University of East London: Role of Nurse in Chronic Heart Disease
VerifiedAdded on 2022/10/19
|20
|4779
|36
Report
AI Summary
This report delves into the crucial role of nurses in managing patients with chronic heart disease. It begins by highlighting the increasing prevalence of cardiovascular diseases and the significance of nursing interventions in mitigating related risks. The literature review covers acute heart failure, pharmacological treatments, and essential patient education topics. The report emphasizes the importance of nursing assessments, interventions, and patient education in managing the condition, including promoting patient comfort, reducing fluid overload, and increasing patient awareness about their health condition. It also provides insights into pharmacological management and the importance of a multidisciplinary approach involving cardiologists, heart failure specialist nurses, and other healthcare providers. The report also explores the importance of psychosocial assessments and provides an overview of essential patient education topics, including understanding the causes and symptoms of heart failure, risk factor modification, and dietary and exercise recommendations. Overall, the report underscores the proactive role nurses play in improving patient outcomes and reducing readmissions in chronic heart disease care.

Running head: ROLE OF THE NURSE IN CARING FOR PATIENTS WITH CHRONIC
HEART DISEASE
Role of the nurse in caring for patients with chronic heart disease
Student Name
Student ID:
Author’s note:
HEART DISEASE
Role of the nurse in caring for patients with chronic heart disease
Student Name
Student ID:
Author’s note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Table of Contents
INTRODUCTION...........................................................................................................................1
Introduction..................................................................................................................................1
Background..................................................................................................................................1
Rationale......................................................................................................................................2
LITERATURE REVIEW................................................................................................................3
Nursing intervention in Acute heart failure.................................................................................3
Pharmacological management.....................................................................................................4
Essential topics in patient education............................................................................................6
Role of the nurses in reducing repeated incidents of CHF..........................................................8
Gap in literature.........................................................................................................................10
Summary........................................................................................................................................10
Reference list.................................................................................................................................11
Table of Contents
INTRODUCTION...........................................................................................................................1
Introduction..................................................................................................................................1
Background..................................................................................................................................1
Rationale......................................................................................................................................2
LITERATURE REVIEW................................................................................................................3
Nursing intervention in Acute heart failure.................................................................................3
Pharmacological management.....................................................................................................4
Essential topics in patient education............................................................................................6
Role of the nurses in reducing repeated incidents of CHF..........................................................8
Gap in literature.........................................................................................................................10
Summary........................................................................................................................................10
Reference list.................................................................................................................................11
3
INTRODUCTION
Introduction
Cardiovascular health is gaining immense prominence in the recent times. Aligning the
current health statistics and health condition of the people, it can be stated cardiovascular
condition, is a major cause of comorbidity (Kutzleb et al. 2015). The current assignment thus
works on understanding the role of nurses and the required nursing intervention for providing
care to the patients suffering from chronic heart conditions. The research literature therefore aims
to understand the importance of educating the patients and the role of the nurses in the mentioned
stage. The literature additionally provides a brief overview about the possible pharmacological
intervention that can be undertaken to improve the chronic conditions such as chronic heart
disease
Cardiovascular disease (CVD) is termed as one of the leading causes of premature death
among individuals, irrespective of gender. In the last twenty years; prevalence of stroke and
CVD increased among the developing countries with low to middle range of income. Schulman‐
Green et al. (2016), stated the fact, series of immutable and modifiable factors are seen to
contribute towards the increasing rates of stroke related incidents. In regards to the mentioned
incident, American Heart Association recognized role of nurses in reducing disability and even
death. Recent statistics show, nearly 25% of death by 2025 (Dharmarajan et al., 2016). For more
than 40 years, registered nurses have taken up the prime role in managing multiple and even
single risks associated with cardiovascular problems such as smoking, hypertension, diabetes and
even cardiac rehabilitation. By embracing primary roles as team leaders in providing case
management as per the patient requirements, nurses are seen to issue rehabilitation centres and
INTRODUCTION
Introduction
Cardiovascular health is gaining immense prominence in the recent times. Aligning the
current health statistics and health condition of the people, it can be stated cardiovascular
condition, is a major cause of comorbidity (Kutzleb et al. 2015). The current assignment thus
works on understanding the role of nurses and the required nursing intervention for providing
care to the patients suffering from chronic heart conditions. The research literature therefore aims
to understand the importance of educating the patients and the role of the nurses in the mentioned
stage. The literature additionally provides a brief overview about the possible pharmacological
intervention that can be undertaken to improve the chronic conditions such as chronic heart
disease
Cardiovascular disease (CVD) is termed as one of the leading causes of premature death
among individuals, irrespective of gender. In the last twenty years; prevalence of stroke and
CVD increased among the developing countries with low to middle range of income. Schulman‐
Green et al. (2016), stated the fact, series of immutable and modifiable factors are seen to
contribute towards the increasing rates of stroke related incidents. In regards to the mentioned
incident, American Heart Association recognized role of nurses in reducing disability and even
death. Recent statistics show, nearly 25% of death by 2025 (Dharmarajan et al., 2016). For more
than 40 years, registered nurses have taken up the prime role in managing multiple and even
single risks associated with cardiovascular problems such as smoking, hypertension, diabetes and
even cardiac rehabilitation. By embracing primary roles as team leaders in providing case
management as per the patient requirements, nurses are seen to issue rehabilitation centres and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
stick to the health guidelines. Such disease programs were seen to exhibit improved outcomes;
coupled with cost effectiveness, in developed and developing countries.
Evidence based data is seen to support role of nurses in playing a proactive role in
regards to stroke prevention. Research based study conducted by Heery et al. (2015), stated the
fact that intervention laid by the nurses to reduce the risks related to CVD documents cause
regression of disease; coupled with reduction related to clinical events. Study conducted in
hospitals found the fact, admitted patients suffering from CAD, were shown to exhibit significant
reduction in rates of mortality and morbidity after a year followed by care from the nurses. It
would be fair enough to state that CVD adherence to guideline recommendations for secondary
and even primary prevention can be substantially improved by the teams directed by the nurses.
stick to the health guidelines. Such disease programs were seen to exhibit improved outcomes;
coupled with cost effectiveness, in developed and developing countries.
Evidence based data is seen to support role of nurses in playing a proactive role in
regards to stroke prevention. Research based study conducted by Heery et al. (2015), stated the
fact that intervention laid by the nurses to reduce the risks related to CVD documents cause
regression of disease; coupled with reduction related to clinical events. Study conducted in
hospitals found the fact, admitted patients suffering from CAD, were shown to exhibit significant
reduction in rates of mortality and morbidity after a year followed by care from the nurses. It
would be fair enough to state that CVD adherence to guideline recommendations for secondary
and even primary prevention can be substantially improved by the teams directed by the nurses.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
LITERATURE REVIEW
An overview of acute heart failure (AHF), impact on patient and nursing strategies
Acute heart failure is not a single disease, rather a combination of multiple worsening
signs that reflects inability of heart to pump blood. The cause of AHF can be termed as build-up
of fatty deposits leading to poor blood supply to the heart. Understanding the collective and even
the individual contribution of the nurses in preventing CVD is a proactive step in transforming
the nurses into leaders. The Global Cardiovascular Nursing Leadership Forum (GCNLF), is such
an intervention, designed to champion the existing nursing intervention across the lifespan of an
individual in both developed and developing countries. Fergenbaum et al. (2015), reaffirmed the
comment restating the global burden of CVD on the provided specifics of both middle income
and low income countries. The challenges can be highlighted on global healthcare platform;
including, cultural, economic and even environmental; widening the gap between the rich and
the poor. The shortage of nurses has been defined as one of the prime deterrents in CVD. While
addressing optimal role of the nurses Ulin et al. (2016), underlined the importance of patient
centred care, quality improvement initiatives and even evidence-based practice. The research
rationale as obtained through previous study leads to the following finding:
LITERATURE REVIEW
An overview of acute heart failure (AHF), impact on patient and nursing strategies
Acute heart failure is not a single disease, rather a combination of multiple worsening
signs that reflects inability of heart to pump blood. The cause of AHF can be termed as build-up
of fatty deposits leading to poor blood supply to the heart. Understanding the collective and even
the individual contribution of the nurses in preventing CVD is a proactive step in transforming
the nurses into leaders. The Global Cardiovascular Nursing Leadership Forum (GCNLF), is such
an intervention, designed to champion the existing nursing intervention across the lifespan of an
individual in both developed and developing countries. Fergenbaum et al. (2015), reaffirmed the
comment restating the global burden of CVD on the provided specifics of both middle income
and low income countries. The challenges can be highlighted on global healthcare platform;
including, cultural, economic and even environmental; widening the gap between the rich and
the poor. The shortage of nurses has been defined as one of the prime deterrents in CVD. While
addressing optimal role of the nurses Ulin et al. (2016), underlined the importance of patient
centred care, quality improvement initiatives and even evidence-based practice. The research
rationale as obtained through previous study leads to the following finding:
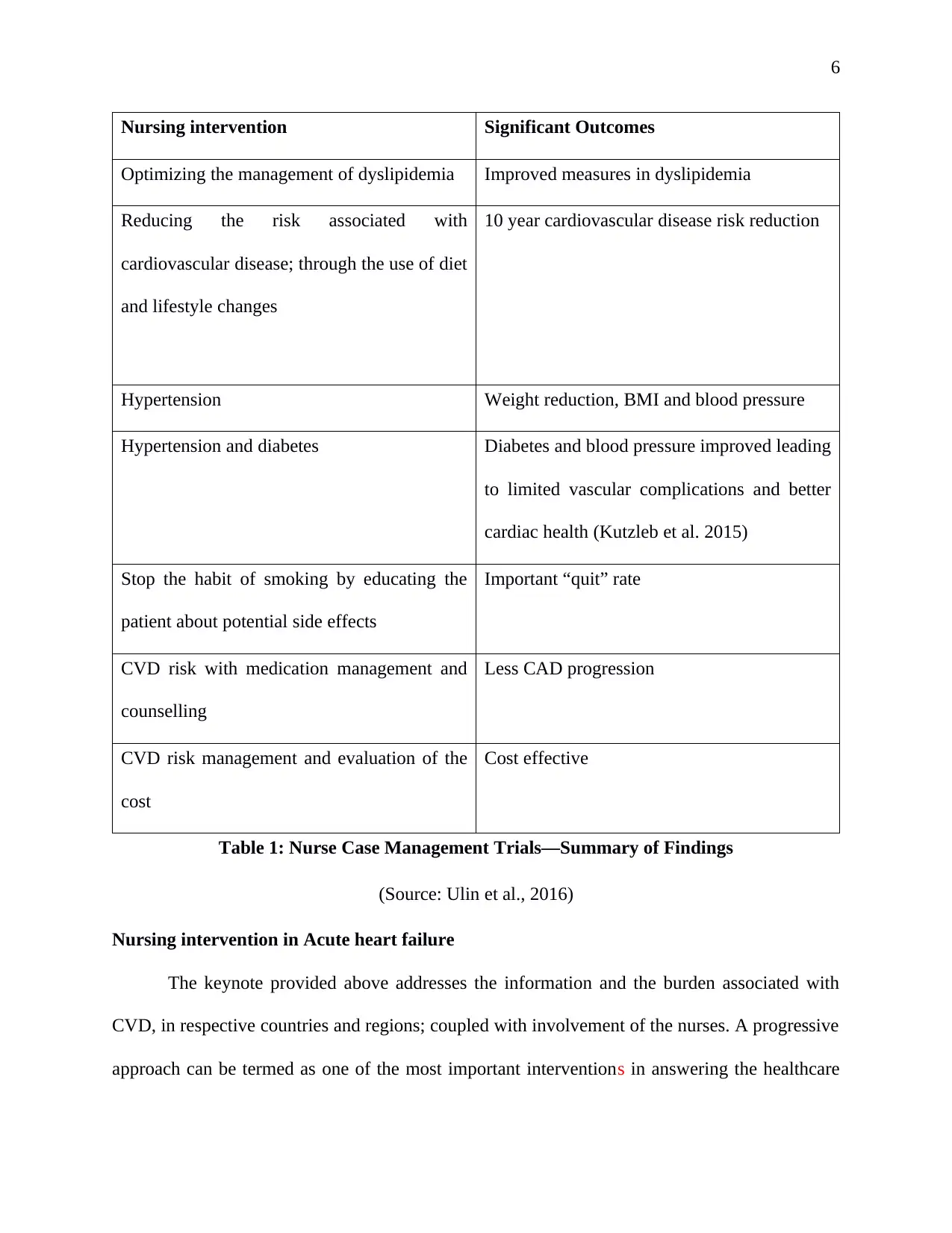
6
Nursing intervention Significant Outcomes
Optimizing the management of dyslipidemia Improved measures in dyslipidemia
Reducing the risk associated with
cardiovascular disease; through the use of diet
and lifestyle changes
10 year cardiovascular disease risk reduction
Hypertension Weight reduction, BMI and blood pressure
Hypertension and diabetes Diabetes and blood pressure improved leading
to limited vascular complications and better
cardiac health (Kutzleb et al. 2015)
Stop the habit of smoking by educating the
patient about potential side effects
Important “quit” rate
CVD risk with medication management and
counselling
Less CAD progression
CVD risk management and evaluation of the
cost
Cost effective
Table 1: Nurse Case Management Trials—Summary of Findings
(Source: Ulin et al., 2016)
Nursing intervention in Acute heart failure
The keynote provided above addresses the information and the burden associated with
CVD, in respective countries and regions; coupled with involvement of the nurses. A progressive
approach can be termed as one of the most important interventions in answering the healthcare
Nursing intervention Significant Outcomes
Optimizing the management of dyslipidemia Improved measures in dyslipidemia
Reducing the risk associated with
cardiovascular disease; through the use of diet
and lifestyle changes
10 year cardiovascular disease risk reduction
Hypertension Weight reduction, BMI and blood pressure
Hypertension and diabetes Diabetes and blood pressure improved leading
to limited vascular complications and better
cardiac health (Kutzleb et al. 2015)
Stop the habit of smoking by educating the
patient about potential side effects
Important “quit” rate
CVD risk with medication management and
counselling
Less CAD progression
CVD risk management and evaluation of the
cost
Cost effective
Table 1: Nurse Case Management Trials—Summary of Findings
(Source: Ulin et al., 2016)
Nursing intervention in Acute heart failure
The keynote provided above addresses the information and the burden associated with
CVD, in respective countries and regions; coupled with involvement of the nurses. A progressive
approach can be termed as one of the most important interventions in answering the healthcare
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
needs of chronic heart condition. The goal within nursing management is established through the
implementation of nursing assessment of patient’s functional capacity and even haemodynamic
status. The importance of nursing intervention was further stated by Qureshi et al. (2016),
providing an idea that nursing assessment can reveal the underlying condition that leads to heart
failure. The nursing goals in regards to care for patient with constant cardiac problems should be
as follows:
Promoting comfort of patient while reducing the events of breathlessness.
Reducing the signs related to fluid overload.
Maintaining the peripheral perfusion.
Increasing the awareness of the patient in educating them in current health condition.
Attending to self-care deficits often arising due to hypoxia and overload of fluid.
Monitoring the patient should be done immediately upon admission and focus should be
made on identifying the response to treatment. As stated by Clark et al. (2015), monitoring a
cardiac patient includes basic observations such as serial ECGs, oxygenation, heart rate,
respiratory rate and even blood pressure. Care of invasive monitoring system are as per local
nursing guidelines with prime intervention to prevent infection. As observed by Friesen-Storms
et al. (2015), nursing implication in regards to cardiac conditions is often seen to monitor the
fluid restrictions.
Advanced monitoring system is inclusive of invasive monitoring system as central
venous pressure monitoring and even arterial line. Hourly nursing assessment is dependent on
the clinical status of the patient. Identification of degrading conditions such as increase in blood
needs of chronic heart condition. The goal within nursing management is established through the
implementation of nursing assessment of patient’s functional capacity and even haemodynamic
status. The importance of nursing intervention was further stated by Qureshi et al. (2016),
providing an idea that nursing assessment can reveal the underlying condition that leads to heart
failure. The nursing goals in regards to care for patient with constant cardiac problems should be
as follows:
Promoting comfort of patient while reducing the events of breathlessness.
Reducing the signs related to fluid overload.
Maintaining the peripheral perfusion.
Increasing the awareness of the patient in educating them in current health condition.
Attending to self-care deficits often arising due to hypoxia and overload of fluid.
Monitoring the patient should be done immediately upon admission and focus should be
made on identifying the response to treatment. As stated by Clark et al. (2015), monitoring a
cardiac patient includes basic observations such as serial ECGs, oxygenation, heart rate,
respiratory rate and even blood pressure. Care of invasive monitoring system are as per local
nursing guidelines with prime intervention to prevent infection. As observed by Friesen-Storms
et al. (2015), nursing implication in regards to cardiac conditions is often seen to monitor the
fluid restrictions.
Advanced monitoring system is inclusive of invasive monitoring system as central
venous pressure monitoring and even arterial line. Hourly nursing assessment is dependent on
the clinical status of the patient. Identification of degrading conditions such as increase in blood
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
pressure, rates of respiration and so on is the primary role of the nurse. If the patient is seen to
respond positively to the implemented nursing intervention, it becomes important to continue the
same (Albert, 2016). The patient may lack the basic ability to execute events in daily life. The
nursing care thus supports the patient in daily activities. Nurses are often held responsible for
identifying the deficits; specially paying special attention towards the skin and associated
pressure areas. Additionally, the patients with pre-existing cardiac problems are often subjected
to peripheral oedema in the limbs leading to breakdown of the skin. Based on the nutritional
perspective, patient may be subjected to nausea and even anorexia; as a result of poor perfusion
to the digestive system. A dietary consultation is of prime importance in the mentioned scenario.
As stated by Reeder et al. (2015), generally the patient would be on low salt diet and advised to
eat in limited amounts to prevent nausea and feeling of fullness. Use of anti-emetic is made 30
minutes before meal for prevent the feeling of nausea. The lack of strong perfusion within the
digestive system risks altering the bowel movement and thus laxatives are often prescribed.
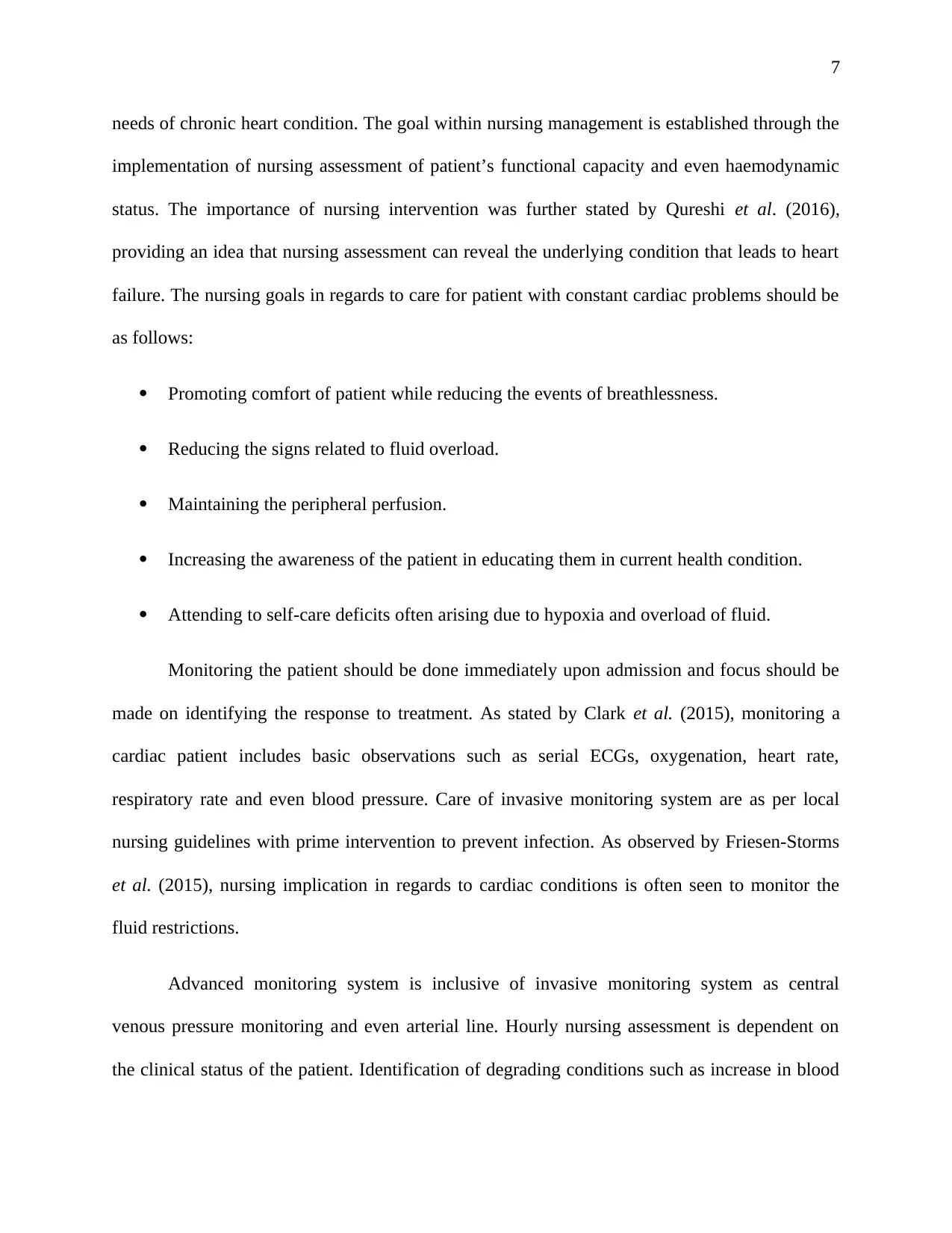
Pharmacological management
Treatment Adverse effects or nursing implication
Morphine Depression in respiratory rate
Vasodilatory effects causing hypotension
Diuretics Imbalance of the electrolytes
Hypotension
Dehydration
Resistance to diuretics if already on oral
diuretics
Vasodilators Headache
pressure, rates of respiration and so on is the primary role of the nurse. If the patient is seen to
respond positively to the implemented nursing intervention, it becomes important to continue the
same (Albert, 2016). The patient may lack the basic ability to execute events in daily life. The
nursing care thus supports the patient in daily activities. Nurses are often held responsible for
identifying the deficits; specially paying special attention towards the skin and associated
pressure areas. Additionally, the patients with pre-existing cardiac problems are often subjected
to peripheral oedema in the limbs leading to breakdown of the skin. Based on the nutritional
perspective, patient may be subjected to nausea and even anorexia; as a result of poor perfusion
to the digestive system. A dietary consultation is of prime importance in the mentioned scenario.
As stated by Reeder et al. (2015), generally the patient would be on low salt diet and advised to
eat in limited amounts to prevent nausea and feeling of fullness. Use of anti-emetic is made 30
minutes before meal for prevent the feeling of nausea. The lack of strong perfusion within the
digestive system risks altering the bowel movement and thus laxatives are often prescribed.
Pharmacological management
Treatment Adverse effects or nursing implication
Morphine Depression in respiratory rate
Vasodilatory effects causing hypotension
Diuretics Imbalance of the electrolytes
Hypotension
Dehydration
Resistance to diuretics if already on oral
diuretics
Vasodilators Headache
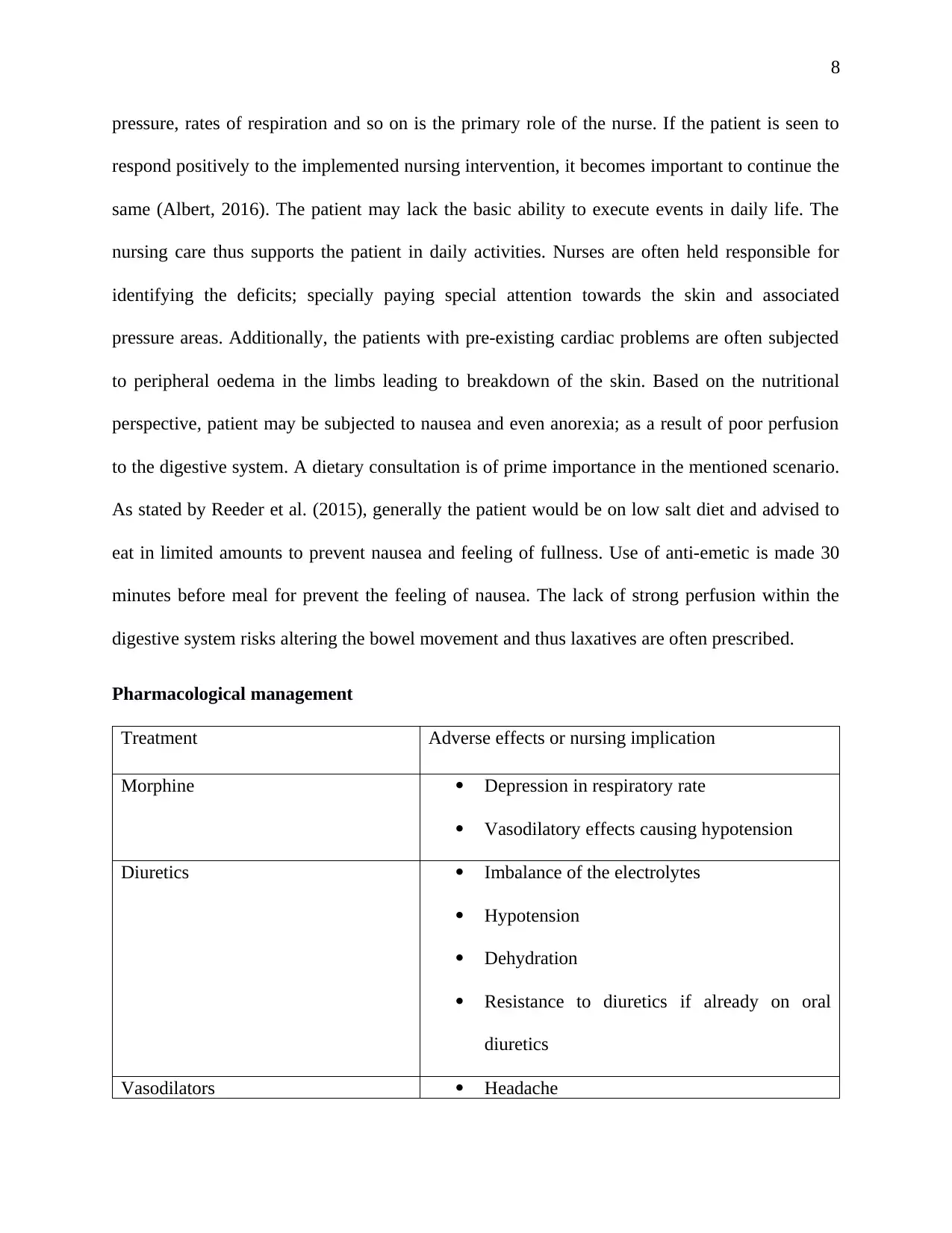
9
Hypotension
Tolerance towards nitrate
Inotropes Increased incidence of atrial and ventricular
arrhythmias
Type III phosphodiesterase inhibitors Monitor the blood pressure
Dobutamine and milrinone may be
administered peripherally
Vasopressors Administer via the use of central line
Observing special incident of vasoconstriction
Table 2 a: Nursing intervention in case of heart problem- a pharmacological intervention
(Source: Reeder et al., 2015)
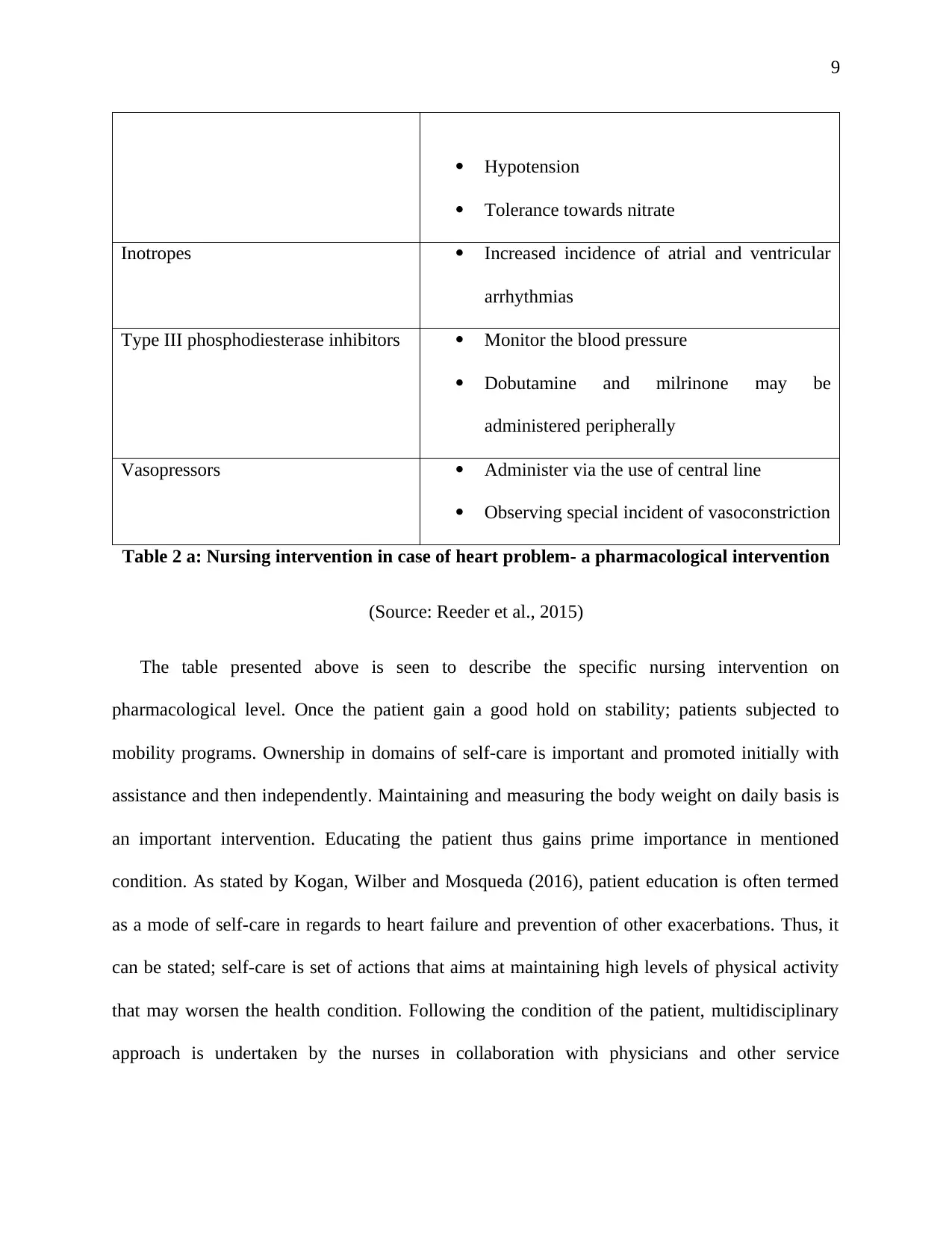
The table presented above is seen to describe the specific nursing intervention on
pharmacological level. Once the patient gain a good hold on stability; patients subjected to
mobility programs. Ownership in domains of self-care is important and promoted initially with
assistance and then independently. Maintaining and measuring the body weight on daily basis is
an important intervention. Educating the patient thus gains prime importance in mentioned
condition. As stated by Kogan, Wilber and Mosqueda (2016), patient education is often termed
as a mode of self-care in regards to heart failure and prevention of other exacerbations. Thus, it
can be stated; self-care is set of actions that aims at maintaining high levels of physical activity
that may worsen the health condition. Following the condition of the patient, multidisciplinary
approach is undertaken by the nurses in collaboration with physicians and other service
Hypotension
Tolerance towards nitrate
Inotropes Increased incidence of atrial and ventricular
arrhythmias
Type III phosphodiesterase inhibitors Monitor the blood pressure
Dobutamine and milrinone may be
administered peripherally
Vasopressors Administer via the use of central line
Observing special incident of vasoconstriction
Table 2 a: Nursing intervention in case of heart problem- a pharmacological intervention
(Source: Reeder et al., 2015)
The table presented above is seen to describe the specific nursing intervention on
pharmacological level. Once the patient gain a good hold on stability; patients subjected to
mobility programs. Ownership in domains of self-care is important and promoted initially with
assistance and then independently. Maintaining and measuring the body weight on daily basis is
an important intervention. Educating the patient thus gains prime importance in mentioned
condition. As stated by Kogan, Wilber and Mosqueda (2016), patient education is often termed
as a mode of self-care in regards to heart failure and prevention of other exacerbations. Thus, it
can be stated; self-care is set of actions that aims at maintaining high levels of physical activity
that may worsen the health condition. Following the condition of the patient, multidisciplinary
approach is undertaken by the nurses in collaboration with physicians and other service
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
providers. Following are the nursing interventions undertaken in case of treating patients with
chronic heart conditions
Contact during the course of hospitalisation, coupled with early follow up after discharge
Targeting high risk symptomatic patients
Facilitating access during the course of decompensation
Optimised medical management
Access to advanced option for treatments
Psychosocial support for the patients and family members
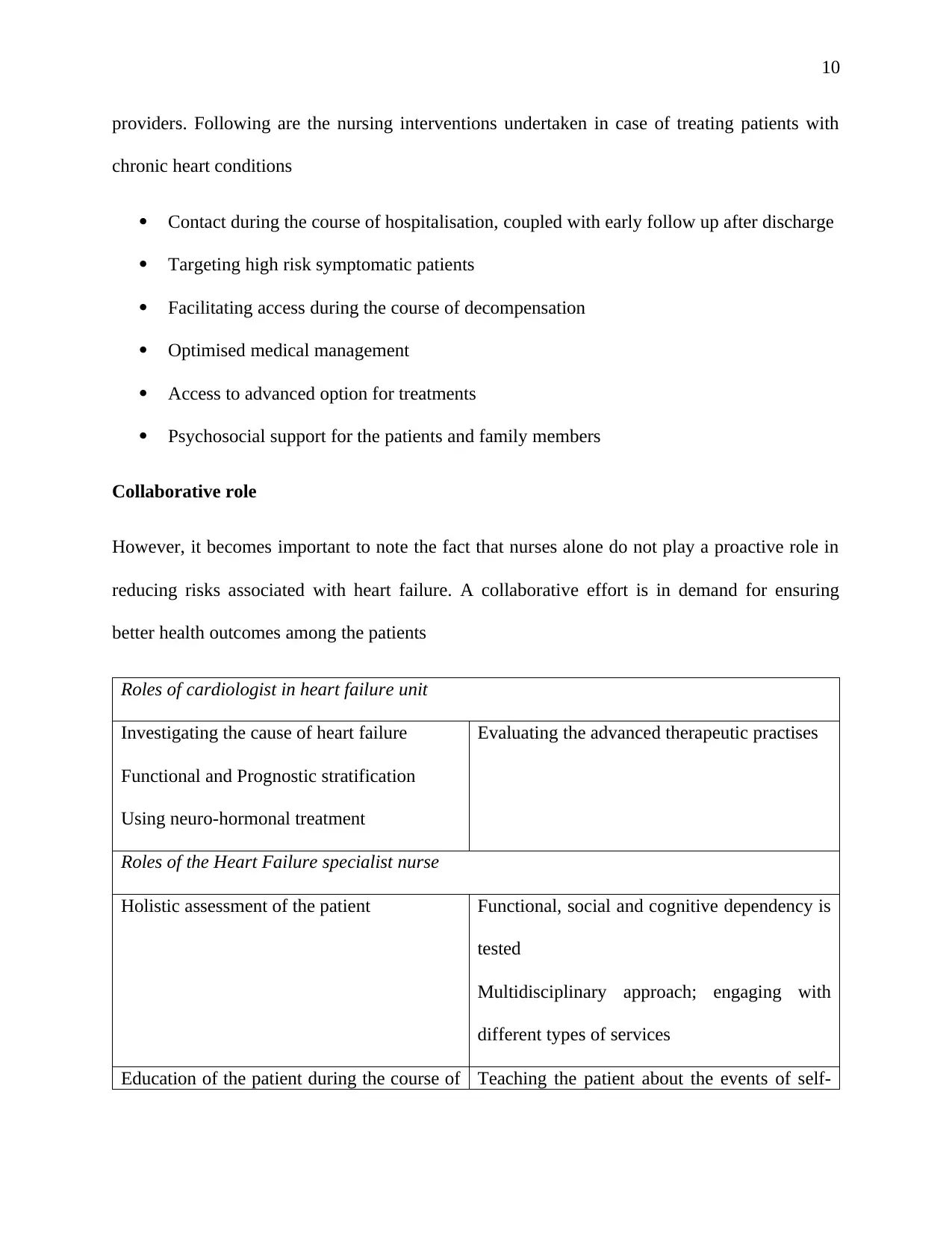
Collaborative role
However, it becomes important to note the fact that nurses alone do not play a proactive role in
reducing risks associated with heart failure. A collaborative effort is in demand for ensuring
better health outcomes among the patients
Roles of cardiologist in heart failure unit
Investigating the cause of heart failure
Functional and Prognostic stratification
Using neuro-hormonal treatment
Evaluating the advanced therapeutic practises
Roles of the Heart Failure specialist nurse
Holistic assessment of the patient Functional, social and cognitive dependency is
tested
Multidisciplinary approach; engaging with
different types of services
Education of the patient during the course of Teaching the patient about the events of self-
providers. Following are the nursing interventions undertaken in case of treating patients with
chronic heart conditions
Contact during the course of hospitalisation, coupled with early follow up after discharge
Targeting high risk symptomatic patients
Facilitating access during the course of decompensation
Optimised medical management
Access to advanced option for treatments
Psychosocial support for the patients and family members
Collaborative role
However, it becomes important to note the fact that nurses alone do not play a proactive role in
reducing risks associated with heart failure. A collaborative effort is in demand for ensuring
better health outcomes among the patients
Roles of cardiologist in heart failure unit
Investigating the cause of heart failure
Functional and Prognostic stratification
Using neuro-hormonal treatment
Evaluating the advanced therapeutic practises
Roles of the Heart Failure specialist nurse
Holistic assessment of the patient Functional, social and cognitive dependency is
tested
Multidisciplinary approach; engaging with
different types of services
Education of the patient during the course of Teaching the patient about the events of self-
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
stay care
Planning the discharge and providing the
primary care to the patients
Follow-up with the patients and ensuring
continuous care
Table 2b: Nursing intervention during the course of in-patient care
(Source: Kogan, Wilber and Mosqueda, 2016)
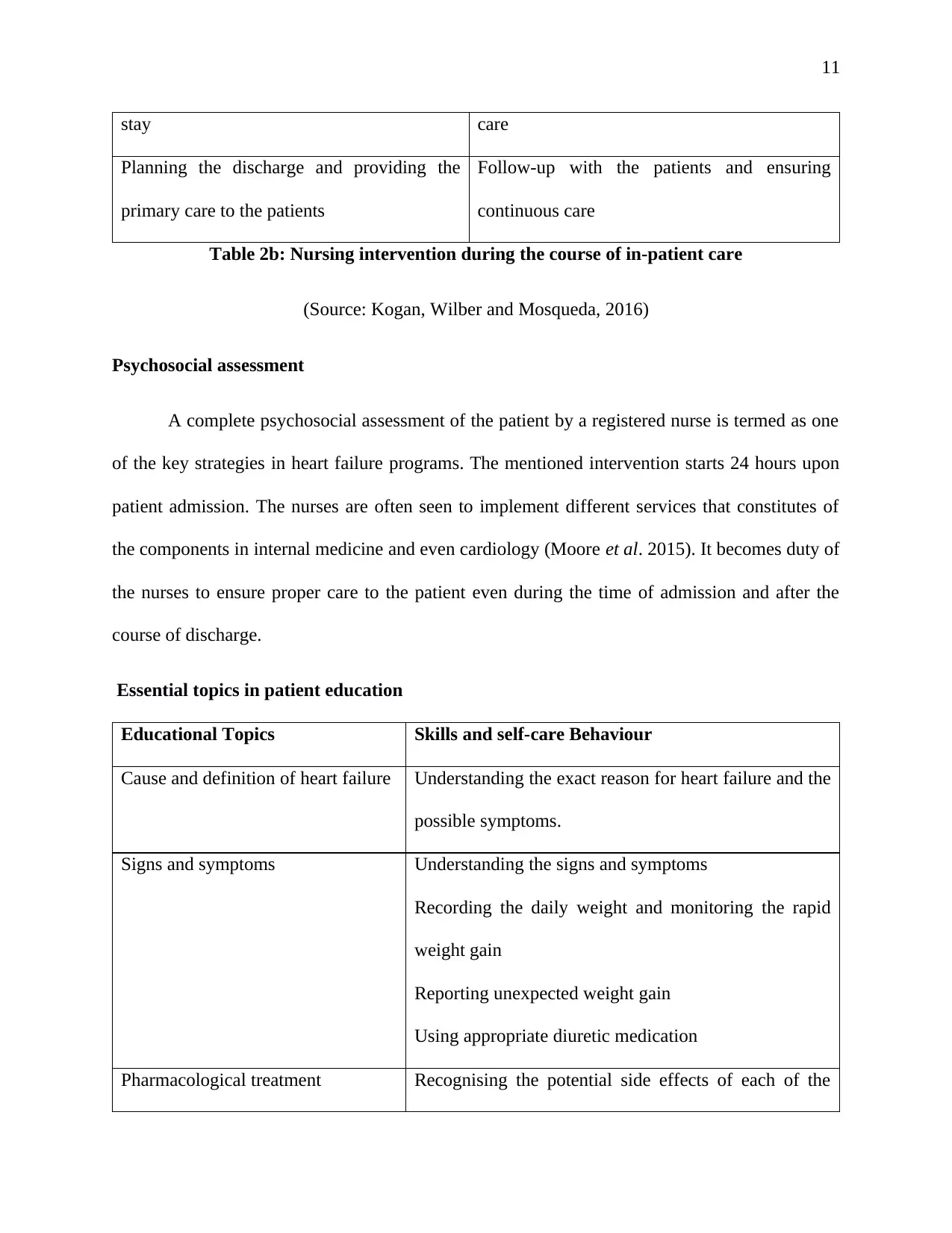
Psychosocial assessment
A complete psychosocial assessment of the patient by a registered nurse is termed as one
of the key strategies in heart failure programs. The mentioned intervention starts 24 hours upon
patient admission. The nurses are often seen to implement different services that constitutes of
the components in internal medicine and even cardiology (Moore et al. 2015). It becomes duty of
the nurses to ensure proper care to the patient even during the time of admission and after the
course of discharge.
Essential topics in patient education
Educational Topics Skills and self-care Behaviour
Cause and definition of heart failure Understanding the exact reason for heart failure and the
possible symptoms.
Signs and symptoms Understanding the signs and symptoms
Recording the daily weight and monitoring the rapid
weight gain
Reporting unexpected weight gain
Using appropriate diuretic medication
Pharmacological treatment Recognising the potential side effects of each of the
stay care
Planning the discharge and providing the
primary care to the patients
Follow-up with the patients and ensuring
continuous care
Table 2b: Nursing intervention during the course of in-patient care
(Source: Kogan, Wilber and Mosqueda, 2016)
Psychosocial assessment
A complete psychosocial assessment of the patient by a registered nurse is termed as one
of the key strategies in heart failure programs. The mentioned intervention starts 24 hours upon
patient admission. The nurses are often seen to implement different services that constitutes of
the components in internal medicine and even cardiology (Moore et al. 2015). It becomes duty of
the nurses to ensure proper care to the patient even during the time of admission and after the
course of discharge.
Essential topics in patient education
Educational Topics Skills and self-care Behaviour
Cause and definition of heart failure Understanding the exact reason for heart failure and the
possible symptoms.
Signs and symptoms Understanding the signs and symptoms
Recording the daily weight and monitoring the rapid
weight gain
Reporting unexpected weight gain
Using appropriate diuretic medication
Pharmacological treatment Recognising the potential side effects of each of the
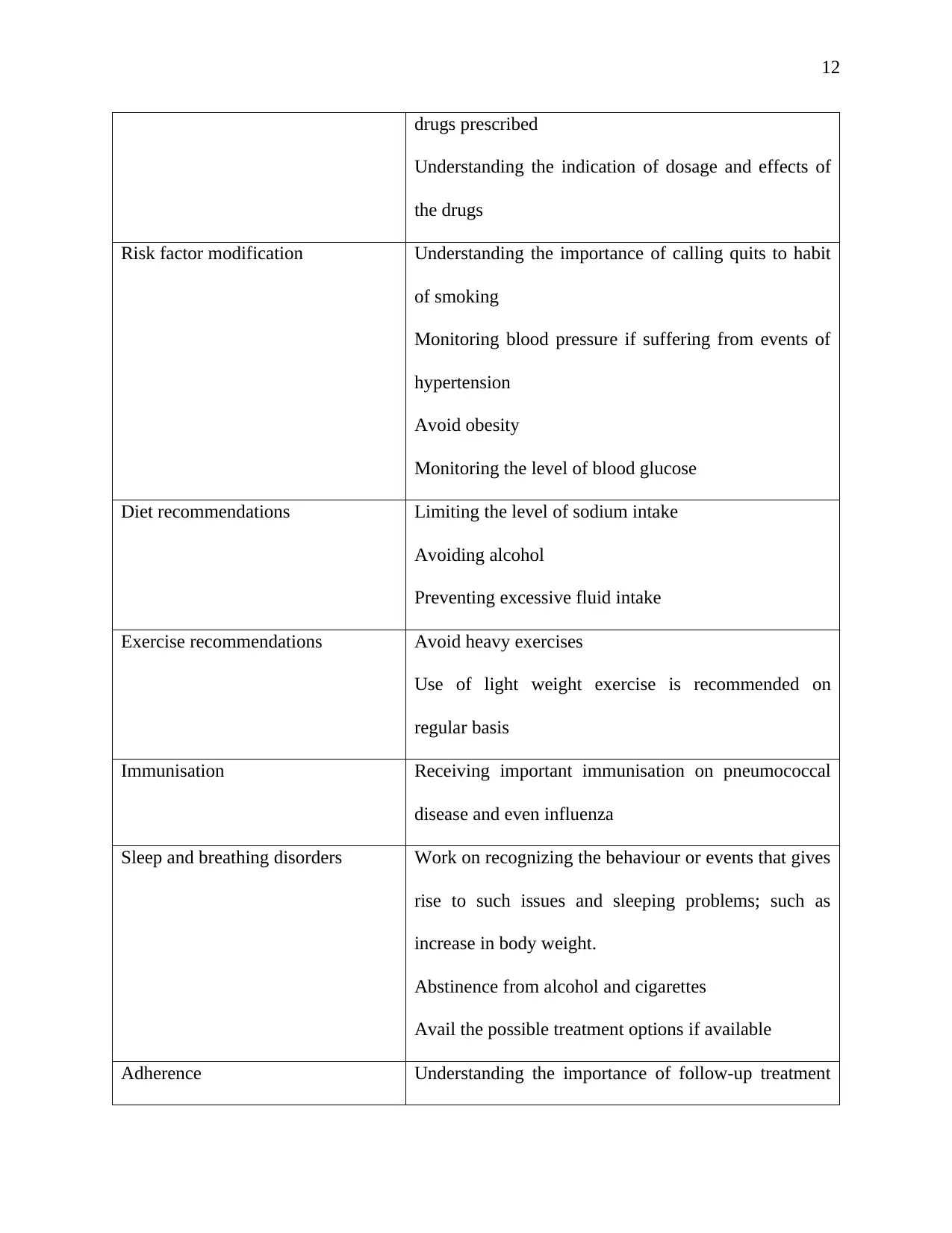
12
drugs prescribed
Understanding the indication of dosage and effects of
the drugs
Risk factor modification Understanding the importance of calling quits to habit
of smoking
Monitoring blood pressure if suffering from events of
hypertension
Avoid obesity
Monitoring the level of blood glucose
Diet recommendations Limiting the level of sodium intake
Avoiding alcohol
Preventing excessive fluid intake
Exercise recommendations Avoid heavy exercises
Use of light weight exercise is recommended on
regular basis
Immunisation Receiving important immunisation on pneumococcal
disease and even influenza
Sleep and breathing disorders Work on recognizing the behaviour or events that gives
rise to such issues and sleeping problems; such as
increase in body weight.
Abstinence from alcohol and cigarettes
Avail the possible treatment options if available
Adherence Understanding the importance of follow-up treatment
drugs prescribed
Understanding the indication of dosage and effects of
the drugs
Risk factor modification Understanding the importance of calling quits to habit
of smoking
Monitoring blood pressure if suffering from events of
hypertension
Avoid obesity
Monitoring the level of blood glucose
Diet recommendations Limiting the level of sodium intake
Avoiding alcohol
Preventing excessive fluid intake
Exercise recommendations Avoid heavy exercises
Use of light weight exercise is recommended on
regular basis
Immunisation Receiving important immunisation on pneumococcal
disease and even influenza
Sleep and breathing disorders Work on recognizing the behaviour or events that gives
rise to such issues and sleeping problems; such as
increase in body weight.
Abstinence from alcohol and cigarettes
Avail the possible treatment options if available
Adherence Understanding the importance of follow-up treatment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





