NUR341 Assessment 2: Person-Centered Assessment and Care for Elderly
VerifiedAdded on 2022/12/27
|24
|5960
|61
Report
AI Summary
This report presents a comprehensive analysis of a 71-year-old patient, Mr. Willie Jungala, admitted to the hospital following a fall with a soft tissue injury to his right hip. The report details the patient's medical history, including hypertension, type 2 diabetes, and unstable angina, along with his social and lifestyle factors. It outlines the goals and relevance of various assessments, including alcohol withdrawal risk, cognitive function, fall risk, functional, and nutritional assessments. Furthermore, the report provides a plan and implementation section, focusing on nursing actions and referrals related to one factor contributing to the patient's fall. The report adheres to the assignment's requirements, including a detailed assessment of the patient's condition and the formulation of a person-centered care plan. The report also examines the importance of the role of the nurse in the interdisciplinary approach to care planning and implementation of care.
NUR341 Assessment 2
Mr Willie Jungala is a 71-year-old
gentleman that has been admitted to
hospital post fall with soft tissue injury to
right hip.
History Assessment data
Patient profile Willie Jungala, 71-year-old man from Alice Springs
Chief complaint Pain to right hip following fall
History of complaint
Was going to kitchen to make a sandwich and tripped on
kids tonka truck. Landed on the floor on his right side.
Following fall, Willie was experiencing pain on movement
and difficulty weight bearing. Two teenage grandchildren
tried to help him up but too painful, so they called an
ambulance.
Phx Hypertension, Type 2 Diabetes, Unstable Angina
Allergies Nil known allergies.
Medications Aspirin 100mg mane
Perindopril 2mg mane
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
1
Mr Willie Jungala is a 71-year-old
gentleman that has been admitted to
hospital post fall with soft tissue injury to
right hip.
History Assessment data
Patient profile Willie Jungala, 71-year-old man from Alice Springs
Chief complaint Pain to right hip following fall
History of complaint
Was going to kitchen to make a sandwich and tripped on
kids tonka truck. Landed on the floor on his right side.
Following fall, Willie was experiencing pain on movement
and difficulty weight bearing. Two teenage grandchildren
tried to help him up but too painful, so they called an
ambulance.
Phx Hypertension, Type 2 Diabetes, Unstable Angina
Allergies Nil known allergies.
Medications Aspirin 100mg mane
Perindopril 2mg mane
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
Metformin 1000mg TDS
GTN 600mcg tablets S/L prn
Alcohol use Social - 2 to 3 beers (mid-strength), 2 to 3 times per week.
Tobacco use
Non-smoker. Regular exposure to campfire smoke. Most
nights have a campfire burning - sit by campfire and enjoy
the night 'yarning' or listening to music.
Drug use Nil.
Home environment
Lives in town camp in house with extended family.
Approximately 12 family members staying at house: wife;
daughter and her 4 teenage boys; daughter and her two
toddlers; son's two adult boys.
Work environment Was a station hand. Retired 5 years ago.
Stress
Sometimes. At the moment, youngest daughter that lives at
home there with her two toddlers, has recently been
diagnosed with cancer. A few drinks and a few laughs help
ease the stress.
Education Year 9 schooling.
Economic status
Own land and house out bush but staying in town for a
while.
Ethnic background
Aboriginal. Speaks Waramungu, Walpiri, Eastern and
Central Arrente, Western Arrentre and English.
Religion/ spirituality
Baptised Catholic by missionaries when young. Only goes
to church for funerals. Willie's spirit is strengthened by
family and country.
Sexual practice Married. Been with wife for 51 years. Have one son and two
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
2
Metformin 1000mg TDS
GTN 600mcg tablets S/L prn
Alcohol use Social - 2 to 3 beers (mid-strength), 2 to 3 times per week.
Tobacco use
Non-smoker. Regular exposure to campfire smoke. Most
nights have a campfire burning - sit by campfire and enjoy
the night 'yarning' or listening to music.
Drug use Nil.
Home environment
Lives in town camp in house with extended family.
Approximately 12 family members staying at house: wife;
daughter and her 4 teenage boys; daughter and her two
toddlers; son's two adult boys.
Work environment Was a station hand. Retired 5 years ago.
Stress
Sometimes. At the moment, youngest daughter that lives at
home there with her two toddlers, has recently been
diagnosed with cancer. A few drinks and a few laughs help
ease the stress.
Education Year 9 schooling.
Economic status
Own land and house out bush but staying in town for a
while.
Ethnic background
Aboriginal. Speaks Waramungu, Walpiri, Eastern and
Central Arrente, Western Arrentre and English.
Religion/ spirituality
Baptised Catholic by missionaries when young. Only goes
to church for funerals. Willie's spirit is strengthened by
family and country.
Sexual practice Married. Been with wife for 51 years. Have one son and two
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
2

NUR341 Assessment 2
daughters.
ADLs Independent.
IADLs
Does not drive any more due to decreased vision (diabetic
retinopathy). Starting to get cataracts. Had glasses a few
years ago but they don't work so well any more.
Cognitive function No worries.
Diet Diabetic diet
Sleep 7-8 hours a night.
Health check ups
Regular check-ups every few months with diabetic doctors/
clinics. Go to medical service if need to. Moves between
medical services depending on where he is staying at.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
3
daughters.
ADLs Independent.
IADLs
Does not drive any more due to decreased vision (diabetic
retinopathy). Starting to get cataracts. Had glasses a few
years ago but they don't work so well any more.
Cognitive function No worries.
Diet Diabetic diet
Sleep 7-8 hours a night.
Health check ups
Regular check-ups every few months with diabetic doctors/
clinics. Go to medical service if need to. Moves between
medical services depending on where he is staying at.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NUR341 Assessment 2
Physical
assessment
Assessment data
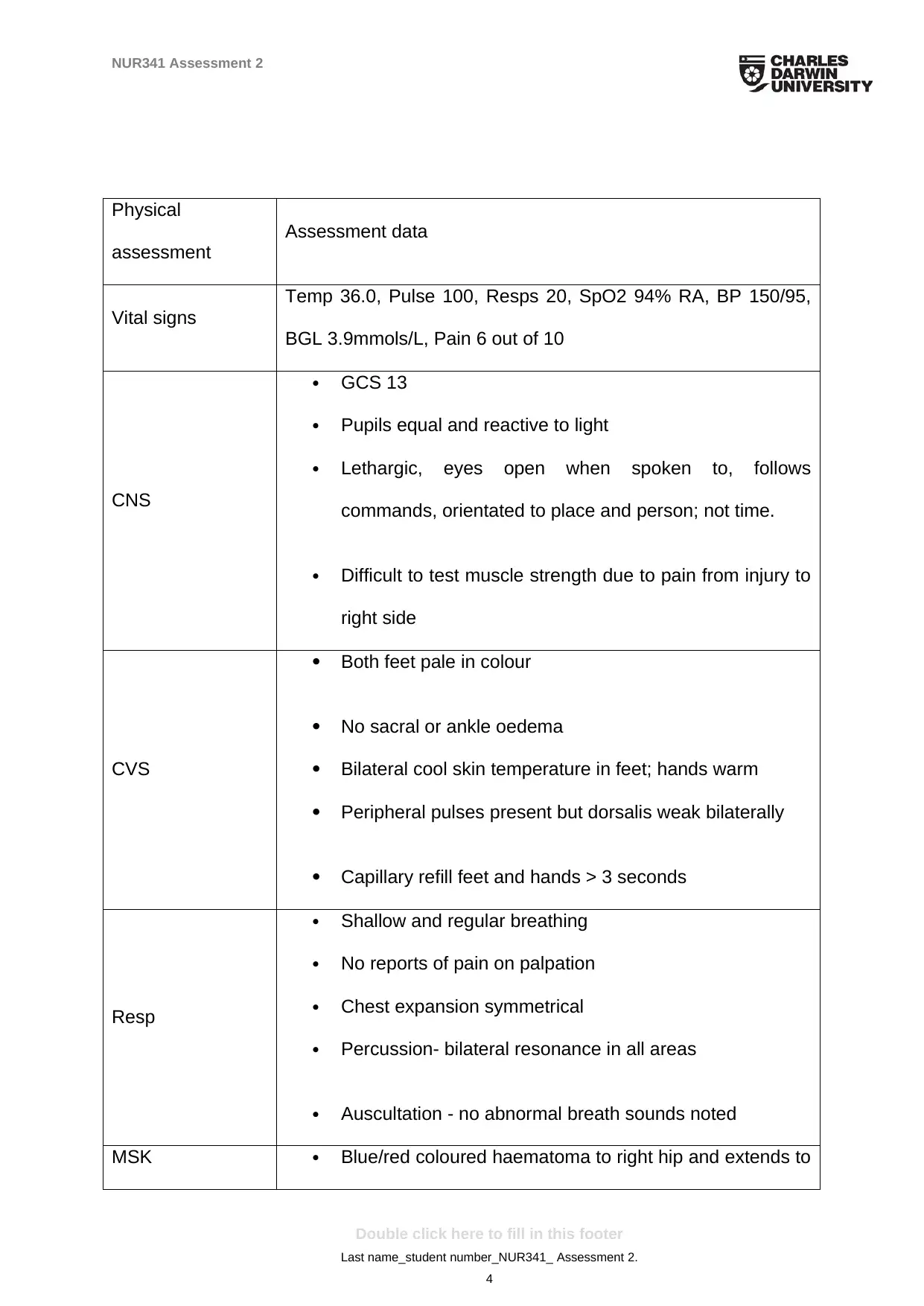
Vital signs
Temp 36.0, Pulse 100, Resps 20, SpO2 94% RA, BP 150/95,
BGL 3.9mmols/L, Pain 6 out of 10
CNS
GCS 13
Pupils equal and reactive to light
Lethargic, eyes open when spoken to, follows
commands, orientated to place and person; not time.
Difficult to test muscle strength due to pain from injury to
right side
CVS
Both feet pale in colour
No sacral or ankle oedema
Bilateral cool skin temperature in feet; hands warm
Peripheral pulses present but dorsalis weak bilaterally
Capillary refill feet and hands > 3 seconds
Resp
Shallow and regular breathing
No reports of pain on palpation
Chest expansion symmetrical
Percussion- bilateral resonance in all areas
Auscultation - no abnormal breath sounds noted
MSK Blue/red coloured haematoma to right hip and extends to
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
4
Physical
assessment
Assessment data
Vital signs
Temp 36.0, Pulse 100, Resps 20, SpO2 94% RA, BP 150/95,
BGL 3.9mmols/L, Pain 6 out of 10
CNS
GCS 13
Pupils equal and reactive to light
Lethargic, eyes open when spoken to, follows
commands, orientated to place and person; not time.
Difficult to test muscle strength due to pain from injury to
right side
CVS
Both feet pale in colour
No sacral or ankle oedema
Bilateral cool skin temperature in feet; hands warm
Peripheral pulses present but dorsalis weak bilaterally
Capillary refill feet and hands > 3 seconds
Resp
Shallow and regular breathing
No reports of pain on palpation
Chest expansion symmetrical
Percussion- bilateral resonance in all areas
Auscultation - no abnormal breath sounds noted
MSK Blue/red coloured haematoma to right hip and extends to
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
right buttock
Swelling evident
Skin intact
Decreased range of movement around hip
Tender on palpation of right hip area
Reluctant to attempt walking due to pain
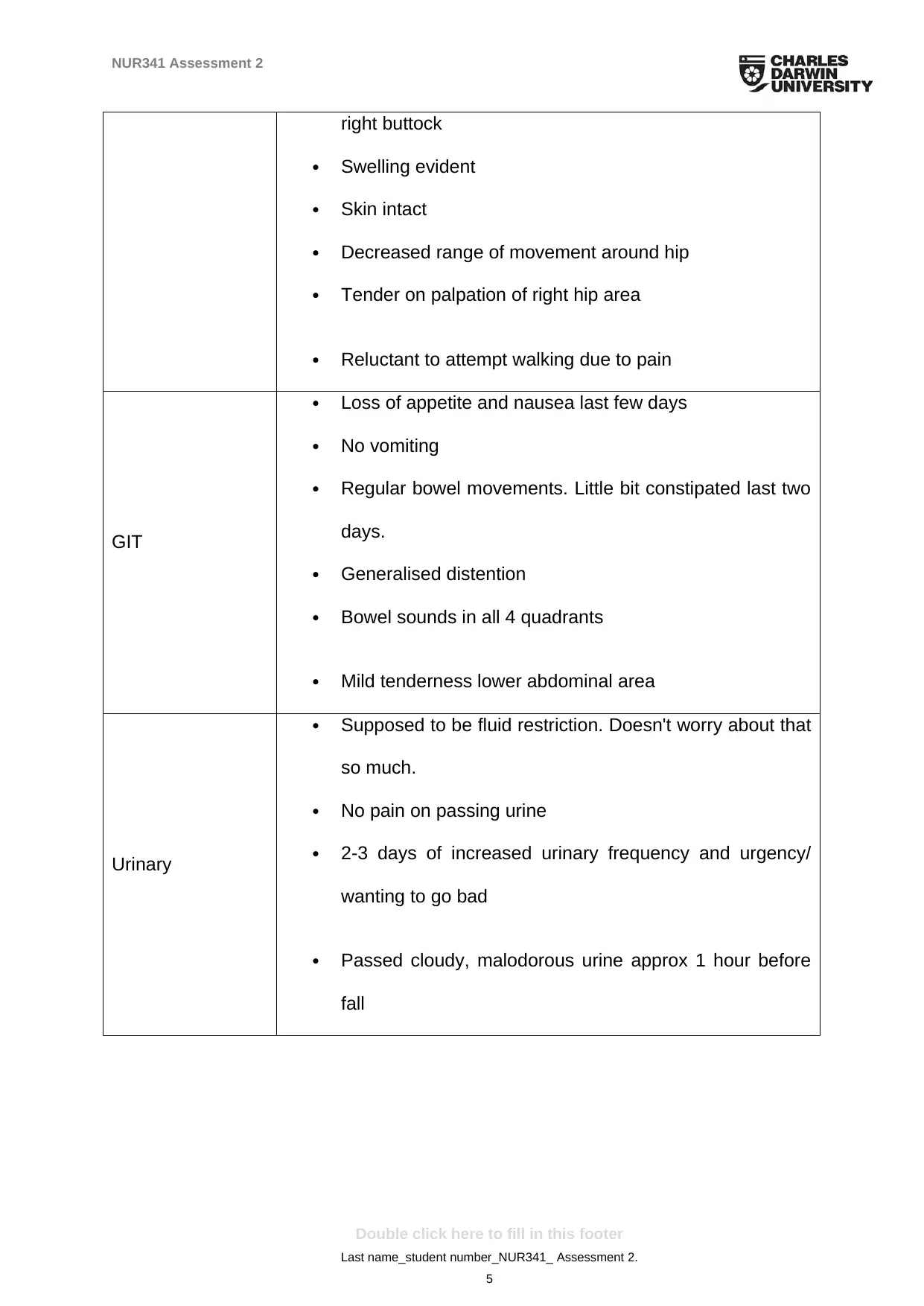
GIT
Loss of appetite and nausea last few days
No vomiting
Regular bowel movements. Little bit constipated last two
days.
Generalised distention
Bowel sounds in all 4 quadrants
Mild tenderness lower abdominal area
Urinary
Supposed to be fluid restriction. Doesn't worry about that
so much.
No pain on passing urine
2-3 days of increased urinary frequency and urgency/
wanting to go bad
Passed cloudy, malodorous urine approx 1 hour before
fall
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
5
right buttock
Swelling evident
Skin intact
Decreased range of movement around hip
Tender on palpation of right hip area
Reluctant to attempt walking due to pain
GIT
Loss of appetite and nausea last few days
No vomiting
Regular bowel movements. Little bit constipated last two
days.
Generalised distention
Bowel sounds in all 4 quadrants
Mild tenderness lower abdominal area
Urinary
Supposed to be fluid restriction. Doesn't worry about that
so much.
No pain on passing urine
2-3 days of increased urinary frequency and urgency/
wanting to go bad
Passed cloudy, malodorous urine approx 1 hour before
fall
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
5
NUR341 Assessment 2
Part 1: Assessment (1000 words)
Hospital policy is that Mr Jungala receive the assessments below. Detail the goal or
the purpose of these assessments and how they relate to Mr Jungala.
Assessment - Description & linkage to patient
Alcohol withdrawal risk assessment
Complications associated with withdrawal of alcohol have been found associated
with a noteworthy demand in several healthcare resources, concomitant with an
elevation in the rates of mortality and morbidity. Alcohol withdrawal is an umbrella
term that is manifested in the form of a plethora of symptoms that generally comprise
of shakiness, anxiety, and vomiting, sweating and increased heart rate. Conducting
an alcohol withdrawal risk assessment is vital owing to the fact that the basic
purpose of this assessment focuses on determining the probability and severity of
symptoms that might be observed among patient who have been identified to
present a major concern for withdrawal of alcohol (Maldonado et al., 2014). Such risk
assessments generally comprise of determining whether the patients feel symptoms
of nausea, vomiting, tremor, anxiety, paraoxysmal sweats, tactile disturbances,
agitation, and auditory disturbances. The assessments are related to Mr Jungala
taking into consideration his habit of being a social drinker, and consuming alcohol
twice or thrice, each week. Subjecting the patient to this assessment will provide
adequate an objective and efficient means of determining alcohol withdrawal. In
addition, usage of the scale might also result in reducing the incidence of
benzodiazepine over-sedation that is commonly administered for treatment of
alcohol dependence (Sachdeva, Choudhary & Chandra, 2015).
Cognitive assessment
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
6
Part 1: Assessment (1000 words)
Hospital policy is that Mr Jungala receive the assessments below. Detail the goal or
the purpose of these assessments and how they relate to Mr Jungala.
Assessment - Description & linkage to patient
Alcohol withdrawal risk assessment
Complications associated with withdrawal of alcohol have been found associated
with a noteworthy demand in several healthcare resources, concomitant with an
elevation in the rates of mortality and morbidity. Alcohol withdrawal is an umbrella
term that is manifested in the form of a plethora of symptoms that generally comprise
of shakiness, anxiety, and vomiting, sweating and increased heart rate. Conducting
an alcohol withdrawal risk assessment is vital owing to the fact that the basic
purpose of this assessment focuses on determining the probability and severity of
symptoms that might be observed among patient who have been identified to
present a major concern for withdrawal of alcohol (Maldonado et al., 2014). Such risk
assessments generally comprise of determining whether the patients feel symptoms
of nausea, vomiting, tremor, anxiety, paraoxysmal sweats, tactile disturbances,
agitation, and auditory disturbances. The assessments are related to Mr Jungala
taking into consideration his habit of being a social drinker, and consuming alcohol
twice or thrice, each week. Subjecting the patient to this assessment will provide
adequate an objective and efficient means of determining alcohol withdrawal. In
addition, usage of the scale might also result in reducing the incidence of
benzodiazepine over-sedation that is commonly administered for treatment of
alcohol dependence (Sachdeva, Choudhary & Chandra, 2015).
Cognitive assessment
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NUR341 Assessment 2
People with cognitive complaints or memory concerns are generally subjected to
cognitive assessment owing to the fact that detecting an impairment in cognition at
an early state provides better opportunities for gaining benefits from the intended
treatment. In addition, evaluation of the results of cognitive assessment also reduces
anxiety and increases the chances of participation in clinical decision making. The
basic purpose of a cognitive assessment can be accredited to the fact that it helps
healthcare practitioners to assess important domains of brain functioning such as,
concentration, language, memory, processing speed, and reasoning capabilities
(Tan et al., 2015). Cognitive assessments are also imperative for gaining complete
wellness and enhanced quality of since they are able to evaluate the health of the
brain that is imperative for conducting all physiological activities (Estes, 2013). In
addition, baseline cognitive assessment will also act in the form of a reference point
for measuring the patient’s health, against brain injury or major illness (Julayanont et
al., 2015). Its relevance to the case scenario can be associated with the fact that
although Mr Jungala does not report any cognitive impairment and is also able to
independently carry out the activities of daily living, age-associated cognitive decline
is a common phenomenon and encompasses a decrease in the size of the brain and
loss of gray matter volume, thus leading to disruption of cognitive faculties.
Falls assessment
Fall assessment are a common tool used in the form of a safety initiative by
healthcare professionals, while caring for patient who are aged, or identified to be at
a high-risk of suffering from falls. Conducting a fall risk assessment is vital owing to
the fact that it comprises of conduction of a validated tool that is imperative in
lowering the risk of falls among older patients. This assessment commonly takes into
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
7
People with cognitive complaints or memory concerns are generally subjected to
cognitive assessment owing to the fact that detecting an impairment in cognition at
an early state provides better opportunities for gaining benefits from the intended
treatment. In addition, evaluation of the results of cognitive assessment also reduces
anxiety and increases the chances of participation in clinical decision making. The
basic purpose of a cognitive assessment can be accredited to the fact that it helps
healthcare practitioners to assess important domains of brain functioning such as,
concentration, language, memory, processing speed, and reasoning capabilities
(Tan et al., 2015). Cognitive assessments are also imperative for gaining complete
wellness and enhanced quality of since they are able to evaluate the health of the
brain that is imperative for conducting all physiological activities (Estes, 2013). In
addition, baseline cognitive assessment will also act in the form of a reference point
for measuring the patient’s health, against brain injury or major illness (Julayanont et
al., 2015). Its relevance to the case scenario can be associated with the fact that
although Mr Jungala does not report any cognitive impairment and is also able to
independently carry out the activities of daily living, age-associated cognitive decline
is a common phenomenon and encompasses a decrease in the size of the brain and
loss of gray matter volume, thus leading to disruption of cognitive faculties.
Falls assessment
Fall assessment are a common tool used in the form of a safety initiative by
healthcare professionals, while caring for patient who are aged, or identified to be at
a high-risk of suffering from falls. Conducting a fall risk assessment is vital owing to
the fact that it comprises of conduction of a validated tool that is imperative in
lowering the risk of falls among older patients. This assessment commonly takes into
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
consideration the different reasons due to which an older patient is prone to suffer
falls such as, falls history, medical conditions, medications, foot problems, sensory
loss, cognitive status, nutritional status, continence, and function (Pfortmueller,
Lindner & Exadaktylos, 2014). The assessment tools determine the probability of a
person from suffering falls by calculating risk scores that also takes into account their
age, patient care equipment, elimination, and mobility. It is imperative for conducting
this risk assessment in the patient Mr Jungala since falls have been identified as a
significant contributor of mortality and morbidity among elderly, and are an essential
category of preventable injuries. In addition, suffering a fall in old age is most often
multifactorial and results in injuries to soft tissues, dislocation, fractures, pressure
sores or disuse atrophy (van Schooten et al., 2015). Mr Jungala had already suffered
a fall, following which he reported presence of pain in his right hip. This would result
in mobility impairment. Therefore, subjecting him to fall assessment would help in
determining his pain severity, followed by implementation of an appropriate care
plan.
Functional assessment
Conducting a functional behaviour assessment (FBA) refers to the procedure of
identification of particular target behaviour in patients, in addition to providing an
insight into the purpose of the manifested behaviour and the underlying factors that
govern it (Bonnechere et al., 2014). In other words, functional assessment acts in the
form of incessant collaborative procedure that comprises of a combination of
observation, inquiring evocative questions, paying attention to family history, and
evaluating the individual behaviour and skills of a person, within commonplace
routines and regular situations. Hence, conducting a geriatric functional assessment
has the primary objective of being able to accurately evaluate the cognitive,
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
8
consideration the different reasons due to which an older patient is prone to suffer
falls such as, falls history, medical conditions, medications, foot problems, sensory
loss, cognitive status, nutritional status, continence, and function (Pfortmueller,
Lindner & Exadaktylos, 2014). The assessment tools determine the probability of a
person from suffering falls by calculating risk scores that also takes into account their
age, patient care equipment, elimination, and mobility. It is imperative for conducting
this risk assessment in the patient Mr Jungala since falls have been identified as a
significant contributor of mortality and morbidity among elderly, and are an essential
category of preventable injuries. In addition, suffering a fall in old age is most often
multifactorial and results in injuries to soft tissues, dislocation, fractures, pressure
sores or disuse atrophy (van Schooten et al., 2015). Mr Jungala had already suffered
a fall, following which he reported presence of pain in his right hip. This would result
in mobility impairment. Therefore, subjecting him to fall assessment would help in
determining his pain severity, followed by implementation of an appropriate care
plan.
Functional assessment
Conducting a functional behaviour assessment (FBA) refers to the procedure of
identification of particular target behaviour in patients, in addition to providing an
insight into the purpose of the manifested behaviour and the underlying factors that
govern it (Bonnechere et al., 2014). In other words, functional assessment acts in the
form of incessant collaborative procedure that comprises of a combination of
observation, inquiring evocative questions, paying attention to family history, and
evaluating the individual behaviour and skills of a person, within commonplace
routines and regular situations. Hence, conducting a geriatric functional assessment
has the primary objective of being able to accurately evaluate the cognitive,
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
8
NUR341 Assessment 2
functional and affective status of the elderly patients, in addition to engaging in
effective communication with them (Ward et al., 2015). Functional assessment also
encompasses asking questions with the aim of identifying presence of impairment (if
any) in the activities of daily living, assessing gait impairment, screening for major
depressive disorder, and facilitating communication (Estes, 2013). Owing to the fact
that Mr Jungala is an elderly patient, reports decreased vision due to diabetic
retinopathy and has also suffered a fall. Thus, subjecting him to functional
assessment will facilitate determination of the health risks of the patient.
Nutritional assessment
Conducting a nutritional assessment involves an in-depth evaluation of subjective
and objective data related to the nutrient and food intake of a person, in addition to
the medical history, and lifestyle habits. The objective of nutritional screening is to
speedily recognise patients who are at a great nutritional risk (Prado & Heymsfield,
2014). In addition, the purpose of subjecting patients to nutritional assessment is to
gain a sound understanding of the nutritional status of the patients, while clinically
defining presence of malnutrition in the patients, while monitoring variations in their
nutritional status. Under most circumstances, failure to accurately identify nutritional
risks often results in under-treatment of patients that directly threatens their health
and wellbeing, and creates a negative impact on their quality of life (Lorenzo-López
et al., 2017). The nutritional assessments would generally comprise of four broad
categories that will take into account biochemical, dietary, clinical and
anthropometric parameters of the patient Mr Jungala. Owing to the fact that he has
been admitted to the hospital following a hip injury, and older adults have been
identified to be at a risk for a compromised nutritional status due to aging related
changes, and several social, psychological and cognitive factors, there is a need to
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
9
functional and affective status of the elderly patients, in addition to engaging in
effective communication with them (Ward et al., 2015). Functional assessment also
encompasses asking questions with the aim of identifying presence of impairment (if
any) in the activities of daily living, assessing gait impairment, screening for major
depressive disorder, and facilitating communication (Estes, 2013). Owing to the fact
that Mr Jungala is an elderly patient, reports decreased vision due to diabetic
retinopathy and has also suffered a fall. Thus, subjecting him to functional
assessment will facilitate determination of the health risks of the patient.
Nutritional assessment
Conducting a nutritional assessment involves an in-depth evaluation of subjective
and objective data related to the nutrient and food intake of a person, in addition to
the medical history, and lifestyle habits. The objective of nutritional screening is to
speedily recognise patients who are at a great nutritional risk (Prado & Heymsfield,
2014). In addition, the purpose of subjecting patients to nutritional assessment is to
gain a sound understanding of the nutritional status of the patients, while clinically
defining presence of malnutrition in the patients, while monitoring variations in their
nutritional status. Under most circumstances, failure to accurately identify nutritional
risks often results in under-treatment of patients that directly threatens their health
and wellbeing, and creates a negative impact on their quality of life (Lorenzo-López
et al., 2017). The nutritional assessments would generally comprise of four broad
categories that will take into account biochemical, dietary, clinical and
anthropometric parameters of the patient Mr Jungala. Owing to the fact that he has
been admitted to the hospital following a hip injury, and older adults have been
identified to be at a risk for a compromised nutritional status due to aging related
changes, and several social, psychological and cognitive factors, there is a need to
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NUR341 Assessment 2
conduct a comprehensive nutritional assessment.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
10
conduct a comprehensive nutritional assessment.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NUR341 Assessment 2
Part 2: Plan and implementation (500 words)
Normal age-related changes, Mr Jungula’s co-morbidities, acute illness and
medications may have contributed to his fall. Choose one factor and outline your
nursing actions and referrals you would execute; include rationales for same.
Falls have been identified as one of the major health problems among older
adults and several people aged more than 65 years report suffering from fall
incidents each year. Some of the major consequences of such falls are related to
fracture of hip and forearm, loss of independence, and an increase in rates of
mortality. A range of risk factors have been identified responsible for increased fall
rates among the elderly, with most common factors being cardiovascular diseases,
functional limitations or cognitive decline (Soto-Varela et al., 2015). Blood pressure
has been identified as one of the major risk factors for falls owing to the fact that
there exists a linear correlation between increase in blood pressure and falls
(Margolis et al., 2014). Thus, the fact that Mr Jungala suffered from hypertension
and under the prescribed medication regimen for the condition can be considered as
the major factor that contributed to his fall. In addition, the risk of fall also increases if
an individual takes four or more medicines simultaneously (Pajewski et al., 2016).
Outpatient evaluation of the elderly patient Mr Jungala who has suffered a fall, will
include collecting relevant information about his health history, with a special
emphasis on his medications.
This will be followed by conduction of a comprehensive physical examination
and test of postural control. The primary goal of the treatment plan would be directed
eliminating the impacts of underlying factors that might have contributed to the fall,
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
11
Part 2: Plan and implementation (500 words)
Normal age-related changes, Mr Jungula’s co-morbidities, acute illness and
medications may have contributed to his fall. Choose one factor and outline your
nursing actions and referrals you would execute; include rationales for same.
Falls have been identified as one of the major health problems among older
adults and several people aged more than 65 years report suffering from fall
incidents each year. Some of the major consequences of such falls are related to
fracture of hip and forearm, loss of independence, and an increase in rates of
mortality. A range of risk factors have been identified responsible for increased fall
rates among the elderly, with most common factors being cardiovascular diseases,
functional limitations or cognitive decline (Soto-Varela et al., 2015). Blood pressure
has been identified as one of the major risk factors for falls owing to the fact that
there exists a linear correlation between increase in blood pressure and falls
(Margolis et al., 2014). Thus, the fact that Mr Jungala suffered from hypertension
and under the prescribed medication regimen for the condition can be considered as
the major factor that contributed to his fall. In addition, the risk of fall also increases if
an individual takes four or more medicines simultaneously (Pajewski et al., 2016).
Outpatient evaluation of the elderly patient Mr Jungala who has suffered a fall, will
include collecting relevant information about his health history, with a special
emphasis on his medications.
This will be followed by conduction of a comprehensive physical examination
and test of postural control. The primary goal of the treatment plan would be directed
eliminating the impacts of underlying factors that might have contributed to the fall,
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
11
NUR341 Assessment 2
helping the patient return to baseline functional activities, and increasing safety in the
care setting and home (Hawley-Hague, Boulton, Hall, Pfeiffer & Todd, 2014). The
patient will be provided assistance in putting on a wristband sensor that has been
designed with the help of wearable technology, in order to provide reminders and
immediate alert to healthcare professionals located within close proximity to the
patient. Presence of an alarm button will immediately send information to software
operated devices that will register any kind of major movement of the patient, such
as, bending, turning, or dropping, followed by sending notifications to the registered
emergency contacts (Brabcova, Bartlova, Hajduchová & Tothova, 2015). Side
rails and grab bars will be installed on the beds and washroom in order to provide
necessary support to the patient during sitting or standing. These will allow Mr
Jungala to get hold of the rails during loss of balance, dizziness or an emergency.
Following conduction of a comprehensive and thorough review of the medications
that he had been prescribed, efforts will be taken to perform deprescribing that
commonly encompasses the process of deliberately stopping a drug or decreasing
its dosage, with the aim of improving the health of the patient (Frank & Weir, 2014).
This in turn will lower his risk of suffering from adverse side effects. Morphine has
been identified as the cornerstone for pain management owing to the analgesic
effects on the central nervous system that helps in reducing the severity of pain.
Owing to the fact that the patient report pain due to injury on the right side,
medication management would involve administration of morphine for treating pain.
Taking into consideration the fact that Mr Jungala has poor vision due to diabetic
retinopathy, efforts will be taken to form a collaboration with an ophthalmologist who
would recommend the patient to use bi-focal eyeglasses in order to deliver refractory
correction for the patient.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
12
helping the patient return to baseline functional activities, and increasing safety in the
care setting and home (Hawley-Hague, Boulton, Hall, Pfeiffer & Todd, 2014). The
patient will be provided assistance in putting on a wristband sensor that has been
designed with the help of wearable technology, in order to provide reminders and
immediate alert to healthcare professionals located within close proximity to the
patient. Presence of an alarm button will immediately send information to software
operated devices that will register any kind of major movement of the patient, such
as, bending, turning, or dropping, followed by sending notifications to the registered
emergency contacts (Brabcova, Bartlova, Hajduchová & Tothova, 2015). Side
rails and grab bars will be installed on the beds and washroom in order to provide
necessary support to the patient during sitting or standing. These will allow Mr
Jungala to get hold of the rails during loss of balance, dizziness or an emergency.
Following conduction of a comprehensive and thorough review of the medications
that he had been prescribed, efforts will be taken to perform deprescribing that
commonly encompasses the process of deliberately stopping a drug or decreasing
its dosage, with the aim of improving the health of the patient (Frank & Weir, 2014).
This in turn will lower his risk of suffering from adverse side effects. Morphine has
been identified as the cornerstone for pain management owing to the analgesic
effects on the central nervous system that helps in reducing the severity of pain.
Owing to the fact that the patient report pain due to injury on the right side,
medication management would involve administration of morphine for treating pain.
Taking into consideration the fact that Mr Jungala has poor vision due to diabetic
retinopathy, efforts will be taken to form a collaboration with an ophthalmologist who
would recommend the patient to use bi-focal eyeglasses in order to deliver refractory
correction for the patient.
Double click here to fill in this footer
Last name_student number_NUR341_ Assessment 2.
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 24
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



