University Nursing Case Study: Patient Assessment and Intervention
VerifiedAdded on 2022/08/14
|11
|2938
|32
Case Study
AI Summary
This case study analyzes the presentation of a 58-year-old patient admitted with flu-like symptoms, cough, and joint pain, presenting a detailed account of the patient's condition, including vital signs (RR, SpO2, BP, HR, T) and medical history. The assignment follows the A-E primary assessment framework, highlighting abnormal findings like high respiratory and heart rates, hypotension, and fever, along with normal ranges. It identifies critical problems such as respiratory acidosis, metabolic alkalosis, and the need for immediate interventions. The study explores interventions like non-invasive positive pressure ventilation, intravenous fluids, and fever management, providing rationales based on blood gas analysis and patient history. The patient, a competitive cyclist, shows symptoms of respiratory distress, and the study emphasizes the need for continuous monitoring and careful medication management, particularly avoiding paracetamol due to potential complications. The case study underscores the importance of evidence-based nursing practices in critical care settings.

Running Head: Nursing Case Study
Case Study Analysis
Name of the Student
Name of the University
Authors Note
Case Study Analysis
Name of the Student
Name of the University
Authors Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Patient presentation
The patient for this case study is 58 years old and admitted to the hospital with severe
flu-like symptoms and less appetite. Jeff, the patient produced cough (with green colouration)
with aches and pains in different joints. The nurses checked his vital signs for assessing
whether he has any pain or aching symptoms. The patient was admitted to the hospital at 5.30
AM. The patient was assessed, and the evaluated vital signs are RR 26, SpO2 94% on RA,
BP 95/55 mmHg, HR 100 and T 38.5 . He had no record of surgery for the premedical℃
history. He was on the low-fat diet and did not have the record of flu vaccination. Jeff was
admitted to the acute bed care in the red area of ICU. His words were broken, and his GCS or
Glasgow coma scale reported a normal condition of the patient. His weight is 62 kg and
height is 183 cm tall. The BMI of the patient is 18.5. He had a high fever so that the
temperature was 38.5 C. Jeff was a competitive cyclist and was trained himself for the racing
the cycling.
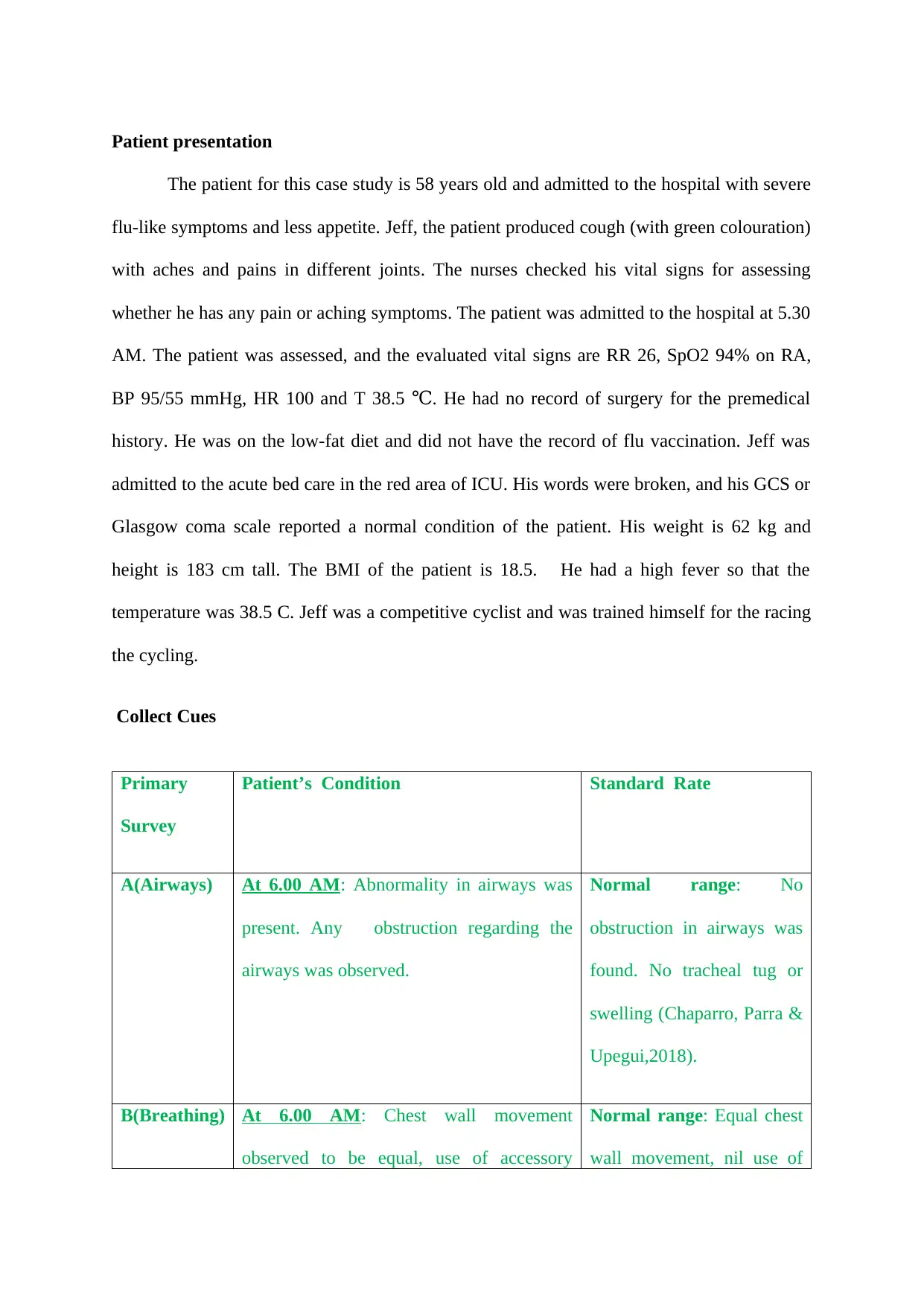
Collect Cues
Primary
Survey
Patient’s Condition Standard Rate
A(Airways) At 6.00 AM: Abnormality in airways was
present. Any obstruction regarding the
airways was observed.
Normal range: No
obstruction in airways was
found. No tracheal tug or
swelling (Chaparro, Parra &
Upegui,2018).
B(Breathing) At 6.00 AM: Chest wall movement
observed to be equal, use of accessory
Normal range: Equal chest
wall movement, nil use of
The patient for this case study is 58 years old and admitted to the hospital with severe
flu-like symptoms and less appetite. Jeff, the patient produced cough (with green colouration)
with aches and pains in different joints. The nurses checked his vital signs for assessing
whether he has any pain or aching symptoms. The patient was admitted to the hospital at 5.30
AM. The patient was assessed, and the evaluated vital signs are RR 26, SpO2 94% on RA,
BP 95/55 mmHg, HR 100 and T 38.5 . He had no record of surgery for the premedical℃
history. He was on the low-fat diet and did not have the record of flu vaccination. Jeff was
admitted to the acute bed care in the red area of ICU. His words were broken, and his GCS or
Glasgow coma scale reported a normal condition of the patient. His weight is 62 kg and
height is 183 cm tall. The BMI of the patient is 18.5. He had a high fever so that the
temperature was 38.5 C. Jeff was a competitive cyclist and was trained himself for the racing
the cycling.
Collect Cues
Primary
Survey
Patient’s Condition Standard Rate
A(Airways) At 6.00 AM: Abnormality in airways was
present. Any obstruction regarding the
airways was observed.
Normal range: No
obstruction in airways was
found. No tracheal tug or
swelling (Chaparro, Parra &
Upegui,2018).
B(Breathing) At 6.00 AM: Chest wall movement
observed to be equal, use of accessory
Normal range: Equal chest
wall movement, nil use of
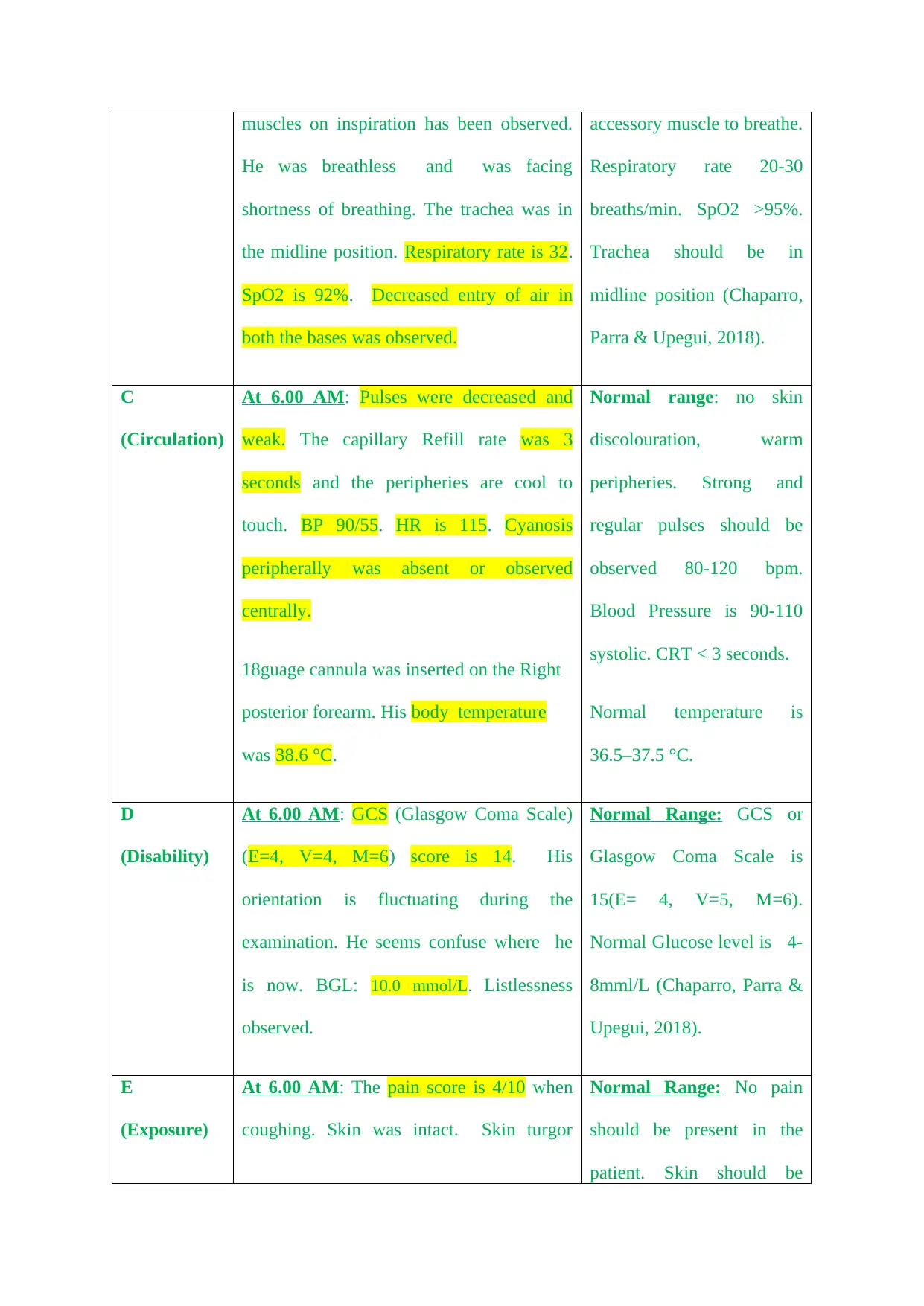
muscles on inspiration has been observed.
He was breathless and was facing
shortness of breathing. The trachea was in
the midline position. Respiratory rate is 32.
SpO2 is 92%. Decreased entry of air in
both the bases was observed.
accessory muscle to breathe.
Respiratory rate 20-30
breaths/min. SpO2 >95%.
Trachea should be in
midline position (Chaparro,
Parra & Upegui, 2018).
C
(Circulation)
At 6.00 AM: Pulses were decreased and
weak. The capillary Refill rate was 3
seconds and the peripheries are cool to
touch. BP 90/55. HR is 115. Cyanosis
peripherally was absent or observed
centrally.
18guage cannula was inserted on the Right
posterior forearm. His body temperature
was 38.6 °C.
Normal range: no skin
discolouration, warm
peripheries. Strong and
regular pulses should be
observed 80-120 bpm.
Blood Pressure is 90-110
systolic. CRT < 3 seconds.
Normal temperature is
36.5–37.5 °C.
D
(Disability)
At 6.00 AM: GCS (Glasgow Coma Scale)
(E=4, V=4, M=6) score is 14. His
orientation is fluctuating during the
examination. He seems confuse where he
is now. BGL: 10.0 mmol/L. Listlessness
observed.
Normal Range: GCS or
Glasgow Coma Scale is
15(E= 4, V=5, M=6).
Normal Glucose level is 4-
8mml/L (Chaparro, Parra &
Upegui, 2018).
E
(Exposure)
At 6.00 AM: The pain score is 4/10 when
coughing. Skin was intact. Skin turgor
Normal Range: No pain
should be present in the
patient. Skin should be
He was breathless and was facing
shortness of breathing. The trachea was in
the midline position. Respiratory rate is 32.
SpO2 is 92%. Decreased entry of air in
both the bases was observed.
accessory muscle to breathe.
Respiratory rate 20-30
breaths/min. SpO2 >95%.
Trachea should be in
midline position (Chaparro,
Parra & Upegui, 2018).
C
(Circulation)
At 6.00 AM: Pulses were decreased and
weak. The capillary Refill rate was 3
seconds and the peripheries are cool to
touch. BP 90/55. HR is 115. Cyanosis
peripherally was absent or observed
centrally.
18guage cannula was inserted on the Right
posterior forearm. His body temperature
was 38.6 °C.
Normal range: no skin
discolouration, warm
peripheries. Strong and
regular pulses should be
observed 80-120 bpm.
Blood Pressure is 90-110
systolic. CRT < 3 seconds.
Normal temperature is
36.5–37.5 °C.
D
(Disability)
At 6.00 AM: GCS (Glasgow Coma Scale)
(E=4, V=4, M=6) score is 14. His
orientation is fluctuating during the
examination. He seems confuse where he
is now. BGL: 10.0 mmol/L. Listlessness
observed.
Normal Range: GCS or
Glasgow Coma Scale is
15(E= 4, V=5, M=6).
Normal Glucose level is 4-
8mml/L (Chaparro, Parra &
Upegui, 2018).
E
(Exposure)
At 6.00 AM: The pain score is 4/10 when
coughing. Skin was intact. Skin turgor
Normal Range: No pain
should be present in the
patient. Skin should be
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
decreased. His orientation was disrupted. intact.
Process Information
The patient had fever with a temperature of 38.3 to 38.9 C. The condition signifies
that the patient was having fever which is mild to severe level fever. The patient was
admitted to the Emergency Department. After half an hour when the nurses checked his
temperature, they found that the temperature was not reduced as it was 38.6 C which is also
higher than normal range which is 36.5–37.5 °C.
The respiratory rate of the patient was recorded as 26 initially. After he was taken to
the red area of the ED, the Respiratory Rate was recorded as 32. Normal respiratory rate is
within 12 to 20 breath per minute. Therefore it can be said that the patient was suffering from
a high respiratory rate. Jeff was suffering from the shortness of breath but the oxygen
saturation rate is normal for the patient. His heart rate was 100 when he was admitted to the
hospital and later it was recorded as 115. The results showed that the patient had tachycardia
and shortness of breath or breathlessness. As the patient had a history of high cholesterol
level, the patient can be suffered from hypertension. The respiratory rate was higher than the
normal range so the patient can suffer from different type of disorders such as lung disease,
COPD and heart disease. The tachycardia was observed after he was taken to the red area of
the ED. On the contrary heart rate and respiratory rate can be increased due to cough and
fever. During fever, respiratory rate and heart rate are increased in a rate of 10 bpm with an
elevation of 1 C.
Process Information
The patient had fever with a temperature of 38.3 to 38.9 C. The condition signifies
that the patient was having fever which is mild to severe level fever. The patient was
admitted to the Emergency Department. After half an hour when the nurses checked his
temperature, they found that the temperature was not reduced as it was 38.6 C which is also
higher than normal range which is 36.5–37.5 °C.
The respiratory rate of the patient was recorded as 26 initially. After he was taken to
the red area of the ED, the Respiratory Rate was recorded as 32. Normal respiratory rate is
within 12 to 20 breath per minute. Therefore it can be said that the patient was suffering from
a high respiratory rate. Jeff was suffering from the shortness of breath but the oxygen
saturation rate is normal for the patient. His heart rate was 100 when he was admitted to the
hospital and later it was recorded as 115. The results showed that the patient had tachycardia
and shortness of breath or breathlessness. As the patient had a history of high cholesterol
level, the patient can be suffered from hypertension. The respiratory rate was higher than the
normal range so the patient can suffer from different type of disorders such as lung disease,
COPD and heart disease. The tachycardia was observed after he was taken to the red area of
the ED. On the contrary heart rate and respiratory rate can be increased due to cough and
fever. During fever, respiratory rate and heart rate are increased in a rate of 10 bpm with an
elevation of 1 C.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
However, the pulses were regular and weak. Both the systolic and diastolic pressure
were low in nature as per the record. In the red area of ED, his BP was checked and it was
90/55mmHg. During the assessment of blood circulation, it was observed that the refilling
time of capillary was 3 seconds, which is slower than the normal. Therefore, the capillaries
are not refilled in a normal range as the patient had hypotension. The patient was an avid
competitive cyclist and trained with the practice of racing cycles with the speed of 80-100 of
KM. The abnormalities regarding respiration and heart rate were quite surprising for the
patient. Tachycardia can be happened due to the higher or faster heart rate. The person was
suffered from cold and cough with fever. Therefore it can be said that the patient’s respiratory
rate is high due to the fever and cough. Fever can also be a cause of the shortness of
breathing.
The electrolytes were not out of the normal range, but the record shows that both the
electrolytes are present in the blood in a borderline of the higher range (Lo & Liu, 2018).
GCS or Glasgow Coma Scale shows that the verbal ability of the patient is not showing any
positive result (Chandrasekhar, Rahim, Quraishi, Theja, & Kiran, 2017). The pain score is
4/10 when coughing, and that shows less severity.
The patient’s history signifies that he practised high level of strenuous exercise in
terms of cycling. Heart failure, severe infection, shock and lower flow of blood can cause
high-level lactate accumulation. The level of haemoglobin is less in number, which can be
another cause of less oxygen circulation or low oxygen saturation rate in the
blood(Zimmerman et al., 2017). The patient also shows that the tendency of hyperglycaemia
as the glucose level in the blood of the patient was 10 mmol. The high level of glucose can be
the cause of higher range of BE and high lactate level.
were low in nature as per the record. In the red area of ED, his BP was checked and it was
90/55mmHg. During the assessment of blood circulation, it was observed that the refilling
time of capillary was 3 seconds, which is slower than the normal. Therefore, the capillaries
are not refilled in a normal range as the patient had hypotension. The patient was an avid
competitive cyclist and trained with the practice of racing cycles with the speed of 80-100 of
KM. The abnormalities regarding respiration and heart rate were quite surprising for the
patient. Tachycardia can be happened due to the higher or faster heart rate. The person was
suffered from cold and cough with fever. Therefore it can be said that the patient’s respiratory
rate is high due to the fever and cough. Fever can also be a cause of the shortness of
breathing.
The electrolytes were not out of the normal range, but the record shows that both the
electrolytes are present in the blood in a borderline of the higher range (Lo & Liu, 2018).
GCS or Glasgow Coma Scale shows that the verbal ability of the patient is not showing any
positive result (Chandrasekhar, Rahim, Quraishi, Theja, & Kiran, 2017). The pain score is
4/10 when coughing, and that shows less severity.
The patient’s history signifies that he practised high level of strenuous exercise in
terms of cycling. Heart failure, severe infection, shock and lower flow of blood can cause
high-level lactate accumulation. The level of haemoglobin is less in number, which can be
another cause of less oxygen circulation or low oxygen saturation rate in the
blood(Zimmerman et al., 2017). The patient also shows that the tendency of hyperglycaemia
as the glucose level in the blood of the patient was 10 mmol. The high level of glucose can be
the cause of higher range of BE and high lactate level.
Identify Critical Problems
In this patient, three significant problems have been identified, such as and high
respiratory rate and heart rate with hypotension, fever with the infection and imbalance of the
blood component and pain. The patient was also suffered from cold and had fever also. The
patient also had a severe chest soreness, and he also reported the appearance of green
colouration in cough. Infection can be detected in the patient with arthralgia. The patient
might suffer from respiratory infection as he had fever along with chest soreness and
shortness of breathing. The respiratory rate might be induced by the consequences of the high
heart rate and respiratory rate.
The respiratory disorders should be treated primarily, for example, respiratory
acidosis and the fever with metabolic alkalosis. The vital signs should be checked with the
help of proper respiration assessment techniques by nursing professionals. To analyse any
condition of the body, especially respiratory system, the physician should check the
appearance, posture and breathing effort. Respiration rate, quality and pattern should be
checked to assess the condition of the patient. Nurses should measure the saturation rate of
oxygen and inspect anterior and posterior thorax with the lateral thorax to check the
palpation. Percussion should be used for assessing the tone of anterior, posterior and lateral
thorax and palpation of trachea helps in assessing the position of the trachea. The nurses
should check the respiratory sound with the stethoscope as the person was suffered from
shortness of breath. The blood reports and other assessment reports signify that the patient is
suffering from respiratory acidosis and metabolic alkalosis. As the symptoms of these two
conditions, the patient shows lower pH level and hypotension with the hyperkalaemia or
metabolic alkalosis (Farfara, Melamed & Sadoun, 2018). The history of this patient shows
that the patient had been taken Panadol for reducing fever or body temperature. The overdose
In this patient, three significant problems have been identified, such as and high
respiratory rate and heart rate with hypotension, fever with the infection and imbalance of the
blood component and pain. The patient was also suffered from cold and had fever also. The
patient also had a severe chest soreness, and he also reported the appearance of green
colouration in cough. Infection can be detected in the patient with arthralgia. The patient
might suffer from respiratory infection as he had fever along with chest soreness and
shortness of breathing. The respiratory rate might be induced by the consequences of the high
heart rate and respiratory rate.
The respiratory disorders should be treated primarily, for example, respiratory
acidosis and the fever with metabolic alkalosis. The vital signs should be checked with the
help of proper respiration assessment techniques by nursing professionals. To analyse any
condition of the body, especially respiratory system, the physician should check the
appearance, posture and breathing effort. Respiration rate, quality and pattern should be
checked to assess the condition of the patient. Nurses should measure the saturation rate of
oxygen and inspect anterior and posterior thorax with the lateral thorax to check the
palpation. Percussion should be used for assessing the tone of anterior, posterior and lateral
thorax and palpation of trachea helps in assessing the position of the trachea. The nurses
should check the respiratory sound with the stethoscope as the person was suffered from
shortness of breath. The blood reports and other assessment reports signify that the patient is
suffering from respiratory acidosis and metabolic alkalosis. As the symptoms of these two
conditions, the patient shows lower pH level and hypotension with the hyperkalaemia or
metabolic alkalosis (Farfara, Melamed & Sadoun, 2018). The history of this patient shows
that the patient had been taken Panadol for reducing fever or body temperature. The overdose
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
of paracetamol can cause hyperkalaemia in the body which can be resulted as metabolic
alkalosis.
Jeff showed the symptoms of hypotension which is one of the most common outcome
of respiratory acidosis and metabolic alkalosis in the body of the patient. He is also suffered
from high cholesterol level, which can lead to hypotension and slow blood flow in the
capillary (Centi et al., 2019).
He was admitted to the hospital due to fever and associated problems such as
shortness of breath and chest congestion.
The above discussed three conditions are the major problems which should be taken
care of immediately.
Interventions
For the treatment of respiratory acidosis, doctors should give thee interventions which
will decrease breathing problems. Physicians must check the arterial blood gas levels with the
levels of PCO2 and PO2. The saturation level of oxygen and carbon dioxide should be checked.
However, the venous blood gas was examined so the arterial blood gas level should be checked to
compare both the conditions of the blood level. By comparing the results of the blood gases help
the physician to suggest different medications such as corticosteroids and bronchodilator to the
patient. As the intervention of the respiratory acidosis, non-invasive positive pressure ventilation
should be suggested to the patient. The supportive devices in different therapies such as
continuous positive airway pressure (CPAP) and bi-level therapy or (BiPAP) therapy
(Wannemuehler, Hubbell & Nelson, 2016). If the patient’s condition deteriorates more, the
intubation procedure can be suggested.
The hypotension must be decreased by administering saline to the body of the patient by
IV fluids, but extra sodium and potassium level should be checked because the elevated level of
alkalosis.
Jeff showed the symptoms of hypotension which is one of the most common outcome
of respiratory acidosis and metabolic alkalosis in the body of the patient. He is also suffered
from high cholesterol level, which can lead to hypotension and slow blood flow in the
capillary (Centi et al., 2019).
He was admitted to the hospital due to fever and associated problems such as
shortness of breath and chest congestion.
The above discussed three conditions are the major problems which should be taken
care of immediately.
Interventions
For the treatment of respiratory acidosis, doctors should give thee interventions which
will decrease breathing problems. Physicians must check the arterial blood gas levels with the
levels of PCO2 and PO2. The saturation level of oxygen and carbon dioxide should be checked.
However, the venous blood gas was examined so the arterial blood gas level should be checked to
compare both the conditions of the blood level. By comparing the results of the blood gases help
the physician to suggest different medications such as corticosteroids and bronchodilator to the
patient. As the intervention of the respiratory acidosis, non-invasive positive pressure ventilation
should be suggested to the patient. The supportive devices in different therapies such as
continuous positive airway pressure (CPAP) and bi-level therapy or (BiPAP) therapy
(Wannemuehler, Hubbell & Nelson, 2016). If the patient’s condition deteriorates more, the
intubation procedure can be suggested.
The hypotension must be decreased by administering saline to the body of the patient by
IV fluids, but extra sodium and potassium level should be checked because the elevated level of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
sodium and potassium might be the cause of heart failure in the aged patients. The patient must
be suggested to drink an adequate amount of water so that the sodium level will be balanced in
the blood of the patient.
To reduce the fever the patient should be kept warm and must be covered by the
bedsheets and warm cloths. Oral naproxen can be given to the patient and another reasons such
as the symptoms of respiratory acidosis must be treated(Hassan & Gumudavelli,2017). As a
result, the fever will be decreased.
Rationale
The partial pressure of the carbon dioxide and oxygen must be checked as the venous
blood gas report was recorded. The check-up helps to measure the pressure of carbon dioxide
and oxygen in the blood, especially in the artery. The ABG report helps to understand the
function of lungs and movement of oxygen and carbon dioxide in the blood. The Bi-PAP
method is used for respiratory problems and lung disease to improve respiration in the
patient.
Hypotension management is essential for the patient to provide proper minerals to the
body with hydrating body cells. Intravenous saline is administered to the body of the patient
to maintain the water balance in the body. Nurses should check the condition of the patient
regularly so that the sodium and potassium levels can be appropriately maintained. The
patient must be hydrated so that the excess sodium and potassium should be excreted from
the body of the patient.
The patient suffered from fever so that his temperature must be regulated manual
observation and regular monitoring of the patient’s condition. The patient should not be
prescribed paracetamol to as respiratory acidosis is the outcome of the uncontrolled usages or
overdose of the paracetamol. However, the fever should be decreased to control body
be suggested to drink an adequate amount of water so that the sodium level will be balanced in
the blood of the patient.
To reduce the fever the patient should be kept warm and must be covered by the
bedsheets and warm cloths. Oral naproxen can be given to the patient and another reasons such
as the symptoms of respiratory acidosis must be treated(Hassan & Gumudavelli,2017). As a
result, the fever will be decreased.
Rationale
The partial pressure of the carbon dioxide and oxygen must be checked as the venous
blood gas report was recorded. The check-up helps to measure the pressure of carbon dioxide
and oxygen in the blood, especially in the artery. The ABG report helps to understand the
function of lungs and movement of oxygen and carbon dioxide in the blood. The Bi-PAP
method is used for respiratory problems and lung disease to improve respiration in the
patient.
Hypotension management is essential for the patient to provide proper minerals to the
body with hydrating body cells. Intravenous saline is administered to the body of the patient
to maintain the water balance in the body. Nurses should check the condition of the patient
regularly so that the sodium and potassium levels can be appropriately maintained. The
patient must be hydrated so that the excess sodium and potassium should be excreted from
the body of the patient.
The patient suffered from fever so that his temperature must be regulated manual
observation and regular monitoring of the patient’s condition. The patient should not be
prescribed paracetamol to as respiratory acidosis is the outcome of the uncontrolled usages or
overdose of the paracetamol. However, the fever should be decreased to control body
temperature. Medications should be prescribed very cautiously so that any adverse situation
should not occur.
Outcomes/Evaluations
After using the Bi-PAP machine, the pO2 should be increased, whereas the pCO2 should
be decreased. The pO2 must be more than the 30mmHg, and the pCO2 must be controlled within
the normal range. The medication should help the patient in maintaining the normal respiratory
rate and reduce chest congestion in the patient. The medications and ventilating system of
respiratory support must cure the difficulties related to breathing.
Interventions related to the hypotension will help to control the minerals of blood with the
maintenance of the blood pressure of the patient. The medication should maintain the bicarbonate
and sodium level of the body. The patient’s blood pressure should be decreased by hydration. By
urination or perspiration, the water balance of the body should be maintained so that minerals
cannot affect the blood pressure.
The fever must be under control after the interventions as the patient was suffering from
cough and cold also. After the treatment of respiratory problems and fever, coughing must be
under control.
should not occur.
Outcomes/Evaluations
After using the Bi-PAP machine, the pO2 should be increased, whereas the pCO2 should
be decreased. The pO2 must be more than the 30mmHg, and the pCO2 must be controlled within
the normal range. The medication should help the patient in maintaining the normal respiratory
rate and reduce chest congestion in the patient. The medications and ventilating system of
respiratory support must cure the difficulties related to breathing.
Interventions related to the hypotension will help to control the minerals of blood with the
maintenance of the blood pressure of the patient. The medication should maintain the bicarbonate
and sodium level of the body. The patient’s blood pressure should be decreased by hydration. By
urination or perspiration, the water balance of the body should be maintained so that minerals
cannot affect the blood pressure.
The fever must be under control after the interventions as the patient was suffering from
cough and cold also. After the treatment of respiratory problems and fever, coughing must be
under control.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Centi, J., Freeman, R., Gibbons, C. H., Neargarder, S., Canova, A. O., & Cronin-Golomb,
A. (2019). Author response: Orthostatic hypotension, per se, can cause transient
worsening of cognition.retrieved from: https://n.neurology.org/content/author-
response-orthostatic-hypotension-se-can-cause-transient-worsening-cognition
Chandrasekhar, S., Rahim, M. A., Quraishi, S. M., Theja, C. R., & Kiran, K. S. (2017).
An observational clinical study of assessing the utility of PSS (Poison Severity Score)
and GCS (Glasgow Coma Scale) scoring systems in predicting severity and clinical
outcomes in op poisoning. J Evidence Based Med Healthcare, 4(38), 2325-2332.
DOI: 10.18410/jebmh/2017/458
Chaparro, D. F. R., Parra, O. J. S., & Upegui, E. (2018, July). Study of Critical Vital
Signs Using Deep Learning. In International Conference on Smart Homes and Health
Telematics (pp. 255-260). Springer, Cham.DOI: https://doi.org/10.1007/978-3-319-
94523-1_23
Farfara, R., Melamed, D., & Sadoun, S. (2018). U.S. Patent Application No. 15/772,276.
Retrieved from: https://patents.google.com/patent/US20180318238A1/en
Hassan, E. M., & Gumudavelli, S. (2017). U.S. Patent No. 9,662,300. Washington, DC:
U.S. Patent and Trademark Office. DOI:
https://patentimages.storage.googleapis.com/86/5f/dc/3d02bc4e0e4216/
US9662300.pdf
Jones, H. (2019). Medical Abbreviations & Normal Ranges: Survival Guide. Routledge.
Retrieved from: https://books.google.co.in/books?
hl=en&lr=&id=zQWQDwAAQBAJ&oi=fnd&pg=PA10&dq=Normal+GCS+
Centi, J., Freeman, R., Gibbons, C. H., Neargarder, S., Canova, A. O., & Cronin-Golomb,
A. (2019). Author response: Orthostatic hypotension, per se, can cause transient
worsening of cognition.retrieved from: https://n.neurology.org/content/author-
response-orthostatic-hypotension-se-can-cause-transient-worsening-cognition
Chandrasekhar, S., Rahim, M. A., Quraishi, S. M., Theja, C. R., & Kiran, K. S. (2017).
An observational clinical study of assessing the utility of PSS (Poison Severity Score)
and GCS (Glasgow Coma Scale) scoring systems in predicting severity and clinical
outcomes in op poisoning. J Evidence Based Med Healthcare, 4(38), 2325-2332.
DOI: 10.18410/jebmh/2017/458
Chaparro, D. F. R., Parra, O. J. S., & Upegui, E. (2018, July). Study of Critical Vital
Signs Using Deep Learning. In International Conference on Smart Homes and Health
Telematics (pp. 255-260). Springer, Cham.DOI: https://doi.org/10.1007/978-3-319-
94523-1_23
Farfara, R., Melamed, D., & Sadoun, S. (2018). U.S. Patent Application No. 15/772,276.
Retrieved from: https://patents.google.com/patent/US20180318238A1/en
Hassan, E. M., & Gumudavelli, S. (2017). U.S. Patent No. 9,662,300. Washington, DC:
U.S. Patent and Trademark Office. DOI:
https://patentimages.storage.googleapis.com/86/5f/dc/3d02bc4e0e4216/
US9662300.pdf
Jones, H. (2019). Medical Abbreviations & Normal Ranges: Survival Guide. Routledge.
Retrieved from: https://books.google.co.in/books?
hl=en&lr=&id=zQWQDwAAQBAJ&oi=fnd&pg=PA10&dq=Normal+GCS+
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
+scale+book&ots=kw-
nmlMJok&sig=6_RzWbYpvZx8NtqMJLgB7BTVY14&redir_esc=y#v=onepage&q&
f=false
Lo, L. J., & Liu, K. D. (2018). Hyponatremia and hypernatremia. Critical Care Secrets E-
Book, 150, 320.retrieved from :https://books.google.co.in/books?
hl=en&lr=&id=cpNNDwAAQBAJ&oi=fnd&pg=PA320&dq=hypernatremia+and+hy
perkalemia&ots=l8ipAqAgBF&sig=LPz4XT-
AQboUeL0FHmaB1iIogSQ&redir_esc=y#v=onepage&q=hypernatremia%20and
%20hyperkalemia&f=false
Wannemuehler, T. J., Hubbell, R. D., & Nelson, R. F. (2016). Tension pneumocephalus
related to spontaneous skull base dehiscence in a patient on BiPAP. Otology &
Neurotology, 37(9), e322-e324. DOI:
https://doi.org/10.1097/MAO.0000000000001141
Zimmerman, R., Tsai, A. G., Vázquez, B. Y. S., Cabrales, P., Hofmann, A., Meier, J., ...
& Intaglietta, M. (2017). Post-transfusion increase of hematocrit per se does not
improve circulatory oxygen delivery due to increased blood viscosity. Anesthesia and
analgesia, 124(5), 1547. DOI:
https://dx.doi.org/10.1213%2FANE.0000000000002008
nmlMJok&sig=6_RzWbYpvZx8NtqMJLgB7BTVY14&redir_esc=y#v=onepage&q&
f=false
Lo, L. J., & Liu, K. D. (2018). Hyponatremia and hypernatremia. Critical Care Secrets E-
Book, 150, 320.retrieved from :https://books.google.co.in/books?
hl=en&lr=&id=cpNNDwAAQBAJ&oi=fnd&pg=PA320&dq=hypernatremia+and+hy
perkalemia&ots=l8ipAqAgBF&sig=LPz4XT-
AQboUeL0FHmaB1iIogSQ&redir_esc=y#v=onepage&q=hypernatremia%20and
%20hyperkalemia&f=false
Wannemuehler, T. J., Hubbell, R. D., & Nelson, R. F. (2016). Tension pneumocephalus
related to spontaneous skull base dehiscence in a patient on BiPAP. Otology &
Neurotology, 37(9), e322-e324. DOI:
https://doi.org/10.1097/MAO.0000000000001141
Zimmerman, R., Tsai, A. G., Vázquez, B. Y. S., Cabrales, P., Hofmann, A., Meier, J., ...
& Intaglietta, M. (2017). Post-transfusion increase of hematocrit per se does not
improve circulatory oxygen delivery due to increased blood viscosity. Anesthesia and
analgesia, 124(5), 1547. DOI:
https://dx.doi.org/10.1213%2FANE.0000000000002008
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





