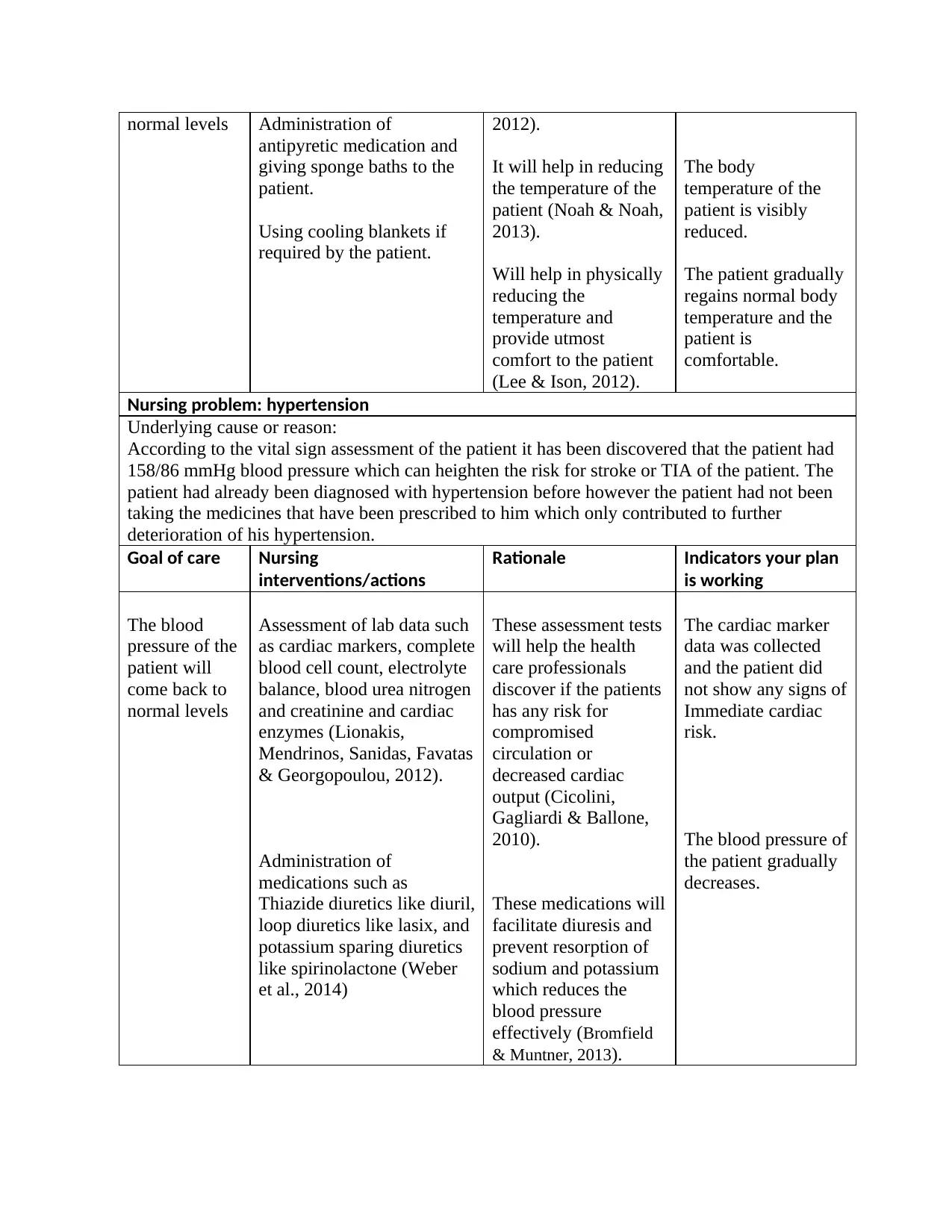
Nursing problem: hypertension
Underlying cause or reason:
According to the vital sign assessment of the patient it has been discovered that the patient had
158/86 mmHg blood pressure which can heighten the risk for stroke or TIA of the patient. The
patient had already been diagnosed with hypertension before however the patient had not been
taking the medicines that have been prescribed to him which only contributed to further
deterioration of his hypertension.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The blood
pressure of the
patient will
come back to
normal levels
Assessment of lab data such
as cardiac markers, complete
blood cell count, electrolyte
balance, blood urea nitrogen
and creatinine and cardiac
enzymes (Lionakis,
Mendrinos, Sanidas, Favatas
& Georgopoulou, 2012).
Administration of
medications such as
Thiazide diuretics like diuril,
loop diuretics like lasix, and
potassium sparing diuretics
like spirinolactone (Weber
et al., 2014)
These assessment tests
will help the health
care professionals
discover if the patients
has any risk for
compromised
circulation or
decreased cardiac
output (Cicolini,
Gagliardi & Ballone,
2010).
These medications will
facilitate diuresis and
prevent resorption of
sodium and potassium
which reduces the
blood pressure
effectively (Bromfield
& Muntner, 2013).
The cardiac marker
data was collected
and the patient did
not show any signs of
Immediate cardiac
risk.
The blood pressure of
the patient gradually
decreases.
antipyretic medication and
giving sponge baths to the
patient.
Using cooling blankets if
required by the patient.
2012).
It will help in reducing
the temperature of the
patient (Noah & Noah,
2013).
Will help in physically
reducing the
temperature and
provide utmost
comfort to the patient
(Lee & Ison, 2012).
The body
temperature of the
patient is visibly
reduced.
The patient gradually
regains normal body
temperature and the
patient is
comfortable.
Nursing problem: hypertension
Underlying cause or reason:
According to the vital sign assessment of the patient it has been discovered that the patient had
158/86 mmHg blood pressure which can heighten the risk for stroke or TIA of the patient. The
patient had already been diagnosed with hypertension before however the patient had not been
taking the medicines that have been prescribed to him which only contributed to further
deterioration of his hypertension.
Goal of care Nursing
interventions/actions
Rationale Indicators your plan
is working
The blood
pressure of the
patient will
come back to
normal levels
Assessment of lab data such
as cardiac markers, complete
blood cell count, electrolyte
balance, blood urea nitrogen
and creatinine and cardiac
enzymes (Lionakis,
Mendrinos, Sanidas, Favatas
& Georgopoulou, 2012).
Administration of
medications such as
Thiazide diuretics like diuril,
loop diuretics like lasix, and
potassium sparing diuretics
like spirinolactone (Weber
et al., 2014)
These assessment tests
will help the health
care professionals
discover if the patients
has any risk for
compromised
circulation or
decreased cardiac
output (Cicolini,
Gagliardi & Ballone,
2010).
These medications will
facilitate diuresis and
prevent resorption of
sodium and potassium
which reduces the
blood pressure
effectively (Bromfield
& Muntner, 2013).
The cardiac marker
data was collected
and the patient did
not show any signs of
Immediate cardiac
risk.
The blood pressure of
the patient gradually
decreases.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Task 3: Medication management
It has to be mentioned in this context that the patient in the case study had been going
through three particular medications for the suspicion of influenza. First and foremost, the
patient had been given oseltamivir 75mg BD oral tablets, now it has to be understood that
oseltamivir acts as an inhibitor of the key protein neuraminidase of the influenza virus (Dobson,
Whitley, Pocock & Monto, 2015). The mechanism of action of this medication is facilitated by
the reaction in the liver. The esterase enzyme in the liver converts this medication into its active
state and facilitates its inhibitory action. The second medication that has been prescribed to the
patient had been paracetamol 4/24, which has both analgesic and antipyretic effect. This
medication was prescribed to the patient to relieve him of his fever, head ache, and his muscle
and joint soreness as well (Jefferies et al., 2016). Lastly the patient had been given Fluvax IM
stat-dose. It has to be mentioned here that there is enhanced risk for the reoccurrence of
Influenza for patients like Jim. Hence, the patient required a Flu shot to ensure that the influenza
does not reoccur for the patient o any secondary infection does not occur for the patient.
For administration guidelines and nursing consideration, it has to be mentioned that
oseltamivir can have a few side effects in patients aside from any allergy. These side effects
include confusion, delirium, hallucinations, or unusual behavior. Hence, the nurse administering
this medication will have to be very careful regarding the dosage and interaction. For
paracetamol, prolonged usage can cause liver failure and disorders; hence the nurse will have to
consider the dosage and any reaction in the patient effectively. Although, the patient is only
allergic to meat and chicken, the Fluvax can cause a few complications like nausea, dizziness
and drowsiness, hence the nurse will have to monitor the patient for any adverse reaction to any
of the medication. The patient will need to be monitored for any changes in his skin integrity,
consciousness state, or for occurrence of nausea, dizziness and even oedema (Iwasaki & Pillai,
2014).
It has to be mentioned in this context that the patient in the case study had been going
through three particular medications for the suspicion of influenza. First and foremost, the
patient had been given oseltamivir 75mg BD oral tablets, now it has to be understood that
oseltamivir acts as an inhibitor of the key protein neuraminidase of the influenza virus (Dobson,
Whitley, Pocock & Monto, 2015). The mechanism of action of this medication is facilitated by
the reaction in the liver. The esterase enzyme in the liver converts this medication into its active
state and facilitates its inhibitory action. The second medication that has been prescribed to the
patient had been paracetamol 4/24, which has both analgesic and antipyretic effect. This
medication was prescribed to the patient to relieve him of his fever, head ache, and his muscle
and joint soreness as well (Jefferies et al., 2016). Lastly the patient had been given Fluvax IM
stat-dose. It has to be mentioned here that there is enhanced risk for the reoccurrence of
Influenza for patients like Jim. Hence, the patient required a Flu shot to ensure that the influenza
does not reoccur for the patient o any secondary infection does not occur for the patient.
For administration guidelines and nursing consideration, it has to be mentioned that
oseltamivir can have a few side effects in patients aside from any allergy. These side effects
include confusion, delirium, hallucinations, or unusual behavior. Hence, the nurse administering
this medication will have to be very careful regarding the dosage and interaction. For
paracetamol, prolonged usage can cause liver failure and disorders; hence the nurse will have to
consider the dosage and any reaction in the patient effectively. Although, the patient is only
allergic to meat and chicken, the Fluvax can cause a few complications like nausea, dizziness
and drowsiness, hence the nurse will have to monitor the patient for any adverse reaction to any
of the medication. The patient will need to be monitored for any changes in his skin integrity,
consciousness state, or for occurrence of nausea, dizziness and even oedema (Iwasaki & Pillai,
2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Task 4: Patient teaching
For the patient in the case study, Jim had been a homeless man with acute self care
deficit, hence there are various health risks that can cause secondary infection or can cause re-
occurrence of the infection as well. First and foremost, the patient will need to be included in the
care planning procedure for him to get a preliminary understanding of the diseases and its
impact. Along with that, it will be the responsibility of the nursing professional to help the
patient understand the role of infection control and preventative behaviour in his case. He will
also need assistance in understanding the basics of hand hygiene and other related infection
control protocols and the basics of how to prevent the influenza infections and the vaccination
benefits that he can avail from the government sponsored health difficulties (Babizhayev &
Deyev, 2012). Furthermore, the patient smokes whenever he can which can have a significant
detrimental effect on his respiratory apparatus and can even deteriorate his hypertension. Hence,
the patient will need counselling and education regarding the hazards of smoking. Lastly, Jim is
homeless and falls under the radar of extreme poverty which increases his risk for poor
nutritional outcomes. Hence the nurse will also have to educate the patient on different
community care and social support units where he can get shelter and proper nutrition along with
basic needs of life. These patient teaching factors will help the patient evade the risk for any
further infection and will help him gain better health and living condition (Essen et al., 2014).
Task 5: Clinical judgement and handover
Part A:
The temperature of the patient is rising and along with that he is showing signs of
laboured breathing and shortness of breath at breaths per minute. His heart rate is also high at
125 beats per minute, however his blood pressure is only slightly high at 124/79 mmHg. The
oxygen saturation of the patient has also decreased fairly from what the patient admitted to the
facility with. From the symptoms it can be mentioned that the patient is undergoing an episode of
shortness of breath accompanied by tachycardia. The deterioration of infection must have
For the patient in the case study, Jim had been a homeless man with acute self care
deficit, hence there are various health risks that can cause secondary infection or can cause re-
occurrence of the infection as well. First and foremost, the patient will need to be included in the
care planning procedure for him to get a preliminary understanding of the diseases and its
impact. Along with that, it will be the responsibility of the nursing professional to help the
patient understand the role of infection control and preventative behaviour in his case. He will
also need assistance in understanding the basics of hand hygiene and other related infection
control protocols and the basics of how to prevent the influenza infections and the vaccination
benefits that he can avail from the government sponsored health difficulties (Babizhayev &
Deyev, 2012). Furthermore, the patient smokes whenever he can which can have a significant
detrimental effect on his respiratory apparatus and can even deteriorate his hypertension. Hence,
the patient will need counselling and education regarding the hazards of smoking. Lastly, Jim is
homeless and falls under the radar of extreme poverty which increases his risk for poor
nutritional outcomes. Hence the nurse will also have to educate the patient on different
community care and social support units where he can get shelter and proper nutrition along with
basic needs of life. These patient teaching factors will help the patient evade the risk for any
further infection and will help him gain better health and living condition (Essen et al., 2014).
Task 5: Clinical judgement and handover
Part A:
The temperature of the patient is rising and along with that he is showing signs of
laboured breathing and shortness of breath at breaths per minute. His heart rate is also high at
125 beats per minute, however his blood pressure is only slightly high at 124/79 mmHg. The
oxygen saturation of the patient has also decreased fairly from what the patient admitted to the
facility with. From the symptoms it can be mentioned that the patient is undergoing an episode of
shortness of breath accompanied by tachycardia. The deterioration of infection must have
contributed to obstruction of the airways and ineffective gas exchange, which manifested as
labored breathing. And due to deficient oxygen delivery, his heart overcompensated to help
manage the oxygen deficiency, which contributed to his tachycardia and resulting palpation. The
nurse will have to immediately perform airway clearance and administer bronchodilators to help
reduce the labored breathing (Alhamad, Al-Ghonaim, Alfaleh, Cal & Said, 2014). The patient might
also need external oxygen along with administration of antipyretics for his fever.
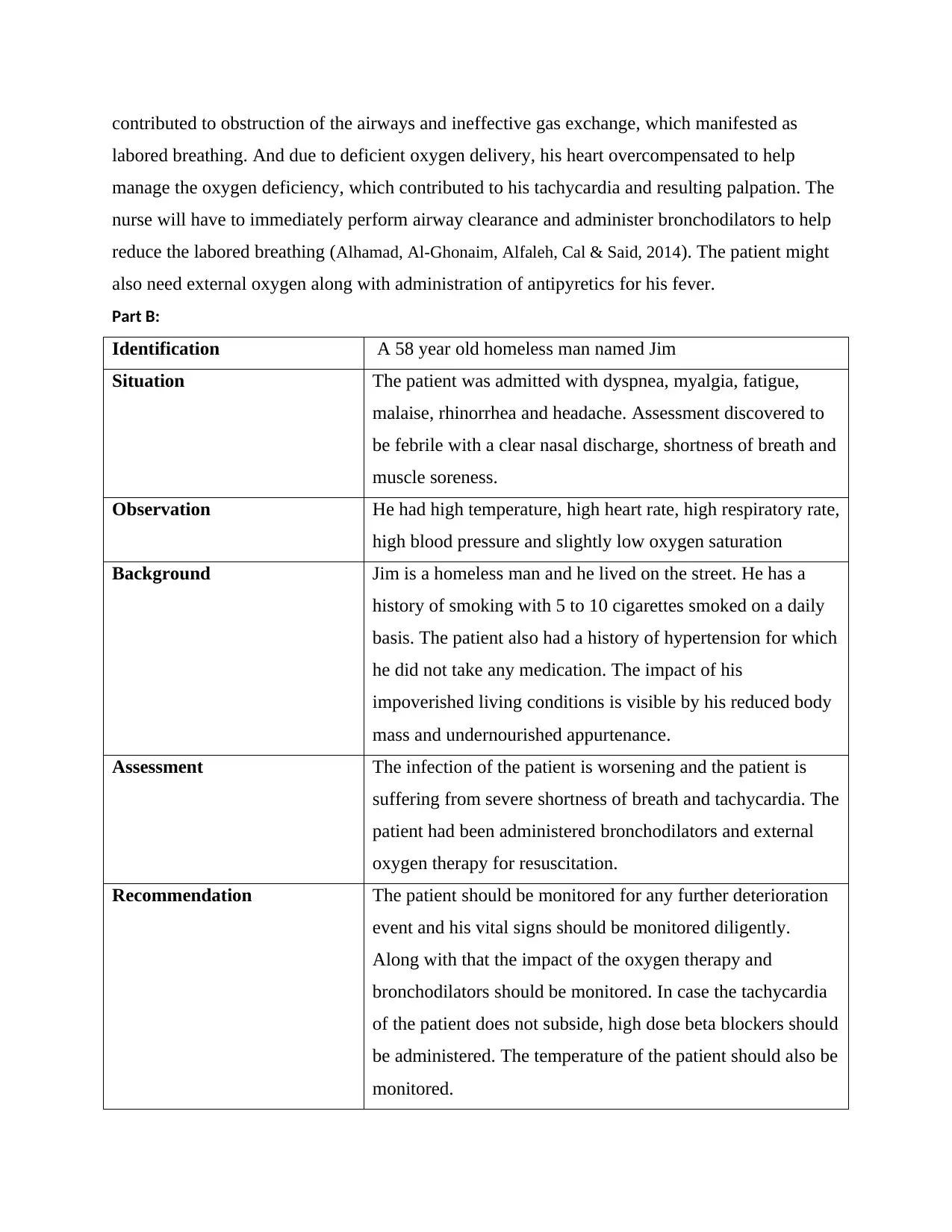
Part B:
Identification A 58 year old homeless man named Jim
Situation The patient was admitted with dyspnea, myalgia, fatigue,
malaise, rhinorrhea and headache. Assessment discovered to
be febrile with a clear nasal discharge, shortness of breath and
muscle soreness.
Observation He had high temperature, high heart rate, high respiratory rate,
high blood pressure and slightly low oxygen saturation
Background Jim is a homeless man and he lived on the street. He has a
history of smoking with 5 to 10 cigarettes smoked on a daily
basis. The patient also had a history of hypertension for which
he did not take any medication. The impact of his
impoverished living conditions is visible by his reduced body
mass and undernourished appurtenance.
Assessment The infection of the patient is worsening and the patient is
suffering from severe shortness of breath and tachycardia. The
patient had been administered bronchodilators and external
oxygen therapy for resuscitation.
Recommendation The patient should be monitored for any further deterioration
event and his vital signs should be monitored diligently.
Along with that the impact of the oxygen therapy and
bronchodilators should be monitored. In case the tachycardia
of the patient does not subside, high dose beta blockers should
be administered. The temperature of the patient should also be
monitored.
labored breathing. And due to deficient oxygen delivery, his heart overcompensated to help
manage the oxygen deficiency, which contributed to his tachycardia and resulting palpation. The
nurse will have to immediately perform airway clearance and administer bronchodilators to help
reduce the labored breathing (Alhamad, Al-Ghonaim, Alfaleh, Cal & Said, 2014). The patient might
also need external oxygen along with administration of antipyretics for his fever.
Part B:
Identification A 58 year old homeless man named Jim
Situation The patient was admitted with dyspnea, myalgia, fatigue,
malaise, rhinorrhea and headache. Assessment discovered to
be febrile with a clear nasal discharge, shortness of breath and
muscle soreness.
Observation He had high temperature, high heart rate, high respiratory rate,
high blood pressure and slightly low oxygen saturation
Background Jim is a homeless man and he lived on the street. He has a
history of smoking with 5 to 10 cigarettes smoked on a daily
basis. The patient also had a history of hypertension for which
he did not take any medication. The impact of his
impoverished living conditions is visible by his reduced body
mass and undernourished appurtenance.
Assessment The infection of the patient is worsening and the patient is
suffering from severe shortness of breath and tachycardia. The
patient had been administered bronchodilators and external
oxygen therapy for resuscitation.
Recommendation The patient should be monitored for any further deterioration
event and his vital signs should be monitored diligently.
Along with that the impact of the oxygen therapy and
bronchodilators should be monitored. In case the tachycardia
of the patient does not subside, high dose beta blockers should
be administered. The temperature of the patient should also be
monitored.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References:
Alhamad, E. H., Al-Ghonaim, M., Alfaleh, H. F., Cal, J. P., & Said, N. (2014). Pulmonary
hypertension in end-stage renal disease and post renal transplantation patients. Journal of
thoracic disease, 6(6), 606.doi: 10.3978/j.issn.2072-1439.2014.04.29.
Babizhayev, M. A., & Deyev, A. I. (2012). Management of the virulent influenza virus infection
by oral formulation of nonhydrolized carnosine and isopeptide of carnosine attenuating
proinflammatory cytokine-induced nitric oxide production. American journal of
therapeutics, 19(1), e25-e47. doi: 10.1097/MJT.0b013e3181dcf589
Bromfield, S., & Muntner, P. (2013). High blood pressure: the leading global burden of disease
risk factor and the need for worldwide prevention programs. Current hypertension
reports, 15(3), 134-136. doi: 10.1007/s11906-013-0340-9.
Cicolini, G., Gagliardi, G., & Ballone, E. (2010). Effect of Fowler’s body position on blood
pressure measurement. Journal of clinical nursing, 19(23‐24), 3581-3583.
https://doi.org/10.1111/j.1365-2702.2010.03418.x
Dobson, J., Whitley, R. J., Pocock, S., & Monto, A. S. (2015). Oseltamivir treatment for
influenza in adults: a meta-analysis of randomised controlled trials. The
Lancet, 385(9979), 1729-1737. http://dx.doi.org/10.1016/ S0140-6736(14)62449-1 Doi:
10.1016/j.vaccine.2013.07.059
Dugas, A. F., Hsieh, Y. H., Levin, S. R., Pines, J. M., Mareiniss, D. P., Mohareb, A., ... &
Rothman, R. E. (2012). Google Flu Trends: correlation with emergency department
influenza rates and crowding metrics. Clinical infectious diseases, 54(4), 463-469.
doi.org/10.1093/cid/cir883
Essen, G. A., Beran, J., Devaster, J. M., Durand, C., Duval, X., Esen, M., ... & Kovac, M. (2014).
Influenza symptoms and their impact on elderly adults: randomised trial of AS03‐
adjuvanted or non‐adjuvanted inactivated trivalent seasonal influenza vaccines. Influenza
and other respiratory viruses, 8(4), 452-462. https://doi.org/10.1111/irv.12245
Iwasaki, A., & Pillai, P. S. (2014). Innate immunity to influenza virus infection. Nature Reviews
Immunology, 14(5), 315. doi: 10.1038/nri3665.
Jefferies, S., Braithwaite, I., Walker, S., Weatherall, M., Jennings, L., Luck, M., ... & Perrin, K.
(2016). Randomized controlled trial of the effect of regular paracetamol on influenza
infection. Respirology, 21(2), 370-377. https://doi.org/10.1111/resp.12685
Alhamad, E. H., Al-Ghonaim, M., Alfaleh, H. F., Cal, J. P., & Said, N. (2014). Pulmonary
hypertension in end-stage renal disease and post renal transplantation patients. Journal of
thoracic disease, 6(6), 606.doi: 10.3978/j.issn.2072-1439.2014.04.29.
Babizhayev, M. A., & Deyev, A. I. (2012). Management of the virulent influenza virus infection
by oral formulation of nonhydrolized carnosine and isopeptide of carnosine attenuating
proinflammatory cytokine-induced nitric oxide production. American journal of
therapeutics, 19(1), e25-e47. doi: 10.1097/MJT.0b013e3181dcf589
Bromfield, S., & Muntner, P. (2013). High blood pressure: the leading global burden of disease
risk factor and the need for worldwide prevention programs. Current hypertension
reports, 15(3), 134-136. doi: 10.1007/s11906-013-0340-9.
Cicolini, G., Gagliardi, G., & Ballone, E. (2010). Effect of Fowler’s body position on blood
pressure measurement. Journal of clinical nursing, 19(23‐24), 3581-3583.
https://doi.org/10.1111/j.1365-2702.2010.03418.x
Dobson, J., Whitley, R. J., Pocock, S., & Monto, A. S. (2015). Oseltamivir treatment for
influenza in adults: a meta-analysis of randomised controlled trials. The
Lancet, 385(9979), 1729-1737. http://dx.doi.org/10.1016/ S0140-6736(14)62449-1 Doi:
10.1016/j.vaccine.2013.07.059
Dugas, A. F., Hsieh, Y. H., Levin, S. R., Pines, J. M., Mareiniss, D. P., Mohareb, A., ... &
Rothman, R. E. (2012). Google Flu Trends: correlation with emergency department
influenza rates and crowding metrics. Clinical infectious diseases, 54(4), 463-469.
doi.org/10.1093/cid/cir883
Essen, G. A., Beran, J., Devaster, J. M., Durand, C., Duval, X., Esen, M., ... & Kovac, M. (2014).
Influenza symptoms and their impact on elderly adults: randomised trial of AS03‐
adjuvanted or non‐adjuvanted inactivated trivalent seasonal influenza vaccines. Influenza
and other respiratory viruses, 8(4), 452-462. https://doi.org/10.1111/irv.12245
Iwasaki, A., & Pillai, P. S. (2014). Innate immunity to influenza virus infection. Nature Reviews
Immunology, 14(5), 315. doi: 10.1038/nri3665.
Jefferies, S., Braithwaite, I., Walker, S., Weatherall, M., Jennings, L., Luck, M., ... & Perrin, K.
(2016). Randomized controlled trial of the effect of regular paracetamol on influenza
infection. Respirology, 21(2), 370-377. https://doi.org/10.1111/resp.12685

Lee, N., & Ison, M. G. (2012). Diagnosis, management and outcomes of adults hospitalized with
influenza. Antiviral therapy, 17(1), 143. doi: 10.3851/IMP2059
Lionakis, N., Mendrinos, D., Sanidas, E., Favatas, G., & Georgopoulou, M. (2012).
Hypertension in the elderly. World journal of cardiology, 4(5), 135.
doi: 10.4330/wjc.v4.i5.135
Noah, D. L., & Noah, J. W. (2013). Adapting global influenza management strategies to address
emerging viruses. American Journal of Physiology-Lung Cellular and Molecular
Physiology, 305(2), L108-L117. Doi: 10.1152/ajplung.00105.2013
Olgers, T. J., Dijkstra, R. S., Drost-de Klerck, A. M., & Ter Maaten, J. C. (2017). The ABCDE
primary assessment in the emergency department in medically ill patients: an
observational pilot study. Red eyes and mucous ulcers; what is your diagnosis?, 106.
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28469050
Ortiz, J. R., Rudd, K. E., Clark, D. V., Jacob, S. T., & West, T. E. (2013). Clinical research
during a public health emergency: a systematic review of severe pandemic influenza
management. Critical care medicine, 41(5), 1345-1352.
doi:10.1097/CCM.0b013e3182771386
Van Buynder, P. G., Konrad, S., Van Buynder, J. L., Brodkin, E., Krajden, M., Ramler, G., &
Bigham, M. (2013). The comparative effectiveness of adjuvanted and unadjuvanted
trivalent inactivated influenza vaccine (TIV) in the elderly. Vaccine, 31(51), 6122-6128.
Doi: 10.1016/j.vaccine.2013.07.059
van Kampen, J. J., Bielefeld‐Buss, A. J., Ott, A., Maaskant, J., Faber, H. J., Lutisan, J. G., &
Boucher, C. A. (2013). Case report: Oseltamivir‐induced resistant pandemic influenza A
(H1N1) Virus infection in a patient with AIDS and Pneumocystis jirovecii
pneumonia. Journal of medical virology, 85(6), 941-943. doi.org/10.1002/jmv.23560
Weber, M. A., Schiffrin, E. L., White, W. B., Mann, S., Lindholm, L. H., Kenerson, J. G., ... &
Cohen, D. L. (2014). Clinical practice guidelines for the management of hypertension in
the community. The journal of clinical hypertension, 16(1),
14-26.DOI:10.1097/HJH.0000000000000065
influenza. Antiviral therapy, 17(1), 143. doi: 10.3851/IMP2059
Lionakis, N., Mendrinos, D., Sanidas, E., Favatas, G., & Georgopoulou, M. (2012).
Hypertension in the elderly. World journal of cardiology, 4(5), 135.
doi: 10.4330/wjc.v4.i5.135
Noah, D. L., & Noah, J. W. (2013). Adapting global influenza management strategies to address
emerging viruses. American Journal of Physiology-Lung Cellular and Molecular
Physiology, 305(2), L108-L117. Doi: 10.1152/ajplung.00105.2013
Olgers, T. J., Dijkstra, R. S., Drost-de Klerck, A. M., & Ter Maaten, J. C. (2017). The ABCDE
primary assessment in the emergency department in medically ill patients: an
observational pilot study. Red eyes and mucous ulcers; what is your diagnosis?, 106.
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28469050
Ortiz, J. R., Rudd, K. E., Clark, D. V., Jacob, S. T., & West, T. E. (2013). Clinical research
during a public health emergency: a systematic review of severe pandemic influenza
management. Critical care medicine, 41(5), 1345-1352.
doi:10.1097/CCM.0b013e3182771386
Van Buynder, P. G., Konrad, S., Van Buynder, J. L., Brodkin, E., Krajden, M., Ramler, G., &
Bigham, M. (2013). The comparative effectiveness of adjuvanted and unadjuvanted
trivalent inactivated influenza vaccine (TIV) in the elderly. Vaccine, 31(51), 6122-6128.
Doi: 10.1016/j.vaccine.2013.07.059
van Kampen, J. J., Bielefeld‐Buss, A. J., Ott, A., Maaskant, J., Faber, H. J., Lutisan, J. G., &
Boucher, C. A. (2013). Case report: Oseltamivir‐induced resistant pandemic influenza A
(H1N1) Virus infection in a patient with AIDS and Pneumocystis jirovecii
pneumonia. Journal of medical virology, 85(6), 941-943. doi.org/10.1002/jmv.23560
Weber, M. A., Schiffrin, E. L., White, W. B., Mann, S., Lindholm, L. H., Kenerson, J. G., ... &
Cohen, D. L. (2014). Clinical practice guidelines for the management of hypertension in
the community. The journal of clinical hypertension, 16(1),
14-26.DOI:10.1097/HJH.0000000000000065
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



