NUR4111 iSAP Framework: Comprehensive Care Plan for Annie's Needs
VerifiedAdded on 2022/09/18
|7
|2418
|27
Homework Assignment
AI Summary
This assignment, focusing on the iSAP Framework (NUR4111), addresses discharge planning and care transitions for a patient named Annie. It begins by defining discharge planning and discussing its significance in relation to Annie's needs, highlighting the importance of individualized arrangements and patient satisfaction. The assignment then explores four key barriers to effective discharge planning in acute care settings, such as inadequate coordination and lack of service clarity. It summarizes the key steps for safe transfer of care, emphasizing the development of a detailed transfer plan and risk assessment. A concept map illustrates a strengths-based, person-centered care plan for Annie, considering her life story, health, environment, functions, and social wellbeing. Finally, the assignment provides evidence-based practice rationales for primary health care principles (cultural safety, health literacy, self-management, and access to services) for Annie's safe transition to community care, drawing on the National Aboriginal and Torres Strait Islander Health Plan and the National Strategic Framework for Chronic Conditions. The assignment uses several references to support the analysis and recommendations.
[Unit code].. [Student ID number]
NUR4111 iSAP Framework: Your Student Response (Part A) (1125 words +/-
10%) must address the following points:
Case Learning Outcomes
1. Define ‘discharge planning’ and discuss the importance of discharge planning and care
transition in relation to Annie’s needs. (approx. 100 words)
Please do not remove these instructions. These instructions are not included in the assessment
word count.
Type your answer here.
Answer: Discharge planning (Commonwealth of Australia., 2013) includes creating individualized
discharge arrangements for patients when they exit the hospital in order to maximize healthcare
service performance (Anderson et al., 2015) and consistency. Nurses are well qualified to assume
a significant part in hospital-to-home discharge preparation for patients, and would be acquainted
with the effects of individualized discharge preparation on patient results.
Discharge preparation is deemed a standard feature in all health care programs, and facilitates the
implementation in individualized arrangements given to a patient while entering the facility, in the
goal of optimizing patient satisfaction and minimizing needless re-hospitalizations. The primary
lingering obstacles in Annie's situation (Reilly et al., 2016) involve a weak perception of the medical
problem as well as a lack of awareness of the medical condition. Annie can experience several
obstacles on her journey home after a hospitalization. The adjustment time introduces patients to
needless hazards associated with insufficient planning before entering the facility, possibly resulting
in mistakes and damage to patients. It is also very necessary to engage patients in self-
management, which was found in order to achieve improved clinical results and improve self-
efficacy.
2. Discuss four known barriers to effective discharge planning in acute care services. (approx.
225 words)
Please do not remove these instructions. These instructions are not included in the assessment
word count.
Type your answer here.
Answer: The dynamic method of discharging patients from intensive treatment to community care
(Fortier et al., 2015) involves a multifaceted relationship between patients and all health care
professionals. Poor contact during the discharge of a patient may result in harmful effects,
readmission, and mortality after hospital. According to the severity of these issues, discharge
preparation was presented as a potential remedy. The four main themes linked to discharge
hurdles (Gibson et al., 2015) in the stated case study of Annie, were established including
adequate coordination, lack of clarification of function and lack of services and factors (Harris et al.,
2017) relevant to consistent delivery of inpatient treatment and excessive readmission to hospital.
Page 1 of 7 Assignment Number Date of submission
NUR4111 iSAP Framework: Your Student Response (Part A) (1125 words +/-
10%) must address the following points:
Case Learning Outcomes
1. Define ‘discharge planning’ and discuss the importance of discharge planning and care
transition in relation to Annie’s needs. (approx. 100 words)
Please do not remove these instructions. These instructions are not included in the assessment
word count.
Type your answer here.
Answer: Discharge planning (Commonwealth of Australia., 2013) includes creating individualized
discharge arrangements for patients when they exit the hospital in order to maximize healthcare
service performance (Anderson et al., 2015) and consistency. Nurses are well qualified to assume
a significant part in hospital-to-home discharge preparation for patients, and would be acquainted
with the effects of individualized discharge preparation on patient results.
Discharge preparation is deemed a standard feature in all health care programs, and facilitates the
implementation in individualized arrangements given to a patient while entering the facility, in the
goal of optimizing patient satisfaction and minimizing needless re-hospitalizations. The primary
lingering obstacles in Annie's situation (Reilly et al., 2016) involve a weak perception of the medical
problem as well as a lack of awareness of the medical condition. Annie can experience several
obstacles on her journey home after a hospitalization. The adjustment time introduces patients to
needless hazards associated with insufficient planning before entering the facility, possibly resulting
in mistakes and damage to patients. It is also very necessary to engage patients in self-
management, which was found in order to achieve improved clinical results and improve self-
efficacy.
2. Discuss four known barriers to effective discharge planning in acute care services. (approx.
225 words)
Please do not remove these instructions. These instructions are not included in the assessment
word count.
Type your answer here.
Answer: The dynamic method of discharging patients from intensive treatment to community care
(Fortier et al., 2015) involves a multifaceted relationship between patients and all health care
professionals. Poor contact during the discharge of a patient may result in harmful effects,
readmission, and mortality after hospital. According to the severity of these issues, discharge
preparation was presented as a potential remedy. The four main themes linked to discharge
hurdles (Gibson et al., 2015) in the stated case study of Annie, were established including
adequate coordination, lack of clarification of function and lack of services and factors (Harris et al.,
2017) relevant to consistent delivery of inpatient treatment and excessive readmission to hospital.
Page 1 of 7 Assignment Number Date of submission
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

[Unit code].. [Student ID number]
These concerns demonstrated that, in addition to cultural (McGough, Wynaden & Wright, 2018)
competence at the scientific, organizational and institutional level of care provision,
acknowledgement of disparities between Aboriginal and non-Aboriginal society, identification and
resolving gaps in influence between patient and service provider, and awareness of the effect of
tradition, political and social circumstances on health. Above all, culturally stable programs are
required to align knowledge of cultural concerns with interventions that resolve them at the
regulation, operational and program level to promote aboriginal engagement in cancer care. In fact,
many reports have found and identified the need for a consistent, well-developed follow-up
program, and it was shown that support networks for continuing treatment have necessary after
patients were discharged from the hospital to maintain continuing treatment of the highest
standard.
3. Summarise in your own words and in dot point format the key steps
for planning and implementing safe transfer of care as outlined in Transfer of care from acute
inpatient services (2014). (approx. 225 words)
Please do not remove these instructions. These instructions are not included in the assessment
word count.
Type your answer here.
Answer: Transfer of care means shifting medical liability and responsibilities to another individual or
specialist, or a mixture of practitioners, for the treatment of a patient. If a patient is released from an
emergency situation, they can pass their continuing treatment to another individual or team. The
aim of care transition is to create a secure, smooth path which will ensure quality of patient care.
Medical transition is a component of the discharge phase. Developing an individual transfer care of
plan includes(Molony et al., 2018):
Include an approximate date of care transition (or discharge) and methods for achieving
the expected date of care transition (such as contact arrangements for service agencies,
families and/or caregivers)
Include details on transfers to hospital and/or community facilities, as well as specifics on
the travel plans for both the patient from the hospital to their place of care
Include details on the medications of the patient and how they should be transported, form
an important part of the clinical notes of the patient when they are hospitalized and revised
as needed
Implementation of the transfer care plan includes the following key steps:
The treatment plan needs to be established and enforced in collaboration with patients,
their relatives and/or caregivers and the individual, their relatives and/or caregivers can
consider certain facets of the care plan transition.
Collection of a treatment checklist (or equivalent) for all patients will be done prior to
discharge or transition of treatment. The transmission of confidential details would adhere
to the standards of privacy set out in the Details Protection Act 2000 and the Health
Page 2 of 7 Assignment Number Date of submission
These concerns demonstrated that, in addition to cultural (McGough, Wynaden & Wright, 2018)
competence at the scientific, organizational and institutional level of care provision,
acknowledgement of disparities between Aboriginal and non-Aboriginal society, identification and
resolving gaps in influence between patient and service provider, and awareness of the effect of
tradition, political and social circumstances on health. Above all, culturally stable programs are
required to align knowledge of cultural concerns with interventions that resolve them at the
regulation, operational and program level to promote aboriginal engagement in cancer care. In fact,
many reports have found and identified the need for a consistent, well-developed follow-up
program, and it was shown that support networks for continuing treatment have necessary after
patients were discharged from the hospital to maintain continuing treatment of the highest
standard.
3. Summarise in your own words and in dot point format the key steps
for planning and implementing safe transfer of care as outlined in Transfer of care from acute
inpatient services (2014). (approx. 225 words)
Please do not remove these instructions. These instructions are not included in the assessment
word count.
Type your answer here.
Answer: Transfer of care means shifting medical liability and responsibilities to another individual or
specialist, or a mixture of practitioners, for the treatment of a patient. If a patient is released from an
emergency situation, they can pass their continuing treatment to another individual or team. The
aim of care transition is to create a secure, smooth path which will ensure quality of patient care.
Medical transition is a component of the discharge phase. Developing an individual transfer care of
plan includes(Molony et al., 2018):
Include an approximate date of care transition (or discharge) and methods for achieving
the expected date of care transition (such as contact arrangements for service agencies,
families and/or caregivers)
Include details on transfers to hospital and/or community facilities, as well as specifics on
the travel plans for both the patient from the hospital to their place of care
Include details on the medications of the patient and how they should be transported, form
an important part of the clinical notes of the patient when they are hospitalized and revised
as needed
Implementation of the transfer care plan includes the following key steps:
The treatment plan needs to be established and enforced in collaboration with patients,
their relatives and/or caregivers and the individual, their relatives and/or caregivers can
consider certain facets of the care plan transition.
Collection of a treatment checklist (or equivalent) for all patients will be done prior to
discharge or transition of treatment. The transmission of confidential details would adhere
to the standards of privacy set out in the Details Protection Act 2000 and the Health
Page 2 of 7 Assignment Number Date of submission
[Unit code].. [Student ID number]
Records Act 2001. Patients such as Annie, who are at higher risk of readmission, should
be recognized as stated in the case study, and interventions adopted to reduce the risk of
readmission.
After conclusion of the risk evaluation, referrals need to be provided to relevant health care
professionals and/or neighborhood support programs. After release from a patient's
residence, appropriate neighborhood social resources need to be engaged. Additionally, it
is necessary to preserve consistency of prescription treatment.
4. Construct a concept map that holistically shows how you have drawn on Annie’s life story, health, environment, functions
and social wellbeing, and demonstrates a strengths-based person-centred care plan to improving her situation. (approx.
125 words)
Import (copy and paste) your concept map into your Student Response here.
Page 3 of 7 Assignment Number Date of submission
Records Act 2001. Patients such as Annie, who are at higher risk of readmission, should
be recognized as stated in the case study, and interventions adopted to reduce the risk of
readmission.
After conclusion of the risk evaluation, referrals need to be provided to relevant health care
professionals and/or neighborhood support programs. After release from a patient's
residence, appropriate neighborhood social resources need to be engaged. Additionally, it
is necessary to preserve consistency of prescription treatment.
4. Construct a concept map that holistically shows how you have drawn on Annie’s life story, health, environment, functions
and social wellbeing, and demonstrates a strengths-based person-centred care plan to improving her situation. (approx.
125 words)
Import (copy and paste) your concept map into your Student Response here.
Page 3 of 7 Assignment Number Date of submission
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
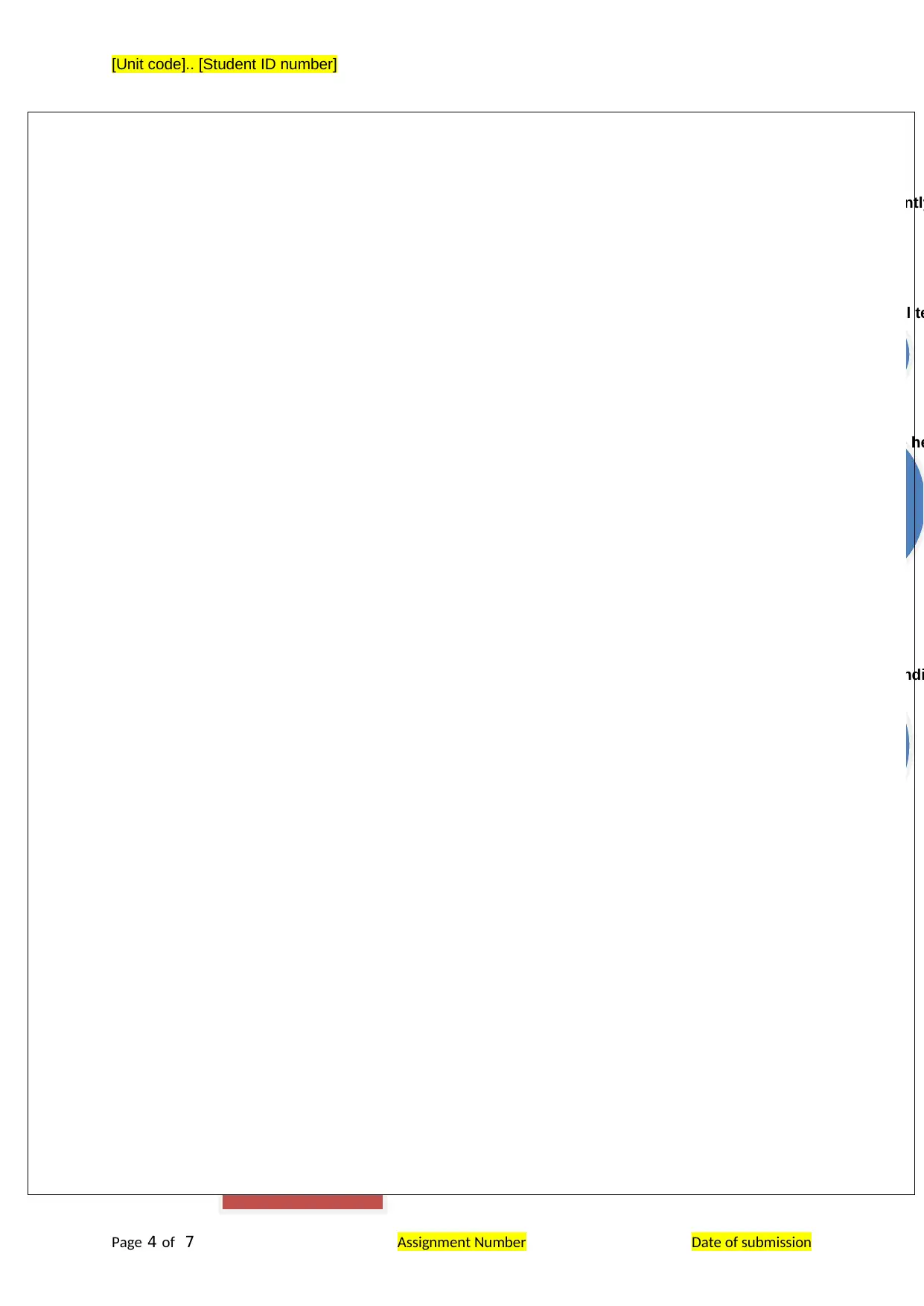
Annie
Life Factors
& Environment
Aboriginal Community Member
Hypertension Lives alone and independently
Worked as a primary school te
Health Factors
Type II diabetes
Geriatric age group
Chronic Kidney Disease
Social wellbeing
Takes part in local community events for indi
Helps daughter to raise he
Helps her son to take care of his daughter Lily
Patient centered & Therapeutic Approach (Reilly et al., 2016)
Emphasizes Acknowledgement
Practice emapathy
&
coommunication
Build a patient-
nurse entrusting
relationship
Patient education &
self
acknowledgement
Safe patient
assessment &
promote better
quality of life
[Unit code].. [Student ID number]
Page 4 of 7 Assignment Number Date of submission
Life Factors
& Environment
Aboriginal Community Member
Hypertension Lives alone and independently
Worked as a primary school te
Health Factors
Type II diabetes
Geriatric age group
Chronic Kidney Disease
Social wellbeing
Takes part in local community events for indi
Helps daughter to raise he
Helps her son to take care of his daughter Lily
Patient centered & Therapeutic Approach (Reilly et al., 2016)
Emphasizes Acknowledgement
Practice emapathy
&
coommunication
Build a patient-
nurse entrusting
relationship
Patient education &
self
acknowledgement
Safe patient
assessment &
promote better
quality of life
[Unit code].. [Student ID number]
Page 4 of 7 Assignment Number Date of submission
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
[Unit code].. [Student ID number]
5. Provide an EBP rationale for the following PHC principles for Annie’s safe transition to community care. The rationale
should include strategies from the National Aboriginal and Torres Strait Islander Health Plan (2013–2023) and
the National Strategic Framework for Chronic Conditions, 2017. (approx. total 450 words (approx. 158 words for each PHC
principle)
o cultural safety
o health literacy and self-management (for practical reasons these two principles have been combined)
o access to services
Type your answer here.
Cultural safety: Community protection definition includes supporting both the health care provider and the customer.
The recipient of treatment determines the determinants of 'free' treatment. Cultural protection (McGough, Wynaden &
Wright, 2018) was originally a reaction to indigenous Australian's poor health status but has subsequently grown to
encompass a large variety of cultural determinants. Importance is imposed on the definition and assessment of one's
own convictions and principles, and the appreciation of their capacity for influence on others. This definition
acknowledges the power indices implicit in any partnership, and the capacity for difference and imbalance in any
relationship. Healthcare practitioner's recognition that enforcing one's own cultural values that disadvantage the
healthcare recipient is central to providing culturally secure care. Implement the Regional Anti-Racism Policy 2010-
2020 to encourage Aboriginal and Torres Strait Islander patients to feel confident recognizing and encouraging best
practices and new strategies that are driven by study, testing and assessment programs will help ensure cultural
health at its finest.
Health literacy and self-management (for practical reasons these two principles have been combined: Improving health
literacy is important if citizens want to be interested in their own health care. Decisions and actions made to maintain
safety and well-being are initiated by individuals themselves on a regular basis: good self-management is a core
component of successful chronic illnesses treatment. Health literacy (Harris et al., 2017) is essential to accountability
and impacts a person's capacity to make sound health and health care choices and to take effective action. Effective
involvement is more than just effective control of oneself. Strong participation in the decision-making process is
especially essential for individuals with specific medical conditions and reduced potential for self-management, so that
they can have greater power over their wellbeing in partnerships with health practitioners.
Access to services: Throughout the health system, transfer points sometimes serve as a obstacle to continued
treatment. Transitional health care points exist during the lifetime, and bet between health care professionals and
programs such as urgent primary care and elderly treatment. Strategies (Bing-Jonsson, Foss & Bjørk, 2016)
addressing quality in treatment and knowledge retention to ensure people such as Annie have consistent and prompt
access to the wide spectrum in resources they need across the health systems. Improving people's exposure to
accessible health knowledge and their abilities to efficiently utilize it would boost patient health awareness and help
patients understand the health system easier.
Page 5 of 7 Assignment Number Date of submission
5. Provide an EBP rationale for the following PHC principles for Annie’s safe transition to community care. The rationale
should include strategies from the National Aboriginal and Torres Strait Islander Health Plan (2013–2023) and
the National Strategic Framework for Chronic Conditions, 2017. (approx. total 450 words (approx. 158 words for each PHC
principle)
o cultural safety
o health literacy and self-management (for practical reasons these two principles have been combined)
o access to services
Type your answer here.
Cultural safety: Community protection definition includes supporting both the health care provider and the customer.
The recipient of treatment determines the determinants of 'free' treatment. Cultural protection (McGough, Wynaden &
Wright, 2018) was originally a reaction to indigenous Australian's poor health status but has subsequently grown to
encompass a large variety of cultural determinants. Importance is imposed on the definition and assessment of one's
own convictions and principles, and the appreciation of their capacity for influence on others. This definition
acknowledges the power indices implicit in any partnership, and the capacity for difference and imbalance in any
relationship. Healthcare practitioner's recognition that enforcing one's own cultural values that disadvantage the
healthcare recipient is central to providing culturally secure care. Implement the Regional Anti-Racism Policy 2010-
2020 to encourage Aboriginal and Torres Strait Islander patients to feel confident recognizing and encouraging best
practices and new strategies that are driven by study, testing and assessment programs will help ensure cultural
health at its finest.
Health literacy and self-management (for practical reasons these two principles have been combined: Improving health
literacy is important if citizens want to be interested in their own health care. Decisions and actions made to maintain
safety and well-being are initiated by individuals themselves on a regular basis: good self-management is a core
component of successful chronic illnesses treatment. Health literacy (Harris et al., 2017) is essential to accountability
and impacts a person's capacity to make sound health and health care choices and to take effective action. Effective
involvement is more than just effective control of oneself. Strong participation in the decision-making process is
especially essential for individuals with specific medical conditions and reduced potential for self-management, so that
they can have greater power over their wellbeing in partnerships with health practitioners.
Access to services: Throughout the health system, transfer points sometimes serve as a obstacle to continued
treatment. Transitional health care points exist during the lifetime, and bet between health care professionals and
programs such as urgent primary care and elderly treatment. Strategies (Bing-Jonsson, Foss & Bjørk, 2016)
addressing quality in treatment and knowledge retention to ensure people such as Annie have consistent and prompt
access to the wide spectrum in resources they need across the health systems. Improving people's exposure to
accessible health knowledge and their abilities to efficiently utilize it would boost patient health awareness and help
patients understand the health system easier.
Page 5 of 7 Assignment Number Date of submission
[Unit code].. [Student ID number]
The resources below are starting
references for the case
Starting references are provided below to assist
you with developing your student response. Please note, however, that
you are expected to find additional references to inform your response.
Anderson, R. A., Bailey Jr, D. E., Wu, B., Corazzini, K., McConnell, E. S., Thygeson, N. M.,
& Docherty, S. L. (2015). Adaptive leadership framework for chronic illness:
framing a research agenda for transforming care delivery. ANS. Advances in
nursing science, 38(2), 83. doi.org/10.1186/s12992-017-0295-8
Australian Health Ministers' Advisory Council. (2017). National Strategic Framework for
Chronic Conditions. Retrieved
from https://www.health.gov.au/internet/main/publishing.nsf/Content/
A0F1B6D61796CF3DCA257E4D001AD4C4/$File/National%20Strategic
%20Framework%20for%20Chronic%20Conditions.pdf
Bing-Jonsson, P. C., Foss, C., & Bjørk, I. T. (2016). The competence gap in community care:
Imbalance between expected and actual nursing staff competence. Nordic
Journal of Nursing Research, 36(1), 27-37.
doi.org/10.1177/0107408315601814
Commonwealth of Australia. (2013). National Aboriginal and Torres Strait Islander Health
Plan 2013-2023. Retrieved
from http://www.health.gov.au/internet/main/publishing.nsf/content/
B92E980680486C3BCA257BF0001BAF01/$File/health-plan.pdf
Fortier, M. E., Fountain, D. M., Vargas, M., Heelan-Fancher, L., Perron, T., Hinic, K., &
Swan, B. A. (2015). Health care in the community: Developing
Page 6 of 7 Assignment Number Date of submission
The resources below are starting
references for the case
Starting references are provided below to assist
you with developing your student response. Please note, however, that
you are expected to find additional references to inform your response.
Anderson, R. A., Bailey Jr, D. E., Wu, B., Corazzini, K., McConnell, E. S., Thygeson, N. M.,
& Docherty, S. L. (2015). Adaptive leadership framework for chronic illness:
framing a research agenda for transforming care delivery. ANS. Advances in
nursing science, 38(2), 83. doi.org/10.1186/s12992-017-0295-8
Australian Health Ministers' Advisory Council. (2017). National Strategic Framework for
Chronic Conditions. Retrieved
from https://www.health.gov.au/internet/main/publishing.nsf/Content/
A0F1B6D61796CF3DCA257E4D001AD4C4/$File/National%20Strategic
%20Framework%20for%20Chronic%20Conditions.pdf
Bing-Jonsson, P. C., Foss, C., & Bjørk, I. T. (2016). The competence gap in community care:
Imbalance between expected and actual nursing staff competence. Nordic
Journal of Nursing Research, 36(1), 27-37.
doi.org/10.1177/0107408315601814
Commonwealth of Australia. (2013). National Aboriginal and Torres Strait Islander Health
Plan 2013-2023. Retrieved
from http://www.health.gov.au/internet/main/publishing.nsf/content/
B92E980680486C3BCA257BF0001BAF01/$File/health-plan.pdf
Fortier, M. E., Fountain, D. M., Vargas, M., Heelan-Fancher, L., Perron, T., Hinic, K., &
Swan, B. A. (2015). Health care in the community: Developing
Page 6 of 7 Assignment Number Date of submission
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
[Unit code].. [Student ID number]
academic/practice partnerships for care coordination and managing
transitions. Nursing Economics, 33(3), 167.
Gibson, O., Lisy, K., Davy, C., Aromataris, E., Kite, E., Lockwood, C., ... & Brown, A. (2015).
Enablers and barriers to the implementation of primary health care
interventions for Indigenous people with chronic diseases: a systematic
review. Implementation Science, 10(1), 71. doi.org/10.1186/s13012-015-
0261-x
Harris, M., Taggart, J., Williams, A., Dennis, S., Newall, A., Shortus, T., ... & Zwar, N. (2017).
Effective determinants for supporting lifestyle health literacy and self
management skills in primary care. https://openresearch-
repository.anu.edu.au/bitstream/1885/119204/3/appendices_17386.pdf
Heiman, H. J., & Artiga, S. (2015). Beyond health care: the role of social determinants in
promoting health and health equity. Health, 20(10), 1-10.
https://www.issuelab.org/resources/22899/22899.pdf
McGough, S., Wynaden, D., & Wright, M. (2018). Experience of providing cultural safety in
mental health to Aboriginal patients: A grounded theory study. International
journal of mental health nursing, 27(1), 204-213. doi.org/10.1111/inm.12310
Molony, S. L., Kolanowski, A., Van Haitsma, K., & Rooney, K. E. (2018). Person-centered
assessment and care planning. The Gerontologist, 58(suppl_1), S32-S47.
doi.org/10.1093/geront/gnx173
Reilly, R., Evans, K., Gomersall, J., Gorham, G., Peters, M. D., Warren, S., ... & Brown, A.
(2016). Effectiveness, cost effectiveness, acceptability and implementation
barriers/enablers of chronic kidney disease management programs for
Indigenous people in Australia, New Zealand and Canada: a systematic
review of mixed evidence. BMC health services research, 16(1), 119.
doi.org/10.1186/s12913-016-1363-0
Rix, E. F., Barclay, L., Stirling, J., Tong, A., & Wilson, S. (2015). The perspectives of A
boriginal patients and their health care providers on improving the quality of
hemodialysis services: A qualitative study. Hemodialysis International, 19(1),
80-89. doi.org/10.1111/hdi.12201
Page 7 of 7 Assignment Number Date of submission
academic/practice partnerships for care coordination and managing
transitions. Nursing Economics, 33(3), 167.
Gibson, O., Lisy, K., Davy, C., Aromataris, E., Kite, E., Lockwood, C., ... & Brown, A. (2015).
Enablers and barriers to the implementation of primary health care
interventions for Indigenous people with chronic diseases: a systematic
review. Implementation Science, 10(1), 71. doi.org/10.1186/s13012-015-
0261-x
Harris, M., Taggart, J., Williams, A., Dennis, S., Newall, A., Shortus, T., ... & Zwar, N. (2017).
Effective determinants for supporting lifestyle health literacy and self
management skills in primary care. https://openresearch-
repository.anu.edu.au/bitstream/1885/119204/3/appendices_17386.pdf
Heiman, H. J., & Artiga, S. (2015). Beyond health care: the role of social determinants in
promoting health and health equity. Health, 20(10), 1-10.
https://www.issuelab.org/resources/22899/22899.pdf
McGough, S., Wynaden, D., & Wright, M. (2018). Experience of providing cultural safety in
mental health to Aboriginal patients: A grounded theory study. International
journal of mental health nursing, 27(1), 204-213. doi.org/10.1111/inm.12310
Molony, S. L., Kolanowski, A., Van Haitsma, K., & Rooney, K. E. (2018). Person-centered
assessment and care planning. The Gerontologist, 58(suppl_1), S32-S47.
doi.org/10.1093/geront/gnx173
Reilly, R., Evans, K., Gomersall, J., Gorham, G., Peters, M. D., Warren, S., ... & Brown, A.
(2016). Effectiveness, cost effectiveness, acceptability and implementation
barriers/enablers of chronic kidney disease management programs for
Indigenous people in Australia, New Zealand and Canada: a systematic
review of mixed evidence. BMC health services research, 16(1), 119.
doi.org/10.1186/s12913-016-1363-0
Rix, E. F., Barclay, L., Stirling, J., Tong, A., & Wilson, S. (2015). The perspectives of A
boriginal patients and their health care providers on improving the quality of
hemodialysis services: A qualitative study. Hemodialysis International, 19(1),
80-89. doi.org/10.1111/hdi.12201
Page 7 of 7 Assignment Number Date of submission
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





