Holmesglen University: Foundations of Care - Asthma Case Study Report
VerifiedAdded on 2023/06/07
|17
|3856
|408
Case Study
AI Summary
This case study report, focusing on a 70-year-old male patient admitted with acute severe asthma, provides a comprehensive overview of nursing care within the Foundations of Care framework. The report details the patient's presentation, including clinical manifestations, diagnostic findings, and risk assessment, leading to a diagnosis of Acute Severe Asthma. It outlines the severity levels, objective assessments, and nursing interventions, including monitoring vital signs, assessing breathing sounds, and managing ineffective breathing patterns and airways. The plan incorporates nursing diagnoses such as ineffective breathing patterns, ineffective airway clearance, deficient knowledge, and anxiety, with corresponding interventions and desired outcomes. The report emphasizes patient empowerment strategies, psychosocial effects of asthma treatment, and the role of nurses in providing holistic patient care, including medication management, patient education, and collaboration. Furthermore, the report stresses the importance of effective communication, and coping mechanisms in managing asthma, and includes the impact of age and cultural factors on patient outcomes.

University
Task
Name
ASSIGNMENT
Task
Name
ASSIGNMENT
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Foundations of Care
Introduction
Nursing offers a critical opportunity for professionals in this area to enhance and promote
recovery care. This case study report illustrates patient case history, risk assessment, health
care admission, nursing diagnosis, nursing plans of care and nursing role in managing patient
disease state.
Case study
Jackson Smith, an 70-years-old male, admitted to the Emergency Department at 9 pm
with severe breathlessness. He has a history of asthma and he was diagnosed when he was
twenty five years old. On admission to the Emergency Department the clinical manifestations
were assessed as followed:
- Severe dyspnea, inability to speak sentences in one breath
- Respiratory rate of 32 breaths/minute
- SpO2 90%, on room air
- BP 150/85 mmHg
- A pulse rate of 130 beats/minute
- Auscultation of lungs identifies diminished breath sounds and widespread wheeze
A chest x-ray was performed and showed a clear and hyper-inflated lung field.
A blood gas was taken:
pH: 7.35
PaO2: 60mmHg PaCO2: 50mmHg HCO3: 25mEq/L Lactate: 1
SaO2 90%
A diagnosis of Acute Severe Asthma was made.
Patient’s risks assessment
Treatment delay and low dosage in asthma attack often adversely affects outcomes.
2
Introduction
Nursing offers a critical opportunity for professionals in this area to enhance and promote
recovery care. This case study report illustrates patient case history, risk assessment, health
care admission, nursing diagnosis, nursing plans of care and nursing role in managing patient
disease state.
Case study
Jackson Smith, an 70-years-old male, admitted to the Emergency Department at 9 pm
with severe breathlessness. He has a history of asthma and he was diagnosed when he was
twenty five years old. On admission to the Emergency Department the clinical manifestations
were assessed as followed:
- Severe dyspnea, inability to speak sentences in one breath
- Respiratory rate of 32 breaths/minute
- SpO2 90%, on room air
- BP 150/85 mmHg
- A pulse rate of 130 beats/minute
- Auscultation of lungs identifies diminished breath sounds and widespread wheeze
A chest x-ray was performed and showed a clear and hyper-inflated lung field.
A blood gas was taken:
pH: 7.35
PaO2: 60mmHg PaCO2: 50mmHg HCO3: 25mEq/L Lactate: 1
SaO2 90%
A diagnosis of Acute Severe Asthma was made.
Patient’s risks assessment
Treatment delay and low dosage in asthma attack often adversely affects outcomes.
2
Foundations of Care
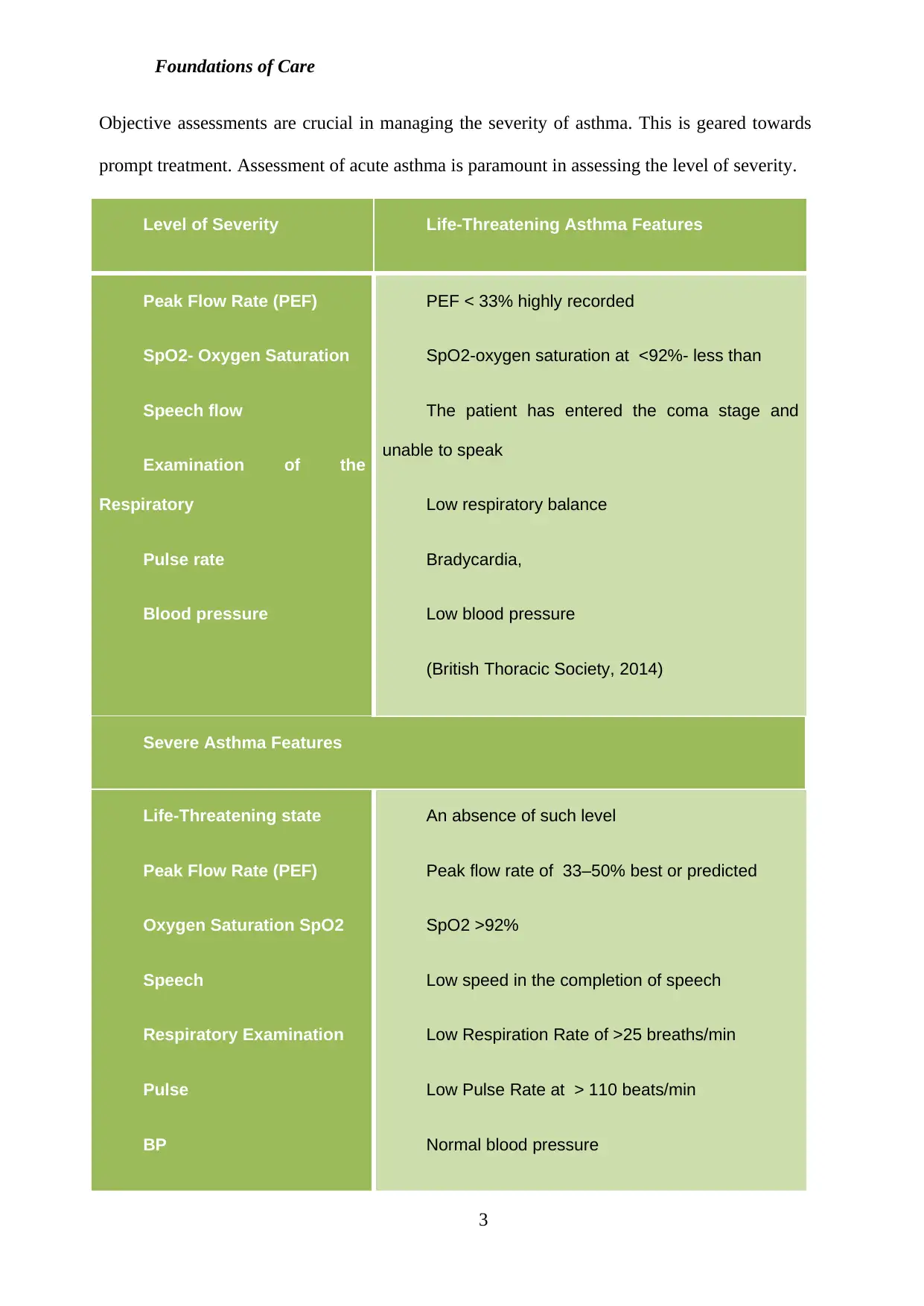
Objective assessments are crucial in managing the severity of asthma. This is geared towards
prompt treatment. Assessment of acute asthma is paramount in assessing the level of severity.
Level of Severity Life-Threatening Asthma Features
Peak Flow Rate (PEF)
SpO2- Oxygen Saturation
Speech flow
Examination of the
Respiratory
Pulse rate
Blood pressure
PEF < 33% highly recorded
SpO2-oxygen saturation at <92%- less than
The patient has entered the coma stage and
unable to speak
Low respiratory balance
Bradycardia,
Low blood pressure
(British Thoracic Society, 2014)
Severe Asthma Features
Life-Threatening state
Peak Flow Rate (PEF)
Oxygen Saturation SpO2
Speech
Respiratory Examination
Pulse
BP
An absence of such level
Peak flow rate of 33–50% best or predicted
SpO2 >92%
Low speed in the completion of speech
Low Respiration Rate of >25 breaths/min
Low Pulse Rate at > 110 beats/min
Normal blood pressure
3
Objective assessments are crucial in managing the severity of asthma. This is geared towards
prompt treatment. Assessment of acute asthma is paramount in assessing the level of severity.
Level of Severity Life-Threatening Asthma Features
Peak Flow Rate (PEF)
SpO2- Oxygen Saturation
Speech flow
Examination of the
Respiratory
Pulse rate
Blood pressure
PEF < 33% highly recorded
SpO2-oxygen saturation at <92%- less than
The patient has entered the coma stage and
unable to speak
Low respiratory balance
Bradycardia,
Low blood pressure
(British Thoracic Society, 2014)
Severe Asthma Features
Life-Threatening state
Peak Flow Rate (PEF)
Oxygen Saturation SpO2
Speech
Respiratory Examination
Pulse
BP
An absence of such level
Peak flow rate of 33–50% best or predicted
SpO2 >92%
Low speed in the completion of speech
Low Respiration Rate of >25 breaths/min
Low Pulse Rate at > 110 beats/min
Normal blood pressure
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Foundations of Care
(British Thoracic Society, 2014)
Objective assessments
Pulse Oximetry
Measuring of oxygen using pulse oximeter aimed at determining oxygen adequacy and
the requirement of measuring arterial blood gas assessment. It is aimed at maintaining the
SpO2 therapy at an estimate of 94%-98%. Among hypoxia patients, it is paramount to assess
another method of offering diagnosis, (Leefebvre et al, 2015).
PEF and PEV1
Assessment of the airway aides in improving the breathing process for the patient while
PEF or PEV1 are important parameters for assessing airway caliber.
Chest X-ray
Routine recommendations are done when there is suspicion of consolidation, non-
response to treatment, life-threatening asthma, and emerging consolidation.
Blood gas
Patients having SpO2 lower than 92%, whether he is on oxygen or not often require ABG
measurement. These assessments are linked to hyper carpenia, (Price et al., 2015).
The intake of inhaled β- agonist during the self-administration is often a good marker for
the severity of the acute attack and being a risk of poor outcome. Priority clinical assessment
for confirming the diagnosis is the assessment of the severity. The appearance of the patient
like the inability to talk, low respiratory rate and decreased heart rate is the basis of severity
clinical assessment. Increase in the pulse rate often is also associated with severe asthma state,
(Irazuzta, Paredes, Pavlicich & Domínguez, 2016).
Nursing intervention and outcome plan
Asthma condition is a lifelong condition which calls for effective self-care management.
4
(British Thoracic Society, 2014)
Objective assessments
Pulse Oximetry
Measuring of oxygen using pulse oximeter aimed at determining oxygen adequacy and
the requirement of measuring arterial blood gas assessment. It is aimed at maintaining the
SpO2 therapy at an estimate of 94%-98%. Among hypoxia patients, it is paramount to assess
another method of offering diagnosis, (Leefebvre et al, 2015).
PEF and PEV1
Assessment of the airway aides in improving the breathing process for the patient while
PEF or PEV1 are important parameters for assessing airway caliber.
Chest X-ray
Routine recommendations are done when there is suspicion of consolidation, non-
response to treatment, life-threatening asthma, and emerging consolidation.
Blood gas
Patients having SpO2 lower than 92%, whether he is on oxygen or not often require ABG
measurement. These assessments are linked to hyper carpenia, (Price et al., 2015).
The intake of inhaled β- agonist during the self-administration is often a good marker for
the severity of the acute attack and being a risk of poor outcome. Priority clinical assessment
for confirming the diagnosis is the assessment of the severity. The appearance of the patient
like the inability to talk, low respiratory rate and decreased heart rate is the basis of severity
clinical assessment. Increase in the pulse rate often is also associated with severe asthma state,
(Irazuzta, Paredes, Pavlicich & Domínguez, 2016).
Nursing intervention and outcome plan
Asthma condition is a lifelong condition which calls for effective self-care management.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Foundations of Care
Practicing nurses often play a crucial role in evaluating and reviewing systematically how the
patients are able to manage their disease state. There are various practices which nurses engage
in managing asthma care. These include medication management, assisting the patients with
inhaler techniques, assisting patients in avoiding asthma through support including smoke
cessation, patients follow up, partnerships collaborations with patients, (Newell, 2015).
At times nurses often encounter patients who meet specialist referral services. The
referral step doesn’t mean that primary care is ineffective but it is a consistent framework,
which is in the best interest of the individual care process, (Nursing & Midwifery Council,
2015).
Effective nursing plans for these patients’ aims at prevention of hypersensitivity,
allergens control, airway maintenance and prevention of reversible complications. Effective
nursing care plans for this patient include;
- Ineffective breathing system
- Ineffective airway
- Deficient knowledge
- Anxiety
Ineffective breathing pattern
This occurs due to inadequate ventilation in the lugs. It is evident by instances of a
cough, dyspnea, nasal fairing, respiratory depth changes, nasal fairing and loss of
consciousness.
Desired outcome
- The patient has a stable breathing pattern which Is able to relax, breath, have
normal respiratory state and lack of dyslexia.
Nursing intervention Rationale
5
Practicing nurses often play a crucial role in evaluating and reviewing systematically how the
patients are able to manage their disease state. There are various practices which nurses engage
in managing asthma care. These include medication management, assisting the patients with
inhaler techniques, assisting patients in avoiding asthma through support including smoke
cessation, patients follow up, partnerships collaborations with patients, (Newell, 2015).
At times nurses often encounter patients who meet specialist referral services. The
referral step doesn’t mean that primary care is ineffective but it is a consistent framework,
which is in the best interest of the individual care process, (Nursing & Midwifery Council,
2015).
Effective nursing plans for these patients’ aims at prevention of hypersensitivity,
allergens control, airway maintenance and prevention of reversible complications. Effective
nursing care plans for this patient include;
- Ineffective breathing system
- Ineffective airway
- Deficient knowledge
- Anxiety
Ineffective breathing pattern
This occurs due to inadequate ventilation in the lugs. It is evident by instances of a
cough, dyspnea, nasal fairing, respiratory depth changes, nasal fairing and loss of
consciousness.
Desired outcome
- The patient has a stable breathing pattern which Is able to relax, breath, have
normal respiratory state and lack of dyslexia.
Nursing intervention Rationale
5
Foundations of Care
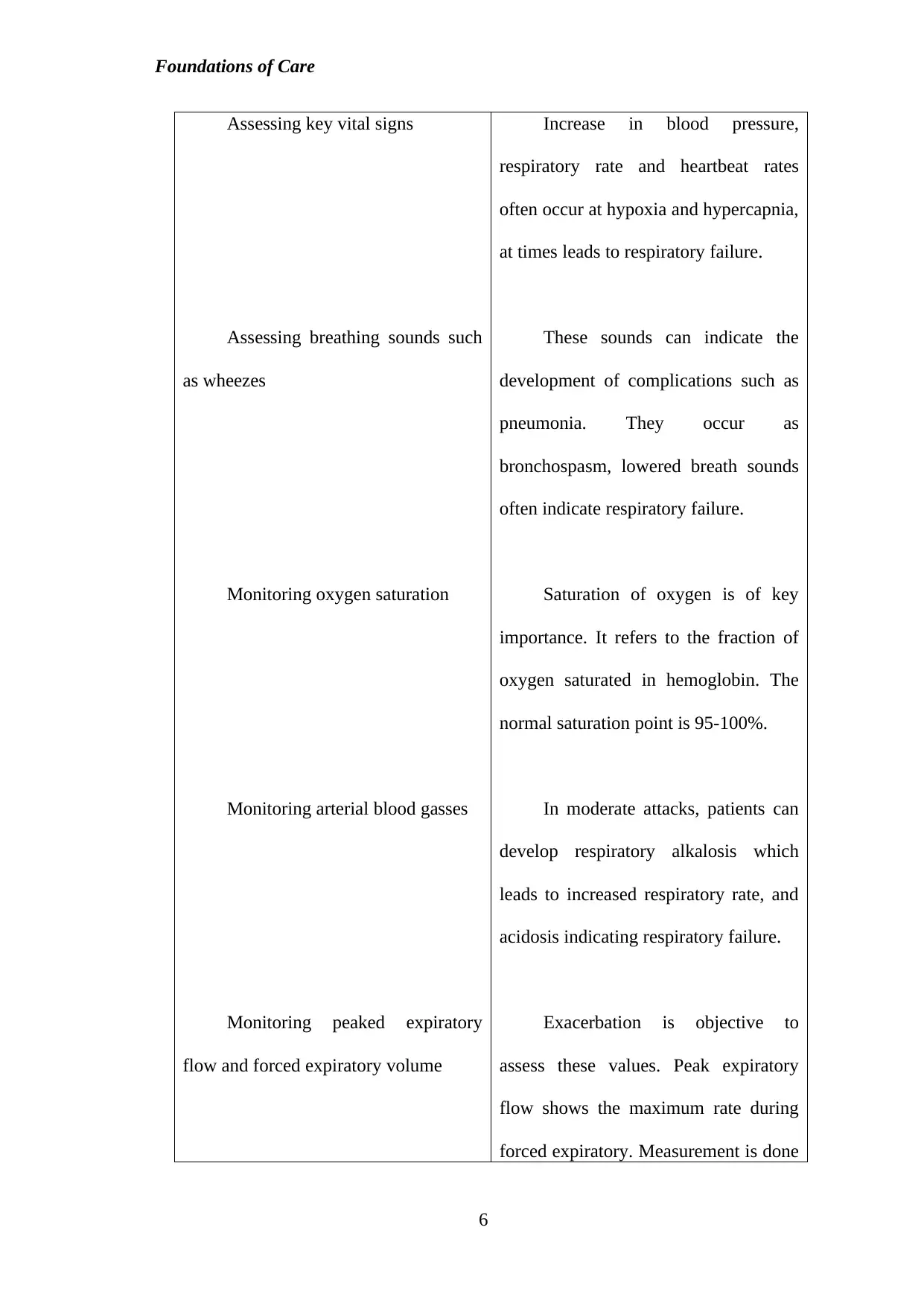
Assessing key vital signs
Assessing breathing sounds such
as wheezes
Monitoring oxygen saturation
Monitoring arterial blood gasses
Monitoring peaked expiratory
flow and forced expiratory volume
Increase in blood pressure,
respiratory rate and heartbeat rates
often occur at hypoxia and hypercapnia,
at times leads to respiratory failure.
These sounds can indicate the
development of complications such as
pneumonia. They occur as
bronchospasm, lowered breath sounds
often indicate respiratory failure.
Saturation of oxygen is of key
importance. It refers to the fraction of
oxygen saturated in hemoglobin. The
normal saturation point is 95-100%.
In moderate attacks, patients can
develop respiratory alkalosis which
leads to increased respiratory rate, and
acidosis indicating respiratory failure.
Exacerbation is objective to
assess these values. Peak expiratory
flow shows the maximum rate during
forced expiratory. Measurement is done
6
Assessing key vital signs
Assessing breathing sounds such
as wheezes
Monitoring oxygen saturation
Monitoring arterial blood gasses
Monitoring peaked expiratory
flow and forced expiratory volume
Increase in blood pressure,
respiratory rate and heartbeat rates
often occur at hypoxia and hypercapnia,
at times leads to respiratory failure.
These sounds can indicate the
development of complications such as
pneumonia. They occur as
bronchospasm, lowered breath sounds
often indicate respiratory failure.
Saturation of oxygen is of key
importance. It refers to the fraction of
oxygen saturated in hemoglobin. The
normal saturation point is 95-100%.
In moderate attacks, patients can
develop respiratory alkalosis which
leads to increased respiratory rate, and
acidosis indicating respiratory failure.
Exacerbation is objective to
assess these values. Peak expiratory
flow shows the maximum rate during
forced expiratory. Measurement is done
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Foundations of Care
in liters, it coordinates with the forced
expiratory volume per second, which
offers a measure of airway obstruction.
(Villa‐Roel et al., 2016)
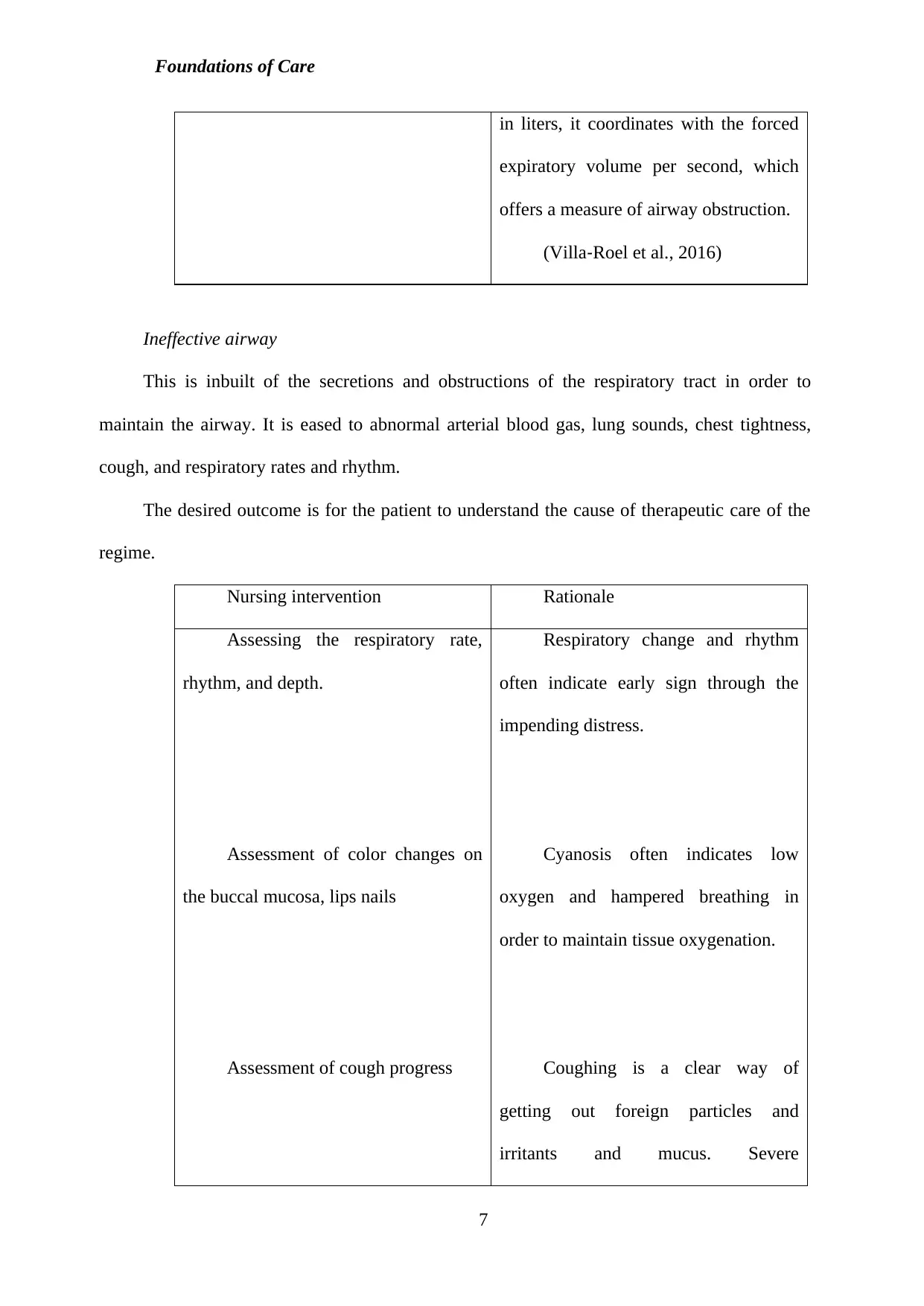
Ineffective airway
This is inbuilt of the secretions and obstructions of the respiratory tract in order to
maintain the airway. It is eased to abnormal arterial blood gas, lung sounds, chest tightness,
cough, and respiratory rates and rhythm.
The desired outcome is for the patient to understand the cause of therapeutic care of the
regime.
Nursing intervention Rationale
Assessing the respiratory rate,
rhythm, and depth.
Assessment of color changes on
the buccal mucosa, lips nails
Assessment of cough progress
Respiratory change and rhythm
often indicate early sign through the
impending distress.
Cyanosis often indicates low
oxygen and hampered breathing in
order to maintain tissue oxygenation.
Coughing is a clear way of
getting out foreign particles and
irritants and mucus. Severe
7
in liters, it coordinates with the forced
expiratory volume per second, which
offers a measure of airway obstruction.
(Villa‐Roel et al., 2016)
Ineffective airway
This is inbuilt of the secretions and obstructions of the respiratory tract in order to
maintain the airway. It is eased to abnormal arterial blood gas, lung sounds, chest tightness,
cough, and respiratory rates and rhythm.
The desired outcome is for the patient to understand the cause of therapeutic care of the
regime.
Nursing intervention Rationale
Assessing the respiratory rate,
rhythm, and depth.
Assessment of color changes on
the buccal mucosa, lips nails
Assessment of cough progress
Respiratory change and rhythm
often indicate early sign through the
impending distress.
Cyanosis often indicates low
oxygen and hampered breathing in
order to maintain tissue oxygenation.
Coughing is a clear way of
getting out foreign particles and
irritants and mucus. Severe
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Foundations of Care
Monitoring chest x-rays
bronchospasm hampers an ineffective
cough.
Chest assessments offer
information on infiltrates, inflation of
lungs and presence.
(Davidson et al., 2016)
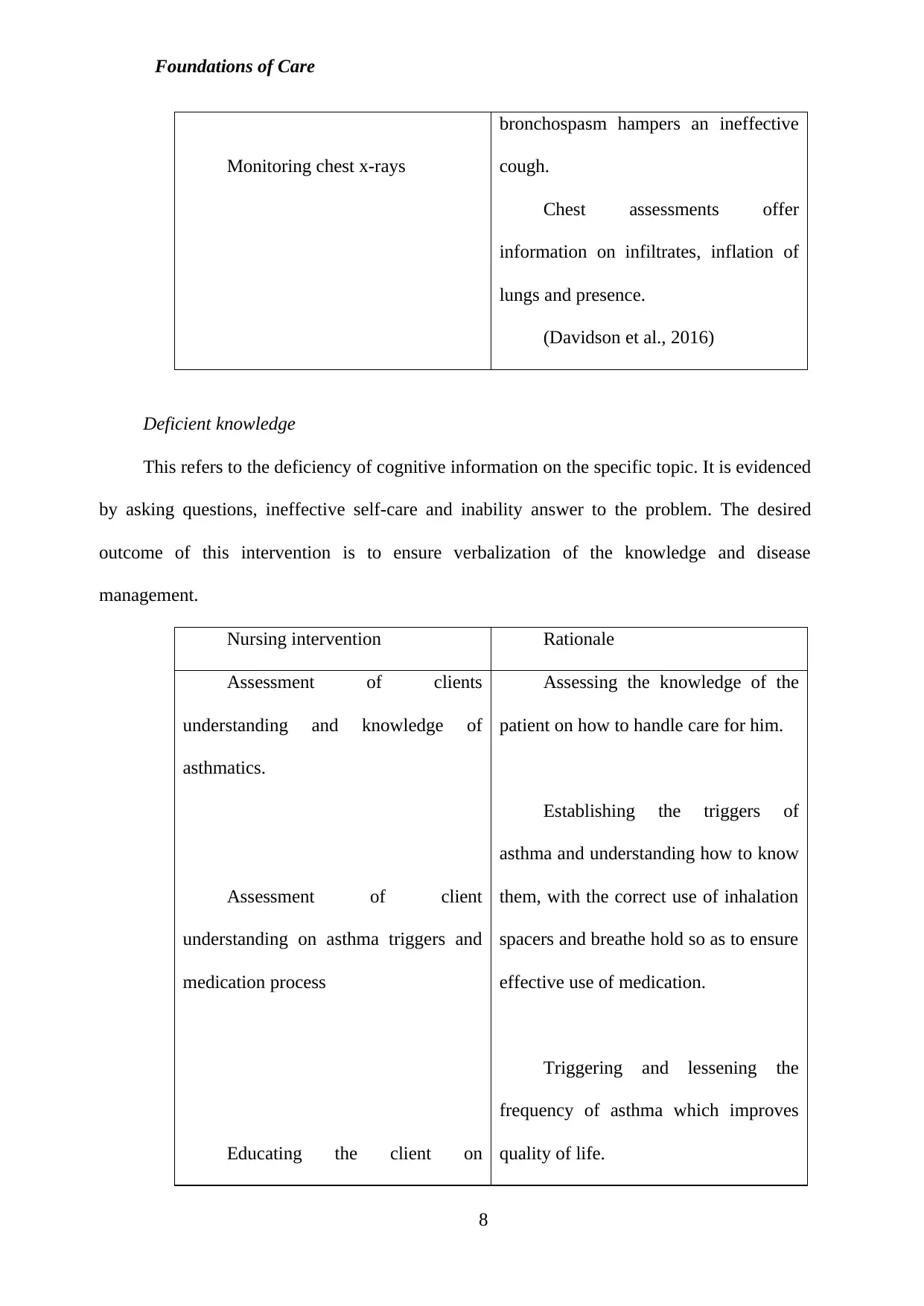
Deficient knowledge
This refers to the deficiency of cognitive information on the specific topic. It is evidenced
by asking questions, ineffective self-care and inability answer to the problem. The desired
outcome of this intervention is to ensure verbalization of the knowledge and disease
management.
Nursing intervention Rationale
Assessment of clients
understanding and knowledge of
asthmatics.
Assessment of client
understanding on asthma triggers and
medication process
Educating the client on
Assessing the knowledge of the
patient on how to handle care for him.
Establishing the triggers of
asthma and understanding how to know
them, with the correct use of inhalation
spacers and breathe hold so as to ensure
effective use of medication.
Triggering and lessening the
frequency of asthma which improves
quality of life.
8
Monitoring chest x-rays
bronchospasm hampers an ineffective
cough.
Chest assessments offer
information on infiltrates, inflation of
lungs and presence.
(Davidson et al., 2016)
Deficient knowledge
This refers to the deficiency of cognitive information on the specific topic. It is evidenced
by asking questions, ineffective self-care and inability answer to the problem. The desired
outcome of this intervention is to ensure verbalization of the knowledge and disease
management.
Nursing intervention Rationale
Assessment of clients
understanding and knowledge of
asthmatics.
Assessment of client
understanding on asthma triggers and
medication process
Educating the client on
Assessing the knowledge of the
patient on how to handle care for him.
Establishing the triggers of
asthma and understanding how to know
them, with the correct use of inhalation
spacers and breathe hold so as to ensure
effective use of medication.
Triggering and lessening the
frequency of asthma which improves
quality of life.
8
Foundations of Care
eradicating allergens such as smoke,
exercise, air pollution, and allergens.
Long-term care for managing
issues
Controlling allergens, avoiding
precipitators, environmental control and
avoiding air pollutants preventing the
occurrence of asthma attacks.
(Davidson et al., 2016)
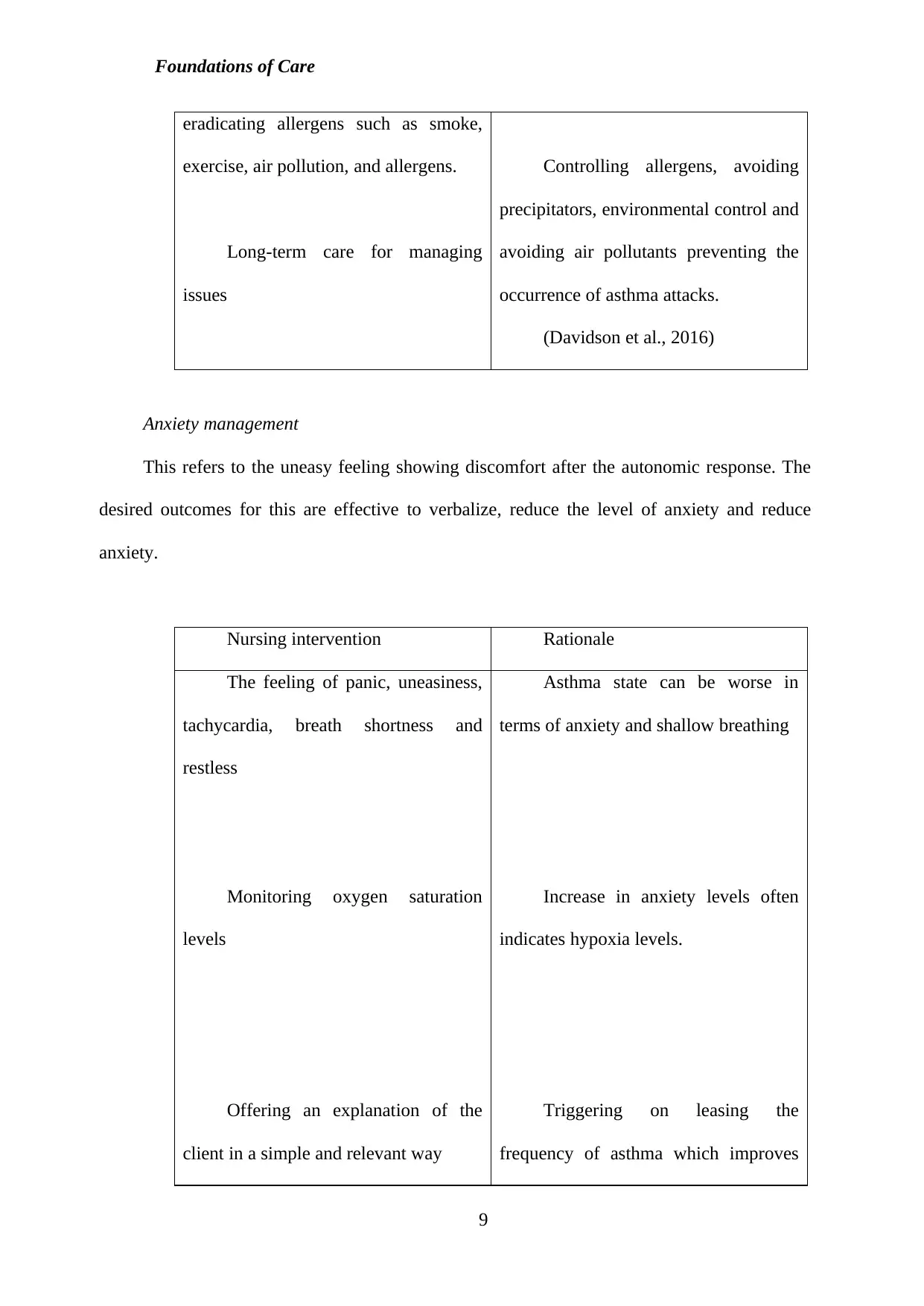
Anxiety management
This refers to the uneasy feeling showing discomfort after the autonomic response. The
desired outcomes for this are effective to verbalize, reduce the level of anxiety and reduce
anxiety.
Nursing intervention Rationale
The feeling of panic, uneasiness,
tachycardia, breath shortness and
restless
Monitoring oxygen saturation
levels
Offering an explanation of the
client in a simple and relevant way
Asthma state can be worse in
terms of anxiety and shallow breathing
Increase in anxiety levels often
indicates hypoxia levels.
Triggering on leasing the
frequency of asthma which improves
9
eradicating allergens such as smoke,
exercise, air pollution, and allergens.
Long-term care for managing
issues
Controlling allergens, avoiding
precipitators, environmental control and
avoiding air pollutants preventing the
occurrence of asthma attacks.
(Davidson et al., 2016)
Anxiety management
This refers to the uneasy feeling showing discomfort after the autonomic response. The
desired outcomes for this are effective to verbalize, reduce the level of anxiety and reduce
anxiety.
Nursing intervention Rationale
The feeling of panic, uneasiness,
tachycardia, breath shortness and
restless
Monitoring oxygen saturation
levels
Offering an explanation of the
client in a simple and relevant way
Asthma state can be worse in
terms of anxiety and shallow breathing
Increase in anxiety levels often
indicates hypoxia levels.
Triggering on leasing the
frequency of asthma which improves
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
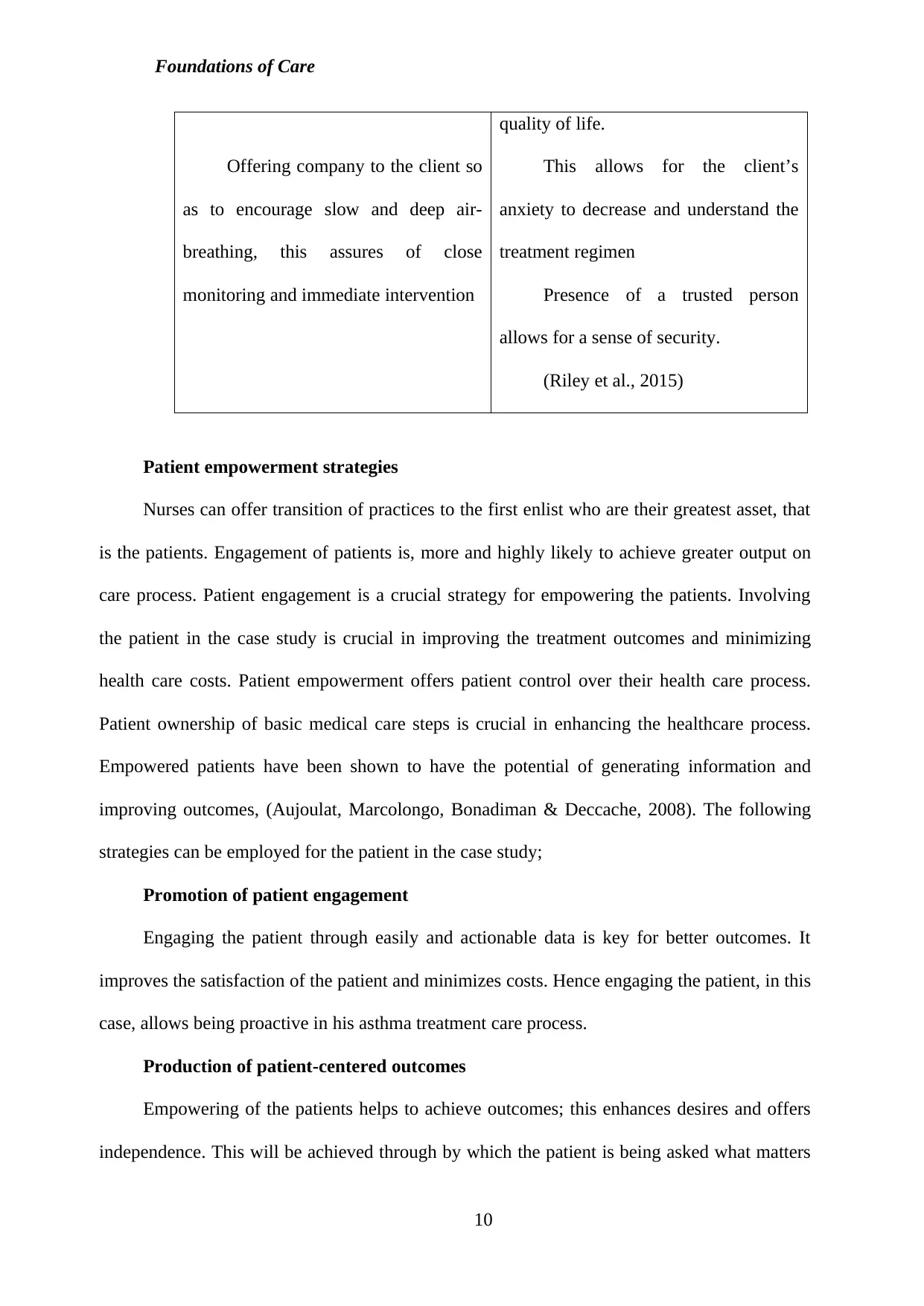
Foundations of Care
Offering company to the client so
as to encourage slow and deep air-
breathing, this assures of close
monitoring and immediate intervention
quality of life.
This allows for the client’s
anxiety to decrease and understand the
treatment regimen
Presence of a trusted person
allows for a sense of security.
(Riley et al., 2015)
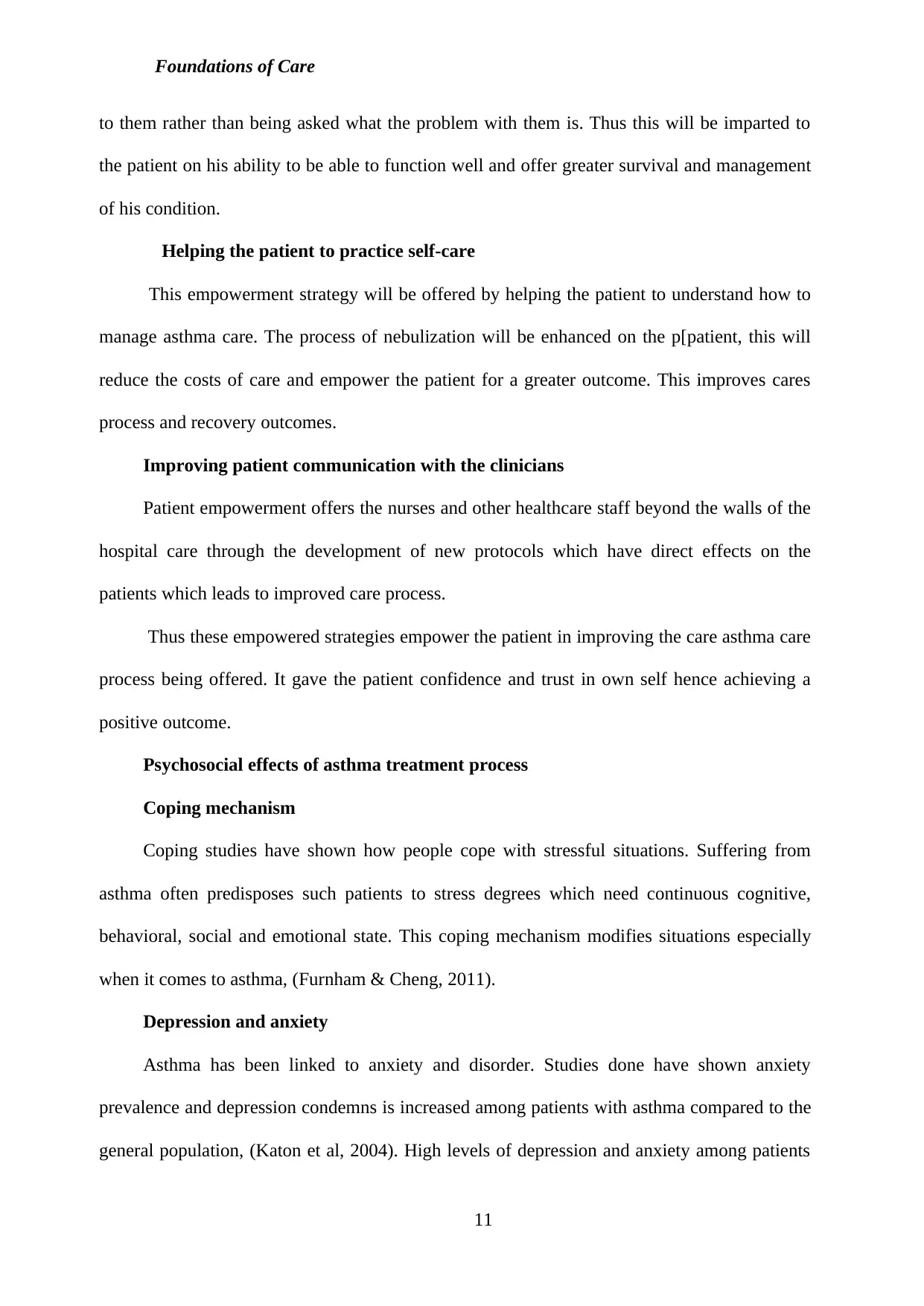
Patient empowerment strategies
Nurses can offer transition of practices to the first enlist who are their greatest asset, that
is the patients. Engagement of patients is, more and highly likely to achieve greater output on
care process. Patient engagement is a crucial strategy for empowering the patients. Involving
the patient in the case study is crucial in improving the treatment outcomes and minimizing
health care costs. Patient empowerment offers patient control over their health care process.
Patient ownership of basic medical care steps is crucial in enhancing the healthcare process.
Empowered patients have been shown to have the potential of generating information and
improving outcomes, (Aujoulat, Marcolongo, Bonadiman & Deccache, 2008). The following
strategies can be employed for the patient in the case study;
Promotion of patient engagement
Engaging the patient through easily and actionable data is key for better outcomes. It
improves the satisfaction of the patient and minimizes costs. Hence engaging the patient, in this
case, allows being proactive in his asthma treatment care process.
Production of patient-centered outcomes
Empowering of the patients helps to achieve outcomes; this enhances desires and offers
independence. This will be achieved through by which the patient is being asked what matters
10
Offering company to the client so
as to encourage slow and deep air-
breathing, this assures of close
monitoring and immediate intervention
quality of life.
This allows for the client’s
anxiety to decrease and understand the
treatment regimen
Presence of a trusted person
allows for a sense of security.
(Riley et al., 2015)
Patient empowerment strategies
Nurses can offer transition of practices to the first enlist who are their greatest asset, that
is the patients. Engagement of patients is, more and highly likely to achieve greater output on
care process. Patient engagement is a crucial strategy for empowering the patients. Involving
the patient in the case study is crucial in improving the treatment outcomes and minimizing
health care costs. Patient empowerment offers patient control over their health care process.
Patient ownership of basic medical care steps is crucial in enhancing the healthcare process.
Empowered patients have been shown to have the potential of generating information and
improving outcomes, (Aujoulat, Marcolongo, Bonadiman & Deccache, 2008). The following
strategies can be employed for the patient in the case study;
Promotion of patient engagement
Engaging the patient through easily and actionable data is key for better outcomes. It
improves the satisfaction of the patient and minimizes costs. Hence engaging the patient, in this
case, allows being proactive in his asthma treatment care process.
Production of patient-centered outcomes
Empowering of the patients helps to achieve outcomes; this enhances desires and offers
independence. This will be achieved through by which the patient is being asked what matters
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Foundations of Care
to them rather than being asked what the problem with them is. Thus this will be imparted to
the patient on his ability to be able to function well and offer greater survival and management
of his condition.
Helping the patient to practice self-care
This empowerment strategy will be offered by helping the patient to understand how to
manage asthma care. The process of nebulization will be enhanced on the p[patient, this will
reduce the costs of care and empower the patient for a greater outcome. This improves cares
process and recovery outcomes.
Improving patient communication with the clinicians
Patient empowerment offers the nurses and other healthcare staff beyond the walls of the
hospital care through the development of new protocols which have direct effects on the
patients which leads to improved care process.
Thus these empowered strategies empower the patient in improving the care asthma care
process being offered. It gave the patient confidence and trust in own self hence achieving a
positive outcome.
Psychosocial effects of asthma treatment process
Coping mechanism
Coping studies have shown how people cope with stressful situations. Suffering from
asthma often predisposes such patients to stress degrees which need continuous cognitive,
behavioral, social and emotional state. This coping mechanism modifies situations especially
when it comes to asthma, (Furnham & Cheng, 2011).
Depression and anxiety
Asthma has been linked to anxiety and disorder. Studies done have shown anxiety
prevalence and depression condemns is increased among patients with asthma compared to the
general population, (Katon et al, 2004). High levels of depression and anxiety among patients
11
to them rather than being asked what the problem with them is. Thus this will be imparted to
the patient on his ability to be able to function well and offer greater survival and management
of his condition.
Helping the patient to practice self-care
This empowerment strategy will be offered by helping the patient to understand how to
manage asthma care. The process of nebulization will be enhanced on the p[patient, this will
reduce the costs of care and empower the patient for a greater outcome. This improves cares
process and recovery outcomes.
Improving patient communication with the clinicians
Patient empowerment offers the nurses and other healthcare staff beyond the walls of the
hospital care through the development of new protocols which have direct effects on the
patients which leads to improved care process.
Thus these empowered strategies empower the patient in improving the care asthma care
process being offered. It gave the patient confidence and trust in own self hence achieving a
positive outcome.
Psychosocial effects of asthma treatment process
Coping mechanism
Coping studies have shown how people cope with stressful situations. Suffering from
asthma often predisposes such patients to stress degrees which need continuous cognitive,
behavioral, social and emotional state. This coping mechanism modifies situations especially
when it comes to asthma, (Furnham & Cheng, 2011).
Depression and anxiety
Asthma has been linked to anxiety and disorder. Studies done have shown anxiety
prevalence and depression condemns is increased among patients with asthma compared to the
general population, (Katon et al, 2004). High levels of depression and anxiety among patients
11
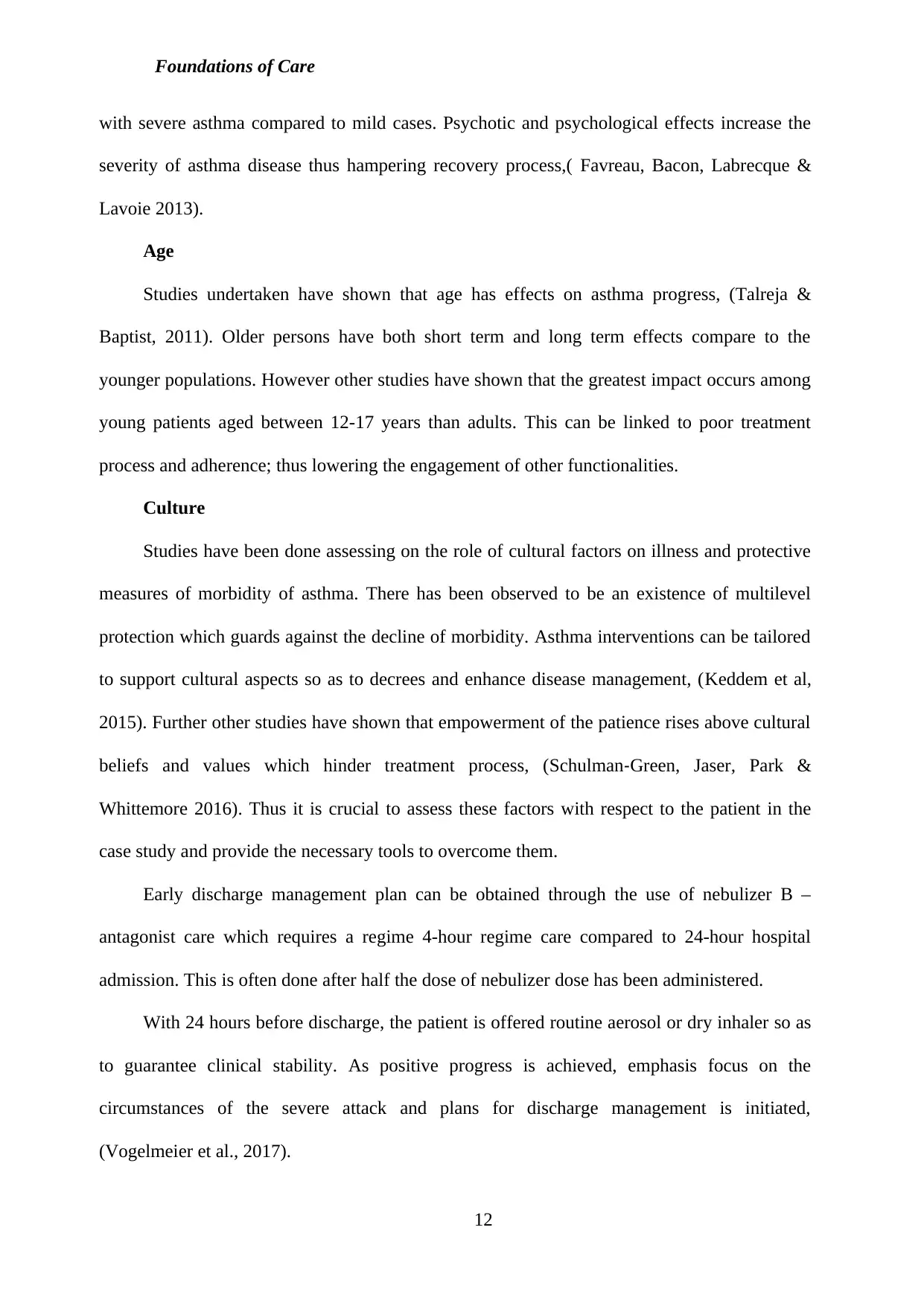
Foundations of Care
with severe asthma compared to mild cases. Psychotic and psychological effects increase the
severity of asthma disease thus hampering recovery process,( Favreau, Bacon, Labrecque &
Lavoie 2013).
Age
Studies undertaken have shown that age has effects on asthma progress, (Talreja &
Baptist, 2011). Older persons have both short term and long term effects compare to the
younger populations. However other studies have shown that the greatest impact occurs among
young patients aged between 12-17 years than adults. This can be linked to poor treatment
process and adherence; thus lowering the engagement of other functionalities.
Culture
Studies have been done assessing on the role of cultural factors on illness and protective
measures of morbidity of asthma. There has been observed to be an existence of multilevel
protection which guards against the decline of morbidity. Asthma interventions can be tailored
to support cultural aspects so as to decrees and enhance disease management, (Keddem et al,
2015). Further other studies have shown that empowerment of the patience rises above cultural
beliefs and values which hinder treatment process, (Schulman‐Green, Jaser, Park &
Whittemore 2016). Thus it is crucial to assess these factors with respect to the patient in the
case study and provide the necessary tools to overcome them.
Early discharge management plan can be obtained through the use of nebulizer B –
antagonist care which requires a regime 4-hour regime care compared to 24-hour hospital
admission. This is often done after half the dose of nebulizer dose has been administered.
With 24 hours before discharge, the patient is offered routine aerosol or dry inhaler so as
to guarantee clinical stability. As positive progress is achieved, emphasis focus on the
circumstances of the severe attack and plans for discharge management is initiated,
(Vogelmeier et al., 2017).
12
with severe asthma compared to mild cases. Psychotic and psychological effects increase the
severity of asthma disease thus hampering recovery process,( Favreau, Bacon, Labrecque &
Lavoie 2013).
Age
Studies undertaken have shown that age has effects on asthma progress, (Talreja &
Baptist, 2011). Older persons have both short term and long term effects compare to the
younger populations. However other studies have shown that the greatest impact occurs among
young patients aged between 12-17 years than adults. This can be linked to poor treatment
process and adherence; thus lowering the engagement of other functionalities.
Culture
Studies have been done assessing on the role of cultural factors on illness and protective
measures of morbidity of asthma. There has been observed to be an existence of multilevel
protection which guards against the decline of morbidity. Asthma interventions can be tailored
to support cultural aspects so as to decrees and enhance disease management, (Keddem et al,
2015). Further other studies have shown that empowerment of the patience rises above cultural
beliefs and values which hinder treatment process, (Schulman‐Green, Jaser, Park &
Whittemore 2016). Thus it is crucial to assess these factors with respect to the patient in the
case study and provide the necessary tools to overcome them.
Early discharge management plan can be obtained through the use of nebulizer B –
antagonist care which requires a regime 4-hour regime care compared to 24-hour hospital
admission. This is often done after half the dose of nebulizer dose has been administered.
With 24 hours before discharge, the patient is offered routine aerosol or dry inhaler so as
to guarantee clinical stability. As positive progress is achieved, emphasis focus on the
circumstances of the severe attack and plans for discharge management is initiated,
(Vogelmeier et al., 2017).
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





