Nursing 1 Course Assignment: Ethics, Legislation, and Nursing Practice
VerifiedAdded on 2023/06/05
|18
|4905
|78
Homework Assignment
AI Summary
This nursing assignment covers a wide range of topics related to nursing practice in Australia. It begins by outlining relevant legislation, including the Health Ombudsman Act and the Health (Drugs and Poisons) Regulation. The assignment then explores the importance of the NMBA code of ethics and professional conduct, emphasizing accountability and confidentiality. Key features of enrolled nurses' roles are discussed, including delegation, accountability, and supervision. Factors to consider when responding to patient complaints, along with communication strategies and organizational guidelines, are also presented. The assignment further delves into consent to treatment, detailing different types of consent and relevant legal considerations. It also addresses restraint practices, relevant laws, and ethical concepts. The document includes a template defining statutory law, common law, relevant legislation, and ethical principles. Finally, the assignment examines legal requirements for documentation, emphasizing the importance of accurate and factual record-keeping.

Nursing 1
NURSING
by [NAME]
Course
Professor’s Name
Institution
Location of Institution
Date
NURSING
by [NAME]
Course
Professor’s Name
Institution
Location of Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nursing 2
Question 2: Legislations
1. Health Ombudsman Act (2013)
This act was enacted to provide for a system of handling complaints related to health, conduct of
health practitioners, and services offered by the various healthcare organizations.
2. Health (Drugs and Poisons) Regulation 1996
This act outlines the standards required to dispense certain drugs or sell particular poisons.
Question 3: Code of Ethics and Code of Conducts
I am guided by the NMBA code of ethics and code of professional conduct to deliver proper and
quality nursing care to patients. One of the codes of conducts that I have used is the one that
states that nurses practice in a safe and competent manner. I understand that as a nurse I am
accountable for providing a safe and competent nursing care. I ensure that the competence levels
are maintained high by participating in professional development to improve my knowledge and
skills. This code enables me to understand that taking part in any care plan that is out of my
scope may compromise the provision of quality and safe care.
Another code of conduct that I have applied in practice states that nurses treat personal
information obtained in a professional capacity as private and confidential. I understand that I am
legally obliged to protect the privacy of the patients I am caring for. I must additionally seek
consent from the patient or their representative before revealing any information that may have
been confidentially acquired in the line of duty.
Question 4: Key features which rely to enrolled nurses
Question 2: Legislations
1. Health Ombudsman Act (2013)
This act was enacted to provide for a system of handling complaints related to health, conduct of
health practitioners, and services offered by the various healthcare organizations.
2. Health (Drugs and Poisons) Regulation 1996
This act outlines the standards required to dispense certain drugs or sell particular poisons.
Question 3: Code of Ethics and Code of Conducts
I am guided by the NMBA code of ethics and code of professional conduct to deliver proper and
quality nursing care to patients. One of the codes of conducts that I have used is the one that
states that nurses practice in a safe and competent manner. I understand that as a nurse I am
accountable for providing a safe and competent nursing care. I ensure that the competence levels
are maintained high by participating in professional development to improve my knowledge and
skills. This code enables me to understand that taking part in any care plan that is out of my
scope may compromise the provision of quality and safe care.
Another code of conduct that I have applied in practice states that nurses treat personal
information obtained in a professional capacity as private and confidential. I understand that I am
legally obliged to protect the privacy of the patients I am caring for. I must additionally seek
consent from the patient or their representative before revealing any information that may have
been confidentially acquired in the line of duty.
Question 4: Key features which rely to enrolled nurses
Nursing 3
It is important to note that these standards provide clarity regarding role relationships,
delegation, and supervision. The key features of the standards are as highlighted below.
1. The enrolled nurse is accountable in providing delegated care.
A registered nurse I must ensure that any activity delegated to an EN is appropriately delegated
since they have a duty of care with regard to the patients. The enrolled nurse must ensure that the
task delegated to them by the registered nurse id within their scope of practice to avoid harming
the patient. Delegation is only appropriate when the RN only delegates tasks that are within the
scope of the EN. The RN must then ensure that the EN is supervised and adequately supported
for quality care outcomes.
2. The enrolled nurse keeps responsibility for their actions
The enrolled nurse must at all times accept responsibility for their actions and decisions that they
make within their scope of practice. They are also responsible for making sure that they have the
necessary skills and knowledge required to conduct any nursing care before they can claim
responsibility.
3. The enrolled nurse should work under the direct or indirect supervision of a registered
nurse
The enrolled nurse must never practice in professional isolation and the registered nurse should
be responsible for providing guidance and feedback regarding the practice of the enrolled nurse.
The supervision may include monthly meetings, review of the contents of work and nursing
activities, discussion of practice issues, and discussions involving professional development.
This close operation between the enrolled nurse and the registered nurse is helpful in ensuring
desirable care outcomes.
It is important to note that these standards provide clarity regarding role relationships,
delegation, and supervision. The key features of the standards are as highlighted below.
1. The enrolled nurse is accountable in providing delegated care.
A registered nurse I must ensure that any activity delegated to an EN is appropriately delegated
since they have a duty of care with regard to the patients. The enrolled nurse must ensure that the
task delegated to them by the registered nurse id within their scope of practice to avoid harming
the patient. Delegation is only appropriate when the RN only delegates tasks that are within the
scope of the EN. The RN must then ensure that the EN is supervised and adequately supported
for quality care outcomes.
2. The enrolled nurse keeps responsibility for their actions
The enrolled nurse must at all times accept responsibility for their actions and decisions that they
make within their scope of practice. They are also responsible for making sure that they have the
necessary skills and knowledge required to conduct any nursing care before they can claim
responsibility.
3. The enrolled nurse should work under the direct or indirect supervision of a registered
nurse
The enrolled nurse must never practice in professional isolation and the registered nurse should
be responsible for providing guidance and feedback regarding the practice of the enrolled nurse.
The supervision may include monthly meetings, review of the contents of work and nursing
activities, discussion of practice issues, and discussions involving professional development.
This close operation between the enrolled nurse and the registered nurse is helpful in ensuring
desirable care outcomes.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Nursing 4
Question 5: Factors to take into consideration when responding to individuals
There may be several reasons that may lead to complaints arising from patients and/or their
families. However, once presented with a complaint, a nurse is required to consider some factors.
These may include gathering facts to collect all the information regarding the rise of the
complaint (Holmes-Bonney, 2010). The nurse should also consider factors that may have led to
the complaint. These may include quality of service, lateness, long queues, and negligence
among others. Once identified, the nurse should assure the patient that changes will be made to
avoid a repeat of a similar incident.
Some of the communication strategies that I might utilize to address such complaints may
include directly talking to the patient preferably face-to-face concerning the complaint. I would
additionally employ active listening skills to ensure effective communication.
An organization must have guidelines on how to handle complaints. The following approach
may be useful in handling complaints from patients. Once a complaint has been received, the
organization should acknowledge the complaint. Suggests a meeting with the complainant
whenever possible and discuss his concerns with him (Holmes-Bonney, 2010). It is also
imperative to keep all the parties involved in the complaint informed.
Question 11: Consent to Treatment
Consent to treatment may be defined as the standard that an individual must give permission
before receiving any form of medical examinations, tests or treatment (Kim, 2009). Consent is
only valid if it is voluntary and informed and the person giving their consent must have the
capacity to make an informed decision. In some situations, an individual may not have the
capacity to make a decision and they also do not have a lasting power of attorney. In such
Question 5: Factors to take into consideration when responding to individuals
There may be several reasons that may lead to complaints arising from patients and/or their
families. However, once presented with a complaint, a nurse is required to consider some factors.
These may include gathering facts to collect all the information regarding the rise of the
complaint (Holmes-Bonney, 2010). The nurse should also consider factors that may have led to
the complaint. These may include quality of service, lateness, long queues, and negligence
among others. Once identified, the nurse should assure the patient that changes will be made to
avoid a repeat of a similar incident.
Some of the communication strategies that I might utilize to address such complaints may
include directly talking to the patient preferably face-to-face concerning the complaint. I would
additionally employ active listening skills to ensure effective communication.
An organization must have guidelines on how to handle complaints. The following approach
may be useful in handling complaints from patients. Once a complaint has been received, the
organization should acknowledge the complaint. Suggests a meeting with the complainant
whenever possible and discuss his concerns with him (Holmes-Bonney, 2010). It is also
imperative to keep all the parties involved in the complaint informed.
Question 11: Consent to Treatment
Consent to treatment may be defined as the standard that an individual must give permission
before receiving any form of medical examinations, tests or treatment (Kim, 2009). Consent is
only valid if it is voluntary and informed and the person giving their consent must have the
capacity to make an informed decision. In some situations, an individual may not have the
capacity to make a decision and they also do not have a lasting power of attorney. In such
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nursing 5
situations, the responsible healthcare professional may go ahead with the treatment if he/she
believes that it is best that way (Kim, 2009). There are three types of consent. The first type is
implied consent. This type of consent is not explicitly given by the patient. It can, however, be
inferred from their actions like when a patient extends there arm out to the doctor to draw blood
(Farrell et al., 2014). The second one is verbal consent where the patient clearly mentions their
mentions their agreement to a treatment procedure. This consent is normally obtained if the
intended procedure is invasive. Finally, we have written consent where the individual puts down
in writing their agreement to a treatment procedure (Farrell et al., 2014). If the procedure has
potentially irreversible side effects then written consent must be obtained.
Question 12: Restraint
i) Leadership for organizational change
ii) Use of data to inform practice
iii) Workforce development
iv) Use of seclusion and restraint prevention tools
v) Consumer and family/carer involvement and roles in inpatient care
vi) Rigorous debriefing
Question 13: Template
ITEM/TERM/QUESTION MEANING OR EXPLANATION
What is statutory law? This is a written law usually enacted by the legislative body and
interpreted by the judiciary. The courts cannot read between the
lines when it comes to statutory laws, they are rather bound by its
express terms.
What is common law? This law is derived from court’s judicial decisions and other
similar tribunals. A common law is massively based on
situations, the responsible healthcare professional may go ahead with the treatment if he/she
believes that it is best that way (Kim, 2009). There are three types of consent. The first type is
implied consent. This type of consent is not explicitly given by the patient. It can, however, be
inferred from their actions like when a patient extends there arm out to the doctor to draw blood
(Farrell et al., 2014). The second one is verbal consent where the patient clearly mentions their
mentions their agreement to a treatment procedure. This consent is normally obtained if the
intended procedure is invasive. Finally, we have written consent where the individual puts down
in writing their agreement to a treatment procedure (Farrell et al., 2014). If the procedure has
potentially irreversible side effects then written consent must be obtained.
Question 12: Restraint
i) Leadership for organizational change
ii) Use of data to inform practice
iii) Workforce development
iv) Use of seclusion and restraint prevention tools
v) Consumer and family/carer involvement and roles in inpatient care
vi) Rigorous debriefing
Question 13: Template
ITEM/TERM/QUESTION MEANING OR EXPLANATION
What is statutory law? This is a written law usually enacted by the legislative body and
interpreted by the judiciary. The courts cannot read between the
lines when it comes to statutory laws, they are rather bound by its
express terms.
What is common law? This law is derived from court’s judicial decisions and other
similar tribunals. A common law is massively based on
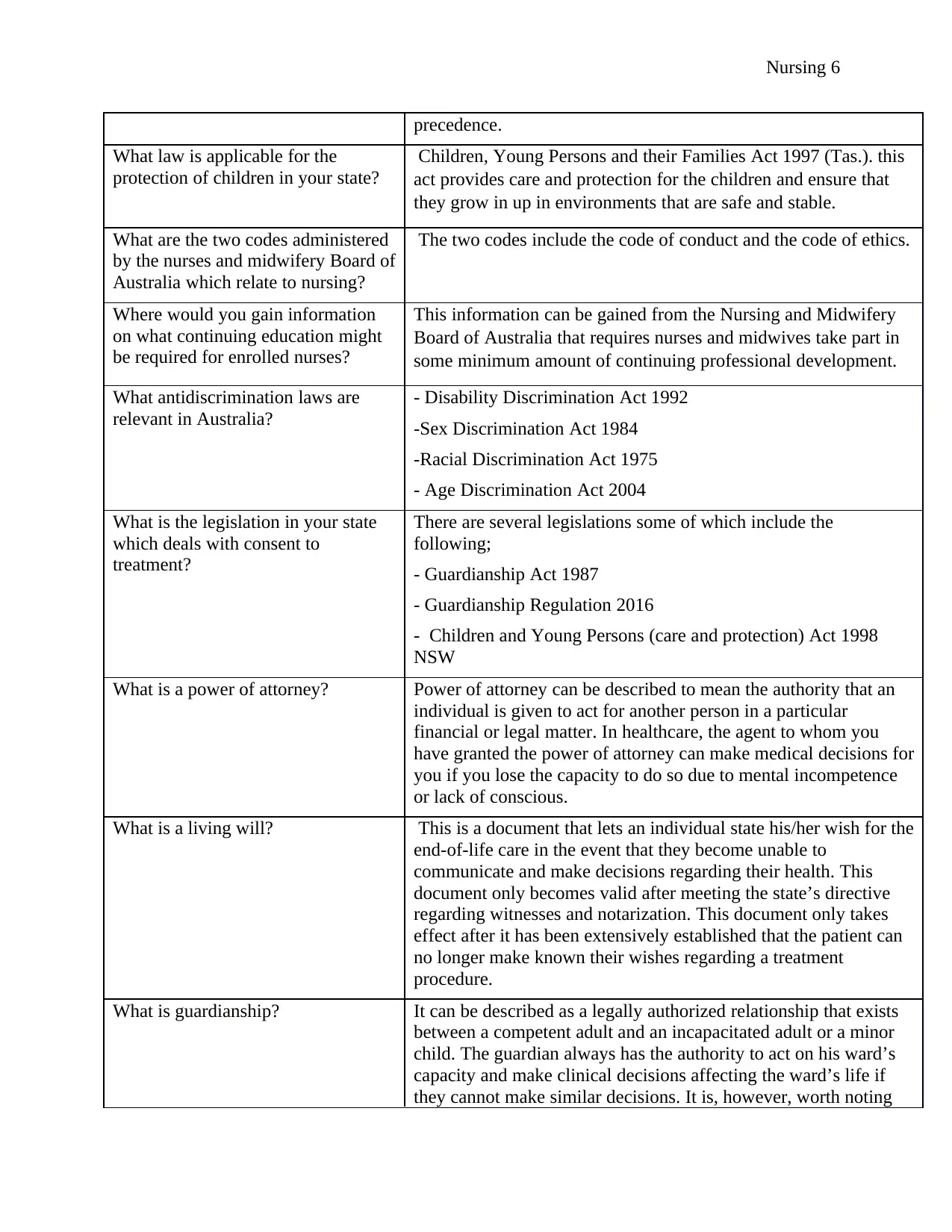
Nursing 6
precedence.
What law is applicable for the
protection of children in your state?
Children, Young Persons and their Families Act 1997 (Tas.). this
act provides care and protection for the children and ensure that
they grow in up in environments that are safe and stable.
What are the two codes administered
by the nurses and midwifery Board of
Australia which relate to nursing?
The two codes include the code of conduct and the code of ethics.
Where would you gain information
on what continuing education might
be required for enrolled nurses?
This information can be gained from the Nursing and Midwifery
Board of Australia that requires nurses and midwives take part in
some minimum amount of continuing professional development.
What antidiscrimination laws are
relevant in Australia?
- Disability Discrimination Act 1992
-Sex Discrimination Act 1984
-Racial Discrimination Act 1975
- Age Discrimination Act 2004
What is the legislation in your state
which deals with consent to
treatment?
There are several legislations some of which include the
following;
- Guardianship Act 1987
- Guardianship Regulation 2016
- Children and Young Persons (care and protection) Act 1998
NSW
What is a power of attorney? Power of attorney can be described to mean the authority that an
individual is given to act for another person in a particular
financial or legal matter. In healthcare, the agent to whom you
have granted the power of attorney can make medical decisions for
you if you lose the capacity to do so due to mental incompetence
or lack of conscious.
What is a living will? This is a document that lets an individual state his/her wish for the
end-of-life care in the event that they become unable to
communicate and make decisions regarding their health. This
document only becomes valid after meeting the state’s directive
regarding witnesses and notarization. This document only takes
effect after it has been extensively established that the patient can
no longer make known their wishes regarding a treatment
procedure.
What is guardianship? It can be described as a legally authorized relationship that exists
between a competent adult and an incapacitated adult or a minor
child. The guardian always has the authority to act on his ward’s
capacity and make clinical decisions affecting the ward’s life if
they cannot make similar decisions. It is, however, worth noting
precedence.
What law is applicable for the
protection of children in your state?
Children, Young Persons and their Families Act 1997 (Tas.). this
act provides care and protection for the children and ensure that
they grow in up in environments that are safe and stable.
What are the two codes administered
by the nurses and midwifery Board of
Australia which relate to nursing?
The two codes include the code of conduct and the code of ethics.
Where would you gain information
on what continuing education might
be required for enrolled nurses?
This information can be gained from the Nursing and Midwifery
Board of Australia that requires nurses and midwives take part in
some minimum amount of continuing professional development.
What antidiscrimination laws are
relevant in Australia?
- Disability Discrimination Act 1992
-Sex Discrimination Act 1984
-Racial Discrimination Act 1975
- Age Discrimination Act 2004
What is the legislation in your state
which deals with consent to
treatment?
There are several legislations some of which include the
following;
- Guardianship Act 1987
- Guardianship Regulation 2016
- Children and Young Persons (care and protection) Act 1998
NSW
What is a power of attorney? Power of attorney can be described to mean the authority that an
individual is given to act for another person in a particular
financial or legal matter. In healthcare, the agent to whom you
have granted the power of attorney can make medical decisions for
you if you lose the capacity to do so due to mental incompetence
or lack of conscious.
What is a living will? This is a document that lets an individual state his/her wish for the
end-of-life care in the event that they become unable to
communicate and make decisions regarding their health. This
document only becomes valid after meeting the state’s directive
regarding witnesses and notarization. This document only takes
effect after it has been extensively established that the patient can
no longer make known their wishes regarding a treatment
procedure.
What is guardianship? It can be described as a legally authorized relationship that exists
between a competent adult and an incapacitated adult or a minor
child. The guardian always has the authority to act on his ward’s
capacity and make clinical decisions affecting the ward’s life if
they cannot make similar decisions. It is, however, worth noting
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
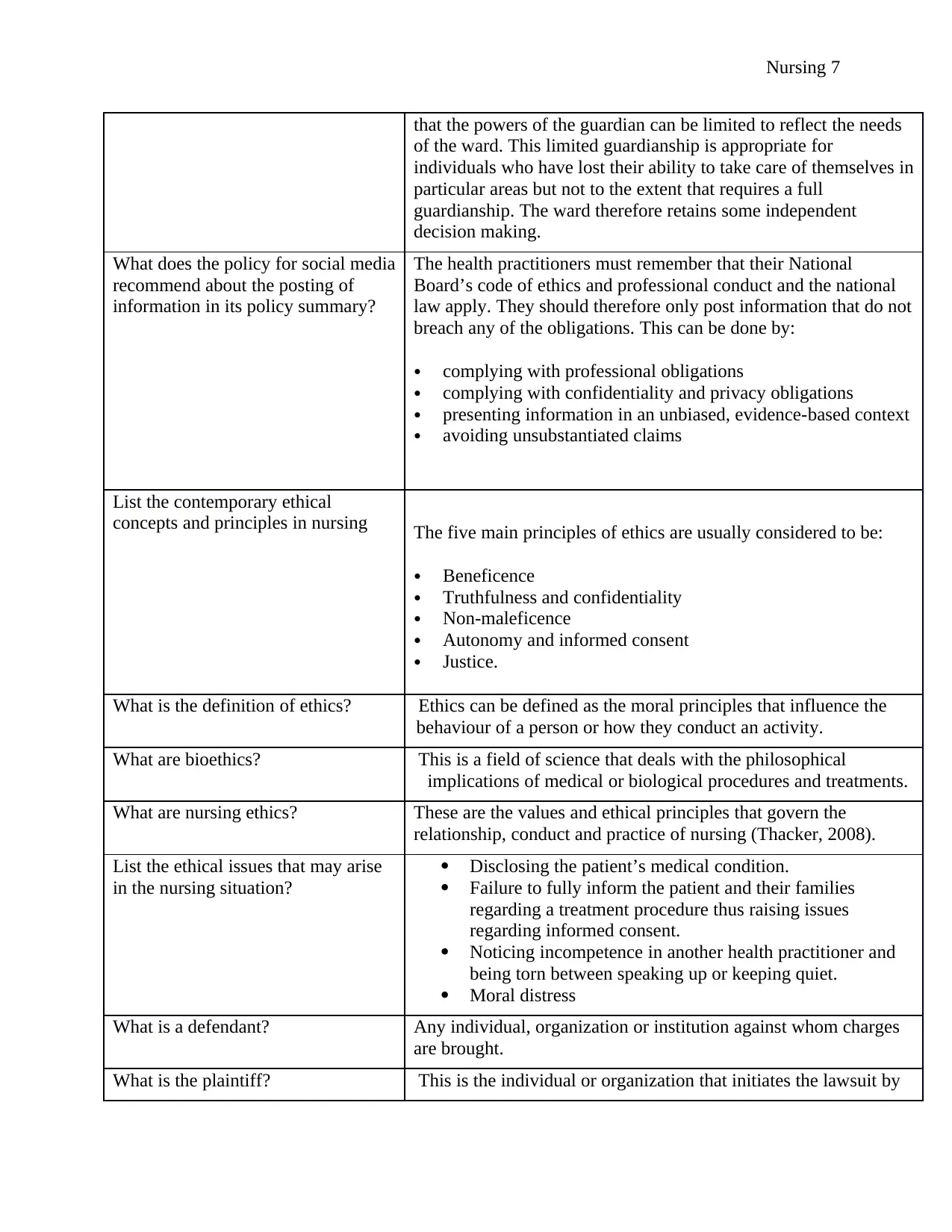
Nursing 7
that the powers of the guardian can be limited to reflect the needs
of the ward. This limited guardianship is appropriate for
individuals who have lost their ability to take care of themselves in
particular areas but not to the extent that requires a full
guardianship. The ward therefore retains some independent
decision making.
What does the policy for social media
recommend about the posting of
information in its policy summary?
The health practitioners must remember that their National
Board’s code of ethics and professional conduct and the national
law apply. They should therefore only post information that do not
breach any of the obligations. This can be done by:
complying with professional obligations
complying with confidentiality and privacy obligations
presenting information in an unbiased, evidence-based context
avoiding unsubstantiated claims
List the contemporary ethical
concepts and principles in nursing The five main principles of ethics are usually considered to be:
Beneficence
Truthfulness and confidentiality
Non-maleficence
Autonomy and informed consent
Justice.
What is the definition of ethics? Ethics can be defined as the moral principles that influence the
behaviour of a person or how they conduct an activity.
What are bioethics? This is a field of science that deals with the philosophical
implications of medical or biological procedures and treatments.
What are nursing ethics? These are the values and ethical principles that govern the
relationship, conduct and practice of nursing (Thacker, 2008).
List the ethical issues that may arise
in the nursing situation?
Disclosing the patient’s medical condition.
Failure to fully inform the patient and their families
regarding a treatment procedure thus raising issues
regarding informed consent.
Noticing incompetence in another health practitioner and
being torn between speaking up or keeping quiet.
Moral distress
What is a defendant? Any individual, organization or institution against whom charges
are brought.
What is the plaintiff? This is the individual or organization that initiates the lawsuit by
that the powers of the guardian can be limited to reflect the needs
of the ward. This limited guardianship is appropriate for
individuals who have lost their ability to take care of themselves in
particular areas but not to the extent that requires a full
guardianship. The ward therefore retains some independent
decision making.
What does the policy for social media
recommend about the posting of
information in its policy summary?
The health practitioners must remember that their National
Board’s code of ethics and professional conduct and the national
law apply. They should therefore only post information that do not
breach any of the obligations. This can be done by:
complying with professional obligations
complying with confidentiality and privacy obligations
presenting information in an unbiased, evidence-based context
avoiding unsubstantiated claims
List the contemporary ethical
concepts and principles in nursing The five main principles of ethics are usually considered to be:
Beneficence
Truthfulness and confidentiality
Non-maleficence
Autonomy and informed consent
Justice.
What is the definition of ethics? Ethics can be defined as the moral principles that influence the
behaviour of a person or how they conduct an activity.
What are bioethics? This is a field of science that deals with the philosophical
implications of medical or biological procedures and treatments.
What are nursing ethics? These are the values and ethical principles that govern the
relationship, conduct and practice of nursing (Thacker, 2008).
List the ethical issues that may arise
in the nursing situation?
Disclosing the patient’s medical condition.
Failure to fully inform the patient and their families
regarding a treatment procedure thus raising issues
regarding informed consent.
Noticing incompetence in another health practitioner and
being torn between speaking up or keeping quiet.
Moral distress
What is a defendant? Any individual, organization or institution against whom charges
are brought.
What is the plaintiff? This is the individual or organization that initiates the lawsuit by
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
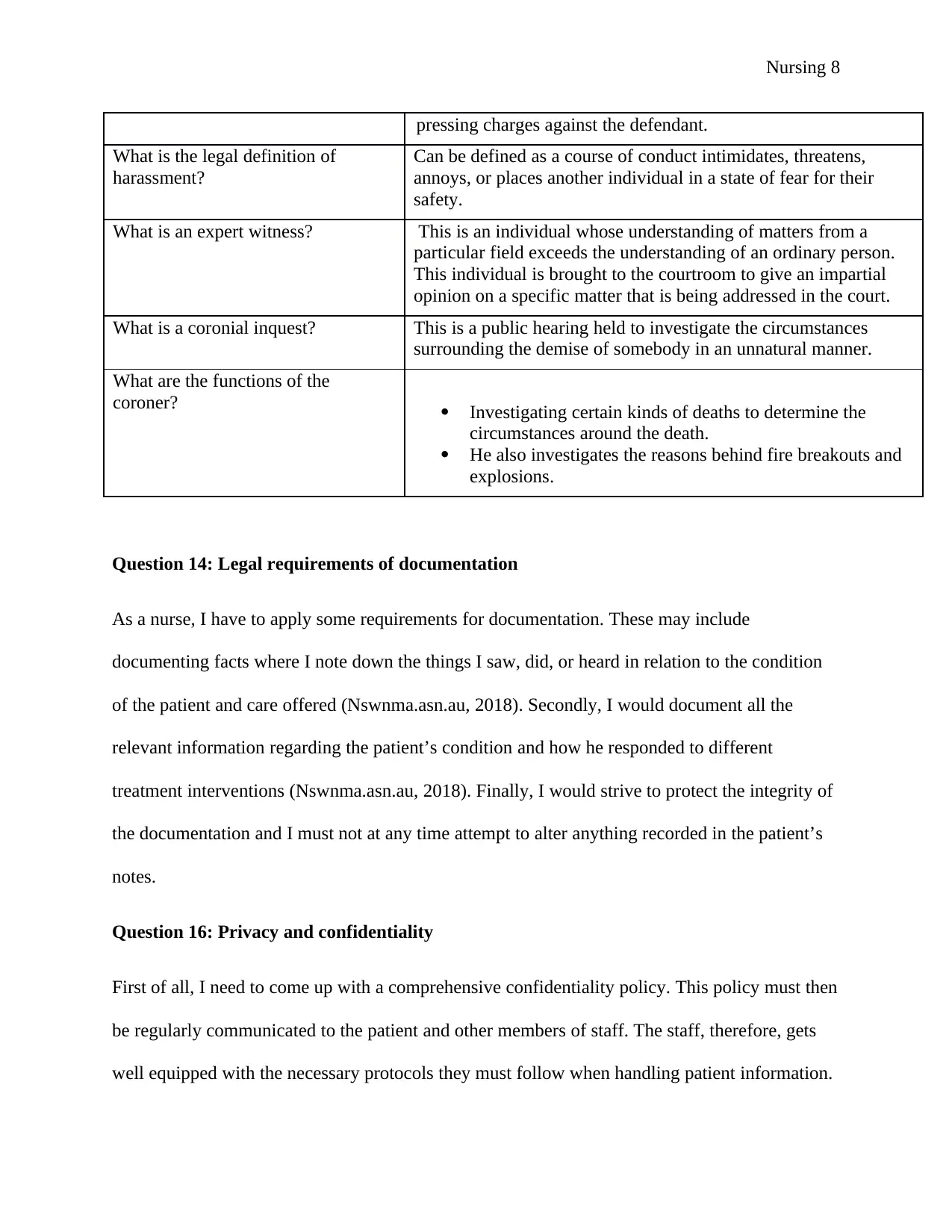
Nursing 8
pressing charges against the defendant.
What is the legal definition of
harassment?
Can be defined as a course of conduct intimidates, threatens,
annoys, or places another individual in a state of fear for their
safety.
What is an expert witness? This is an individual whose understanding of matters from a
particular field exceeds the understanding of an ordinary person.
This individual is brought to the courtroom to give an impartial
opinion on a specific matter that is being addressed in the court.
What is a coronial inquest? This is a public hearing held to investigate the circumstances
surrounding the demise of somebody in an unnatural manner.
What are the functions of the
coroner? Investigating certain kinds of deaths to determine the
circumstances around the death.
He also investigates the reasons behind fire breakouts and
explosions.
Question 14: Legal requirements of documentation
As a nurse, I have to apply some requirements for documentation. These may include
documenting facts where I note down the things I saw, did, or heard in relation to the condition
of the patient and care offered (Nswnma.asn.au, 2018). Secondly, I would document all the
relevant information regarding the patient’s condition and how he responded to different
treatment interventions (Nswnma.asn.au, 2018). Finally, I would strive to protect the integrity of
the documentation and I must not at any time attempt to alter anything recorded in the patient’s
notes.
Question 16: Privacy and confidentiality
First of all, I need to come up with a comprehensive confidentiality policy. This policy must then
be regularly communicated to the patient and other members of staff. The staff, therefore, gets
well equipped with the necessary protocols they must follow when handling patient information.
pressing charges against the defendant.
What is the legal definition of
harassment?
Can be defined as a course of conduct intimidates, threatens,
annoys, or places another individual in a state of fear for their
safety.
What is an expert witness? This is an individual whose understanding of matters from a
particular field exceeds the understanding of an ordinary person.
This individual is brought to the courtroom to give an impartial
opinion on a specific matter that is being addressed in the court.
What is a coronial inquest? This is a public hearing held to investigate the circumstances
surrounding the demise of somebody in an unnatural manner.
What are the functions of the
coroner? Investigating certain kinds of deaths to determine the
circumstances around the death.
He also investigates the reasons behind fire breakouts and
explosions.
Question 14: Legal requirements of documentation
As a nurse, I have to apply some requirements for documentation. These may include
documenting facts where I note down the things I saw, did, or heard in relation to the condition
of the patient and care offered (Nswnma.asn.au, 2018). Secondly, I would document all the
relevant information regarding the patient’s condition and how he responded to different
treatment interventions (Nswnma.asn.au, 2018). Finally, I would strive to protect the integrity of
the documentation and I must not at any time attempt to alter anything recorded in the patient’s
notes.
Question 16: Privacy and confidentiality
First of all, I need to come up with a comprehensive confidentiality policy. This policy must then
be regularly communicated to the patient and other members of staff. The staff, therefore, gets
well equipped with the necessary protocols they must follow when handling patient information.
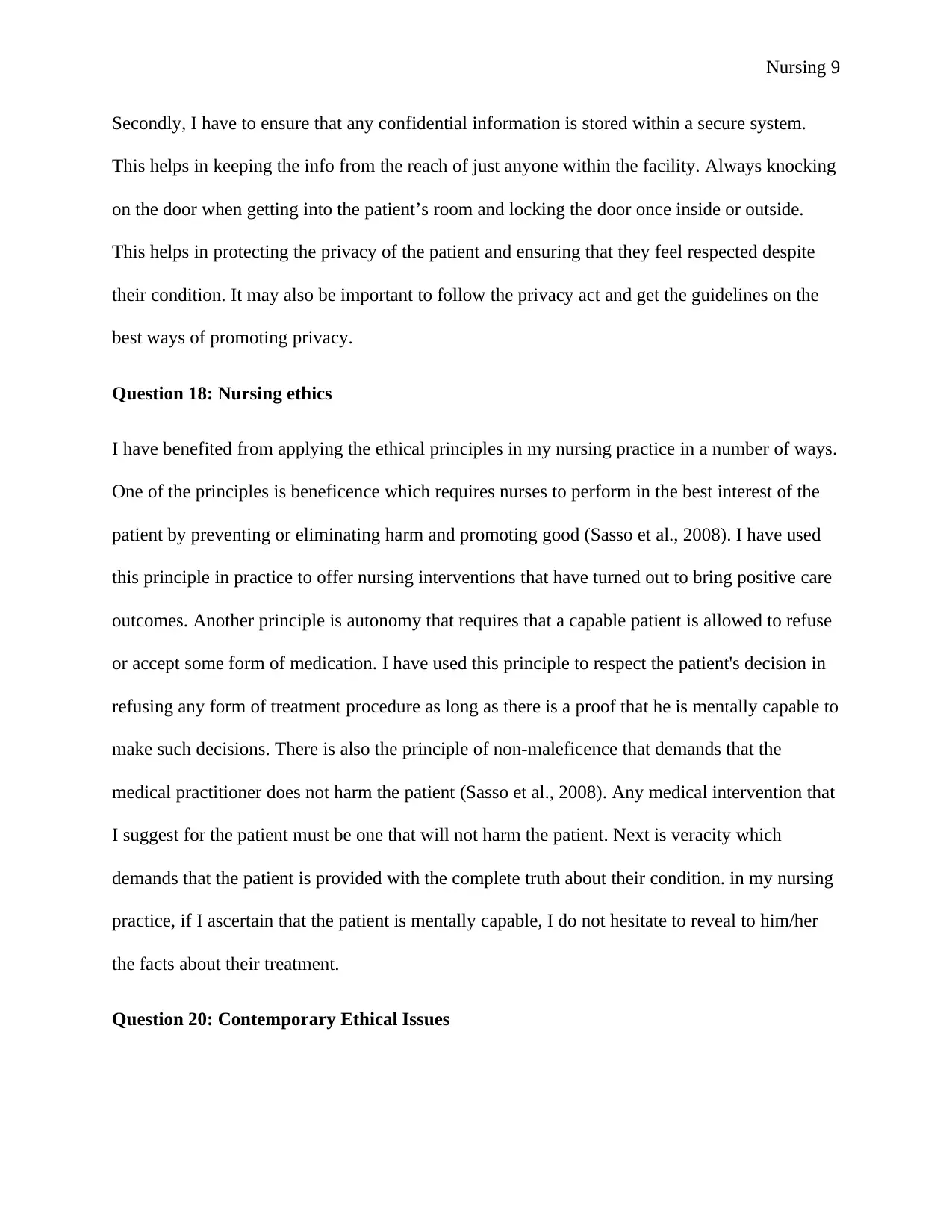
Nursing 9
Secondly, I have to ensure that any confidential information is stored within a secure system.
This helps in keeping the info from the reach of just anyone within the facility. Always knocking
on the door when getting into the patient’s room and locking the door once inside or outside.
This helps in protecting the privacy of the patient and ensuring that they feel respected despite
their condition. It may also be important to follow the privacy act and get the guidelines on the
best ways of promoting privacy.
Question 18: Nursing ethics
I have benefited from applying the ethical principles in my nursing practice in a number of ways.
One of the principles is beneficence which requires nurses to perform in the best interest of the
patient by preventing or eliminating harm and promoting good (Sasso et al., 2008). I have used
this principle in practice to offer nursing interventions that have turned out to bring positive care
outcomes. Another principle is autonomy that requires that a capable patient is allowed to refuse
or accept some form of medication. I have used this principle to respect the patient's decision in
refusing any form of treatment procedure as long as there is a proof that he is mentally capable to
make such decisions. There is also the principle of non-maleficence that demands that the
medical practitioner does not harm the patient (Sasso et al., 2008). Any medical intervention that
I suggest for the patient must be one that will not harm the patient. Next is veracity which
demands that the patient is provided with the complete truth about their condition. in my nursing
practice, if I ascertain that the patient is mentally capable, I do not hesitate to reveal to him/her
the facts about their treatment.
Question 20: Contemporary Ethical Issues
Secondly, I have to ensure that any confidential information is stored within a secure system.
This helps in keeping the info from the reach of just anyone within the facility. Always knocking
on the door when getting into the patient’s room and locking the door once inside or outside.
This helps in protecting the privacy of the patient and ensuring that they feel respected despite
their condition. It may also be important to follow the privacy act and get the guidelines on the
best ways of promoting privacy.
Question 18: Nursing ethics
I have benefited from applying the ethical principles in my nursing practice in a number of ways.
One of the principles is beneficence which requires nurses to perform in the best interest of the
patient by preventing or eliminating harm and promoting good (Sasso et al., 2008). I have used
this principle in practice to offer nursing interventions that have turned out to bring positive care
outcomes. Another principle is autonomy that requires that a capable patient is allowed to refuse
or accept some form of medication. I have used this principle to respect the patient's decision in
refusing any form of treatment procedure as long as there is a proof that he is mentally capable to
make such decisions. There is also the principle of non-maleficence that demands that the
medical practitioner does not harm the patient (Sasso et al., 2008). Any medical intervention that
I suggest for the patient must be one that will not harm the patient. Next is veracity which
demands that the patient is provided with the complete truth about their condition. in my nursing
practice, if I ascertain that the patient is mentally capable, I do not hesitate to reveal to him/her
the facts about their treatment.
Question 20: Contemporary Ethical Issues
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Nursing 10
Contemporary ethical issues may be described as the current topics surrounding ethics in
nursing. These issues requires that the person in charge of the organization to make a choice
between several alternatives and evaluate them as ethical or unethical (Steinbock et al., 2013).
Some of the contemporary ethical issues include;
Disclosing the patient’s medical condition.
Failure to fully inform the patient and their families regarding a treatment procedure thus
raising issues regarding informed consent.
Noticing incompetence in another health practitioner and being torn between speaking up
or keeping quiet.
Question 22: Solving an ethical issue
There are times when an organization faces ethical issues such as disclosing the patient’s
information or even failing to inform the patient and their family regarding the full details of a
particular treatment procedure. When such issues arise, it is best that they are solved swiftly to
prevent escalation and protect the image of the organization. This can be done through
effectively communicating with the individuals responsible. Having a word with him/her them in
private and reminding them of what is expected of them. This communication is further extended
to the other working stuff before a disciplinary action on the person responsible for the mistake
can be initiated. It could also be important to apologize to the offended patient and assure them
that the same can never happen again.
Question 24: Rights of a patient (Uhsystem.com, 2018)
i) Access to care
Contemporary ethical issues may be described as the current topics surrounding ethics in
nursing. These issues requires that the person in charge of the organization to make a choice
between several alternatives and evaluate them as ethical or unethical (Steinbock et al., 2013).
Some of the contemporary ethical issues include;
Disclosing the patient’s medical condition.
Failure to fully inform the patient and their families regarding a treatment procedure thus
raising issues regarding informed consent.
Noticing incompetence in another health practitioner and being torn between speaking up
or keeping quiet.
Question 22: Solving an ethical issue
There are times when an organization faces ethical issues such as disclosing the patient’s
information or even failing to inform the patient and their family regarding the full details of a
particular treatment procedure. When such issues arise, it is best that they are solved swiftly to
prevent escalation and protect the image of the organization. This can be done through
effectively communicating with the individuals responsible. Having a word with him/her them in
private and reminding them of what is expected of them. This communication is further extended
to the other working stuff before a disciplinary action on the person responsible for the mistake
can be initiated. It could also be important to apologize to the offended patient and assure them
that the same can never happen again.
Question 24: Rights of a patient (Uhsystem.com, 2018)
i) Access to care
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nursing 11
All individuals shall be given an impartial access to the available and indicated medical care
irrespective of sex, gender, religion, or sexual orientation among others.
ii) Respect and Dignity
The patient shall be afforded a respectful and considerate care at all times while at the same time
recognizing their dignity and worth.
iii) Privacy and confidentiality
The patient has the right to both personal and information privacy as stipulated by the law.
iv) Personal safety and security
The patient has every right to expect reasonable safety in as long as he/she remains within the
confines of the hospital.
v) Consent
The patient has the right of reasonable participation in decisions regarding his/her health \.
vi) Consultation
The patient has the right to consult a specialist at their own request and expense.
Question 25: Strategies to encourage people to exercise their right to make informed
decisions
I would apply good communication and listening skills to inform the patients, assess their
understanding, and help them in making clear their preferences regarding treatment
interventions. This can be done by providing clear and evidence-based information about the
available options and the likely outcomes. I would further make this easier by telling the patient
All individuals shall be given an impartial access to the available and indicated medical care
irrespective of sex, gender, religion, or sexual orientation among others.
ii) Respect and Dignity
The patient shall be afforded a respectful and considerate care at all times while at the same time
recognizing their dignity and worth.
iii) Privacy and confidentiality
The patient has the right to both personal and information privacy as stipulated by the law.
iv) Personal safety and security
The patient has every right to expect reasonable safety in as long as he/she remains within the
confines of the hospital.
v) Consent
The patient has the right of reasonable participation in decisions regarding his/her health \.
vi) Consultation
The patient has the right to consult a specialist at their own request and expense.
Question 25: Strategies to encourage people to exercise their right to make informed
decisions
I would apply good communication and listening skills to inform the patients, assess their
understanding, and help them in making clear their preferences regarding treatment
interventions. This can be done by providing clear and evidence-based information about the
available options and the likely outcomes. I would further make this easier by telling the patient
Nursing 12
about the benefits, risks, and alternatives to a particular intervention. I would also apply the use
of numbers and graphical illustrations to improve the understanding of the patient.
Question 26: Demonstrating respect and support for Dignity
i) Involving the patient in decisions regarding their health
Involving a patient in decisions regarding their health is important because it makes them feel
valued and connected while at the same time giving them the feeling that their opinion is
respected.
ii) Respecting the patient’s personal space
It is important to always knock and ask for permission before getting into a room of the patient
you are caring for (Lin and Tsai, 2011). Barging into their personal space is inappropriate and
disrespectful.
iii) Promoting social activities
It is important to get the patients involved in social life as it instills them with a sense of
belonging, purpose, and satisfaction which eventually helps in improving the quality of life.
iv) Engaging the patient in friendly chats
Their lives in care may seem boring and uneventful and therefore sparing a few minutes to have
a chat with them can lift their spirits by fulfilling their desire for social interaction (Lin and Tsai,
2011).
v) Properly address the patient
about the benefits, risks, and alternatives to a particular intervention. I would also apply the use
of numbers and graphical illustrations to improve the understanding of the patient.
Question 26: Demonstrating respect and support for Dignity
i) Involving the patient in decisions regarding their health
Involving a patient in decisions regarding their health is important because it makes them feel
valued and connected while at the same time giving them the feeling that their opinion is
respected.
ii) Respecting the patient’s personal space
It is important to always knock and ask for permission before getting into a room of the patient
you are caring for (Lin and Tsai, 2011). Barging into their personal space is inappropriate and
disrespectful.
iii) Promoting social activities
It is important to get the patients involved in social life as it instills them with a sense of
belonging, purpose, and satisfaction which eventually helps in improving the quality of life.
iv) Engaging the patient in friendly chats
Their lives in care may seem boring and uneventful and therefore sparing a few minutes to have
a chat with them can lift their spirits by fulfilling their desire for social interaction (Lin and Tsai,
2011).
v) Properly address the patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





