Nurse Staffing and Patient Outcomes: A Systematic Review and Analysis
VerifiedAdded on 2023/03/20
|17
|11001
|34
Literature Review
AI Summary
This systematic review and meta-analysis investigates the association between nurse staffing levels and nurse-sensitive patient outcomes in acute specialist units. The review analyzed 35 cross-sectional studies from 2006 to 2017, primarily utilizing large administrative databases. Key findings indicate that higher nurse staffing levels correlate with reduced mortality, fewer medication errors, decreased incidence of ulcers and infections, and increased rates of timely percutaneous coronary intervention. A meta-analysis of six studies, involving 175,755 patients in intensive care and cardiac units, demonstrated a 14% reduction in in-hospital mortality with higher staffing levels, though significant heterogeneity was noted. The review concludes that nurse-to-patient ratios significantly influence patient outcomes, particularly in-hospital mortality, and emphasizes the need for more robust research to establish optimal staffing recommendations. Desklib offers access to this study along with a wealth of resources for students.
EUROPEAN
SOCIETY OF
CARDIOLOGY®
https://doi.org/10.1177/1474515117721561
European Journal of Cardiovascular Nursing
2018, Vol. 17(1) 6 –22
© The European Society of Cardiology 2017
Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
DOI: 10.1177/1474515117721561
journals.sagepub.com/home/cnu
The effect of nurse-to-patient ratios
on nurse-sensitive patient outcomes
in acute specialist units: a systematic
review and meta-analysis
Andrea Driscoll1, Maria J Grant2, Diane Carroll3, Sally Dalton4,
Christi Deaton5, Ian Jones6, Daniela Lehwaldt7, Gabrielle McKee8,
Theresa Munyombwe9 and Felicity Astin10
Abstract
Background: Nurses are pivotal in the provision of high quality care in acute hospitals. However, the optima
the number of nurses caring for patients remains elusive. In light of this, an updated review of the evidence o
of nurse staffing levels on patient outcomes is required.
Aim: To undertake a systematic review and meta-analysis examining the association between nurse staffing
nurse-sensitive patient outcomes in acute specialist units.
Methods: Nine electronic databases were searched for English articles published between 2006 and 2017. T
outcomes were nurse-sensitive patient outcomes.
Results: Of 3429 unique articles identified, 35 met the inclusion criteria. All were cross-sectional and the ma
utilised large administrative databases. Higher staffing levels were associated with reduced mortality, medica
ulcers, restraint use, infections, pneumonia, higher aspirin use and a greater number of patients receiving pe
coronary intervention within 90 minutes. A meta-analysis involving 175,755 patients, from six studies, admitt
intensive care unit and/or cardiac/cardiothoracic units showed that a higher nurse staffing level decreased th
inhospital mortality by 14% (0.86, 95% confidence interval 0.79–0.94). However, the meta-analysis also show
heterogeneity (I2=86%).
Conclusion: Nurse-to-patient ratios influence many patient outcomes, most markedly inhospital morta
studies need to be conducted on the association of nurse-to-patient ratios with nurse-sensitive patient outcom
offset the paucity and weaknesses of research in this area. This would provide further evidence for recommen
optimal nurse-to-patient ratios in acute specialist units.
Keywords
Nursing, workforce, staffing, systematic review, nurse-to-patient ratio
Date received: 14 February 2016; accepted: 28 June 2017
1 Quality and Patient Safety Research, School of Nursing and Midwifery,
Deakin University, Australia
2 School of Nursing, Midwifery, Social Work & Social Sciences,
University of Salford, UK
3Munn Center for Nursing Research, Massachusetts General Hospital,
USA
4Library, University of Leeds, UK
5Department of Public Health and Primary Care, University of
Cambridge, UK
6School of Nursing and Allied Health, Liverpool John Moores
University, UK
7Department of Nursing and Human Sciences, Dublin City University,
Ireland
8School of Nursing & Midwifery, Trinity College Dublin, Ireland
9Divison of Epidemiology and Biostatistics, University of Leeds, UK
10 Research and Development Department, University of Huddersfield
and Calderdale and Huddersfield NHS Foundation Trust, UK
Corresponding author:
Andrea Driscoll, School of Nursing and Midwifery, Quality and Patient
Safety Research (QPS), Deakin University, Locked Bag 20000, Geelong,
VIC 3220, Australia.
Email: andrea.driscoll@deakin.edu.au
721561 CNU0010.1177/1474515117721561European Journal of Cardiovascular Nursing Drisc oll et al.
review-article 2017
Review Article
SOCIETY OF
CARDIOLOGY®
https://doi.org/10.1177/1474515117721561
European Journal of Cardiovascular Nursing
2018, Vol. 17(1) 6 –22
© The European Society of Cardiology 2017
Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
DOI: 10.1177/1474515117721561
journals.sagepub.com/home/cnu
The effect of nurse-to-patient ratios
on nurse-sensitive patient outcomes
in acute specialist units: a systematic
review and meta-analysis
Andrea Driscoll1, Maria J Grant2, Diane Carroll3, Sally Dalton4,
Christi Deaton5, Ian Jones6, Daniela Lehwaldt7, Gabrielle McKee8,
Theresa Munyombwe9 and Felicity Astin10
Abstract
Background: Nurses are pivotal in the provision of high quality care in acute hospitals. However, the optima
the number of nurses caring for patients remains elusive. In light of this, an updated review of the evidence o
of nurse staffing levels on patient outcomes is required.
Aim: To undertake a systematic review and meta-analysis examining the association between nurse staffing
nurse-sensitive patient outcomes in acute specialist units.
Methods: Nine electronic databases were searched for English articles published between 2006 and 2017. T
outcomes were nurse-sensitive patient outcomes.
Results: Of 3429 unique articles identified, 35 met the inclusion criteria. All were cross-sectional and the ma
utilised large administrative databases. Higher staffing levels were associated with reduced mortality, medica
ulcers, restraint use, infections, pneumonia, higher aspirin use and a greater number of patients receiving pe
coronary intervention within 90 minutes. A meta-analysis involving 175,755 patients, from six studies, admitt
intensive care unit and/or cardiac/cardiothoracic units showed that a higher nurse staffing level decreased th
inhospital mortality by 14% (0.86, 95% confidence interval 0.79–0.94). However, the meta-analysis also show
heterogeneity (I2=86%).
Conclusion: Nurse-to-patient ratios influence many patient outcomes, most markedly inhospital morta
studies need to be conducted on the association of nurse-to-patient ratios with nurse-sensitive patient outcom
offset the paucity and weaknesses of research in this area. This would provide further evidence for recommen
optimal nurse-to-patient ratios in acute specialist units.
Keywords
Nursing, workforce, staffing, systematic review, nurse-to-patient ratio
Date received: 14 February 2016; accepted: 28 June 2017
1 Quality and Patient Safety Research, School of Nursing and Midwifery,
Deakin University, Australia
2 School of Nursing, Midwifery, Social Work & Social Sciences,
University of Salford, UK
3Munn Center for Nursing Research, Massachusetts General Hospital,
USA
4Library, University of Leeds, UK
5Department of Public Health and Primary Care, University of
Cambridge, UK
6School of Nursing and Allied Health, Liverpool John Moores
University, UK
7Department of Nursing and Human Sciences, Dublin City University,
Ireland
8School of Nursing & Midwifery, Trinity College Dublin, Ireland
9Divison of Epidemiology and Biostatistics, University of Leeds, UK
10 Research and Development Department, University of Huddersfield
and Calderdale and Huddersfield NHS Foundation Trust, UK
Corresponding author:
Andrea Driscoll, School of Nursing and Midwifery, Quality and Patient
Safety Research (QPS), Deakin University, Locked Bag 20000, Geelong,
VIC 3220, Australia.
Email: andrea.driscoll@deakin.edu.au
721561 CNU0010.1177/1474515117721561European Journal of Cardiovascular Nursing Drisc oll et al.
review-article 2017
Review Article
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Driscoll et al. 7
Introduction
Over the past decade there has been a renewed focus on
what constitutes an adequate level of nurse staffing. This is
in part due to some spectacular failures that have occurred in
care provision for hospital inpatients leading to loss of
life.1,2 Organisations across countries have adopted different
approaches to managing the nursing workforce. In Victoria,
Australia, and California, USA, standardised and manda-
tory nurse staffing levels have been in place for over a dec-
ade. In the UK and Ireland there are national nurse staffing
recommendations, but these are not mandated by law.3–5
Wales has a similar situation, they recently introduced the
Nurse Staffing Levels Act 2016; however, there are no man-
dated nurse-to-patient ratios (NPRs) only recommendations
to guide decisions about nurse staffing levels.6 The notion of
an optimal level of nurse staffing is somewhat controversial
because there is no one-size-fits-all approach to assessing
staffing levels. This lack of clarity is further aggravated by a
lack of consensus about the most appropriate way of esti-
mating the size and mix of nursing teams because all meas-
urement approaches have limitations.4,7
One of the challenges faced by managers responsible
for staffing is finding a way to understand the influence of
the multiple factors that make up each individual care
environment which are likely to differ across organisations
and countries. Donabedian grouped potential factors into
three broad domains: structural factors (the people, para-
phernalia and place that make up the healthcare delivery
system); processes of care (how care is done through the
interactions between health professionals and patients);
and subsequent outcomes (the end results of the care that
takes place in the context of the organisation).8
To determine nurse staffing levels, managers need to
understand the underlying determinants which are patient
factors (patient nursing need according to acuity and
dependency levels), ward factors (patient throughput) and
nursing staff factors (number and skill level).9 Findings
from a systematic review and meta-analysis, now a decade
old, reported a significant association between increased
nursing staffing in hospitals and improved nurse-sensitive
patients outcomes.10 A more recent literature review by
Penoyer found an association between nurse staffing levels
and patient outcomes in the intensive care unit (ICU).11
However, their review only included studies from 1998 to
2008. In light of this an updated literature review is war-
ranted. This review will examine recently published studies
investigating associations between nurse staffing levels and
nurse-sensitive patient outcomes in acute specialist units.
Methods
To support the quality of the systematic review, a protocol
was developed based on the PRISMA statement.12 The
review protocol was not registered.
Review objective
To identify studies conducted in acute specialist units,
which examine the association between nurse staffing lev-
els (NPRs) and nurse-sensitive patient outcomes (as
defined below).
Definitions
Nurse-to-patient ratio.NPRs are typically expressed in two
ways: the number of nurses working per shift or over a 24
hour period divided by the number of beds occupied by a
patient over the same time period; or the number of nursing
hours per patient bed days (NHPPD). There are other more
complex approaches to measure nurse staffing require-
ments but there is no single recommended approach.3 Many
of the studies included in this review have determined
NPRs. A higher level of nursing staff indicates more nurses
(or higher proportion of nurses) for assigned patients.
Lower nurse staffing is defined as fewer nurses (or lower
proportion) for the number of assigned patients.11
Moreover, little is known about how nurse staffing lev-
els are managed across hospitals in Europe. NPRs are eas-
ily and cheaply measured but it is a relatively blunt
instrument that can function as one indicator, and can be
triangulated with other measurement approaches to estab-
lish safe nurse staffing levels.
Nurse-sensitive patient outcome measures.The nurse-sensi-
tive patient outcomes measures included in this study were
based on adverse events from previous studies that have
been sensitive to changes in nurse staffing.10,13 The nurse-
sensitive patient outcome measures we included were:
mortality, failure to rescue (FTR), shock (including sepsis
resuscitation), cardiac arrest, unplanned extubation, hospi-
tal acquired pneumonia, respiratory failure, surgical bleed-
ing, heart failure/fluid overload, catheter-associated urinary
tract infection, pressure sores, patient falls, nosocomial
bloodstream infection, medication error, length of stay,
hospital-acquired sepsis, deep vein thrombosis, central
nervous system complications, death, wound infection,
pulmonary failure, and metabolic derangement.
Search strategy
The search strategy was developed by the research team
with input from expert information technologists (see
Supplementary Appendix 1). Electronic databases and
grey literature were searched (Medline (OvidSP), Medline
in Process (OvidSP), CINAHL (Cumulative Index to
Nursing and Allied Health Literature) (EBSCO), PsycInfo
(OvidSP), Embase (OvidSP), HMIC (Health Management
Information Consortium) (OvidSP), Cochrane Database of
Systematic Reviews, Web of Science; Science Citation
Index Expanded (ISI Web of Knowledge), Web of Science;
Introduction
Over the past decade there has been a renewed focus on
what constitutes an adequate level of nurse staffing. This is
in part due to some spectacular failures that have occurred in
care provision for hospital inpatients leading to loss of
life.1,2 Organisations across countries have adopted different
approaches to managing the nursing workforce. In Victoria,
Australia, and California, USA, standardised and manda-
tory nurse staffing levels have been in place for over a dec-
ade. In the UK and Ireland there are national nurse staffing
recommendations, but these are not mandated by law.3–5
Wales has a similar situation, they recently introduced the
Nurse Staffing Levels Act 2016; however, there are no man-
dated nurse-to-patient ratios (NPRs) only recommendations
to guide decisions about nurse staffing levels.6 The notion of
an optimal level of nurse staffing is somewhat controversial
because there is no one-size-fits-all approach to assessing
staffing levels. This lack of clarity is further aggravated by a
lack of consensus about the most appropriate way of esti-
mating the size and mix of nursing teams because all meas-
urement approaches have limitations.4,7
One of the challenges faced by managers responsible
for staffing is finding a way to understand the influence of
the multiple factors that make up each individual care
environment which are likely to differ across organisations
and countries. Donabedian grouped potential factors into
three broad domains: structural factors (the people, para-
phernalia and place that make up the healthcare delivery
system); processes of care (how care is done through the
interactions between health professionals and patients);
and subsequent outcomes (the end results of the care that
takes place in the context of the organisation).8
To determine nurse staffing levels, managers need to
understand the underlying determinants which are patient
factors (patient nursing need according to acuity and
dependency levels), ward factors (patient throughput) and
nursing staff factors (number and skill level).9 Findings
from a systematic review and meta-analysis, now a decade
old, reported a significant association between increased
nursing staffing in hospitals and improved nurse-sensitive
patients outcomes.10 A more recent literature review by
Penoyer found an association between nurse staffing levels
and patient outcomes in the intensive care unit (ICU).11
However, their review only included studies from 1998 to
2008. In light of this an updated literature review is war-
ranted. This review will examine recently published studies
investigating associations between nurse staffing levels and
nurse-sensitive patient outcomes in acute specialist units.
Methods
To support the quality of the systematic review, a protocol
was developed based on the PRISMA statement.12 The
review protocol was not registered.
Review objective
To identify studies conducted in acute specialist units,
which examine the association between nurse staffing lev-
els (NPRs) and nurse-sensitive patient outcomes (as
defined below).
Definitions
Nurse-to-patient ratio.NPRs are typically expressed in two
ways: the number of nurses working per shift or over a 24
hour period divided by the number of beds occupied by a
patient over the same time period; or the number of nursing
hours per patient bed days (NHPPD). There are other more
complex approaches to measure nurse staffing require-
ments but there is no single recommended approach.3 Many
of the studies included in this review have determined
NPRs. A higher level of nursing staff indicates more nurses
(or higher proportion of nurses) for assigned patients.
Lower nurse staffing is defined as fewer nurses (or lower
proportion) for the number of assigned patients.11
Moreover, little is known about how nurse staffing lev-
els are managed across hospitals in Europe. NPRs are eas-
ily and cheaply measured but it is a relatively blunt
instrument that can function as one indicator, and can be
triangulated with other measurement approaches to estab-
lish safe nurse staffing levels.
Nurse-sensitive patient outcome measures.The nurse-sensi-
tive patient outcomes measures included in this study were
based on adverse events from previous studies that have
been sensitive to changes in nurse staffing.10,13 The nurse-
sensitive patient outcome measures we included were:
mortality, failure to rescue (FTR), shock (including sepsis
resuscitation), cardiac arrest, unplanned extubation, hospi-
tal acquired pneumonia, respiratory failure, surgical bleed-
ing, heart failure/fluid overload, catheter-associated urinary
tract infection, pressure sores, patient falls, nosocomial
bloodstream infection, medication error, length of stay,
hospital-acquired sepsis, deep vein thrombosis, central
nervous system complications, death, wound infection,
pulmonary failure, and metabolic derangement.
Search strategy
The search strategy was developed by the research team
with input from expert information technologists (see
Supplementary Appendix 1). Electronic databases and
grey literature were searched (Medline (OvidSP), Medline
in Process (OvidSP), CINAHL (Cumulative Index to
Nursing and Allied Health Literature) (EBSCO), PsycInfo
(OvidSP), Embase (OvidSP), HMIC (Health Management
Information Consortium) (OvidSP), Cochrane Database of
Systematic Reviews, Web of Science; Science Citation
Index Expanded (ISI Web of Knowledge), Web of Science;
8 European Journal of Cardiovascular Nursing 17(1)
Social Sciences Citation Index (ISI Web of Knowledge),
Web of Science; Conference Proceedings Citation Index
– Science (ISI Web of Knowledge), Web of Science;
Conference Proceedings Citation Index- Social Science
and Humanities (ISI Web of Knowledge), Index to Theses,
Proquest Dissertations and Theses). A combination of key-
words was used and controlled vocabulary such as MeSH
(medical subject headings) when available. Search terms
included 18 terms on settings, i.e. coronary care, high
dependency, critical care, intensive care, cardiac ward,
intensive treatment unit and 17 terms relating to nursing or
manpower or skill mix, i.e. nurse staffing, nurse ratio,
nurse mix, nurse dose, nurse workload and 78 nurse-sensi-
tive outcomes, i.e. wound infection, pulmonary failure,
shock, pneumonia, length of stay, outcome, patient safety.
The search was limited to English language and conducted
from January 2006 to February 2017. Conference abstracts
and reference lists of included studies were manually
searched and additional studies identified.
Inclusion criteria
Following the literature search, a team of reviewers worked
in pairs to screen titles and abstracts independently accord-
ing to the inclusion criteria. Any disagreement between
reviewers was resolved by a third reviewer. Studies that
met the following inclusion criteria were included:
•• Patients admitted to acute specialist units (e.g. inten-
sive therapy units/critical care/intensive care/coronary
care, high dependency, and cardiothoracic surgery
units, where a proportion of the nurses are required to
have a postgraduate critical care qualification) with
care provision for adults (over 18 years of age). Studies
with a mixed population ward were included.
•• Investigating the effect of NPRs using either the
number of nurses divided by the number of patients
over 24 hours or the NHPPD.
•• Published from January 2006 to February 2017 in
English.
•• Quantitative methodology.
•• Primary outcome measures:
|| at least one nurse-sensitive outcome such as
mortality, FTR, shock, cardiac arrest, unplanned
extubation, hospital acquired pneumonia, res-
piratory failure, surgical bleeding, heart failure/
fluid overload/imbalance, urinary tract infec-
tion, pressure sores, patient falls, nosocomial
bloodstream infection, medication error, pain
control, unplanned readmission.
Data extraction
A tailor-made data extraction tool was developed a priori
and piloted and refined.
The tool included six screening questions to ensure
papers fit with the review inclusion criteria (see
Supplementary Appendix 2). Information was also extracted
from each study to record under the following headings:
bibliographic details; setting/country; study design; out-
comes, findings/conclusions and quality assessment.
Quality assessment
All included studies were assessed by the Newcastle–
Ottawa scale (NOS) to determine the quality of non-
randomised studies. 14 This tool was designed to facilitate
the incorporation of quality assessment into the system-
atic review. This tool has been used in previous Cochrane
reviews for assessment of risk of bias in non-randomised
studies. The content validity and inter-rater reliability of
this scale was previously established. The NOS consists
of eight items: representativeness of cohort, selection of
cohort, ascertainment of exposure, outcome of interest
was not present at baseline, comparability of cohorts,
assessment of outcome, length of follow-up and ade-
quacy of follow-up. 14 Each item was awarded a ‘*’ for
meeting the criterion. A study was also awarded an addi-
tional ‘*’ if the analysis was adjusted for potential con-
founding variables. The quality of each study was graded
as low, medium or high according to the number of stars
(*). The quality assessment was conducted independently
by two reviewers. Disagreements were resolved by a
third reviewer.
Statistical analysis
As this systematic review involved cross-sectional studies
we used adjusted measures, as reported by authors, as the
primary effect measures to control for confounding when
it was available. Odds ratios (ORs) were used as an appro-
priate effect measure if available. Other effect measures
were: hazard ratios or risk ratios.
A meta-analysis was conducted on homogenous studies
using a random-effect model with inhospital mortality as
the primary outcome. In studies where patient-to-nurse
ratios were used, these were converted to NPRs by calcu-
lating the inverse ratio. The overall effect sizes will be pre-
sented in a forest plot. In studies in which a pooled
meta-analysis was unable to be performed, a narrative
analysis will be undertaken.
Clinical homogeneity was assessed in terms of study
cohort, hospital units, diagnosis and risk of bias. The I 2
was also used to determine statistical heterogeneity. If I 2
is greater than 40% a random effects model will be used.
A sensitivity analysis will also be conducted using a
fixed effects model to determine if the conclusions were
different.
Data analysis was conducted using Review Manager
version 5.3.15
Social Sciences Citation Index (ISI Web of Knowledge),
Web of Science; Conference Proceedings Citation Index
– Science (ISI Web of Knowledge), Web of Science;
Conference Proceedings Citation Index- Social Science
and Humanities (ISI Web of Knowledge), Index to Theses,
Proquest Dissertations and Theses). A combination of key-
words was used and controlled vocabulary such as MeSH
(medical subject headings) when available. Search terms
included 18 terms on settings, i.e. coronary care, high
dependency, critical care, intensive care, cardiac ward,
intensive treatment unit and 17 terms relating to nursing or
manpower or skill mix, i.e. nurse staffing, nurse ratio,
nurse mix, nurse dose, nurse workload and 78 nurse-sensi-
tive outcomes, i.e. wound infection, pulmonary failure,
shock, pneumonia, length of stay, outcome, patient safety.
The search was limited to English language and conducted
from January 2006 to February 2017. Conference abstracts
and reference lists of included studies were manually
searched and additional studies identified.
Inclusion criteria
Following the literature search, a team of reviewers worked
in pairs to screen titles and abstracts independently accord-
ing to the inclusion criteria. Any disagreement between
reviewers was resolved by a third reviewer. Studies that
met the following inclusion criteria were included:
•• Patients admitted to acute specialist units (e.g. inten-
sive therapy units/critical care/intensive care/coronary
care, high dependency, and cardiothoracic surgery
units, where a proportion of the nurses are required to
have a postgraduate critical care qualification) with
care provision for adults (over 18 years of age). Studies
with a mixed population ward were included.
•• Investigating the effect of NPRs using either the
number of nurses divided by the number of patients
over 24 hours or the NHPPD.
•• Published from January 2006 to February 2017 in
English.
•• Quantitative methodology.
•• Primary outcome measures:
|| at least one nurse-sensitive outcome such as
mortality, FTR, shock, cardiac arrest, unplanned
extubation, hospital acquired pneumonia, res-
piratory failure, surgical bleeding, heart failure/
fluid overload/imbalance, urinary tract infec-
tion, pressure sores, patient falls, nosocomial
bloodstream infection, medication error, pain
control, unplanned readmission.
Data extraction
A tailor-made data extraction tool was developed a priori
and piloted and refined.
The tool included six screening questions to ensure
papers fit with the review inclusion criteria (see
Supplementary Appendix 2). Information was also extracted
from each study to record under the following headings:
bibliographic details; setting/country; study design; out-
comes, findings/conclusions and quality assessment.
Quality assessment
All included studies were assessed by the Newcastle–
Ottawa scale (NOS) to determine the quality of non-
randomised studies. 14 This tool was designed to facilitate
the incorporation of quality assessment into the system-
atic review. This tool has been used in previous Cochrane
reviews for assessment of risk of bias in non-randomised
studies. The content validity and inter-rater reliability of
this scale was previously established. The NOS consists
of eight items: representativeness of cohort, selection of
cohort, ascertainment of exposure, outcome of interest
was not present at baseline, comparability of cohorts,
assessment of outcome, length of follow-up and ade-
quacy of follow-up. 14 Each item was awarded a ‘*’ for
meeting the criterion. A study was also awarded an addi-
tional ‘*’ if the analysis was adjusted for potential con-
founding variables. The quality of each study was graded
as low, medium or high according to the number of stars
(*). The quality assessment was conducted independently
by two reviewers. Disagreements were resolved by a
third reviewer.
Statistical analysis
As this systematic review involved cross-sectional studies
we used adjusted measures, as reported by authors, as the
primary effect measures to control for confounding when
it was available. Odds ratios (ORs) were used as an appro-
priate effect measure if available. Other effect measures
were: hazard ratios or risk ratios.
A meta-analysis was conducted on homogenous studies
using a random-effect model with inhospital mortality as
the primary outcome. In studies where patient-to-nurse
ratios were used, these were converted to NPRs by calcu-
lating the inverse ratio. The overall effect sizes will be pre-
sented in a forest plot. In studies in which a pooled
meta-analysis was unable to be performed, a narrative
analysis will be undertaken.
Clinical homogeneity was assessed in terms of study
cohort, hospital units, diagnosis and risk of bias. The I 2
was also used to determine statistical heterogeneity. If I 2
is greater than 40% a random effects model will be used.
A sensitivity analysis will also be conducted using a
fixed effects model to determine if the conclusions were
different.
Data analysis was conducted using Review Manager
version 5.3.15
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Driscoll et al. 9
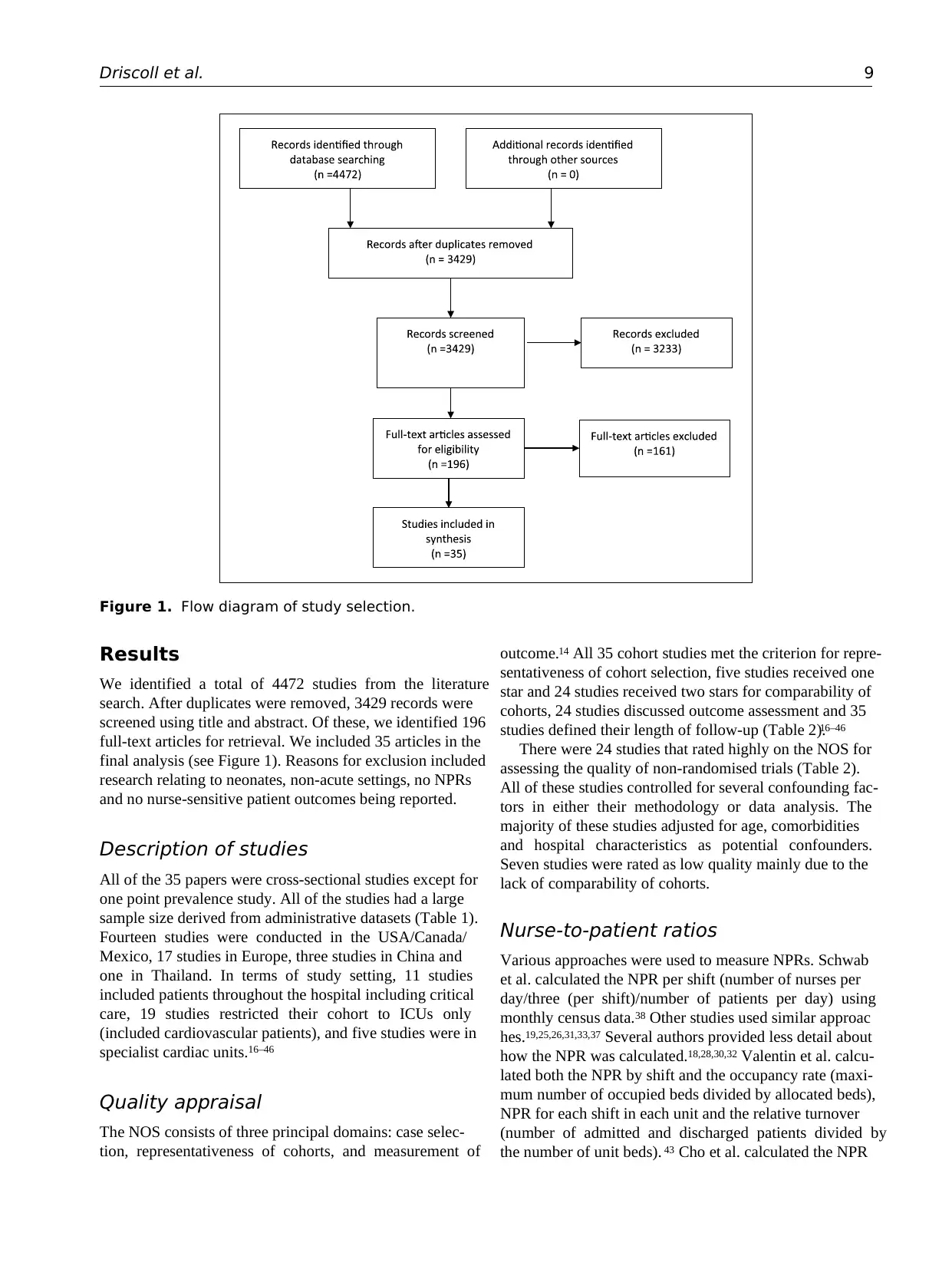
Results
We identified a total of 4472 studies from the literature
search. After duplicates were removed, 3429 records were
screened using title and abstract. Of these, we identified 196
full-text articles for retrieval. We included 35 articles in the
final analysis (see Figure 1). Reasons for exclusion included
research relating to neonates, non-acute settings, no NPRs
and no nurse-sensitive patient outcomes being reported.
Description of studies
All of the 35 papers were cross-sectional studies except for
one point prevalence study. All of the studies had a large
sample size derived from administrative datasets (Table 1).
Fourteen studies were conducted in the USA/Canada/
Mexico, 17 studies in Europe, three studies in China and
one in Thailand. In terms of study setting, 11 studies
included patients throughout the hospital including critical
care, 19 studies restricted their cohort to ICUs only
(included cardiovascular patients), and five studies were in
specialist cardiac units.16–46
Quality appraisal
The NOS consists of three principal domains: case selec-
tion, representativeness of cohorts, and measurement of
outcome.14 All 35 cohort studies met the criterion for repre-
sentativeness of cohort selection, five studies received one
star and 24 studies received two stars for comparability of
cohorts, 24 studies discussed outcome assessment and 35
studies defined their length of follow-up (Table 2).16–46
There were 24 studies that rated highly on the NOS for
assessing the quality of non-randomised trials (Table 2).
All of these studies controlled for several confounding fac-
tors in either their methodology or data analysis. The
majority of these studies adjusted for age, comorbidities
and hospital characteristics as potential confounders.
Seven studies were rated as low quality mainly due to the
lack of comparability of cohorts.
Nurse-to-patient ratios
Various approaches were used to measure NPRs. Schwab
et al. calculated the NPR per shift (number of nurses per
day/three (per shift)/number of patients per day) using
monthly census data.38 Other studies used similar approac
hes.19,25,26,31,33,37 Several authors provided less detail about
how the NPR was calculated.18,28,30,32 Valentin et al. calcu-
lated both the NPR by shift and the occupancy rate (maxi-
mum number of occupied beds divided by allocated beds),
NPR for each shift in each unit and the relative turnover
(number of admitted and discharged patients divided by
the number of unit beds). 43 Cho et al. calculated the NPR
Figure 1. Flow diagram of study selection.
Results
We identified a total of 4472 studies from the literature
search. After duplicates were removed, 3429 records were
screened using title and abstract. Of these, we identified 196
full-text articles for retrieval. We included 35 articles in the
final analysis (see Figure 1). Reasons for exclusion included
research relating to neonates, non-acute settings, no NPRs
and no nurse-sensitive patient outcomes being reported.
Description of studies
All of the 35 papers were cross-sectional studies except for
one point prevalence study. All of the studies had a large
sample size derived from administrative datasets (Table 1).
Fourteen studies were conducted in the USA/Canada/
Mexico, 17 studies in Europe, three studies in China and
one in Thailand. In terms of study setting, 11 studies
included patients throughout the hospital including critical
care, 19 studies restricted their cohort to ICUs only
(included cardiovascular patients), and five studies were in
specialist cardiac units.16–46
Quality appraisal
The NOS consists of three principal domains: case selec-
tion, representativeness of cohorts, and measurement of
outcome.14 All 35 cohort studies met the criterion for repre-
sentativeness of cohort selection, five studies received one
star and 24 studies received two stars for comparability of
cohorts, 24 studies discussed outcome assessment and 35
studies defined their length of follow-up (Table 2).16–46
There were 24 studies that rated highly on the NOS for
assessing the quality of non-randomised trials (Table 2).
All of these studies controlled for several confounding fac-
tors in either their methodology or data analysis. The
majority of these studies adjusted for age, comorbidities
and hospital characteristics as potential confounders.
Seven studies were rated as low quality mainly due to the
lack of comparability of cohorts.
Nurse-to-patient ratios
Various approaches were used to measure NPRs. Schwab
et al. calculated the NPR per shift (number of nurses per
day/three (per shift)/number of patients per day) using
monthly census data.38 Other studies used similar approac
hes.19,25,26,31,33,37 Several authors provided less detail about
how the NPR was calculated.18,28,30,32 Valentin et al. calcu-
lated both the NPR by shift and the occupancy rate (maxi-
mum number of occupied beds divided by allocated beds),
NPR for each shift in each unit and the relative turnover
(number of admitted and discharged patients divided by
the number of unit beds). 43 Cho et al. calculated the NPR
Figure 1. Flow diagram of study selection.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10 European Journal of Cardiovascular Nursing 17(1)
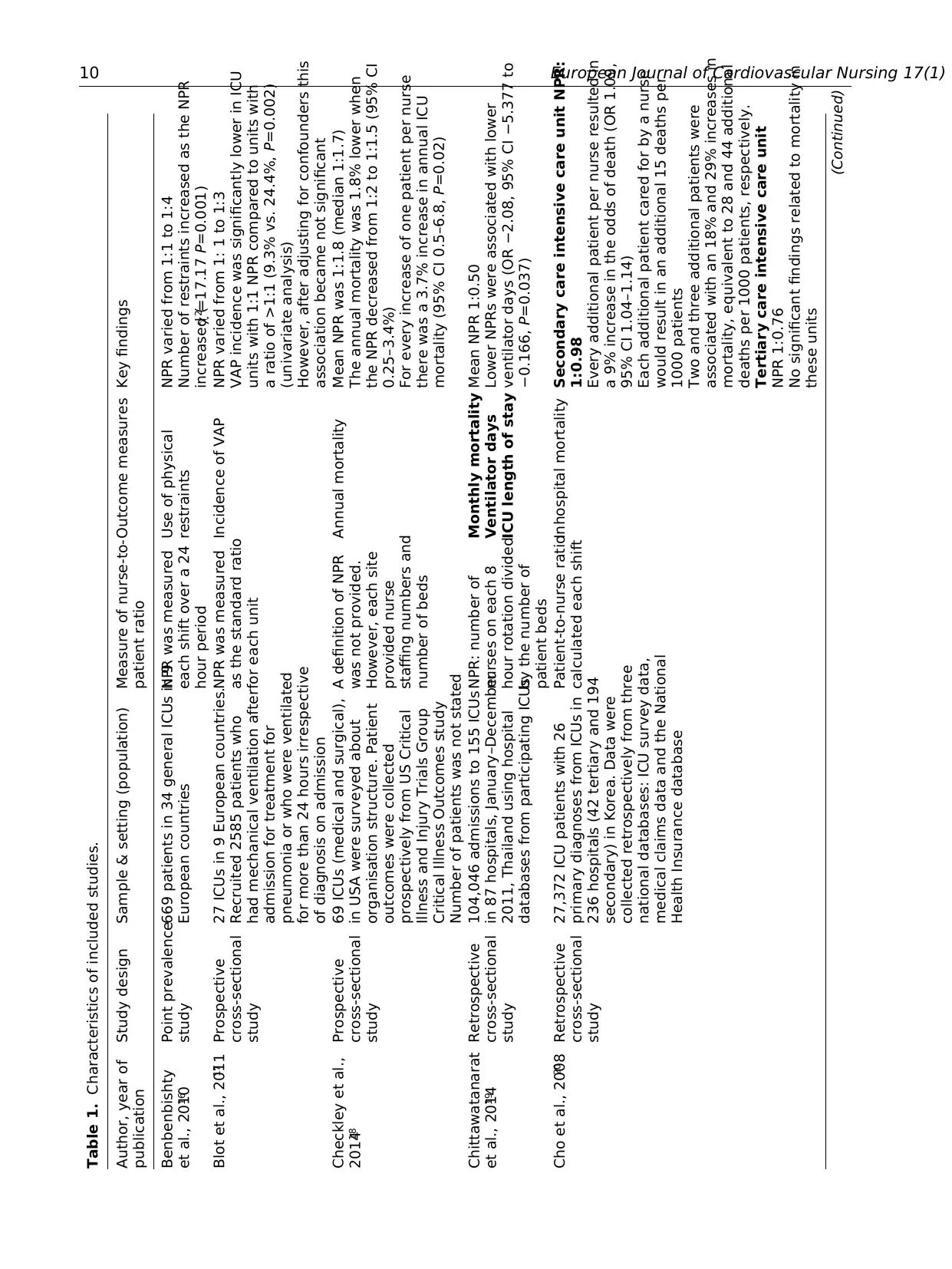
Table 1. Characteristics of included studies.
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Benbenbishty
et al., 201016
Point prevalence
study
669 patients in 34 general ICUs in 9
European countries
NPR was measured
each shift over a 24
hour period
Use of physical
restraints
NPR varied from 1:1 to 1:4
Number of restraints increased as the NPR
increased (χ2=17.17 P=0.001)
Blot et al., 201117 Prospective
cross-sectional
study
27 ICUs in 9 European countries.
Recruited 2585 patients who
had mechanical ventilation after
admission for treatment for
pneumonia or who were ventilated
for more than 24 hours irrespective
of diagnosis on admission
NPR was measured
as the standard ratio
for each unit
Incidence of VAP NPR varied from 1: 1 to 1:3
VAP incidence was significantly lower in ICU
units with 1:1 NPR compared to units with
a ratio of >1:1 (9.3% vs. 24.4%, P=0.002)
(univariate analysis)
However, after adjusting for confounders this
association became not significant
Checkley et al.,
201418
Prospective
cross-sectional
study
69 ICUs (medical and surgical),
in USA were surveyed about
organisation structure. Patient
outcomes were collected
prospectively from US Critical
Illness and Injury Trials Group
Critical Illness Outcomes study
Number of patients was not stated
A definition of NPR
was not provided.
However, each site
provided nurse
staffing numbers and
number of beds
Annual mortality Mean NPR was 1:1.8 (median 1:1.7)
The annual mortality was 1.8% lower when
the NPR decreased from 1:2 to 1:1.5 (95% CI
0.25–3.4%)
For every increase of one patient per nurse
there was a 3.7% increase in annual ICU
mortality (95% CI 0.5–6.8, P=0.02)
Chittawatanarat
et al., 201419
Retrospective
cross-sectional
study
104,046 admissions to 155 ICUs
in 87 hospitals, January–December
2011, Thailand using hospital
databases from participating ICUs
NPR: number of
nurses on each 8
hour rotation divided
by the number of
patient beds
Monthly mortality
Ventilator days
ICU length of stay
Mean NPR 1:0.50
Lower NPRs were associated with lower
ventilator days (OR −2.08, 95% CI −5.377 to
−0.166, P=0.037)
Cho et al., 200820 Retrospective
cross-sectional
study
27,372 ICU patients with 26
primary diagnoses from ICUs in
236 hospitals (42 tertiary and 194
secondary) in Korea. Data were
collected retrospectively from three
national databases: ICU survey data,
medical claims data and the National
Health Insurance database
Patient-to-nurse ratio
calculated each shift
Inhospital mortality Secondary care intensive care unit NPR:
1:0.98
Every additional patient per nurse resulted in
a 9% increase in the odds of death (OR 1.09,
95% CI 1.04–1.14)
Each additional patient cared for by a nurse
would result in an additional 15 deaths per
1000 patients
Two and three additional patients were
associated with an 18% and 29% increases in
mortality, equivalent to 28 and 44 additional
deaths per 1000 patients, respectively.
Tertiary care intensive care unit
NPR 1:0.76
No significant findings related to mortality in
these units
(Continued)
Table 1. Characteristics of included studies.
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Benbenbishty
et al., 201016
Point prevalence
study
669 patients in 34 general ICUs in 9
European countries
NPR was measured
each shift over a 24
hour period
Use of physical
restraints
NPR varied from 1:1 to 1:4
Number of restraints increased as the NPR
increased (χ2=17.17 P=0.001)
Blot et al., 201117 Prospective
cross-sectional
study
27 ICUs in 9 European countries.
Recruited 2585 patients who
had mechanical ventilation after
admission for treatment for
pneumonia or who were ventilated
for more than 24 hours irrespective
of diagnosis on admission
NPR was measured
as the standard ratio
for each unit
Incidence of VAP NPR varied from 1: 1 to 1:3
VAP incidence was significantly lower in ICU
units with 1:1 NPR compared to units with
a ratio of >1:1 (9.3% vs. 24.4%, P=0.002)
(univariate analysis)
However, after adjusting for confounders this
association became not significant
Checkley et al.,
201418
Prospective
cross-sectional
study
69 ICUs (medical and surgical),
in USA were surveyed about
organisation structure. Patient
outcomes were collected
prospectively from US Critical
Illness and Injury Trials Group
Critical Illness Outcomes study
Number of patients was not stated
A definition of NPR
was not provided.
However, each site
provided nurse
staffing numbers and
number of beds
Annual mortality Mean NPR was 1:1.8 (median 1:1.7)
The annual mortality was 1.8% lower when
the NPR decreased from 1:2 to 1:1.5 (95% CI
0.25–3.4%)
For every increase of one patient per nurse
there was a 3.7% increase in annual ICU
mortality (95% CI 0.5–6.8, P=0.02)
Chittawatanarat
et al., 201419
Retrospective
cross-sectional
study
104,046 admissions to 155 ICUs
in 87 hospitals, January–December
2011, Thailand using hospital
databases from participating ICUs
NPR: number of
nurses on each 8
hour rotation divided
by the number of
patient beds
Monthly mortality
Ventilator days
ICU length of stay
Mean NPR 1:0.50
Lower NPRs were associated with lower
ventilator days (OR −2.08, 95% CI −5.377 to
−0.166, P=0.037)
Cho et al., 200820 Retrospective
cross-sectional
study
27,372 ICU patients with 26
primary diagnoses from ICUs in
236 hospitals (42 tertiary and 194
secondary) in Korea. Data were
collected retrospectively from three
national databases: ICU survey data,
medical claims data and the National
Health Insurance database
Patient-to-nurse ratio
calculated each shift
Inhospital mortality Secondary care intensive care unit NPR:
1:0.98
Every additional patient per nurse resulted in
a 9% increase in the odds of death (OR 1.09,
95% CI 1.04–1.14)
Each additional patient cared for by a nurse
would result in an additional 15 deaths per
1000 patients
Two and three additional patients were
associated with an 18% and 29% increases in
mortality, equivalent to 28 and 44 additional
deaths per 1000 patients, respectively.
Tertiary care intensive care unit
NPR 1:0.76
No significant findings related to mortality in
these units
(Continued)
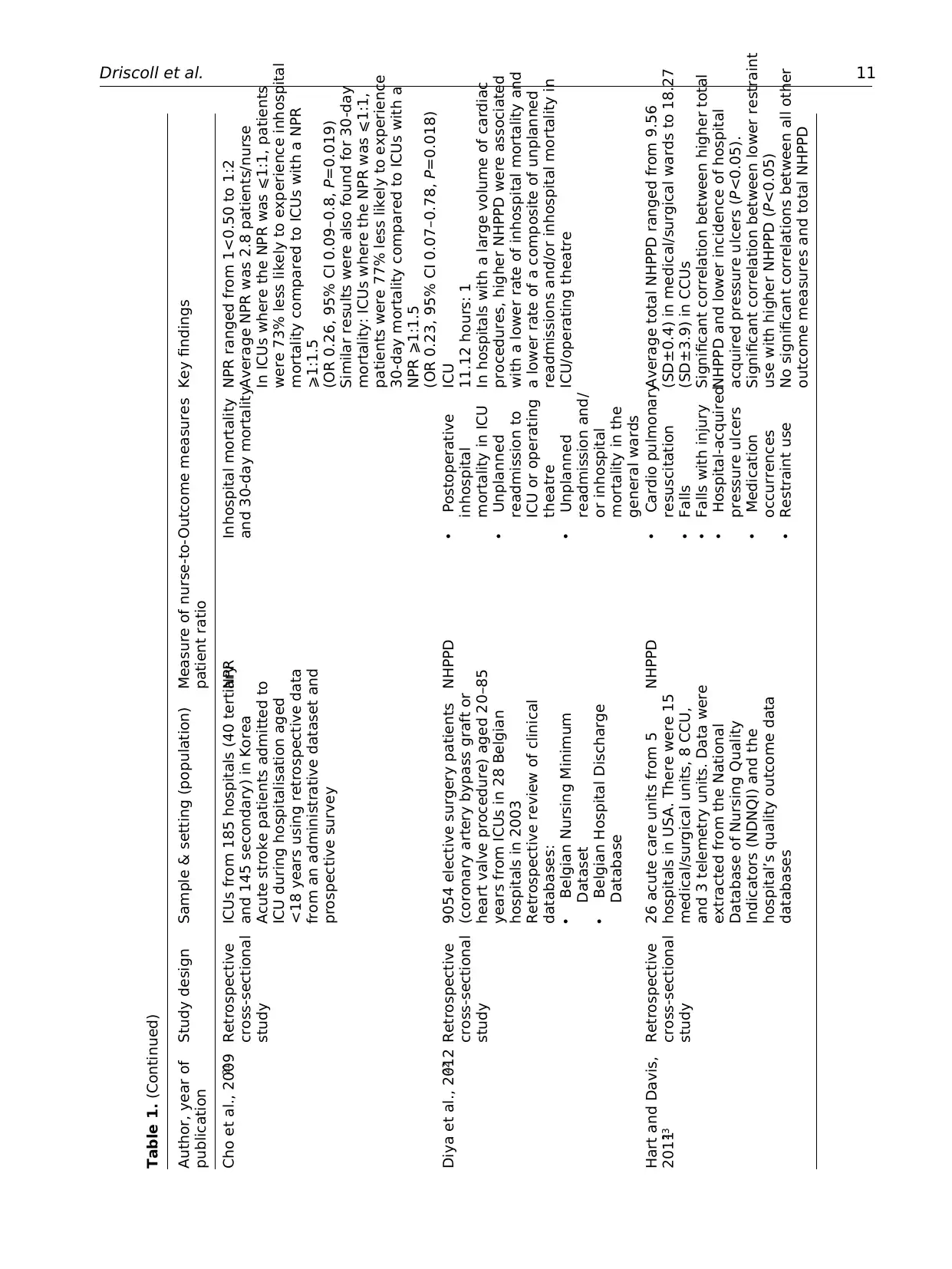
Driscoll et al. 11
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Cho et al., 200921 Retrospective
cross-sectional
study
ICUs from 185 hospitals (40 tertiary
and 145 secondary) in Korea
Acute stroke patients admitted to
ICU during hospitalisation aged
<18 years using retrospective data
from an administrative dataset and
prospective survey
NPR Inhospital mortality
and 30-day mortality
NPR ranged from 1<0.50 to 1:2
Average NPR was 2.8 patients/nurse
In ICUs where the NPR was ⩽1:1, patients
were 73% less likely to experience inhospital
mortality compared to ICUs with a NPR
⩾1:1.5
(OR 0.26, 95% CI 0.09–0.8, P=0.019)
Similar results were also found for 30-day
mortality: ICUs where the NPR was ⩽1:1,
patients were 77% less likely to experience
30-day mortality compared to ICUs with a
NPR ⩾1:1.5
(OR 0.23, 95% CI 0.07–0.78, P=0.018)
Diya et al., 201222 Retrospective
cross-sectional
study
9054 elective surgery patients
(coronary artery bypass graft or
heart valve procedure) aged 20–85
years from ICUs in 28 Belgian
hospitals in 2003
Retrospective review of clinical
databases:
• Belgian Nursing Minimum
Dataset
• Belgian Hospital Discharge
Database
NHPPD • Postoperative
inhospital
mortality in ICU
• Unplanned
readmission to
ICU or operating
theatre
• Unplanned
readmission and/
or inhospital
mortality in the
general wards
ICU
11.12 hours: 1
In hospitals with a large volume of cardiac
procedures, higher NHPPD were associated
with a lower rate of inhospital mortality and
a lower rate of a composite of unplanned
readmissions and/or inhospital mortality in
ICU/operating theatre
Hart and Davis,
201123
Retrospective
cross-sectional
study
26 acute care units from 5
hospitals in USA. There were 15
medical/surgical units, 8 CCU,
and 3 telemetry units. Data were
extracted from the National
Database of Nursing Quality
Indicators (NDNQI) and the
hospital’s quality outcome data
databases
NHPPD • Cardio pulmonary
resuscitation
• Falls
• Falls with injury
• Hospital-acquired
pressure ulcers
• Medication
occurrences
• Restraint use
Average total NHPPD ranged from 9.56
(SD±0.4) in medical/surgical wards to 18.27
(SD±3.9) in CCUs
Significant correlation between higher total
NHPPD and lower incidence of hospital
acquired pressure ulcers (P<0.05).
Significant correlation between lower restraint
use with higher NHPPD (P<0.05)
No significant correlations between all other
outcome measures and total NHPPD
Table 1. (Continued)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Cho et al., 200921 Retrospective
cross-sectional
study
ICUs from 185 hospitals (40 tertiary
and 145 secondary) in Korea
Acute stroke patients admitted to
ICU during hospitalisation aged
<18 years using retrospective data
from an administrative dataset and
prospective survey
NPR Inhospital mortality
and 30-day mortality
NPR ranged from 1<0.50 to 1:2
Average NPR was 2.8 patients/nurse
In ICUs where the NPR was ⩽1:1, patients
were 73% less likely to experience inhospital
mortality compared to ICUs with a NPR
⩾1:1.5
(OR 0.26, 95% CI 0.09–0.8, P=0.019)
Similar results were also found for 30-day
mortality: ICUs where the NPR was ⩽1:1,
patients were 77% less likely to experience
30-day mortality compared to ICUs with a
NPR ⩾1:1.5
(OR 0.23, 95% CI 0.07–0.78, P=0.018)
Diya et al., 201222 Retrospective
cross-sectional
study
9054 elective surgery patients
(coronary artery bypass graft or
heart valve procedure) aged 20–85
years from ICUs in 28 Belgian
hospitals in 2003
Retrospective review of clinical
databases:
• Belgian Nursing Minimum
Dataset
• Belgian Hospital Discharge
Database
NHPPD • Postoperative
inhospital
mortality in ICU
• Unplanned
readmission to
ICU or operating
theatre
• Unplanned
readmission and/
or inhospital
mortality in the
general wards
ICU
11.12 hours: 1
In hospitals with a large volume of cardiac
procedures, higher NHPPD were associated
with a lower rate of inhospital mortality and
a lower rate of a composite of unplanned
readmissions and/or inhospital mortality in
ICU/operating theatre
Hart and Davis,
201123
Retrospective
cross-sectional
study
26 acute care units from 5
hospitals in USA. There were 15
medical/surgical units, 8 CCU,
and 3 telemetry units. Data were
extracted from the National
Database of Nursing Quality
Indicators (NDNQI) and the
hospital’s quality outcome data
databases
NHPPD • Cardio pulmonary
resuscitation
• Falls
• Falls with injury
• Hospital-acquired
pressure ulcers
• Medication
occurrences
• Restraint use
Average total NHPPD ranged from 9.56
(SD±0.4) in medical/surgical wards to 18.27
(SD±3.9) in CCUs
Significant correlation between higher total
NHPPD and lower incidence of hospital
acquired pressure ulcers (P<0.05).
Significant correlation between lower restraint
use with higher NHPPD (P<0.05)
No significant correlations between all other
outcome measures and total NHPPD
Table 1. (Continued)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
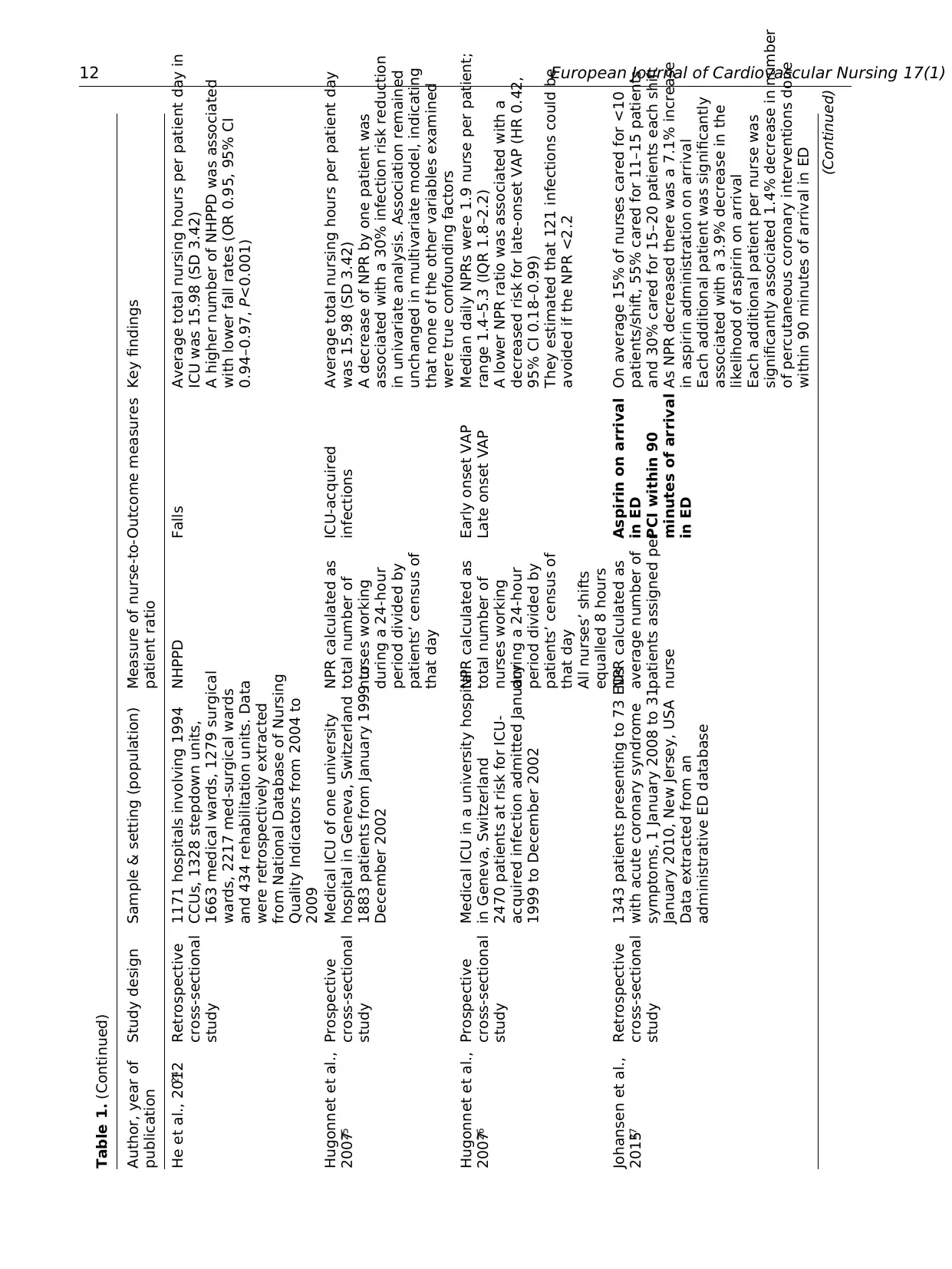
12 European Journal of Cardiovascular Nursing 17(1)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
He et al., 201224 Retrospective
cross-sectional
study
1171 hospitals involving 1994
CCUs, 1328 stepdown units,
1663 medical wards, 1279 surgical
wards, 2217 med-surgical wards
and 434 rehabilitation units. Data
were retrospectively extracted
from National Database of Nursing
Quality Indicators from 2004 to
2009
NHPPD Falls Average total nursing hours per patient day in
ICU was 15.98 (SD 3.42)
A higher number of NHPPD was associated
with lower fall rates (OR 0.95, 95% CI
0.94–0.97, P<0.001)
Hugonnet et al.,
200725
Prospective
cross-sectional
study
Medical ICU of one university
hospital in Geneva, Switzerland
1883 patients from January 1999 to
December 2002
NPR calculated as
total number of
nurses working
during a 24-hour
period divided by
patients’ census of
that day
ICU-acquired
infections
Average total nursing hours per patient day
was 15.98 (SD 3.42)
A decrease of NPR by one patient was
associated with a 30% infection risk reduction
in univariate analysis. Association remained
unchanged in multivariate model, indicating
that none of the other variables examined
were true confounding factors
Hugonnet et al.,
200726
Prospective
cross-sectional
study
Medical ICU in a university hospital
in Geneva, Switzerland
2470 patients at risk for ICU-
acquired infection admitted January
1999 to December 2002
NPR calculated as
total number of
nurses working
during a 24-hour
period divided by
patients’ census of
that day
All nurses’ shifts
equalled 8 hours
Early onset VAP
Late onset VAP
Median daily NPRs were 1.9 nurse per patient;
range 1.4–5.3 (IQR 1.8–2.2)
A lower NPR ratio was associated with a
decreased risk for late-onset VAP (HR 0.42,
95% CI 0.18–0.99)
They estimated that 121 infections could be
avoided if the NPR <2.2
Johansen et al.,
201527
Retrospective
cross-sectional
study
1343 patients presenting to 73 EDs
with acute coronary syndrome
symptoms, 1 January 2008 to 31
January 2010, New Jersey, USA
Data extracted from an
administrative ED database
NPR calculated as
average number of
patients assigned per
nurse
Aspirin on arrival
in ED
PCI within 90
minutes of arrival
in ED
On average 15% of nurses cared for <10
patients/shift, 55% cared for 11–15 patients
and 30% cared for 15–20 patients each shift
As NPR decreased there was a 7.1% increase
in aspirin administration on arrival
Each additional patient was significantly
associated with a 3.9% decrease in the
likelihood of aspirin on arrival
Each additional patient per nurse was
significantly associated 1.4% decrease in number
of percutaneous coronary interventions done
within 90 minutes of arrival in ED
(Continued)
Table 1. (Continued)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
He et al., 201224 Retrospective
cross-sectional
study
1171 hospitals involving 1994
CCUs, 1328 stepdown units,
1663 medical wards, 1279 surgical
wards, 2217 med-surgical wards
and 434 rehabilitation units. Data
were retrospectively extracted
from National Database of Nursing
Quality Indicators from 2004 to
2009
NHPPD Falls Average total nursing hours per patient day in
ICU was 15.98 (SD 3.42)
A higher number of NHPPD was associated
with lower fall rates (OR 0.95, 95% CI
0.94–0.97, P<0.001)
Hugonnet et al.,
200725
Prospective
cross-sectional
study
Medical ICU of one university
hospital in Geneva, Switzerland
1883 patients from January 1999 to
December 2002
NPR calculated as
total number of
nurses working
during a 24-hour
period divided by
patients’ census of
that day
ICU-acquired
infections
Average total nursing hours per patient day
was 15.98 (SD 3.42)
A decrease of NPR by one patient was
associated with a 30% infection risk reduction
in univariate analysis. Association remained
unchanged in multivariate model, indicating
that none of the other variables examined
were true confounding factors
Hugonnet et al.,
200726
Prospective
cross-sectional
study
Medical ICU in a university hospital
in Geneva, Switzerland
2470 patients at risk for ICU-
acquired infection admitted January
1999 to December 2002
NPR calculated as
total number of
nurses working
during a 24-hour
period divided by
patients’ census of
that day
All nurses’ shifts
equalled 8 hours
Early onset VAP
Late onset VAP
Median daily NPRs were 1.9 nurse per patient;
range 1.4–5.3 (IQR 1.8–2.2)
A lower NPR ratio was associated with a
decreased risk for late-onset VAP (HR 0.42,
95% CI 0.18–0.99)
They estimated that 121 infections could be
avoided if the NPR <2.2
Johansen et al.,
201527
Retrospective
cross-sectional
study
1343 patients presenting to 73 EDs
with acute coronary syndrome
symptoms, 1 January 2008 to 31
January 2010, New Jersey, USA
Data extracted from an
administrative ED database
NPR calculated as
average number of
patients assigned per
nurse
Aspirin on arrival
in ED
PCI within 90
minutes of arrival
in ED
On average 15% of nurses cared for <10
patients/shift, 55% cared for 11–15 patients
and 30% cared for 15–20 patients each shift
As NPR decreased there was a 7.1% increase
in aspirin administration on arrival
Each additional patient was significantly
associated with a 3.9% decrease in the
likelihood of aspirin on arrival
Each additional patient per nurse was
significantly associated 1.4% decrease in number
of percutaneous coronary interventions done
within 90 minutes of arrival in ED
(Continued)
Table 1. (Continued)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
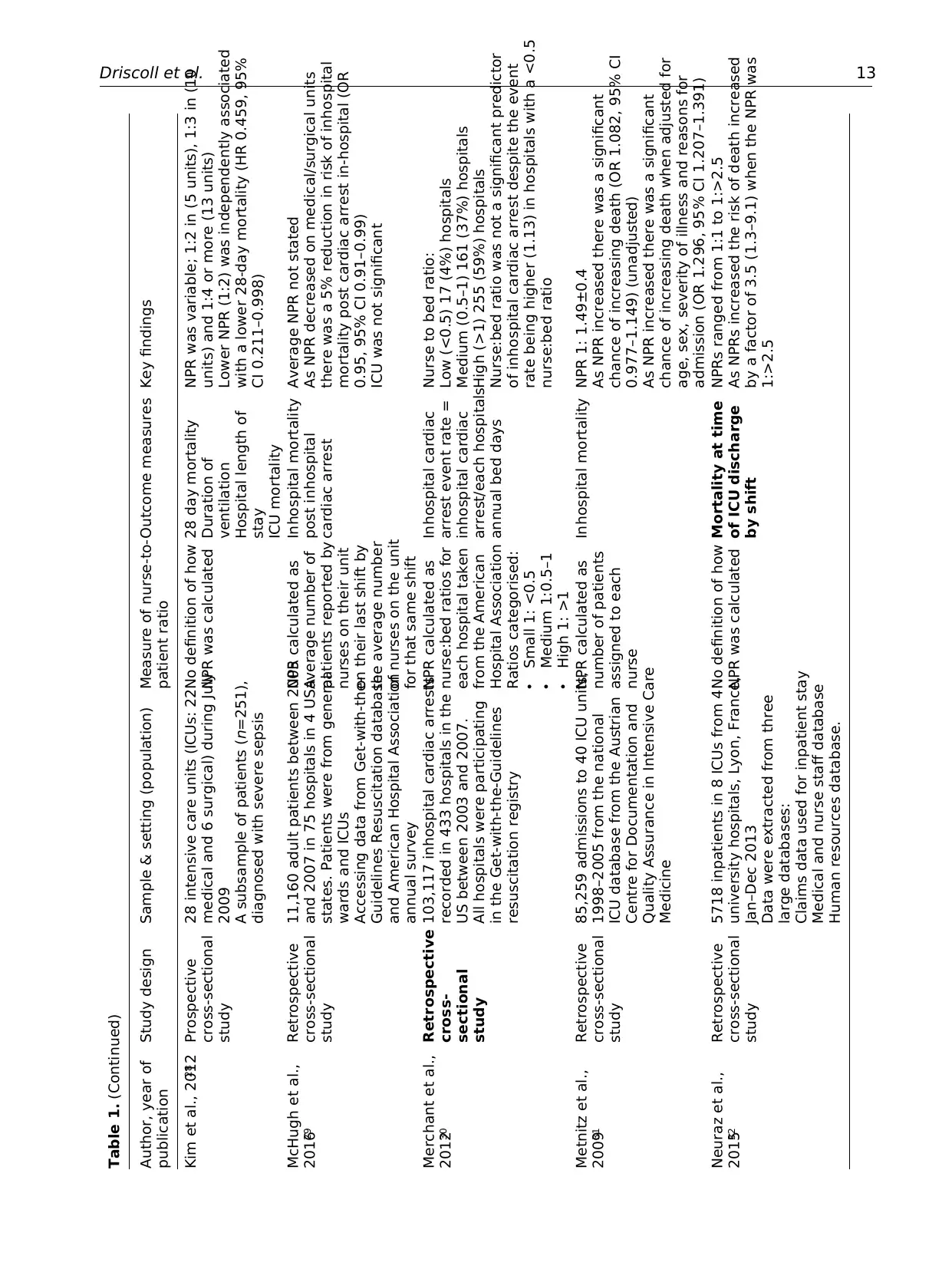
Driscoll et al. 13
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Kim et al., 201228 Prospective
cross-sectional
study
28 intensive care units (ICUs: 22
medical and 6 surgical) during July
2009
A subsample of patients (n=251),
diagnosed with severe sepsis
No definition of how
NPR was calculated
28 day mortality
Duration of
ventilation
Hospital length of
stay
ICU mortality
NPR was variable; 1:2 in (5 units), 1:3 in (10
units) and 1:4 or more (13 units)
Lower NPR (1:2) was independently associated
with a lower 28-day mortality (HR 0.459, 95%
CI 0.211–0.998)
McHugh et al.,
201629
Retrospective
cross-sectional
study
11,160 adult patients between 2005
and 2007 in 75 hospitals in 4 USA
states. Patients were from general
wards and ICUs
Accessing data from Get-with-the-
Guidelines Resuscitation database
and American Hospital Association
annual survey
NPR calculated as
average number of
patients reported by
nurses on their unit
on their last shift by
the average number
of nurses on the unit
for that same shift
Inhospital mortality
post inhospital
cardiac arrest
Average NPR not stated
As NPR decreased on medical/surgical units
there was a 5% reduction in risk of inhospital
mortality post cardiac arrest in-hospital (OR
0.95, 95% CI 0.91–0.99)
ICU was not significant
Merchant et al.,
201230
Retrospective
cross-
sectional
study
103,117 inhospital cardiac arrests
recorded in 433 hospitals in the
US between 2003 and 2007.
All hospitals were participating
in the Get-with-the-Guidelines
resuscitation registry
NPR calculated as
nurse:bed ratios for
each hospital taken
from the American
Hospital Association
Ratios categorised:
• Small 1: <0.5
• Medium 1:0.5–1
• High 1: >1
Inhospital cardiac
arrest event rate =
inhospital cardiac
arrest/each hospitals
annual bed days
Nurse to bed ratio:
Low (<0.5) 17 (4%) hospitals
Medium (0.5–1) 161 (37%) hospitals
High (>1) 255 (59%) hospitals
Nurse:bed ratio was not a significant predictor
of inhospital cardiac arrest despite the event
rate being higher (1.13) in hospitals with a <0.5
nurse:bed ratio
Metnitz et al.,
200931
Retrospective
cross-sectional
study
85,259 admissions to 40 ICU units,
1998–2005 from the national
ICU database from the Austrian
Centre for Documentation and
Quality Assurance in Intensive Care
Medicine
NPR calculated as
number of patients
assigned to each
nurse
Inhospital mortality NPR 1: 1.49±0.4
As NPR increased there was a significant
chance of increasing death (OR 1.082, 95% CI
0.977–1.149) (unadjusted)
As NPR increased there was a significant
chance of increasing death when adjusted for
age, sex, severity of illness and reasons for
admission (OR 1.296, 95% CI 1.207–1.391)
Neuraz et al.,
201532
Retrospective
cross-sectional
study
5718 inpatients in 8 ICUs from 4
university hospitals, Lyon, France,
Jan–Dec 2013
Data were extracted from three
large databases:
Claims data used for inpatient stay
Medical and nurse staff database
Human resources database.
No definition of how
NPR was calculated
Mortality at time
of ICU discharge
by shift
NPRs ranged from 1:1 to 1:>2.5
As NPRs increased the risk of death increased
by a factor of 3.5 (1.3–9.1) when the NPR was
1:>2.5
Table 1. (Continued)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Kim et al., 201228 Prospective
cross-sectional
study
28 intensive care units (ICUs: 22
medical and 6 surgical) during July
2009
A subsample of patients (n=251),
diagnosed with severe sepsis
No definition of how
NPR was calculated
28 day mortality
Duration of
ventilation
Hospital length of
stay
ICU mortality
NPR was variable; 1:2 in (5 units), 1:3 in (10
units) and 1:4 or more (13 units)
Lower NPR (1:2) was independently associated
with a lower 28-day mortality (HR 0.459, 95%
CI 0.211–0.998)
McHugh et al.,
201629
Retrospective
cross-sectional
study
11,160 adult patients between 2005
and 2007 in 75 hospitals in 4 USA
states. Patients were from general
wards and ICUs
Accessing data from Get-with-the-
Guidelines Resuscitation database
and American Hospital Association
annual survey
NPR calculated as
average number of
patients reported by
nurses on their unit
on their last shift by
the average number
of nurses on the unit
for that same shift
Inhospital mortality
post inhospital
cardiac arrest
Average NPR not stated
As NPR decreased on medical/surgical units
there was a 5% reduction in risk of inhospital
mortality post cardiac arrest in-hospital (OR
0.95, 95% CI 0.91–0.99)
ICU was not significant
Merchant et al.,
201230
Retrospective
cross-
sectional
study
103,117 inhospital cardiac arrests
recorded in 433 hospitals in the
US between 2003 and 2007.
All hospitals were participating
in the Get-with-the-Guidelines
resuscitation registry
NPR calculated as
nurse:bed ratios for
each hospital taken
from the American
Hospital Association
Ratios categorised:
• Small 1: <0.5
• Medium 1:0.5–1
• High 1: >1
Inhospital cardiac
arrest event rate =
inhospital cardiac
arrest/each hospitals
annual bed days
Nurse to bed ratio:
Low (<0.5) 17 (4%) hospitals
Medium (0.5–1) 161 (37%) hospitals
High (>1) 255 (59%) hospitals
Nurse:bed ratio was not a significant predictor
of inhospital cardiac arrest despite the event
rate being higher (1.13) in hospitals with a <0.5
nurse:bed ratio
Metnitz et al.,
200931
Retrospective
cross-sectional
study
85,259 admissions to 40 ICU units,
1998–2005 from the national
ICU database from the Austrian
Centre for Documentation and
Quality Assurance in Intensive Care
Medicine
NPR calculated as
number of patients
assigned to each
nurse
Inhospital mortality NPR 1: 1.49±0.4
As NPR increased there was a significant
chance of increasing death (OR 1.082, 95% CI
0.977–1.149) (unadjusted)
As NPR increased there was a significant
chance of increasing death when adjusted for
age, sex, severity of illness and reasons for
admission (OR 1.296, 95% CI 1.207–1.391)
Neuraz et al.,
201532
Retrospective
cross-sectional
study
5718 inpatients in 8 ICUs from 4
university hospitals, Lyon, France,
Jan–Dec 2013
Data were extracted from three
large databases:
Claims data used for inpatient stay
Medical and nurse staff database
Human resources database.
No definition of how
NPR was calculated
Mortality at time
of ICU discharge
by shift
NPRs ranged from 1:1 to 1:>2.5
As NPRs increased the risk of death increased
by a factor of 3.5 (1.3–9.1) when the NPR was
1:>2.5
Table 1. (Continued)
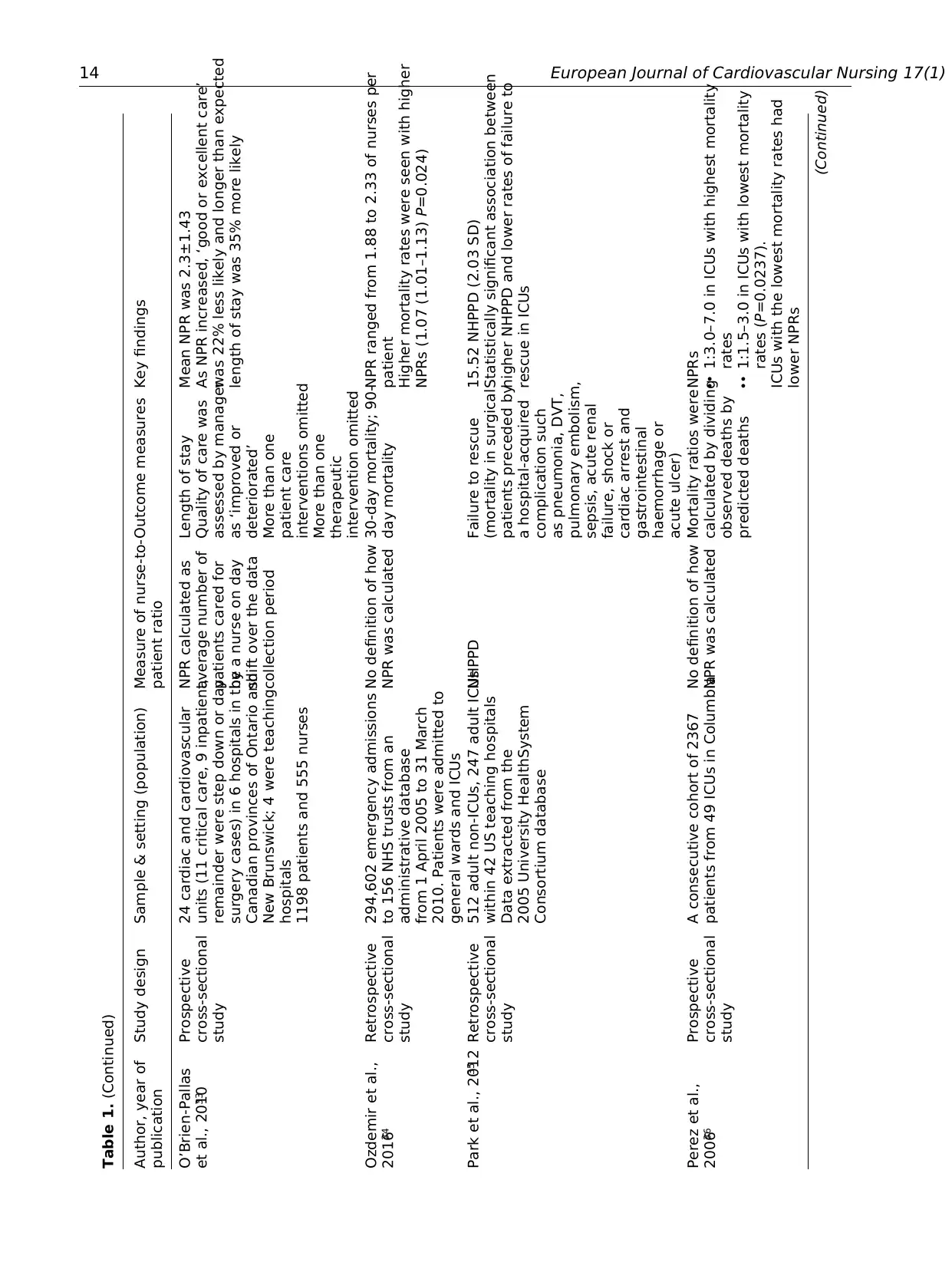
14 European Journal of Cardiovascular Nursing 17(1)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
O’Brien-Pallas
et al., 201033
Prospective
cross-sectional
study
24 cardiac and cardiovascular
units (11 critical care, 9 inpatient,
remainder were step down or day
surgery cases) in 6 hospitals in the
Canadian provinces of Ontario and
New Brunswick; 4 were teaching
hospitals
1198 patients and 555 nurses
NPR calculated as
average number of
patients cared for
by a nurse on day
shift over the data
collection period
Length of stay
Quality of care was
assessed by manager
as ‘improved or
deteriorated’
More than one
patient care
interventions omitted
More than one
therapeutic
intervention omitted
Mean NPR was 2.3±1.43
As NPR increased, ‘good or excellent care’
was 22% less likely and longer than expected
length of stay was 35% more likely
Ozdemir et al.,
201634
Retrospective
cross-sectional
study
294,602 emergency admissions
to 156 NHS trusts from an
administrative database
from 1 April 2005 to 31 March
2010. Patients were admitted to
general wards and ICUs
No definition of how
NPR was calculated
30-day mortality; 90-
day mortality
NPR ranged from 1.88 to 2.33 of nurses per
patient
Higher mortality rates were seen with higher
NPRs (1.07 (1.01–1.13) P=0.024)
Park et al., 201235 Retrospective
cross-sectional
study
512 adult non-ICUs, 247 adult ICUs
within 42 US teaching hospitals
Data extracted from the
2005 University HealthSystem
Consortium database
NHPPD Failure to rescue
(mortality in surgical
patients preceded by
a hospital-acquired
complication such
as pneumonia, DVT,
pulmonary embolism,
sepsis, acute renal
failure, shock or
cardiac arrest and
gastrointestinal
haemorrhage or
acute ulcer)
15.52 NHPPD (2.03 SD)
Statistically significant association between
higher NHPPD and lower rates of failure to
rescue in ICUs
Perez et al.,
200636
Prospective
cross-sectional
study
A consecutive cohort of 2367
patients from 49 ICUs in Columbia
No definition of how
NPR was calculated
Mortality ratios were
calculated by dividing
observed deaths by
predicted deaths
NPRs
•• 1:3.0–7.0 in ICUs with highest mortality
rates
•• 1:1.5–3.0 in ICUs with lowest mortality
rates (P=0.0237).
ICUs with the lowest mortality rates had
lower NPRs
(Continued)
Table 1. (Continued)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
O’Brien-Pallas
et al., 201033
Prospective
cross-sectional
study
24 cardiac and cardiovascular
units (11 critical care, 9 inpatient,
remainder were step down or day
surgery cases) in 6 hospitals in the
Canadian provinces of Ontario and
New Brunswick; 4 were teaching
hospitals
1198 patients and 555 nurses
NPR calculated as
average number of
patients cared for
by a nurse on day
shift over the data
collection period
Length of stay
Quality of care was
assessed by manager
as ‘improved or
deteriorated’
More than one
patient care
interventions omitted
More than one
therapeutic
intervention omitted
Mean NPR was 2.3±1.43
As NPR increased, ‘good or excellent care’
was 22% less likely and longer than expected
length of stay was 35% more likely
Ozdemir et al.,
201634
Retrospective
cross-sectional
study
294,602 emergency admissions
to 156 NHS trusts from an
administrative database
from 1 April 2005 to 31 March
2010. Patients were admitted to
general wards and ICUs
No definition of how
NPR was calculated
30-day mortality; 90-
day mortality
NPR ranged from 1.88 to 2.33 of nurses per
patient
Higher mortality rates were seen with higher
NPRs (1.07 (1.01–1.13) P=0.024)
Park et al., 201235 Retrospective
cross-sectional
study
512 adult non-ICUs, 247 adult ICUs
within 42 US teaching hospitals
Data extracted from the
2005 University HealthSystem
Consortium database
NHPPD Failure to rescue
(mortality in surgical
patients preceded by
a hospital-acquired
complication such
as pneumonia, DVT,
pulmonary embolism,
sepsis, acute renal
failure, shock or
cardiac arrest and
gastrointestinal
haemorrhage or
acute ulcer)
15.52 NHPPD (2.03 SD)
Statistically significant association between
higher NHPPD and lower rates of failure to
rescue in ICUs
Perez et al.,
200636
Prospective
cross-sectional
study
A consecutive cohort of 2367
patients from 49 ICUs in Columbia
No definition of how
NPR was calculated
Mortality ratios were
calculated by dividing
observed deaths by
predicted deaths
NPRs
•• 1:3.0–7.0 in ICUs with highest mortality
rates
•• 1:1.5–3.0 in ICUs with lowest mortality
rates (P=0.0237).
ICUs with the lowest mortality rates had
lower NPRs
(Continued)
Table 1. (Continued)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Driscoll et al. 15
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Sakr et al., 201537 Point prevalence
study
13796 adults in 1265 ICU in 75
countries on 7 May 2007
NPR recorded
10:00–11.00 am and
10.00–11.00 pm on
a single day. Number
of nurses working at
the bedside during
these time points and
number of occupied
beds
Inhospital
mortality
Median NPR was 1.6 and interquartile range
from 1.05 to 2.2
NPR <1:1.5 is independently associated with a
lower risk of inhospital death (OR 0.69, 95%
CI 0.53–0.90, P<0.001) compared to NPR >1:2
Schwab et al.,
201238
Prospective
cross-sectional
study
182 ICUs in Germany participated
in 2007 involving 563,177 patient
days
45.5% interdisciplinary
21.4% medical
23.6% surgical
9.3% other specific ICU
NPR calculated as
nurses per day (3 per
shift)/patients per day
Number of patients
per day = number of
patient-days in that
month
Nosocomial device
associated infections:
• number of
ventilator
infections
• number of central
venous catheter
associated
infections per
1000 device days
Median NPR (per shift): 1:1.5 and IQR
1:1.3 -1:1.8
In univariate analysis lower NPRs were
associated with fewer nosocomial infections
(RR 0.42, 95% CI 0.32–0.55)
In multivariate analysis, NPR was not
associated with nocosomial infections
Sheetz et al.,
201639
Retrospective
cross-sectional
study
Patients undergoing colectomy,
pancreatectomy, esophagectomy,
abdominal aortic aneurysm repair,
lower-extremity revascularisation,
or lower extremity amputation.
Data extracted from the Medicare
Provider Analysis and Review
(MEDPAR) file claims data and
American Hospital Association
(AHA) Annual Survey Database from
2007 to 2010. Patients were admitted
to general surgical wards and ICUs
NPR calculated as
nursing full-time
equivalents (FTE) ×
1768/adjusted patient
days
30-day mortality,
major complications,
and failure to rescue
No average NPR was provided
Increasing NPR (range OR 1.02 (1.01–1.03) to
OR 1.14 (1.08–1.20), significantly influenced
failure to rescue rates for all procedures
Shuldham et al.,
200940
Retrospective
cross-sectional
study
25,507 patients who were admitted
to general wards or ICUs in a
tertiary cardiorespiratory NHS
trust in England, April 2006 to end
of March 2007
Wards were grouped into lower
dependency areas and the high
dependency areas (ICU and high
dependency unit). Data were
extracted from the corporate
patient administration system
NHPPD: Overall
number of nursing
hours worked in a
given day, divided
this by the total
number of patient
hours on the ward
or unit for that day
and multiplied by 24
(h), i.e. nurse hours/
patient hours × 24
• Deep vein
thrombosis
• Patient falls
• Pneumonia
• Pressure sores
• Sepsis
• Shock
• Upper GI bleed
No average NHPPD was provided
As the NHPPD decreased so did the risk of
developing shock increase 3-fold (RR 3.48,
95% CI 1.368–6.865, P=0.009)
Table 1. (Continued)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Sakr et al., 201537 Point prevalence
study
13796 adults in 1265 ICU in 75
countries on 7 May 2007
NPR recorded
10:00–11.00 am and
10.00–11.00 pm on
a single day. Number
of nurses working at
the bedside during
these time points and
number of occupied
beds
Inhospital
mortality
Median NPR was 1.6 and interquartile range
from 1.05 to 2.2
NPR <1:1.5 is independently associated with a
lower risk of inhospital death (OR 0.69, 95%
CI 0.53–0.90, P<0.001) compared to NPR >1:2
Schwab et al.,
201238
Prospective
cross-sectional
study
182 ICUs in Germany participated
in 2007 involving 563,177 patient
days
45.5% interdisciplinary
21.4% medical
23.6% surgical
9.3% other specific ICU
NPR calculated as
nurses per day (3 per
shift)/patients per day
Number of patients
per day = number of
patient-days in that
month
Nosocomial device
associated infections:
• number of
ventilator
infections
• number of central
venous catheter
associated
infections per
1000 device days
Median NPR (per shift): 1:1.5 and IQR
1:1.3 -1:1.8
In univariate analysis lower NPRs were
associated with fewer nosocomial infections
(RR 0.42, 95% CI 0.32–0.55)
In multivariate analysis, NPR was not
associated with nocosomial infections
Sheetz et al.,
201639
Retrospective
cross-sectional
study
Patients undergoing colectomy,
pancreatectomy, esophagectomy,
abdominal aortic aneurysm repair,
lower-extremity revascularisation,
or lower extremity amputation.
Data extracted from the Medicare
Provider Analysis and Review
(MEDPAR) file claims data and
American Hospital Association
(AHA) Annual Survey Database from
2007 to 2010. Patients were admitted
to general surgical wards and ICUs
NPR calculated as
nursing full-time
equivalents (FTE) ×
1768/adjusted patient
days
30-day mortality,
major complications,
and failure to rescue
No average NPR was provided
Increasing NPR (range OR 1.02 (1.01–1.03) to
OR 1.14 (1.08–1.20), significantly influenced
failure to rescue rates for all procedures
Shuldham et al.,
200940
Retrospective
cross-sectional
study
25,507 patients who were admitted
to general wards or ICUs in a
tertiary cardiorespiratory NHS
trust in England, April 2006 to end
of March 2007
Wards were grouped into lower
dependency areas and the high
dependency areas (ICU and high
dependency unit). Data were
extracted from the corporate
patient administration system
NHPPD: Overall
number of nursing
hours worked in a
given day, divided
this by the total
number of patient
hours on the ward
or unit for that day
and multiplied by 24
(h), i.e. nurse hours/
patient hours × 24
• Deep vein
thrombosis
• Patient falls
• Pneumonia
• Pressure sores
• Sepsis
• Shock
• Upper GI bleed
No average NHPPD was provided
As the NHPPD decreased so did the risk of
developing shock increase 3-fold (RR 3.48,
95% CI 1.368–6.865, P=0.009)
Table 1. (Continued)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
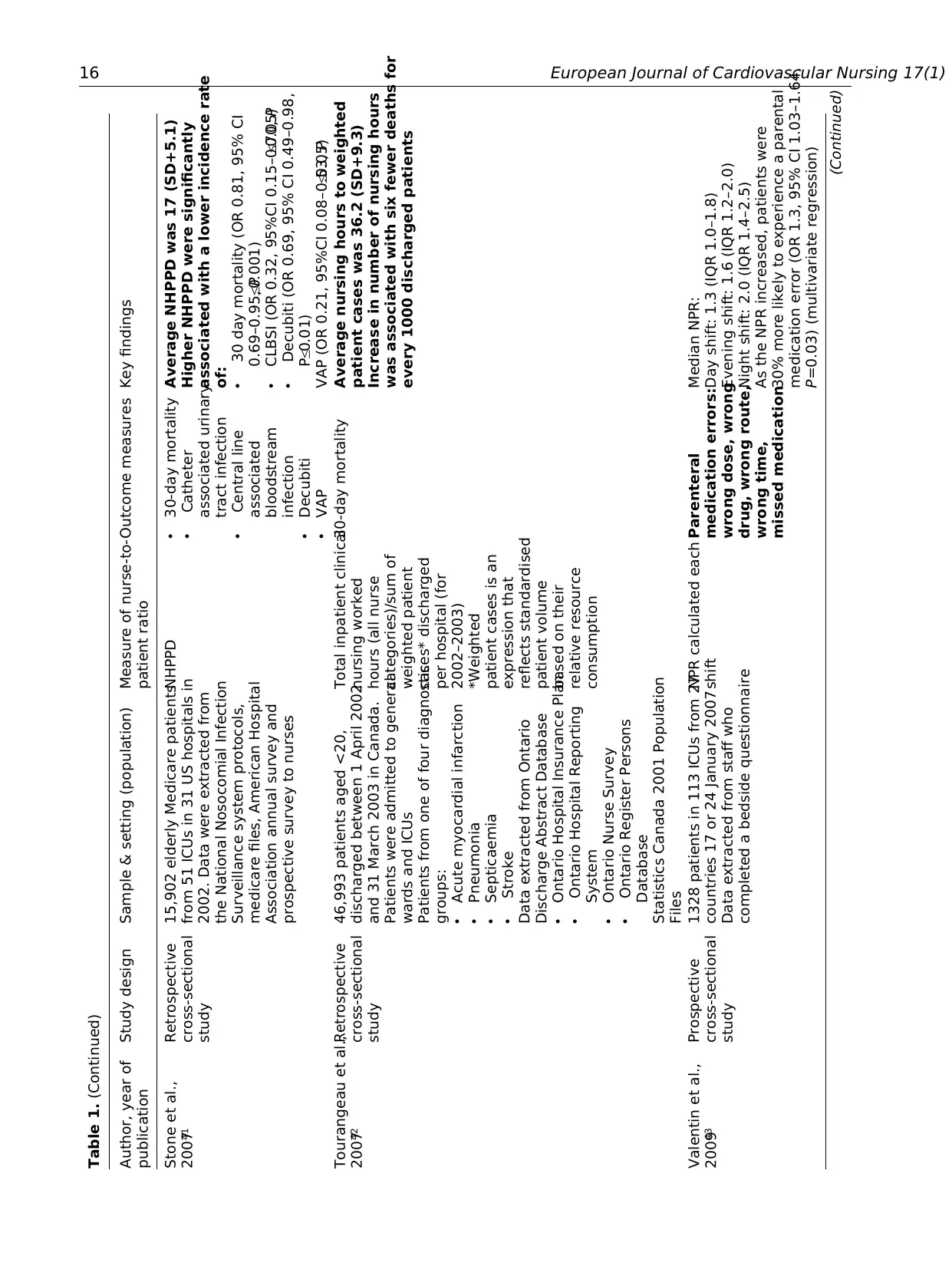
16 European Journal of Cardiovascular Nursing 17(1)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Stone et al.,
200741
Retrospective
cross-sectional
study
15,902 elderly Medicare patients
from 51 ICUs in 31 US hospitals in
2002. Data were extracted from
the National Nosocomial Infection
Surveillance system protocols,
medicare files, American Hospital
Association annual survey and
prospective survey to nurses
NHPPD • 30-day mortality
• Catheter
associated urinary
tract infection
• Central line
associated
bloodstream
infection
• Decubiti
• VAP
Average NHPPD was 17 (SD+5.1)
Higher NHPPD were significantly
associated with a lower incidence rate
of:
• 30 day mortality (OR 0.81, 95% CI
0.69–0.95, P≤0.001)
• CLBSI (OR 0.32, 95%CI 0.15–0.70, P≤0.05)
• Decubiti (OR 0.69, 95% CI 0.49–0.98,
P≤0.01)
VAP (OR 0.21, 95%CI 0.08–0.53, P≤0.05)
Tourangeau et al.,
200742
Retrospective
cross-sectional
study
46,993 patients aged <20,
discharged between 1 April 2002
and 31 March 2003 in Canada.
Patients were admitted to general
wards and ICUs
Patients from one of four diagnostic
groups:
• Acute myocardial infarction
• Pneumonia
• Septicaemia
• Stroke
Data extracted from Ontario
Discharge Abstract Database
• Ontario Hospital Insurance Plan
• Ontario Hospital Reporting
System
• Ontario Nurse Survey
• Ontario Register Persons
Database
Statistics Canada 2001 Population
Files
Total inpatient clinical
nursing worked
hours (all nurse
categories)/sum of
weighted patient
cases* discharged
per hospital (for
2002–2003)
*Weighted
patient cases is an
expression that
reflects standardised
patient volume
based on their
relative resource
consumption
30-day mortality Average nursing hours to weighted
patient cases was 36.2 (SD+9.3)
Increase in number of nursing hours
was associated with six fewer deaths for
every 1000 discharged patients
Valentin et al.,
200943
Prospective
cross-sectional
study
1328 patients in 113 ICUs from 27
countries 17 or 24 January 2007
Data extracted from staff who
completed a bedside questionnaire
NPR calculated each
shift
Parenteral
medication errors:
wrong dose, wrong
drug, wrong route,
wrong time,
missed medication
Median NPR:
Day shift: 1.3 (IQR 1.0–1.8)
Evening shift: 1.6 (IQR 1.2–2.0)
Night shift: 2.0 (IQR 1.4–2.5)
As the NPR increased, patients were
30% more likely to experience a parental
medication error (OR 1.3, 95% CI 1.03–1.64,
P=0.03) (multivariate regression)
(Continued)
Table 1. (Continued)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Stone et al.,
200741
Retrospective
cross-sectional
study
15,902 elderly Medicare patients
from 51 ICUs in 31 US hospitals in
2002. Data were extracted from
the National Nosocomial Infection
Surveillance system protocols,
medicare files, American Hospital
Association annual survey and
prospective survey to nurses
NHPPD • 30-day mortality
• Catheter
associated urinary
tract infection
• Central line
associated
bloodstream
infection
• Decubiti
• VAP
Average NHPPD was 17 (SD+5.1)
Higher NHPPD were significantly
associated with a lower incidence rate
of:
• 30 day mortality (OR 0.81, 95% CI
0.69–0.95, P≤0.001)
• CLBSI (OR 0.32, 95%CI 0.15–0.70, P≤0.05)
• Decubiti (OR 0.69, 95% CI 0.49–0.98,
P≤0.01)
VAP (OR 0.21, 95%CI 0.08–0.53, P≤0.05)
Tourangeau et al.,
200742
Retrospective
cross-sectional
study
46,993 patients aged <20,
discharged between 1 April 2002
and 31 March 2003 in Canada.
Patients were admitted to general
wards and ICUs
Patients from one of four diagnostic
groups:
• Acute myocardial infarction
• Pneumonia
• Septicaemia
• Stroke
Data extracted from Ontario
Discharge Abstract Database
• Ontario Hospital Insurance Plan
• Ontario Hospital Reporting
System
• Ontario Nurse Survey
• Ontario Register Persons
Database
Statistics Canada 2001 Population
Files
Total inpatient clinical
nursing worked
hours (all nurse
categories)/sum of
weighted patient
cases* discharged
per hospital (for
2002–2003)
*Weighted
patient cases is an
expression that
reflects standardised
patient volume
based on their
relative resource
consumption
30-day mortality Average nursing hours to weighted
patient cases was 36.2 (SD+9.3)
Increase in number of nursing hours
was associated with six fewer deaths for
every 1000 discharged patients
Valentin et al.,
200943
Prospective
cross-sectional
study
1328 patients in 113 ICUs from 27
countries 17 or 24 January 2007
Data extracted from staff who
completed a bedside questionnaire
NPR calculated each
shift
Parenteral
medication errors:
wrong dose, wrong
drug, wrong route,
wrong time,
missed medication
Median NPR:
Day shift: 1.3 (IQR 1.0–1.8)
Evening shift: 1.6 (IQR 1.2–2.0)
Night shift: 2.0 (IQR 1.4–2.5)
As the NPR increased, patients were
30% more likely to experience a parental
medication error (OR 1.3, 95% CI 1.03–1.64,
P=0.03) (multivariate regression)
(Continued)
Table 1. (Continued)
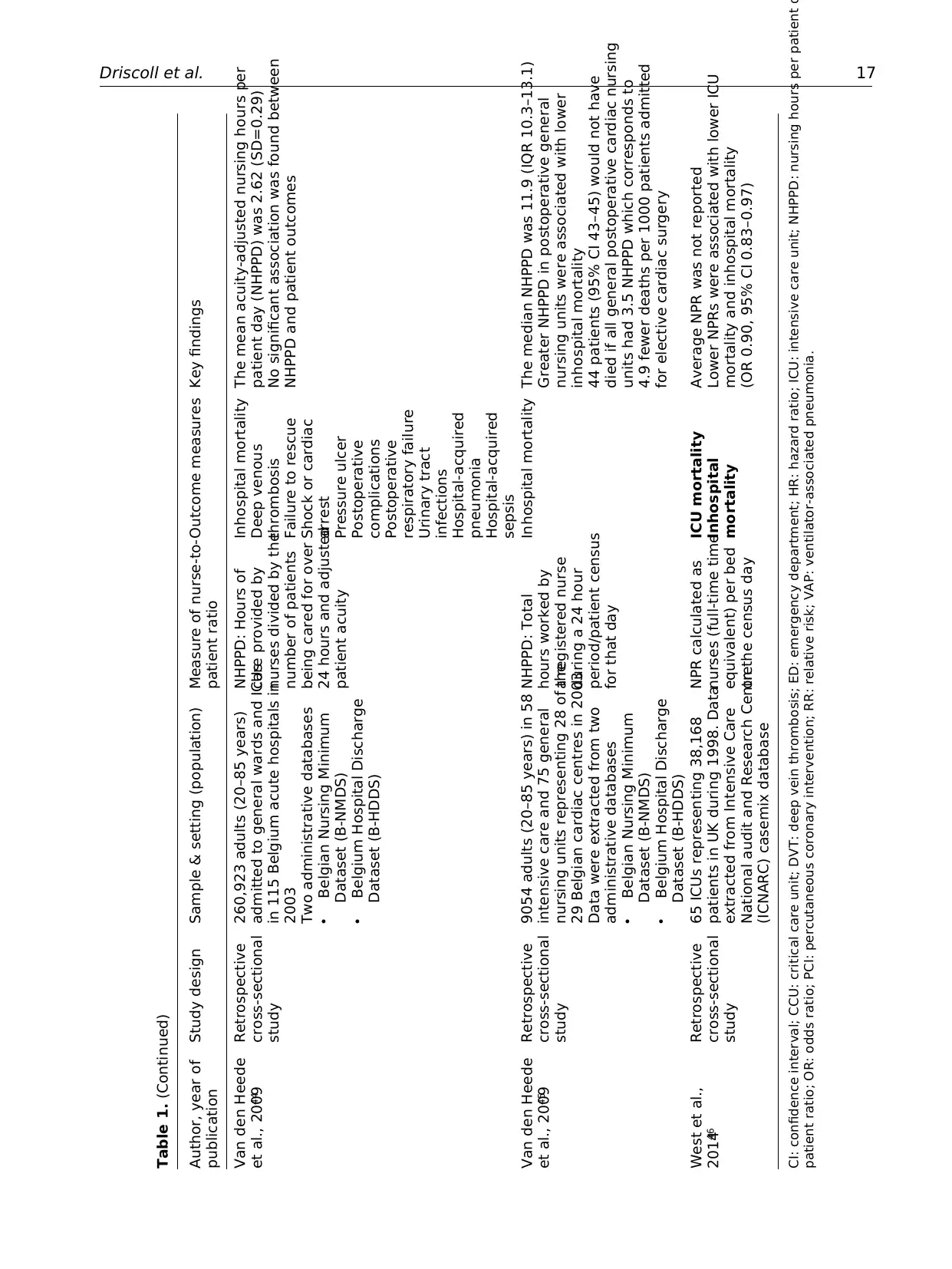
Driscoll et al. 17
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Van den Heede
et al., 200944
Retrospective
cross-sectional
study
260,923 adults (20–85 years)
admitted to general wards and ICUs
in 115 Belgium acute hospitals in
2003
Two administrative databases
• Belgian Nursing Minimum
Dataset (B-NMDS)
• Belgium Hospital Discharge
Dataset (B-HDDS)
NHPPD: Hours of
care provided by
nurses divided by the
number of patients
being cared for over
24 hours and adjusted
patient acuity
Inhospital mortality
Deep venous
thrombosis
Failure to rescue
Shock or cardiac
arrest
Pressure ulcer
Postoperative
complications
Postoperative
respiratory failure
Urinary tract
infections
Hospital-acquired
pneumonia
Hospital-acquired
sepsis
The mean acuity-adjusted nursing hours per
patient day (NHPPD) was 2.62 (SD=0.29)
No significant association was found between
NHPPD and patient outcomes
Van den Heede
et al., 200945
Retrospective
cross-sectional
study
9054 adults (20–85 years) in 58
intensive care and 75 general
nursing units representing 28 of the
29 Belgian cardiac centres in 2003
Data were extracted from two
administrative databases
• Belgian Nursing Minimum
Dataset (B-NMDS)
• Belgium Hospital Discharge
Dataset (B-HDDS)
NHPPD: Total
hours worked by
a registered nurse
during a 24 hour
period/patient census
for that day
Inhospital mortality The median NHPPD was 11.9 (IQR 10.3–13.1)
Greater NHPPD in postoperative general
nursing units were associated with lower
inhospital mortality
44 patients (95% CI 43–45) would not have
died if all general postoperative cardiac nursing
units had 3.5 NHPPD which corresponds to
4.9 fewer deaths per 1000 patients admitted
for elective cardiac surgery
West et al.,
201446
Retrospective
cross-sectional
study
65 ICUs representing 38,168
patients in UK during 1998. Data
extracted from Intensive Care
National audit and Research Centre
(ICNARC) casemix database
NPR calculated as
nurses (full-time time
equivalent) per bed
on the census day
ICU mortality
Inhospital
mortality
Average NPR was not reported
Lower NPRs were associated with lower ICU
mortality and inhospital mortality
(OR 0.90, 95% CI 0.83–0.97)
CI: confidence interval; CCU: critical care unit; DVT: deep vein thrombosis; ED: emergency department; HR: hazard ratio; ICU: intensive care unit; NHPPD: nursing hours per patient d
patient ratio; OR: odds ratio; PCI: percutaneous coronary intervention; RR: relative risk; VAP: ventilator-associated pneumonia.
Table 1. (Continued)
Author, year of
publication
Study design Sample & setting (population) Measure of nurse-to-
patient ratio
Outcome measures Key findings
Van den Heede
et al., 200944
Retrospective
cross-sectional
study
260,923 adults (20–85 years)
admitted to general wards and ICUs
in 115 Belgium acute hospitals in
2003
Two administrative databases
• Belgian Nursing Minimum
Dataset (B-NMDS)
• Belgium Hospital Discharge
Dataset (B-HDDS)
NHPPD: Hours of
care provided by
nurses divided by the
number of patients
being cared for over
24 hours and adjusted
patient acuity
Inhospital mortality
Deep venous
thrombosis
Failure to rescue
Shock or cardiac
arrest
Pressure ulcer
Postoperative
complications
Postoperative
respiratory failure
Urinary tract
infections
Hospital-acquired
pneumonia
Hospital-acquired
sepsis
The mean acuity-adjusted nursing hours per
patient day (NHPPD) was 2.62 (SD=0.29)
No significant association was found between
NHPPD and patient outcomes
Van den Heede
et al., 200945
Retrospective
cross-sectional
study
9054 adults (20–85 years) in 58
intensive care and 75 general
nursing units representing 28 of the
29 Belgian cardiac centres in 2003
Data were extracted from two
administrative databases
• Belgian Nursing Minimum
Dataset (B-NMDS)
• Belgium Hospital Discharge
Dataset (B-HDDS)
NHPPD: Total
hours worked by
a registered nurse
during a 24 hour
period/patient census
for that day
Inhospital mortality The median NHPPD was 11.9 (IQR 10.3–13.1)
Greater NHPPD in postoperative general
nursing units were associated with lower
inhospital mortality
44 patients (95% CI 43–45) would not have
died if all general postoperative cardiac nursing
units had 3.5 NHPPD which corresponds to
4.9 fewer deaths per 1000 patients admitted
for elective cardiac surgery
West et al.,
201446
Retrospective
cross-sectional
study
65 ICUs representing 38,168
patients in UK during 1998. Data
extracted from Intensive Care
National audit and Research Centre
(ICNARC) casemix database
NPR calculated as
nurses (full-time time
equivalent) per bed
on the census day
ICU mortality
Inhospital
mortality
Average NPR was not reported
Lower NPRs were associated with lower ICU
mortality and inhospital mortality
(OR 0.90, 95% CI 0.83–0.97)
CI: confidence interval; CCU: critical care unit; DVT: deep vein thrombosis; ED: emergency department; HR: hazard ratio; ICU: intensive care unit; NHPPD: nursing hours per patient d
patient ratio; OR: odds ratio; PCI: percutaneous coronary intervention; RR: relative risk; VAP: ventilator-associated pneumonia.
Table 1. (Continued)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





