Annals of Internal Medicine: Nurse-Patient Ratios and Patient Safety
VerifiedAdded on 2023/03/20
|7
|7222
|89
Report
AI Summary
This report summarizes a systematic review published in the Annals of Internal Medicine, focusing on the relationship between nurse-patient ratios and patient safety. The review examined existing literature, including cross-sectional and longitudinal studies, to assess the impact of nurse staffing levels on hospital mortality and other patient outcomes. The findings indicate a consistent relationship between higher RN staffing and lower hospital-related mortality, supported by both a meta-analysis and a narrative review. The strongest evidence comes from a longitudinal study that carefully accounted for nurse staffing and patient comorbid conditions. The review also highlights limitations, such as the lack of evaluations of intentional interventions to increase nurse staffing ratios. The report discusses various factors influencing patient outcomes, including nurse burnout, job satisfaction, and the overall nursing environment. The review suggests that improved surveillance, facilitated by adequate staffing, is a critical factor in reducing inpatient mortality. The review also mentions the need for further research to establish a causal relationship and explore the underlying mechanisms.
Nurse–Patient Ratios as a Patient Safety Strategy
A Systematic Review
Paul G. Shekelle, MD, PhD
A smallpercentage of patients die during hospitalization or shortly
thereafter, and it is widely believed that more or better nursing care
could preventsome of these deaths.The authorsystematically
reviewed the evidence aboutnurse staffing ratios and in-hospital
death through September 2012.From 550 titles,87 articles were
reviewed and 15 new studies thataugmented the 2 existing re-
views were selected.The strongestevidence supporting a causal
relationship between highernurse staffing levelsand decreased
inpatientmortality comesfrom a longitudinalstudy in a single
hospitalthat carefully accounted fornurse staffing and patient
comorbid conditionsand a meta-analysisthat found a “dose–
response relationship” in observationalstudies of nurse staffing and
death.No studies reported any serious harms associated with an
increase in nurse staffing.Limiting any stronger conclusions is the
lack of an evaluation of an intervention to increase nurse staffing
ratios. The formalcosts of increasing the nurse–patient ratio cannot
be calculated because there has been no evaluation ofan inten-
tionalchange in nurse staffing to improve patient outcomes.
Ann Intern Med. 2013;158:404-409. www.annals.org
For author affiliation,see end of text.
THE PROBLEM
A smallpercentage of hospitalized patients die during
or shortlyafterhospitalization.Evidencesuggeststhat
some proportion ofthese deathscould probably be pre-
vented with more nursing care.For example,in 1 early
study of 232 342 surgical discharges from several Pennsyl-
vania hospitals, 4535 patients (2%) died within 30 days of
hospitalization;the investigators estimated that the differ-
ence between 4:1 and 8:1 patient–nurse ratios may be ap-
proximately 1000 deaths in a group of this size (1). Other
studieshave produced roughly similarestimates,namely
approximately 1 to 5 fewer deaths per 1000 inpatient days
with more nurse staffing per patient (2– 4).The rationale
for suggesting that increasing the ratio of registered nurses
(RNs) to patients will lead to decreased illness or mortality
rates rests on the belief that improved attention to patients
is the criticalfactor.This systematic review examined the
evidence on the effects of interventions aimed at increasing
nurse–patient ratios on patient illness and death.
PATIENTSAFETYSTRATEGIES
There has been no evaluation of an intentional change
in RN staffing to improve patient outcomes; therefore, the
patientsafety strategy referred to in thisarticle remains
somewhat unclear.Most studies have been cross-sectional
or longitudinalassessments ofdifferences in nursing staff
variables, with the most commonly assessed measure being
the proportion of RN time per some measure of inpatient
load and the most commonly assessed outcome being mor-
tality. However, many other factors have been proposed as
being causal with respect to the relationship between nurs-
ing care and reductions in hospital mortality, potentiall
addition to orinstead ofa simplenurse–patientratio.
These factorsinclude measuresof nursing burnout,job
satisfaction,teamwork,nurse turnover,nursing leadership
in hospitals, and nurse practice environment.
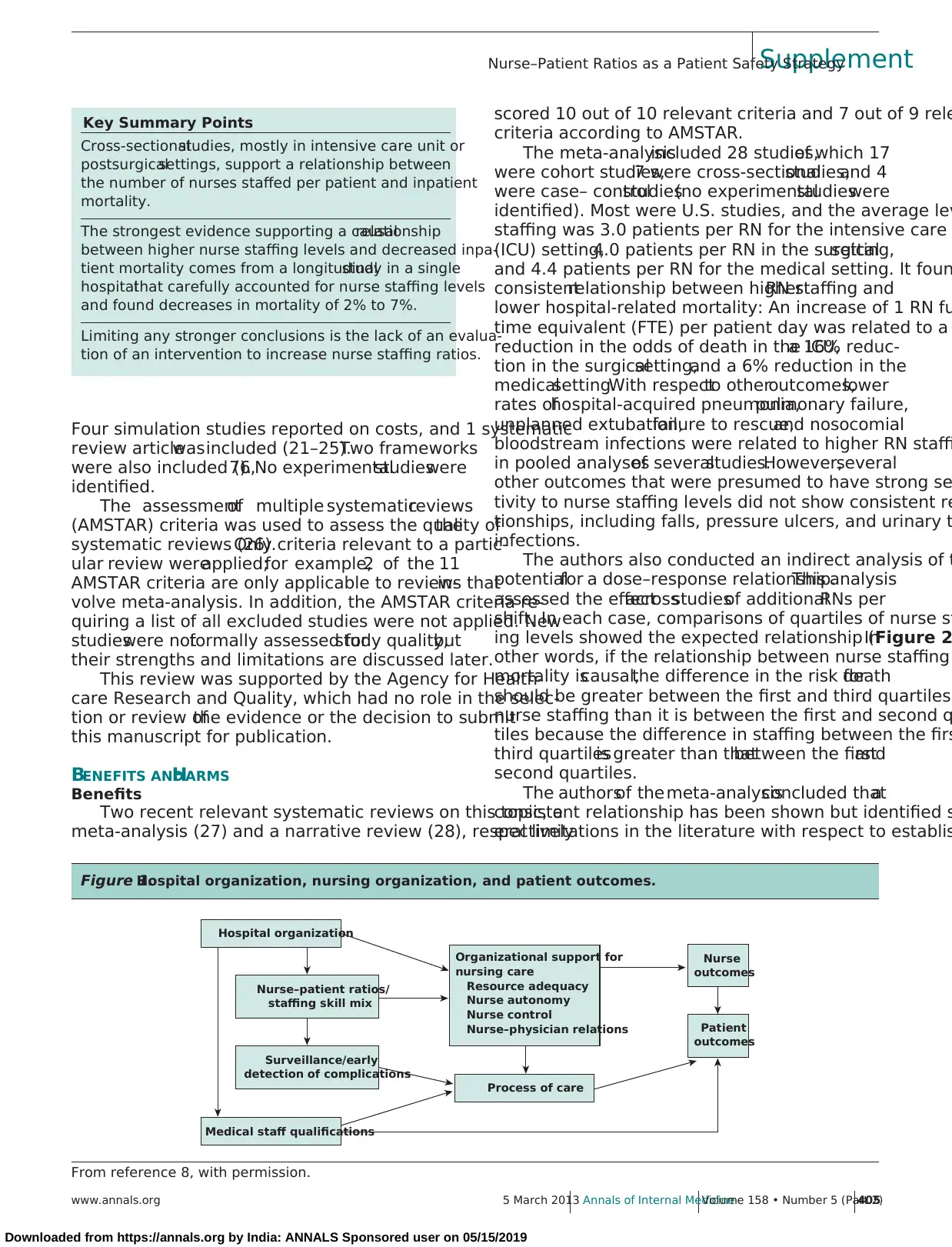
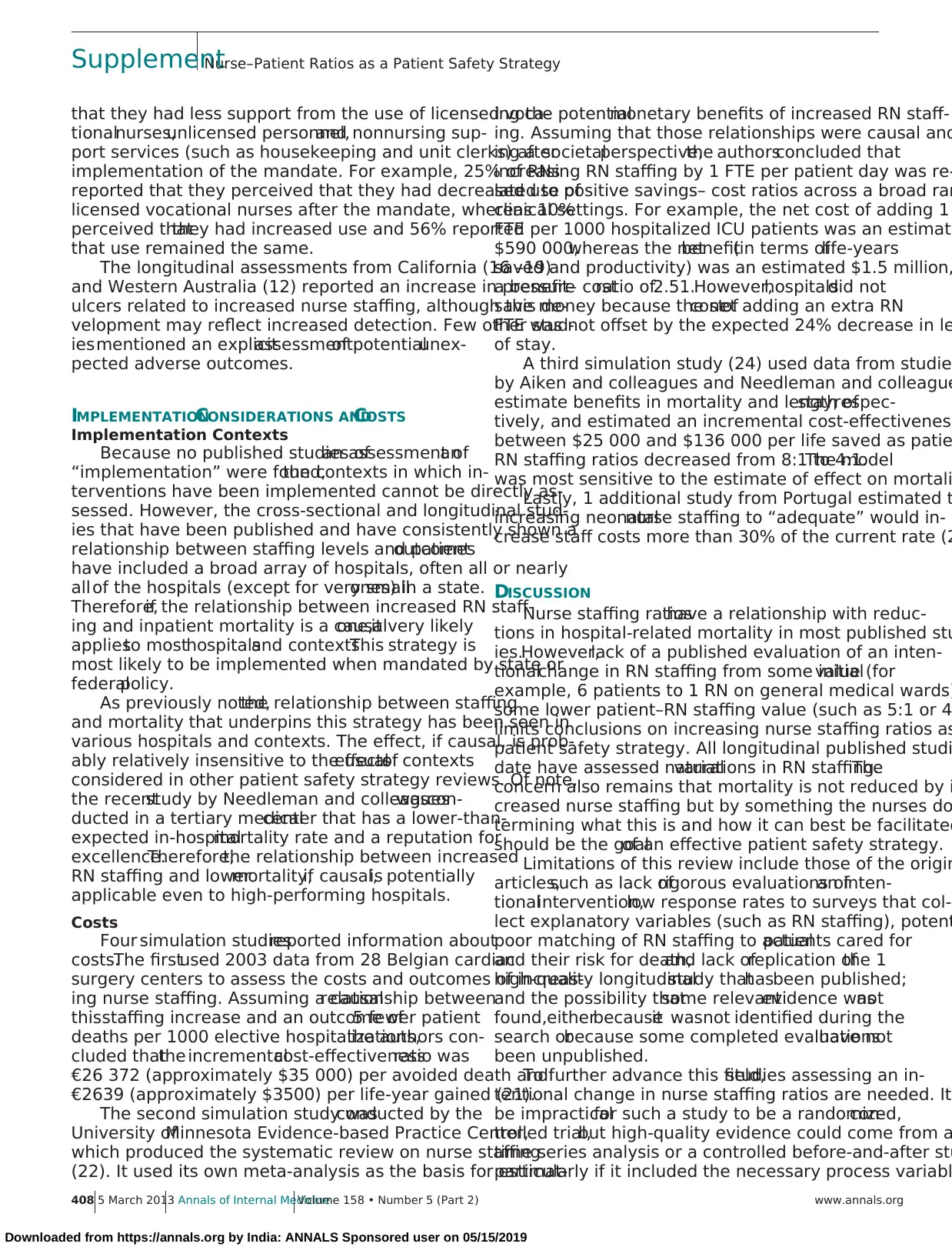
Severalresearch groupshaveproposed conceptual
frameworksto explain why more effective nursing care
may reduce inpatientmortality (5– 8).Underlying allof
these conceptualframeworks is the belief that surveillance
is a criticalfactor that can be improved with more staff,
better-educated staff, or a better working environment
A representative framework by Aiken and colleagues(8)
positsthatnurse–patientratios,along with staffing skill
mix,can lead to bettersurveillance,which,along with
many other factors,can influence the process of care and
lead to better patient outcomes (Figure 1).
REVIEWPROCESSES
Two existing reviews relevant to the topic were iden
tified,by using methods described by Whitlock and col-
leagues (10).These reviews were supplemented by search
ing the Web ofScience for articles published from 2009
(the end date of the search from the most recent revie
September2012 thatcited any of4 key articlesin this
field, including the older of the 2 reviews, and was limi
to studies published in English. For a complete descript
of the search strategies,literature flow diagram,and evi-
dence tables, see the Supplement (available at www.
.org). The update search identified 546 titles, and 4 art
came from reference mining.Titles and abstracts were re-
viewed and selected if they reported empiricaldata on the
relationship between nurse staffing ratios and mortality
nursing-sensitive outcomes, such as pressure ulcers an
ure to rescue.Because severalcross-sectionalstudies have
assessed this relationship,only 1 additionalcross-sectional
study was included for detailed review. The exception
a cross-sectionalstudy that evaluated a quasi-intervention
(11).Nine longitudinalstudieswere identified (12–20).
See also:
Web-Only
CME quiz (ProfessionalResponsibility Credit)
Supplement
Annals of Internal MediciSupplement
404 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2) www.annals.org
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
A Systematic Review
Paul G. Shekelle, MD, PhD
A smallpercentage of patients die during hospitalization or shortly
thereafter, and it is widely believed that more or better nursing care
could preventsome of these deaths.The authorsystematically
reviewed the evidence aboutnurse staffing ratios and in-hospital
death through September 2012.From 550 titles,87 articles were
reviewed and 15 new studies thataugmented the 2 existing re-
views were selected.The strongestevidence supporting a causal
relationship between highernurse staffing levelsand decreased
inpatientmortality comesfrom a longitudinalstudy in a single
hospitalthat carefully accounted fornurse staffing and patient
comorbid conditionsand a meta-analysisthat found a “dose–
response relationship” in observationalstudies of nurse staffing and
death.No studies reported any serious harms associated with an
increase in nurse staffing.Limiting any stronger conclusions is the
lack of an evaluation of an intervention to increase nurse staffing
ratios. The formalcosts of increasing the nurse–patient ratio cannot
be calculated because there has been no evaluation ofan inten-
tionalchange in nurse staffing to improve patient outcomes.
Ann Intern Med. 2013;158:404-409. www.annals.org
For author affiliation,see end of text.
THE PROBLEM
A smallpercentage of hospitalized patients die during
or shortlyafterhospitalization.Evidencesuggeststhat
some proportion ofthese deathscould probably be pre-
vented with more nursing care.For example,in 1 early
study of 232 342 surgical discharges from several Pennsyl-
vania hospitals, 4535 patients (2%) died within 30 days of
hospitalization;the investigators estimated that the differ-
ence between 4:1 and 8:1 patient–nurse ratios may be ap-
proximately 1000 deaths in a group of this size (1). Other
studieshave produced roughly similarestimates,namely
approximately 1 to 5 fewer deaths per 1000 inpatient days
with more nurse staffing per patient (2– 4).The rationale
for suggesting that increasing the ratio of registered nurses
(RNs) to patients will lead to decreased illness or mortality
rates rests on the belief that improved attention to patients
is the criticalfactor.This systematic review examined the
evidence on the effects of interventions aimed at increasing
nurse–patient ratios on patient illness and death.
PATIENTSAFETYSTRATEGIES
There has been no evaluation of an intentional change
in RN staffing to improve patient outcomes; therefore, the
patientsafety strategy referred to in thisarticle remains
somewhat unclear.Most studies have been cross-sectional
or longitudinalassessments ofdifferences in nursing staff
variables, with the most commonly assessed measure being
the proportion of RN time per some measure of inpatient
load and the most commonly assessed outcome being mor-
tality. However, many other factors have been proposed as
being causal with respect to the relationship between nurs-
ing care and reductions in hospital mortality, potentiall
addition to orinstead ofa simplenurse–patientratio.
These factorsinclude measuresof nursing burnout,job
satisfaction,teamwork,nurse turnover,nursing leadership
in hospitals, and nurse practice environment.
Severalresearch groupshaveproposed conceptual
frameworksto explain why more effective nursing care
may reduce inpatientmortality (5– 8).Underlying allof
these conceptualframeworks is the belief that surveillance
is a criticalfactor that can be improved with more staff,
better-educated staff, or a better working environment
A representative framework by Aiken and colleagues(8)
positsthatnurse–patientratios,along with staffing skill
mix,can lead to bettersurveillance,which,along with
many other factors,can influence the process of care and
lead to better patient outcomes (Figure 1).
REVIEWPROCESSES
Two existing reviews relevant to the topic were iden
tified,by using methods described by Whitlock and col-
leagues (10).These reviews were supplemented by search
ing the Web ofScience for articles published from 2009
(the end date of the search from the most recent revie
September2012 thatcited any of4 key articlesin this
field, including the older of the 2 reviews, and was limi
to studies published in English. For a complete descript
of the search strategies,literature flow diagram,and evi-
dence tables, see the Supplement (available at www.
.org). The update search identified 546 titles, and 4 art
came from reference mining.Titles and abstracts were re-
viewed and selected if they reported empiricaldata on the
relationship between nurse staffing ratios and mortality
nursing-sensitive outcomes, such as pressure ulcers an
ure to rescue.Because severalcross-sectionalstudies have
assessed this relationship,only 1 additionalcross-sectional
study was included for detailed review. The exception
a cross-sectionalstudy that evaluated a quasi-intervention
(11).Nine longitudinalstudieswere identified (12–20).
See also:
Web-Only
CME quiz (ProfessionalResponsibility Credit)
Supplement
Annals of Internal MediciSupplement
404 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2) www.annals.org
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Four simulation studies reported on costs, and 1 systematic
review articlewasincluded (21–25).Two frameworks
were also included (6,7). No experimentalstudieswere
identified.
The assessmentof multiple systematicreviews
(AMSTAR) criteria was used to assess the quality ofthe
systematic reviews (26).Only criteria relevant to a partic-
ular review wereapplied;for example,2 of the 11
AMSTAR criteria are only applicable to reviews thatin-
volve meta-analysis. In addition, the AMSTAR criteria re-
quiring a list of all excluded studies were not applied. New
studieswere notformally assessed forstudy quality,but
their strengths and limitations are discussed later.
This review was supported by the Agency for Health-
care Research and Quality, which had no role in the selec-
tion or review ofthe evidence or the decision to submit
this manuscript for publication.
BENEFITS ANDHARMS
Benefits
Two recent relevant systematic reviews on this topic, a
meta-analysis (27) and a narrative review (28), respectively
scored 10 out of 10 relevant criteria and 7 out of 9 rele
criteria according to AMSTAR.
The meta-analysisincluded 28 studies,of which 17
were cohort studies,7 were cross-sectionalstudies,and 4
were case– controlstudies(no experimentalstudieswere
identified). Most were U.S. studies, and the average lev
staffing was 3.0 patients per RN for the intensive care
(ICU) setting,4.0 patients per RN in the surgicalsetting,
and 4.4 patients per RN for the medical setting. It foun
consistentrelationship between higherRN staffing and
lower hospital-related mortality: An increase of 1 RN fu
time equivalent (FTE) per patient day was related to a
reduction in the odds of death in the ICU,a 16% reduc-
tion in the surgicalsetting,and a 6% reduction in the
medicalsetting.With respectto otheroutcomes,lower
rates ofhospital-acquired pneumonia,pulmonary failure,
unplanned extubation,failure to rescue,and nosocomial
bloodstream infections were related to higher RN staffi
in pooled analysesof severalstudies.However,several
other outcomes that were presumed to have strong se
tivity to nurse staffing levels did not show consistent re
tionships, including falls, pressure ulcers, and urinary t
infections.
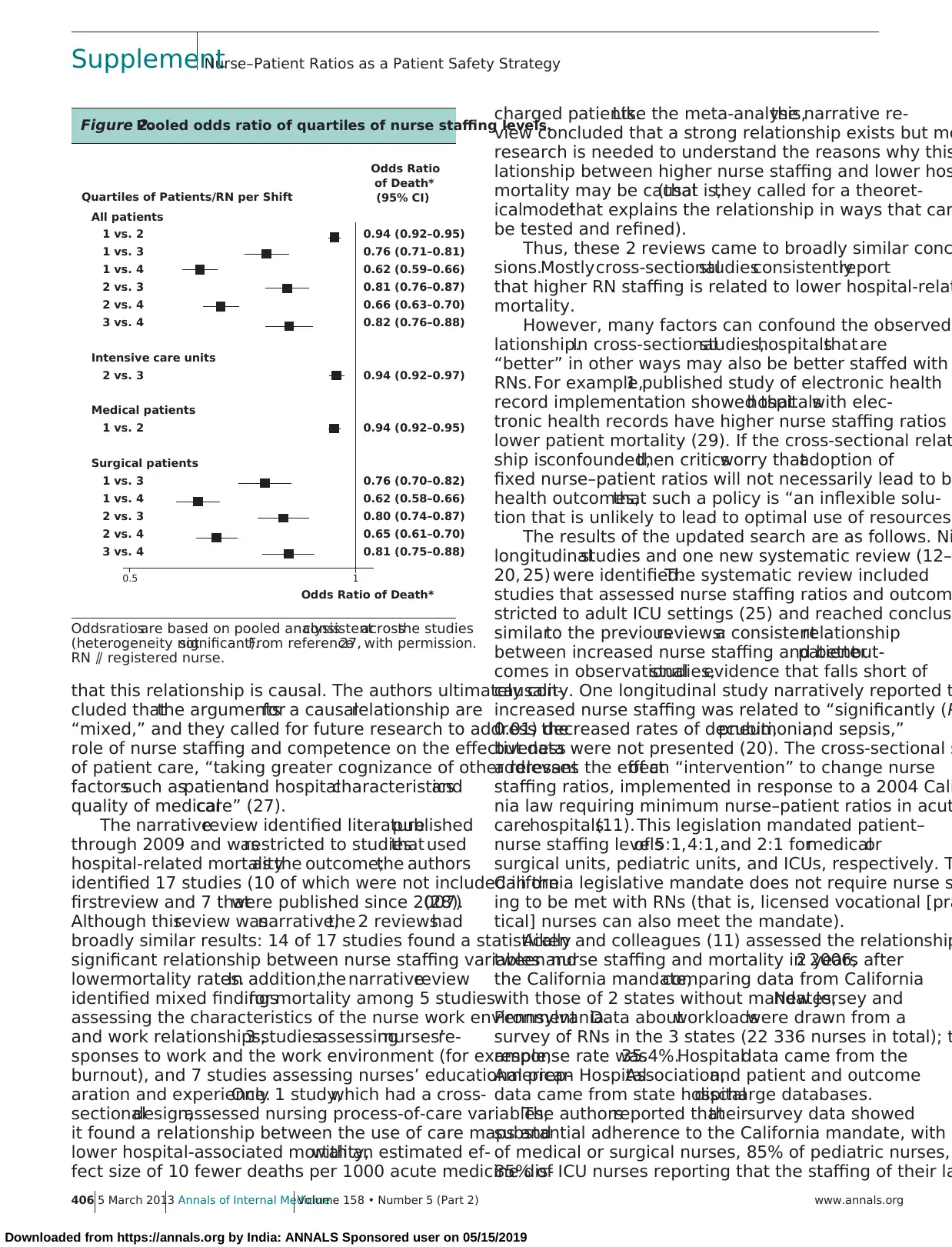
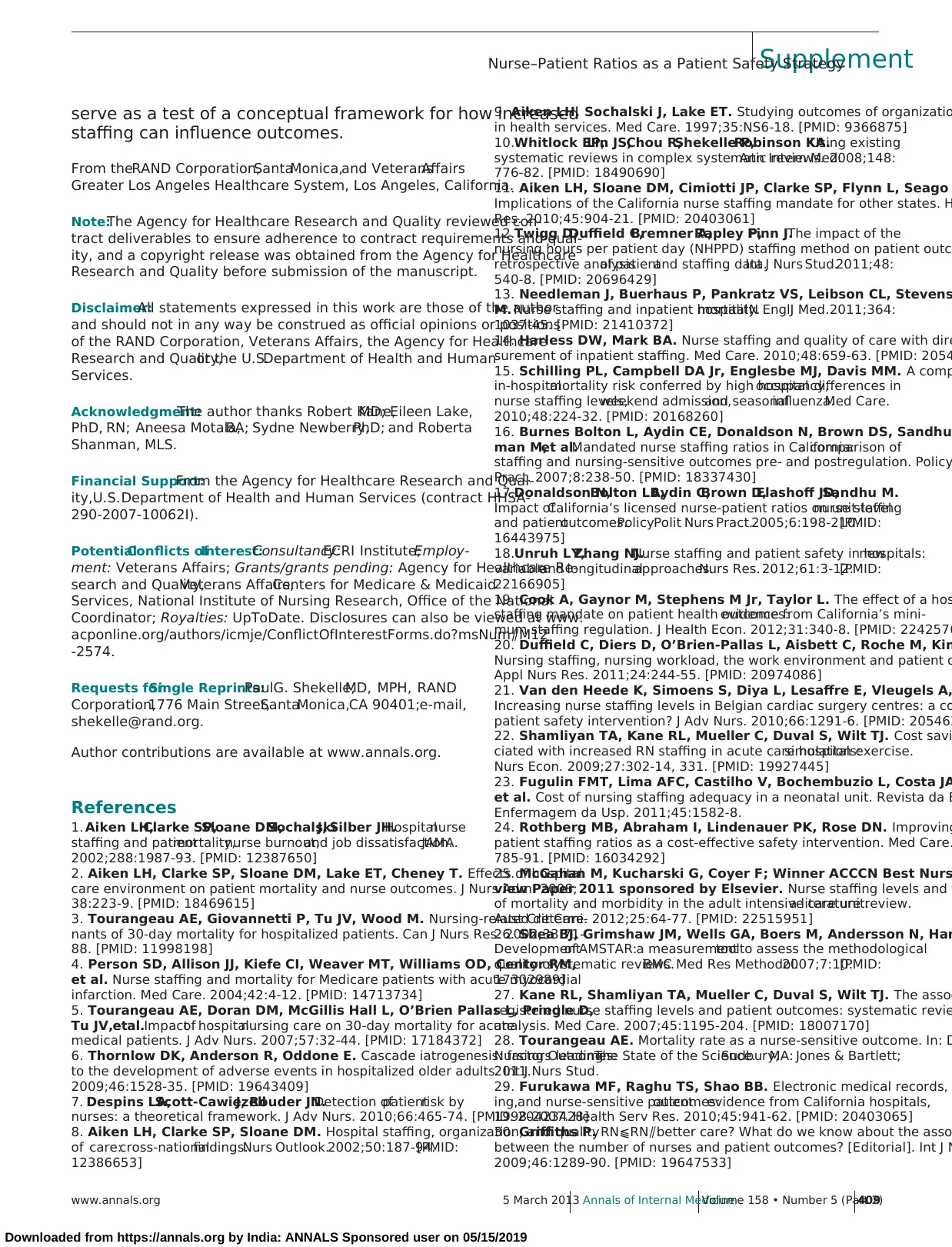
The authors also conducted an indirect analysis of t
potentialfor a dose–response relationship.This analysis
assessed the effectacrossstudiesof additionalRNs per
shift. In each case, comparisons of quartiles of nurse st
ing levels showed the expected relationship (Figure 2In
other words, if the relationship between nurse staffing
mortality iscausal,the difference in the risk fordeath
should be greater between the first and third quartiles
nurse staffing than it is between the first and second q
tiles because the difference in staffing between the firs
third quartilesis greater than thatbetween the firstand
second quartiles.
The authorsof the meta-analysisconcluded thata
consistent relationship has been shown but identified s
eral limitations in the literature with respect to establis
Key Summary Points
Cross-sectionalstudies, mostly in intensive care unit or
postsurgicalsettings, support a relationship between
the number of nurses staffed per patient and inpatient
mortality.
The strongest evidence supporting a causalrelationship
between higher nurse staffing levels and decreased inpa-
tient mortality comes from a longitudinalstudy in a single
hospitalthat carefully accounted for nurse staffing levels
and found decreases in mortality of 2% to 7%.
Limiting any stronger conclusions is the lack of an evalua-
tion of an intervention to increase nurse staffing ratios.
Figure 1.Hospital organization, nursing organization, and patient outcomes.
Hospital organization
Process of care
Medical staff qualifications
Nurse
outcomes
Patient
outcomes
Organizational support for
nursing care
Resource adequacy
Nurse autonomy
Nurse control
Nurse–physician relations
Nurse–patient ratios/
staffing skill mix
Surveillance/early
detection of complications
From reference 8, with permission.
SupplementNurse–Patient Ratios as a Patient Safety Strategy
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)405
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
review articlewasincluded (21–25).Two frameworks
were also included (6,7). No experimentalstudieswere
identified.
The assessmentof multiple systematicreviews
(AMSTAR) criteria was used to assess the quality ofthe
systematic reviews (26).Only criteria relevant to a partic-
ular review wereapplied;for example,2 of the 11
AMSTAR criteria are only applicable to reviews thatin-
volve meta-analysis. In addition, the AMSTAR criteria re-
quiring a list of all excluded studies were not applied. New
studieswere notformally assessed forstudy quality,but
their strengths and limitations are discussed later.
This review was supported by the Agency for Health-
care Research and Quality, which had no role in the selec-
tion or review ofthe evidence or the decision to submit
this manuscript for publication.
BENEFITS ANDHARMS
Benefits
Two recent relevant systematic reviews on this topic, a
meta-analysis (27) and a narrative review (28), respectively
scored 10 out of 10 relevant criteria and 7 out of 9 rele
criteria according to AMSTAR.
The meta-analysisincluded 28 studies,of which 17
were cohort studies,7 were cross-sectionalstudies,and 4
were case– controlstudies(no experimentalstudieswere
identified). Most were U.S. studies, and the average lev
staffing was 3.0 patients per RN for the intensive care
(ICU) setting,4.0 patients per RN in the surgicalsetting,
and 4.4 patients per RN for the medical setting. It foun
consistentrelationship between higherRN staffing and
lower hospital-related mortality: An increase of 1 RN fu
time equivalent (FTE) per patient day was related to a
reduction in the odds of death in the ICU,a 16% reduc-
tion in the surgicalsetting,and a 6% reduction in the
medicalsetting.With respectto otheroutcomes,lower
rates ofhospital-acquired pneumonia,pulmonary failure,
unplanned extubation,failure to rescue,and nosocomial
bloodstream infections were related to higher RN staffi
in pooled analysesof severalstudies.However,several
other outcomes that were presumed to have strong se
tivity to nurse staffing levels did not show consistent re
tionships, including falls, pressure ulcers, and urinary t
infections.
The authors also conducted an indirect analysis of t
potentialfor a dose–response relationship.This analysis
assessed the effectacrossstudiesof additionalRNs per
shift. In each case, comparisons of quartiles of nurse st
ing levels showed the expected relationship (Figure 2In
other words, if the relationship between nurse staffing
mortality iscausal,the difference in the risk fordeath
should be greater between the first and third quartiles
nurse staffing than it is between the first and second q
tiles because the difference in staffing between the firs
third quartilesis greater than thatbetween the firstand
second quartiles.
The authorsof the meta-analysisconcluded thata
consistent relationship has been shown but identified s
eral limitations in the literature with respect to establis
Key Summary Points
Cross-sectionalstudies, mostly in intensive care unit or
postsurgicalsettings, support a relationship between
the number of nurses staffed per patient and inpatient
mortality.
The strongest evidence supporting a causalrelationship
between higher nurse staffing levels and decreased inpa-
tient mortality comes from a longitudinalstudy in a single
hospitalthat carefully accounted for nurse staffing levels
and found decreases in mortality of 2% to 7%.
Limiting any stronger conclusions is the lack of an evalua-
tion of an intervention to increase nurse staffing ratios.
Figure 1.Hospital organization, nursing organization, and patient outcomes.
Hospital organization
Process of care
Medical staff qualifications
Nurse
outcomes
Patient
outcomes
Organizational support for
nursing care
Resource adequacy
Nurse autonomy
Nurse control
Nurse–physician relations
Nurse–patient ratios/
staffing skill mix
Surveillance/early
detection of complications
From reference 8, with permission.
SupplementNurse–Patient Ratios as a Patient Safety Strategy
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)405
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
that this relationship is causal. The authors ultimately con-
cluded thatthe argumentsfor a causalrelationship are
“mixed,” and they called for future research to address the
role of nurse staffing and competence on the effectiveness
of patient care, “taking greater cognizance of other relevant
factorssuch aspatientand hospitalcharacteristicsand
quality of medicalcare” (27).
The narrativereview identified literaturepublished
through 2009 and wasrestricted to studiesthat used
hospital-related mortalityas the outcome;the authors
identified 17 studies (10 of which were not included in the
firstreview and 7 thatwere published since 2007)(28).
Although thisreview wasnarrative,the 2 reviewshad
broadly similar results: 14 of 17 studies found a statistically
significant relationship between nurse staffing variables and
lowermortality rates.In addition,the narrativereview
identified mixed findingsfor mortality among 5 studies
assessing the characteristics of the nurse work environment
and work relationships,3 studiesassessingnurses’re-
sponses to work and the work environment (for example,
burnout), and 7 studies assessing nurses’ educational prep-
aration and experience.Only 1 study,which had a cross-
sectionaldesign,assessed nursing process-of-care variables;
it found a relationship between the use of care maps and
lower hospital-associated mortality,with an estimated ef-
fect size of 10 fewer deaths per 1000 acute medicine dis-
charged patients.Like the meta-analysis,the narrative re-
view concluded that a strong relationship exists but mo
research is needed to understand the reasons why this
lationship between higher nurse staffing and lower hos
mortality may be causal(that is,they called for a theoret-
icalmodelthat explains the relationship in ways that can
be tested and refined).
Thus, these 2 reviews came to broadly similar conc
sions.Mostlycross-sectionalstudiesconsistentlyreport
that higher RN staffing is related to lower hospital-relat
mortality.
However, many factors can confound the observed
lationship.In cross-sectionalstudies,hospitalsthat are
“better” in other ways may also be better staffed with
RNs.For example,1 published study of electronic health
record implementation showed thathospitalswith elec-
tronic health records have higher nurse staffing ratios
lower patient mortality (29). If the cross-sectional relat
ship isconfounded,then criticsworry thatadoption of
fixed nurse–patient ratios will not necessarily lead to b
health outcomes,that such a policy is “an inflexible solu-
tion that is unlikely to lead to optimal use of resources”
The results of the updated search are as follows. Ni
longitudinalstudies and one new systematic review (12–
20, 25) were identified.The systematic review included
studies that assessed nurse staffing ratios and outcom
stricted to adult ICU settings (25) and reached conclusi
similarto the previousreviews:a consistentrelationship
between increased nurse staffing and betterpatientout-
comes in observationalstudies,evidence that falls short of
causality. One longitudinal study narratively reported t
increased nurse staffing was related to “significantly (P
0.01) decreased rates of decubiti,pneumonia,and sepsis,”
but data were not presented (20). The cross-sectional s
addresses the effectof an “intervention” to change nurse
staffing ratios, implemented in response to a 2004 Cali
nia law requiring minimum nurse–patient ratios in acut
carehospitals(11).This legislation mandated patient–
nurse staffing levelsof 5:1,4:1,and 2:1 formedicalor
surgical units, pediatric units, and ICUs, respectively. T
California legislative mandate does not require nurse s
ing to be met with RNs (that is, licensed vocational [pra
tical] nurses can also meet the mandate).
Aiken and colleagues (11) assessed the relationship
tween nurse staffing and mortality in 2006,2 years after
the California mandate,comparing data from California
with those of 2 states without mandates,New Jersey and
Pennsylvania.Data aboutworkloadswere drawn from a
survey of RNs in the 3 states (22 336 nurses in total); t
response rate was35.4%.Hospitaldata came from the
American HospitalAssociation,and patient and outcome
data came from state hospitaldischarge databases.
The authorsreported thattheirsurvey data showed
substantial adherence to the California mandate, with 8
of medical or surgical nurses, 85% of pediatric nurses,
85% of ICU nurses reporting that the staffing of their la
Figure 2.Pooled odds ratio of quartiles of nurse staffing levels.
Quartiles of Patients/RN per Shift
All patients
1 vs. 2
1 vs. 3
1 vs. 4
2 vs. 3
2 vs. 4
3 vs. 4
Intensive care units
2 vs. 3
Medical patients
1 vs. 2
Surgical patients
1 vs. 3
1 vs. 4
2 vs. 3
2 vs. 4
3 vs. 4
Odds Ratio
of Death*
(95% CI)
Odds Ratio of Death*
0.94 (0.92–0.95)
0.76 (0.71–0.81)
0.62 (0.59–0.66)
0.81 (0.76–0.87)
0.66 (0.63–0.70)
0.82 (0.76–0.88)
0.94 (0.92–0.97)
0.94 (0.92–0.95)
0.76 (0.70–0.82)
0.62 (0.58–0.66)
0.80 (0.74–0.87)
0.65 (0.61–0.70)
0.81 (0.75–0.88)
0.5 1
Oddsratiosare based on pooled analysisconsistentacrossthe studies
(heterogeneity notsignificant).From reference27, with permission.
RN ⫽ registered nurse.
SupplementNurse–Patient Ratios as a Patient Safety Strategy
406 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2) www.annals.org
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
cluded thatthe argumentsfor a causalrelationship are
“mixed,” and they called for future research to address the
role of nurse staffing and competence on the effectiveness
of patient care, “taking greater cognizance of other relevant
factorssuch aspatientand hospitalcharacteristicsand
quality of medicalcare” (27).
The narrativereview identified literaturepublished
through 2009 and wasrestricted to studiesthat used
hospital-related mortalityas the outcome;the authors
identified 17 studies (10 of which were not included in the
firstreview and 7 thatwere published since 2007)(28).
Although thisreview wasnarrative,the 2 reviewshad
broadly similar results: 14 of 17 studies found a statistically
significant relationship between nurse staffing variables and
lowermortality rates.In addition,the narrativereview
identified mixed findingsfor mortality among 5 studies
assessing the characteristics of the nurse work environment
and work relationships,3 studiesassessingnurses’re-
sponses to work and the work environment (for example,
burnout), and 7 studies assessing nurses’ educational prep-
aration and experience.Only 1 study,which had a cross-
sectionaldesign,assessed nursing process-of-care variables;
it found a relationship between the use of care maps and
lower hospital-associated mortality,with an estimated ef-
fect size of 10 fewer deaths per 1000 acute medicine dis-
charged patients.Like the meta-analysis,the narrative re-
view concluded that a strong relationship exists but mo
research is needed to understand the reasons why this
lationship between higher nurse staffing and lower hos
mortality may be causal(that is,they called for a theoret-
icalmodelthat explains the relationship in ways that can
be tested and refined).
Thus, these 2 reviews came to broadly similar conc
sions.Mostlycross-sectionalstudiesconsistentlyreport
that higher RN staffing is related to lower hospital-relat
mortality.
However, many factors can confound the observed
lationship.In cross-sectionalstudies,hospitalsthat are
“better” in other ways may also be better staffed with
RNs.For example,1 published study of electronic health
record implementation showed thathospitalswith elec-
tronic health records have higher nurse staffing ratios
lower patient mortality (29). If the cross-sectional relat
ship isconfounded,then criticsworry thatadoption of
fixed nurse–patient ratios will not necessarily lead to b
health outcomes,that such a policy is “an inflexible solu-
tion that is unlikely to lead to optimal use of resources”
The results of the updated search are as follows. Ni
longitudinalstudies and one new systematic review (12–
20, 25) were identified.The systematic review included
studies that assessed nurse staffing ratios and outcom
stricted to adult ICU settings (25) and reached conclusi
similarto the previousreviews:a consistentrelationship
between increased nurse staffing and betterpatientout-
comes in observationalstudies,evidence that falls short of
causality. One longitudinal study narratively reported t
increased nurse staffing was related to “significantly (P
0.01) decreased rates of decubiti,pneumonia,and sepsis,”
but data were not presented (20). The cross-sectional s
addresses the effectof an “intervention” to change nurse
staffing ratios, implemented in response to a 2004 Cali
nia law requiring minimum nurse–patient ratios in acut
carehospitals(11).This legislation mandated patient–
nurse staffing levelsof 5:1,4:1,and 2:1 formedicalor
surgical units, pediatric units, and ICUs, respectively. T
California legislative mandate does not require nurse s
ing to be met with RNs (that is, licensed vocational [pra
tical] nurses can also meet the mandate).
Aiken and colleagues (11) assessed the relationship
tween nurse staffing and mortality in 2006,2 years after
the California mandate,comparing data from California
with those of 2 states without mandates,New Jersey and
Pennsylvania.Data aboutworkloadswere drawn from a
survey of RNs in the 3 states (22 336 nurses in total); t
response rate was35.4%.Hospitaldata came from the
American HospitalAssociation,and patient and outcome
data came from state hospitaldischarge databases.
The authorsreported thattheirsurvey data showed
substantial adherence to the California mandate, with 8
of medical or surgical nurses, 85% of pediatric nurses,
85% of ICU nurses reporting that the staffing of their la
Figure 2.Pooled odds ratio of quartiles of nurse staffing levels.
Quartiles of Patients/RN per Shift
All patients
1 vs. 2
1 vs. 3
1 vs. 4
2 vs. 3
2 vs. 4
3 vs. 4
Intensive care units
2 vs. 3
Medical patients
1 vs. 2
Surgical patients
1 vs. 3
1 vs. 4
2 vs. 3
2 vs. 4
3 vs. 4
Odds Ratio
of Death*
(95% CI)
Odds Ratio of Death*
0.94 (0.92–0.95)
0.76 (0.71–0.81)
0.62 (0.59–0.66)
0.81 (0.76–0.87)
0.66 (0.63–0.70)
0.82 (0.76–0.88)
0.94 (0.92–0.97)
0.94 (0.92–0.95)
0.76 (0.70–0.82)
0.62 (0.58–0.66)
0.80 (0.74–0.87)
0.65 (0.61–0.70)
0.81 (0.75–0.88)
0.5 1
Oddsratiosare based on pooled analysisconsistentacrossthe studies
(heterogeneity notsignificant).From reference27, with permission.
RN ⫽ registered nurse.
SupplementNurse–Patient Ratios as a Patient Safety Strategy
406 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2) www.annals.org
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
shift was within the mandated ratio.In logistic regression
analysesadjusted formany patientcharacteristicsand 3
hospitalcharacteristics(such asbed size,teaching status,
and technology use),Aiken and colleagues found statisti-
cally significant relationships between the estimation of the
average number of patients per nurse and 2 outcomes: 30-
day mortality and failure to rescue (11).
Although the study collected data after implementa-
tion of the California staffing mandate,it did not test the
effect of that mandate per se because it had no comparison
data from the period before the mandate went into effect.
The possibility that the relationship is causal is blunted by
longitudinalstudies thatexamined measures from before
and after the California mandate,which showed the ex-
pected changes in nurse staffing and proportion of licensed
staff per patient but no improvement in other patient out-
comes believed to be nursing-sensitive (such as falls,pres-
sure ulcers,and failure to rescue) (16,17,19).In fact,an
unexpected statistically significant increase in pressure ul-
cers was related to a greater number of hours of care for the
patient(which may have been because ofgreaterdetec-
tion). These studies did not assess mortality.
Five additionallongitudinalstudies add further infor-
mation to this picture.The firstis a longitudinalassess-
ment of nurse staffing and hospital mortality and failure to
rescue in 283 California hospitals between 1996 and 2001,
which had access to direct measures of nurse staffing (14).
In multivariable models that included many hospital mar-
ket characteristicsas well as risk adjustmentusing the
MedstatDisease Staging methodology to produce a pre-
dicted probability for complications or death,the authors
found that an increase of1 RN FTE per 1000 inpatient
dayswasrelated to a statistically significantdecrease in
mortality of 4.3%.
The second longitudinalstudy assessed careat 39
Michigan hospitalsbetween 2003 and 2006;it included
adults admitted through the emergency departmentwith
acute myocardial infarction, heart failure, stroke, pneumo-
nia,hip fracture,or gastrointestinalbleeding (15).This
study simultaneously controlled for 4 factors—high hospi-
taloccupancy on hospitalization,weekend hospitalization,
seasonal influenza, and nurse staffing levels—each of which
had a statistically significant effect on in-hospital mortality.
Each additionalRN FTE per patient day was related to a
0.25% decrease in mortality.
The third longitudinalstudy assessed the effectof a
mandate in 3 Western Australia public hospitals to imple-
ment a new staffing method,the Nursing Hours per Pa-
tient Day (12).The study assessed 3 periods:20 months
before implementation, 7 months of a “transition period,”
and 2 monthsafterimplementation.The authorsfound
that the totalnursing hours and RN hours increased dur-
ing the observation period.However,the percentage of
total nursing hours provided by RNs decreased (from 87%
to 84%). Also, the article stated that “although the nursing
hoursincreasedfor all threehospitals(in the post-
implementation period),the changes were not statistically
significant”(12). Mortalityrateswerereduced during
this period. Among many other outcomes, some impro
othersdid not, and somechangeswereinconsistent
across hospitals.Although the study was described as an
interrupted time series,it wasanalyzed asa before–after
study.
The fourth longitudinalstudyassessed changesin
nurse staffing over9 yearsin 124 Florida hospitalsand
related these to changes in Agency for Healthcare Res
and Quality Patient Safety Indicators (18). The study us
both initialstaffing ratiosand changesin staffing ratios.
Resultswere mixed butgenerally favored betterpatient
safety outcomes with higher RN staffing levels.
The methodologically strongestlongitudinalstudy is
thatof Needleman and colleagues(13).The researchers
used data overtime from a single hospitalto assessthe
relationship between naturaldifferencesin levelsof RN
staffing in the same hospitaland inpatient mortality.The
study isfurthercharacterized by a carefulmatching of
nurse staffing on a shift-by-shift basis with the actualpa-
tients cared for during that shift.Knowing the actualpa-
tients cared for allowed for more sophisticated adjustm
of risk for death at the patient level. The study was don
a tertiary academic hospitalbetween 2003 and 2006 and
included 197 691 hospitalizationsand 176 696 nursing
shifts across 43 hospital units. The patients themselves
eraged 60 years of age,and approximately 50% were cov-
ered under Medicare. The variable of interest was expo
of the patientto nursing care thatwasbelow the target
level(for that type of unit) for that shift (that is,the pro-
portion of shifts below target level staffing on a per-pat
basis).An additionalexposurevariablewas a “high-
turnover” shift (that is, a shift with many hospitalizatio
discharges,or transfers).The authors found that exposure
to each shift of below-target staffing or high turnover w
related to a 2% to 7% increase in mortality,with higher
levels of risk if the high-turnover or below-target shift o
curred in the first 5 days after hospitalization. For patie
who were not in an ICU,this risk was increased by 12%
and 15% during below-targetand high-turnovershifts,
respectively.
The data from Needleman and colleagues contribut
to the “causality” determination because the study is l
gitudinalin 1 hospital,thus controlling for the “hospital
effect” potentially present in all cross-sectional studies
has detailed measures ofexposure and confounding vari-
ables.These resultsand the dose–response analysisfrom
the meta-analysis provide the strongest evidence in su
of causality.
Harms
The survey administered as part of the cross-sectio
study previously described,which collected data 2 years
after the California mandate for minimum nurse staffin
ratios(11),found thatsome California nursesperceived
SupplementNurse–Patient Ratios as a Patient Safety Strategy
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)407
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
analysesadjusted formany patientcharacteristicsand 3
hospitalcharacteristics(such asbed size,teaching status,
and technology use),Aiken and colleagues found statisti-
cally significant relationships between the estimation of the
average number of patients per nurse and 2 outcomes: 30-
day mortality and failure to rescue (11).
Although the study collected data after implementa-
tion of the California staffing mandate,it did not test the
effect of that mandate per se because it had no comparison
data from the period before the mandate went into effect.
The possibility that the relationship is causal is blunted by
longitudinalstudies thatexamined measures from before
and after the California mandate,which showed the ex-
pected changes in nurse staffing and proportion of licensed
staff per patient but no improvement in other patient out-
comes believed to be nursing-sensitive (such as falls,pres-
sure ulcers,and failure to rescue) (16,17,19).In fact,an
unexpected statistically significant increase in pressure ul-
cers was related to a greater number of hours of care for the
patient(which may have been because ofgreaterdetec-
tion). These studies did not assess mortality.
Five additionallongitudinalstudies add further infor-
mation to this picture.The firstis a longitudinalassess-
ment of nurse staffing and hospital mortality and failure to
rescue in 283 California hospitals between 1996 and 2001,
which had access to direct measures of nurse staffing (14).
In multivariable models that included many hospital mar-
ket characteristicsas well as risk adjustmentusing the
MedstatDisease Staging methodology to produce a pre-
dicted probability for complications or death,the authors
found that an increase of1 RN FTE per 1000 inpatient
dayswasrelated to a statistically significantdecrease in
mortality of 4.3%.
The second longitudinalstudy assessed careat 39
Michigan hospitalsbetween 2003 and 2006;it included
adults admitted through the emergency departmentwith
acute myocardial infarction, heart failure, stroke, pneumo-
nia,hip fracture,or gastrointestinalbleeding (15).This
study simultaneously controlled for 4 factors—high hospi-
taloccupancy on hospitalization,weekend hospitalization,
seasonal influenza, and nurse staffing levels—each of which
had a statistically significant effect on in-hospital mortality.
Each additionalRN FTE per patient day was related to a
0.25% decrease in mortality.
The third longitudinalstudy assessed the effectof a
mandate in 3 Western Australia public hospitals to imple-
ment a new staffing method,the Nursing Hours per Pa-
tient Day (12).The study assessed 3 periods:20 months
before implementation, 7 months of a “transition period,”
and 2 monthsafterimplementation.The authorsfound
that the totalnursing hours and RN hours increased dur-
ing the observation period.However,the percentage of
total nursing hours provided by RNs decreased (from 87%
to 84%). Also, the article stated that “although the nursing
hoursincreasedfor all threehospitals(in the post-
implementation period),the changes were not statistically
significant”(12). Mortalityrateswerereduced during
this period. Among many other outcomes, some impro
othersdid not, and somechangeswereinconsistent
across hospitals.Although the study was described as an
interrupted time series,it wasanalyzed asa before–after
study.
The fourth longitudinalstudyassessed changesin
nurse staffing over9 yearsin 124 Florida hospitalsand
related these to changes in Agency for Healthcare Res
and Quality Patient Safety Indicators (18). The study us
both initialstaffing ratiosand changesin staffing ratios.
Resultswere mixed butgenerally favored betterpatient
safety outcomes with higher RN staffing levels.
The methodologically strongestlongitudinalstudy is
thatof Needleman and colleagues(13).The researchers
used data overtime from a single hospitalto assessthe
relationship between naturaldifferencesin levelsof RN
staffing in the same hospitaland inpatient mortality.The
study isfurthercharacterized by a carefulmatching of
nurse staffing on a shift-by-shift basis with the actualpa-
tients cared for during that shift.Knowing the actualpa-
tients cared for allowed for more sophisticated adjustm
of risk for death at the patient level. The study was don
a tertiary academic hospitalbetween 2003 and 2006 and
included 197 691 hospitalizationsand 176 696 nursing
shifts across 43 hospital units. The patients themselves
eraged 60 years of age,and approximately 50% were cov-
ered under Medicare. The variable of interest was expo
of the patientto nursing care thatwasbelow the target
level(for that type of unit) for that shift (that is,the pro-
portion of shifts below target level staffing on a per-pat
basis).An additionalexposurevariablewas a “high-
turnover” shift (that is, a shift with many hospitalizatio
discharges,or transfers).The authors found that exposure
to each shift of below-target staffing or high turnover w
related to a 2% to 7% increase in mortality,with higher
levels of risk if the high-turnover or below-target shift o
curred in the first 5 days after hospitalization. For patie
who were not in an ICU,this risk was increased by 12%
and 15% during below-targetand high-turnovershifts,
respectively.
The data from Needleman and colleagues contribut
to the “causality” determination because the study is l
gitudinalin 1 hospital,thus controlling for the “hospital
effect” potentially present in all cross-sectional studies
has detailed measures ofexposure and confounding vari-
ables.These resultsand the dose–response analysisfrom
the meta-analysis provide the strongest evidence in su
of causality.
Harms
The survey administered as part of the cross-sectio
study previously described,which collected data 2 years
after the California mandate for minimum nurse staffin
ratios(11),found thatsome California nursesperceived
SupplementNurse–Patient Ratios as a Patient Safety Strategy
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)407
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
that they had less support from the use of licensed voca-
tionalnurses,unlicensed personnel,and nonnursing sup-
port services (such as housekeeping and unit clerks) after
implementation of the mandate. For example, 25% of RNs
reported that they perceived that they had decreased use of
licensed vocational nurses after the mandate, whereas 10%
perceived thatthey had increased use and 56% reported
that use remained the same.
The longitudinal assessments from California (16 –19)
and Western Australia (12) reported an increase in pressure
ulcers related to increased nurse staffing, although this de-
velopment may reflect increased detection. Few other stud-
iesmentioned an explicitassessmentof potentialunex-
pected adverse outcomes.
IMPLEMENTATIONCONSIDERATIONS ANDCOSTS
Implementation Contexts
Because no published studies ofan assessment ofan
“implementation” were found,the contexts in which in-
terventions have been implemented cannot be directly as-
sessed. However, the cross-sectional and longitudinal stud-
ies that have been published and have consistently shown a
relationship between staffing levels and patientoutcomes
have included a broad array of hospitals, often all or nearly
all of the hospitals (except for very smallones) in a state.
Therefore,if the relationship between increased RN staff-
ing and inpatient mortality is a causalone,it very likely
appliesto mosthospitalsand contexts.This strategy is
most likely to be implemented when mandated by state or
federalpolicy.
As previously noted,the relationship between staffing
and mortality that underpins this strategy has been seen in
various hospitals and contexts. The effect, if causal, is prob-
ably relatively insensitive to the usualeffectsof contexts
considered in other patient safety strategy reviews. Of note,
the recentstudy by Needleman and colleagueswascon-
ducted in a tertiary medicalcenter that has a lower-than-
expected in-hospitalmortality rate and a reputation for
excellence.Therefore,the relationship between increased
RN staffing and lowermortality,if causal,is potentially
applicable even to high-performing hospitals.
Costs
Four simulation studiesreported information about
costs.The firstused 2003 data from 28 Belgian cardiac
surgery centers to assess the costs and outcomes of increas-
ing nurse staffing. Assuming a causalrelationship between
thisstaffing increase and an outcome of5 fewer patient
deaths per 1000 elective hospitalizations,the authors con-
cluded thatthe incrementalcost-effectivenessratio was
€26 372 (approximately $35 000) per avoided death and
€2639 (approximately $3500) per life-year gained (21).
The second simulation study wasconducted by the
University ofMinnesota Evidence-based Practice Center,
which produced the systematic review on nurse staffing
(22). It used its own meta-analysis as the basis for estimat-
ing the potentialmonetary benefits of increased RN staff-
ing. Assuming that those relationships were causal and
ing a societalperspective,the authorsconcluded that
increasing RN staffing by 1 FTE per patient day was re-
lated to positive savings– cost ratios across a broad ran
clinical settings. For example, the net cost of adding 1
FTE per 1000 hospitalized ICU patients was an estimate
$590 000,whereas the netbenefit(in terms oflife-years
saved and productivity) was an estimated $1.5 million,
a benefit– costratio of2.51.However,hospitalsdid not
save money because the netcostof adding an extra RN
FTE was not offset by the expected 24% decrease in le
of stay.
A third simulation study (24) used data from studie
by Aiken and colleagues and Needleman and colleague
estimate benefits in mortality and length ofstay,respec-
tively, and estimated an incremental cost-effectiveness
between $25 000 and $136 000 per life saved as patie
RN staffing ratios decreased from 8:1 to 4:1.The model
was most sensitive to the estimate of effect on mortali
Lastly, 1 additional study from Portugal estimated t
increasing neonatalnurse staffing to “adequate” would in-
crease staff costs more than 30% of the current rate (2
DISCUSSION
Nurse staffing ratioshave a relationship with reduc-
tions in hospital-related mortality in most published stu
ies.However,lack of a published evaluation of an inten-
tionalchange in RN staffing from some initialvalue (for
example, 6 patients to 1 RN on general medical wards)
some lower patient–RN staffing value (such as 5:1 or 4
limits conclusions on increasing nurse staffing ratios as
patient safety strategy. All longitudinal published studi
date have assessed naturalvariations in RN staffing.The
concern also remains that mortality is not reduced by i
creased nurse staffing but by something the nurses do
termining what this is and how it can best be facilitated
should be the goalof an effective patient safety strategy.
Limitations of this review include those of the origin
articles,such as lack ofrigorous evaluations ofan inten-
tionalintervention,low response rates to surveys that col-
lect explanatory variables (such as RN staffing), potent
poor matching of RN staffing to actualpatients cared for
and their risk for death,and lack ofreplication ofthe 1
high-quality longitudinalstudy thathasbeen published;
and the possibility thatsome relevantevidence wasnot
found,eitherbecauseit wasnot identified during the
search orbecause some completed evaluationshave not
been unpublished.
To further advance this field,studies assessing an in-
tentional change in nurse staffing ratios are needed. It
be impracticalfor such a study to be a randomized,con-
trolled trial,but high-quality evidence could come from a
time series analysis or a controlled before-and-after stu
particularly if it included the necessary process variabl
SupplementNurse–Patient Ratios as a Patient Safety Strategy
408 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2) www.annals.org
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
tionalnurses,unlicensed personnel,and nonnursing sup-
port services (such as housekeeping and unit clerks) after
implementation of the mandate. For example, 25% of RNs
reported that they perceived that they had decreased use of
licensed vocational nurses after the mandate, whereas 10%
perceived thatthey had increased use and 56% reported
that use remained the same.
The longitudinal assessments from California (16 –19)
and Western Australia (12) reported an increase in pressure
ulcers related to increased nurse staffing, although this de-
velopment may reflect increased detection. Few other stud-
iesmentioned an explicitassessmentof potentialunex-
pected adverse outcomes.
IMPLEMENTATIONCONSIDERATIONS ANDCOSTS
Implementation Contexts
Because no published studies ofan assessment ofan
“implementation” were found,the contexts in which in-
terventions have been implemented cannot be directly as-
sessed. However, the cross-sectional and longitudinal stud-
ies that have been published and have consistently shown a
relationship between staffing levels and patientoutcomes
have included a broad array of hospitals, often all or nearly
all of the hospitals (except for very smallones) in a state.
Therefore,if the relationship between increased RN staff-
ing and inpatient mortality is a causalone,it very likely
appliesto mosthospitalsand contexts.This strategy is
most likely to be implemented when mandated by state or
federalpolicy.
As previously noted,the relationship between staffing
and mortality that underpins this strategy has been seen in
various hospitals and contexts. The effect, if causal, is prob-
ably relatively insensitive to the usualeffectsof contexts
considered in other patient safety strategy reviews. Of note,
the recentstudy by Needleman and colleagueswascon-
ducted in a tertiary medicalcenter that has a lower-than-
expected in-hospitalmortality rate and a reputation for
excellence.Therefore,the relationship between increased
RN staffing and lowermortality,if causal,is potentially
applicable even to high-performing hospitals.
Costs
Four simulation studiesreported information about
costs.The firstused 2003 data from 28 Belgian cardiac
surgery centers to assess the costs and outcomes of increas-
ing nurse staffing. Assuming a causalrelationship between
thisstaffing increase and an outcome of5 fewer patient
deaths per 1000 elective hospitalizations,the authors con-
cluded thatthe incrementalcost-effectivenessratio was
€26 372 (approximately $35 000) per avoided death and
€2639 (approximately $3500) per life-year gained (21).
The second simulation study wasconducted by the
University ofMinnesota Evidence-based Practice Center,
which produced the systematic review on nurse staffing
(22). It used its own meta-analysis as the basis for estimat-
ing the potentialmonetary benefits of increased RN staff-
ing. Assuming that those relationships were causal and
ing a societalperspective,the authorsconcluded that
increasing RN staffing by 1 FTE per patient day was re-
lated to positive savings– cost ratios across a broad ran
clinical settings. For example, the net cost of adding 1
FTE per 1000 hospitalized ICU patients was an estimate
$590 000,whereas the netbenefit(in terms oflife-years
saved and productivity) was an estimated $1.5 million,
a benefit– costratio of2.51.However,hospitalsdid not
save money because the netcostof adding an extra RN
FTE was not offset by the expected 24% decrease in le
of stay.
A third simulation study (24) used data from studie
by Aiken and colleagues and Needleman and colleague
estimate benefits in mortality and length ofstay,respec-
tively, and estimated an incremental cost-effectiveness
between $25 000 and $136 000 per life saved as patie
RN staffing ratios decreased from 8:1 to 4:1.The model
was most sensitive to the estimate of effect on mortali
Lastly, 1 additional study from Portugal estimated t
increasing neonatalnurse staffing to “adequate” would in-
crease staff costs more than 30% of the current rate (2
DISCUSSION
Nurse staffing ratioshave a relationship with reduc-
tions in hospital-related mortality in most published stu
ies.However,lack of a published evaluation of an inten-
tionalchange in RN staffing from some initialvalue (for
example, 6 patients to 1 RN on general medical wards)
some lower patient–RN staffing value (such as 5:1 or 4
limits conclusions on increasing nurse staffing ratios as
patient safety strategy. All longitudinal published studi
date have assessed naturalvariations in RN staffing.The
concern also remains that mortality is not reduced by i
creased nurse staffing but by something the nurses do
termining what this is and how it can best be facilitated
should be the goalof an effective patient safety strategy.
Limitations of this review include those of the origin
articles,such as lack ofrigorous evaluations ofan inten-
tionalintervention,low response rates to surveys that col-
lect explanatory variables (such as RN staffing), potent
poor matching of RN staffing to actualpatients cared for
and their risk for death,and lack ofreplication ofthe 1
high-quality longitudinalstudy thathasbeen published;
and the possibility thatsome relevantevidence wasnot
found,eitherbecauseit wasnot identified during the
search orbecause some completed evaluationshave not
been unpublished.
To further advance this field,studies assessing an in-
tentional change in nurse staffing ratios are needed. It
be impracticalfor such a study to be a randomized,con-
trolled trial,but high-quality evidence could come from a
time series analysis or a controlled before-and-after stu
particularly if it included the necessary process variabl
SupplementNurse–Patient Ratios as a Patient Safety Strategy
408 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2) www.annals.org
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
serve as a test of a conceptual framework for how increased
staffing can influence outcomes.
From theRAND Corporation,SantaMonica,and VeteransAffairs
Greater Los Angeles Healthcare System, Los Angeles, California.
Note:The Agency for Healthcare Research and Quality reviewed con-
tract deliverables to ensure adherence to contract requirements and qual-
ity, and a copyright release was obtained from the Agency for Healthcare
Research and Quality before submission of the manuscript.
Disclaimer:All statements expressed in this work are those of the author
and should not in any way be construed as official opinions or positions
of the RAND Corporation, Veterans Affairs, the Agency for Healthcare
Research and Quality,or the U.S.Department of Health and Human
Services.
Acknowledgment:The author thanks Robert Kane,MD; Eileen Lake,
PhD, RN; Aneesa Motala,BA; Sydne Newberry,PhD; and Roberta
Shanman, MLS.
Financial Support:From the Agency for Healthcare Research and Qual-
ity,U.S.Department of Health and Human Services (contract HHSA-
290-2007-10062I).
PotentialConflicts ofInterest:Consultancy:ECRI Institute;Employ-
ment: Veterans Affairs; Grants/grants pending: Agency for Healthcare Re-
search and Quality,Veterans Affairs,Centers for Medicare & Medicaid
Services, National Institute of Nursing Research, Office of the National
Coordinator; Royalties: UpToDate. Disclosures can also be viewed at www.
acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum⫽M12
-2574.
Requests forSingle Reprints:PaulG. Shekelle,MD, MPH, RAND
Corporation,1776 Main Street,SantaMonica,CA 90401;e-mail,
shekelle@rand.org.
Author contributions are available at www.annals.org.
References
1. Aiken LH,Clarke SP,Sloane DM,SochalskiJ, Silber JH.Hospitalnurse
staffing and patientmortality,nurse burnout,and job dissatisfaction.JAMA.
2002;288:1987-93. [PMID: 12387650]
2. Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital
care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;
38:223-9. [PMID: 18469615]
3. Tourangeau AE, Giovannetti P, Tu JV, Wood M. Nursing-related determi-
nants of 30-day mortality for hospitalized patients. Can J Nurs Res. 2002;33:71-
88. [PMID: 11998198]
4. Person SD, Allison JJ, Kiefe CI, Weaver MT, Williams OD, Centor RM,
et al. Nurse staffing and mortality for Medicare patients with acute myocardial
infarction. Med Care. 2004;42:4-12. [PMID: 14713734]
5. Tourangeau AE, Doran DM, McGillis Hall L, O’Brien Pallas L, Pringle D,
Tu JV,etal.Impactof hospitalnursing care on 30-day mortality for acute
medical patients. J Adv Nurs. 2007;57:32-44. [PMID: 17184372]
6. Thornlow DK, Anderson R, Oddone E. Cascade iatrogenesis: factors leading
to the development of adverse events in hospitalized older adults. Int J Nurs Stud.
2009;46:1528-35. [PMID: 19643409]
7. Despins LA,Scott-CawiezellJ, Rouder JN.Detection ofpatientrisk by
nurses: a theoretical framework. J Adv Nurs. 2010;66:465-74. [PMID: 20423428]
8. Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality
of care:cross-nationalfindings.Nurs Outlook.2002;50:187-94.[PMID:
12386653]
9. Aiken LH, Sochalski J, Lake ET. Studying outcomes of organizatio
in health services. Med Care. 1997;35:NS6-18. [PMID: 9366875]
10.Whitlock EP,Lin JS,Chou R,Shekelle P,Robinson KA.Using existing
systematic reviews in complex systematic reviews.Ann Intern Med.2008;148:
776-82. [PMID: 18490690]
11. Aiken LH, Sloane DM, Cimiotti JP, Clarke SP, Flynn L, Seago
Implications of the California nurse staffing mandate for other states. H
Res. 2010;45:904-21. [PMID: 20403061]
12.Twigg D,Duffield C,Bremner A,Rapley P,Finn J.The impact of the
nursing hours per patient day (NHPPD) staffing method on patient outco
retrospective analysisof patientand staffing data.Int J Nurs Stud.2011;48:
540-8. [PMID: 20696429]
13. Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens
M. Nurse staffing and inpatient hospitalmortality.N EnglJ Med.2011;364:
1037-45. [PMID: 21410372]
14. Harless DW, Mark BA. Nurse staffing and quality of care with dire
surement of inpatient staffing. Med Care. 2010;48:659-63. [PMID: 2054
15. Schilling PL, Campbell DA Jr, Englesbe MJ, Davis MM. A comp
in-hospitalmortality risk conferred by high hospitaloccupancy,differences in
nurse staffing levels,weekend admission,and seasonalinfluenza.Med Care.
2010;48:224-32. [PMID: 20168260]
16. Burnes Bolton L, Aydin CE, Donaldson N, Brown DS, Sandhu
man M,et al.Mandated nurse staffing ratios in California:a comparison of
staffing and nursing-sensitive outcomes pre- and postregulation. Policy
Pract. 2007;8:238-50. [PMID: 18337430]
17.Donaldson N,Bolton LB,Aydin C,Brown D,Elashoff JD,Sandhu M.
Impact ofCalifornia’s licensed nurse-patient ratios on unit-levelnurse staffing
and patientoutcomes.PolicyPolit Nurs Pract.2005;6:198-210.[PMID:
16443975]
18.Unruh LY,Zhang NJ.Nurse staffing and patient safety in hospitals:new
variableand longitudinalapproaches.Nurs Res. 2012;61:3-12.[PMID:
22166905]
19. Cook A, Gaynor M, Stephens M Jr, Taylor L. The effect of a hos
staffing mandate on patient health outcomes:evidence from California’s mini-
mum staffing regulation. J Health Econ. 2012;31:340-8. [PMID: 2242576
20. Duffield C, Diers D, O’Brien-Pallas L, Aisbett C, Roche M, Kin
Nursing staffing, nursing workload, the work environment and patient o
Appl Nurs Res. 2011;24:244-55. [PMID: 20974086]
21. Van den Heede K, Simoens S, Diya L, Lesaffre E, Vleugels A,
Increasing nurse staffing levels in Belgian cardiac surgery centres: a co
patient safety intervention? J Adv Nurs. 2010;66:1291-6. [PMID: 205463
22. Shamliyan TA, Kane RL, Mueller C, Duval S, Wilt TJ. Cost savi
ciated with increased RN staffing in acute care hospitals:simulation exercise.
Nurs Econ. 2009;27:302-14, 331. [PMID: 19927445]
23. Fugulin FMT, Lima AFC, Castilho V, Bochembuzio L, Costa JA
et al. Cost of nursing staffing adequacy in a neonatal unit. Revista da E
Enfermagem da Usp. 2011;45:1582-8.
24. Rothberg MB, Abraham I, Lindenauer PK, Rose DN. Improving
patient staffing ratios as a cost-effective safety intervention. Med Care.
785-91. [PMID: 16034292]
25. McGahan M, Kucharski G, Coyer F; Winner ACCCN Best Nurs
view Paper 2011 sponsored by Elsevier. Nurse staffing levels and t
of mortality and morbidity in the adult intensive care unit:a literature review.
Aust Crit Care. 2012;25:64-77. [PMID: 22515951]
26. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Ham
Developmentof AMSTAR:a measurementtoolto assess the methodological
quality ofsystematic reviews.BMC Med Res Methodol.2007;7:10.[PMID:
17302989]
27. Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The assoc
registered nurse staffing levels and patient outcomes: systematic revie
analysis. Med Care. 2007;45:1195-204. [PMID: 18007170]
28. Tourangeau AE. Mortality rate as a nurse-sensitive outcome. In: D
Nursing Outcomes:The State of the Science.Sudbury,MA: Jones & Bartlett;
2011.
29. Furukawa MF, Raghu TS, Shao BB. Electronic medical records,
ing,and nurse-sensitive patientoutcomes:evidence from California hospitals,
1998-2007. Health Serv Res. 2010;45:941-62. [PMID: 20403065]
30. Griffiths P. RN⫹RN⫽better care? What do we know about the asso
between the number of nurses and patient outcomes? [Editorial]. Int J N
2009;46:1289-90. [PMID: 19647533]
SupplementNurse–Patient Ratios as a Patient Safety Strategy
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)409
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
staffing can influence outcomes.
From theRAND Corporation,SantaMonica,and VeteransAffairs
Greater Los Angeles Healthcare System, Los Angeles, California.
Note:The Agency for Healthcare Research and Quality reviewed con-
tract deliverables to ensure adherence to contract requirements and qual-
ity, and a copyright release was obtained from the Agency for Healthcare
Research and Quality before submission of the manuscript.
Disclaimer:All statements expressed in this work are those of the author
and should not in any way be construed as official opinions or positions
of the RAND Corporation, Veterans Affairs, the Agency for Healthcare
Research and Quality,or the U.S.Department of Health and Human
Services.
Acknowledgment:The author thanks Robert Kane,MD; Eileen Lake,
PhD, RN; Aneesa Motala,BA; Sydne Newberry,PhD; and Roberta
Shanman, MLS.
Financial Support:From the Agency for Healthcare Research and Qual-
ity,U.S.Department of Health and Human Services (contract HHSA-
290-2007-10062I).
PotentialConflicts ofInterest:Consultancy:ECRI Institute;Employ-
ment: Veterans Affairs; Grants/grants pending: Agency for Healthcare Re-
search and Quality,Veterans Affairs,Centers for Medicare & Medicaid
Services, National Institute of Nursing Research, Office of the National
Coordinator; Royalties: UpToDate. Disclosures can also be viewed at www.
acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum⫽M12
-2574.
Requests forSingle Reprints:PaulG. Shekelle,MD, MPH, RAND
Corporation,1776 Main Street,SantaMonica,CA 90401;e-mail,
shekelle@rand.org.
Author contributions are available at www.annals.org.
References
1. Aiken LH,Clarke SP,Sloane DM,SochalskiJ, Silber JH.Hospitalnurse
staffing and patientmortality,nurse burnout,and job dissatisfaction.JAMA.
2002;288:1987-93. [PMID: 12387650]
2. Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital
care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;
38:223-9. [PMID: 18469615]
3. Tourangeau AE, Giovannetti P, Tu JV, Wood M. Nursing-related determi-
nants of 30-day mortality for hospitalized patients. Can J Nurs Res. 2002;33:71-
88. [PMID: 11998198]
4. Person SD, Allison JJ, Kiefe CI, Weaver MT, Williams OD, Centor RM,
et al. Nurse staffing and mortality for Medicare patients with acute myocardial
infarction. Med Care. 2004;42:4-12. [PMID: 14713734]
5. Tourangeau AE, Doran DM, McGillis Hall L, O’Brien Pallas L, Pringle D,
Tu JV,etal.Impactof hospitalnursing care on 30-day mortality for acute
medical patients. J Adv Nurs. 2007;57:32-44. [PMID: 17184372]
6. Thornlow DK, Anderson R, Oddone E. Cascade iatrogenesis: factors leading
to the development of adverse events in hospitalized older adults. Int J Nurs Stud.
2009;46:1528-35. [PMID: 19643409]
7. Despins LA,Scott-CawiezellJ, Rouder JN.Detection ofpatientrisk by
nurses: a theoretical framework. J Adv Nurs. 2010;66:465-74. [PMID: 20423428]
8. Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality
of care:cross-nationalfindings.Nurs Outlook.2002;50:187-94.[PMID:
12386653]
9. Aiken LH, Sochalski J, Lake ET. Studying outcomes of organizatio
in health services. Med Care. 1997;35:NS6-18. [PMID: 9366875]
10.Whitlock EP,Lin JS,Chou R,Shekelle P,Robinson KA.Using existing
systematic reviews in complex systematic reviews.Ann Intern Med.2008;148:
776-82. [PMID: 18490690]
11. Aiken LH, Sloane DM, Cimiotti JP, Clarke SP, Flynn L, Seago
Implications of the California nurse staffing mandate for other states. H
Res. 2010;45:904-21. [PMID: 20403061]
12.Twigg D,Duffield C,Bremner A,Rapley P,Finn J.The impact of the
nursing hours per patient day (NHPPD) staffing method on patient outco
retrospective analysisof patientand staffing data.Int J Nurs Stud.2011;48:
540-8. [PMID: 20696429]
13. Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens
M. Nurse staffing and inpatient hospitalmortality.N EnglJ Med.2011;364:
1037-45. [PMID: 21410372]
14. Harless DW, Mark BA. Nurse staffing and quality of care with dire
surement of inpatient staffing. Med Care. 2010;48:659-63. [PMID: 2054
15. Schilling PL, Campbell DA Jr, Englesbe MJ, Davis MM. A comp
in-hospitalmortality risk conferred by high hospitaloccupancy,differences in
nurse staffing levels,weekend admission,and seasonalinfluenza.Med Care.
2010;48:224-32. [PMID: 20168260]
16. Burnes Bolton L, Aydin CE, Donaldson N, Brown DS, Sandhu
man M,et al.Mandated nurse staffing ratios in California:a comparison of
staffing and nursing-sensitive outcomes pre- and postregulation. Policy
Pract. 2007;8:238-50. [PMID: 18337430]
17.Donaldson N,Bolton LB,Aydin C,Brown D,Elashoff JD,Sandhu M.
Impact ofCalifornia’s licensed nurse-patient ratios on unit-levelnurse staffing
and patientoutcomes.PolicyPolit Nurs Pract.2005;6:198-210.[PMID:
16443975]
18.Unruh LY,Zhang NJ.Nurse staffing and patient safety in hospitals:new
variableand longitudinalapproaches.Nurs Res. 2012;61:3-12.[PMID:
22166905]
19. Cook A, Gaynor M, Stephens M Jr, Taylor L. The effect of a hos
staffing mandate on patient health outcomes:evidence from California’s mini-
mum staffing regulation. J Health Econ. 2012;31:340-8. [PMID: 2242576
20. Duffield C, Diers D, O’Brien-Pallas L, Aisbett C, Roche M, Kin
Nursing staffing, nursing workload, the work environment and patient o
Appl Nurs Res. 2011;24:244-55. [PMID: 20974086]
21. Van den Heede K, Simoens S, Diya L, Lesaffre E, Vleugels A,
Increasing nurse staffing levels in Belgian cardiac surgery centres: a co
patient safety intervention? J Adv Nurs. 2010;66:1291-6. [PMID: 205463
22. Shamliyan TA, Kane RL, Mueller C, Duval S, Wilt TJ. Cost savi
ciated with increased RN staffing in acute care hospitals:simulation exercise.
Nurs Econ. 2009;27:302-14, 331. [PMID: 19927445]
23. Fugulin FMT, Lima AFC, Castilho V, Bochembuzio L, Costa JA
et al. Cost of nursing staffing adequacy in a neonatal unit. Revista da E
Enfermagem da Usp. 2011;45:1582-8.
24. Rothberg MB, Abraham I, Lindenauer PK, Rose DN. Improving
patient staffing ratios as a cost-effective safety intervention. Med Care.
785-91. [PMID: 16034292]
25. McGahan M, Kucharski G, Coyer F; Winner ACCCN Best Nurs
view Paper 2011 sponsored by Elsevier. Nurse staffing levels and t
of mortality and morbidity in the adult intensive care unit:a literature review.
Aust Crit Care. 2012;25:64-77. [PMID: 22515951]
26. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Ham
Developmentof AMSTAR:a measurementtoolto assess the methodological
quality ofsystematic reviews.BMC Med Res Methodol.2007;7:10.[PMID:
17302989]
27. Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The assoc
registered nurse staffing levels and patient outcomes: systematic revie
analysis. Med Care. 2007;45:1195-204. [PMID: 18007170]
28. Tourangeau AE. Mortality rate as a nurse-sensitive outcome. In: D
Nursing Outcomes:The State of the Science.Sudbury,MA: Jones & Bartlett;
2011.
29. Furukawa MF, Raghu TS, Shao BB. Electronic medical records,
ing,and nurse-sensitive patientoutcomes:evidence from California hospitals,
1998-2007. Health Serv Res. 2010;45:941-62. [PMID: 20403065]
30. Griffiths P. RN⫹RN⫽better care? What do we know about the asso
between the number of nurses and patient outcomes? [Editorial]. Int J N
2009;46:1289-90. [PMID: 19647533]
SupplementNurse–Patient Ratios as a Patient Safety Strategy
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)409
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Author Contributions:Conception and design:P.G. Shekelle.
Analysis and interpretation of the data: P.G. Shekelle.
Drafting of the article: P.G. Shekelle.
Criticalrevisionof the articlefor importantintellectualcontent:
P.G. Shekelle.
Finalapprovalof the article: P.G. Shekelle.
Obtaining of funding: P.G. Shekelle.
Administrative, technical, or logistic support: P.G. Shekelle.
Collection and assembly of data: P.G. Shekelle.
31.Stone PW,Pogorzelska M,Kunches L,Hirschhorn LR.Hospitalstaffing
and health care-associated infections:a systematic review of the literature.Clin
Infect Dis. 2008;47:937-44. [PMID: 18767987]
32. Cummings GG, MacGregor T, Davey M, Lee H, Wong CA, Lo E, et al.
Leadership styles and outcome patterns for the nursing workforce and work en-
vironment:a systematic review.Int J NursStud.2010;47:363-85.[PMID:
19781702]
33. Butler M, Collins R, Drennan J, Halligan P, O’Mathu´na DP, Schultz TJ,
et al. Hospital nurse staffing models and patient and staff-related outcomes. Co-
chrane Database Syst Rev. 2011:CD007019. [PMID: 21735407]
34. Flynn M, McKeown M. Nurse staffing levels revisited: a consideration of key
issues in nurse staffing levels and skill mix research. J Nurs Manag. 2009;17:759-
66. [PMID: 19694919]
35. Cho SH, Hwang JH, Kim J. Nurse staffing and patient mortality in intensive
care units. Nurs Res. 2008;57:322-30. [PMID: 18794716]
36. Kiekkas P, Sakellaropoulos GC, Brokalaki H, Manolis E, Samios A, Skart-
sani C, et al. Association between nursing workload and mortality of intensive
care unit patients. J Nurs Scholarsh. 2008;40:385-90. [PMID: 19094155]
37. Hamilton KE, Redshaw ME, Tarnow-Mordi W. Nurse staffing in
to risk-adjusted mortality in neonatalcare.Arch Dis Child FetalNeonatalEd.
2007;92:F99-F103. [PMID: 17088341]
38. Mark BA, Harless DW, Berman WF. Nurse staffing and adverse
hospitalized children. Policy Polit Nurs Pract. 2007;8:83-92. [PMID: 1765
39.Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, et a
comes of variation in hospital nurse staffing in English hospitals: cross-
analysis of survey data and discharge records. Int J Nurs Stud. 2007;44
[PMID: 17064706]
40. Stone PW, Mooney-Kane C, Larson EL, Horan T, Glance LG, Z
J, et al. Nurse working conditions and patient safety outcomes. Med Ca
45:571-8. [PMID: 17515785]
41. Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giova
The impact of hospitalnursing characteristics on 30-day mortality.Nurs Res.
2005;54:74-84. [PMID: 15778649]
42.Halm M,Peterson M,Kandels M,Sabo J,Blalock M,Braden R,et al.
Hospital nurse staffing and patient mortality, emotional exhaustion, and
satisfaction. Clin Nurse Spec. 2005;19:241-51. [PMID: 16179855]
43.Aiken LH,Clarke SP,Cheung RB,Sloane DM,Silber JH.Educational
levels of hospitalnurses and surgicalpatient mortality.JAMA. 2003;290:1617-
23. [PMID: 14506121]
44. Sasichay-Akkadechanunt T, Scalzi CC, Jawad AF. The relations
nurse staffing and patientoutcomes.J Nurs Adm.2003;33:478-85.[PMID:
14501564]
45.Needleman J,Buerhaus P,Mattke S,Stewart M,Zelevinsky K.Nurse-
staffing levels and the quality of care in hospitals. N Engl J Med. 2002;3
22. [PMID: 12037152]
46. Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mo
relation to staff workload: a 4-year study in an adult intensive-care unit
2000;356:185-9. [PMID: 10963195]
Annals of Internal Medicine
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)W-183
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
Analysis and interpretation of the data: P.G. Shekelle.
Drafting of the article: P.G. Shekelle.
Criticalrevisionof the articlefor importantintellectualcontent:
P.G. Shekelle.
Finalapprovalof the article: P.G. Shekelle.
Obtaining of funding: P.G. Shekelle.
Administrative, technical, or logistic support: P.G. Shekelle.
Collection and assembly of data: P.G. Shekelle.
31.Stone PW,Pogorzelska M,Kunches L,Hirschhorn LR.Hospitalstaffing
and health care-associated infections:a systematic review of the literature.Clin
Infect Dis. 2008;47:937-44. [PMID: 18767987]
32. Cummings GG, MacGregor T, Davey M, Lee H, Wong CA, Lo E, et al.
Leadership styles and outcome patterns for the nursing workforce and work en-
vironment:a systematic review.Int J NursStud.2010;47:363-85.[PMID:
19781702]
33. Butler M, Collins R, Drennan J, Halligan P, O’Mathu´na DP, Schultz TJ,
et al. Hospital nurse staffing models and patient and staff-related outcomes. Co-
chrane Database Syst Rev. 2011:CD007019. [PMID: 21735407]
34. Flynn M, McKeown M. Nurse staffing levels revisited: a consideration of key
issues in nurse staffing levels and skill mix research. J Nurs Manag. 2009;17:759-
66. [PMID: 19694919]
35. Cho SH, Hwang JH, Kim J. Nurse staffing and patient mortality in intensive
care units. Nurs Res. 2008;57:322-30. [PMID: 18794716]
36. Kiekkas P, Sakellaropoulos GC, Brokalaki H, Manolis E, Samios A, Skart-
sani C, et al. Association between nursing workload and mortality of intensive
care unit patients. J Nurs Scholarsh. 2008;40:385-90. [PMID: 19094155]
37. Hamilton KE, Redshaw ME, Tarnow-Mordi W. Nurse staffing in
to risk-adjusted mortality in neonatalcare.Arch Dis Child FetalNeonatalEd.
2007;92:F99-F103. [PMID: 17088341]
38. Mark BA, Harless DW, Berman WF. Nurse staffing and adverse
hospitalized children. Policy Polit Nurs Pract. 2007;8:83-92. [PMID: 1765
39.Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, et a
comes of variation in hospital nurse staffing in English hospitals: cross-
analysis of survey data and discharge records. Int J Nurs Stud. 2007;44
[PMID: 17064706]
40. Stone PW, Mooney-Kane C, Larson EL, Horan T, Glance LG, Z
J, et al. Nurse working conditions and patient safety outcomes. Med Ca
45:571-8. [PMID: 17515785]
41. Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giova
The impact of hospitalnursing characteristics on 30-day mortality.Nurs Res.
2005;54:74-84. [PMID: 15778649]
42.Halm M,Peterson M,Kandels M,Sabo J,Blalock M,Braden R,et al.
Hospital nurse staffing and patient mortality, emotional exhaustion, and
satisfaction. Clin Nurse Spec. 2005;19:241-51. [PMID: 16179855]
43.Aiken LH,Clarke SP,Cheung RB,Sloane DM,Silber JH.Educational
levels of hospitalnurses and surgicalpatient mortality.JAMA. 2003;290:1617-
23. [PMID: 14506121]
44. Sasichay-Akkadechanunt T, Scalzi CC, Jawad AF. The relations
nurse staffing and patientoutcomes.J Nurs Adm.2003;33:478-85.[PMID:
14501564]
45.Needleman J,Buerhaus P,Mattke S,Stewart M,Zelevinsky K.Nurse-
staffing levels and the quality of care in hospitals. N Engl J Med. 2002;3
22. [PMID: 12037152]
46. Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mo
relation to staff workload: a 4-year study in an adult intensive-care unit
2000;356:185-9. [PMID: 10963195]
Annals of Internal Medicine
www.annals.org 5 March 2013 Annals of Internal MedicineVolume 158 • Number 5 (Part 2)W-183
Downloaded from https://annals.org by India: ANNALS Sponsored user on 05/15/2019
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





