Pediatric Nurses' Perceptions of EOL Care Barriers in Southeast Iran
VerifiedAdded on 2023/06/09
|9
|8403
|433
Report
AI Summary
This research paper, published in the American Journal of Hospice & Palliative Medicine, investigates pediatric nurses' perceptions of barriers encountered when providing end-of-life (EOL) care to terminally ill children in Southeast Iran. The study utilized a modified version of the National Survey of Critical Care Nurses’ Regarding End-of-Life Care questionnaire to assess nurses' views on the intensity and frequency of various barriers. The findings revealed that family-related issues were among the most significant barriers perceived by nurses. The study highlights the absence of palliative care (PC) education and dedicated PC units in Iran as a contributing factor to these challenges. The authors suggest that developing EOL/PC education could improve nurses' knowledge and skills in managing the complexities of EOL care. The context of Iran, its healthcare system, and cultural perspectives on death are also discussed, providing a comprehensive understanding of the challenges faced by healthcare professionals in this setting.
Nursing Manuscript
Nursing Staff’s Perception of Barriers in
Providing End-of-Life Care to Terminally Ill
Pediatric Patients in Southeast Iran
Sedigheh Iranmanesh, PhD, MSc1, Marjan Banazadeh, MSc1,
and Mansoure Azizzadeh Forozy, MSc2
Abstract
Objective:To determine pediatric nurses’perceptions ofintensity,frequency occurrence,and magnitude score ofselected
barriers in providing pediatric end-of-life (EOL) care. Method: A translated modified version of National Survey o
Nurses’ s Regarding End-of-Life Care questionnaire was used to assess 151 nurses’ perceptions of intensity and
rence of barriers in caring for dying children. Results: The highest/lowest perceived barriers magnitude scores w
accepting poor child prognosis’’ (5.04) and ‘‘continuing to provide advanced treatment to dying child because o
to the hospital’’ (2.19). conclusion: More high perceived barriers by nurses were family-related issues. One of th
of such deficiencies was lack of palliative care (PC) education/PC units in Iran. Thus, developing EOL/PC educati
nurses’knowledge/skillto face EOL care challenges.
Keywords
nurses’perception,barriers,end-of-life care,terminally illchildren,Southeast Iran
Introduction
The idea that a child may die is simply unimaginable to most
people,yet children die daily.1 According to Morgan,2 when
a child dies, this cycle seems unnatural, causing loss of human
potential,and dreamsquickly shatter.2 Children represent
health and hope, and their death calls into question the under-
standing of life.3 Unfortunately, annually about 50 000 children
die in the United States.4 Of these, over half die during the first
year of life.5 A child’s chronic illness may progress to the point
of becoming a terminal illness that deemed to be incurable, ulti-
mately leading to death.1 Unlike adult populations, who more
frequently die at home or in hospice-type settings,more than
half of the children with acute and chronic illnesses die in inpa-
tient hospital settings.6 So providing comprehensive and com-
passionate end-of-life (EOL) care for these children within a
family-centered and developmentally appropriate contextis
necessary.7 End-of-life care is an important method of care for
infants and children with terminal illness through the preven-
tion or alleviation of physical, emotional, social, and spiritual
suffering.8 Unfortunately,the transition to EOL care is often
late and abrupt in pediatrics9 and seems inherently unnatural
in the mind of many parents and doctors,who often struggle
to accept that nothing more can be done for a child.10Pediatric
palliative care (PPC) is a relatively new and developing speci-
alty,11which begins when an illness is diagnosed and continues
regardless of whether or not a child receives treatment directed
at the disease.12Health care professionals face numerous obst
cles and challenges while providing care to this unique pop
tion of clients and their families,2 which differ from those cited
for adults.13 Although interdisciplinary care is essentialfor
EOL care quality,nurses play the key role ofchild-family
advocate.1
Reviewing literature indicated a few studies13-15
that exam-
ined the views of pediatric nurses on providing pediatric EO
care.14 In Western countries including United States,Beck-
strand etal14 using modified version of NationalSurvey of
critical Nurses’ Perceptions Regarding End-of-Life Care que
tionnaire asked 474 pediatric intensive care unit (PICU) nu
to rate size and frequency of listed obstacles and supportiv
behaviors in providing pediatric EOL care. They found that
item ‘‘language barriers’’ was the highestperceived obstacle
with both the highestmean intensity and frequency scores.14
In Spain,Iglesias et al16 used the samequestionnaire to deter-
mine the relative importance of helpful behaviors and obst
1Razifaculty of Nursing and Midwifery,Kerman,Iran
2Neuroscience Research Center,Institute ofNeuropharmacology,Kerman
University of MedicalSciences,Kerman,Iran
Corresponding Author:
Marjan Banazadeh,MSc,Razi faculty ofNursingand Midwifery,Kerman,
86618 Iran.
Email:banazadeh54@yahoo.com
American Journalof Hospice
& Palliative Medicine®
1-9
ª The Author(s) 2014
Reprints and permission:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/1049909114556878
ajhpm.sagepub.com
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
Nursing Staff’s Perception of Barriers in
Providing End-of-Life Care to Terminally Ill
Pediatric Patients in Southeast Iran
Sedigheh Iranmanesh, PhD, MSc1, Marjan Banazadeh, MSc1,
and Mansoure Azizzadeh Forozy, MSc2
Abstract
Objective:To determine pediatric nurses’perceptions ofintensity,frequency occurrence,and magnitude score ofselected
barriers in providing pediatric end-of-life (EOL) care. Method: A translated modified version of National Survey o
Nurses’ s Regarding End-of-Life Care questionnaire was used to assess 151 nurses’ perceptions of intensity and
rence of barriers in caring for dying children. Results: The highest/lowest perceived barriers magnitude scores w
accepting poor child prognosis’’ (5.04) and ‘‘continuing to provide advanced treatment to dying child because o
to the hospital’’ (2.19). conclusion: More high perceived barriers by nurses were family-related issues. One of th
of such deficiencies was lack of palliative care (PC) education/PC units in Iran. Thus, developing EOL/PC educati
nurses’knowledge/skillto face EOL care challenges.
Keywords
nurses’perception,barriers,end-of-life care,terminally illchildren,Southeast Iran
Introduction
The idea that a child may die is simply unimaginable to most
people,yet children die daily.1 According to Morgan,2 when
a child dies, this cycle seems unnatural, causing loss of human
potential,and dreamsquickly shatter.2 Children represent
health and hope, and their death calls into question the under-
standing of life.3 Unfortunately, annually about 50 000 children
die in the United States.4 Of these, over half die during the first
year of life.5 A child’s chronic illness may progress to the point
of becoming a terminal illness that deemed to be incurable, ulti-
mately leading to death.1 Unlike adult populations, who more
frequently die at home or in hospice-type settings,more than
half of the children with acute and chronic illnesses die in inpa-
tient hospital settings.6 So providing comprehensive and com-
passionate end-of-life (EOL) care for these children within a
family-centered and developmentally appropriate contextis
necessary.7 End-of-life care is an important method of care for
infants and children with terminal illness through the preven-
tion or alleviation of physical, emotional, social, and spiritual
suffering.8 Unfortunately,the transition to EOL care is often
late and abrupt in pediatrics9 and seems inherently unnatural
in the mind of many parents and doctors,who often struggle
to accept that nothing more can be done for a child.10Pediatric
palliative care (PPC) is a relatively new and developing speci-
alty,11which begins when an illness is diagnosed and continues
regardless of whether or not a child receives treatment directed
at the disease.12Health care professionals face numerous obst
cles and challenges while providing care to this unique pop
tion of clients and their families,2 which differ from those cited
for adults.13 Although interdisciplinary care is essentialfor
EOL care quality,nurses play the key role ofchild-family
advocate.1
Reviewing literature indicated a few studies13-15
that exam-
ined the views of pediatric nurses on providing pediatric EO
care.14 In Western countries including United States,Beck-
strand etal14 using modified version of NationalSurvey of
critical Nurses’ Perceptions Regarding End-of-Life Care que
tionnaire asked 474 pediatric intensive care unit (PICU) nu
to rate size and frequency of listed obstacles and supportiv
behaviors in providing pediatric EOL care. They found that
item ‘‘language barriers’’ was the highestperceived obstacle
with both the highestmean intensity and frequency scores.14
In Spain,Iglesias et al16 used the samequestionnaire to deter-
mine the relative importance of helpful behaviors and obst
1Razifaculty of Nursing and Midwifery,Kerman,Iran
2Neuroscience Research Center,Institute ofNeuropharmacology,Kerman
University of MedicalSciences,Kerman,Iran
Corresponding Author:
Marjan Banazadeh,MSc,Razi faculty ofNursingand Midwifery,Kerman,
86618 Iran.
Email:banazadeh54@yahoo.com
American Journalof Hospice
& Palliative Medicine®
1-9
ª The Author(s) 2014
Reprints and permission:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/1049909114556878
ajhpm.sagepub.com
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
that affect EOL care for pediatric patients and their families in
PICUs as perceived by nurses. Nurses viewed ‘‘evasive physi-
cians’’ and ‘‘families are not accepting of a poor prognosis’’ as
obstacles.16In California, Davies et al13also conducted a study
using a self-report questionnaire to explore the barriers to pal-
liative care (PC) experienced by pediatric health professionals
(117 nurses and 81 doctors).Approximately one half of the
respondents reported ‘‘uncertain prognosis,’’ ‘‘family not ready
to acknowledge incurable condition,’’ and ‘‘language barriers’’
as frequently or almost always occurring barriers.13 In Egypt,
Moawad15 using the NSCCNR-EOLC questionnaire assessed
94 PICU and NICU nurses’ perceptions of obstacles and sup-
portive behaviors in providing EOL care. He revealed that the
most perceived obstacle by nurses was ‘‘child having pain that
is difficult to control or alleviate.’’15
To our knowledge, in the context of Iran, no study has been
conducted to assess barriers in providing pediatric EOL care.
This study,thus,conducted to assess nurses’ perceptions of
intensity,frequency,and magnitude score of selected barriers
in providing pediatric EOL care in pediatric units in Kerman
hospitals.
Context
Death in different cultures has become inextricably linked in
the particularceremonies and customs,which originated in
inconsolable affections and feelings that has been painful expe-
rience.17 Therefore, it seems necessary to mention the context
in this study. Iran, officially the Islamic Republic of Iran, is a
diverse country consisting of people with many ethnic back-
grounds cemented by the Persian culture.The main language
spoken is Farsi or Persian.18Persian literature, which is heavily
informed and influenced by Islamic and mysticalspiritual
beliefs,is fraughtwith poems and stories thatportray death
as a glorious incident that takes people from one stage of their
material/mortalexistencethrough to therealm of divine
immortality.19,20
In the most celebrated and the great mystical
Persian poems, Masnavi, Rumi narrates that death is the time of
release from this cage of the body; the time when the bird of the
soul flies free.The body,like a mother,is pregnant with the
spirit-child: death is the labor of birth. All the spirits who have
passed over are waiting to see how that proud spirit shall be
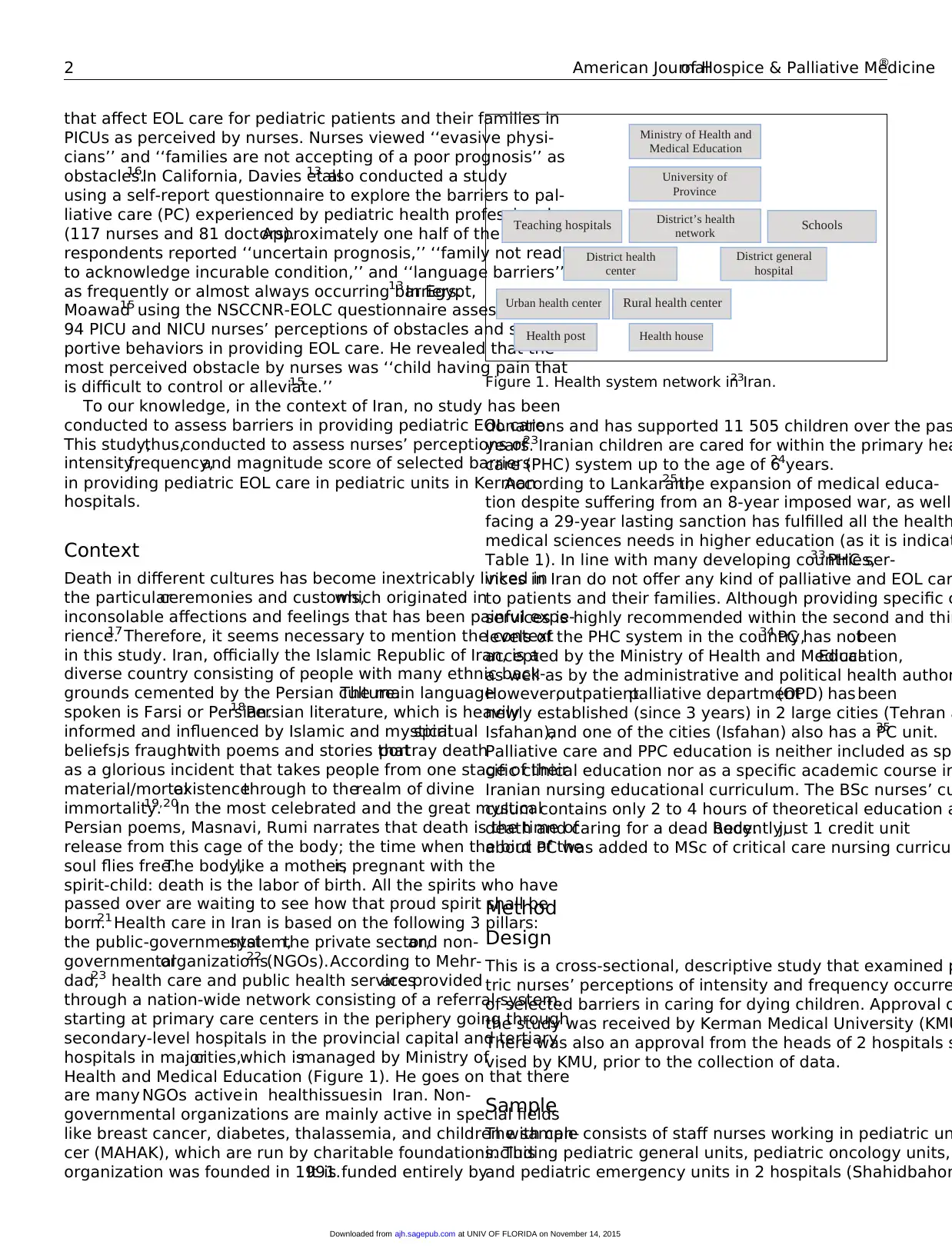
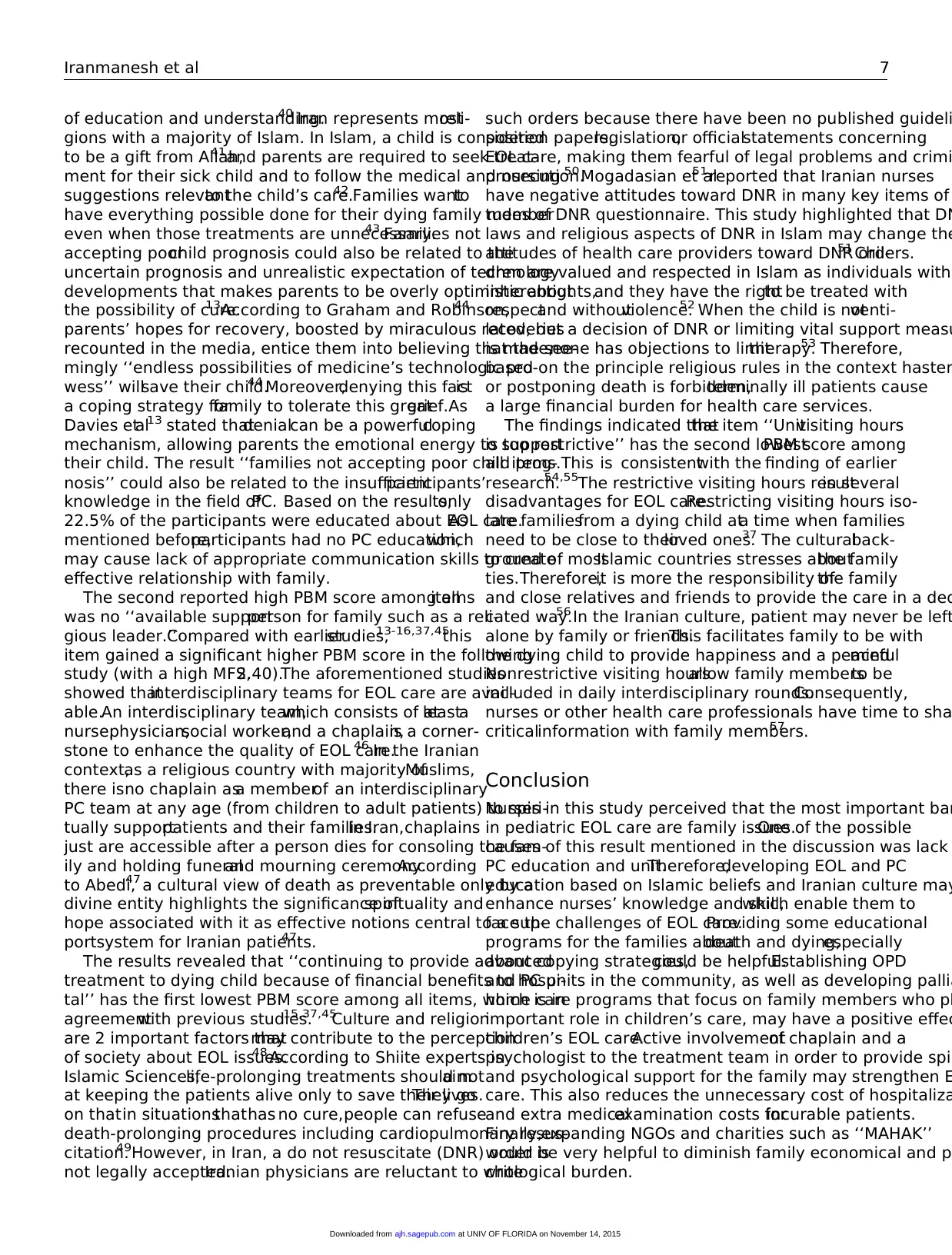
born.21 Health care in Iran is based on the following 3 pillars:
the public-governmentalsystem,the private sector,and non-
governmentalorganizations22 (NGOs).According to Mehr-
dad,23 health care and public health servicesare provided
through a nation-wide network consisting of a referral system,
starting at primary care centers in the periphery going through
secondary-level hospitals in the provincial capital and tertiary
hospitals in majorcities,which is.managed by Ministry of
Health and Medical Education (Figure 1). He goes on that there
are many NGOs activein healthissuesin Iran. Non-
governmental organizations are mainly active in special fields
like breast cancer, diabetes, thalassemia, and children with can-
cer (MAHAK), which are run by charitable foundations. This
organization was founded in 1991.It is funded entirely by
donations and has supported 11 505 children over the pas
years.23Iranian children are cared for within the primary hea
care (PHC) system up to the age of 6 years.24
According to Lankarani,25the expansion of medical educa-
tion despite suffering from an 8-year imposed war, as well
facing a 29-year lasting sanction has fulfilled all the health
medical sciences needs in higher education (as it is indicat
Table 1). In line with many developing countries,33 PHC ser-
vices in Iran do not offer any kind of palliative and EOL car
to patients and their families. Although providing specific c
services is highly recommended within the second and thir
levels of the PHC system in the country,34 PC has notbeen
accepted by the Ministry of Health and MedicalEducation,
as well as by the administrative and political health author
However,outpatientpalliative department(OPD) hasbeen
newly established (since 3 years) in 2 large cities (Tehran a
Isfahan),and one of the cities (Isfahan) also has a PC unit.35
Palliative care and PPC education is neither included as spe
cific clinical education nor as a specific academic course in
Iranian nursing educational curriculum. The BSc nurses’ cu
culum contains only 2 to 4 hours of theoretical education a
death and caring for a dead body.Recently,just 1 credit unit
about PC was added to MSc of critical care nursing curricul
Method
Design
This is a cross-sectional, descriptive study that examined p
tric nurses’ perceptions of intensity and frequency occurre
of selected barriers in caring for dying children. Approval o
the study was received by Kerman Medical University (KMU
There was also an approval from the heads of 2 hospitals s
vised by KMU, prior to the collection of data.
Sample
The sample consists of staff nurses working in pediatric un
including pediatric general units, pediatric oncology units,
and pediatric emergency units in 2 hospitals (Shahidbahon
University of
Province
SchoolsTeaching hospitals
District general
hospital
District’s health
network
District health
center
Urban health center
Health post
Rural health center
Health house
Ministry of Health and
Medical Education
Figure 1. Health system network in Iran.23
2 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
PICUs as perceived by nurses. Nurses viewed ‘‘evasive physi-
cians’’ and ‘‘families are not accepting of a poor prognosis’’ as
obstacles.16In California, Davies et al13also conducted a study
using a self-report questionnaire to explore the barriers to pal-
liative care (PC) experienced by pediatric health professionals
(117 nurses and 81 doctors).Approximately one half of the
respondents reported ‘‘uncertain prognosis,’’ ‘‘family not ready
to acknowledge incurable condition,’’ and ‘‘language barriers’’
as frequently or almost always occurring barriers.13 In Egypt,
Moawad15 using the NSCCNR-EOLC questionnaire assessed
94 PICU and NICU nurses’ perceptions of obstacles and sup-
portive behaviors in providing EOL care. He revealed that the
most perceived obstacle by nurses was ‘‘child having pain that
is difficult to control or alleviate.’’15
To our knowledge, in the context of Iran, no study has been
conducted to assess barriers in providing pediatric EOL care.
This study,thus,conducted to assess nurses’ perceptions of
intensity,frequency,and magnitude score of selected barriers
in providing pediatric EOL care in pediatric units in Kerman
hospitals.
Context
Death in different cultures has become inextricably linked in
the particularceremonies and customs,which originated in
inconsolable affections and feelings that has been painful expe-
rience.17 Therefore, it seems necessary to mention the context
in this study. Iran, officially the Islamic Republic of Iran, is a
diverse country consisting of people with many ethnic back-
grounds cemented by the Persian culture.The main language
spoken is Farsi or Persian.18Persian literature, which is heavily
informed and influenced by Islamic and mysticalspiritual
beliefs,is fraughtwith poems and stories thatportray death
as a glorious incident that takes people from one stage of their
material/mortalexistencethrough to therealm of divine
immortality.19,20
In the most celebrated and the great mystical
Persian poems, Masnavi, Rumi narrates that death is the time of
release from this cage of the body; the time when the bird of the
soul flies free.The body,like a mother,is pregnant with the
spirit-child: death is the labor of birth. All the spirits who have
passed over are waiting to see how that proud spirit shall be
born.21 Health care in Iran is based on the following 3 pillars:
the public-governmentalsystem,the private sector,and non-
governmentalorganizations22 (NGOs).According to Mehr-
dad,23 health care and public health servicesare provided
through a nation-wide network consisting of a referral system,
starting at primary care centers in the periphery going through
secondary-level hospitals in the provincial capital and tertiary
hospitals in majorcities,which is.managed by Ministry of
Health and Medical Education (Figure 1). He goes on that there
are many NGOs activein healthissuesin Iran. Non-
governmental organizations are mainly active in special fields
like breast cancer, diabetes, thalassemia, and children with can-
cer (MAHAK), which are run by charitable foundations. This
organization was founded in 1991.It is funded entirely by
donations and has supported 11 505 children over the pas
years.23Iranian children are cared for within the primary hea
care (PHC) system up to the age of 6 years.24
According to Lankarani,25the expansion of medical educa-
tion despite suffering from an 8-year imposed war, as well
facing a 29-year lasting sanction has fulfilled all the health
medical sciences needs in higher education (as it is indicat
Table 1). In line with many developing countries,33 PHC ser-
vices in Iran do not offer any kind of palliative and EOL car
to patients and their families. Although providing specific c
services is highly recommended within the second and thir
levels of the PHC system in the country,34 PC has notbeen
accepted by the Ministry of Health and MedicalEducation,
as well as by the administrative and political health author
However,outpatientpalliative department(OPD) hasbeen
newly established (since 3 years) in 2 large cities (Tehran a
Isfahan),and one of the cities (Isfahan) also has a PC unit.35
Palliative care and PPC education is neither included as spe
cific clinical education nor as a specific academic course in
Iranian nursing educational curriculum. The BSc nurses’ cu
culum contains only 2 to 4 hours of theoretical education a
death and caring for a dead body.Recently,just 1 credit unit
about PC was added to MSc of critical care nursing curricul
Method
Design
This is a cross-sectional, descriptive study that examined p
tric nurses’ perceptions of intensity and frequency occurre
of selected barriers in caring for dying children. Approval o
the study was received by Kerman Medical University (KMU
There was also an approval from the heads of 2 hospitals s
vised by KMU, prior to the collection of data.
Sample
The sample consists of staff nurses working in pediatric un
including pediatric general units, pediatric oncology units,
and pediatric emergency units in 2 hospitals (Shahidbahon
University of
Province
SchoolsTeaching hospitals
District general
hospital
District’s health
network
District health
center
Urban health center
Health post
Rural health center
Health house
Ministry of Health and
Medical Education
Figure 1. Health system network in Iran.23
2 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
Afzalipour) supervised by KMU. Afzalipour is a general hos-
pital with 462 active beds and Shahidbahonar is a trauma hos-
pital with 367 active beds. These hospitals located in an area
called Kerman in the center of Kerman Province in Southeast
Iran, which provides medical services for the whole province.
All nurses working in the aforementioned units were surveyed.
Staff nurses who were considered eligible for the study had at
least six-months working experience in these units and pro
vided care to dying children.
Background Information
First,a demographic questionnaire consisting of 17 questio
thatwas assumed to influence pediatric nurses’perceptions
Table 1. Health Indicators in Iran.
Indicators Rate Indicators Rate
Population26 77 352 373 Life expectancy,average (years)27 71.4
World population rank 17th Totalhealth care spending in 2013.28 US$50 billion
World area rank 18th Localhealth services accessibility27 Urban 100%,Rural86%
Religion,% World health care system rank28 45th
Shia Muslim 89 Health houses/inhabitants 1 /1200
SuniMuslim 10 Health Houses/inhabitants 1/1200
Christian,Zoroastrian,Bahai,and Jewish 1 RuralHealth Centers/inhabitants29 1/7000
Mortality rate/1000 live births Health care coverage27 73% of totalpopulation
Infants 18.9 Medicalschools30 52
Under 5 years 22 Medicalstudents 1 million
Cause of death in children under 5 years,%31 Professor of medicine 20 000
Prematurity 23 Hospitalbeds 120 000
Congenitalanomalies 19 Village clinics 20 000
Other disease 15 Doctors 100 000
Acute respiratory infections 13 Nurses 120 000
Birth asphyxia 11
Injuries 7
Neonatalsepsis 4
Diarrhea 4
Under 5 years cancer rate annualy32 1500-2000
0
1
2
3
4
5
6
7
8
9
5.04
4.97
4.96
4.9
4.86
4.68
4.33
4.26
4.2
4.12
4.07
4.03
3.94
3.93
3.67
3.65
3.5
3.41
3.39
3.37
3.23
3.24
2.96
2.94
2.87
2.73
2.52
2.51
2.25
2.19
P
B
M
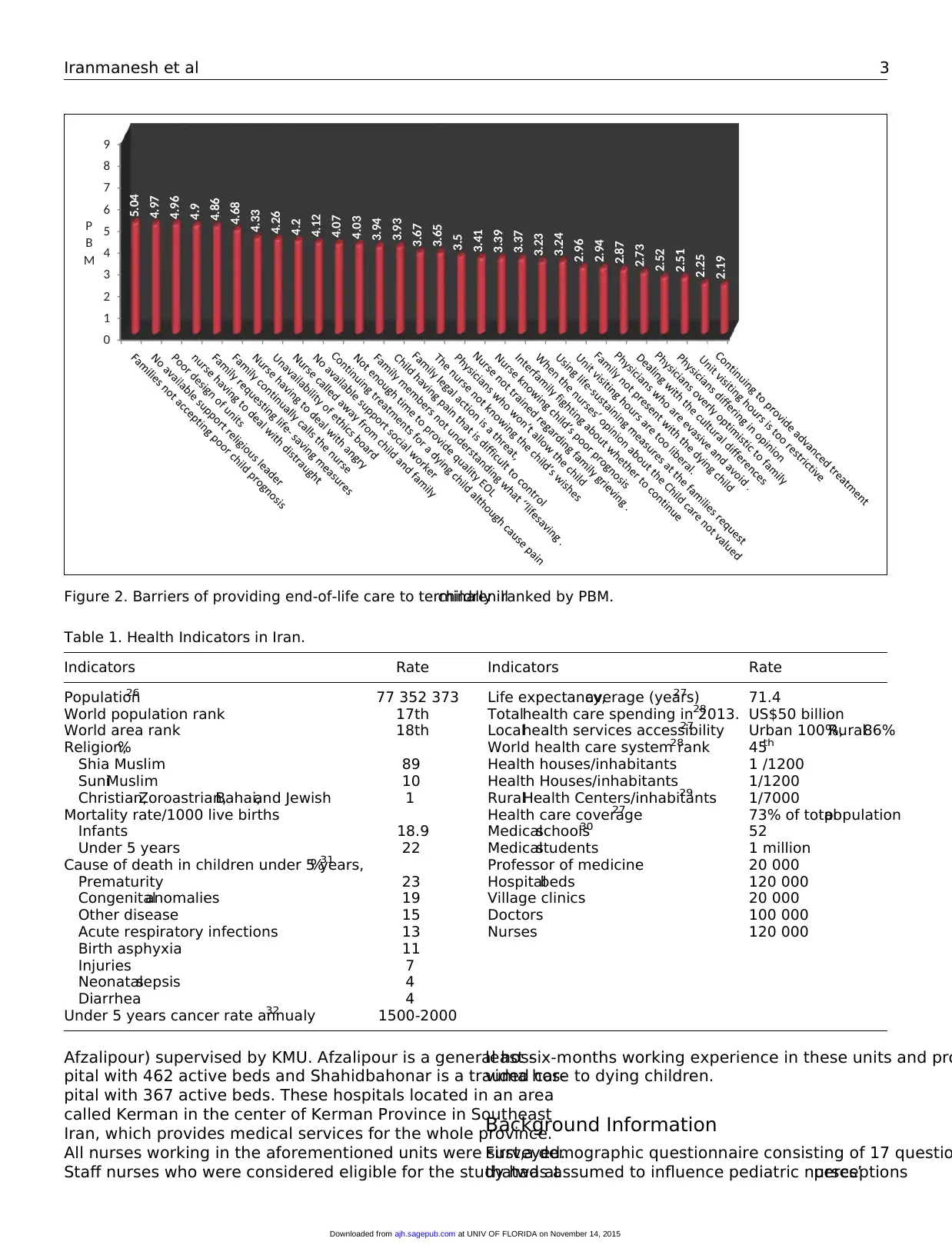
Figure 2. Barriers of providing end-of-life care to terminally illchildren ranked by PBM.
Iranmanesh et al 3
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
pital with 462 active beds and Shahidbahonar is a trauma hos-
pital with 367 active beds. These hospitals located in an area
called Kerman in the center of Kerman Province in Southeast
Iran, which provides medical services for the whole province.
All nurses working in the aforementioned units were surveyed.
Staff nurses who were considered eligible for the study had at
least six-months working experience in these units and pro
vided care to dying children.
Background Information
First,a demographic questionnaire consisting of 17 questio
thatwas assumed to influence pediatric nurses’perceptions
Table 1. Health Indicators in Iran.
Indicators Rate Indicators Rate
Population26 77 352 373 Life expectancy,average (years)27 71.4
World population rank 17th Totalhealth care spending in 2013.28 US$50 billion
World area rank 18th Localhealth services accessibility27 Urban 100%,Rural86%
Religion,% World health care system rank28 45th
Shia Muslim 89 Health houses/inhabitants 1 /1200
SuniMuslim 10 Health Houses/inhabitants 1/1200
Christian,Zoroastrian,Bahai,and Jewish 1 RuralHealth Centers/inhabitants29 1/7000
Mortality rate/1000 live births Health care coverage27 73% of totalpopulation
Infants 18.9 Medicalschools30 52
Under 5 years 22 Medicalstudents 1 million
Cause of death in children under 5 years,%31 Professor of medicine 20 000
Prematurity 23 Hospitalbeds 120 000
Congenitalanomalies 19 Village clinics 20 000
Other disease 15 Doctors 100 000
Acute respiratory infections 13 Nurses 120 000
Birth asphyxia 11
Injuries 7
Neonatalsepsis 4
Diarrhea 4
Under 5 years cancer rate annualy32 1500-2000
0
1
2
3
4
5
6
7
8
9
5.04
4.97
4.96
4.9
4.86
4.68
4.33
4.26
4.2
4.12
4.07
4.03
3.94
3.93
3.67
3.65
3.5
3.41
3.39
3.37
3.23
3.24
2.96
2.94
2.87
2.73
2.52
2.51
2.25
2.19
P
B
M
Figure 2. Barriers of providing end-of-life care to terminally illchildren ranked by PBM.
Iranmanesh et al 3
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

of barriers in providing pediatric EOL care was designed. The
questions developed were based on previous literature review
and authors’ experiences.The items included the following 4
categories: (1) personal characteristics like gender,age,mar-
riage status, and level of education; (2) professional character-
istics like ward, work hours per week, number, and age range of
dying children who were cared for;(3) previouspersonal
experiences related to death and dying,such as family and
closed friends’ death experience,dying family member care
experience, duration of caring for a dying family member, and
personal EOL care education; and (4) religiosity index consist-
ing of intrinsic (belief in God) and extrinsic (attendance at reli-
gious services and activities) religiosity.
Instrument
To determine pediatric nurses’perceptions ofintensity,fre-
quency occurrence,and magnitude score of selected barriers
in providing pediatric EOL care, a translated modified version
of the NSCCNR-EOLC questionnaire was used. This question-
naire was developed, pretested, and administered in 1998 and
revised in 2005.36 The final version of questionnaire consists
of 56 items including 29 obstacle items,24 supportive beha-
viors,and 3 open-ended questions.37 Separate responses are
required for intensity and frequency. Barriers intensity and fre-
quency were rated on a 6-pointLikert-type scale.For this
study, the 6 intensity and frequency alternatives in the original
article were grouped together in a single category, and 6 levels
were reduced to 4 levels including 0 ¼ not a barrier, 1 ¼ little
barrier,2 ¼ moderate barrier,and 3 ¼ large barrier and 0 ¼
never happens,1 ¼ rarely happens,2 ¼ sometimes happens,
and 3 ¼ always happens.The items are ranked from highest
to lowest based on their mean scores to determine which items
are perceived to be the mostintense obstacles or supportive
behaviors and which items are perceived to occur mostfre-
quent. To determine which barrier items were perceived as the
most intense and the most frequently occurring, the mean inten-
sity score (MIS) of each item was multiplied by the item’s
mean frequency score (MFS) to achieve an overall perceived
barriers magnitude (PBM) score. The possible perceived mag-
nitude score for each item ranged from 0 to 25 and for the fol-
lowing study 0 to 9. For the current study, facilitator items and
3 open-ended questions were omitted and just barriers subscale
was used. For translation of the questionnaire from English into
Farsi,the standard forward-backward procedure was applied.
Translation of the items was performed by 2 professional trans-
lators (SI and MAF) who are nurse educators. Their native lan-
guage is Farsi,and their second language is English.Both of
them have had experience of living abroad,and SI was edu-
cated about PC in a Western country for 5 years. Therefore, she
has knowledge about EOL and PC in both Eastern and Western
cultures.A helpful reference atthis stage wasthe Haiiem
English-Farsi dictionary. Based on their religious beliefs, they
suggested that it is better to divide the item ‘‘Family not having
a support person, for example, social worker or religious leader’’
to 2 items including family not having a support person,for
example, social worker and family not having a support pe
for example,religious leader.They believed thateach item
should not be devoted to more than one concept.Therefore,
the totalbarriers were 30 items.Afterward they were back-
translated into English, and after a careful cultural adaptat
the final versions were provided. The translated questionn
wentthrough pilottesting.Suggestions by nurses (n ¼ 20)
were combined into the final questionnaire versions.
Reliability and Validity
Reliability and content validity for NSCCNR-EOLC has been
checked in previous research.27The authors found an accepta-
ble validity and reliability for the instrument. In Iran, no stu
was found that assessed the reliability and validity of this s
therefore,the validity and reliabilityof the scale was
rechecked. The validity of scale was assessed through a co
validity.Ten faculty members at the Nursing and Midwifery
School reviewed the contents of the scales from cultural an
religious perspectives.They leftthe same suggestions as the
translators. They agreed that the translated scale has an a
table validity. These experts were also asked to independe
rate each item in terms of its relevance, clarity, and simpli
on a 4-point scale. According to their comments, to reasse
reliability of translated scale, an a coefficient of internal co
sistency (n ¼ 20) was computed. The a coefficient for the
was 0.91. Therefore, the translated scale presented accep
reliability.The questionnaire obtained an acceptable validity
(content validity index [CVI] ¼ 0.92) for barriers section an
for facilitators section (CVI ¼ 0.89).
Data Collection and Analysis
Accompanied by a letter, including some information abou
aim of the study, the questionnaires were handed out by th
ond author to all the convenient staff nurses (registered nu
and auxiliary nurses) working in the mentioned pediatric u
during the 2 months (November/December 2013).Some oral
information aboutthe study was also given by the second
author to all participants in a seminar. Informed consent fo
was obtained from allthe participants.Participation in the
study was voluntary and anonymous. In total, 173 sets of q
tionnaires were distributed with a dropout of 22.Finally,151
nurses (response rate, 87.2%) were included in the study.
from the questionnaires were analyzed using Statistical Pa
age for SocialScientists (SPSS version 21).A Kolmogorov-
Smirnov test indicated that the data were extracted from a
ulation with a normaldistribution descriptive statistics was
computed for the study variables. Mean scores were indivi
ally computed for the intensity and frequency for each item
Items were ranked according to their mean scores to deter
which ones were perceived as the most intense barriers, a
as the most frequent barriers. In addition, the PBM scores
ranked from highest to lowest.Based on the purposes of this
study,emphasis was placed on the overallmagnitude scores
to answer the research questions (Table 2).
4 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
questions developed were based on previous literature review
and authors’ experiences.The items included the following 4
categories: (1) personal characteristics like gender,age,mar-
riage status, and level of education; (2) professional character-
istics like ward, work hours per week, number, and age range of
dying children who were cared for;(3) previouspersonal
experiences related to death and dying,such as family and
closed friends’ death experience,dying family member care
experience, duration of caring for a dying family member, and
personal EOL care education; and (4) religiosity index consist-
ing of intrinsic (belief in God) and extrinsic (attendance at reli-
gious services and activities) religiosity.
Instrument
To determine pediatric nurses’perceptions ofintensity,fre-
quency occurrence,and magnitude score of selected barriers
in providing pediatric EOL care, a translated modified version
of the NSCCNR-EOLC questionnaire was used. This question-
naire was developed, pretested, and administered in 1998 and
revised in 2005.36 The final version of questionnaire consists
of 56 items including 29 obstacle items,24 supportive beha-
viors,and 3 open-ended questions.37 Separate responses are
required for intensity and frequency. Barriers intensity and fre-
quency were rated on a 6-pointLikert-type scale.For this
study, the 6 intensity and frequency alternatives in the original
article were grouped together in a single category, and 6 levels
were reduced to 4 levels including 0 ¼ not a barrier, 1 ¼ little
barrier,2 ¼ moderate barrier,and 3 ¼ large barrier and 0 ¼
never happens,1 ¼ rarely happens,2 ¼ sometimes happens,
and 3 ¼ always happens.The items are ranked from highest
to lowest based on their mean scores to determine which items
are perceived to be the mostintense obstacles or supportive
behaviors and which items are perceived to occur mostfre-
quent. To determine which barrier items were perceived as the
most intense and the most frequently occurring, the mean inten-
sity score (MIS) of each item was multiplied by the item’s
mean frequency score (MFS) to achieve an overall perceived
barriers magnitude (PBM) score. The possible perceived mag-
nitude score for each item ranged from 0 to 25 and for the fol-
lowing study 0 to 9. For the current study, facilitator items and
3 open-ended questions were omitted and just barriers subscale
was used. For translation of the questionnaire from English into
Farsi,the standard forward-backward procedure was applied.
Translation of the items was performed by 2 professional trans-
lators (SI and MAF) who are nurse educators. Their native lan-
guage is Farsi,and their second language is English.Both of
them have had experience of living abroad,and SI was edu-
cated about PC in a Western country for 5 years. Therefore, she
has knowledge about EOL and PC in both Eastern and Western
cultures.A helpful reference atthis stage wasthe Haiiem
English-Farsi dictionary. Based on their religious beliefs, they
suggested that it is better to divide the item ‘‘Family not having
a support person, for example, social worker or religious leader’’
to 2 items including family not having a support person,for
example, social worker and family not having a support pe
for example,religious leader.They believed thateach item
should not be devoted to more than one concept.Therefore,
the totalbarriers were 30 items.Afterward they were back-
translated into English, and after a careful cultural adaptat
the final versions were provided. The translated questionn
wentthrough pilottesting.Suggestions by nurses (n ¼ 20)
were combined into the final questionnaire versions.
Reliability and Validity
Reliability and content validity for NSCCNR-EOLC has been
checked in previous research.27The authors found an accepta-
ble validity and reliability for the instrument. In Iran, no stu
was found that assessed the reliability and validity of this s
therefore,the validity and reliabilityof the scale was
rechecked. The validity of scale was assessed through a co
validity.Ten faculty members at the Nursing and Midwifery
School reviewed the contents of the scales from cultural an
religious perspectives.They leftthe same suggestions as the
translators. They agreed that the translated scale has an a
table validity. These experts were also asked to independe
rate each item in terms of its relevance, clarity, and simpli
on a 4-point scale. According to their comments, to reasse
reliability of translated scale, an a coefficient of internal co
sistency (n ¼ 20) was computed. The a coefficient for the
was 0.91. Therefore, the translated scale presented accep
reliability.The questionnaire obtained an acceptable validity
(content validity index [CVI] ¼ 0.92) for barriers section an
for facilitators section (CVI ¼ 0.89).
Data Collection and Analysis
Accompanied by a letter, including some information abou
aim of the study, the questionnaires were handed out by th
ond author to all the convenient staff nurses (registered nu
and auxiliary nurses) working in the mentioned pediatric u
during the 2 months (November/December 2013).Some oral
information aboutthe study was also given by the second
author to all participants in a seminar. Informed consent fo
was obtained from allthe participants.Participation in the
study was voluntary and anonymous. In total, 173 sets of q
tionnaires were distributed with a dropout of 22.Finally,151
nurses (response rate, 87.2%) were included in the study.
from the questionnaires were analyzed using Statistical Pa
age for SocialScientists (SPSS version 21).A Kolmogorov-
Smirnov test indicated that the data were extracted from a
ulation with a normaldistribution descriptive statistics was
computed for the study variables. Mean scores were indivi
ally computed for the intensity and frequency for each item
Items were ranked according to their mean scores to deter
which ones were perceived as the most intense barriers, a
as the most frequent barriers. In addition, the PBM scores
ranked from highest to lowest.Based on the purposes of this
study,emphasis was placed on the overallmagnitude scores
to answer the research questions (Table 2).
4 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Results
Participants
The sample consisted of 151 participants. A descriptive analy-
sis of background information (Table 3) revealed that the par-
ticipants’ age ranged from 20 to 65 years with a mean age of
32.7 years (standard deviation [SD] ¼ 6.12). They were mainly
female (98.7%) and married (80.1). Most of them had a B Sc in
nursing (82.1) and stated that they receive no education about
EOL care (77.5%).Approximately half (54.3) of participants
were working in non-ICUs including pediatric generalunits,
pediatric oncology units,and pediatric emergency unit.Rest
(45.7)of them wasworking in PICUs. The participants
reported that they had experience of 0.5 to 31 years in nu
with a mean of 8.7 years (SD ¼ 6.63). All the participants e
rienced caring for dying children. More than half (62.9) of t
cared for less than 10 dying children during their professio
career. The age of less than half of the dying pediatric pati
(42.4) ranged between 2 and 5 years. Reported weekly em
menthours ranged from less than 30 hours to more than 40
hours;46% ofthe participants worked more than 40 hours
weekly;25.8% ofthe participants experienced caring fora
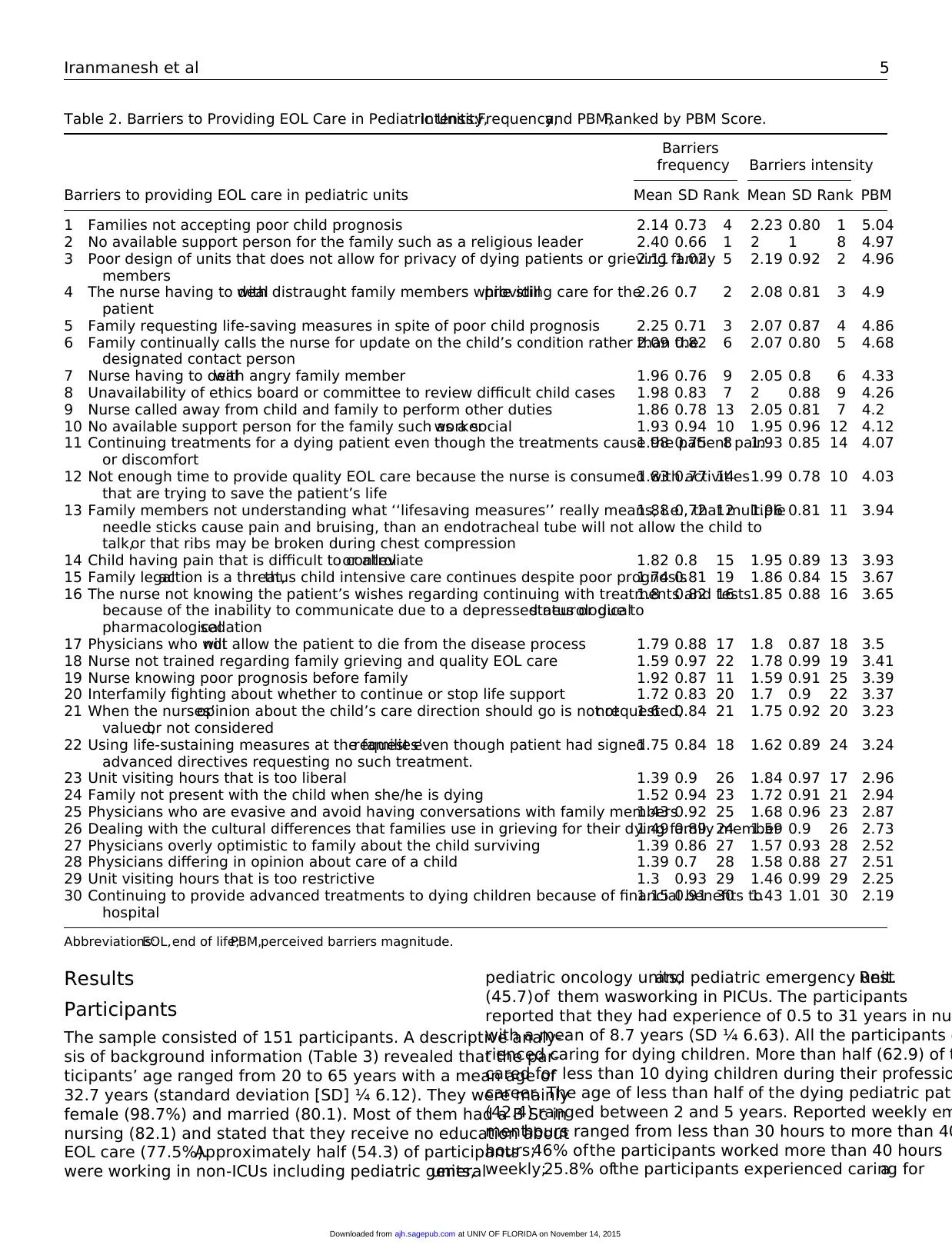
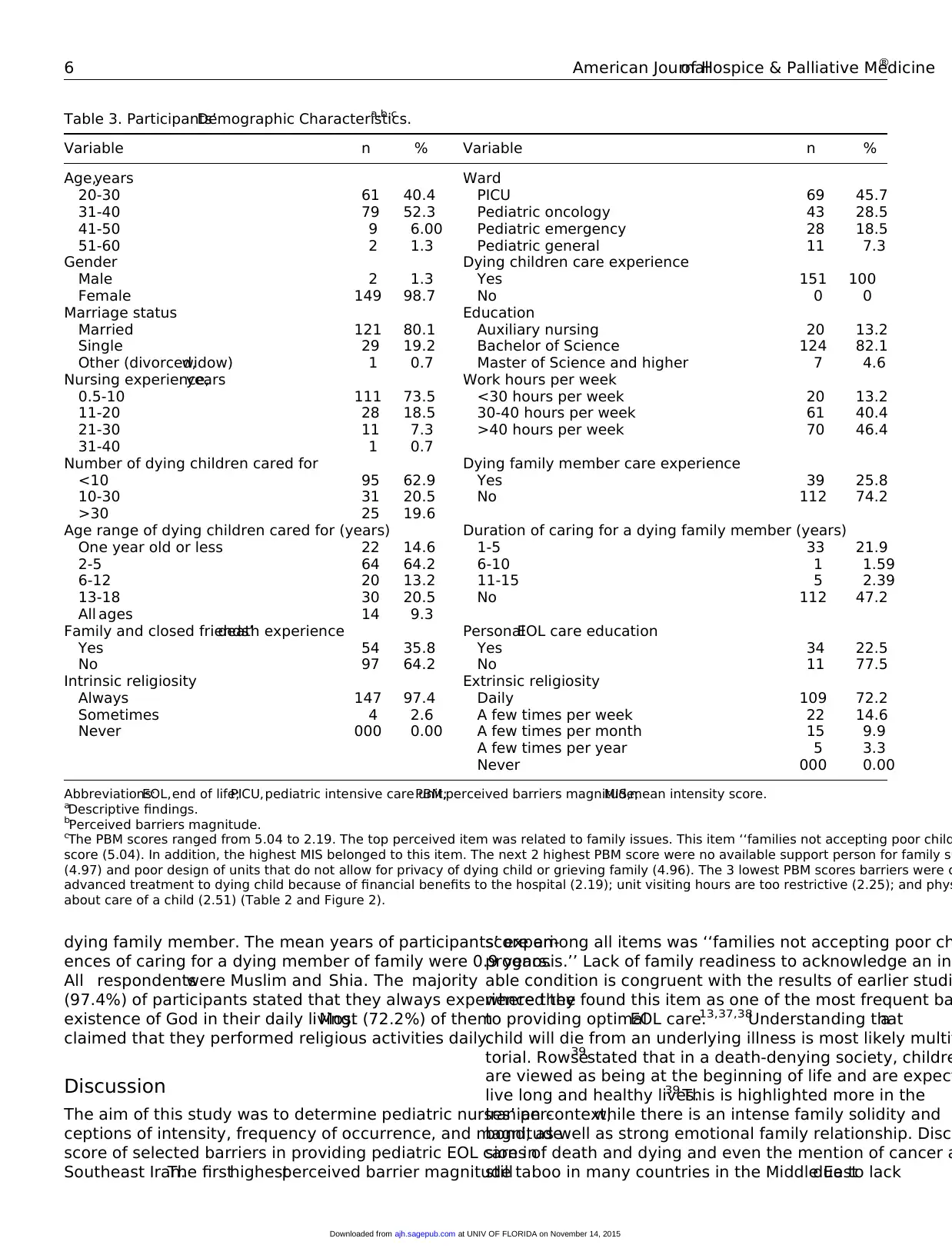
Table 2. Barriers to Providing EOL Care in Pediatric Units:Intensity,Frequency,and PBM,Ranked by PBM Score.
Barriers to providing EOL care in pediatric units
Barriers
frequency Barriers intensity
PBMMean SD Rank Mean SD Rank
1 Families not accepting poor child prognosis 2.14 0.73 4 2.23 0.80 1 5.04
2 No available support person for the family such as a religious leader 2.40 0.66 1 2 1 8 4.97
3 Poor design of units that does not allow for privacy of dying patients or grieving family
members
2.11 1.02 5 2.19 0.92 2 4.96
4 The nurse having to dealwith distraught family members while stillproviding care for the
patient
2.26 0.7 2 2.08 0.81 3 4.9
5 Family requesting life-saving measures in spite of poor child prognosis 2.25 0.71 3 2.07 0.87 4 4.86
6 Family continually calls the nurse for update on the child’s condition rather than the
designated contact person
2.09 0.82 6 2.07 0.80 5 4.68
7 Nurse having to dealwith angry family member 1.96 0.76 9 2.05 0.8 6 4.33
8 Unavailability of ethics board or committee to review difficult child cases 1.98 0.83 7 2 0.88 9 4.26
9 Nurse called away from child and family to perform other duties 1.86 0.78 13 2.05 0.81 7 4.2
10 No available support person for the family such as a socialworker 1.93 0.94 10 1.95 0.96 12 4.12
11 Continuing treatments for a dying patient even though the treatments cause the patient pain
or discomfort
1.98 0.75 8 1.93 0.85 14 4.07
12 Not enough time to provide quality EOL care because the nurse is consumed with activities
that are trying to save the patient’s life
1.83 0.77 14 1.99 0.78 10 4.03
13 Family members not understanding what ‘‘lifesaving measures’’ really means, i.e., that multiple
needle sticks cause pain and bruising, than an endotracheal tube will not allow the child to
talk,or that ribs may be broken during chest compression
1.88 0.72 12 1.96 0.81 11 3.94
14 Child having pain that is difficult to controlor alleviate 1.82 0.8 15 1.95 0.89 13 3.93
15 Family legalaction is a threat,thus child intensive care continues despite poor prognosis1.74 0.81 19 1.86 0.84 15 3.67
16 The nurse not knowing the patient’s wishes regarding continuing with treatments and tests
because of the inability to communicate due to a depressed neurologicalstatus or due to
pharmacologicalsedation
1.8 0.82 16 1.85 0.88 16 3.65
17 Physicians who willnot allow the patient to die from the disease process 1.79 0.88 17 1.8 0.87 18 3.5
18 Nurse not trained regarding family grieving and quality EOL care 1.59 0.97 22 1.78 0.99 19 3.41
19 Nurse knowing poor prognosis before family 1.92 0.87 11 1.59 0.91 25 3.39
20 Interfamily fighting about whether to continue or stop life support 1.72 0.83 20 1.7 0.9 22 3.37
21 When the nurses’opinion about the child’s care direction should go is not requested,not
valued,or not considered
1.6 0.84 21 1.75 0.92 20 3.23
22 Using life-sustaining measures at the families’request even though patient had signed
advanced directives requesting no such treatment.
1.75 0.84 18 1.62 0.89 24 3.24
23 Unit visiting hours that is too liberal 1.39 0.9 26 1.84 0.97 17 2.96
24 Family not present with the child when she/he is dying 1.52 0.94 23 1.72 0.91 21 2.94
25 Physicians who are evasive and avoid having conversations with family members1.43 0.92 25 1.68 0.96 23 2.87
26 Dealing with the cultural differences that families use in grieving for their dying family member1.49 0.89 24 1.59 0.9 26 2.73
27 Physicians overly optimistic to family about the child surviving 1.39 0.86 27 1.57 0.93 28 2.52
28 Physicians differing in opinion about care of a child 1.39 0.7 28 1.58 0.88 27 2.51
29 Unit visiting hours that is too restrictive 1.3 0.93 29 1.46 0.99 29 2.25
30 Continuing to provide advanced treatments to dying children because of financial benefits to
hospital
1.15 0.91 30 1.43 1.01 30 2.19
Abbreviations:EOL,end of life;PBM,perceived barriers magnitude.
Iranmanesh et al 5
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
Participants
The sample consisted of 151 participants. A descriptive analy-
sis of background information (Table 3) revealed that the par-
ticipants’ age ranged from 20 to 65 years with a mean age of
32.7 years (standard deviation [SD] ¼ 6.12). They were mainly
female (98.7%) and married (80.1). Most of them had a B Sc in
nursing (82.1) and stated that they receive no education about
EOL care (77.5%).Approximately half (54.3) of participants
were working in non-ICUs including pediatric generalunits,
pediatric oncology units,and pediatric emergency unit.Rest
(45.7)of them wasworking in PICUs. The participants
reported that they had experience of 0.5 to 31 years in nu
with a mean of 8.7 years (SD ¼ 6.63). All the participants e
rienced caring for dying children. More than half (62.9) of t
cared for less than 10 dying children during their professio
career. The age of less than half of the dying pediatric pati
(42.4) ranged between 2 and 5 years. Reported weekly em
menthours ranged from less than 30 hours to more than 40
hours;46% ofthe participants worked more than 40 hours
weekly;25.8% ofthe participants experienced caring fora
Table 2. Barriers to Providing EOL Care in Pediatric Units:Intensity,Frequency,and PBM,Ranked by PBM Score.
Barriers to providing EOL care in pediatric units
Barriers
frequency Barriers intensity
PBMMean SD Rank Mean SD Rank
1 Families not accepting poor child prognosis 2.14 0.73 4 2.23 0.80 1 5.04
2 No available support person for the family such as a religious leader 2.40 0.66 1 2 1 8 4.97
3 Poor design of units that does not allow for privacy of dying patients or grieving family
members
2.11 1.02 5 2.19 0.92 2 4.96
4 The nurse having to dealwith distraught family members while stillproviding care for the
patient
2.26 0.7 2 2.08 0.81 3 4.9
5 Family requesting life-saving measures in spite of poor child prognosis 2.25 0.71 3 2.07 0.87 4 4.86
6 Family continually calls the nurse for update on the child’s condition rather than the
designated contact person
2.09 0.82 6 2.07 0.80 5 4.68
7 Nurse having to dealwith angry family member 1.96 0.76 9 2.05 0.8 6 4.33
8 Unavailability of ethics board or committee to review difficult child cases 1.98 0.83 7 2 0.88 9 4.26
9 Nurse called away from child and family to perform other duties 1.86 0.78 13 2.05 0.81 7 4.2
10 No available support person for the family such as a socialworker 1.93 0.94 10 1.95 0.96 12 4.12
11 Continuing treatments for a dying patient even though the treatments cause the patient pain
or discomfort
1.98 0.75 8 1.93 0.85 14 4.07
12 Not enough time to provide quality EOL care because the nurse is consumed with activities
that are trying to save the patient’s life
1.83 0.77 14 1.99 0.78 10 4.03
13 Family members not understanding what ‘‘lifesaving measures’’ really means, i.e., that multiple
needle sticks cause pain and bruising, than an endotracheal tube will not allow the child to
talk,or that ribs may be broken during chest compression
1.88 0.72 12 1.96 0.81 11 3.94
14 Child having pain that is difficult to controlor alleviate 1.82 0.8 15 1.95 0.89 13 3.93
15 Family legalaction is a threat,thus child intensive care continues despite poor prognosis1.74 0.81 19 1.86 0.84 15 3.67
16 The nurse not knowing the patient’s wishes regarding continuing with treatments and tests
because of the inability to communicate due to a depressed neurologicalstatus or due to
pharmacologicalsedation
1.8 0.82 16 1.85 0.88 16 3.65
17 Physicians who willnot allow the patient to die from the disease process 1.79 0.88 17 1.8 0.87 18 3.5
18 Nurse not trained regarding family grieving and quality EOL care 1.59 0.97 22 1.78 0.99 19 3.41
19 Nurse knowing poor prognosis before family 1.92 0.87 11 1.59 0.91 25 3.39
20 Interfamily fighting about whether to continue or stop life support 1.72 0.83 20 1.7 0.9 22 3.37
21 When the nurses’opinion about the child’s care direction should go is not requested,not
valued,or not considered
1.6 0.84 21 1.75 0.92 20 3.23
22 Using life-sustaining measures at the families’request even though patient had signed
advanced directives requesting no such treatment.
1.75 0.84 18 1.62 0.89 24 3.24
23 Unit visiting hours that is too liberal 1.39 0.9 26 1.84 0.97 17 2.96
24 Family not present with the child when she/he is dying 1.52 0.94 23 1.72 0.91 21 2.94
25 Physicians who are evasive and avoid having conversations with family members1.43 0.92 25 1.68 0.96 23 2.87
26 Dealing with the cultural differences that families use in grieving for their dying family member1.49 0.89 24 1.59 0.9 26 2.73
27 Physicians overly optimistic to family about the child surviving 1.39 0.86 27 1.57 0.93 28 2.52
28 Physicians differing in opinion about care of a child 1.39 0.7 28 1.58 0.88 27 2.51
29 Unit visiting hours that is too restrictive 1.3 0.93 29 1.46 0.99 29 2.25
30 Continuing to provide advanced treatments to dying children because of financial benefits to
hospital
1.15 0.91 30 1.43 1.01 30 2.19
Abbreviations:EOL,end of life;PBM,perceived barriers magnitude.
Iranmanesh et al 5
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
dying family member. The mean years of participants’ experi-
ences of caring for a dying member of family were 0.9 years.
All respondentswere Muslim and Shia. The majority
(97.4%) of participants stated that they always experienced the
existence of God in their daily living.Most (72.2%) of them
claimed that they performed religious activities daily.
Discussion
The aim of this study was to determine pediatric nurses’ per-
ceptions of intensity, frequency of occurrence, and magnitude
score of selected barriers in providing pediatric EOL care in
Southeast Iran.The firsthighestperceived barrier magnitude
score among all items was ‘‘families not accepting poor ch
prognosis.’’ Lack of family readiness to acknowledge an in
able condition is congruent with the results of earlier studi
where they found this item as one of the most frequent ba
to providing optimalEOL care.13,37,38
Understanding thata
child will die from an underlying illness is most likely multif
torial. Rowse39stated that in a death-denying society, childre
are viewed as being at the beginning of life and are expect
live long and healthy lives.39 This is highlighted more in the
Iranian context,while there is an intense family solidity and
bond, as well as strong emotional family relationship. Discu
sions of death and dying and even the mention of cancer a
still taboo in many countries in the Middle Eastdue to lack
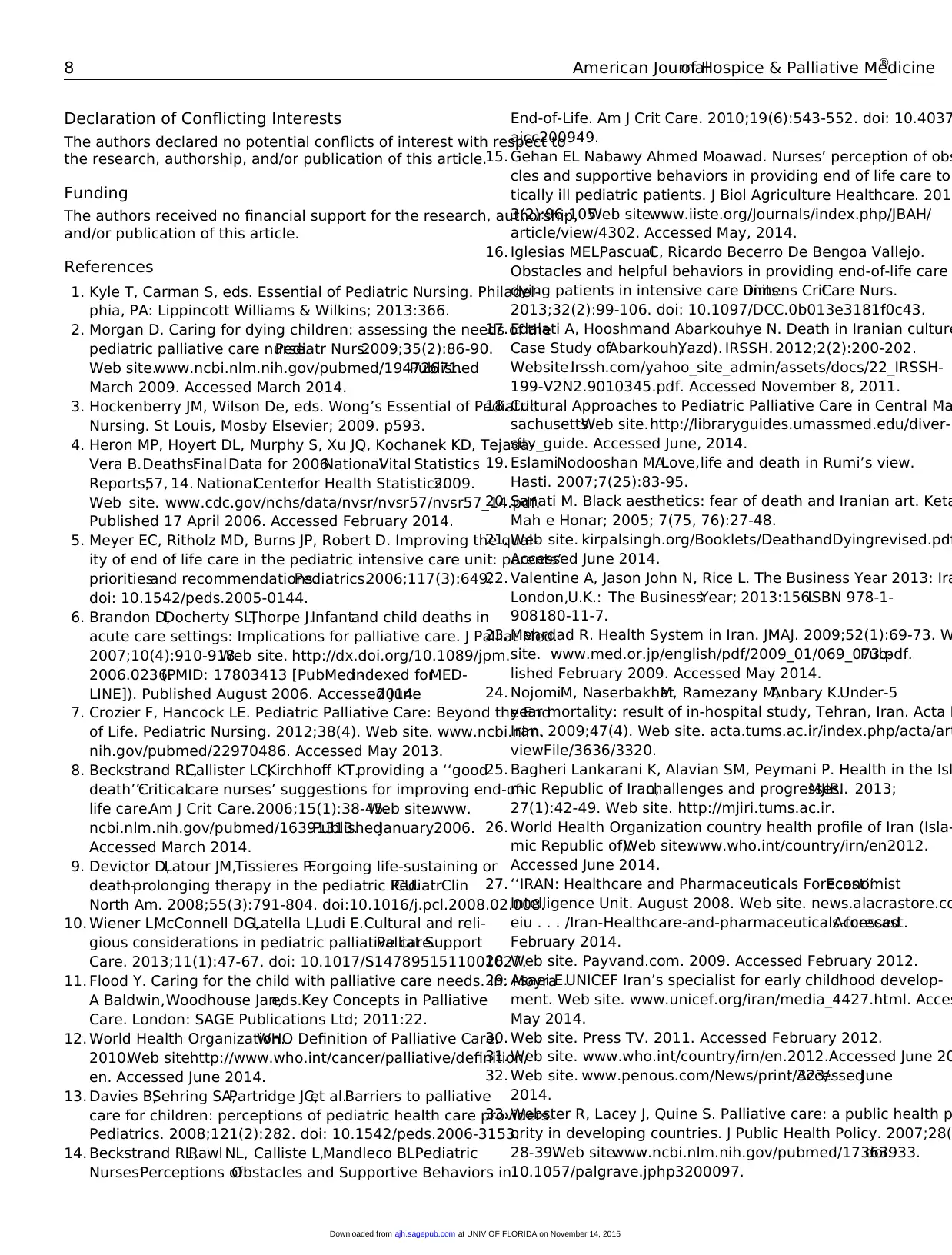
Table 3. Participants’Demographic Characteristics.a,b,c
Variable n % Variable n %
Age,years Ward
20-30 61 40.4 PICU 69 45.7
31-40 79 52.3 Pediatric oncology 43 28.5
41-50 9 6.00 Pediatric emergency 28 18.5
51-60 2 1.3 Pediatric general 11 7.3
Gender Dying children care experience
Male 2 1.3 Yes 151 100
Female 149 98.7 No 0 0
Marriage status Education
Married 121 80.1 Auxiliary nursing 20 13.2
Single 29 19.2 Bachelor of Science 124 82.1
Other (divorced,widow) 1 0.7 Master of Science and higher 7 4.6
Nursing experience,years Work hours per week
0.5-10 111 73.5 <30 hours per week 20 13.2
11-20 28 18.5 30-40 hours per week 61 40.4
21-30 11 7.3 >40 hours per week 70 46.4
31-40 1 0.7
Number of dying children cared for Dying family member care experience
<10 95 62.9 Yes 39 25.8
10-30 31 20.5 No 112 74.2
>30 25 19.6
Age range of dying children cared for (years) Duration of caring for a dying family member (years)
One year old or less 22 14.6 1-5 33 21.9
2-5 64 64.2 6-10 1 1.59
6-12 20 13.2 11-15 5 2.39
13-18 30 20.5 No 112 47.2
All ages 14 9.3
Family and closed friends’death experience PersonalEOL care education
Yes 54 35.8 Yes 34 22.5
No 97 64.2 No 11 77.5
Intrinsic religiosity Extrinsic religiosity
Always 147 97.4 Daily 109 72.2
Sometimes 4 2.6 A few times per week 22 14.6
Never 000 0.00 A few times per month 15 9.9
A few times per year 5 3.3
Never 000 0.00
Abbreviations:EOL,end of life;PICU,pediatric intensive care unit;PBM,perceived barriers magnitude;MIS,mean intensity score.
aDescriptive findings.
bPerceived barriers magnitude.
cThe PBM scores ranged from 5.04 to 2.19. The top perceived item was related to family issues. This item ‘‘families not accepting poor child
score (5.04). In addition, the highest MIS belonged to this item. The next 2 highest PBM score were no available support person for family su
(4.97) and poor design of units that do not allow for privacy of dying child or grieving family (4.96). The 3 lowest PBM scores barriers were c
advanced treatment to dying child because of financial benefits to the hospital (2.19); unit visiting hours are too restrictive (2.25); and phys
about care of a child (2.51) (Table 2 and Figure 2).
6 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
ences of caring for a dying member of family were 0.9 years.
All respondentswere Muslim and Shia. The majority
(97.4%) of participants stated that they always experienced the
existence of God in their daily living.Most (72.2%) of them
claimed that they performed religious activities daily.
Discussion
The aim of this study was to determine pediatric nurses’ per-
ceptions of intensity, frequency of occurrence, and magnitude
score of selected barriers in providing pediatric EOL care in
Southeast Iran.The firsthighestperceived barrier magnitude
score among all items was ‘‘families not accepting poor ch
prognosis.’’ Lack of family readiness to acknowledge an in
able condition is congruent with the results of earlier studi
where they found this item as one of the most frequent ba
to providing optimalEOL care.13,37,38
Understanding thata
child will die from an underlying illness is most likely multif
torial. Rowse39stated that in a death-denying society, childre
are viewed as being at the beginning of life and are expect
live long and healthy lives.39 This is highlighted more in the
Iranian context,while there is an intense family solidity and
bond, as well as strong emotional family relationship. Discu
sions of death and dying and even the mention of cancer a
still taboo in many countries in the Middle Eastdue to lack
Table 3. Participants’Demographic Characteristics.a,b,c
Variable n % Variable n %
Age,years Ward
20-30 61 40.4 PICU 69 45.7
31-40 79 52.3 Pediatric oncology 43 28.5
41-50 9 6.00 Pediatric emergency 28 18.5
51-60 2 1.3 Pediatric general 11 7.3
Gender Dying children care experience
Male 2 1.3 Yes 151 100
Female 149 98.7 No 0 0
Marriage status Education
Married 121 80.1 Auxiliary nursing 20 13.2
Single 29 19.2 Bachelor of Science 124 82.1
Other (divorced,widow) 1 0.7 Master of Science and higher 7 4.6
Nursing experience,years Work hours per week
0.5-10 111 73.5 <30 hours per week 20 13.2
11-20 28 18.5 30-40 hours per week 61 40.4
21-30 11 7.3 >40 hours per week 70 46.4
31-40 1 0.7
Number of dying children cared for Dying family member care experience
<10 95 62.9 Yes 39 25.8
10-30 31 20.5 No 112 74.2
>30 25 19.6
Age range of dying children cared for (years) Duration of caring for a dying family member (years)
One year old or less 22 14.6 1-5 33 21.9
2-5 64 64.2 6-10 1 1.59
6-12 20 13.2 11-15 5 2.39
13-18 30 20.5 No 112 47.2
All ages 14 9.3
Family and closed friends’death experience PersonalEOL care education
Yes 54 35.8 Yes 34 22.5
No 97 64.2 No 11 77.5
Intrinsic religiosity Extrinsic religiosity
Always 147 97.4 Daily 109 72.2
Sometimes 4 2.6 A few times per week 22 14.6
Never 000 0.00 A few times per month 15 9.9
A few times per year 5 3.3
Never 000 0.00
Abbreviations:EOL,end of life;PICU,pediatric intensive care unit;PBM,perceived barriers magnitude;MIS,mean intensity score.
aDescriptive findings.
bPerceived barriers magnitude.
cThe PBM scores ranged from 5.04 to 2.19. The top perceived item was related to family issues. This item ‘‘families not accepting poor child
score (5.04). In addition, the highest MIS belonged to this item. The next 2 highest PBM score were no available support person for family su
(4.97) and poor design of units that do not allow for privacy of dying child or grieving family (4.96). The 3 lowest PBM scores barriers were c
advanced treatment to dying child because of financial benefits to the hospital (2.19); unit visiting hours are too restrictive (2.25); and phys
about care of a child (2.51) (Table 2 and Figure 2).
6 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
of education and understanding.40 Iran represents mostreli-
gions with a majority of Islam. In Islam, a child is considered
to be a gift from Allah,41and parents are required to seek treat-
ment for their sick child and to follow the medical and nursing
suggestions relevantto the child’s care.42 Families wantto
have everything possible done for their dying family member
even when those treatments are unnecessary.43 Families not
accepting poorchild prognosis could also be related to the
uncertain prognosis and unrealistic expectation of technology
developments that makes parents to be overly optimistic about
the possibility of cure.13According to Graham and Robinson,44
parents’ hopes for recovery, boosted by miraculous recoveries
recounted in the media, entice them into believing that the see-
mingly ‘‘endless possibilities of medicine’s technologic pro-
wess’’ willsave their child.44 Moreover,denying this factis
a coping strategy forfamily to tolerate this greatgrief.As
Davies etal13 stated thatdenialcan be a powerfulcoping
mechanism, allowing parents the emotional energy to support
their child. The result ‘‘families not accepting poor child prog-
nosis’’ could also be related to the insufficientparticipants’
knowledge in the field ofPC. Based on the results,only
22.5% of the participants were educated about EOL care.As
mentioned before,participants had no PC education,which
may cause lack of appropriate communication skills to create
effective relationship with family.
The second reported high PBM score among allitems
was no ‘‘available supportperson for family such as a reli-
gious leader.’’Compared with earlierstudies,13-16,37,45
this
item gained a significant higher PBM score in the following
study (with a high MFS,2.40).The aforementioned studies
showed thatinterdisciplinary teams for EOL care are avail-
able.An interdisciplinary team,which consists of atleasta
nurse,physician,social worker,and a chaplain,is a corner-
stone to enhance the quality of EOL care.46 In the Iranian
context,as a religious country with majority ofMuslims,
there isno chaplain asa memberof an interdisciplinary
PC team at any age (from children to adult patients) to spiri-
tually supportpatients and their families.In Iran,chaplains
just are accessible after a person dies for consoling the fam-
ily and holding funeraland mourning ceremony.According
to Abedi,47 a cultural view of death as preventable only by a
divine entity highlights the significance ofspirituality and
hope associated with it as effective notions central to a sup-
portsystem for Iranian patients.47
The results revealed that ‘‘continuing to provide advanced
treatment to dying child because of financial benefits to hospi-
tal’’ has the first lowest PBM score among all items, which is in
agreementwith previous studies.15,37,45
Culture and religion
are 2 important factors thatmay contribute to the perception
of society about EOL issues.48 According to Shiite experts in
Islamic Sciences,life-prolonging treatments should notaim
at keeping the patients alive only to save their lives.They go
on thatin situationsthathas no cure,people can refuse
death-prolonging procedures including cardiopulmonary resus-
citation.49However, in Iran, a do not resuscitate (DNR) order is
not legally accepted.Iranian physicians are reluctant to write
such orders because there have been no published guideli
position papers,legislation,or officialstatements concerning
EOL care, making them fearful of legal problems and crimi
prosecution.50 Mogadasian et al51 reported that Iranian nurses
have negative attitudes toward DNR in many key items of
tudes of DNR questionnaire. This study highlighted that DN
laws and religious aspects of DNR in Islam may change the
attitudes of health care providers toward DNR orders.51 Chil-
dren are valued and respected in Islam as individuals with
inherentrights,and they have the rightto be treated with
respectand withoutviolence.52 When the child is notventi-
lated, but a decision of DNR or limiting vital support measu
is made,none has objections to limittherapy.53 Therefore,
based on the principle religious rules in the context hasten
or postponing death is forbidden,terminally ill patients cause
a large financial burden for health care services.
The findings indicated thatthe item ‘‘Unitvisiting hours
is too restrictive’’ has the second lowestPBM score among
all items.This is consistentwith the finding of earlier
research.54,55The restrictive visiting hours resultin several
disadvantages for EOL care.Restricting visiting hours iso-
late familiesfrom a dying child ata time when families
need to be close to theirloved ones.37 The culturalback-
ground of mostIslamic countries stresses aboutthe family
ties.Therefore,it is more the responsibility ofthe family
and close relatives and friends to provide the care in a ded
cated way.56 In the Iranian culture, patient may never be left
alone by family or friends.This facilitates family to be with
the dying child to provide happiness and a peacefulmind.
Nonrestrictive visiting hoursallow family membersto be
included in daily interdisciplinary rounds.Consequently,
nurses or other health care professionals have time to sha
criticalinformation with family members.57
Conclusion
Nurses in this study perceived that the most important bar
in pediatric EOL care are family issues.One of the possible
causes of this result mentioned in the discussion was lack
PC education and unit.Therefore,developing EOL and PC
education based on Islamic beliefs and Iranian culture may
enhance nurses’ knowledge and skill,which enable them to
face the challenges of EOL care.Providing some educational
programs for the families aboutdeath and dying,especially
about copying strategies,could be helpful.Establishing OPD
and PC units in the community, as well as developing pallia
home care programs that focus on family members who pl
important role in children’s care, may have a positive effec
children’s EOL care.Active involvementof chaplain and a
psychologist to the treatment team in order to provide spir
and psychological support for the family may strengthen E
care. This also reduces the unnecessary cost of hospitaliza
and extra medicalexamination costs forincurable patients.
Finally,expanding NGOs and charities such as ‘‘MAHAK’’
would be very helpful to diminish family economical and p
chological burden.
Iranmanesh et al 7
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
gions with a majority of Islam. In Islam, a child is considered
to be a gift from Allah,41and parents are required to seek treat-
ment for their sick child and to follow the medical and nursing
suggestions relevantto the child’s care.42 Families wantto
have everything possible done for their dying family member
even when those treatments are unnecessary.43 Families not
accepting poorchild prognosis could also be related to the
uncertain prognosis and unrealistic expectation of technology
developments that makes parents to be overly optimistic about
the possibility of cure.13According to Graham and Robinson,44
parents’ hopes for recovery, boosted by miraculous recoveries
recounted in the media, entice them into believing that the see-
mingly ‘‘endless possibilities of medicine’s technologic pro-
wess’’ willsave their child.44 Moreover,denying this factis
a coping strategy forfamily to tolerate this greatgrief.As
Davies etal13 stated thatdenialcan be a powerfulcoping
mechanism, allowing parents the emotional energy to support
their child. The result ‘‘families not accepting poor child prog-
nosis’’ could also be related to the insufficientparticipants’
knowledge in the field ofPC. Based on the results,only
22.5% of the participants were educated about EOL care.As
mentioned before,participants had no PC education,which
may cause lack of appropriate communication skills to create
effective relationship with family.
The second reported high PBM score among allitems
was no ‘‘available supportperson for family such as a reli-
gious leader.’’Compared with earlierstudies,13-16,37,45
this
item gained a significant higher PBM score in the following
study (with a high MFS,2.40).The aforementioned studies
showed thatinterdisciplinary teams for EOL care are avail-
able.An interdisciplinary team,which consists of atleasta
nurse,physician,social worker,and a chaplain,is a corner-
stone to enhance the quality of EOL care.46 In the Iranian
context,as a religious country with majority ofMuslims,
there isno chaplain asa memberof an interdisciplinary
PC team at any age (from children to adult patients) to spiri-
tually supportpatients and their families.In Iran,chaplains
just are accessible after a person dies for consoling the fam-
ily and holding funeraland mourning ceremony.According
to Abedi,47 a cultural view of death as preventable only by a
divine entity highlights the significance ofspirituality and
hope associated with it as effective notions central to a sup-
portsystem for Iranian patients.47
The results revealed that ‘‘continuing to provide advanced
treatment to dying child because of financial benefits to hospi-
tal’’ has the first lowest PBM score among all items, which is in
agreementwith previous studies.15,37,45
Culture and religion
are 2 important factors thatmay contribute to the perception
of society about EOL issues.48 According to Shiite experts in
Islamic Sciences,life-prolonging treatments should notaim
at keeping the patients alive only to save their lives.They go
on thatin situationsthathas no cure,people can refuse
death-prolonging procedures including cardiopulmonary resus-
citation.49However, in Iran, a do not resuscitate (DNR) order is
not legally accepted.Iranian physicians are reluctant to write
such orders because there have been no published guideli
position papers,legislation,or officialstatements concerning
EOL care, making them fearful of legal problems and crimi
prosecution.50 Mogadasian et al51 reported that Iranian nurses
have negative attitudes toward DNR in many key items of
tudes of DNR questionnaire. This study highlighted that DN
laws and religious aspects of DNR in Islam may change the
attitudes of health care providers toward DNR orders.51 Chil-
dren are valued and respected in Islam as individuals with
inherentrights,and they have the rightto be treated with
respectand withoutviolence.52 When the child is notventi-
lated, but a decision of DNR or limiting vital support measu
is made,none has objections to limittherapy.53 Therefore,
based on the principle religious rules in the context hasten
or postponing death is forbidden,terminally ill patients cause
a large financial burden for health care services.
The findings indicated thatthe item ‘‘Unitvisiting hours
is too restrictive’’ has the second lowestPBM score among
all items.This is consistentwith the finding of earlier
research.54,55The restrictive visiting hours resultin several
disadvantages for EOL care.Restricting visiting hours iso-
late familiesfrom a dying child ata time when families
need to be close to theirloved ones.37 The culturalback-
ground of mostIslamic countries stresses aboutthe family
ties.Therefore,it is more the responsibility ofthe family
and close relatives and friends to provide the care in a ded
cated way.56 In the Iranian culture, patient may never be left
alone by family or friends.This facilitates family to be with
the dying child to provide happiness and a peacefulmind.
Nonrestrictive visiting hoursallow family membersto be
included in daily interdisciplinary rounds.Consequently,
nurses or other health care professionals have time to sha
criticalinformation with family members.57
Conclusion
Nurses in this study perceived that the most important bar
in pediatric EOL care are family issues.One of the possible
causes of this result mentioned in the discussion was lack
PC education and unit.Therefore,developing EOL and PC
education based on Islamic beliefs and Iranian culture may
enhance nurses’ knowledge and skill,which enable them to
face the challenges of EOL care.Providing some educational
programs for the families aboutdeath and dying,especially
about copying strategies,could be helpful.Establishing OPD
and PC units in the community, as well as developing pallia
home care programs that focus on family members who pl
important role in children’s care, may have a positive effec
children’s EOL care.Active involvementof chaplain and a
psychologist to the treatment team in order to provide spir
and psychological support for the family may strengthen E
care. This also reduces the unnecessary cost of hospitaliza
and extra medicalexamination costs forincurable patients.
Finally,expanding NGOs and charities such as ‘‘MAHAK’’
would be very helpful to diminish family economical and p
chological burden.
Iranmanesh et al 7
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to
the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship,
and/or publication of this article.
References
1. Kyle T, Carman S, eds. Essential of Pediatric Nursing. Philadel-
phia, PA: Lippincott Williams & Wilkins; 2013:366.
2. Morgan D. Caring for dying children: assessing the needs of the
pediatric palliative care nurse.Pediatr Nurs.2009;35(2):86-90.
Web site.www.ncbi.nlm.nih.gov/pubmed/19472671.Published
March 2009. Accessed March 2014.
3. Hockenberry JM, Wilson De, eds. Wong’s Essential of Pediatric
Nursing. St Louis, Mosby Elsevier; 2009. p593.
4. Heron MP, Hoyert DL, Murphy S, Xu JQ, Kochanek KD, Tejada-
Vera B.Deaths:FinalData for 2006.NationalVital Statistics
Reports,57, 14. NationalCenterfor Health Statistics.2009.
Web site. www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf.
Published 17 April 2006. Accessed February 2014.
5. Meyer EC, Ritholz MD, Burns JP, Robert D. Improving the qual-
ity of end of life care in the pediatric intensive care unit: parents’
prioritiesand recommendations.Pediatrics.2006;117(3):649.
doi: 10.1542/peds.2005-0144.
6. Brandon D,Docherty SL,Thorpe J.Infantand child deaths in
acute care settings: Implications for palliative care. J Palliat Med.
2007;10(4):910-918.Web site. http://dx.doi.org/10.1089/jpm.
2006.0236.(PMID: 17803413 [PubMed -indexed forMED-
LINE]). Published August 2006. Accessed June2014.
7. Crozier F, Hancock LE. Pediatric Palliative Care: Beyond the End
of Life. Pediatric Nursing. 2012;38(4). Web site. www.ncbi.nlm.
nih.gov/pubmed/22970486. Accessed May 2013.
8. Beckstrand RL,Callister LC,Kirchhoff KT.providing a ‘‘good
death’’:Criticalcare nurses’ suggestions for improving end-of-
life care.Am J Crit Care.2006;15(1):38-45.Web site.www.
ncbi.nlm.nih.gov/pubmed/16391313.PublishedJanuary2006.
Accessed March 2014.
9. Devictor D,Latour JM,Tissieres P.Forgoing life-sustaining or
death-prolonging therapy in the pediatric ICU.PediatrClin
North Am. 2008;55(3):791-804. doi:10.1016/j.pcl.2008.02.008.
10. Wiener L,McConnell DG,Latella L,Ludi E.Cultural and reli-
gious considerations in pediatric palliative care.Palliat Support
Care. 2013;11(1):47-67. doi: 10.1017/S1478951511001027.
11. Flood Y. Caring for the child with palliative care needs. In: Moyra
A Baldwin,Woodhouse Jan,eds.Key Concepts in Palliative
Care. London: SAGE Publications Ltd; 2011:22.
12. World Health Organization.WHO Definition of Palliative Care.
2010.Web site.http://www.who.int/cancer/palliative/definition/
en. Accessed June 2014.
13. Davies B,Sehring SA,Partridge JC,et al.Barriers to palliative
care for children: perceptions of pediatric health care providers.
Pediatrics. 2008;121(2):282. doi: 10.1542/peds.2006-3153.
14. Beckstrand RL,Rawl NL, Calliste L,Mandleco BL.Pediatric
Nurses’Perceptions ofObstacles and Supportive Behaviors in
End-of-Life. Am J Crit Care. 2010;19(6):543-552. doi: 10.4037
ajcc200949.
15. Gehan EL Nabawy Ahmed Moawad. Nurses’ perception of obs
cles and supportive behaviors in providing end of life care to
tically ill pediatric patients. J Biol Agriculture Healthcare. 2013
3(2):96-105.Web site.www.iiste.org/Journals/index.php/JBAH/
article/view/4302. Accessed May, 2014.
16. Iglesias MEL,PascualC, Ricardo Becerro De Bengoa Vallejo.
Obstacles and helpful behaviors in providing end-of-life care
dying patients in intensive care units.Dimens CritCare Nurs.
2013;32(2):99-106. doi: 10.1097/DCC.0b013e3181f0c43.
17. Edalati A, Hooshmand Abarkouhye N. Death in Iranian culture
Case Study ofAbarkouh,Yazd). IRSSH. 2012;2(2):200-202.
Website.Irssh.com/yahoo_site_admin/assets/docs/22_IRSSH-
199-V2N2.9010345.pdf. Accessed November 8, 2011.
18. Cultural Approaches to Pediatric Palliative Care in Central Ma
sachusetts.Web site.http://libraryguides.umassmed.edu/diver-
sity_guide. Accessed June, 2014.
19. EslamiNodooshan MA.Love,life and death in Rumi’s view.
Hasti. 2007;7(25):83-95.
20. Sanati M. Black aesthetics: fear of death and Iranian art. Keta
Mah e Honar; 2005; 7(75, 76):27-48.
21. Web site. kirpalsingh.org/Booklets/DeathandDyingrevised.pdf
Accessed June 2014.
22. Valentine A, Jason John N, Rice L. The Business Year 2013: Ira
London,U.K.: The BusinessYear; 2013:156.ISBN 978-1-
908180-11-7.
23. Mehrdad R. Health System in Iran. JMAJ. 2009;52(1):69-73. W
site. www.med.or.jp/english/pdf/2009_01/069_073.pdf.Pub-
lished February 2009. Accessed May 2014.
24. NojomiM, NaserbakhatM, Ramezany M,Anbary K.Under-5
year mortality: result of in-hospital study, Tehran, Iran. Acta M
Iran. 2009;47(4). Web site. acta.tums.ac.ir/index.php/acta/art
viewFile/3636/3320.
25. Bagheri Lankarani K, Alavian SM, Peymani P. Health in the Isl
mic Republic of Iran,challenges and progresses.MJIRI. 2013;
27(1):42-49. Web site. http://mjiri.tums.ac.ir.
26. World Health Organization country health profile of Iran (Isla-
mic Republic of).Web site.www.who.int/country/irn/en2012.
Accessed June 2014.
27. ‘‘IRAN: Healthcare and Pharmaceuticals Forecast’’.Economist
Intelligence Unit. August 2008. Web site. news.alacrastore.co
eiu . . . /Iran-Healthcare-and-pharmaceuticals-forecast.Accessed
February 2014.
28. Web site. Payvand.com. 2009. Accessed February 2012.
29. Asaei E.UNICEF Iran’s specialist for early childhood develop-
ment. Web site. www.unicef.org/iran/media_4427.html. Acces
May 2014.
30. Web site. Press TV. 2011. Accessed February 2012.
31. Web site. www.who.int/country/irn/en.2012.Accessed June 20
32. Web site. www.penous.com/News/print/323/.AccessedJune
2014.
33. Webster R, Lacey J, Quine S. Palliative care: a public health p
ority in developing countries. J Public Health Policy. 2007;28(
28-39.Web site.www.ncbi.nlm.nih.gov/pubmed/17363933.doi:
10.1057/palgrave.jphp3200097.
8 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
The authors declared no potential conflicts of interest with respect to
the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship,
and/or publication of this article.
References
1. Kyle T, Carman S, eds. Essential of Pediatric Nursing. Philadel-
phia, PA: Lippincott Williams & Wilkins; 2013:366.
2. Morgan D. Caring for dying children: assessing the needs of the
pediatric palliative care nurse.Pediatr Nurs.2009;35(2):86-90.
Web site.www.ncbi.nlm.nih.gov/pubmed/19472671.Published
March 2009. Accessed March 2014.
3. Hockenberry JM, Wilson De, eds. Wong’s Essential of Pediatric
Nursing. St Louis, Mosby Elsevier; 2009. p593.
4. Heron MP, Hoyert DL, Murphy S, Xu JQ, Kochanek KD, Tejada-
Vera B.Deaths:FinalData for 2006.NationalVital Statistics
Reports,57, 14. NationalCenterfor Health Statistics.2009.
Web site. www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf.
Published 17 April 2006. Accessed February 2014.
5. Meyer EC, Ritholz MD, Burns JP, Robert D. Improving the qual-
ity of end of life care in the pediatric intensive care unit: parents’
prioritiesand recommendations.Pediatrics.2006;117(3):649.
doi: 10.1542/peds.2005-0144.
6. Brandon D,Docherty SL,Thorpe J.Infantand child deaths in
acute care settings: Implications for palliative care. J Palliat Med.
2007;10(4):910-918.Web site. http://dx.doi.org/10.1089/jpm.
2006.0236.(PMID: 17803413 [PubMed -indexed forMED-
LINE]). Published August 2006. Accessed June2014.
7. Crozier F, Hancock LE. Pediatric Palliative Care: Beyond the End
of Life. Pediatric Nursing. 2012;38(4). Web site. www.ncbi.nlm.
nih.gov/pubmed/22970486. Accessed May 2013.
8. Beckstrand RL,Callister LC,Kirchhoff KT.providing a ‘‘good
death’’:Criticalcare nurses’ suggestions for improving end-of-
life care.Am J Crit Care.2006;15(1):38-45.Web site.www.
ncbi.nlm.nih.gov/pubmed/16391313.PublishedJanuary2006.
Accessed March 2014.
9. Devictor D,Latour JM,Tissieres P.Forgoing life-sustaining or
death-prolonging therapy in the pediatric ICU.PediatrClin
North Am. 2008;55(3):791-804. doi:10.1016/j.pcl.2008.02.008.
10. Wiener L,McConnell DG,Latella L,Ludi E.Cultural and reli-
gious considerations in pediatric palliative care.Palliat Support
Care. 2013;11(1):47-67. doi: 10.1017/S1478951511001027.
11. Flood Y. Caring for the child with palliative care needs. In: Moyra
A Baldwin,Woodhouse Jan,eds.Key Concepts in Palliative
Care. London: SAGE Publications Ltd; 2011:22.
12. World Health Organization.WHO Definition of Palliative Care.
2010.Web site.http://www.who.int/cancer/palliative/definition/
en. Accessed June 2014.
13. Davies B,Sehring SA,Partridge JC,et al.Barriers to palliative
care for children: perceptions of pediatric health care providers.
Pediatrics. 2008;121(2):282. doi: 10.1542/peds.2006-3153.
14. Beckstrand RL,Rawl NL, Calliste L,Mandleco BL.Pediatric
Nurses’Perceptions ofObstacles and Supportive Behaviors in
End-of-Life. Am J Crit Care. 2010;19(6):543-552. doi: 10.4037
ajcc200949.
15. Gehan EL Nabawy Ahmed Moawad. Nurses’ perception of obs
cles and supportive behaviors in providing end of life care to
tically ill pediatric patients. J Biol Agriculture Healthcare. 2013
3(2):96-105.Web site.www.iiste.org/Journals/index.php/JBAH/
article/view/4302. Accessed May, 2014.
16. Iglesias MEL,PascualC, Ricardo Becerro De Bengoa Vallejo.
Obstacles and helpful behaviors in providing end-of-life care
dying patients in intensive care units.Dimens CritCare Nurs.
2013;32(2):99-106. doi: 10.1097/DCC.0b013e3181f0c43.
17. Edalati A, Hooshmand Abarkouhye N. Death in Iranian culture
Case Study ofAbarkouh,Yazd). IRSSH. 2012;2(2):200-202.
Website.Irssh.com/yahoo_site_admin/assets/docs/22_IRSSH-
199-V2N2.9010345.pdf. Accessed November 8, 2011.
18. Cultural Approaches to Pediatric Palliative Care in Central Ma
sachusetts.Web site.http://libraryguides.umassmed.edu/diver-
sity_guide. Accessed June, 2014.
19. EslamiNodooshan MA.Love,life and death in Rumi’s view.
Hasti. 2007;7(25):83-95.
20. Sanati M. Black aesthetics: fear of death and Iranian art. Keta
Mah e Honar; 2005; 7(75, 76):27-48.
21. Web site. kirpalsingh.org/Booklets/DeathandDyingrevised.pdf
Accessed June 2014.
22. Valentine A, Jason John N, Rice L. The Business Year 2013: Ira
London,U.K.: The BusinessYear; 2013:156.ISBN 978-1-
908180-11-7.
23. Mehrdad R. Health System in Iran. JMAJ. 2009;52(1):69-73. W
site. www.med.or.jp/english/pdf/2009_01/069_073.pdf.Pub-
lished February 2009. Accessed May 2014.
24. NojomiM, NaserbakhatM, Ramezany M,Anbary K.Under-5
year mortality: result of in-hospital study, Tehran, Iran. Acta M
Iran. 2009;47(4). Web site. acta.tums.ac.ir/index.php/acta/art
viewFile/3636/3320.
25. Bagheri Lankarani K, Alavian SM, Peymani P. Health in the Isl
mic Republic of Iran,challenges and progresses.MJIRI. 2013;
27(1):42-49. Web site. http://mjiri.tums.ac.ir.
26. World Health Organization country health profile of Iran (Isla-
mic Republic of).Web site.www.who.int/country/irn/en2012.
Accessed June 2014.
27. ‘‘IRAN: Healthcare and Pharmaceuticals Forecast’’.Economist
Intelligence Unit. August 2008. Web site. news.alacrastore.co
eiu . . . /Iran-Healthcare-and-pharmaceuticals-forecast.Accessed
February 2014.
28. Web site. Payvand.com. 2009. Accessed February 2012.
29. Asaei E.UNICEF Iran’s specialist for early childhood develop-
ment. Web site. www.unicef.org/iran/media_4427.html. Acces
May 2014.
30. Web site. Press TV. 2011. Accessed February 2012.
31. Web site. www.who.int/country/irn/en.2012.Accessed June 20
32. Web site. www.penous.com/News/print/323/.AccessedJune
2014.
33. Webster R, Lacey J, Quine S. Palliative care: a public health p
ority in developing countries. J Public Health Policy. 2007;28(
28-39.Web site.www.ncbi.nlm.nih.gov/pubmed/17363933.doi:
10.1057/palgrave.jphp3200097.
8 American Journalof Hospice & Palliative Medicine®
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
34. Asadi-Lari, Madjd Z, Akbari ME. The need for palliative care ser-
vices in Iran; an introductory Iranian Journal of Cancer Preven-
tion.2008;1(1):1-5.Web site.journals.sbmu.ac.ir/index.php/cp/
article/view/3109.Published January2008.Accessed January
2013.
35. Iranmanesh S, Razban F, Tirgary B, Ghazanfari Z. Nurses’ knowl-
edge about palliative care in Southeast Iran. Palliate Support Care.
2014;12(3):203-210. doi: 10.1017/S1478951512001058.
36. Kirchhoff KT, Beckstrand RL. Critical care nurses’ perceptions of
obstacles and helpfulbehaviors in providing end-of-life care to
dying patients.Am J Crit Care.2000;9(2):96-105.Web site.
www.ncbi.nlm.nih.gov/pubmed/10705423. Accessed June 2013.
37. Beckstrand RL,KirchhoffKT. Providing end-of-life care to
patients: Critical care nurses’ perceived obstacles and supportive
behaviors.Am J Crit Care.2005;14(5):395-403.Web site.ajcc.
aacnjournals.org/content/14/5/395.full.(PMID: 16120891
[PubMed - indexed for MEDLINE]). Published September 2005.
Accessed February 2014.
38. Nelson JE. Identifying and overcoming the barriersto high-
quality palliative care in the intensive care unit.Crit Care Med.
2006;34(11 suppl):S324-S331.doi: 10.1097/01.CCM.0000237
249.39179.B1.
39. Rowse V.Palliative care for children: a public health initiative.
Pediatr Nurs.2006;18(4):41-45.Web site.www.ncbi.nlm.nih.
gov/pubmed/16719043. Accessed May 2006.
40. Silbermann M, Khleif A, Tuncer M, et al. Can we overcome the
effect of conflicts in rendering palliative care? Curr Top Oncol.
2011;13(4):302-307. doi: 10.1007/s11912-011-0174-z.
41. Bennett H. A guide to end of life care: care of children and young
people before death,at the time of death and after death.2012.
P14.Web site.www.togetherforshortlives.org.uk/ . . . A_Guide_
to_End_of_Life_Care_5 . . . Accessed July 2014.
42. Ott BB, Al-Khadhiri J, Al-Junaibi S. Preventing ethical dilemmas:
the Muslim people. Pediatr Nurs. 2003;29(3):227-330. Web site.
www.medscape.com > PediatricNursing.(PMID: 12837004
[PubMed - indexed for MEDLINE]).Published May/June 2003.
Accessed May 2013.
43. Larson DG, Tobin DR. End-of-life conversations: evolving prac-
tice and theory. J Am Med Assoc. 2000;284(12):1573-1578. Web
site.jama.jamanetwork.com/article.aspx?articleid¼193119.doi:
10.1001/jama.284.12.1573.
44. Graham RJ,Robinson WM.Integrating palliativecare into
chronic care for children with severe neurodevelopmental disabil-
ities. J Dev Behav Pediatr. 2005;26(5):361-365. Web site. www.
ncbi.nlm.nih.gov/pubmed/16222176.doi: 10.1097/00004703-
200510000-00004.
45. Crump SK, Schaffer MA, Schulte E. Critical care nurses’ percep-
tions of obstacles, supports, and knowledge needed in providing
quality end-of-life care.DimensCrit Care Nurs.2010;29(6):
297-306. doi: 10.1097/DCC.0b013e3181f0c43c.
46. Sourkes B, Frankel L, Brown M, et al. Food, toys, and love: pe
tric palliative care.Curr Probl Pediatr Adolesc Health Care.
2005;35(9):350-386.Web site.www.ncbi.nlm.nih.gov/pubmed/
16301200. doi:10.1016/j.cppeds.2005.09.002.
47. Abedi M.Palliative care within the Iranian context: re-defining
palliative care,deploying spirituality as a supportmeasure and
need for cultural sensitivity. 2012. Web site. www.interdiscipl
ary.net/wpcontent/ . . . /2012/02/abedisppaper.Pdf. Accessed
2014.
48. Steinberg SM. Cultural and religious aspects of palliative care
J Crit Illn Inj Sci.2011;1(2):154-156.doi:10.4103/2229-5151.
84804.
49. Mobasher M,Aramesh K, Zahedi F, Nakhaee N,Tahmasebi M,
Larijani B. End-of-Life care ethical decision making: Shiite sch
lar views. J Med Ethics Hist Med. 2014;7:2. Web site. knrc.ac.i
upload . . . /DR.Nakhaei_CV_0_15575.Published14 January,
2014. Accessed June 2014.
50. Atashzadeh Shorideh F, Ashktorab T, Yaghmaei F. Iranian inte
sive care unitNurses’moraldistress:a contentanalysis.Nurs
Ethics. 2012;19(4):464-478. doi: 10.1177/096973301243798
51. Mogadasian S, Abdollahzadeh F, Rahmani A, et al. The attitud
of Iranian nurses about do not resuscitate orders. Indian J Pal
Care. 2014;20(1):21-25. doi: 10.4103/0973-1075.125550.
52. Hedayat KM, Pirzadeh R.Issues in Islamic biomedical ethics: a
primerfor the pediatrician.Pediatrics.2001;108(4):965.Web
site.pediatrics.aappublications.org/content/108/4/965.short.doi:
10.1542/peds.108.4.965
53. Da Costa D E, Ghazal H, Al Khusaiby S. Do not resuscitate ord
and ethical decisions in a neonatal intensive care unit in a Mu
community.Arch Dis Child Fetal NeonatalEd. 2002;86(2):
F115-F119. doi: 10.1136/fn.86.2.F115.
54. Beckstrand RL,Smith MD,Heaston S,Bond AE.Emergency
nurses’ perceptions of size, frequency, and magnitude of obs
and supportive behaviors in end-of-life care. J Emerg Nurs. 20
34(4):290-300. Web site. http://dx.doi.org/10.1016/j.jen.2007
004. doi: 10.1016/j.jen.2007.09.004.
55. Gross AG. End-of-life care obstacles and facilitators in the crit
care units of a community hospital. J Hospice Palliat Nurs. 200
8(2):92-102. Web site. journals.lww.com > Home > March/Ap
2006. doi: 10.1097/00129191-200603000-00013
56. Asadi-Lari1 M, Madjd Z, Goushegir SA. Gaps in the provision
of spiritual care for terminally ill patients in Islamic societies -
a systematic review. Adv Pall Med. 2008;7(2):73-80. Web site
czasopisma.viamedica.pl/apm/article/download/29426/24182
Accessed May 2014.
57. Maxwell KE,StuenkelD, Saylor C.Needs of family members
of critically ill patients: A comparison of nurse and family per
ceptions.Heart Lung.2007;36(5):367-376.Web site.www.
ncbi.nlm.nih.gov/pubmed/17845883.doi:10.1016/j.hrtlng.2007.
02.005
Iranmanesh et al 9
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
vices in Iran; an introductory Iranian Journal of Cancer Preven-
tion.2008;1(1):1-5.Web site.journals.sbmu.ac.ir/index.php/cp/
article/view/3109.Published January2008.Accessed January
2013.
35. Iranmanesh S, Razban F, Tirgary B, Ghazanfari Z. Nurses’ knowl-
edge about palliative care in Southeast Iran. Palliate Support Care.
2014;12(3):203-210. doi: 10.1017/S1478951512001058.
36. Kirchhoff KT, Beckstrand RL. Critical care nurses’ perceptions of
obstacles and helpfulbehaviors in providing end-of-life care to
dying patients.Am J Crit Care.2000;9(2):96-105.Web site.
www.ncbi.nlm.nih.gov/pubmed/10705423. Accessed June 2013.
37. Beckstrand RL,KirchhoffKT. Providing end-of-life care to
patients: Critical care nurses’ perceived obstacles and supportive
behaviors.Am J Crit Care.2005;14(5):395-403.Web site.ajcc.
aacnjournals.org/content/14/5/395.full.(PMID: 16120891
[PubMed - indexed for MEDLINE]). Published September 2005.
Accessed February 2014.
38. Nelson JE. Identifying and overcoming the barriersto high-
quality palliative care in the intensive care unit.Crit Care Med.
2006;34(11 suppl):S324-S331.doi: 10.1097/01.CCM.0000237
249.39179.B1.
39. Rowse V.Palliative care for children: a public health initiative.
Pediatr Nurs.2006;18(4):41-45.Web site.www.ncbi.nlm.nih.
gov/pubmed/16719043. Accessed May 2006.
40. Silbermann M, Khleif A, Tuncer M, et al. Can we overcome the
effect of conflicts in rendering palliative care? Curr Top Oncol.
2011;13(4):302-307. doi: 10.1007/s11912-011-0174-z.
41. Bennett H. A guide to end of life care: care of children and young
people before death,at the time of death and after death.2012.
P14.Web site.www.togetherforshortlives.org.uk/ . . . A_Guide_
to_End_of_Life_Care_5 . . . Accessed July 2014.
42. Ott BB, Al-Khadhiri J, Al-Junaibi S. Preventing ethical dilemmas:
the Muslim people. Pediatr Nurs. 2003;29(3):227-330. Web site.
www.medscape.com > PediatricNursing.(PMID: 12837004
[PubMed - indexed for MEDLINE]).Published May/June 2003.
Accessed May 2013.
43. Larson DG, Tobin DR. End-of-life conversations: evolving prac-
tice and theory. J Am Med Assoc. 2000;284(12):1573-1578. Web
site.jama.jamanetwork.com/article.aspx?articleid¼193119.doi:
10.1001/jama.284.12.1573.
44. Graham RJ,Robinson WM.Integrating palliativecare into
chronic care for children with severe neurodevelopmental disabil-
ities. J Dev Behav Pediatr. 2005;26(5):361-365. Web site. www.
ncbi.nlm.nih.gov/pubmed/16222176.doi: 10.1097/00004703-
200510000-00004.
45. Crump SK, Schaffer MA, Schulte E. Critical care nurses’ percep-
tions of obstacles, supports, and knowledge needed in providing
quality end-of-life care.DimensCrit Care Nurs.2010;29(6):
297-306. doi: 10.1097/DCC.0b013e3181f0c43c.
46. Sourkes B, Frankel L, Brown M, et al. Food, toys, and love: pe
tric palliative care.Curr Probl Pediatr Adolesc Health Care.
2005;35(9):350-386.Web site.www.ncbi.nlm.nih.gov/pubmed/
16301200. doi:10.1016/j.cppeds.2005.09.002.
47. Abedi M.Palliative care within the Iranian context: re-defining
palliative care,deploying spirituality as a supportmeasure and
need for cultural sensitivity. 2012. Web site. www.interdiscipl
ary.net/wpcontent/ . . . /2012/02/abedisppaper.Pdf. Accessed
2014.
48. Steinberg SM. Cultural and religious aspects of palliative care
J Crit Illn Inj Sci.2011;1(2):154-156.doi:10.4103/2229-5151.
84804.
49. Mobasher M,Aramesh K, Zahedi F, Nakhaee N,Tahmasebi M,
Larijani B. End-of-Life care ethical decision making: Shiite sch
lar views. J Med Ethics Hist Med. 2014;7:2. Web site. knrc.ac.i
upload . . . /DR.Nakhaei_CV_0_15575.Published14 January,
2014. Accessed June 2014.
50. Atashzadeh Shorideh F, Ashktorab T, Yaghmaei F. Iranian inte
sive care unitNurses’moraldistress:a contentanalysis.Nurs
Ethics. 2012;19(4):464-478. doi: 10.1177/096973301243798
51. Mogadasian S, Abdollahzadeh F, Rahmani A, et al. The attitud
of Iranian nurses about do not resuscitate orders. Indian J Pal
Care. 2014;20(1):21-25. doi: 10.4103/0973-1075.125550.
52. Hedayat KM, Pirzadeh R.Issues in Islamic biomedical ethics: a
primerfor the pediatrician.Pediatrics.2001;108(4):965.Web
site.pediatrics.aappublications.org/content/108/4/965.short.doi:
10.1542/peds.108.4.965
53. Da Costa D E, Ghazal H, Al Khusaiby S. Do not resuscitate ord
and ethical decisions in a neonatal intensive care unit in a Mu
community.Arch Dis Child Fetal NeonatalEd. 2002;86(2):
F115-F119. doi: 10.1136/fn.86.2.F115.
54. Beckstrand RL,Smith MD,Heaston S,Bond AE.Emergency
nurses’ perceptions of size, frequency, and magnitude of obs
and supportive behaviors in end-of-life care. J Emerg Nurs. 20
34(4):290-300. Web site. http://dx.doi.org/10.1016/j.jen.2007
004. doi: 10.1016/j.jen.2007.09.004.
55. Gross AG. End-of-life care obstacles and facilitators in the crit
care units of a community hospital. J Hospice Palliat Nurs. 200
8(2):92-102. Web site. journals.lww.com > Home > March/Ap
2006. doi: 10.1097/00129191-200603000-00013
56. Asadi-Lari1 M, Madjd Z, Goushegir SA. Gaps in the provision
of spiritual care for terminally ill patients in Islamic societies -
a systematic review. Adv Pall Med. 2008;7(2):73-80. Web site
czasopisma.viamedica.pl/apm/article/download/29426/24182
Accessed May 2014.
57. Maxwell KE,StuenkelD, Saylor C.Needs of family members
of critically ill patients: A comparison of nurse and family per
ceptions.Heart Lung.2007;36(5):367-376.Web site.www.
ncbi.nlm.nih.gov/pubmed/17845883.doi:10.1016/j.hrtlng.2007.
02.005
Iranmanesh et al 9
at UNIV OF FLORIDA on November 14, 2015ajh.sagepub.comDownloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


